Urbanization and Unfavorable Changes in Metabolic Profiles: A Prospective Cohort Study of Indonesian Young Adults
Abstract
:1. Introduction
2. Methods
2.1. Study Design and Population
2.2. Anthropometric Measurements
2.3. Fasting Blood Glucose, HbA1c, Fasting Insulin, and HOMA-IR Measurement
2.4. Leptin, Adiponectin, and Leptin/Adiponectin Ratio
2.5. Dietary Intake Analysis
2.6. Physical Activity Analysis
2.7. Statistical Analysis
3. Results
3.1. Study Population
3.2. Metabolic Profiles of Urban vs. Rural Subjects at Baseline
3.3. Dietary Intake and Physical Activity at Baseline
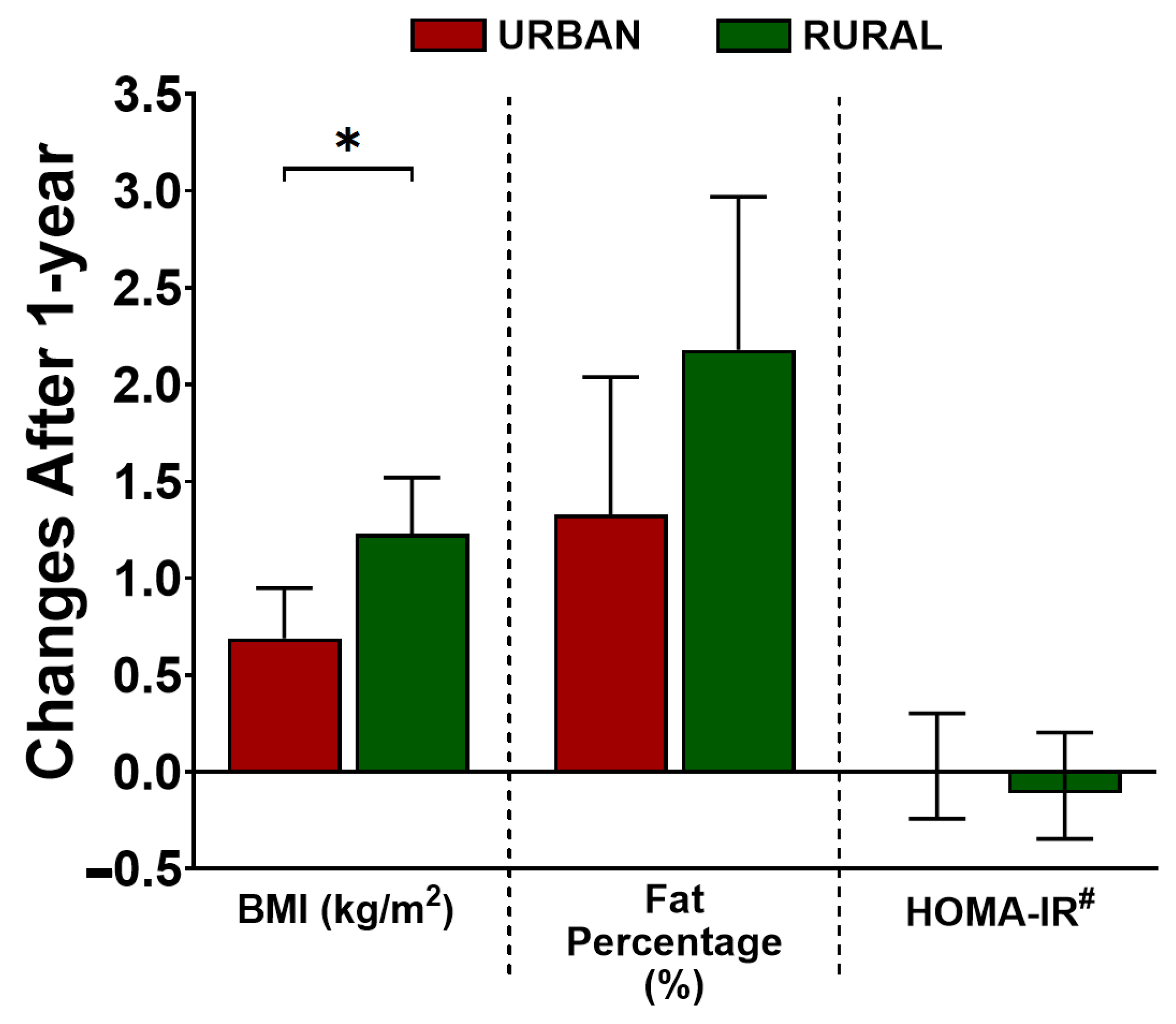
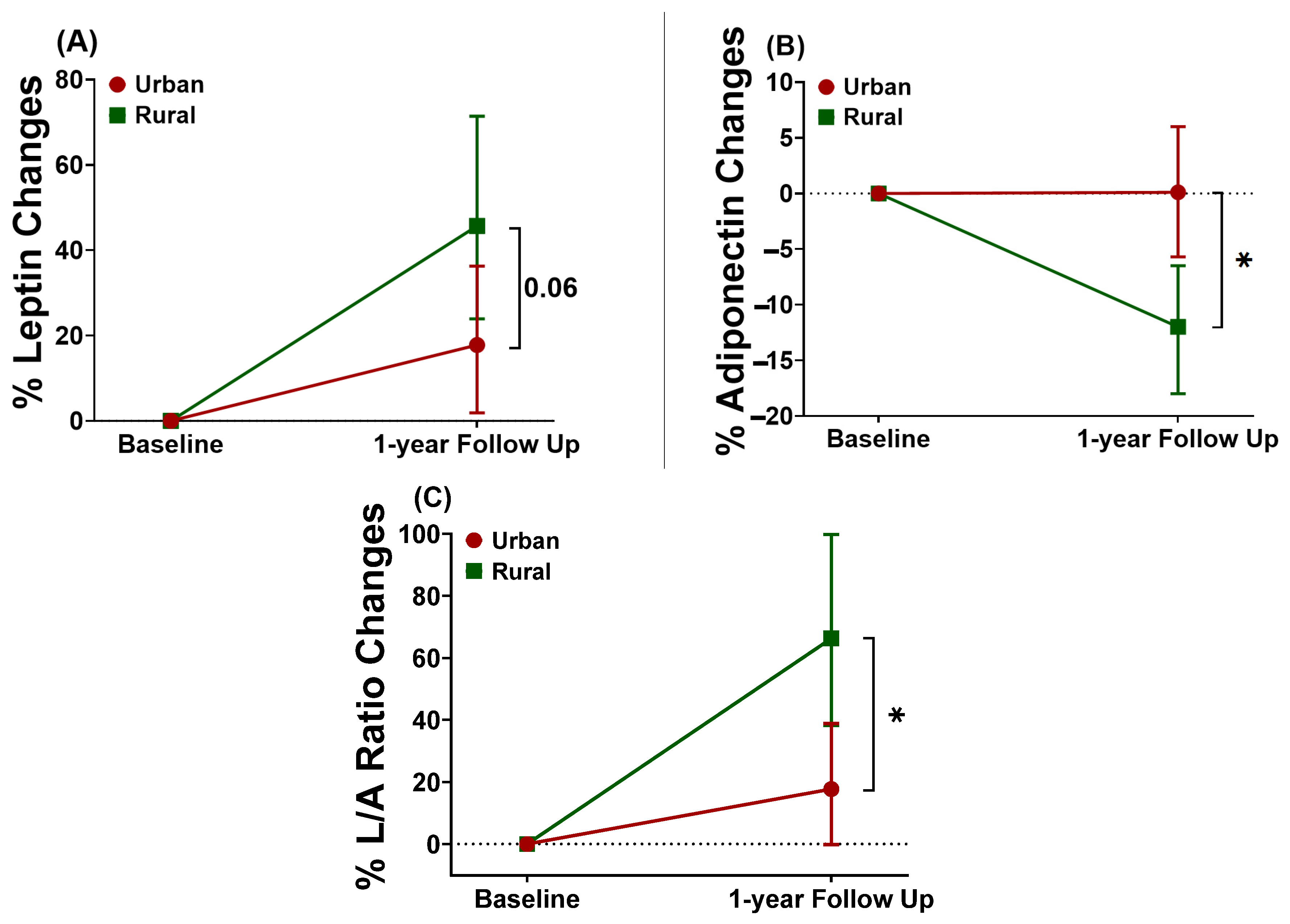
3.4. Effect of Urbanization over Time on Adiposity Profiles, Insulin Resistance, and Adipokines
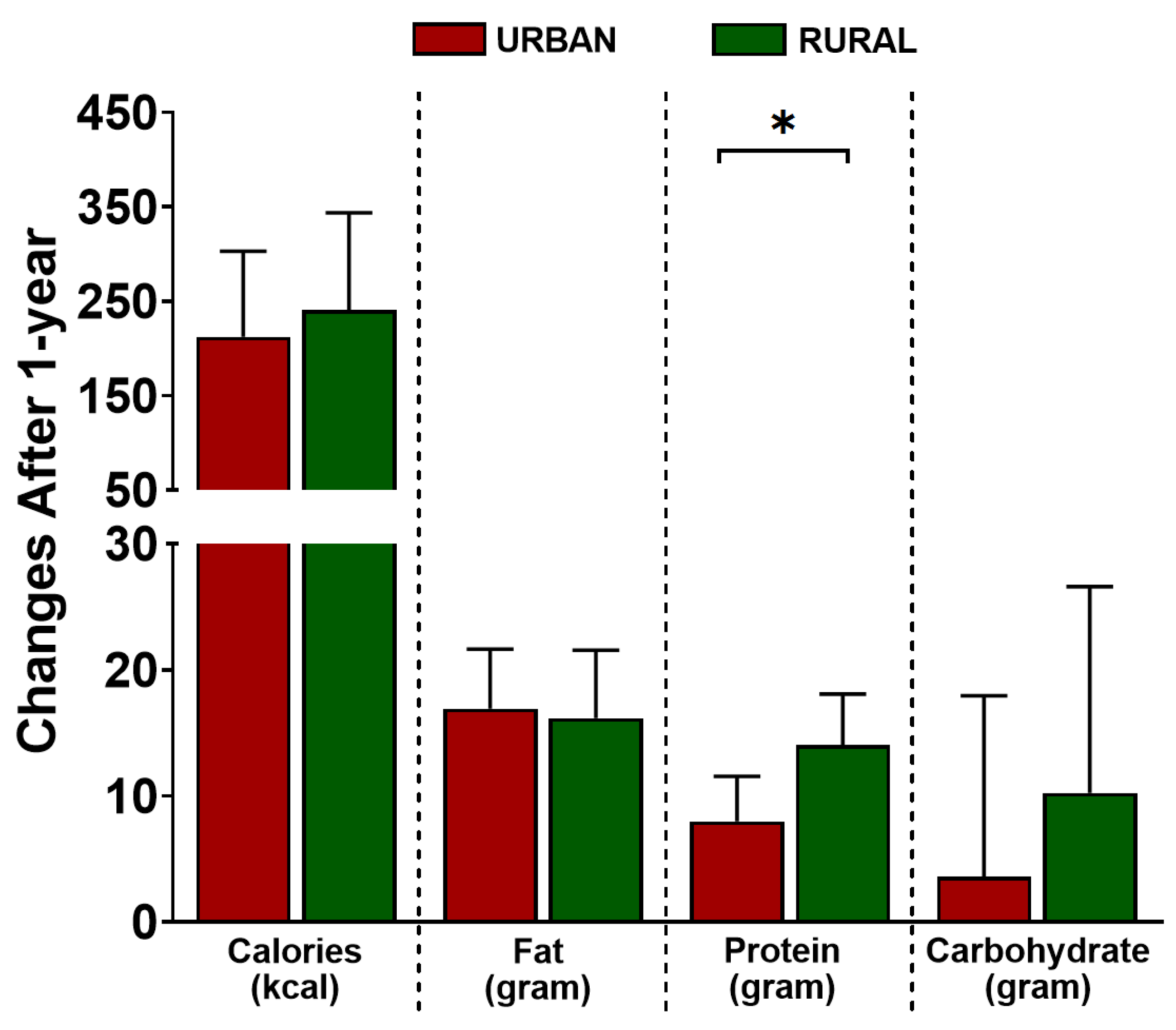
3.5. Effect of Urbanization over Time on Dietary Intake and Physical Activity
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Htet, A.S.; Bjertness, M.B.; Sherpa, L.Y.; Kjollesdal, M.K.; Oo, W.M.; Meyer, H.E.; Stigum, H.; Bjertness, E. Urban-rural differences in the prevalence of non-communicable diseases risk factors among 25–74 years old citizens in Yangon Region, Myanmar: A cross sectional study. BMC Public Health 2016, 16, 1225. [Google Scholar] [CrossRef]
- Neiderud, C.J. How urbanization affects the epidemiology of emerging infectious diseases. Infect Ecol Epidemiol. 2015, 5, 27060. [Google Scholar] [CrossRef] [PubMed]
- Mayen, A.L.; Marques-Vidal, P.; Paccaud, F.; Bovet, P.; Stringhini, S. Socioeconomic determinants of dietary patterns in low- and middle-income countries: A systematic review. Am. J. Clin. Nutr. 2014, 100, 1520–1531. [Google Scholar] [CrossRef] [PubMed]
- Mashili, F.L.; Kagaruki, G.B.; Mbatia, J.; Nanai, A.; Saguti, G.; Maongezi, S.; Magimba, A.; Mghamba, J.; Kamugisha, M.; Mgina, E.; et al. Physical activity and associated socioeconomic determinants in rural and urban Tanzania: Results from the 2012 WHO-STEPS Survey. Int. J. Popul. Res. 2018, 4965193. [Google Scholar] [CrossRef]
- Hall, K.D.; Heymsfield, S.B.; Kemnitz, J.W.; Klein, S.; Schoeller, D.A.; Speakman, J.R. Energy balance and its components: Implications for body weight regulation. Am. J. Clin. Nutr. 2012, 95, 989–994. [Google Scholar] [CrossRef] [PubMed]
- Hill, J.O.; Wyatt, H.R.; Peters, J.C. Energy balance and obesity. Circulation 2012, 126, 126–132. [Google Scholar] [CrossRef] [PubMed]
- Schuster, D.P. Obesity and the development of type 2 diabetes: The effects of fatty tissue inflammation. Diabetes Metab Syndr Obes 2010, 3, 253–262. [Google Scholar] [CrossRef] [PubMed]
- Chen, P.; Hou, X.; Hu, G.; Wei, L.; Jiao, L.; Wang, H.; Chen, S.; Wu, J.; Bao, Y.; Jia, W. Abdominal subcutaneous adipose tissue: A favorable adipose depot for diabetes? Cardiovasc. Diabetol 2018, 17, 93. [Google Scholar] [CrossRef] [PubMed]
- Ha, E.E.; Bauer, R.C. Emerging roles for adipose tissue in cardiovascular disease. Arter. Thromb. Vasc. Biol. 2018, 38, e137–e144. [Google Scholar] [CrossRef]
- Bloom, D.E.; Canning, D.; Fink, G. Urbanization and the wealth of nations. Science 2008, 319, 772–775. [Google Scholar] [CrossRef]
- Ebrahim, S.; Kinra, S.; Bowen, L.; Andersen, E.; Ben-Shlomo, Y.; Lyngdoh, T.; Ramakrishnan, L.; Ahuja, R.C.; Joshi, P.; Das, S.M.; et al. The effect of rural-to-urban migration on obesity and diabetes in India: A cross-sectional study. PLoS Med. 2010, 7, e1000268. [Google Scholar] [CrossRef] [PubMed]
- Ruiz-Alejos, A.; Carrillo-Larco, R.M.; Miranda, J.J.; Anderson, C.A.M.; Gilman, R.H.; Smeeth, L.; Bernabe-Ortiz, A. Addressing the impact of urban exposure on the incidence of type 2 diabetes mellitus: The PERU MIGRANT Study. Sci. Rep. 2018, 8, 5512. [Google Scholar] [CrossRef] [PubMed]
- Sobngwi, E.; Mbanya, J.C.; Unwin, N.C.; Porcher, R.; Kengne, A.P.; Fezeu, L.; Minkoulou, E.M.; Tournoux, C.; Gautier, J.F.; Aspray, T.J.; et al. Exposure over the life course to an urban environment and its relation with obesity, diabetes, and hypertension in rural and urban Cameroon. Int. J. Epidemiol. 2004, 33, 769–776. [Google Scholar] [CrossRef] [PubMed]
- Poobalan, A.; Aucott, L. Obesity Among Young Adults in Developing Countries: A Systematic Overview. Curr. Obes. Rep. 2016, 5, 2–13. [Google Scholar] [CrossRef] [PubMed]
- National Institute for Health Research and Development (NIHRD), Ministry of Health, Republic of Indonesia. Laporan Nasional RISKESDAS. Jakarta. 2018. Available online: http://labdata.litbang.kemkes.go.id/riset-badan-litbangkes/menu-riskesnas/menu-riskesdas/426-rkd-2018 (accessed on 24 April 2021).
- Indonesian Central Bureau of Statistics, Hasil Sensus Penduduk 2020. Report No.: Berita Resmi Statistik No. 7/01/Th. XXIV; Indonesian Central Bureau of Statistics: Jakarta, Indonesia, 2021.
- Radziuk, J. Homeostastic model assessment and insulin sensitivity/resistance. Diabetes 2014, 63, 1850–1854. [Google Scholar] [CrossRef]
- Lopez-Jaramillo, P.; Gomez-Arbelaez, D.; Lopez-Lopez, J.; Lopez-Lopez, C.; Martinez-Ortega, J.; Gomez-Rodriguez, A.; Triana-Cubillos, S. The role of leptin/adiponectin ratio in metabolic syndrome and diabetes. Horm. Mol. Biol. Clin. Investig. 2014, 18, 37–45. [Google Scholar] [CrossRef]
- Ortega, R.M.; Perez-Rodrigo, C.; Lopez-Sobaler, A.M. Dietary assessment methods: Dietary records. Nutr. Hosp. 2015, 31, 38–45. [Google Scholar]
- Rupasinghe, W.S.; Perera, H.; Wickramaratne, N. A comprehensive review on dietary assessment methods in epidemiological research. J. Pub. Health Nutri. 2020, 3, 204–211. [Google Scholar]
- Armstrong, T.; Bull, F. Development of the World Health Organization Global Physical Activity Questionnaire (GPAQ). J. Public Health-Heid 2006, 14, 66–70. [Google Scholar] [CrossRef]
- Bull, F.C.; Maslin, T.S.; Armstrong, T. Global physical activity questionnaire (GPAQ): Nine country reliability and validity study. J. Phys. Act. Health 2009, 6, 790–804. [Google Scholar] [CrossRef]
- Global Physical Activity Questionnaire (GPAQ) Analysis Guide. World Health Organization. 2012. Available online: http://www.who.int/chp/steps/resources/GPAQ_Analysis_Guide.pdf (accessed on 2 April 2021).
- Wanner, M.; Hartmann, C.; Pestoni, G.; Martin, B.W.; Siegrist, M.; Martin-Diener, E. Validation of the Global Physical Activity Questionnaire for self-administration in a European context. BMJ Open Sport Exerc. Med. 2017, 3, e000206. [Google Scholar] [CrossRef] [PubMed]
- Hayes, A.H. Introduction to Mediation, Moderation, and Conditional Process Analysis. In A Regression-Based Approach, 3rd ed.; Guilford Press: New York, NY, USA, 2022. [Google Scholar]
- Bates, D.; Mächler, M.; Bolker, B.; Walker, S. Fitting linear mixed-effects models using lme4. J. Stat. Softw. 2015, 67, 1–48. [Google Scholar] [CrossRef]
- Kuznetsova, A.; Brockhoff, P.B.; Christensen, R.H.B. lmerTest package: Tests in linear mixed effects models. J. Stat. Softw. 2017, 82, 1–26. [Google Scholar] [CrossRef]
- World Health Organization. Regional Office for the Western Pacific Region. In The Asia-Pacific perspective: Redefining Obesity and Its Treatment; Health Communications: Sydney, Australia, 2000. [Google Scholar]
- Nurwanti, E.; Hadi, H.; Chang, J.S.; Chao, J.C.J.; Paramashanti, B.A.; Gittelsohn, J.; Bai, C.H. Rural-urban differences in dietary behavior and obesity: Results of the Riskesdas study in 10-18-year-old Indonesian children and adolescents. Nutrients 2019, 11, 2813. [Google Scholar] [CrossRef]
- Beaudry, K.M.; Ludwa, I.A.; Thomas, A.M.; Ward, W.E.; Falk, B.; Josse, A.R. First-year university is associated with greater body weight, body composition and adverse dietary changes in males than females. PLoS ONE 2019, 14, e0218554. [Google Scholar] [CrossRef]
- Vadeboncoeur, C.; Foster, C.; Townsend, N. Freshman 15 in England: A longitudinal evaluation of first year university student’s weight change. BMC Obes. 2016, 3, 45. [Google Scholar]
- Vergnaud, A.C.; Norat, T.; Romaguera, D.; Mouw, T.; May, A.M.; Travier, N.; Luan, J.; Wareham, N.; Slimani, N.; Rinaldi, S.; et al. Meat consumption and prospective weight change in participants of the EPIC-PANACEA study. Am. J. Clin. Nutr. 2010, 92, 398–407. [Google Scholar] [CrossRef]
- Ojiambo, R.M.; Easton, C.; Casajus, J.A.; Konstabel, K.; Reilly, J.J.; Pitsiladis, Y. Effect of urbanization on objectively measured physical activity levels, sedentary time, and indices of adiposity in Kenyan adolescents. J. Phys. Act. Health 2012, 9, 115–123. [Google Scholar] [CrossRef]
- Bowen, L.; Taylor, A.E.; Sullivan, R.; Ebrahim, S.; Kinra, S.; Krishna, K.V.R.; Kulkarni, B.; Ben-Shlomo, Y.; Ekelund, U.; Wells, J.C.K.; et al. Associations between diet, physical activity and body fat distribution: A cross sectional study in an Indian population. BMC Public Health 2015, 15, 281. [Google Scholar] [CrossRef]
- Martin, S.L.; Kirkner, G.J.; Mayo, K.; Matthews, C.E.; Durstine, J.L.; Hebert, J.R. Urban, rural, and regional variations in physical activity. J. Rural Health 2005, 21, 239–244. [Google Scholar] [CrossRef]
- Mumu, S.J.; Ali, L.; Barnett, A.; Merom, D. Validity of the global physical activity questionnaire (GPAQ) in Bangladesh. BMC Public Health 2017, 17, 650. [Google Scholar] [CrossRef] [PubMed]
- Murphy, E.F.; Cotter, P.D.; Healy, S.; Marques, T.M.; O’Sullivan, O.; Fouhy, F.; Clarke, S.F.; O’Toole, P.W.; Quigley, E.M.; Stanton, C.; et al. Composition and energy harvesting capacity of the gut microbiota: Relationship to diet, obesity and time in mouse models. Gut 2010, 59, 1635–1642. [Google Scholar] [CrossRef] [PubMed]
- Cuevas-Sierra, A.; Ramos-Lopez, O.; Riezu-Boj, J.I.; Milagro, F.I.; Martinez, J.A. Diet, gut microbiota, and obesity: Links with host genetics and epigenetics and potential applications. Adv. Nutr. 2019, 10, S17–S30. [Google Scholar] [CrossRef] [PubMed]
- Boyce, J.A.; Kuijer, R.G. Perceived stress and freshman weight change: The moderating role of baseline body mass index. Physiol. Behav. 2015, 139, 491–496. [Google Scholar] [CrossRef]
- Arnetz, B.B.; Templin, T.N.; Jen, K.C.; Sudan, S.; Arnetz, J.E. Lifestyle and psychosocial factors associated with maintenance of normal body mass index in college students: A cross sectional study. BMC Res. Notes 2020, 13, 516. [Google Scholar]
- Baum, C.L. The effects of college on weight: Examining the ‘Freshman 15’ myth and other effects of college over the life cycle. Demography 2017, 54, 311–336. [Google Scholar] [CrossRef]
- Haldar, S.; Chia, S.C.; Henry, C.J. Body composition in Asians and Caucasians: Comparative analyses and influences on cardiometabolic outcomes. Adv. Food Nutr. Res. 2015, 75, 97–154. [Google Scholar]
- Wulan, S.N.; Westerterp, K.R.; Plasqui, G. Ethnic differences in body composition and the associated metabolic profile: A comparative study between Asians and Caucasians. Maturitas 2010, 65, 315–319. [Google Scholar] [CrossRef]
- Grillol, L.P.; Siqueira, A.F.; Silva, A.C.; Martins, P.A.; Verreschi, I.T.; Sawaya, A.L. Lower resting metabolic rate and higher velocity of weight gain in a prospective study of stunted vs nonstunted girls living in the shantytowns of Sao Paulo, Brazil. Eur. J. Clin. Nutr. 2005, 59, 835–842. [Google Scholar] [CrossRef]
- Hoffman, D.J.; Sawaya, A.L.; Verreschi, I.; Tucker, K.L.; Roberts, S.B. Why are nutritionally stunted children at increased risk of obesity? Studies of metabolic rate and fat oxidation in shantytown children from Sao Paulo, Brazil. Am. J. Clin. Nutr. 2000, 72, 702–707. [Google Scholar] [CrossRef]
- Wells, J.C.; Sawaya, A.L.; Wibaek, R.; Mwangome, M.; Poullas, M.S.; Yajnik, C.S.; Demaio, A. The double burden of malnutrition: Aetiological pathways and consequences for health. Lancet 2020, 395, 75–88. [Google Scholar] [CrossRef]
- Thanikachalam, M.; Fuller, C.H.; Lane, K.J.; Sunderarajan, J.; Harivanzan, V.; Brugge, D.; Thanikachalam, S. Urban environment as an independent predictor of insulin resistance in a South Asian population. Int. J. Health Geogr. 2019, 18, 5. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; Li, H.; Franco, O.H.; Yu, Z.; Liu, Y.; Lin, X. Adiponectin and metabolic syndrome in middle-aged and elderly Chinese. Obesity 2008, 16, 172–178. [Google Scholar] [CrossRef] [PubMed]
- Yao, H.; Fan, C.; Fan, X.; Lu, Y.; Wang, Y.; Wang, R.; Tang, T.; Qi, K. Effects of gut microbiota on leptin expression and body weight are lessened by high-fat diet in mice. Br. J. Nutr. 2020, 124, 396–406. [Google Scholar] [CrossRef]
- Yao, H.Y.; Fan, C.N.; Lu, Y.Y.; Fan, X.Q.; Xia, L.L.; Li, P.; Wang, R.; Tang, T.T.; Wang, Y.Y.; Qi, K.M. Alteration of gut microbiota affects expression of adiponectin and resistin through modifying DNA methylation in high-fat diet-induced obese mice. Genes Nutr. 2020, 15, 12. [Google Scholar] [CrossRef]
- Bidulescu, A.; Dinh, P.C.; Sarwary, S.; Forsyth, E.; Luetke, M.C.; King, D.B.; Liu, J.K.; Davis, S.K.; Correa, A. Associations of leptin and adiponectin with incident type 2 diabetes and interactions among African Americans: The Jackson heart study. BMC Endocr. Disord. 2020, 20, 31. [Google Scholar] [CrossRef]
- Aguayo-Mazzucato, C. Functional changes in beta cells during ageing and senescence. Diabetologia 2020, 63, 2022–2029. [Google Scholar] [CrossRef]
- Wengreen, H.J.; Moncur, C. Change in diet, physical activity, and body weight among young-adults during the transition from high school to college. Nutr. J. 2009, 8, 32. [Google Scholar] [CrossRef]
- Bixby, H.; Bentham, J.; Zhou, B.; Di Cesare, M.; Paciorek, C.J.; Bennett, J.E.; Taddei, C.; Stevens, G.A.; Rodriguez-Martinez, A.; Carrillo-Larco, R.M.; et al. Rising rural body-mass index is the main driver of the global obesity epidemic in adults. Nature 2019, 569, 260–264. [Google Scholar]
| Variables | Urban N = 106 | Rural N = 83 | p Values # (Adjusted for Age and Sex) | p Values # (Adjusted for Age, Sex, and BMI) |
|---|---|---|---|---|
| Age, yrs old (mean, SD) | 18.4 (0.7) | 18.6 (0.7) | 0.09 | |
| Sex, n male (%) | 39 (36.8) | 31 (37.3) | 0.94 | |
| BMI, kg/m2 (mean, SD) | 22.9 (5.0) | 20.0 (3.2) | <0.001 | |
BMI grouping, n (%)
| 14 (13.2) 50 (47.2) 17 (16.0) 25 (23.6) | 28 (33.7) 41 (49.4) 7 (8.4) 7 (8.4) | 0.001 | |
| Waist circumference, cm (mean, SD) | 78.5 (12.8) | 72.1 (8.2) | <0.001 | |
| Fat percentage, % (mean, SD) | 28.2 (9.1) | 22.8 (8.3) | <0.001 | |
| FBG, mg/dL (mean, SD) | 87.1 (8.2) | 86.7 (7.8) | 0.54 | |
| HbA1c, % (mean, SD) | 5.1 (0.4) | 5.1 (0.3) | 0.24 | |
| Fasting insulin †, IU/mL | 5.3 (4.3–6.6) | 2.9 (2.2–3.8) | 0.001 | 0.06 |
| HOMA-IR † | 1.1 (0.9–1.4) | 0.6 (0.5–0.8) | 0.001 | 0.06 |
| Leptin †, ng/mL | 11.6 (9.7–13.8) | 6.9 (5.3–9.1) | <0.001 | 0.07 |
| Adiponectin †, µg/mL | 4.1 (3.7–4.5) | 4.9 (4.4–5.3) | 0.02 | 0.19 |
| Leptin-Adiponectin (L/A) Ratio † | 2.9 (2.3–3.5) | 1.4 (1.1–1.9) | <0.001 | 0.03 |
Dietary intake, mean (SD)
| 1444 (335) 52 (15) 50 (14) | 1289 (422) 44 (16) 41 (13) | 0.002 <0.001 <0.001 | 0.009 0.01 0.001 |
| 193 (55) | 179 (73) | 0.08 | 0.06 |
| Variables † | Adjusted for Age and Sex | Pint | Adjusted for Age, Sex, and BMI | Pint | ||||
|---|---|---|---|---|---|---|---|---|
| Urban | Rural | Urban | Indirect Effect # | Rural | Indirect Effect # | |||
| Leptin | 0.24 | 0.54 | 0.06 | 0.09 | −0.25; −0.07 | 0.33 | −0.29; −0.12 | 0.12 |
| (0.03; 0.45) | (0.31; 0.78) | (−0.11; 0.29) | (0.10; 0.55) | |||||
| p = 0.03 | p < 0.001 | p = 0.38 | p = 0.005 | |||||
| Adiponectin | 0.002 | −0.19 | 0.003 | 0.04 | 0.01; 0.06 | −0.12 | 0.03; 0.10 | 0.008 |
| (−0.08; 0.09) | (−0.29; −0.10) | (−0.04; 0.12) | (−0.22; −0.03) | |||||
| p = 0.97 | p < 0.001 | p = 0.34 | p = 0.008 | |||||
| L/A ratio | 0.23 | 0.73 | 0.006 | 0.06 | −0.30, −0.08 | 0.45 | −0.39; −0.17 | 0.02 |
| (−0.003; 0.47) | (0.47; 1.00) | (−0.16; 0.28) | (0.20; 0.70) | |||||
| p = 0.05 | p < 0.001 | p = 0.60 | p < 0.001 | |||||
| Model † | Urban | Rural | Pint | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Estimate (95%CI) | p Values | % Changes †† | Indirect Effect # (95%CI) | Estimate (95%CI) | p Values | % Changes †† | Indirect Effect # (95%CI) | ||
| Adjusted for age and sex | 0.69 (0.43, 0.95) | <0.001 | 1.23 (0.94; 1.52) | <0.001 | 0.007 | ||||
| Model with changes in dietary intake | |||||||||
| (+) Total calories intake | 0.55 (0.28; 0.28) | <0.001 | −20.3 | −0.13 (−0.33; −0.02) | 1.02 (0.71; 1.32) | <0.001 | −17.1 | −0.15 (−0.52; −0.04) | 0.02 |
| (+) Carbohydrate intake | 0.68 (0.42; 0.93) | <0.001 | −1.4 | −0.01 (−0.12; 0.03) | 1.14 (0.85; 1.43) | <0.001 | −7.3 | −0.09 (−0.34; 0.01) | 0.02 |
| (+) Fat intake | 0.49 (0.20; 0.78) | <0.001 | −29.0 | −0.20 (−0.47; −0.04) | 0.99 (0.67; 1.31) | <0.001 | −19.5 | −0.24 (−0.54; −0.06) | 0.01 |
| (+) Protein intake | 0.65 (0.38; 0.93) | <0.001 | −5.8 | −0.04 (−0.22; 0.08) | 1.12 (0.78; 1.45) | <0.001 | −8.9 | −0.11 (−0.43; 0.14) | 0.02 |
| (+) Fat and protein intake | 0.50 (0.21; 0.79) | <0.001 | −27.5 | −0.19 (−0.48; 0.02) | 1.04 (0.70; 1.37) | <0.001 | −15.4 | −0.19 (−0.53; 0.05) | 0.007 |
| Model with changes in physical activity | |||||||||
| (+) Total volume of MVPA | 0.68 (0.42; 0.95) | <0.001 | −1.4 | −0.01 (−0.14; 0.05) | 1.23 (0.94; 1.52) | <0.001 | 0.0 | 0.0 (−0.10; 0.04) | 0.007 |
| (+) Total minutes of MVPA | 0.68 (0.42; 0.95) | <0.001 | −1.4 | −0.01 (−0.15; 0.06) | 1.23 (0.94; 1.52) | <0.001 | 0.0 | 0.0 (−0.10; 0.05) | 0.007 |
| (+) Total sedentary time | 0.70 (0.44; 0.96) | <0.001 | 1.4 | 0.01 (−0.03; 0.10) | 1.26 (0.94; 1.58) | <0.001 | 2.4 | 0.03 (−0.11; 0.22) | 0.007 |
| Model with changes in dietary intake and physical activity | |||||||||
| (+) Fat and protein intake and total volume of MVPA | 0.48 (0.19; 0.78) | 0.001 | −30.4 | −0.21 (−0.50; −0.01) | 1.10 (0.75; 1.44) | <0.001 | −10.6 | −0.13 (−0.49; 0.15) | 0.003 |
| (+) Fat and protein intake and total minutes of MVPA | 0.49 (0.19; 0.78) | 0.001 | −29.0 | −0.20 (−0.51; −0.01) | 1.09 (0.75; 1.44) | <0.001 | −11.4 | −0.14 (−0.52; 0.14) | 0.003 |
| (+) Fat and protein intake and total sedentary time | 0.51 (0.22; 0.80) | <0.001 | −26.1 | −0.18 (−0.47; 0.001) | 1.15 (0.79; 1.50) | <0.001 | −6.5 | −0.08 (−0.47; 0.21) | 0.002 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kurniawan, F.; Manurung, M.D.; Harbuwono, D.S.; Yunir, E.; Tsonaka, R.; Pradnjaparamita, T.; Vidiawati, D.; Anggunadi, A.; Soewondo, P.; Yazdanbakhsh, M.; et al. Urbanization and Unfavorable Changes in Metabolic Profiles: A Prospective Cohort Study of Indonesian Young Adults. Nutrients 2022, 14, 3326. https://doi.org/10.3390/nu14163326
Kurniawan F, Manurung MD, Harbuwono DS, Yunir E, Tsonaka R, Pradnjaparamita T, Vidiawati D, Anggunadi A, Soewondo P, Yazdanbakhsh M, et al. Urbanization and Unfavorable Changes in Metabolic Profiles: A Prospective Cohort Study of Indonesian Young Adults. Nutrients. 2022; 14(16):3326. https://doi.org/10.3390/nu14163326
Chicago/Turabian StyleKurniawan, Farid, Mikhael D. Manurung, Dante S. Harbuwono, Em Yunir, Roula Tsonaka, Tika Pradnjaparamita, Dhanasari Vidiawati, Angelica Anggunadi, Pradana Soewondo, Maria Yazdanbakhsh, and et al. 2022. "Urbanization and Unfavorable Changes in Metabolic Profiles: A Prospective Cohort Study of Indonesian Young Adults" Nutrients 14, no. 16: 3326. https://doi.org/10.3390/nu14163326
APA StyleKurniawan, F., Manurung, M. D., Harbuwono, D. S., Yunir, E., Tsonaka, R., Pradnjaparamita, T., Vidiawati, D., Anggunadi, A., Soewondo, P., Yazdanbakhsh, M., Sartono, E., & Tahapary, D. L. (2022). Urbanization and Unfavorable Changes in Metabolic Profiles: A Prospective Cohort Study of Indonesian Young Adults. Nutrients, 14(16), 3326. https://doi.org/10.3390/nu14163326






