Good Adherence to the Mediterranean Diet Lowered Risk of Renal Glomerular Impairment in Children: A Longitudinal Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Participants
2.2. Urine Collection and Measurements
2.3. Assessment of Adherence to the Mediterranean Diet
2.4. Data Collection of Covariates
2.5. Statistical Analysis
3. Results
3.1. Sociodemographic Characteristics
3.2. Linear Associations of Kidney Impairment Indicators with KIDMED Scores
3.3. Longitudinal Associations of Kidney Impairment with KIDMED Index
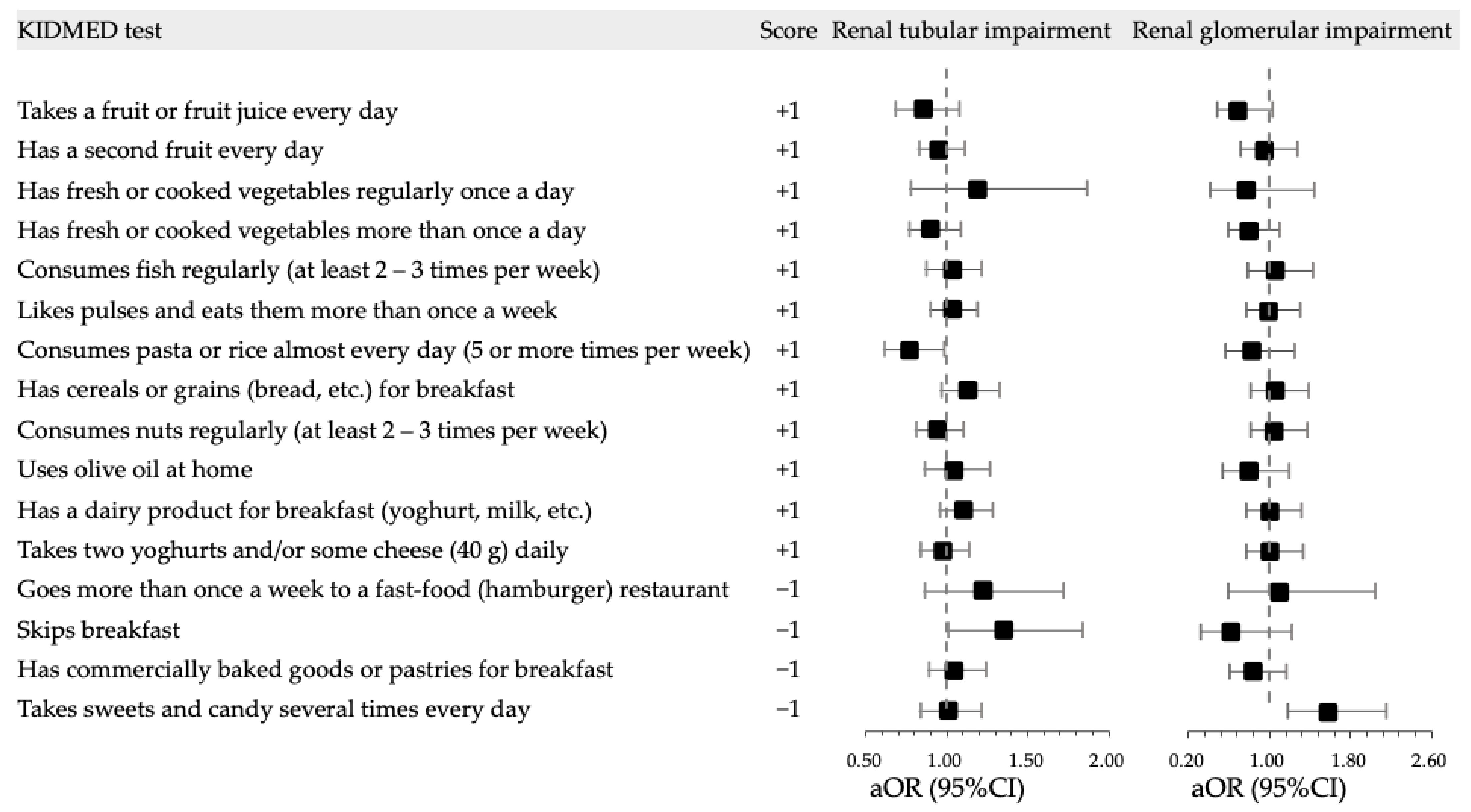
3.4. Longitudinal Associations of Kidney Impairment with KIDMED Test
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Gomez-Delgado, F.; Katsiki, N.; Lopez-Miranda, J.; Perez-Martinez, P. Dietary habits, lipoprotein metabolism and cardiovascular disease: From individual foods to dietary patterns. Crit. Rev. Food Sci. Nutr. 2021, 61, 1651–1669. [Google Scholar] [CrossRef] [PubMed]
- Zeraattalab-Motlagh, S.; Jayedi, A.; Shab-Bidar, S. Mediterranean dietary pattern and the risk of type 2 diabetes: A systematic review and dose-response meta-analysis of prospective cohort studies. Eur. J. Nutr. 2022, 61, 1735–1748. [Google Scholar] [CrossRef] [PubMed]
- De Cosmi, V.; Mazzocchi, A.; Milani, G.P.; Agostoni, C. Dietary Patterns vs. Dietary Recommendations. Front. Nutr. 2022, 9, 883806. [Google Scholar] [CrossRef]
- Chen, M.; Xiong, J.; Zhao, L.; Cheng, G.; Zhang, Q.; Ding, G. Epidemiological research progress on the relationship between children’s dietary patterns and health. Chin. J. Prev. Med. 2022, 56, 139–145. [Google Scholar]
- Guasch-Ferré, M.; Willett, W.C. The Mediterranean diet and health: A comprehensive overview. J. Intern. Med. 2021, 290, 549–566. [Google Scholar] [CrossRef]
- Di Renzo, L.; Gualtieri, P.; Lorenzo, A.D. Diet, Nutrition and Chronic Degenerative Diseases. Nutrients 2021, 13, 1372. [Google Scholar] [CrossRef]
- Bach, K.E.; Kelly, J.T.; Palmer, S.C.; Khalesi, S.; Strippoli, G.F.M.; Campbell, K.L. Healthy Dietary Patterns and Incidence of CKD: A Meta-Analysis of Cohort Studies. Clin. J. Am. Soc. Nephrol. 2019, 14, 1441–1449. [Google Scholar] [CrossRef]
- Romero-Robles, M.A.; Ccami-Bernal, F.; Ortiz-Benique, Z.N.; Pinto-Ruiz, D.F.; Benites-Zapata, V.A.; Casas Patiño, D. Adherence to Mediterranean diet associated with health-related quality of life in children and adolescents: A systematic review. BMC Nutr. 2022, 8, 57. [Google Scholar] [CrossRef]
- Martíncrespo-Blanco, M.C.; Varillas-Delgado, D.; Blanco-Abril, S.; Cid-Exposito, M.G.; Robledo-Martín, J. Effectiveness of an Intervention Programme on Adherence to the Mediterranean Diet in a Preschool Child: A Randomised Controlled Trial. Nutrients 2022, 14, 1536. [Google Scholar] [CrossRef]
- Archero, F.; Ricotti, R.; Solito, A.; Carrera, D.; Civello, F.; Di Bella, R.; Bellone, S.; Prodam, F. Adherence to the Mediterranean Diet among School Children and Adolescents Living in Northern Italy and Unhealthy Food Behaviors Associated to Overweight. Nutrients 2018, 10, 1322. [Google Scholar] [CrossRef]
- Mazaraki, A.; Tsioufis, C.; Dimitriadis, K.; Tsiachris, D.; Stefanadi, E.; Zampelas, A.; Richter, D.; Mariolis, A.; Panagiotakos, D.; Tousoulis, D.; et al. Adherence to the Mediterranean diet and albuminuria levels in Greek adolescents: Data from the Leontio Lyceum ALbuminuria (3L study). Eur. J. Clin. Nutr. 2011, 65, 219–225. [Google Scholar] [CrossRef]
- Zhen, S.; Ma, Y.; Zhao, Z.; Yang, X.; Wen, D. Dietary pattern is associated with obesity in Chinese children and adolescents: Data from China Health and Nutrition Survey (CHNS). Nutr. J. 2018, 17, 68. [Google Scholar] [CrossRef]
- Serra-Majem, L.; Ribas, L.; Ngo, J.; Ortega, R.M.; García, A.; Pérez-Rodrigo, C.; Aranceta, J. Food, youth and the Mediterranean diet in Spain. Development of KIDMED, Mediterranean Diet Quality Index in children and adolescents. Public Health Nutr. 2004, 7, 931–935. [Google Scholar] [CrossRef]
- Galan-Lopez, P.; Domínguez, R.; Pihu, M.; Gísladóttir, T.; Sánchez-Oliver, A.J.; Ries, F. Evaluation of Physical Fitness, Body Composition, and Adherence to Mediterranean Diet in Adolescents from Estonia: The AdolesHealth Study. Int. J. Environ. Res. Public Health 2019, 16, 4479. [Google Scholar] [CrossRef]
- Kim, R.J.; Lopez, R.; Snair, M.; Tang, A. Mediterranean diet adherence and metabolic syndrome in US adolescents. Int. J. Food Sci. Nutr. 2021, 72, 537–547. [Google Scholar] [CrossRef]
- Martino, F.; Puddu, P.E.; Lamacchia, F.; Colantoni, C.; Zanoni, C.; Barillà, F.; Martino, E.; Angelico, F. Mediterranean diet and physical activity impact on metabolic syndrome among children and adolescents from Southern Italy: Contribution from the Calabrian Sierras Community Study (CSCS). Int. J. Cardiol. 2016, 225, 284–288. [Google Scholar] [CrossRef]
- Dominguez-Riscart, J.; Buero-Fernandez, N.; Garcia-Zarzuela, A.; Morales-Perez, C.; Garcia-Ojanguren, A.; Lechuga-Sancho, A.M. Adherence to Mediterranean Diet Is Associated With Better Glycemic Control in Children With Type 1 Diabetes: A Cross-Sectional Study. Front. Nutr. 2022, 9, 813989. [Google Scholar] [CrossRef]
- Della Corte, C.; Mosca, A.; Vania, A.; Alterio, A.; Iasevoli, S.; Nobili, V. Good adherence to the Mediterranean diet reduces the risk for NASH and diabetes in pediatric patients with obesity: The results of an Italian Study. Nutrition 2017, 39-40, 8–14. [Google Scholar] [CrossRef]
- Agostinis-Sobrinho, C.; Santos, R.; Rosário, R.; Moreira, C.; Lopes, L.; Mota, J.; Martinkenas, A.; García-Hermoso, A.; Correa-Bautista, J.E.; Ramírez-Vélez, R. Optimal Adherence to a Mediterranean Diet May Not Overcome the Deleterious Effects of Low Physical Fitness on Cardiovascular Disease Risk in Adolescents: A Cross-Sectional Pooled Analysis. Nutrients 2018, 10, 815. [Google Scholar] [CrossRef]
- Wärnberg, J.; Pérez-Farinós, N.; Benavente-Marín, J.C.; Gómez, S.F.; Labayen, I.; Zapico, A.G.; Gusi, N.; Aznar, S.; Alcaraz, P.E.; González-Valeiro, M.; et al. Screen Time and Parents’ Education Level Are Associated with Poor Adherence to the Mediterranean Diet in Spanish Children and Adolescents: The PASOS Study. J. Clin. Med. 2021, 10, 795. [Google Scholar] [CrossRef]
- Lampropoulou, M.; Chaini, M.; Rigopoulos, N.; Evangeliou, A.; Papadopoulou-Legbelou, K.; Koutelidakis, A.E. Association Between Serum Lipid Levels in Greek Children with Dyslipidemia and Mediterranean Diet Adherence, Dietary Habits, Lifestyle and Family Socioeconomic Factors. Nutrients 2020, 12, 1600. [Google Scholar] [CrossRef] [PubMed]
- Wu, H.Y.; Huang, J.W.; Peng, Y.S.; Hung, K.Y.; Wu, K.D.; Lai, M.S.; Chien, K.L. Microalbuminuria screening for detecting chronic kidney disease in the general population: A systematic review. Ren. Fail. 2013, 35, 607–614. [Google Scholar] [CrossRef] [PubMed]
- Kadam, P.; Yachha, M.; Srivastava, G.; Pillai, A.; Pandita, A. Urinary beta-2 microglobulin as an early predictive biomarker of acute kidney injury in neonates with perinatal asphyxia. Eur. J. Pediatrics 2022, 181, 281–286. [Google Scholar] [CrossRef]
- Li, M.; Shu, W.; Zunong, J.; Amaerjiang, N.; Xiao, H.; Li, D.; Vermund, S.H.; Hu, Y. Predictors of non-alcoholic fatty liver disease in children. Pediatric Res. 2021, 1–9. [Google Scholar] [CrossRef]
- Li, M.; Shu, W.; Amaerjiang, N.; Xiao, H.; Zunong, J.; Vermund, S.H.; Huang, D.; Hu, Y. Interaction of Hydration Status and Physical Activity Level on Early Renal Damage in Children: A Longitudinal Study. Front. Nutr. 2022, 9, 910291. [Google Scholar] [CrossRef]
- Li, M.; Amaerjiang, N.; Li, Z.; Xiao, H.; Zunong, J.; Gao, L.; Vermund, S.H.; Hu, Y. Insufficient Fruit and Vegetable Intake and Low Potassium Intake Aggravate Early Renal Damage in Children: A Longitudinal Study. Nutrients 2022, 14, 1228. [Google Scholar] [CrossRef]
- Amaerjiang, N.; Li, M.; Xiao, H.; Zunong, J.; Li, Z.; Huang, D.; Vermund, S.H.; Pérez-Escamilla, R.; Jiang, X.; Hu, Y. Dehydration Status Aggravates Early Renal Impairment in Children: A Longitudinal Study. Nutrients 2022, 14, 335. [Google Scholar] [CrossRef]
- Barton, K.T.; Kakajiwala, A.; Dietzen, D.J.; Goss, C.W.; Gu, H.; Dharnidharka, V.R. Using the newer Kidney Disease: Improving Global Outcomes criteria, beta-2-microglobulin levels associate with severity of acute kidney injury. Clin. Kidney J. 2018, 11, 797–802. [Google Scholar] [CrossRef]
- Shatat, I.F.; Qanungo, S.; Hudson, S.; Laken, M.A.; Hailpern, S.M. Changes in Urine Microalbumin-to-Creatinine Ratio in Children with Sickle Cell Disease over Time. Front. Pediatrics 2016, 4, 106. [Google Scholar] [CrossRef]
- Owens, J.A.; Spirito, A.; McGuinn, M. The Children’s Sleep Habits Questionnaire (CSHQ): Psychometric properties of a survey instrument for school-aged children. Sleep 2000, 23, 1043–1051. [Google Scholar] [CrossRef]
- Amaerjiang, N.; Xiao, H.; Zunong, J.; Shu, W.; Li, M.; Pérez-Escamilla, R.; Hu, Y. Sleep disturbances in children newly enrolled in elementary school are associated with parenting stress in China. Sleep Med. 2021, 88, 247–255. [Google Scholar] [CrossRef]
- Li, H.; Chen, P.; Zhuang, J. Revision and reliability validity assessment of children’s leisure activities study survey. Chin. J. Sch. Health 2011, 32, 268–270. [Google Scholar]
- Naja, F.; Hasan, H.; Khadem, S.H.; Buanq, M.A.; Al-Mulla, H.K.; Aljassmi, A.K.; Faris, M.E. Adherence to the Mediterranean Diet and Its Association With Sleep Quality and Chronotype Among Youth: A Cross-Sectional Study. Front. Nutr. 2021, 8, 805955. [Google Scholar] [CrossRef]
- Naber, T.; Purohit, S. Chronic Kidney Disease: Role of Diet for a Reduction in the Severity of the Disease. Nutrients 2021, 13, 3277. [Google Scholar] [CrossRef]
- Swärd, P.; Tofik, R.; Bakoush, O.; Torffvit, O.; Nilsson, P.M.; Christensson, A. Patterns of urinary albumin and IgM associate with markers of vascular ageing in young to middle-aged individuals in the Malmö offspring study. BMC Cardiovasc. Disord. 2020, 20, 358. [Google Scholar] [CrossRef]
- Lambers Heerspink, H.J.; Gansevoort, R.T. Albuminuria Is an Appropriate Therapeutic Target in Patients with CKD: The Pro View. Clin. J. Am. Soc. Nephrol. 2015, 10, 1079–1088. [Google Scholar] [CrossRef]
- Leone, A.; Fernández-Montero, A.; de la Fuente-Arrillaga, C.; Martínez-González, M.; Bertoli, S.; Battezzati, A.; Bes-Rastrollo, M. Adherence to the Mediterranean Dietary Pattern and Incidence of Nephrolithiasis in the Seguimiento Universidad de Navarra Follow-up (SUN) Cohort. Am. J. Kidney Dis. Off. J. Natl. Kidney Found. 2017, 70, 778–786. [Google Scholar] [CrossRef]
- Djukanović, L.; Djordjević, V.; Ležaić, V.; Cukuranović, R.; Marić, I.; Bukvić, D.; Marinković, J.; Cukuranović, J.; Rajić, M.; Stefanović, V. Urinary protein patterns in patients with Balkan endemic nephropathy. Int. Urol. Nephrol. 2013, 45, 1661–1669. [Google Scholar] [CrossRef]
- Chen, S.; Chen, J.; Li, S.; Guo, F.; Li, A.; Wu, H.; Chen, J.; Pan, Q.; Liao, S.; Liu, H.F.; et al. High-Fat Diet-Induced Renal Proximal Tubular Inflammatory Injury: Emerging Risk Factor of Chronic Kidney Disease. Front. Physiol. 2021, 12, 786599. [Google Scholar] [CrossRef]
- Altavilla, C.; Caballero-Pérez, P. An update of the KIDMED questionnaire, a Mediterranean Diet Quality Index in children and adolescents. Public Health Nutr. 2019, 22, 2543–2547. [Google Scholar] [CrossRef]
- Blazek, K.; van Zwieten, A.; Saglimbene, V.; Teixeira-Pinto, A. A practical guide to multiple imputation of missing data in nephrology. Kidney Int. 2021, 99, 68–74. [Google Scholar] [CrossRef]
| Characteristics | KIDMED Index (Mediterranean Diet Adherence) | p | ||
|---|---|---|---|---|
| 0–3 (Low n = 173) | 4–7 (Intermediate n = 1042) | 8–12 (Good n = 699) | ||
| At baseline | ||||
| Boy (n (%))1 | 90 (52.0) | 506 (48.6) | 360 (51.5) | 0.41 |
| Age (year) 2 | 6.6 ± 0.3 | 6.6 ± 0.3 | 6.6 ± 0.3 | 0.64 |
| Height z-score 2 | 0.73 ± 0.94 | 0.62 ± 0.96 | 0.71 ± 0.95 | 0.12 |
| Weight z-score 2 | 0.78 ± 1.42 | 0.67 ± 1.43 | 0.74 ± 1.38 | 0.41 |
| Body mass index z-score 2 | 0.45 ± 1.58 | 0.37 ± 1.54 | 0.41 ± 1.52 | 0.76 |
| Systolic blood pressure (mmHg) 2 | 100 ± 9 | 101 ± 9 | 101 ± 8 | 0.27 |
| Diastolic blood pressure (mmHg) 2 | 56 ± 6 | 56 ± 6 | 56 ± 6 | 0.60 |
| Short sleep (<10 h/d) 1 | 149 (86.1) | 792 (76.0) | 500 (71.5) | <0.001 |
| Long screen time (≥2 h/d) 1 | 10 (5.8) | 55 (5.3) | 30 (4.3) | 0.57 |
| Insufficient physical activity (<1 h/d) 1 | 136 (78.6) | 789 (75.7) | 526 (75.3) | 0.65 |
| Urinary β2-MG excretion (mg/L) 3 | ||||
| Wave 1 | 0.09 (0.04–0.15) | 0.08 (0.04–0.13) | 0.08 (0.04–0.12) | 0.34 |
| Wave 2 | 0.15 (0.12–0.18) | 0.14 (0.12–0.18) | 0.14 (0.12–0.18) | 0.15 |
| Wave 3 | 0.16 (0.13–0.21) | 0.17 (0.13–0.21) | 0.16 (0.13–0.20) | 0.017 |
| Wave 4 | 0.17 (0.13–0.22) | 0.16 (0.13–0.21) | 0.16 (0.13–0.21) | 0.42 |
| Urinary MA excretion (mg/L) 3 | ||||
| Wave 1 | 9.67 (6.57–13.14) | 9.19 (6.54–12.78) | 8.76 (6.30–11.80) | 0.027 |
| Wave 2 | 7.15 (6.20–9.20) | 6.70 (6.10–8.50) | 6.60 (6.00–8.40) | 0.046 |
| Wave 3 | 7.30 (6.30–9.20) | 7.10 (6.30–9.50) | 7.00 (6.20–8.80) | 0.10 |
| Wave 4 | 6.90 (6.00–10.50) | 6.80 (6.00–9.00) | 6.65 (6.00–8.70) | 0.089 |
| Dependent Variable | Independent Variable | Model 1 | Model 2 | Model 3 | |||
|---|---|---|---|---|---|---|---|
| Estimate (95%CI) | p | Estimate (95%CI) | p | Estimate (95%CI) | p | ||
| Urinary β2-MG excretion | KIDMED score | −0.001 (−0.003, 0.001) | 0.20 | −0.001 (−0.002, 0.001) | 0.28 | −0.001 (−0.003, 0) | 0.13 |
| Urinary MA excretion | KIDMED score | −0.218 (−0.359, −0.076) | 0.003 | −0.206 (−0.347, −0.065) | 0.004 | −0.216 (−0.358, −0.074) | 0.003 |
| Dependent Variable | Independent Variable | Model 1 | Model 2 | Model 3 | |||
|---|---|---|---|---|---|---|---|
| cOR (95%CI) | p | aOR (95%CI) | p | aOR (95%CI) | p | ||
| Renal tubular impairment | KIDMED index 0–3 | 1 | 1 | 1 | |||
| KIDMED index 4–7 | 0.90 (0.72, 1.12) | 0.33 | 0.90 (0.72, 1.12) | 0.35 | 0.88 (0.70, 1.10) | 0.25 | |
| KIDMED index 8–12 | 0.86 (0.69, 1.09) | 0.22 | 0.87 (0.69, 1.10) | 0.26 | 0.84 (0.67, 1.07) | 0.16 | |
| Renal glomerular impairment | KIDMED index 0–3 | 1 | 1 | 1 | |||
| KIDMED index 4–7 | 0.71 (0.50, 1.03) | 0.068 | 0.70 (0.48, 1.00) | 0.051 | 0.68 (0.47, 0.99) | 0.044 | |
| KIDMED index 8–12 | 0.61 (0.41, 0.91) | 0.016 | 0.62 (0.41, 0.92) | 0.018 | 0.60 (0.40, 0.90) | 0.014 | |
| KIDMED Test Item | Score | Renal Tubular Impairment n (%) | Renal Glomerular Impairment n (%) |
|---|---|---|---|
| Takes a fruit or fruit juice every day | |||
| Yes | +1 | 1190 (19.1) | 294 (4.7) |
| No | 0 | 161 (21.8) | 49 (6.6) |
| Has a second fruit every day | |||
| Yes | +1 | 752 (18.7) | 187 (4.6) |
| No | 0 | 599 (20.4) | 156 (5.3) |
| Has fresh or cooked vegetables regularly once a day | |||
| Yes | +1 | 1312 (19.4) | 327 (4.8) |
| No | 0 | 39 (18.0) | 16 (7.4) |
| Has fresh or cooked vegetables more than once a day | |||
| Yes | +1 | 1044 (19.0) | 244 (4.4) |
| No | 0 | 307 (20.8) | 99 (6.7) |
| Consumes fish regularly (at least 2–3 times per week) | |||
| Yes | +1 | 409 (19.5) | 99 (4.7) |
| No | 0 | 942 (19.4) | 244 (5.0) |
| Likes pulses and eats them more than once a week | |||
| Yes | +1 | 813 (19.4) | 200 (4.8) |
| No | 0 | 538 (19.4) | 143 (5.2) |
| Consumes pasta or rice almost every day (5 or more times per week) | |||
| Yes | +1 | 1210 (18.9) | 308 (4.8) |
| No | 0 | 141 (24.5) | 35 (6.1) |
| Has cereals or grains (bread, etc.) for breakfast | |||
| Yes | +1 | 851 (20.1) | 208 (4.9) |
| No | 0 | 500 (18.3) | 135 (4.9) |
| Consumes nuts regularly (at least 2–3 times per week) | |||
| Yes | +1 | 516 (19.4) | 128 (4.8) |
| No | 0 | 835 (19.4) | 215 (5.0) |
| Uses olive oil at home | |||
| Yes | +1 | 196 (19.0) | 47 (4.6) |
| No | 0 | 1155 (19.5) | 296 (5.0) |
| Has a dairy product for breakfast (yoghurt, milk, etc.) | |||
| Yes | +1 | 872 (19.8) | 202 (4.6) |
| No | 0 | 479 (18.7) | 141 (5.5) |
| Takes two yoghurts and/or some cheese (40 g) daily | |||
| Yes | +1 | 464 (19.4) | 104 (4.4) |
| No | 0 | 887 (19.4) | 239 (5.2) |
| Goes more than once a week to a fast-food (hamburger) restaurant | |||
| Yes | −1 | 54 (23.0) | 14 (6.0) |
| No | 0 | 1297 (19.3) | 329 (4.9) |
| Skips breakfast | |||
| Yes | −1 | 78 (22.8) | 12 (3.5) |
| No | 0 | 1273 (19.2) | 331 (5.0) |
| Has commercially baked goods or pastries for breakfast | |||
| Yes | −1 | 322 (19.7) | 76 (4.6) |
| No | 0 | 1029 (19.3) | 267 (5.0) |
| Takes sweets and candy several times every day | |||
| Yes | −1 | 199 (19.7) | 76 (7.5) |
| No | 0 | 1152 (19.3) | 267 (4.5) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Li, M.; Xiao, H.; Shu, W.; Amaerjiang, N.; Zunong, J.; Huang, D.; Hu, Y. Good Adherence to the Mediterranean Diet Lowered Risk of Renal Glomerular Impairment in Children: A Longitudinal Study. Nutrients 2022, 14, 3343. https://doi.org/10.3390/nu14163343
Li M, Xiao H, Shu W, Amaerjiang N, Zunong J, Huang D, Hu Y. Good Adherence to the Mediterranean Diet Lowered Risk of Renal Glomerular Impairment in Children: A Longitudinal Study. Nutrients. 2022; 14(16):3343. https://doi.org/10.3390/nu14163343
Chicago/Turabian StyleLi, Menglong, Huidi Xiao, Wen Shu, Nubiya Amaerjiang, Jiawulan Zunong, Dayong Huang, and Yifei Hu. 2022. "Good Adherence to the Mediterranean Diet Lowered Risk of Renal Glomerular Impairment in Children: A Longitudinal Study" Nutrients 14, no. 16: 3343. https://doi.org/10.3390/nu14163343
APA StyleLi, M., Xiao, H., Shu, W., Amaerjiang, N., Zunong, J., Huang, D., & Hu, Y. (2022). Good Adherence to the Mediterranean Diet Lowered Risk of Renal Glomerular Impairment in Children: A Longitudinal Study. Nutrients, 14(16), 3343. https://doi.org/10.3390/nu14163343







