Abstract
The objective was to determine the most frequently consumed food items, food subcategories, and food categories, and those that contributed most to total energy intake for the group of U.S. adults reporting taking insulin, those with type 2 diabetes (T2D) not taking insulin, and those without diabetes. Laboratory tests and questionnaires of the National Health and Nutrition Examination Survey 2009–2016 classified 774 participants reporting taking insulin, 2758 participants reporting T2D not taking insulin, and 17,796 participants without diabetes. Raw and weighted frequency and energy contributions of each food item, food subcategory, and food category were calculated and ranked. Comparisons among groups by broad food category used the Rao–Scott modified chi-square test. Soft drinks ranked as the 8th and 6th most consumed food subcategory of participants with T2D not taking insulin and those without diabetes, and contributed 5th and 2nd most to energy, respectively. The group reporting taking insulin is likely to consume more protein foods and less soft drink compared to the other two groups. Lists of the most frequently reported foods and foods contributing most to energy may be helpful for nutrition education, prescribing diets, and digital-based dietary assessment for the group reporting taking insulin.
1. Introduction
Diabetes is a chronic disease highly influenced by diet where individuals either do not produce enough insulin to regulate blood glucose level or they are not able to use the insulin they produce to effectively move blood glucose into body cells [1]. Over time, diabetes can cause additional serious health problems, including heart disease, vision loss, and kidney disease. About 34.2 million U.S. individuals (10.5% of the U.S. population) had diabetes—type 1 (T1D), type 2 (T2D), and gestational diabetes—in 2020 [2].
Both those with T1D and T2D may use injectable insulin to control their blood glucose levels. Proper insulin dosing to control blood glucose levels and reduce the risk of severe consequences is dependent on dietary intake, particularly the frequency and energy from macronutrients: carbohydrate, protein, and fat [3,4]. Thus, quantification of the foods comprising dietary intake may be used to inform insulin dosing algorithms to enhance blood glucose level control [5,6], and knowledge of the foods comprising overall dietary intake may also aid in the creation of meal plans, inform substitutions, and other interventions. Furthermore, it is likely that insulin use may differentiate food and beverage choice and intake among those reporting diabetes, as dietary attention to manage blood glucose levels is necessary for insulin treatment. Glycemic control through insulin administration, as well as through oral antidiabetic agents, may be influenced by the macronutrients in the foods and also through insulin resistance, which may be boosted by some foods [7]. Therefore, among those with diabetes, whether T1D or T2D, using insulin may homogenize dietary behaviors compared to those with T2D but not taking insulin, and both groups may vary from the group of adults who do not have diabetes. Yet, very little information on the food intake of those taking insulin or those with T2D but not taking insulin is available [8]. Previous studies found that groups with diabetes had low diet quality or diets with little alignment to dietary recommendations [9,10] or evidence of significant differences in nutrient intake between groups with and without diabetes. Specifically, the group with diabetes consumed more calcium and sodium than the group without diabetes, and the group with continuous glucose monitoring and/or continuous subcutaneous insulin infusion consumed more protein and lipids but less carbohydrates and fiber than the group without continuous glucose monitoring and/or continuous subcutaneous insulin infusion [9,10,11]. Further studies evaluating differences among those using and not using insulin were not identified.
Therefore, the objectives of this study were to (1) determine and compare the lists of the most frequently consumed food items, food subcategories, and food categories and the food items, food subcategories, and food categories that contributed most to energy intake, and (2) compare the differences in the frequency of reported intake of the broad food categories and the contributions to energy of the broad food categories among those reporting taking insulin, those with T2D but not taking insulin, and those without diabetes among U.S. adults aged 18 years old or older using data from the National Health and Nutrition Examination Survey (NHANES) 2009–2016.
2. Materials and Methods
2.1. Participants and Dataset
NHANES is a cross-sectional survey that is conducted by the National Center for Health Statistics (NCHS) of the U.S. Centers for Disease Control and Prevention to assess the health and nutritional status of the non-institutionalized civilian population in the U.S. [12]. Participants’ sociodemographic information was obtained via questionnaires during the in-person household interview, which included age, sex, race/ethnicity, and poverty to income ratio (PIR). Participants’ BMI was obtained from health examination. The NCHS Research Ethics Review Board approved the survey, and all participants consented to participate [13].
2.2. Analytic Sample
NHANES 2009–2016 was used to include the most recent available dietary data and sufficient sample size. Reliable first 24-hour dietary recall used in the analysis, reliable laboratory test results, and valid answers to diabetic-related questions were drawn from adults aged 18 or older to make up the analytic sample data.
NHANES diabetes-related questions and laboratory test results were used to divide the sample into three groups: participants reporting taking insulin, participants with diabetes not taking insulin, and participants without diabetes. The number of the group reporting taking insulin was determined by the question “Are you/is the sample person now taking insulin?” Those participants with diabetes who were not taking insulin were identified by subtracting those using insulin from the total number of participants with diabetes. Diabetes was classified by self-reporting, being told they had diabetes by a doctor or taking medications that lowered glucose, or by fasting plasma glucose concentration ≥126 mg/dL or hemoglobin A1c ≥ 6.5% [14]. Since T1D was classified when a participant reported being diagnosed with diabetes before the age of 30 years and reporting continuous insulin use since diagnosis [15], the group reporting taking insulin encompassed all those with T1D, so participants with diabetes not taking insulin were in the same group as participants with T2D but not taking insulin. Those participants without diabetes were identified by subtracting the number of participants with diabetes from the sample. As a result, the study sample of foods and beverages used in the analysis was drawn from 774 participants reporting taking insulin, 2758 participants with T2D but not taking insulin, and 17,796 participants who did not have diabetes (Figure 1).
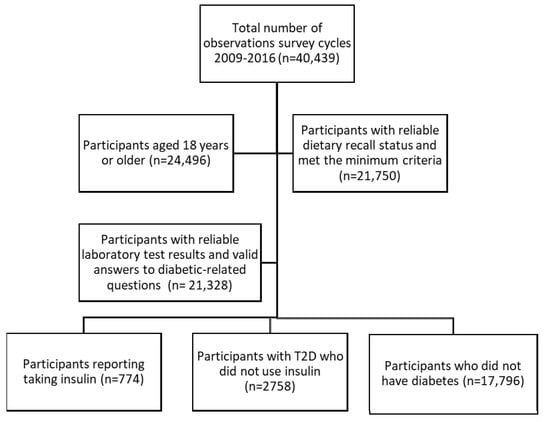
Figure 1.
Flowchart representing sample-size attrition and reasons for inclusion.
2.3. Sociodemographic and Sample Characteristics
Data used to describe the characteristics of those from which dietary information was included in the analysis were survey year (2009–2010, 2011–2012, 2013–2014, and 2015–2016) and self-reported sex (male or female), race/ethnicity (grouped as Hispanic, non-Hispanic white, non-Hispanic black, and other, including multirace), age (grouped as 18–34, 35–49, and 50–80 years), and PIR, which was the reported household income divided by the federal poverty guideline for household income, and grouped as 0–0.99 (below poverty threshold), 1–1.99, 2–2.99, 3–3.99, and >4 based on the U.S. Census Bureau’s definition of being in poverty and maintaining an equitable PIR range for low-income categories [16]. BMI was classified as underweight and normal weight (<25 kg/m2) because only a few participants were underweight, overweight (25.0–29.9 kg/m2), and obese (≥30.0 kg/m2) [17].
2.4. Dietary Assessment
The U.S. Department of Agriculture (USDA) Automated Multiple-Pass Method [18] was used to collect dietary recall recorded during the physical health examination, where participants reported all of the foods consumed during the previous 24-hour period, including information on the time of intake, amount and type of each food, and detailed food descriptions [19]. Each reported food item was then linked to the USDA’s Food and Nutrient Database for Dietary Studies (FNDDS) [20,21,22,23] to assign 8-digit food codes. The USDA food codes were also used to sort the reported foods into the What We Eat in America (WWEIA) food categories and subcategories [24].
2.5. Statistical Analysis
The Rao–Scott modified chi-square test was used to compare sociodemographic variables created from the survey data among the three groups.
All analysis was based on the foods and beverages reported as consumed within the three groups and not the individual participant. The weighted frequencies of reported foods were computed by determining the weighted sum of the number of food items, food subcategories, and food categories using the population ratio approach:
where n = the sample size, i = each participant, Ri = number of reports of individual food code for the ith participant, and Wi = dietary day 1 sample weight for the ith participant [25,26]. The number of reports of foods for each participant was multiplied by the dietary day 1 sample weight, and then summed to yield the total weighted frequency of the particular food or beverage for each respective group, which represented how often that food or beverage was consumed by the respective group in the U.S. in 1 day. The weighted frequency of the food or beverage was also divided by the total weighted frequency of all foods or beverages reported in a single day to get the weighted percentage of the frequency of that food or beverage being consumed out of all reported foods and beverages consumed.
The weighted energy contribution of reported food items, food subcategories, and food categories was computed by determining the weighted sum using the population ratio approach:
where n = the sample size, i = each participant, Ei = total energy for an individual food code for the ith participant, and Wi = dietary day 1 sample weight for the ith participant [25,26]. The energy contributed by a particular food or beverage was first summed for each participant and then multiplied by the dietary day 1 sample weight of the participant, then summed for all participants in the sample for each group, which represented how much energy that food or beverage contributed to the total energy for the respective group in the U.S. in 1 day. The weighted energy of the particular food or beverage was also divided by the total weighted energy from all reported foods and beverages to get the weighted percentage of energy from that food or beverage out of the energy estimated from all reported foods and beverages.
Kruskal–Wallis tests were used to compare the differences among the top 10 ranking lists with the various food hierarchy levels in the three groups, while Rao–Scott modified chi-square goodness-of-fit tests were used to compare the frequency and energy contributions of the individual food categories at the broad food category level among the three groups. Significant differences were indicated when p < 0.05/42 or p < 0.0012 using a Bonferroni-type adjustment for multiple comparisons for food intake among the 14 broad food categories × 3 groups. Survey weights, or the reciprocal of sample inclusion probability, were used in all computations to allow for inference to the non-institutionalized U.S. population. Further adjustments were performed to account for the clustering and stratification inherent to the survey design.
All analyses were completed in SAS 9.4 (SAS Institute Inc., Cary, NC, USA).
3. Results
3.1. Sociodemographic and Sample Characteristics
The sociodemographic and sample characteristics of participants taking insulin, with T2D but not taking insulin, and participants without diabetes are shown in Table 1. Sex, age, race/ethnicity, PIR, and BMI were significantly different among the three groups.

Table 1.
Characteristics of participants and data of U.S. adults 18 year or older taking insulin, with type 2 diabetes but not taking insulin, and without diabetes as drawn from the NHANES, 2009–2016 1.
Most participants reporting taking insulin, and those with T2D but not using insulin were aged 50–80 years. Participants without diabetes were more evenly distributed in the three age-groups (18–34, 35–49, 50–80). About half of the group using insulin and with T2D but not taking insulin had PIR < 2. Furthermore, 28.1% of the group reporting taking insulin had PIR below the poverty threshold (PIR < 1). The group without diabetes had higher incomes, with more than 25% of participants having a PIR greater than 4. In addition, BMI ≥ 30 was heavily represented among participants in the group reporting taking insulin (64.7%) and in the group reporting T2D but not taking insulin (58.1%). The three categories of BMI were evenly distributed in the group without diabetes (33.9%, 33.0%, and 33.1%, respectively).
3.2. The Most Frequently Consumed Food Items, Food Subcategories, and Food Categories
The top 10 most frequently reported food items, food subcategories, and food categories for the group reporting taking insulin, those with T2D but not using insulin, and participants without diabetes are shown in Table 2, Table 3 and Table 4.

Table 2.
Top 10 most frequently consumed foods items or beverages 1, unweighted and weighted frequency of reported foods items or beverages, percentage of reported foods or beverages, and standard error of percentage of reported foods or beverages among all reported foods or beverages for U.S. adults 18 year or older taking insulin, with type 2 diabetes but not taking insulin, and without diabetes drawn from 2009–2016 NHANES data 2.

Table 3.
Top 10 most frequently consumed What We Eat in America foods or beverage subcategories 1, unweighted and weighted frequency of reported foods or beverage subcategories, percentage of reported foods or beverage subcategory out of the total, and standard error of the percentage of reported foods or beverage represented by the subcategory among all reported foods or beverage subcategories for U.S. adults 18 years or older taking insulin, with type 2 diabetes but not taking insulin, and without diabetes drawn from 2009–2016 NHANES dat 2.

Table 4.
Top 10 most frequently consumed What We Eat In America food or beverage categories 1, unweighted and weighted frequency of reported food or beverage categories, percentage of the reported foods or beverage category out of total, and standard error of the percentage of reported foods or beverage represented by the category among all reported foods or beverage categories for U.S. adults 18 years or older taking insulin, with type 2 diabetes but not taking insulin, and without diabetes drawn from 2009–2016 NHANES data 2.
The ranked lists were not statistically different (p-value = 0.69, 0.73, 0.96, respectively), however they allow insight to the dietary context and patterns of these 3 groups. Foods are presented in descending weighted frequency order by their FNDDS short food descriptions. In these frequency lists, 7 food items (Table 2), 6 food subcategories (Table 3), and 8 food categories (Table 4) are common across the three groups, but their rankings were varied (but not in a statistically significant manner). Notably, diet soft drink was the 4th most frequently consumed food subcategory among the group reporting taking insulin, the 7th among those with T2D but not taking insulin, and did not appear in the top 10 food subcategory frequency list among those without diabetes (Table 3). Regular soft drink did not appear in the top 10 food subcategory frequency list for the group reporting taking insulin, but was the 8th most frequently consumed food subcategory among those with T2D but not taking insulin, and the 6th most frequently consumed food subcategory among participants without diabetes (Table 3). In addition, sugar substitutes and cold cuts and cured meats ranked 8th and 10th, respectively, in the top 10 list of the group reporting taking insulin but not the other groups (Table 3), while other vegetables and combinations ranked in top 10 list of the group reporting T2D but not taking insulin (9th) and in the group without diabetes (8th) but not for those taking insulin (Table 3).
3.3. The Highest Energy Contributing Food Items, Food Subcategories, and Food Categories
The top 10 highest energy contributing food items, food subcategories, and food categories for the participants reporting taking insulin, those with T2D but not using insulin, and participants without diabetes are shown in Table 5, Table 6 and Table 7.

Table 5.
Top 10 highest energy contributing food items or beverages 1, the unweighted frequency and weighted energy contribution of reported food items or beverages, percentage of the total represented by the reported food or beverage items 1, and standard error of the percentage of the total represented by the reported food or beverage items among all reported food or beverage items for U.S. adults 18 year or older taking insulin, with type 2 diabetes but not taking insulin, and without diabetes drawn from 2009–2016 NHANES data 2.

Table 6.
Top 10 highest energy contributing What We Eat in America food and beverage subcategories 1, the unweighted frequency and weighted energy contribution of reported foods items or beverages, percentage of the total represented by the reported food or beverage subcategory, and standard error of the percentage of the total represented by the reported food or beverage subcategories among all reported food or beverage subcategories for U.S. adults 18 year or older taking insulin, with type 2 diabetes but not taking insulin, and without diabetes drawn from 2009–2016 NHANES data 2.

Table 7.
Top 10 highest energy contributing What We Eat in America food and beverage categories 1, the unweighted frequency and weighted energy contribution of reported food items or beverages, percentage of the total represented by the reported food or beverage category, and standard error of the percentage of the total represented by the reported food or beverage categories among all reported food or beverage categories for U.S. adults 18 year or older taking insulin, with type 2 diabetes but not taking insulin, and without diabetes drawn from 2009–2016 NHANES data 2.
Similar to the frequency lists, the list of top energy contributing foods and beverages were not statistically different (p-value = 0.11, 0.34, 0.61, respectively), but provide context to the diets consumed by the 3 groups. Foods are presented in descending weighted order according to their energy contribution by their FNDDS short food descriptions. In these energy contribution lists, 5 food items (Table 5), 6 food subcategories (Table 6), and 5 food categories (Table 7) were similar among the three groups, but their rankings varied (but not statistically significant manner). Regular soft drinks did not rank in the top 10 most energy contributing food subcategories list among the group reporting taking insulin, but was ranked 5th among those with T2D but not taking insulin, and 2nd among participants without diabetes (Table 6). Furthermore, the group reporting taking insulin consumed less energy from food subcategories with added sugars compared with the other two groups (cakes and pies were 6th and cookies and brownies 7th among the group reporting taking insulin; cakes and pies were 3rd and cookies and brownies 6th among those with T2D but not taking insulin; cookies and brownies were 8th and cakes and pies 9th among participants without diabetes). More protein food subcategories ranked high within the top 10 list (whole pieces of chicken ranked 3rd place, eggs and omelets ranked 4th place, meat mixed dishes ranked 5th place, cold cuts and cured meats ranked 10th) among the group reporting taking insulin compared to the other two groups (whole pieces of chicken ranked 4th place, eggs and omelets 9th place, meat mixed dishes 10th place in those with T2D but not using insulin, and whole pieces of chicken ranked 5th place in participants without diabetes) (Table 6). In addition, whole wheat bread and white potato ranked 6th and 8th (Table 5) in the top 10 lists of the group reporting taking insulin, but was not ranked in the lists of the other groups, while French fries ranked 5th in the top 10 lists of the group reporting T2D but not taking insulin and 3rd in the group without diabetes, but was not ranked in the lists of the group taking insulin (Table 5). Moreover, lite beer and beer ranked in the top 10 lists of the group without diabetes (5th in Table 5 and 4th in Table 6) but was not ranked in the lists of the other groups. Fruit-flavored soft drink ranked 10th only in the top 10 lists of the group without diabetes (Table 5).
3.4. Broad Food Category Intake by Frequency and Energy Contribution
The results of the comparisons of the frequencies and energy contributions of the individual broad WWEIA food or beverage categories among the three groups are shown in Table 8.

Table 8.
Broad What We Eat In America food and beverage category 1 intake comparisons by frequency and energy among U.S. adults 18 year or older taking insulin, with type 2 diabetes but not taking insulin, and without diabetes drawn from NHANES 2009–2016 2.
The percentage of intake from the broad categories of grains and alcohol were statistically significantly different in both intake frequency and energy contribution across the three groups. From the group reporting taking insulin to those with T2D but not using insulin to participants without diabetes, grains exhibited a decreasing trend in consumption frequency and energy contribution, while alcohol showed an increasing trend. The percentage of snacks/sweets were statistically significantly different in consumption frequency, but not energy contribution among the three groups, which showed an increasing trend from the group reporting taking insulin to those with T2D not using insulin to participants without diabetes. The percentage of intake from protein foods, vegetables, beverages, water, and other were statistically significantly different in energy contribution across the three groups. From the group reporting taking insulin to participants without diabetes, protein foods and vegetables exhibited a decreasing trend in percentage of energy contribution, while beverages, water, and other showed an increasing trend.
4. Discussion
Few studies have investigated the diets of those reporting taking insulin [9,10,11], nor have these studies included consideration of the dietary intake contributions of foods to both energy and frequency of intake. To our knowledge, this is the first study to investigate and compare the diets of the group reporting taking insulin, those with T2D but not taking insulin, and participants without diabetes. Participants with varying diabetes and insulin-use status showed significant differences in both the frequency of which certain broad food or beverage categories are consumed and the energy contributions attributed to certain food or beverage food categories, implying that insulin-use status may be linked to dietary behaviors and the importance of certain foods or beverages in the overall diet. In some of the broad WWEIA food categories, the statistically significant differences observed in the frequency were also observed in energy contribution. Both the percentage of consumption frequency and energy contribution of grains (wheat bread) and alcoholic beverages (beer) were statistically significantly different among the three groups.
The results also included statistically significant findings where either the frequency or energy contribution percentage differed among the groups but not both. Beverages, water, and the “other” (nutrition powder) broad food categories did not exhibit significantly different percentage of frequency of intake across the three groups, but the share of energy contributed by these broad food categories was lower among the participants reporting taking insulin compared to those without diabetes. The share of energy contributed by protein (eggs and omelets, cold cuts and cured meats) and vegetables (tomatoes and lettuce) was also greater among the group reporting taking insulin compared with participants without diabetes. Snacks/sweets (cookies and brownies, and cakes and pies) exhibited a lower percentage of consumption frequency among the group reporting taking insulin compared with participants without diabetes, but the percentage of energy intake attributed to snacks/sweets was not significantly different across all three groups.
Results of this study suggest the group reporting taking insulin exhibited a pattern of higher quality regarding dietary intake for the foods they consumed frequently and that contributed most to energy compared to those with T2D not using insulin and participants without diabetes. However, actual diet quality analyses among the three groups at the person rather than food unit of analysis level needs further evaluation. Since older adults accounted for the majority of the group reporting taking insulin, this finding is consistent with previous studies showing that older adults have higher-quality diets [11,25,27,28]. Yet, almost two thirds of the group that reported taking insulin and more than half of the group with T2D but not taking insulin were obese, which has previously been inversely related to diet quality [29,30] as has poverty-income ratio [31]. The proportion of various race/ethnicities among the groups and gender distribution were also differentially distributed and may have influenced the dietary quality, selection, and patterns of foods among the three groups in the study. Other factors may have also influenced the patterns observed, such as the length of time since diagnosis or since insulin use [32,33,34]. Yet, this study focused on the foods themselves, and not the person as the unit of analysis. Therefore, the personal characteristics of the individuals in each of the three groups compared were not controlled for in the analysis.
In addition, the finding that the group reporting taking insulin may have a higher diet quality is also supported by a previous study [34], suggesting that those with diabetes who are using insulin engage in dietary behaviors promoting a more healthful mix of dietary intake compared with those who do not have diabetes and those with T2D but not taking insulin. The group using insulin reported a higher percentage of consumption frequency of grains, energy contribution from grains, vegetables, and protein foods; and lower percentage consumption frequency of alcohol and sweets/snacks and energy contributed by beverages and alcohol compared to participants without diabetes. One explanation is that grains, protein foods, and vegetables have been promoted as foods to consume to help manage blood glucose control for those taking insulin. Carbohydrate intake is highly related to postprandial glycemia, whole grains are a source of carbohydrates that have a favorable influence on postprandial blood glucose levels [35]. Protein foods may also aid dietary compliance and weight loss maintenance, which is beneficial for diabetes [36,37]. Vegetable consumption has been associated with the improvement of diabetes due to benefits offered by the bioactive compounds comprising them including dietary fiber, resistant starch, antioxidant vitamins, phytochemicals (polyphenols, tannins, and others) and minerals [38,39,40], which may explain why the group reporting taking insulin selected a higher percentage of their calories from vegetables compared with those who do not have diabetes. Furthermore, alcohol, sweets/snacks, and beverages (heavily influenced by sweetened beverages) are foods that those taking insulin may try to avoid due to their negative impact on glycemic control. These foods that may add solid fats or added sugar intake and should be reduced according to the Dietary Guidelines for Americans, 2020–2025 [41,42].
With regard to differences among the percentage of beverage and alcohol intake of the groups, previous studies found that those with diabetes drink less alcohol than those without diabetes [43,44], which supports the findings here that those who used insulin and those with T2D not using insulin, consumed lower percentages of alcohol than participants without diabetes. Even though the long-term effect of alcohol consumption on glycemic management remains to be investigated [45], heavy alcohol consumption is associated with an increased incidence of diabetes [45] and alcohol consumption may be a negative indicator of diabetes self-care behavior [46]. The beverage intake of the group using insulin further varied from the other two groups in the pattern of energy contribution from soft drinks (Table 5), which was supported by the statically significant lower percentage of energy contribution of beverages at the broad food category level in the group reporting taking insulin compared to the group without diabetes (Table 8). Yet, the percentage of the frequency of consuming beverages at the broad food category level was not significantly different among these two groups (Table 8) and those reporting taking insulin consumed diet soft drinks more frequently (Table 3), which may be viewed as an alternative choice that avoids added sugars. Interestingly, this significant difference in energy from beverages was not observed in the categories of “cookies and brownies” or “cakes and pies” (Table 8), which are categories that also have high amounts of added sugars but may not have similar alternatives. Furthermore, within the same food category, the group taking insulin may prefer to choose white potato rather than the fried version of French fries that the group with T2D not using insulin and the group without diabetes choose (Table 5).The findings related to lower frequency of sweets/snacks and beverages among those using insulin compared to those without diabetes is supported by a previous study where participants with diabetes consumed lower amounts of sweets and beverage (juice) compared to those without diabetes [44]. Sweets/snacks and beverages, especially sweetened beverages that heavily add to energy intake, are typically high in added sugars and may to lead nonalcoholic fatty liver disease [47]. Excessive added sugar intake is not only a significant contributor to weight gain that may lead to increased risk of diabetes but also increased dietary glycemic load and fructose metabolism that may lead to inflammation and insulin resistance [48]. Fructose consumption, for instance, has been associated to diabetes onset and progression as well as nonalcoholic fatty liver disease development and progression, stressing the role of metabolic syndrome with increase deposition of epicardial fat and worsening clinical outcomes [49,50]. In addition, it should be noted that the literature reviewed here includes studies focused on those with diabetes, not specifically those using insulin, due to the extremely limited evidence of dietary intake among those using insulin [39,40,44]. Therefore, the findings here should be further explored among those taking insulin.
Limitations of this analysis may be due to the aggregation of foods to subcategories and categories that may obscure specific food items or types of food that could be related to many of the characteristic differences among groups and that is agnostic of the individual when statistical comparisons were made. As mentioned, the focus of the analysis was on the foods, not the individual person, meaning sociodemographic characteristics were not adjusted for in the analysis. The addition or removal of specific foods or beverages from a food category has the potential to change statistically significant comparisons, so the results and interpretation should be viewed as one perspective on the dietary intake among these three groups, keeping in mind that analysis of alternative food categorization, splitting to subcategories, or itemization may yield differential results. However, the application of the WWEIA food categories lends standardization and consistency to other reporting by USDA and other researchers [51,52,53]. In addition, the ranking lists (Table 2, Table 3, Table 4, Table 5, Table 6 and Table 7) were generated from the foods and beverages reported over all times of the day, so separating out the most frequently consumed foods and foods that highly contributed to energy intake for different times or meals of the day may be helpful to inform interventions or dosing algorithms as the timing of dietary intake and combinations of foods consumed at the same time influences glucose metabolism [54,55,56,57,58]. It is important to note that the comparison of ranking lists among the 3 groups did not consider the amount or magnitude of the consumption frequency or energy contribution of different food hierarchy levels, it only considered sequence of ranking order. Furthermore, the comparisons of these ranked lists were limited to the top 10 foods which were not different between groups. The inclusion of more foods in the ranked lists may have yielded different results. Yet, the lists contribute a descriptive context of the diets of these three groups that is not available elsewhere in the literature and may be helpful to inform menus, aid the development of nutrition assessment tools, and create nutrition interventions. Furthermore, the NHANES dietary data this study used are only a 1-day dietary recall of the participants, which may not be accurate due to participants’ memory and may not represent the usual dietary intake [59]. Moreover, misreported dietary intake may have been presented in this study sample resulting in errors in energy, frequency, food item, subcategory, and category representation and comparisons [60]. Those with diabetes and those reporting taking insulin may exhibit different patterns of misreporting compared with other population groups [44]. Previous studies have shown that dietary intake misreporting and especially underreporting is more prevalent in overweight and obese individuals compared to normal weight individuals [61,62,63], and prevalence of underreporting in diabetic patients may be even higher [64], considering that obesity is a risk factor of diabetes that 81% of diabetic patients are obese [65]. Another previous study pointed out that energy misreporters are prone to misreport foods that highly contributed to glycemic index and glycemic load such as underreporting foods including sugars, cookies, and milk products and overreporting foods including fruit and vegetables [63]. In the future, studies evaluating the differences in misreporting by diabetic status should be evaluated. Furthermore, the dietary behaviors of families may be related and the habits of children may predict future risk of metabolic syndrome. Therefore, the relationship of the dietary intake of parents using insulin and their children should be evaluated.
There are several implications and applications for the results of this study. Diabetes is a chronic disease that is highly related to diet [66]. The lists of foods generated in this study may be used to fill the gap in knowledge of the diets for the group reporting taking insulin or diabetic patients among U.S. adults [9,11], specifically, menus and dietary interventions developed to improve diabetes management may be informed by the lists. Although frequently consumed foods and those contributing most to energy may not satisfy the preferences of every person, they are generally accepted as indicated by their selection in the population. Those using insulin may be more likely to adhere to a diet they accept, thus forming healthier eating habits. Second, the findings of this study may inform future studies to gain a greater knowledge of the diets of those using insulin. For example, the list of frequently consumed foods and those most contributing to energy may inform the prioritization of foods and beverages to include in food frequency questionnaires. Third, the findings of this study may aid the development of nutrition assessment tools as researchers should concentrate efforts on developing the most accurate identification methods for the foods and beverages that are consumed the most frequently and contribute the most to total energy intake in the group they are tailored for [25].
5. Conclusions
Differences in dietary intake exist among U.S. adults by insulin use and diabetes status using NHANES 2009–2016. The group reporting taking insulin consumed grains more frequently, while consuming snack/sweet and alcohol less frequently compared to participants without diabetes. Protein, grains, and vegetables contributed more to the group reporting taking insulin’s daily total energy intake compared to participants without diabetes, whereas beverage and alcohol contributed less. Frequently consumed foods and those contributing to energy may inform diabetes control and management; be used to tailor food recipes; and applied in consumer education, questionnaire design, and dietary assessment.
Author Contributions
Conceptualization, L.L., H.A.E.-M., F.Z. and E.J.D.; methodology, L.L., H.A.E.-M.; formal analysis, L.L.; investigation, L.L.; writing—original draft preparation, L.L.; writing—review and editing, L.L., H.A.E.-M., F.Z. and E.J.D.; supervision, H.A.E.-M.; funding acquisition, H.A.E.-M. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by Eli Lilly and Company.
Institutional Review Board Statement
Approval for data collection was obtained from the NCHS Research Institutional/Ethics Review Board (IRB/ERB) (Continuation of Protocol #2005-06, Protocol #2011-17, Continuation of Protocol #2011-17).
Informed Consent Statement
All NHANES participants provided written informed consent.
Data Availability Statement
Data described in the manuscript are publicly and freely available without restriction at https://www.cdc.gov/nchs/nhanes/index.htm (accessed on 14 July 2021). Analytic code is available upon request.
Conflicts of Interest
The authors declare no conflict of interest. The funders had no role in the design of the study, the collection, analyses, or interpretation of data, in the writing of the manuscript, or in the decision to publish the results.
References
- Centers for Disease Control and Prevention. What is Diabetes? 11 June 2020. Available online: https://www.cdc.gov/diabetes/basics/diabetes.html (accessed on 14 July 2021).
- Centers for Disease Control and Prevention. National Diabetes Statistics Report. 2020. Available online: https://www.cdc.gov/diabetes/pdfs/data/statistics/national-diabetes-statistics-report.pdf (accessed on 14 July 2021).
- Centers for Disease Control and Prevention. The Insulin Resistance–Diabetes Connection. 23 July 2020. Available online: https://www.cdc.gov/diabetes/basics/insulin-resistance.html (accessed on 14 July 2021).
- Centers for Disease Control and Prevention. Types of Insulin. 2 April 2021. Available online: https://www.cdc.gov/diabetes/basics/type-1-types-of-insulin.html (accessed on 14 July 2021).
- Joslin, E.P.; Kahn, C.R. Joslin’s Diabetes Mellitus; Kahn, C.R., Weir, G.C., King, G.L., Moses, A.C., Smith, R.J., Jacobson, A.M., Eds.; Lippincott Williams & Wilkins: Philadelphia, PA, USA, 2005. [Google Scholar]
- Gillespie, S.J.; Kulkarni, K.D.; Daly, A.E. Using Carbohydrate Counting in Diabetes Clinical Practice. J. Am. Diet. Assoc. 1998, 98, 897–905. [Google Scholar] [CrossRef]
- Acierno, C.; Caturano, A.; Pafundi, P.C.; Nevola, R.; Adinolfi, L.E.; Sasso, F.C. Nonalcoholic fatty liver disease and type 2 diabetes: Pathophysiological mechanisms shared between the two faces of the same coin. Explor Med. 2020, 1, 287–306. [Google Scholar] [CrossRef]
- Patton, S.R. Adherence to Diet in Youth with Type 1 Diabetes. J. Am. Diet. Assoc. 2011, 111, 550–555. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- McClure, S.T.; Schlechter, H.; Oh, S.; White, K.; Wu, B.; Pilla, S.J.; Maruthur, N.M.; Yeh, H.C.; Miller, E.R.; Appel, L.J. Dietary intake of adults with and without diabetes: Results from NHANES 2013–2016. BMJ Open Diabetes Res. Care 2020, 8, e001681. [Google Scholar] [CrossRef] [PubMed]
- Muñoz-Pareja, M.; León-Muñoz, L.M.; Guallar-Castillón, P.; Graciani, A.; López-García, E.; Banegas, J.R.; Rodríguez-Artalejo, F. The Diet of Diabetic Patients in Spain in 2008–2010: Accordance with the Main Dietary Recommendations—A Cross-Sectional Study. PLoS ONE 2012, 7, e39454. [Google Scholar] [CrossRef] [Green Version]
- Maffeis, C.; Tomasselli, F.; Tommasi, M.; Bresadola, I.; Trandev, T.; Fornari, E.; Marigliano, M.; Morandi, A.; Olivieri, F.; Piona, C. Nutrition habits of children and adolescents with type 1 diabetes changed in a 10 years span. Pediatr. Diabetes 2020, 21, 960–968. [Google Scholar] [CrossRef]
- NHANES—National Health and Nutrition Examination Survey Homepage. 24 June 2021. Available online: https://www.cdc.gov/nchs/nhanes/index.htm (accessed on 14 July 2021).
- NHANES—NCHS Research Ethics Review Board Approval. 8 May 2019. Available online: https://www.cdc.gov/nchs/nhanes/irba98.htm (accessed on 14 July 2021).
- American Diabetes Association. Diagnosis and Classification of Diabetes Mellitus. Diabetes Care 2014, 37 (Suppl. S1), S81–S90. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nelson, K.M.; Reiber, G.; Boyko, E.J. Diet and Exercise Among Adults with Type 2 Diabetes: Findings from the Third National Health and Nutrition Examination Survey (NHANES III). Diabetes Care 2002, 25, 1722–1728. [Google Scholar] [CrossRef] [Green Version]
- U.C. Bureau. How the Census Bureau Measures Poverty. The United States Census Bureau. Available online: https://www.census.gov/topics/income-poverty/poverty/guidance/poverty-measures.html (accessed on 15 July 2021).
- Body Mass Index—BMI. Available online: https://www.euro.who.int/en/health-topics/disease-prevention/nutrition/a-healthy-lifestyle/body-mass-index-bmi (accessed on 11 June 2021).
- AMPM—USDA Automated Multiple-Pass Method: USDA ARS. Available online: https://www.ars.usda.gov/northeast-area/beltsville-md-bhnrc/beltsville-human-nutrition-research-center/food-surveys-research-group/docs/ampm-usda-automated-multiple-pass-method/#what (accessed on 16 July 2020).
- NHANES Dietary Data. Available online: https://wwwn.cdc.gov/nchs/nhanes/Search/DataPage.aspx?Component=Dietary (accessed on 14 July 2021).
- U.S. Department of Agriculture. Agricultural Research Service. 2012. USDA Food and Nutrient Database for Dietary Studies, 5.0. Food Surveys Research Group Home Page. Available online: http://www.ars.usda.gov/ba/bhnrc/fsrg (accessed on 14 July 2021).
- U.S. Department of Agriculture. Agricultural Research Service. 2014. USDA Food and Nutrient Database for Dietary Studies 2011–2012. Food Surveys Research Group Home Page. Available online: http://www.ars.usda.gov/ba/bhnrc/fsrg (accessed on 14 July 2021).
- U.S. Department of Agriculture. Agricultural Research Service. 2016. USDA Food and Nutrient Database for Dietary Studies 2013–2014. Food Surveys Research Group Home Page. Available online: http://www.ars.usda.gov/nea/bhnrc/fsrg (accessed on 14 July 2021).
- U.S. Department of Agriculture. Agricultural Research Service. 2018. USDA Food and Nutrient Database for Dietary Studies 2015–2016. Food Surveys Research Group Home Page. Available online: http://www.ars.usda.gov/nea/bhnrc/fsrg”.https://www.ars.usda.gov/northeast-area/beltsville-md-bhnrc/beltsville-human-nutrition-research-center/food-surveys-research-group/docs/fndds-download-databases/ (accessed on 13 September 2021).
- U.S. Department of Agriculture. Agricultural Research Service. What We Eat in America Food Categories 2015–2016. Available online: https://www.ars.usda.gov/ARSUserFiles/80400530/pdf/1516/Food_categories_2015-2016.pdf (accessed on 14 July 2021).
- Eicher-Miller, H.A.; Boushey, C.J. How Often and How Much? Differences in Dietary Intake by Frequency and Energy Contribution Vary among U.S. Adults in NHANES 2007–2012. Nutrients 2017, 9, 86. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Eicher-Miller, H.A.; Boushey, C.J.; Bailey, R.L.; Yang, Y.J. Frequently Consumed Foods and Energy Contributions among Food Secure and Insecure U.S. Children and Adolescents. Nutrients 2020, 12, 304. [Google Scholar] [CrossRef] [Green Version]
- Hiza, H.A.B.; Casavale, K.O.; Guenther, P.M.; Davis, C.A. Diet Quality of Americans Differs by Age, Sex, Race/Ethnicity, Income, and Education Level. J. Acad. Nutr. Diet. 2013, 113, 297–306. [Google Scholar] [CrossRef]
- Forshee, R.A.; Storey, M.L. Demographics, not beverage consumption, is associated with diet quality. Int. J. Food Sci. Nutr. 2006, 57, 494–511. [Google Scholar] [CrossRef]
- Sundararajan, K.K.M.; Campbell, C.Y.-H.; Sarma, S. The Relationship Between Diet Quality and Adult Obesity: Evidence from Canada. J. Am. Coll. Nutr. 2014, 33, 1–17. [Google Scholar] [CrossRef] [PubMed]
- Livingstone, K.M.; McNaughton, S.A. Diet quality is associated with obesity and hypertension in Australian adults: A cross sectional study. BMC Public Health 2016, 16, 1037. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- NHANES-FSP.pdf. Available online: https://fns-prod.azureedge.us/sites/default/files/NHANES-FSP.pdf (accessed on 10 April 2022).
- Wang, Z.; Adair, L.S.; Cai, J.; Gordon-Larsen, P.; Siega-Riz, A.M.; Zhang, B.; Popkin, B.M. Diet Quality Is Linked to Insulin Resistance among Adults in China. J. Nutr. 2017, 147, 2102–2108. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sebire, S.J.; Toumpakari, Z.; Turner, K.M.; Cooper, A.R.; Page, A.S.; Malpass, A.; Andrews, R.C. “I’ve made this my lifestyle now”: A prospective qualitative study of motivation for lifestyle change among people with newly diagnosed type two diabetes mellitus. BMC Public Health 2018, 18, 204. [Google Scholar] [CrossRef] [Green Version]
- Niewind, A.C.; Friele, R.D.; Kandou, C.T.; Hautvast, J.G.a.J.; Edema, J.M.P. Changes in food choices of recently diagnosed insulin-dependent diabetic patients. Eur. J. Clin. Nutr. 1990, 44, 505–513. [Google Scholar]
- Fung, T.T.; Hu, F.B.; Pereira, M.A.; Liu, S.; Stampfer, M.J.; Colditz, G.A.; Willett, W.C. Whole-grain intake and the risk of type 2 diabetes: A prospective study in men. Am. J. Clin. Nutr. 2002, 76, 535–540. [Google Scholar] [CrossRef] [Green Version]
- Clifton, P. High-protein and low-glycaemic diets improve dietary compliance and maintenance of weight loss in overweight adults who have lost weight on a low-calorie diet. BMJ Evid.-Based Med. 2011, 16, 112–113. [Google Scholar] [CrossRef] [PubMed]
- MWesterterp-Plantenga, S.; Nieuwenhuizen, A.; Tomé, D.; Soenen, S.; Westerterp, K.R. Dietary Protein, Weight Loss, and Weight Maintenance. Annu. Rev. Nutr. 2009, 29, 21–41. [Google Scholar] [CrossRef] [Green Version]
- Dias, J.S. Nutritional Quality and Health Benefits of Vegetables: A Review. Food Nutr. Sci. 2012, 3, 1354–1374. [Google Scholar] [CrossRef] [Green Version]
- Carlos, J.; Dias, J.; Imai, S. Vegetables Consumption and its Benefits on Diabetes. J. Nutr. Ther. 2017, 6, 1–10. [Google Scholar] [CrossRef]
- Platel, K.; Srinivasan, K. Plant foods in the management of Diabetes mellitus: Vegetables as potential hypoglycaemic agents. Food Nahr. 1997, 41, 68–74. [Google Scholar] [CrossRef]
- Nicklas, T.A.; O’Neil, C.E. Development of the SoFAS (Solid Fats and Added Sugars) Concept: The 2010 Dietary Guidelines for Americans. Adv. Nutr. 2015, 6, 368S–375S. [Google Scholar] [CrossRef] [Green Version]
- U.S. Department of Agriculture; U.S. Department of Health and Human Services. Dietary Guidelines for Americans, 2020–2025; The U.S. Department of Agriculture: Washington, DC, USA; U.S. Department of Health and Human Services: Washington, DC, USA; p. 164.
- Mackenzie, T.; Brooks, B.; O’Connor, G. Beverage Intake, Diabetes, and Glucose Control of Adults in America. Ann. Epidemiol. 2006, 16, 88–691. [Google Scholar] [CrossRef]
- Nöthlings, U.; Boeing, H.; Maskarinec, G.; Sluik, D.; Teucher, B.; Kaaks, R.; Tjønneland, A.; Halkjaer, J.; Dethlefsen, C.; K Overvad, P.A.; et al. Food intake of individuals with and without diabetes across different countries and ethnic groups. Eur. J. Clin. Nutr. 2011, 65, 635–641. [Google Scholar] [CrossRef]
- Howard, A.A.; Arnsten, J.H.; Gourevitch, M.N. Effect of Alcohol Consumption on Diabetes Mellitus. Ann. Intern. Med. 2004, 140, 211–219. [Google Scholar] [CrossRef]
- Ahmed, A.T.; Karter, A.J.; Liu, J. Alcohol consumption is inversely associated with adherence to diabetes self-care behaviours. Diabet. Med. 2006, 23, 795–802. [Google Scholar] [CrossRef] [Green Version]
- Chhimwal, J.; Patial, V.; Padwad, Y. Beverages and Non-alcoholic fatty liver disease (NAFLD): Think before you drink. Clin. Nutr. 2021, 40, 2508–2519. [Google Scholar] [CrossRef]
- Malik, V.S.; Popkin, B.M.; Bray, G.A.; Després, J.-P.; Hu, F.B. Sugar-Sweetened Beverages, Obesity, Type 2 Diabetes Mellitus, and Cardiovascular Disease Risk. Circulation 2010, 121, 1356–1364. [Google Scholar] [CrossRef]
- Caturano, A.; Acierno, C.; Nevola, R.; Pafundi, P.C.; Galiero, R.; Rinaldi, L.; Salvatore, T.; Adinolfi, L.E.; Sasso, F.C. Non-Alcoholic Fatty Liver Disease: From Pathogenesis to Clinical Impact. Processes 2021, 9, 135. [Google Scholar] [CrossRef]
- Salvatore, T.; Galiero, R.; Caturano, A.; Vetrano, E.; Rinaldi, L.; Coviello, F.; di Martino, A.; Albanese, G.; Colantuoni, S.; Medicamento, G.; et al. Dysregulated Epicardial Adipose Tissue as a Risk Factor and Potential Therapeutic Target of Heart Failure with Preserved Ejection Fraction in Diabetes. Biomolecules 2022, 12, 176. [Google Scholar] [CrossRef]
- Hess, J.M.; Cifelli, C.J.; Agarwal, S.; Fulgoni, V.L. Comparing the cost of essential nutrients from different food sources in the American diet using NHANES 2011–2014. Nutr. J. 2019, 18, 68. [Google Scholar] [CrossRef] [Green Version]
- Murphy, M.M.; Scrafford, C.G.; Barraj, L.M.; Bi, X.; Higgins, K.A.; Jaykus, L.A.; Tran, N.L. Potassium chloride-based replacers: Modeling effects on sodium and potassium intakes of the US population with cross-sectional data from NHANES 2015–2016 and 2009–2010. Am. J. Clin. Nutr. 2021, 114, 220–230. [Google Scholar] [CrossRef]
- Slining, M.M.; Popkin, B.M. Trends in intakes and sources of solid fats and added sugars among U.S. children and adolescents: 1994–2010. Pediatr. Obes. 2013, 8, 307–324. [Google Scholar] [CrossRef] [Green Version]
- Lowden, A.; Moreno, C.; Holmbäck, U.; Lennernäs, M.; Tucker, P. Eating and shift work—Effects on habits, metabolism, and performance. Scand. J. Work. Environ. Health 2010, 36, 150–162. [Google Scholar] [CrossRef]
- Aqeel, M.; Forster, A.; Richards, E.A.; Hennessy, E.; McGowan, B.; Bhadra, A.; Guo, J.; Gelfand, S.; Delp, E.; Eicher-Miller, H.A. The Effect of Timing of Exercise and Eating on Postprandial Response in Adults: A Systematic Review. Nutrients 2020, 12, 221. [Google Scholar] [CrossRef] [Green Version]
- Johnston, J.D. Physiological responses to food intake throughout the day. Nutr. Res. Rev. 2014, 27, 107–118. [Google Scholar] [CrossRef] [Green Version]
- Jacobs, D.R., Jr.; Steffen, L.M. Nutrients, foods, and dietary patterns as exposures in research: A framework for food synergy. Am. J. Clin. Nutr. 2003, 78, 508S–513S. [Google Scholar] [CrossRef]
- Winham, D.M.; Hutchins, A.M.; Thompson, S.V. Glycemic Response to Black Beans and Chickpeas as Part of a Rice Meal: A Randomized Cross-Over Trial. Nutrients 2017, 9, 95. [Google Scholar] [CrossRef] [Green Version]
- Klesges, R.C.; Eck, L.H.; Ray, J.W. Who underreports dietary intake in a dietary recall? Evidence from the Second National Health and Nutrition Examination Survey. J. Consult. Clin. Psychol. 1995, 63, 438–444. [Google Scholar] [CrossRef]
- Freedman, L.S.; Commins, J.M.; Moler, J.E.; Arab, L.; Baer, D.J.; Kipnis, V.; Midthune, D.; Moshfegh, A.J.; Neuhouser, M.L.; Prentice, R.L. Pooled Results From 5 Validation Studies of Dietary Self-Report Instruments Using Recovery Biomarkers for Energy and Protein Intake. Am. J. Epidemiol. 2014, 180, 172–188. [Google Scholar] [CrossRef] [Green Version]
- Lissner, L.; Troiano, R.P.; Midthune, D.; Heitmann, B.L.; Kipnis, V.; Subar, A.F.; Potischman, N. OPEN about obesity: Recovery biomarkers, dietary reporting errors and BMI. Int. J. Obes. 2007, 31, 956–961. [Google Scholar] [CrossRef] [Green Version]
- Ocké, M.C.; Larrañaga, N.; Grioni, S.; van den Berg, S.W.; Ferrari, P.; Salvini, S.; Benetou, V.; Linseisen, J.; Wirfält, E.; Rinaldi, S.; et al. Energy intake and sources of energy intake in the European Prospective Investigation into Cancer and Nutrition. Eur. J. Clin. Nutr. 2009, 63, S3–S15. [Google Scholar] [CrossRef] [Green Version]
- Livingstone, M.B.E.; Black, A.E. Markers of the Validity of Reported Energy Intake. J. Nutr. 2003, 133, 895S–920S. [Google Scholar] [CrossRef]
- Underreporting of Food Intake in Obese Diabetic and Nondiabetic Patients. Diabetes Care. Available online: https://care.diabetesjournals.org/content/29/12/2726.short (accessed on 6 September 2021).
- Gregg, E.W.; Cheng, Y.J.; Narayan, K.M.V.; Thompson, T.J.; Williamson, D.F. The relative contributions of different levels of overweight and obesity to the increased prevalence of diabetes in the United States: 1976–2004. Prev. Med. 2007, 45, 348–352. [Google Scholar] [CrossRef]
- Nuttall, F.Q. Diet and the Diabetic Patient. Diabetes Care 1983, 6, 11. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).