Adherence to Mediterranean Diet in Croatia: Lessons Learned Today for a Brighter Tomorrow
Abstract
:1. Introduction
2. Materials and Methods
2.1. Ethics
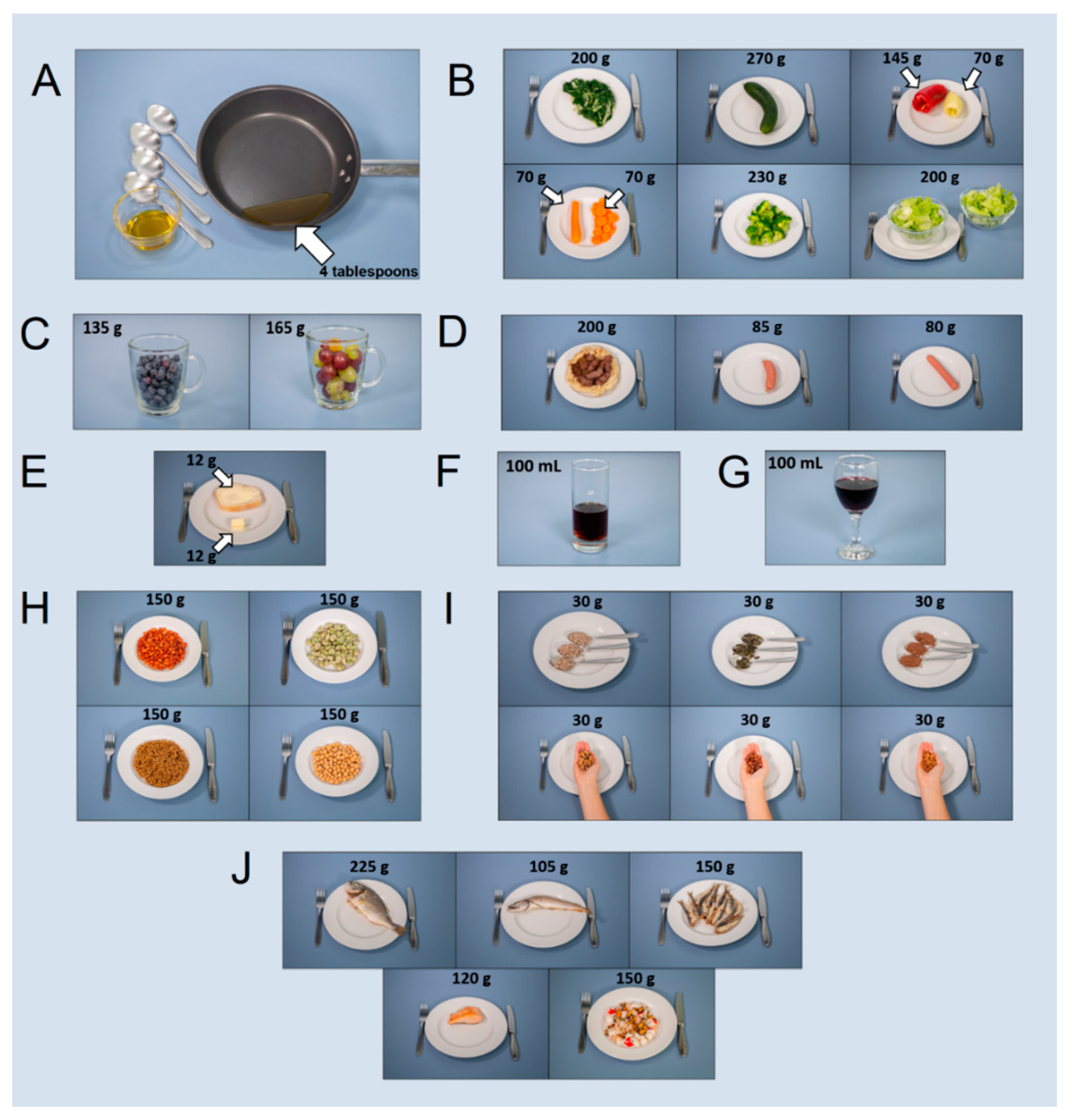
2.2. Mediterranean Diet Adherence Questionnaire, Its Refinement, and Adaptation for Online Use
2.3. Study Population
2.4. Price Assessment for MedD
2.5. Statistical Analysis
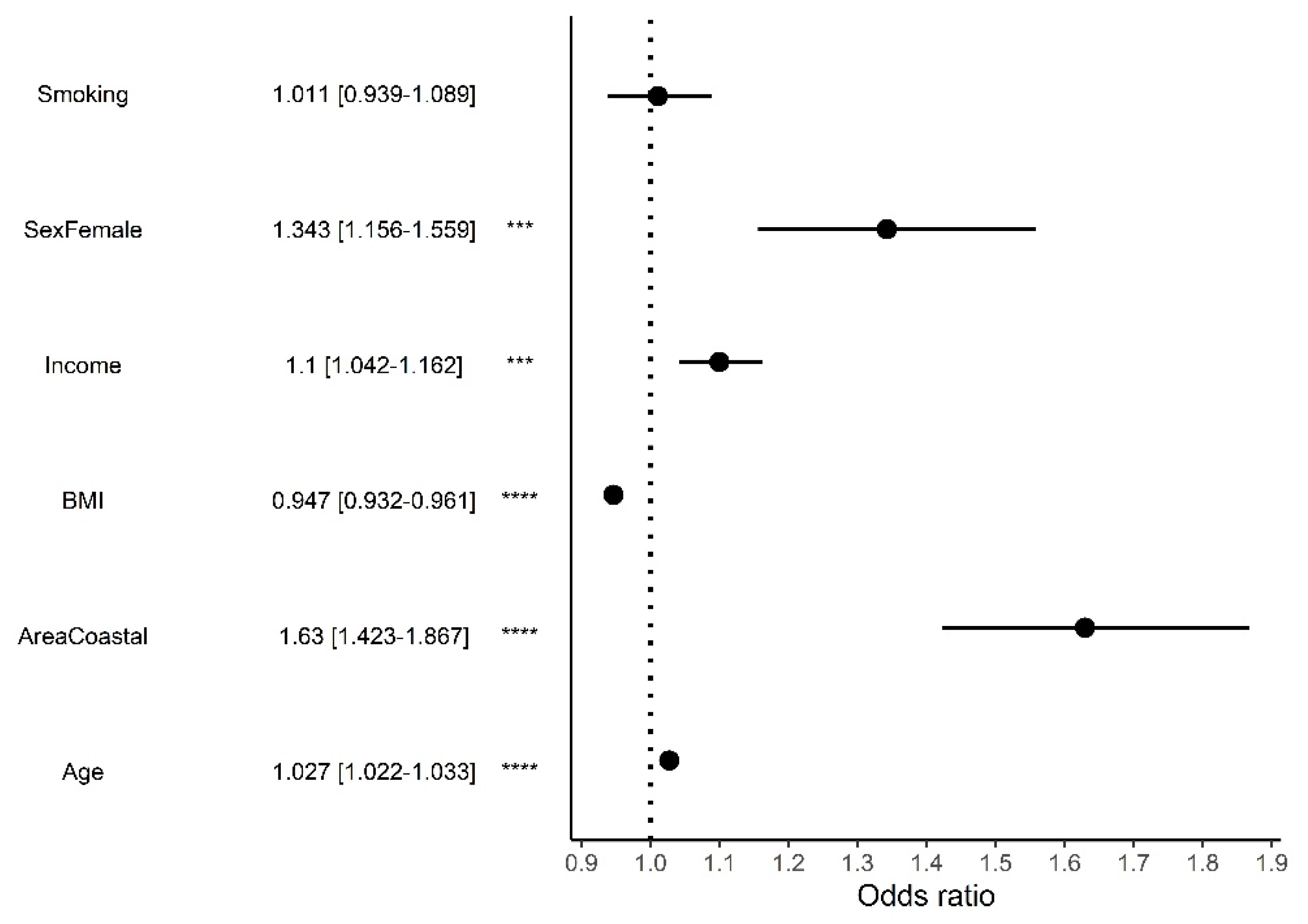
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- WHO. Global Health Estimates 2020: Deaths by Cause, Age, Sex, by Country and by Region, 2000–2019; WHO: Geneva, Switzerland, 2020. [Google Scholar]
- Ritchie, H.; Roser, M. Causes of Death—Our World in Data. Available online: https://ourworldindata.org/causes-of-death#citation (accessed on 11 May 2022).
- Poirier, P.; Giles, T.D.; Bray, G.A.; Hong, Y.; Stern, J.S.; Pi-Sunyer, F.X.; Eckel, R.H. Obesity and Cardiovascular Disease: Pathophysiology, Evaluation, and Effect of Weight Loss: An Update of the 1997 American Heart Association Scientific Statement on Obesity and Heart Disease from the Obesity Committee of the Council on Nutrition, Physical. Circulation 2006, 113, 898–918. [Google Scholar] [CrossRef] [PubMed]
- D’Agostino, R.B.; Vasan, R.S.; Pencina, M.J.; Wolf, P.A.; Cobain, M.; Massaro, J.M.; Kannel, W.B. General Cardiovascular Risk Profile for Use in Primary Care: The Framingham Heart Study. Circulation 2008, 117, 743–753. [Google Scholar] [CrossRef] [PubMed]
- Lim, S.S.; Vos, T.; Flaxman, A.D.; Danaei, G.; Shibuya, K.; Adair-Rohani, H.; Amann, M.; Anderson, H.R.; Andrews, K.G.; Aryee, M.; et al. A Comparative Risk Assessment of Burden of Disease and Injury Attributable to 67 Risk Factors and Risk Factor Clusters in 21 Regions, 1990-2010: A Systematic Analysis for the Global Burden of Disease Study 2010. Lancet 2012, 380, 2224–2260. [Google Scholar] [CrossRef]
- Achilleos, S.; Quattrocchi, A.; Gabel, J.; Heraclides, A.; Kolokotroni, O.; Constantinou, C.; Ugarte, M.P.; Nicolaou, N.; Rodriguez-Llanes, J.M.; Bennett, C.M.; et al. Excess All-Cause Mortality and COVID-19-Related Mortality: A Temporal Analysis in 22 Countries, from January until August 2020. Int. J. Epidemiol. 2022, 51, 35–53. [Google Scholar] [CrossRef]
- Williamson, E.J.; Walker, A.J.; Bhaskaran, K.; Bacon, S.; Bates, C.; Morton, C.E.; Curtis, H.J.; Mehrkar, A.; Evans, D.; Inglesby, P.; et al. Factors Associated with COVID-19-Related Death Using OpenSAFELY. Nature 2020, 584, 430–436. [Google Scholar] [CrossRef]
- Richardson, S.; Hirsch, J.S.; Narasimhan, M.; Crawford, J.M.; McGinn, T.; Davidson, K.W.; Barnaby, D.P.; Becker, L.B.; Chelico, J.D.; Cohen, S.L.; et al. Presenting Characteristics, Comorbidities, and Outcomes among 5700 Patients Hospitalized with COVID-19 in the New York City Area. JAMA 2020, 323, 2052–2059. [Google Scholar] [CrossRef] [PubMed]
- EUROSTAT Overweight and Obesity—BMI Statistics—Statistics Explained. 2021. Available online: https://ec.europa.eu/eurostat/statistics-explained/index.php?title=Overweight_and_obesity_-_BMI_statistics (accessed on 25 April 2022).
- Di Cesare, M.; Bentham, J.; Stevens, G.A.; Zhou, B.; Danaei, G.; Lu, Y.; Bixby, H.; Cowan, M.J.; Riley, L.M.; Hajifathalian, K.; et al. Trends in Adult Body-Mass Index in 200 Countries from 1975 to 2014: A Pooled Analysis of 1698 Population-Based Measurement Studies with 19.2 Million Participants. Lancet 2016, 387, 1377–1396. [Google Scholar] [CrossRef]
- Milanović, S.M.; Morović, M.L.; Bukal, D.; Križan, H.; Buoncristiano, M.; Breda, J. Regional and Sociodemographic Determinants of the Prevalence of Overweight and Obesity in Children Aged 7-9 Years in Croatia. Acta Clin. Croat. 2020, 59, 303–311. [Google Scholar] [CrossRef]
- Rito, A.I.; Buoncristiano, M.; Spinelli, A.; Salanave, B.; Kunešová, M.; Hejgaard, T.; Solano, M.G.; Fijałkowska, A.; Sturua, L.; Hyska, J.; et al. Association between Characteristics at Birth, Breastfeeding and Obesity in 22 Countries: The WHO European Childhood Obesity Surveillance Initiative—COSI 2015/2017. Obes. Facts 2019, 12, 226–243. [Google Scholar] [CrossRef]
- Spinelli, A.; Buoncristiano, M.; Nardone, P.; Starc, G.; Hejgaard, T.; Júlíusson, P.B.; Fismen, A.S.; Weghuber, D.; Musić Milanović, S.; García-Solano, M.; et al. Thinness, Overweight, and Obesity in 6- to 9-Year-Old Children from 36 Countries: The World Health Organization European Childhood Obesity Surveillance Initiative—COSI 2015–2017. Obes. Rev. 2021, 22, e13214. [Google Scholar] [CrossRef]
- Seidell, J.C.; Halberstadt, J. The Global Burden of Obesity and the Challenges of Prevention. Ann. Nutr. Metab. 2015, 66, 7–12. [Google Scholar] [CrossRef] [PubMed]
- Haslam, D.W.; James, W.P.T. Obesity. Lancet 2005, 366, 1197–1209. [Google Scholar] [CrossRef]
- Viegas, S.; Ladeira, C.; Costa-veiga, A.; Perelman, J.; Gajski, G. Forgotten Public Health Impacts of Cancer—An Overview. Arh Hig. Rada Toksikol. 2017, 68, 287–297. [Google Scholar] [CrossRef]
- European Commission. Special Eurobaromter 505—Making our Food Fit for the Future—Citizens’ Expectations; European Commission: Brussels, Belgium, 2020. [Google Scholar] [CrossRef]
- Andreyeva, T.; Long, M.W.; Brownell, K.D. The impact of food prices on consumption: A systematic review of research on the price elasticity of demand for food. Am. J. Public Health 2010, 100, 216–222. [Google Scholar] [CrossRef] [PubMed]
- Estruch, R.; Ros, E.; Salas-Salvadó, J.; Covas, M.-I.; Corella, D.; Arós, F.; Gómez-Gracia, E.; Ruiz-Gutiérrez, V.; Fiol, M.; Lapetra, J.; et al. Primary Prevention of Cardiovascular Disease with a Mediterranean Diet Supplemented with Extra-Virgin Olive Oil or Nuts. N. Engl. J. Med. 2018, 378, e34. [Google Scholar] [CrossRef] [PubMed]
- Dernini, S.; Berry, E.M.; Serra-Majem, L.; La Vecchia, C.; Capone, R.; Medina, F.X.; Aranceta-Bartrina, J.; Belahsen, R.; Burlingame, B.; Calabrese, G.; et al. Med Diet 4.0: The Mediterranean Diet with Four Sustainable Benefits. Public Health Nutr. 2017, 20, 1322–1330. [Google Scholar] [CrossRef]
- Molina-Montes, E.; Ubago-Guisado, E.; Petrova, D.; Amiano, P.; Chirlaque, M.D.; Agudo, A.; Sánchez, M.J. The Role of Diet, Alcohol, Bmi, and Physical Activity in Cancer Mortality: Summary Findings of the Epic Study. Nutrients 2021, 13, 4293. [Google Scholar] [CrossRef]
- Sofi, F.; Abbate, R.; Gensini, G.F.; Casini, A. Accruing Evidence on Benefits of Adherence to the Mediterranean Diet on Health: An Updated Systematic Review and Meta-Analysis. Am. J. Clin. Nutr. 2010, 92, 1189–1196. [Google Scholar] [CrossRef] [PubMed]
- De Filippis, F.; Pellegrini, N.; Vannini, L.; Jeffery, I.B.; La Storia, A.; Laghi, L.; Serrazanetti, D.; Di Cagno, R.; Ferrocino, I.; Lazzi, C.; et al. High-Level Adherence to a Mediterranean Diet Beneficially Impacts the Gut Microbiota and Associated Metabolome. Gut 2016, 65, 1812–1821. [Google Scholar] [CrossRef]
- D’Alessandro, A.; Lampignano, L.; De Pergola, G. Mediterranean Diet Pyramid: A Proposal for Italian People. A Systematic Review of Prospective Studies to Derive Serving Sizes. Nutrients 2019, 11, 1296. [Google Scholar] [CrossRef]
- Bach-Faig, A.; Berry, E.M.; Lairon, D.; Reguant, J.; Trichopoulou, A.; Dernini, S.; Medina, F.X.; Battino, M.; Belahsen, R.; Miranda, G.; et al. Mediterranean Diet Pyramid Today Science and Cultural Updates. Public Health Nutr. 2011, 14, 2274–2284. [Google Scholar] [CrossRef]
- Davis, C.; Bryan, J.; Hodgson, J.; Murphy, K. Definition of the Mediterranean Diet; a Literature Review. Nutrients 2015, 7, 9139. [Google Scholar] [CrossRef]
- Vilarnau, C.; Stracker, D.M.; Funtikov, A.; da Silva, R.; Estruch, R.; Bach-Faig, A. Worldwide Adherence to Mediterranean Diet between 1960 and 2011. Eur. J. Clin. Nutr. 2019, 72, 83–91. [Google Scholar] [CrossRef] [PubMed]
- Kolčić, I.; Relja, A.; Gelemanović, A.; Miljković, A.; Boban, K.; Hayward, C.; Rudan, I.; Polašek, O. Mediterranean Diet in the Southern Croatia—Does It Still Exist? Croat. Med. J. 2016, 57, 415–424. [Google Scholar] [CrossRef] [PubMed]
- Schröder, H.; Fitó, M.; Estruch, R.; Martínez-González, M.A.; Corella, D.; Salas-Salvadó, J.; Lamuela-Raventós, R.; Ros, E.; Salaverría, I.; Fiol, M.; et al. A Short Screener Is Valid for Assessing Mediterranean Diet Adherence among Older Spanish Men and Women. J. Nutr. 2011, 141, 1140–1145. [Google Scholar] [CrossRef]
- EFSA. Food Consumption Data; EFSA: Parma, Italy, 2021. [Google Scholar]
- Ocké, M.; Boer, E.; De Brants, H.; Laan, J. External Efsa Scientific Report: Pancake—Pilot Study for the Assessment of Nutrient Intake and Food Consumption Among Kids in Europe. EFSA 2012, 9, 339E. [Google Scholar]
- U.S. Department of Agriculture. U.S. Department of Health and Human Services Dietary Guidelines for Americans 2020–2025; US Department of Agriculture: Washington, DC, USA, 2020; Volume 9.
- Oldways: A Food And Nutrition Nonprofit Helping People Live Healthier, Happier Lives. Available online: https://oldwayspt.org/traditional-diets/mediterranean-diet/traditional-med-diet (accessed on 23 June 2022).
- van Buuren, S.; Groothuis-Oudshoorn, K. Mice: Multivariate Imputation by Chained Equations in R. J. Stat. Softw. 2011, 45, 1–67. [Google Scholar] [CrossRef]
- Bentham, J.; Di Cesare, M.; Bilano, V.; Bixby, H.; Zhou, B.; Stevens, G.A.; Riley, L.M.; Taddei, C.; Hajifathalian, K.; Lu, Y.; et al. Worldwide Trends in Body-Mass Index, Underweight, Overweight, and Obesity from 1975 to 2016: A Pooled Analysis of 2416 Population-Based Measurement Studies in 128·9 Million Children, Adolescents, and Adults. Lancet 2017, 390, 2627–2642. [Google Scholar] [CrossRef]
- Afshin, A.; the GBD 2015 Obesity Collaborators. Health Effects of Overweight and Obesity in 195 Countries over 25 Years. N. Engl. J. Med. 2017, 377, 13–27. [Google Scholar] [CrossRef]
- Iacobini, C.; Vitale, M.; Haxhi, J.; Pesce, C.; Pugliese, G.; Menini, S. Food-Related Carbonyl Stress in Cardiometabolic and Cancer Risk Linked to Unhealthy Modern Diet. Nutrients 2022, 14, 1061. [Google Scholar] [CrossRef]
- Rubio-Tomás, T.; Rueda-Robles, A.; Plaza-Díaz, J.; Álvarez-Mercado, A.I. Nutrition and cellular senescence in obesity-related disorders. J. Nutr. Biochem. 2022, 99, 108861. [Google Scholar] [CrossRef] [PubMed]
- Kopelman, P.G. Obesity as a medical problem. Nature 2000, 404, 635–643. [Google Scholar] [CrossRef] [PubMed]
- Sánchez, M.G.; Sánchez, L.G.; Patino-Alonso, M.C.; Alonso-Domínguez, R.; Sánchez-Aguadero, N.; Lugones-Sánchez, C.; Sánchez, E.R.; Ortiz, L.G.; Gómez-Marcos, M.A. Adherence to the Mediterranean Diet in Spanish Population and Its Relationship with Early Vascular Aging According to Sex and Age: EVA Study. Nutrients 2020, 12, 1025. [Google Scholar] [CrossRef] [PubMed]
- Jones, J.P.H.; Abdullah, M.M.H.; Wood, D.; Jones, P.J.H. Economic Modeling for Improved Prediction of Saving Estimates in Healthcare Costs from Consumption of Healthy Foods: The Mediterranean-Style Diet Case Study. Food Nutr. Res. 2019, 63. [Google Scholar] [CrossRef]
- Sofi, F.; Macchi, C.; Abbate, R.; Gensini, G.F.; Casini, A. Mediterranean Diet and Health Status: An Updated Meta-Analysis and a Proposal for a Literature-Based Adherence Score. Public Health Nutr. 2014, 17, 2769–2782. [Google Scholar] [CrossRef] [PubMed]
- Tognon, G.; Lissner, L.; Sæbye, D.; Walker, K.Z.; Heitmann, B.L. The Mediterranean Diet in Relation to Mortality and CVD: A Danish Cohort Study. Br. J. Nutr. 2014, 111, 151–159. [Google Scholar] [CrossRef]
- Trichopoulou, A.; Costacou, T.; Bamia, C.; Trichopoulos, D. Adherence to a Mediterranean Diet and Survival in a Greek Population. Vasc. Med. 2009, 348, 2599–2608. [Google Scholar] [CrossRef]
- Castelló, A.; Boldo, E.; Pérez-Gómez, B.; Lope, V.; Altzibar, J.M.; Martín, V.; Castaño-Vinyals, G.; Guevara, M.; Dierssen-Sotos, T.; Tardón, A.; et al. Adherence to the Western, Prudent and Mediterranean Dietary Patterns and Breast Cancer Risk: MCC-Spain Study. Maturitas 2017, 103, 8–15. [Google Scholar] [CrossRef]
- Sureda, A.; del Mar Bibiloni, M.; Julibert, A.; Bouzas, C.; Argelich, E.; Llompart, I.; Pons, A.; Tur, J.A. Adherence to the Mediterranean Diet and Inflammatory Markers. Nutrients 2018, 10, 62. [Google Scholar] [CrossRef]
- Lagiou, P.; Trichopoulos, D.; Sandin, S.; Lagiou, A.; Mucci, L.; Wolk, A.; Weiderpass, E.; Adami, H.-O. Mediterranean Dietary Pattern and Mortality among Young Women: A Cohort Study in Sweden. Br. J. Nutr. 2006, 96, 384–392. [Google Scholar] [CrossRef]
- Gajski, G.; Gerić, M.; Vučić Lovrenčić, M.; Božičević, S.; Rubelj, I.; Nanić, L.; Škrobot Vidaček, N.; Bendix, L.; Peraica, M.; Rašić, D.; et al. Analysis of Health-Related Biomarkers between Vegetarians and Non-Vegetarians: A Multi-Biomarker Approach. J. Funct. Foods 2018, 48, 643–653. [Google Scholar] [CrossRef]
- Gajski, G.; Gerić, M.; Jakaša, I.; Peremin, I.; Domijan, A.M.; Vučić Lovrenčić, M.; Kežić, S.; Bituh, M.; Moraes de Andrade, V. Inflammatory, Oxidative and DNA Damage Status in Vegetarians: Is the Future of Human Diet Green? Crit. Rev. Food Sci. Nutr. 2021, 1–33. [Google Scholar] [CrossRef] [PubMed]
- Scoditti, E.; Tumolo, M.R.; Garbarino, S. Mediterranean Diet on Sleep: A Health Alliance. Nutrients 2022, 14, 2998. [Google Scholar] [CrossRef] [PubMed]
- Evans, J.R.; Mathur, A. The Value of Online Surveys: A Look Back and a Look Ahead. Internet Res. 2018, 28, 854–887. [Google Scholar] [CrossRef]
- Smith, W.G. Does Gender Influence Online Survey Participation? A Record-Linkage Analysis of University Faculty Online Survey Response Behavior; San José State University: San Jose, CA, USA, 2008. [Google Scholar]
- Havaš Auguštin, D.; Šarac, J.; Lovrić, M.; Živković, J.; Malev, O.; Fuchs, N.; Novokmet, N.; Turkalj, M.; Missoni, S. Adherence to Mediterranean Diet and Maternal Lifestyle during Pregnancy: Island–Mainland Differentiation in the CRIBS Birth Cohort. Nutrients 2020, 12, 2179. [Google Scholar] [CrossRef] [PubMed]
- Dinu, M.; Pagliai, G.; Giangrandi, I.; Colombini, B.; Toniolo, L.; Gensini, G.; Sofi, F. Adherence to the Mediterranean Diet among Italian Adults: Results from the Web-Based Medi-Lite Questionnaire. Int. J. Food Sci. Nutr. 2021, 72, 271–279. [Google Scholar] [CrossRef]
- Pfeifer, D.; Rešetar, J.; Gajdoš Kljusurić, J.; Panjkota Krbavčić, I.; Vranešić Bender, D.; Rodríguez-Pérez, C.; Ruíz-López, M.D.; Šatalić, Z. Cooking at Home and Adherence to the Mediterranean Diet During the COVID-19 Confinement: The Experience From the Croatian COVIDiet Study. Front. Nutr. 2021, 8, 617721. [Google Scholar] [CrossRef]
- Cuschieri, S.; Libra, M. Adherence to the Mediterranean Diet in Maltese Adults. Int. J. Environ. Res. Public Health 2021, 18, 10. [Google Scholar] [CrossRef]
- del Mar Bibiloni, M.; González, M.; Julibert, A.; Llompart, I.; Pons, A.; Tur, J.A. Ten-Year Trends (1999–2010) of Adherence to the Mediterranean Diet among the Balearic Islands’ Adult Population. Nutrients 2017, 9, 749. [Google Scholar] [CrossRef]
- Crichton, G.E.; Bryan, J.; Hodgson, J.M.; Murphy, K.J. Mediterranean Diet Adherence and Self-Reported Psychological Functioning in an Australian Sample. Appetite 2013, 70, 53–59. [Google Scholar] [CrossRef]
- Fiore, M.; Ledda, C.; Rapisarda, V.; Sentina, E.; Mauceri, C.; DAgati, P.; Conti, G.O.; Serra-Majem, L.; Ferrante, M. Medical School Fails to Improve Mediterranean Diet Adherence among Medical Students. Eur. J. Public Health 2015, 25, 1019–1023. [Google Scholar] [CrossRef] [PubMed]
- Grosso, G.; Marventano, S.; Buscemi, S.; Scuderi, A.; Matalone, M.; Platania, A.; Giorgianni, G.; Rametta, S.; Nolfo, F.; Galvano, F.; et al. Factors Associated with Adherence to the Mediterranean Diet among Adolescents Living in Sicily, Southern Italy. Nutrients 2013, 5, 4908–4923. [Google Scholar] [CrossRef] [PubMed]
- Grosso, G.; Marventano, S.; Giorgianni, G.; Raciti, T.; Galvano, F.; Mistretta, A. Mediterranean Diet Adherence Rates in Sicily, Southern Italy. Public Health Nutr. 2014, 17, 2001–2009. [Google Scholar] [CrossRef]
- Papadaki, A.; Wood, L.; Sebire, S.J.; Jago, R. Adherence to the Mediterranean Diet among Employees in South West England: Formative Research to Inform a Web-Based, Work-Place Nutrition Intervention. Prev. Med. Rep. 2015, 2, 223–228. [Google Scholar] [CrossRef] [PubMed]
- Pelucchi, C.; Galone, C.; Negri, E.; La Vecchia, C. Trends in Adherence to the Mediterranean Diet in an Italian Population between 1991 and 2006. Eur. J. Clin. Nutr. 2010, 64, 1052–1056. [Google Scholar] [CrossRef] [PubMed]
- Ruggiero, E.; Di Castelnuovo, A.; Costanzo, S.; Persichillo, M.; Bracone, F.; Cerletti, C.; Donati, M.B.; De Gaetano, G.; Iacoviello, L.; Bonaccio, M.; et al. Socioeconomic and Psychosocial Determinants of Adherence to the Mediterranean Diet in a General Adult Italian Population. Eur. J. Public Health 2019, 29, 328–335. [Google Scholar] [CrossRef] [PubMed]
- Obradovic Salcin, L.; Karin, Z.; Damjanovic, V.M.; Ostojic, M.; Vrdoljak, A.; Gilic, B.; Sekulic, D.; Lang-Morovic, M.; Markic, J.; Sajber, D. Physical Activity, Body Mass, and Adherence to the Mediterranean Diet in Preschool Children: A Cross-Sectional Analysis in the Split-Dalmatia County (Croatia). Int. J. Environ. Res. Public Health 2019, 16, 3237. [Google Scholar] [CrossRef] [PubMed]
- Pavičić Žeželj, S.; Jovanović, G.K.; Zubalj, N.D.; Mićović, V.; Sesar, Ž. Associations between Adherence to the Mediterranean Diet and Lifestyle Assessed with the MEDLIFE Index among the Working Population. Int. J. Environ. Res. Public Health 2018, 15, 2126. [Google Scholar] [CrossRef]
- Štefan, L.; Čule, M.; Milinović, I.; Sporiš, G.; Juranko, D. The Relationship between Adherence to the Mediterranean Diet and Body Composition in Croatian University Students. Eur. J. Integr. Med. 2017, 13, 41–46. [Google Scholar] [CrossRef]
- Aljabri, M.K.; Al-Raddadi, R.; Bahijri, S.M.; Al Ahmadi, J.; Ajabnoor, G.; Jambi, H.A. Factors Associated with Adherence to Mediterranean Diet among Saudi Non-Diabetic Patients Attending Primary Health Care Centers: A Cross-Sectional Study. J. Taibah Univ. Med. Sci. 2019, 14, 139–148. [Google Scholar] [CrossRef]
- Bottcher, M.R.; Marincic, P.Z.; Nahay, K.L.; Baerlocher, B.E.; Willis, A.W.; Park, J.; Gaillard, P.; Greene, M.W. Nutrition Knowledge and Mediterranean Diet Adherence in the Southeast United States: Validation of a Field-Based Survey Instrument. Appetite 2017, 111, 166–176. [Google Scholar] [CrossRef] [PubMed]
- Rodrigues, S.; Caraher, M.; Trichopoulou, A.; de Almeida, M. Portuguese Households’ Diet Quality (Adherence to Mediterranean Food Pattern and Compliance with WHO Population Dietary Goals): Trends, Regional Disparities and Socioeconomic Determinants. Eur. J. Clin. Nutr. 2008, 62, 1263–1272. [Google Scholar] [CrossRef] [PubMed]
- Baydemir, C.; Ozgur, E.G.; Balci, S. Evaluation of Adherence to Mediterranean Diet in Medical Students at Kocaeli University, Turkey. J. Int. Med. Res. 2018, 46, 1585–1594. [Google Scholar] [CrossRef] [PubMed]
- Robine, J.M.; Herrmann, F.R.; Arai, Y.; Willcox, D.C.; Gondo, Y.; Hirose, N.; Suzuki, M.; Saito, Y. Accuracy of the Centenarian Numbers in Okinawa and the Role of the Okinawan Diet on Longevity. Responses to Le Bourg about the Article “Exploring the Impact of Climate on Human Longevity. Exp. Gerontol. 2013, 48, 840–842. [Google Scholar] [CrossRef] [PubMed]
- Willcox, D.; John Willcox, B.; Yasura, S.; Willcox, D.; Willcox, B.; Yasura, S.; Ashitomi, I.; Suzuki, M. Gender Gap in Healthspan and Life Expectancy in Okinawa: Health Behaviours. Asian J. Gerontol. Geriatr. 2012, 7, 49–58. [Google Scholar]
- Willcox, B.J.; Willcox, D.C.; Todoriki, H.; Fujiyoshi, A.; Yano, K.; He, Q.; Curb, J.D.; Suzuki, M. Caloric Restriction, the Traditional Okinawan Diet, and Healthy Aging: The Diet of the World’s Longest-Lived People and Its Potential Impact on Morbidity and Life Span. Ann. N. Y. Acad. Sci. 2007, 1114, 434–455. [Google Scholar] [CrossRef]
- Ferrières, J. The French Paradox: Lessons for Other Countries. Heart 2004, 90, 107–111. [Google Scholar] [CrossRef]
- Abdelhamid, A.S.; Brown, T.J.; Brainard, J.S.; Biswas, P.; Thorpe, G.C.; Moore, H.J.; Deane, K.H.O.; Summerbell, C.D.; Worthington, H.V.; Song, F.; et al. Omega-3 Fatty Acids for the Primary and Secondary Prevention of Cardiovascular Disease. Cochrane Database Syst. Rev. 2020, 2020, 1158–1159. [Google Scholar] [CrossRef]
- George, E.S.; Marshall, S.; Mayr, H.L.; Trakman, G.L.; Tatucu-Babet, O.A.; Lassemillante, A.C.M.; Bramley, A.; Reddy, A.J.; Forsyth, A.; Tierney, A.C.; et al. The Effect of High-Polyphenol Extra Virgin Olive Oil on Cardiovascular Risk Factors: A Systematic Review and Meta-Analysis. Crit. Rev. Food Sci. Nutr. 2019, 59, 2772–2795. [Google Scholar] [CrossRef]
- Schwingshackl, L.; Hoffmann, G. Monounsaturated Fatty Acids, Olive Oil and Health Status: A Systematic Review and Meta-Analysis of Cohort Studies. Lipids Health Dis. 2014, 13, 154. [Google Scholar] [CrossRef]
- Briški, M.; Jarec, M. Cultural and Geographical Overview of Traditional Diet in Croatia. Coll. Antropol. 2014, 38, 1081–1092. [Google Scholar] [PubMed]
- Šarac, J.; Auguštin, D.H.; Lovrić, M.; Stryeck, S.; Šunić, I.; Novokmet, N.; Missoni, S. A Generation Shift in Mediterranean Diet Adherence and Its Association with Biological Markers and Health in Dalmatia, Croatia. Nutrients 2021, 13, 4564. [Google Scholar] [CrossRef] [PubMed]
- Colić-Barić, I.; Kajfež, R.; Šatalić, Z.; Cvjetić, S. Comparison of Dietary Habits in the Urban and Rural Croatian Schoolchildren. Eur. J. Nutr. 2004, 43, 169–174. [Google Scholar] [CrossRef] [PubMed]
- Sarić, M.M.; Ljubičić, M.; Lapčić, I.; Guiné, R.P.F. Contribution of Fruit, Vegetables, Whole Cereals, and Legumes to Total Fibre Intake in Adult Croatian Dalmatian Population. Arh. Hig. Rada Toksikol. 2020, 71, 138–145. [Google Scholar] [CrossRef] [PubMed]
- Ljubičić, M.; Sarić, M.M.; Barić, I.C.; Rumbak, I.; Komes, D.; Šatalić, Z.; Guiné, R.P.F. Consumer Knowledge and Attitudes toward Healthy Eating in Croatia: A Cross-Sectional Study. Arh. Hig. Rada Toksikol. 2017, 68, 153–158. [Google Scholar] [CrossRef]
- Ilić, A.; Rumbak, I.; Marić, L.; Karlović, T.; Brečić, R.; Colić Barić, I.; Bituh, M. The Proportion of Differently Processed Foods in the Diet of Croatian School-Aged Children and Its Impact on Daily Energy and Nutrient Intake. Croat. J. Food Sci. Technol. 2019, 14, 129–140. [Google Scholar] [CrossRef]
- Krešić, G.; Kenđel Jovanović, G.; Pavičić Žeželj, S.; Pleadin, J.; Liović, N.; Plepel, K. Parental Adherence to Mediterranean Diet Is Associated with Their Adolescents’ Cereals Intake. Croat. J. Food Sci. Technol. 2018, 10, 81–88. [Google Scholar] [CrossRef]
- Rao, M.; Afshin, A.; Singh, G.; Mozaffarian, D. Do Healthier Foods and Diet Patterns Cost More than Less Healthy Options? A Systematic Review and Meta-Analysis. BMJ Open 2013, 3, e004277. [Google Scholar] [CrossRef]
- Mozaffarian, D.; Afshin, A.; Benowitz, N.L.; Bittner, V.; Daniels, S.R.; Franch, H.A.; Jacobs, D.R.; Kraus, W.E.; Kris-Etherton, P.M.; Krummel, D.A.; et al. Population Approaches to Improve Diet, Physical Activity, and Smoking Habits: A Scientific Statement from the American Heart Association. Circulation 2012, 126, 1514–1563. [Google Scholar] [CrossRef]
- Lee, A.J.; Kane, S.; Ramsey, R.; Good, E.; Dick, M. Testing the Price and Affordability of Healthy and Current (Unhealthy) Diets and the Potential Impacts of Policy Change in Australia. BMC Public Health 2016, 16, 315. [Google Scholar] [CrossRef]
- Drewnowski, A.; Eichelsdoerfer, P. The Mediterranean Diet: Does It Have to Cost More? Public Health Nutr. 2009, 12, 1621–1628. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Darmon, N.; Drewnowski, A. Contribution of food prices and diet cost to socioeconomic disparities in diet quality and health: A systematic review and analysis. Nutr. Rev. 2015, 73, 643–660. [Google Scholar] [CrossRef] [PubMed]
- Vidaček, N.Š.; Nanić, L.; Ravlić, S.; Sopta, M.; Gerić, M.; Gajski, G.; Garaj-Vrhovac, V.; Rubelj, I. Telomeres, Nutrition, and Longevity: Can We Really Navigate Our Aging? J. Gerontol. Ser. A Biol. Sci. Med. Sci. 2018, 73, 39–47. [Google Scholar] [CrossRef] [PubMed] [Green Version]





Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gerić, M.; Matković, K.; Gajski, G.; Rumbak, I.; Štancl, P.; Karlić, R.; Bituh, M. Adherence to Mediterranean Diet in Croatia: Lessons Learned Today for a Brighter Tomorrow. Nutrients 2022, 14, 3725. https://doi.org/10.3390/nu14183725
Gerić M, Matković K, Gajski G, Rumbak I, Štancl P, Karlić R, Bituh M. Adherence to Mediterranean Diet in Croatia: Lessons Learned Today for a Brighter Tomorrow. Nutrients. 2022; 14(18):3725. https://doi.org/10.3390/nu14183725
Chicago/Turabian StyleGerić, Marko, Katarina Matković, Goran Gajski, Ivana Rumbak, Paula Štancl, Rosa Karlić, and Martina Bituh. 2022. "Adherence to Mediterranean Diet in Croatia: Lessons Learned Today for a Brighter Tomorrow" Nutrients 14, no. 18: 3725. https://doi.org/10.3390/nu14183725
APA StyleGerić, M., Matković, K., Gajski, G., Rumbak, I., Štancl, P., Karlić, R., & Bituh, M. (2022). Adherence to Mediterranean Diet in Croatia: Lessons Learned Today for a Brighter Tomorrow. Nutrients, 14(18), 3725. https://doi.org/10.3390/nu14183725







