Retail Cost and Energy Adjusted Cost Are Associated with Dietary Diversity and Nutrient Adequacy for Diets of 6–24 Months Children
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Study Population
2.2. Cost of Total Intake
2.3. Diet Quality Indicators
2.4. Statistical Analysis
3. Results
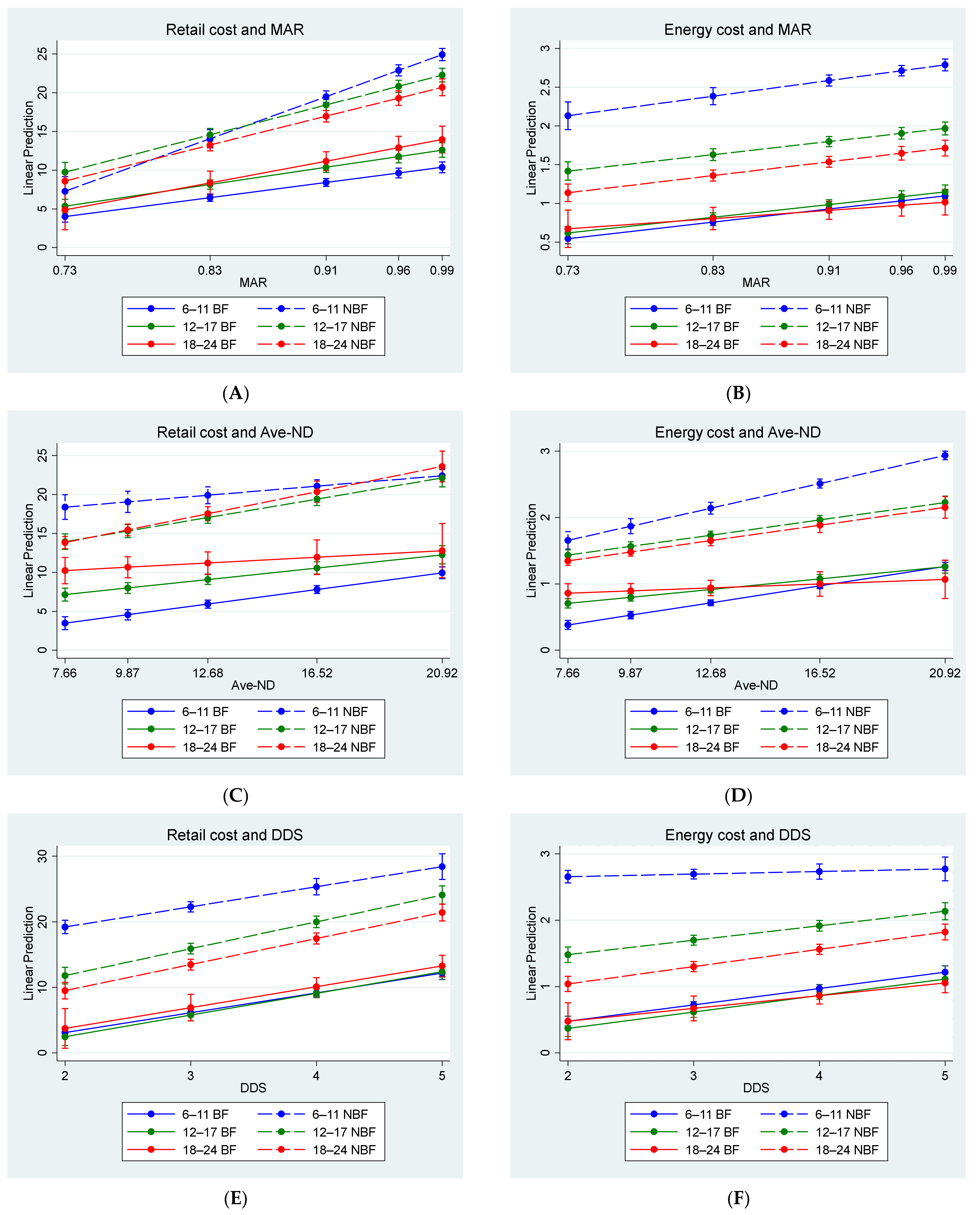
3.1. Associations between Cost and Diet Quality
3.2. Food Groups Included in the Diet According to Cost Tertiles
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Black, R.E.; Victora, C.G.; Walker, S.P.; Bhutta, Z.A.; Christian, P.; de Onis, M.; Ezzati, M.; Grantham-McGregor, S.; Katz, J.; Martorell, R.; et al. Maternal and child undernutrition and overweight in low-income and middle-income countries. Lancet 2013, 382, 427–451. [Google Scholar] [CrossRef]
- Herforth, A.; Bai, Y.; Venkat, A.; Mahrt, K.; Ebel, A.; Masters, W. Cost and Affordability of Healthy Diets across and within Countries: Background Paper for The State of Food Security and Nutrition in the World 2020; Food and Agriculture Organization of the United Nations: Rome, Italy, 2020; Volume 9, p. 108. [Google Scholar] [CrossRef]
- UNICEF (United Nations Children’s Fund). The State of the World’s Children 2019: Children, Food and Nutrition: Growing Well in a Changing World. UNICEF. 2019. Available online: https://www.unicef.org/reports/state-of-worlds-children-2019 (accessed on 27 June 2022).
- UNICEF/WHO/The World Bank Group Joint Child Malnutrition Estimates: Levels and Trends in Child Malnutrition: Key Findings of the 2021 Edition. Available online: https://data.unicef.org/resources/jme-report-2021/ (accessed on 27 June 2022).
- Bailey, R.L.; West, K.P., Jr.; Black, R.E. The epidemiology of global micronutrient deficiencies. Ann. Nutr. Metab. 2015, 66 (Suppl. 2), 22–33. [Google Scholar] [CrossRef] [PubMed]
- Gatica-Domínguez, G.; Neves, P.A.R.; Barros, A.J.D.; Victora, C.G. Complementary feeding practices in 80 low- and middle-income countries: Prevalence of and socioeconomic inequalities in dietary diversity, meal frequency, and dietary adequacy. J. Nutr. 2021, 151, 1956–1964. [Google Scholar] [CrossRef]
- Pries, A.M.; Filteau, S.; Ferguson, E.L. Snack food and beverage consumption and young child nutrition in low- and middle-income countries: A systematic review. Matern. Child Nutr. 2019, 15 (Suppl. 4), e12729. [Google Scholar] [CrossRef] [PubMed]
- Pries, A.M.; Rehman, A.M.; Filteau, S.; Sharma, N.; Upadhyay, A.; Ferguson, E.L. Unhealthy snack food and beverage consumption is associated with lower dietary adequacy and length-for-age z-scores among 12-23-month-olds in Kathmandu Valley, Nepal. J. Nutr. 2019, 149, 1843–1851. [Google Scholar] [CrossRef] [PubMed]
- Pries, A.M.; Huffman, S.L.; Champeny, M.; Adhikary, I.; Benjamin, M.; Coly, A.N.; Diop, E.H.I.; Mengkheang, K.; Sy, N.Y.; Dhungel, S.; et al. Consumption of commercially produced snack foods and sugar-sweetened beverages during the complementary feeding period in four African and Asian urban contexts. Matern. Child Nutr. 2017, 13 (Suppl. 2), e12412. [Google Scholar] [CrossRef] [PubMed]
- National Department of Health (NDoH); Statistics South Africa (Stats SA); South African Medical Research Council (SAMRC); ICF. South Africa Demographic and Health Survey 2016; NDoH, Stats SA, SAMRC: Pretoria, South Africa; ICF: Rockville, MA, USA, 2019. [Google Scholar]
- White, J.M.; Beal, T.; Arsenault, J.E.; Okronipa, H.; Hinnouho, G.-M.; Chimanya, K.; Matji, J.; Gar, A. Micronutrient gaps during the complementary feeding period in 6 countries in Eastern and Southern Africa: A Comprehensive Nutrient Gap Assessment. Nutr. Rev. 2021, 79, 16–25. [Google Scholar] [CrossRef] [PubMed]
- Beal, T.; White, J.M.; Arsenault, J.E.; Okronipa, H.; Hinnouho, G.-M.; Murira, Z.; Torlesse, H.; Garg, A. Micronutrient gaps during the complementary feeding period in South Asia: A comprehensive nutrient gap assessment. Nutr. Rev. 2021, 79 (Suppl. 1), 26–34. [Google Scholar] [CrossRef]
- Dewey, K.G. The challenge of meeting nutrient needs of infants and young children during the period of complementary feeding: An evolutionary perspective. J. Nutr. 2013, 143, 2050–2054. [Google Scholar] [CrossRef]
- Osendarp, S.J.; Broersen, B.; van Liere, M.J.; De-Regil, L.M.; Bahirathan, L.; Klassen, E.; Neufeld, L.M. Complementary feeding diets made of local foods can be optimized, but additional interventions will be needed to meet iron and zinc requirements in 6- to 23-month-old children in low- and middle-income countries. Food Nutr. Bull. 2016, 37, 544–570. [Google Scholar] [CrossRef]
- Fahmida, U.; Santika, O. Development of complementary feeding recommendations for 12–23-month-old children from low and middle socio-economic status in West Java, Indonesia: Contribution of fortified foods towards meeting the nutrient requirement. Br. J. Nutr. 2016, 116, S8–S15. [Google Scholar] [CrossRef]
- Bai, Y.; Alemu, R.; Block, S.A.; Headey, D.; Masters, W.A. Cost and affordability of nutritious diets at retail prices: Evidence from 177 countries. Food Policy 2021, 99, 101983. [Google Scholar] [CrossRef] [PubMed]
- Headey, D.D.; Alderman, H.H. The relative caloric prices of healthy and unhealthy foods differ systematically across income levels and continents. J. Nutr. 2019, 149, 2020–2033. [Google Scholar] [CrossRef]
- Visser, M.; Van Zyl, T.; Hanekom, S.M.; Baumgartner, J.; Van der Hoeven, M.; Taljaard-Krugell, C.; Smuts, C.M.; Faber, M. Nutrient density, but not cost of diet, is associated with anemia and iron deficiency in school-age children in South Africa. Nutrition 2021, 84, 111096. [Google Scholar] [CrossRef] [PubMed]
- Gupta, S.; Hawk, T.; Aggarwal, A.; Drewnowski, A. Characterizing ultra-processed foods by energy density, nutrient density, and cost. Front. Nutr. 2019, 6, 70. [Google Scholar] [CrossRef] [PubMed]
- Department of Health, South Africa. Regulations Relating to the Fortification of Certain Foodstuffs. (Government Notice no. R504). Government Gazette. 7 April 2003, p. 2475. Available online: http://faolex.fao.org (accessed on 20 January 2018).
- Faber, M.; Rothman, M.; Laubscher, R.; Smuts, C.M. Dietary patterns of 6–24-month-old children are associated with nutrient content and quality of the diet. Matern. Child Nutr. 2020, 16, e12901. [Google Scholar] [CrossRef] [PubMed]
- Faber, M. Complementary foods consumed by 6–12-month-old rural infants in South Africa are inadequate in micronutrients. Public Health Nutr. 2005, 8, 373–381. [Google Scholar] [CrossRef]
- Faber, M.; Kvalsvig, J.D.; Lombard, C.J.; Benadé, A.J.S. Effect of a fortified maize-meal porridge on anemia, micronutrient status, and motor development of infants. Am. J. Clin. Nutr. 2005, 82, 1032–1039. [Google Scholar] [CrossRef]
- Smuts, C.M.; Dhansay, M.A.; Faber, M.; van Stuijvenberg, M.E.; Swanevelder, S.; Gross, R.; Benadé, A.J.S. Efficacy of multiple micronutrient supplementation for improving anemia, micronutrient status, and growth in South African infants. J. Nutr. 2005, 135, 653S–659S. [Google Scholar] [CrossRef]
- Faber, M.; Laubscher, R.; Berti, C. Poor dietary diversity and low nutrient density of the complementary diet for 6-to 24-month-old children in urban and rural KwaZulu-Natal, South Africa. Matern. Child Nutr. 2016, 12, 528–545. [Google Scholar] [CrossRef] [PubMed]
- Smuts, C.M.; Matsungo, T.M.; Malan, L.; Kruger, H.S.; Rothman, M.; Kvalsvig, J.D.; Covic, N.; Joosten, K.; Osendarp, S.J.; Bruins, M.J. Effect of small-quantity lipid-based nutrient supplements on growth, psychomotor development, iron status, and morbidity among 6-to 12-mo-old infants in South Africa: A randomized controlled trial. Am. J. Clin. Nutr. 2019, 109, 55–68. [Google Scholar] [CrossRef] [PubMed]
- Swanepoel, E.; Havemann-Nel, L.; Rothman, M.; Laubscher, R.; Matsungo, T.M.; Smuts, C.M.; Faber, M. Contribution of commercial infant products and fortified staple foods to nutrient intake at ages 6, 12, and 18 months in a cohort of children from a low socio-economic community in South Africa. Matern. Child Nutr. 2019, 15, e12674. [Google Scholar] [CrossRef]
- SAFOODS. SAMRC Food Composition Tables for South Africa, 5th ed.; South African Medical Research Council: Cape Town, South Africa, 2017. [Google Scholar]
- World Health Organization. Complementary Feeding of Young Children in Developing Countries: A Review of Current Scientific Knowledge; WHO/NUT/98.1; World Health Organization: Geneva, Switzerland, 1998. [Google Scholar]
- Bognár, A. Tables on Weight Yield of Food and Retention Factors of food Constituents for the Calculation of Nutrient COMPOSITION of Cooked Foods (Dishes). BFE Karlsruhe. 2002. Available online: https://www.fao.org/uploads/media/bognar_bfe-r-02-03.pdf (accessed on 22 January 2019).
- SAFOODS. SAMRC Food Quantities Manual for South Africa, 3rd ed.; South African Medical Research Council: Cape Town, South Africa, 2018. [Google Scholar]
- Otten, J.J.; Meyers, L.D.; Hellwig, J.P. Dietary Reference Intakes: The Essential Guide to Nutrient Requirements; National Academies Press: Cambridge, MA, USA, 2006. [Google Scholar]
- Institute of Medicine. Dietary Reference Intakes for Calcium and Vitamin D; Institute of Medicine; The National Academies Press: Washington, DC, USA, 2011; Available online: https://www.nap.edu/search/?term=DRIMAR (accessed on 5 January 2018).
- INDDEX Project. Data4Diets: Building Blocks for Diet-Related Food Security Analysis. Tufts University: Boston, MA, USA, 2018; Available online: https://inddex.nutrition.tufts.edu/data4diets (accessed on 5 January 2021).
- World Health Organization. Indicators for Assessing Infant and Young Child Feeding Practices: Definitions and Measurement Methods. 2021. Available online: https://apps.who.int/iris/bitstream/handle/10665/340706/9789240018389-eng.pdf?sequence=1 (accessed on 8 June 2021).
- World Health Organization. Global Strategy on Infant and Young Child Feeding. 2003. Available online: https://apps.who.int/iris/bitstream/handle/10665/42590/9241562218.pdf (accessed on 20 April 2021).
- Pietermaritzburg Economic Justice & Dignity Group. Household Affordability Index. 2022. Available online: https://pmbejd.org.za/index.php/household-affordability-index (accessed on 27 June 2022).
- Walters, D.D.; Phan, L.T.H.; Mathisen, R. The cost of not breastfeeding: Global results from a new tool. Health Policy Plan 2019, 34, 407–417. [Google Scholar] [CrossRef] [PubMed]
- Senekal, M.; Nel, J.; Malczyk, S.; Drummond, L.; Steyn, N.P. Provincial Dietary Intake Study (PDIS): Micronutrient intakes of children in a representative/random sample of 1-to<10-year-old children in two economically active and urbanized provinces in South Africa. Int. J. Environ. Res. Public Health 2020, 17, 5924. [Google Scholar]
- Van Stuijvenberg, M.E.; Nel, J.; Schoeman, S.E.; Lombard, C.J.; du Plessis, L.M.; Dhansay, M.A. Low intake of calcium and vitamin D, but not zinc, iron or vitamin A, is associated with stunting in 2-to 5-year-old children. Nutrition 2015, 31, 841–846. [Google Scholar] [CrossRef] [PubMed]
- Dror, D.K.; Allen, L.H. Dairy product intake in children and adolescents in developed countries: Trends, nutritional contribution, and a review of association with health outcomes. Nutr. Rev. 2014, 72, 68–81. [Google Scholar] [CrossRef] [PubMed]
- Sayed, N.; Schönfeldt, H.C. A review of complementary feeding practices in South Africa. S. Afr. J. Clin. Nutr. 2020, 33, 36–43. [Google Scholar] [CrossRef]
- Labadarios, D.; Steyn, N.P.; Nel, J. How diverse is the diet of adult South Africans? Nutr. J. 2011, 10, 33. [Google Scholar] [CrossRef]
- Lutter, C.K.; Grummer-Strawn, L.; Rogers, L. Complementary feeding of infants and young children 6 to 23 months of age. Nutr. Rev. 2021, 79, 825–846. [Google Scholar] [CrossRef]
- Moursi, M.M.; Arimond, M.; Dewey, K.G.; Treche, S.; Ruel, M.T.; Delpeuch, F. Dietary diversity is a good predictor of the micronutrient density of the diet of 6-to 23-month-old children in Madagascar. J. Nutr. 2008, 138, 2448–2453. [Google Scholar] [CrossRef]
- FAO; IFAD; UNICEF; WFP; WHO. The State of Food Security and Nutrition in the World 2020; Transforming Food Systems for Affordable Healthy Diets; FAO: Rome, Italy, 2020; Available online: https://doi.org/10.4060/ca9692en (accessed on 17 January 2022).
- Chakona, G. Social circumstances and cultural beliefs influence maternal nutrition, breastfeeding and child feeding practices in South Africa. Nutr. J. 2020, 19, 47. [Google Scholar] [CrossRef] [PubMed]
- Shisana, O.; Labadarios, D.; Rehle, T.; Simbayi, L.; Zuma, K.; Dhansay, A.; Reddy, P.; Parker, W.; Hoosain, E.; Naidoo, P.; et al. SANHANES-1 Team. South African National Health and Nutrition Examination Survey (SANHANES-1); Human Sciences Research Council and MRC: Cape Town, South Africa, 2013. [Google Scholar]
- Drewnowski, A. The Nutrient Rich Foods Index helps to identify healthy, affordable foods. Am. J. Clin. Nutr. 2010, 91, 1095S–1101S. [Google Scholar] [CrossRef] [PubMed]
- Dewey, K.G.; Vitta, B.S. Strategies for Ensuring Adequate Nutrient Intake for Infants and Young Children during the Period of Complementary Feeding; Alive & Thrive: Washington, DC, USA, 2013. [Google Scholar]
- SAPA (South African Poultry Association). South African Poultry Association 2019 Industry Profile. 2019. Available online: http://www.sapoultry.co.za/pdf-docs/sapa-industry-profile.pdf (accessed on 25 May 2022).
- NAMC. The South African Food Cost Review. 2020. Available online: https://www.namc.co.za/wp-content/uploads/2021/03/Food-Cost-Review-2020-_-final.pdf (accessed on 27 June 2022).
- Du Plessis, L.; Daniels, L.; Koornhof, H.; Samuels, S.; Möller, I.; Röhrs, S. Overview of field-testing of the revised, draft South African Paediatric Food-Based Dietary Guidelines amongst mothers/caregivers of children aged 0–5 years in the Western Cape and Mpumalanga, South Africa. S. Afr. J. Clin. Nutr. 2021, 34, 132–138. [Google Scholar] [CrossRef]
- Kuyper, E.; Vitta, B.; Dewey, K. Novel and Underused Food Sources of Key Nutrients for Complementary Feeding. A&T Tech Brief, 6. 2013. Available online: https://www.aliveandthrive.org/en/resources/novel-and-underused-food-sources-of-key-nutrients-for-complementary-feeding-insight-series (accessed on 27 June 2022).
- FAO. Dietary Assessment: A Resource Guide to Method Selection and Application in Low Resource Settings; Food and Agriculture Organization: Rome, Italy, 2018. [Google Scholar]
- Dror, D.K.; Allen, L.H. Overview of nutrients in human milk. Adv. Nutr. 2018, 9, 278S–294S. [Google Scholar] [CrossRef] [PubMed]



| 6–11 Months | 12–17 Months | 18–24 Months | ||||
|---|---|---|---|---|---|---|
| BF-Diet | NBF-Diet | BF-Diet | NBF-Diet | BF-Diet | NBF-Diet | |
| Sample size | 1119 | 466 | 658 | 473 | 154 | 466 |
| Retail cost (ZAR) | 6.68 | 21.92 | 8.66 | 17.77 | 11.12 | 14.89 |
| (3.42, 11.75) | (16.06, 28.67) | (5.08, 13.43) | (12.05, 24.8) | (7.14, 15.31) | (9.79, 21.99) | |
| Energy cost (ZAR/100 kcal) | 0.82 | 2.70 | 0.88 | 1.80 | 0.92 | 1.45 |
| (0.46, 1.34) | (2.10, 3.32) | (0.56, 1.27) | (1.37, 2.31) | (0.70, 1.20) | (1.03, 1.98) | |
| MAR | 0.88 | 0.97 | 0.88 | 0.94 | 0.92 | 0.89 |
| (0.80, 0.94) | (0.93, 1.00) | (0.80, 0.94) | (0.86, 0.98) | (0.86, 0.97) | (0.82, 0.95) | |
| Ave-ND | 13.88 | 18.23 | 11.05 | 12.48 | 10.03 | 8.39 |
| (11.63, 16.60) | (15.25, 21.85) | (9.54, 13.79) | (9.01, 16.42) | (8.99, 11.80) | (6.38, 11.08) | |
| DDS | 3.0 | 3.0 | 4.0 | 3.0 | 4.0 | 3.0 |
| (3.0, 4.0) | (2.0, 3.0) | (3.0, 5.0) | (3.0, 4.0) | (3.0, 5.0) | (3.0, 4.0) | |
| 6–11 Months | 12–17 Months | 18–24 Months | ||||
|---|---|---|---|---|---|---|
| BF-Diet | NBF-Diet | BF-Diet | NBF-Diet | BF-Diet | NBF-Diet | |
| Sample size | 1119 | 466 | 658 | 473 | 154 | 466 |
| Breastmilk | 1119 (100) | 0 (0) | 658 (100) | 0 (0) | 154 (100) | 0 (0) |
| Grains, roots and tubers | 1083 (96.8) | 451 (96.8) | 655 (99.7) | 470 (99.4) | 154 (100) | 466 (100) |
| Legumes | 243 (21.7) | 102 (21.9) | 232 (35.3) | 152 (32.1) | 50 (32.5) | 176 (37.8) |
| Dairy (incl. formula milk) | 480 (42.9) | 445 (95.5) | 332 (50.5) | 375 (79.9) | 89 (57.8) | 281 (60.3) |
| Formula milk | 275 (24.6) | 400 (85.8) | 70 (10.6) | 207 (43.8) | 5 (3.2) | 63 (13.5) |
| Flesh foods 1 | 87 (7.8) | 40 (8.6) | 228 (34.7) | 118 (39.7) | 80 (51.9) | 244 (52.4) |
| Eggs | 70 (6.3) | 23 (4.9) | 51 (7.8) | 42 (8.9) | 17 (11.0) | 41 (8.8) |
| Vit A-rich fruits & vegetables | 277 (20.3) | 96 (20.6) | 185 (28.1) | 127 (26.8) | 42 (27.3) | 124 (26.6) |
| Other fruits & vegetables | 326 (29.1) | 150 (32.2) | 297 (45.1) | 246 (52.0) | 71 (46.1) | 286 (61.4) |
| Minimum DD (≥5 groups) | 121 (10.8) | 25 (5.4) | 198 (30.1) | 66 (14.0) | 55 (35.7) | 82 (17.6) |
| 6–11 Months | 12–17 Months | 18–24 Months | |||||
|---|---|---|---|---|---|---|---|
| BF-Diet | NBF-Diet | BF-Diet | NBF-Diet | BF-Diet | NBF-Diet | ||
| Sample size | 1119 | 466 | 658 | 473 | 154 | 466 | |
| Retail cost versus energy cost | r | 0.961 | 0.550 | 0.933 | 0.748 | 0.870 | 0.848 |
| p-value | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | |
| Retail cost versus MAR | r | 0.610 | 0.680 | 0.671 | 0.732 | 0.664 | 0.682 |
| p-value | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | |
| Retail cost versus Ave-ND | r | 0.311 | 0.175 | 0.283 | 0.464 | 0.181 | 0.417 |
| p-value | <0.001 | <0.001 | <0.001 | <0.001 | 0.025 | <0.001 | |
| Retail cost versus DDS | r | 0.516 | 0.279 | 0.606 | 0.415 | 0.575 | 0.500 |
| p-value | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | |
| Energy costs versus MAR | r | 0.436 | 0.028 | 0.466 | 0.387 | 0.343 | 0.422 |
| p-value | <0.001 | 0.542 | <0.001 | <0.001 | <0.001 | <0.001 | |
| Energy cost versus Ave-ND | r | 0.409 | 0.523 | 0.401 | 0.601 | 0.200 | 0.417 |
| p-value | <0.001 | <0.001 | <0.001 | <0.001 | 0.013 | <0.001 | |
| Energy cost versus DDS | r | 0.441 | 0.104 | 0.566 | 0.298 | 0.598 | 0.452 |
| p-value | <0.001 | 0.025 | <0.001 | <0.001 | <0.001 | <0.001 | |
| DDS versus MAR | r | 0.515 | 0.243 | 0.478 | 0.306 | 0.356 | 0.462 |
| p-value | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | |
| MAR versus Ave-ND | r | 0.137 | 0.077 | 0.211 | 0.538 | 0.335 | 0.646 |
| p-value | <0.001 | 0.096 | <0.001 | <0.001 | <0.001 | <0.001 | |
| DDS versus Ave-ND | r | −0.045 | −0.185 | 0.091 | 0.094 | 0.122 | 0.327 |
| p-value | 0.137 | <0.001 | 0.020 | 0.040 | 0.132 | <0.001 | |
| Age Category | Retail Cost Tertiles | ||
|---|---|---|---|
| Tertile 1 | Tertile 2 | Tertile 3 | |
| 6–11 months | Grains/roots/tubers Breastmilk | Grains/roots/tubers Breastmilk Dairy | Grains/roots/tubers Dairy |
| 12–17 months | Starchy foods Breastmilk | Starchy foods Breastmilk Dairy Fruit and vegetables | Starchy foods Dairy Fruit and vegetables |
| 18–24 months | Starchy foods Fruit and vegetables | Starchy foods Fruit and vegetables Dairy Flesh food | Starchy foods Fruit and vegetables Dairy Flesh food |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mulabisano, T.A.; Laubscher, R.; Hoffman, M.; Hill, J.; Kunneke, E.; Smuts, C.M.; Faber, M. Retail Cost and Energy Adjusted Cost Are Associated with Dietary Diversity and Nutrient Adequacy for Diets of 6–24 Months Children. Nutrients 2022, 14, 3376. https://doi.org/10.3390/nu14163376
Mulabisano TA, Laubscher R, Hoffman M, Hill J, Kunneke E, Smuts CM, Faber M. Retail Cost and Energy Adjusted Cost Are Associated with Dietary Diversity and Nutrient Adequacy for Diets of 6–24 Months Children. Nutrients. 2022; 14(16):3376. https://doi.org/10.3390/nu14163376
Chicago/Turabian StyleMulabisano, Tshavhuyo A., Ria Laubscher, Marinel Hoffman, Jillian Hill, Ernesta Kunneke, Cornelius M. Smuts, and Mieke Faber. 2022. "Retail Cost and Energy Adjusted Cost Are Associated with Dietary Diversity and Nutrient Adequacy for Diets of 6–24 Months Children" Nutrients 14, no. 16: 3376. https://doi.org/10.3390/nu14163376
APA StyleMulabisano, T. A., Laubscher, R., Hoffman, M., Hill, J., Kunneke, E., Smuts, C. M., & Faber, M. (2022). Retail Cost and Energy Adjusted Cost Are Associated with Dietary Diversity and Nutrient Adequacy for Diets of 6–24 Months Children. Nutrients, 14(16), 3376. https://doi.org/10.3390/nu14163376






