Prevalence of Metabolic Syndrome in Relation to Cardiovascular Biomarkers and Dietary Factors among Adolescents with Type 1 Diabetes Mellitus
Abstract
:1. Introduction
2. Materials and Methods
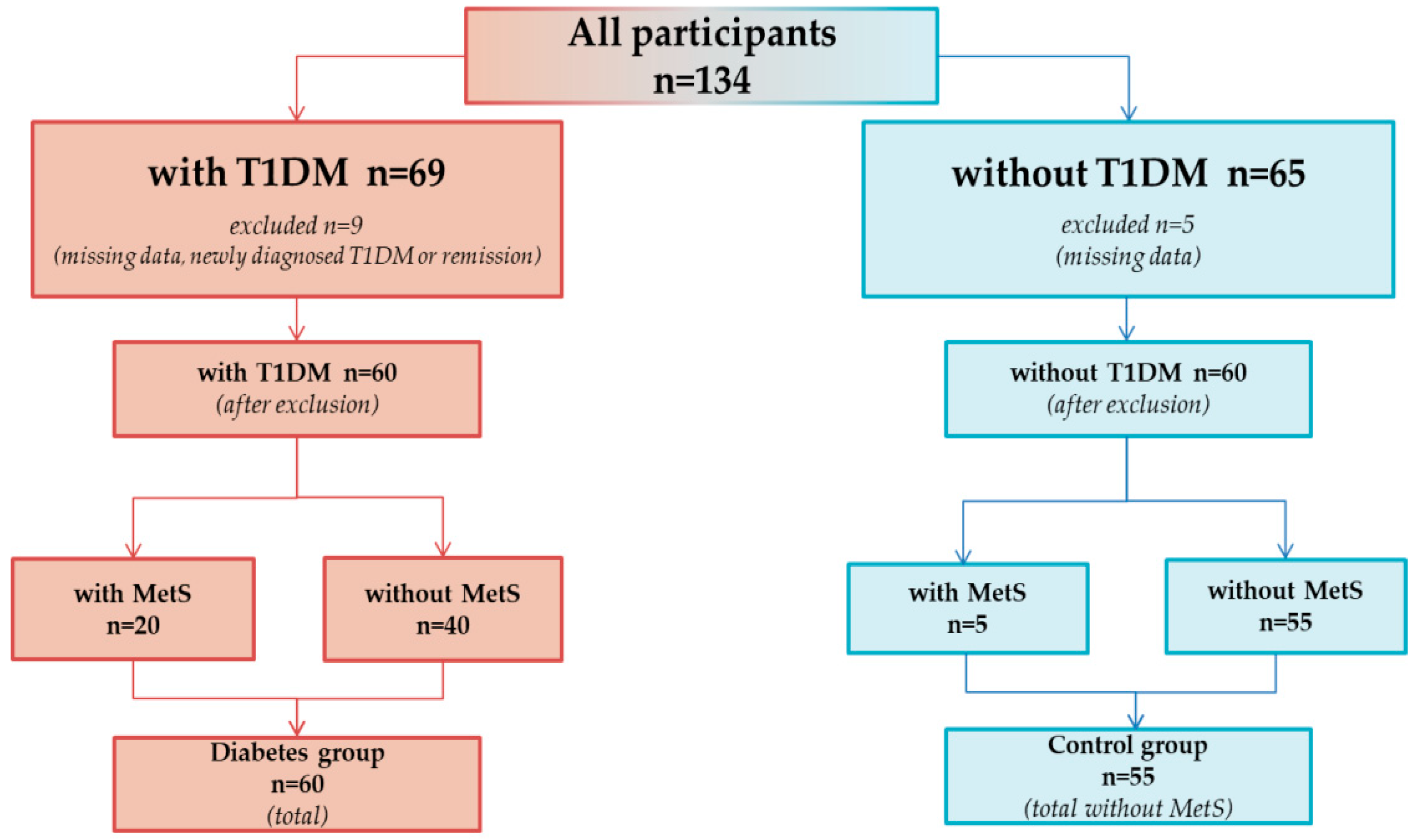
2.1. Study Group
2.2. Blood Samples Analysis of Cardiovascular Biomarkers
2.3. Nutritional Status and Nutrients Intake
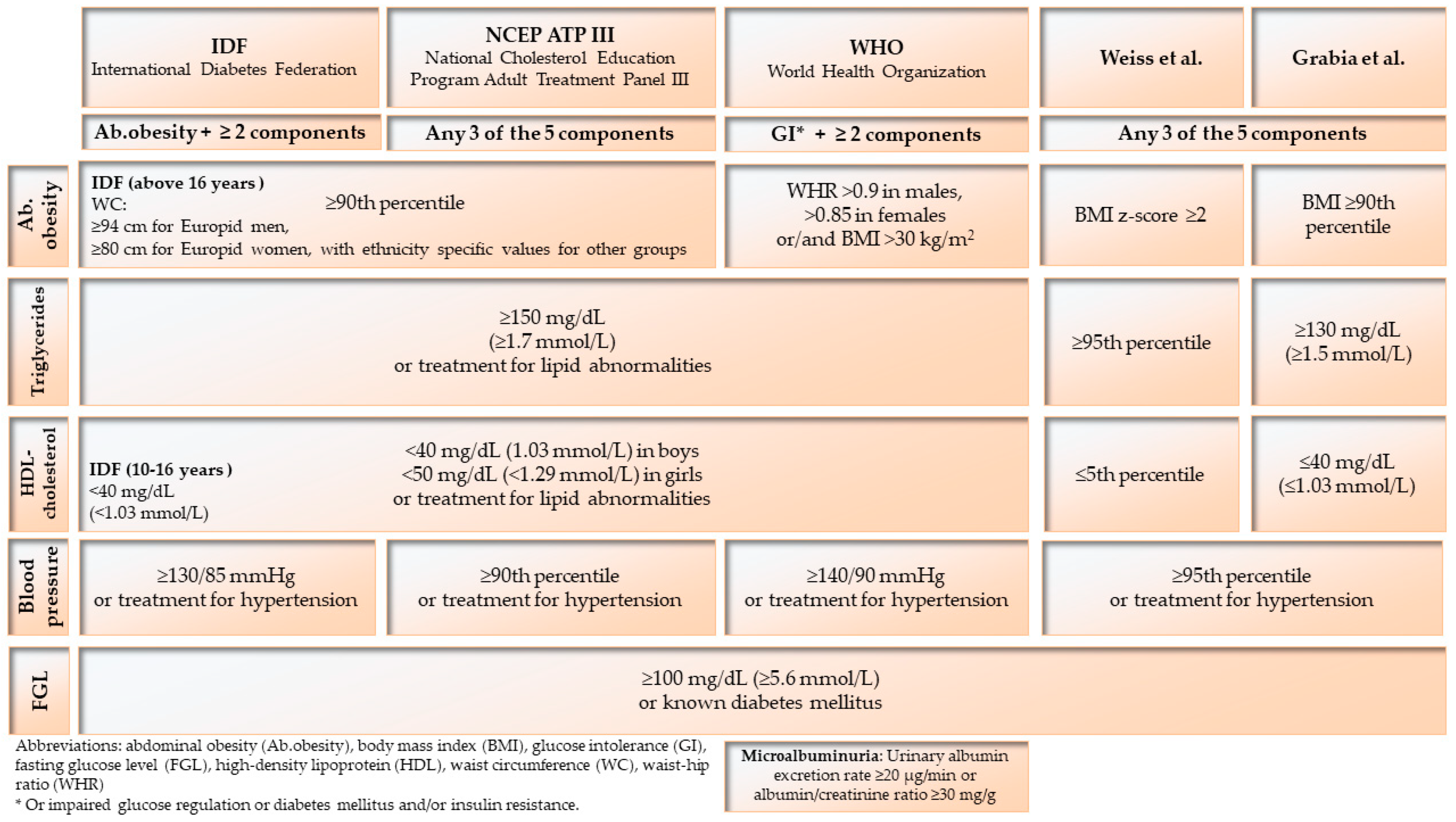
2.4. Metabolic Syndrome Diagnosis
2.5. Statistical Analysis
3. Results
3.1. Study Characteristic
3.2. Prevalence of Metabolic Syndrome
3.3. Nutritional Status
3.4. Nutrients Intake
3.5. Nutritional Habits
3.6. Insulin Therapy and Modern Glucose-Monitoring Systems
3.7. Multiple Correspondence Analysis
- (1)
- The first quadrant contained participants with MetS, characterized by poor metabolic management (HbA1c > 7%), low eGDR (<8 mg/kg/min), low TAS (<1.3 mmol/L), and medium (>50 cm2) to high (>100 cm2) VFA, was not supported by FGM or CGM.
- (2)
- The opposite (III) and side quadrant (II) included healthy peers with moderate (1.3–1.8 mmol/L) to high (>1.8 mmol/L) TAS and normal VFA (<50 cm2).
- (3)
- The last quadrant (IV) included individuals without MetS with optimal metabolic control (HbA1c < 7%) and high eGDR (>8 mg/kg/min), who were using CSII or MDI and FGM or CGM.

4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Sun, H.; Saeedi, P.; Karuranga, S.; Pinkepank, M.; Ogurtsova, K.; Duncan, B.B.; Stein, C.; Basit, A.; Chan, J.C.N.; Mbanya, J.C.; et al. IDF Diabetes Atlas: Global, Regional and Country-Level Diabetes Prevalence Estimates for 2021 and Projections for 2045. Diabetes Res. Clin. Pract. 2022, 183, 109–119. [Google Scholar] [CrossRef] [PubMed]
- Yeh, H.-C.; Brown, T.T.; Maruthur, N.; Ranasinghe, P.; Berger, Z.; Suh, Y.D.; Wilson, L.M.; Haberl, E.B.; Brick, J.; Bass, E.B.; et al. Comparative Effectiveness and Safety of Methods of Insulin Delivery and Glucose Monitoring for Diabetes Mellitus. Ann. Intern. Med. 2012, 157, 336–347. [Google Scholar] [CrossRef] [PubMed]
- Freckmann, G.; Ulbrich, S. Continuous Glucose Monitoring (CGM) in Diabetes Therapy. Med. Monatsschr. Pharm. 2018, 41, 455–460. [Google Scholar] [CrossRef]
- Grabia, M.; Markiewicz-Żukowska, R. Nutritional Status of Pediatric Patients with Type 1 Diabetes Mellitus from Northeast Poland: A Case-Control Study. Diabetes Ther. 2021, 12, 329–343. [Google Scholar] [CrossRef]
- Minges, K.E.; Whittemore, R.; Grey, M. Overweight and Obesity in Youth with Type 1 Diabetes. Annu. Rev. Nurs. Res. 2013, 31, 47–69. [Google Scholar] [CrossRef]
- Purnell, J.Q.; Zinman, B.; Brunzell, J.D. The Effect of Excess Weight Gain with Intensive Diabetes Mellitus Treatment on Cardiovascular Disease Risk Factors and Atherosclerosis in Type 1 Diabetes Mellitus: Results from the Diabetes Control and Complications Trial/Epidemiology of Diabetes Interventions and Complications Study (DCCT/EDIC) Study. Circulation 2013, 127, 180–187. [Google Scholar] [CrossRef]
- Zimmet, P.; Alberti, K.G.M.; Kaufman, F.; Tajima, N.; Silink, M.; Arslanian, S.; Wong, G.; Bennett, P.; Shaw, J.; Caprio, S.; et al. The Metabolic Syndrome in Children and Adolescents–An IDF Consensus Report. Pediatr. Diabetes 2007, 8, 299–306. [Google Scholar] [CrossRef]
- Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults. Executive Summary of the Third Report of the National Cholesterol Education Program (NCEP). JAMA 2001, 285, 2486–2497. [Google Scholar] [CrossRef]
- World Health Organization. Definition, Diagnosis and Classification of Diabetes Mellitus and Its Complications: Report of a WHO Consultation. Part 1, Diagnosis and Classification of Diabetes Mellitus; World Health Organisation: Geneva, Switzerland, 1999. [Google Scholar]
- Grabia, M.; Markiewicz-Żukowska, R.; Socha, K. Prevalence of Metabolic Syndrome in Children and Adolescents with Type 1 Diabetes Mellitus and Possibilities of Prevention and Treatment: A Systematic Review. Nutrients 2021, 13, 1782. [Google Scholar] [CrossRef]
- American Diabetes Association. Classification and Diagnosis of Diabetes: Standards of Medical Care in Diabetes—2021. Diabetes Care 2021, 44 (Suppl. S1), S15–S33. [Google Scholar] [CrossRef]
- Miller, N.J.; Rice-Evans, C.; Davies, M.J.; Gopinathan, V.; Milner, A. A Novel Method for Measuring Antioxidant Capacity and Its Application to Monitoring the Antioxidant Status in Premature Neonates. Clin. Sci. 1993, 84, 407–412. [Google Scholar] [CrossRef] [PubMed]
- Williams, K.V.; Erbey, J.R.; Becker, D.; Arslanian, S.; Orchard, T.J. Can Clinical Factors Estimate Insulin Resistance in Type 1 Diabetes? Diabetes 2000, 49, 626–632. [Google Scholar] [CrossRef] [PubMed]
- Chillarón, J.J.; Goday, A.; Flores-Le-Roux, J.A.; Benaiges, D.; Carrera, M.J.; Puig, J.; Cano-Pérez, J.F.; Pedro-Botet, J. Estimated Glucose Disposal Rate in Assessment of the Metabolic Syndrome and Microvascular Complications in Patients with Type 1 Diabetes. J. Clin. Endocrinol. Metab. 2009, 94, 3530–3534. [Google Scholar] [CrossRef] [PubMed]
- Köken, Ö.Y.; Kara, C.; Yılmaz, G.C.; Aydın, H.M. Utility of Estimated Glucose Disposal Rate for Predicting Metabolic Syndrome in Children and Adolescents with Type-1 Diabetes. J. Clin. Endocrinol. Metab. 2020, 33, 859–864. [Google Scholar] [CrossRef] [PubMed]
- Kowalkowska, J.; Wadolowska, L.; Czarnocinska, J.; Czlapka-Matyasik, M.; Galinski, G.; Jezewska-Zychowicz, M.; Bronkowska, M.; Dlugosz, A.; Loboda, D.; Wyka, J. Reproducibility of A Questionnaire for Dietary Habits, Lifestyle and Nutrition Knowledge Assessment (Kompan) in Polish Adolescents and Adults. Nutrients 2018, 10, 1845. [Google Scholar] [CrossRef]
- Jarosz, M.R.E.; Stoś, K.; Charzewska, J. Nutrition Standards for the Population of Poland and Their Application. Available online: https://www.pzh.gov.pl/normy-zywienia-2020/ (accessed on 20 March 2021).
- Araszkiewicz, A.; Bandurska-Stankiewicz, E.; Borys, S.; Budzyński, A.; Cyganek, K.; Cypryk, K.; Czech, A.; Czupryniak, L.; Drzewoski, J.; Dzida, G.; et al. 2021 Guidelines on the Management of Patients with Diabetes. A Position of Diabetes Poland. Clin. Diabetol. 2021, 10, 1–113. [Google Scholar] [CrossRef]
- Smart, C.E.; Annan, F.; Higgins, L.A.; Jelleryd, E.; Lopez, M.; Acerini, C.L. ISPAD Clinical Practice Consensus Guidelines 2018: Nutritional Management in Children and Adolescents with Diabetes. Pediatr. Diabetes 2018, 19 (Suppl. S27), 136–154. [Google Scholar] [CrossRef]
- Weiss, R.; Dziura, J.; Burgert, T.S.; Tamborlane, W.V.; Taksali, S.E.; Yeckel, C.W.; Allen, K.; Lopes, M.; Savoye, M.; Morrison, J.; et al. Obesity and the Metabolic Syndrome in Children and Adolescents. N. Engl. J. Med. 2004, 350, 2362–2374. [Google Scholar] [CrossRef]
- Kułaga, Z.; Litwin, M.; Tkaczyk, M.; Palczewska, I.; Zajączkowska, M.; Zwolińska, D.; Krynicki, T.; Wasilewska, A.; Moczulska, A.; Morawiec-Knysak, A.; et al. Polish 2010 Growth References for School-Aged Children and Adolescents. Eur. J. Pediatr. 2011, 170, 599–609. [Google Scholar] [CrossRef]
- Kułaga, Z.; Litwin, M.; Grajda, A.; Kułaga, K.; Gurzkowska, B.; Góźdź, M.; Pan, H. Oscillometric Blood Pressure Percentiles for Polish Normal-Weight School-Aged Children and Adolescents. J. Hypertens 2012, 30, 1942–1954. [Google Scholar] [CrossRef]
- Dembińska-Kieć, A.; Naskalski, J.W.; Solnica, B. Diagnostyka Laboratoryjna Z Elementami Biochemii Klinicznej; Edra Urban & Partner: Wrocław, Poland, 2018. [Google Scholar]
- Narodowy Fundusz Zdrowia. NFZ O Zdrowiu: Cukrzyca. Centrala Narodowego Funduszu Zdrowia, A.N. Narodowy Fundusz Zdrowia. NFZ O Zdrowiu: Cukrzyca. Centrala Narodowego Funduszu Zdrowia. Available online: https://www.nfz.gov.pl (accessed on 15 November 2019).
- Köken, Ö.Y.; Kara, C.; Can Yılmaz, G.; Aydın, H.M. Prevalence of Obesity and Metabolic Syndrome in Children with Type 1 Diabetes: A Comparative Assessment Based on Criteria Established by the International Diabetes Federation, World Health Organisation and National Cholesterol Education Program. J. Clin. Res. Pediatr. Endocrinol. 2020, 12, 55–62. [Google Scholar] [CrossRef] [PubMed]
- Saki, F.; Setoodehnia, Z.; Javanmardi, H.; Omrani, G. Association between Metabolic Syndrome Criteria and Body-Composition Components in Children with Type 1 Diabetes Mellitus. Int. J. Pediatr. 2016, 4, 3709–3717. [Google Scholar] [CrossRef]
- Łuczyński, W.; Szypowska, A.; Głowińska-Olszewska, B.; Bossowski, A. Overweight, Obesity and Features of Metabolic Syndrome in Children with Diabetes Treated with Insulin Pump Therapy. Eur. J. Pediatr. 2011, 170, 891–898. [Google Scholar] [CrossRef]
- Soliman, H.M.; Mosaad, Y.O.; Ibrahim, A. The Prevalence and the Clinical Profile of Metabolic Syndrome in Children and Adolescents with Type 1 Diabetes. Diabetes Metab. Syndr. 2019, 13, 1723–1726. [Google Scholar] [CrossRef]
- Saki, F. Prevalence of Metabolic Syndrome in Children with Type 1 Diabetes in South of Iran. J. Compr. Ped. 2016, 7, E37703. [Google Scholar] [CrossRef]
- Hurrle, S.; Hsu, W.H. The Etiology of Oxidative Stress in Insulin Resistance. BioMed. J. 2017, 40, 257–262. [Google Scholar] [CrossRef] [PubMed]
- Hou, X.; Liu, J.; Song, J.; Wang, C.; Liang, K.; Sun, Y.; Ma, Z.; Yang, W.; Li, C.; Zhang, X.; et al. Relationship of Hemoglobin A1c with Β Cell Function and Insulin Resistance in Newly Diagnosed and Drug Naive Type 2 Diabetes Patients. J. Diabetes Res. 2016, 2016, 8797316. [Google Scholar] [CrossRef]
- Parthasarathy, L.; Khadilkar, V.; Chiplonkar, S.; Khadilkar, A. Effect of Antioxidant Supplementation on Total Antioxidant Status in Indian Children with Type 1 Diabetes. J. Diet Suppl. 2019, 16, 390–400. [Google Scholar] [CrossRef]
- Salmonowicz, B.; Krzystek-Korpacka, M.; Noczyńska, A. Trace Elements, Magnesium, and the Efficacy of Antioxidant Systems in Children with Type 1 Diabetes Mellitus and in Their Siblings. Adv. Clin. Exp. Med. 2014, 23, 259–268. [Google Scholar] [CrossRef]
- Stefan, N. Causes, Consequences, and Treatment of Metabolically Unhealthy Fat Distribution. Lancet Diabetes Endocrinol. 2020, 8, 616–627. [Google Scholar] [CrossRef]
- Maffeis, C.; Fornari, E.; Morandi, A.; Piona, C.; Tomasselli, F.; Tommasi, M.; Marigliano, M. Glucose-Independent Association of Adiposity and Diet Composition with Cardiovascular Risk in Children and Adolescents with Type 1 Diabetes. Acta Diabetologica 2017, 54, 599–605. [Google Scholar] [CrossRef] [PubMed]
- Lipsky, L.; Gee, B.; Liu, A.; Nansel, T. Body Mass Index and Adiposity Indicators Associated with Cardiovascular Biomarkers in Youth with Type 1 Diabetes Followed Prospectively. Pediatr. Obes. 2017, 12, 468–476. [Google Scholar] [CrossRef] [PubMed]
- Komatsu, W.R.; Gabbay, M.A.L.; Castro, M.L.; Saraiva, G.L.; Chacra, A.R.; De Barros Neto, T.L.; Dib, S.A. Aerobic Exercise Capacity in Normal Adolescents and Those with Type 1 Diabetes Mellitus. Pediatr. Diabetes 2005, 6, 145–149. [Google Scholar] [CrossRef]
- Pietrzak, I.; Mianowska, B.; Gadzicka, A.; Młynarski, W.; Szadkowska, A. Blood Pressure in Children and Adolescents with Type 1 Diabetes Mellitus—The Influence of Body Mass Index and Fat Mass. Pediatr. Endocrinol. Diabetes Metab. 2009, 15, 240–245. [Google Scholar]
- Cherubini, V.; Marino, M.; Marigliano, M.; Maffeis, C.; Zanfardino, A.; Rabbone, I.; Giorda, S.; Schiaffini, R.; Lorubbio, A.; Rollato, S.; et al. Rethinking Carbohydrate Intake and Time in Range in Children and Adolescents with Type 1 Diabetes. Nutrients 2021, 13, 3869. [Google Scholar] [CrossRef]
- Lodefalk, M.; Aman, J. Food Habits, Energy and Nutrient Intake in Adolescents with Type 1 Diabetes Mellitus. Diabet Med. 2006, 23, 1225–1232. [Google Scholar] [CrossRef]
- Katz, M.L.; Mehta, S.; Nansel, T.; Quinn, H.; Lipsky, L.M.; Laffel, L.M. Associations of Nutrient Intake with Glycemic Control in Youth with Type 1 Diabetes: Differences by Insulin Regimen. Diabetes Technol. Ther. 2014, 16, 512–518. [Google Scholar] [CrossRef]
- Thomson, R.; Adams, L.; Anderson, J.; Maftei, O.; Couper, J.; Giles, L.; Peña, A.S. Australian Children with Type 1 Diabetes Consume High Sodium and High Saturated Fat Diets: Comparison with National and International Guidelines. J. Paediatr. Child Health 2019, 55, 1188–1193. [Google Scholar] [CrossRef]
- Kraus, W.E.; Houmard, J.A.; Duscha, B.D.; Knetzger, K.J.; Wharton, M.B.; Mccartney, J.S.; Bales, C.W.; Henes, S.; Samsa, G.P.; Otvos, J.D.; et al. Effects of the Amount and Intensity of Exercise on Plasma Lipoproteins. N. Engl. J. Med. 2002, 347, 1483–1492. [Google Scholar] [CrossRef]
- Nordmann, A.J.; Nordmann, A.; Briel, M.; Keller, U.; Yancy, W.S., Jr.; Brehm, B.J.; Bucher, H.C. Effects of Low-Carbohydrate Vs Low-Fat Diets on Weight Loss and Cardiovascular Risk Factors: A Meta-Analysis of Randomized Controlled Trials. Arch. Intern. Med. 2006, 166, 285–293. [Google Scholar] [CrossRef]
- Zomer, E.; Gurusamy, K.; Leach, R.; Trimmer, C.; Lobstein, T.; Morris, S.; James, W.P.; Finer, N. Interventions That Cause Weight Loss and the Impact on Cardiovascular Risk Factors: A Systematic Review and Meta-Analysis. Obes. Rev. 2016, 17, 1001–1011. [Google Scholar] [CrossRef] [PubMed]
- Mozaffarian, D.; Micha, R.; Wallace, S. Effects on Coronary Heart Disease of Increasing Polyunsaturated Fat in Place of Saturated Fat: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. PLoS Med. 2010, 7, E1000252. [Google Scholar] [CrossRef] [PubMed]
- Jacobson, T.A.; Glickstein, S.B.; Rowe, J.D.; Soni, P.N. Effects of Eicosapentaenoic Acid and Docosahexaenoic Acid on Low-Density Lipoprotein Cholesterol and Other Lipids: A Review. J. Clin. Lipidol. 2012, 6, 5–18. [Google Scholar] [CrossRef] [PubMed]
- De Natale, C.; Annuzzi, G.; Bozzetto, L.; Mazzarella, R.; Costabile, G.; Ciano, O.; Riccardi, G.; Rivellese, A.A. Effects of A Plant-Based High-Carbohydrate/High-Fiber Diet Versus High-Monounsaturated Fat/Low-Carbohydrate Diet on Postprandial Lipids in Type 2 Diabetic Patients. Diabetes Care 2009, 32, 2168–2173. [Google Scholar] [CrossRef]
- Tykarski, A.; Filipiak, K.J.; Januszewicz, A.; Litwin, M.; Narkiewicz, K.; Prejbisz, A.; Ostalska-Nowicka, D.; Widecka, K.; Kostka-Jeziorny, K. Zasady Postępowania W Nadciśnieniu Tętniczym—2019 Rok. Nadciśnienie Tętnicze W Prakt. 2019, 5, 1–86. [Google Scholar]
- Aburto, N.J.; Ziolkovska, A.; Hooper, L.; Elliott, P.; Cappuccio, F.P.; Meerpohl, J.J. Effect of Lower Sodium Intake on Health: Systematic Review and Meta-Analyses. BMJ 2013, 346, F1326. [Google Scholar] [CrossRef]

| Nutrients | Polish Standards for Healthy Children [17] | Diabetes Poland Standards [18] | ISPAD Standards [19] |
|---|---|---|---|
| Protein | 10–20% | 15–20% | 15–20% |
| Carbohydrates | 45–65% | 45% (up to 60% if low-GI, high-fiber food) | 45–50% |
| Fat | 20–35% | 25–40% | up to 30–35% |
| SFA | as low as possible | <10% | <10% |
| MUFA | - | <20% | - |
| PUFA | - | 6–10% | - |
| EPA + DHA | 250 mg | - | - |
| ALA | 0.5% | - | - |
| LA | 4% | - | - |
| Dietary fiber | 19 g (10–15 y), 21 g (16–18 y) | >25 g or 15 g/1000 kcal | Age (y) + 5 g |
| Parameter | Participants | |
|---|---|---|
| with T1DM (n = 60) | without T1DM (n = 60) | |
| Me ± IQR | ||
| Age (years) | 14 (12–16) | 15 (13–16) |
| Body height (cm) | 166 (156–173) | 168 (162–176) |
| Body weight (kg) | 54 (45–66) | 58 (47–69) |
| Age of diagnosis (years) | 9 (7–11) | |
| Diabetes duration (years) | 5 (2–7) | |
| HbA1c (%) | 7.6 (6.6–10.2) | |
| n (%) | ||
| Gender (girls/boys) | 27 (45%)/33 (55%) | 16 (27%)/44 (73%) |
| Type of insulin therapy (MDI/CSII) | 23 (38%)/37 (52%) | |
| Type of glucose-monitoring system (FGM/CGM) | 18 (70%)/8 (30%) | |
| Criteria | T1DM Group (n = 60) | Patients without T1DM (n = 60) | ||
|---|---|---|---|---|
| Total | Girls/Boys | Total | Girls/Boys | |
| ATP | 15 (25%) | 11 (41%)/4 (12%) | 3 (5%) | 1 (6%)/2 (5%) |
| IDF | 5 (8%) | 3 (11%)/2 (6%) | 3 (5%) | 0/3 (7%) |
| WHO | 8 (13%) | 4 (15%)/4 (12%) | 1 (2%) | 0/1 (2%) |
| Grabia et al. (modified Weiss et al.) | 11 (18%) | 9 (33%)/2 (6%) | 1 (2%) | 0/1 (2%) |
| Parameter | MetS+ (n = 20) | MetS− (n = 40) | Control Group (n = 55) | p-Value | |
|---|---|---|---|---|---|
| Me ± IQR | MetS+ vs. MetS− | MetS+ vs. Control | |||
| WC (cm) | 73 (69–78) | 66 (62–70) | 70 (67–74) | <0.001 | N/S |
| WHR | 0.87 (0.84–0.9) | 0.87 (0.81–0.91) | 0.88 (0.85–0.92) | N/S | N/S |
| WHtR | 0.40 (0.39–0.42) | 0.40 (0.38–0.42) | 0.44 (0.42–0.48) | <0.001 | <0.001 |
| BMI (kg/m2) | 22.6 (19.9–24.5) | 19.8 (17.9–21.2) | 20.3 (18.6–22.0) | <0.01 | <0.5 |
| FGL (mg/dL) | - | - | 98 (93–103) | - | - |
| HbA1c (%) | 8.9 (7.4–11.4) | 6.9 (6.4–9.2) | - | <0.001 | - |
| eGDR (mg/kg/min) | 8.0 (6.3–10.0) | 10.8 (8.8–11.6) | - | <0.001 | - |
| TC (mg/dL) | 157 (124–187) | 148 (123–170) | 143 (131–187) | N/S | N/S |
| LDL-ch (mg/dL) | 102 (74–111) | 80 (66–101) | 86 (76–110) | <0.5 | N/S |
| HDL-ch (mg/dL) | 44.5 (34.5–57.5) | 59 (48–71) | 57 (52–64) | <0.001 | <0.001 |
| TG (mg/dL) | 101 (67–143) | 60 (47–91) | 59 (45–76) | <0.001 | <0.001 |
| SBP (mmHg) | 120 (110–128) | 114 (109–118) | 118 (110–125) | <0.5 | N/S |
| DBP (mmHg) | 74 (70–80) | 70 (66–73) | 70 (65–74) | <0.01 | <0.5 |
| Study Group | HbA1c (%) | TAS (mmol/L) | p-Value | HbA1c Group | HbA1c | p-Value | HbA1c (%) | p-Value | TAS (mmol/L) | p-Value |
|---|---|---|---|---|---|---|---|---|---|---|
| Me ± IQR | n(%) | Me ± IQR | Me ± IQR | |||||||
| MetS+ (n = 20) | 8.9 (7.4–11.4) | 1.249 (1.054–1.322) | MetS+ vs. MetS− <0.01HbA1c, TAS | (<7%) | 3 (12%) | <0.01 | 6.7 (6.2–7.0) | <0.001 | 1.230 (1.212–1.382) | MetS+HbA1c>7% vs. MetS−HbA1c>7% <0.01 |
| (>7%) | 17 (49%) | 9.9 (7.7–12.2) | 1.243 (1.041–1.314) | |||||||
| MetS− (n = 40) | 6.9 (6.4–9.2) | 1.394 (1.225–1.595) | MetS+ vs. Control MetS− vs. Control <0.001TAS | (<7%) | 22 (88%) | 6.4 (6.0–6.7) | <0.001 | 1.403 (1.206–1.533) | ||
| (>7%) | 18 (51%) | 9.7 (7.8–12.1) | 1.370 (1.256–1.655) | |||||||
| Control group (n = 55) | - | 1.579 (1.457–1.799) | - | |||||||
| Parameter | MetS+ (n = 20) | MetS− (n = 40) | Control Group (n = 55) | p-Value | |
|---|---|---|---|---|---|
| Me ± IQR | MetS+ vs. MetS− | MetS+ vs. Control | |||
| Body weight (kg) | 64 (52–73) | 52 (43–59) | 58 (48–68) | <0.5 | NS |
| Body height (cm) | 167 (156–173) | 164 (155–173) | 169 (163–176) | NS | NS |
| TBW (L) | 33 (28–38) | 30 (26–38) | 37 (31–41) | NS | NS |
| SMM (kg) | 24 (21–29) | 22 (19–29) | 24 (18–30) | NS | NS |
| Protein (kg) | 8.6 (7.6–10.2) | 8.1 (6.9–10.2) | 9.1 (7.9–10.5) | NS | NS |
| Minerals (kg) | 3.3 (2.7–3.6) | 2.9 (2.5–3.5) | 3.2 (2.8–3.9) | NS | NS |
| PBF (%) | 26 (21–33) | 16 (12–23) | 14 (12–16) | <0.001 | <0.001 |
| VFA (cm2) | 77 (54–100) | 42 (28–48) | 35 (26–44) | <0.001 | <0.001 |
| Nutrient | MetS+ (n = 20) | MetS− (n = 40) | Control Group (n = 55) | p-Value (MetS+ vs. Control) |
|---|---|---|---|---|
| Me ± IQR | ||||
| Main nutrients | ||||
| Energy (kcal) | 1760 (1697–1924) | 1803 (1574–1916) | 1859 (1735–1935) | N/S |
| Protein (%TDEE) | 20.0 (16.4–20.8) | 18.1 (15.8–20.6) | 16.4 (13.1–18.6) | <0.01 |
| Carbohydrate (%TDEE) | 56.5 (50.8–59.9) | 54.8 (50.6–59.5) | 55.4 (51.5–61.1) | N/S |
| Fat (%TDEE) | 22.8 (20.0–28.1) | 24.3 (21.2–29.1) | 28.1 (23.7–32.4) | <0.01 |
| Fatty acids | ||||
| SFA (g) | 17.6 (14.3–20.7) | 16.4 (15.3–17.5) | 16.0 (15.1–17.9) | N/S |
| Palmitic acid (g) | 10.4 (9.4–11.4) | 10.1 (8.9–11.6) | 9.8(8.6–10.8) | N/S |
| MUFA (g) | 14.2 (11.9–17.7) | 14.2 (11.2–19.2) | 24.6 (20.5–28.5) | <0.001 |
| Oleic acid (g) | 12.3 (10.6–14.8) | 13.1 (10.8–16.3) | 21.4 (16.6–25.4) | <0.001 |
| PUFA (g) | 5.8 (5.0–7.1) | 6.2 (4.6–8.1) | 9.8 (7.4–11.6) | <0.001 |
| LC-PUFA (g) | 0.069 (0.036–0.205) | 0.069 (0.04–0.093) | 0.093 (0.06–0.231) | <0.05 |
| ω-3 (g) | 0.831 (0.569–1.178) | 0.688 (0.554–1.28) | 1.3 (0.948–1.6) | <0.001 |
| ALA (g) | 0.688 (0.524–0.817) | 0.554 (0.478–0.879) | 1.2 (0.822–1.4) | <0.001 |
| EPA (g) | 0.014 (0.006–0.045) | 0.012 (0.007–0.017) | 0.024 (0.008–0.052) | N/S |
| DHA (g) | 0.039 (0.024–0.148) | 0.038 (0.022–0.066) | 0.066 (0.038–0.137) | <0.001 |
| ω-6 (g) | 4.9 (4.2–5.9) | 5.5 (3.9–6.5) | 7.6 (6.1–9.6) | <0.001 |
| LA (g) | 4.8 (4.1–5.9) | 5.5 (3.8–6.4) | 7.3 (6.0–9.4) | <0.001 |
| AA (g) | 0.048 (0.032–0.151) | 0.048 (0.031–0.096) | 0.111 (0.073–0.181) | <0.05 |
| Carbohydrates | ||||
| Glucose (g) | 8.1 (4.0–9.6) | 4.8 (2.6–6.5) | 6.8 (5.1–8.1) | N/S |
| Fructose (g) | 10.1 (4.6–12.9) | 7.3 (4.2–11.1) | 8.3 (6.5–11.0) | N/S |
| Saccharose (g) | 39.5 (30.2–54.8) | 33.1 (13.7–45.0) | 44.1 (35.1–51.6) | N/S |
| Dietary fiber (g) | 18.1 (16.6–21.4) | 18.0 (13.8–20.8) | 19.6 (16.0–23.0) | N/S |
| Nutrient | Recommendation | MetS+ (n = 20) | MetS− (n = 40) | Control Group (n = 55) | p-Value (MetS+ vs. Control) |
|---|---|---|---|---|---|
| Main nutrients | |||||
| Protein | <10% | 0 (0%) | 0 (0%) | 3 (5%) | <0.05 |
| 10–20% | 15 (75%) | 33 (83%) | 49 (90%) | ||
| >20% | 5 (25%) | 7 (17%) | 3 (5%) | ||
| Protein PolDiab | <15% | 2 (10%) | 6 (15%) | 21 (38%) | <0.01 |
| 15–20% | 13 (65%) | 27 (68%) | 31 (56%) | ||
| >20% | 5 (25%) | 7 (17%) | 3 (6%) | ||
| Fat | <20% | 5 (25%) | 6 (15%) | 4 (7%) | <0.05 |
| 20–35% | 15 (75%) | 33 (83%) | 47 (86%) | ||
| >35% | 0 (0%) | 1 (2%) | 4 (7%) | ||
| Fat PolDiab | <25% | 14 (70%) | 23 (58%) | 20 (36%) | <0.01 |
| 25–40% | 6 (30%) | 17 (43%) | 35 (64%) | ||
| >40% | 0 (0%) | 0 (0%) | 0 (0%) | ||
| Carbohydrates | <45% | 0 (0%) | 2 (5%) | 2 (3%) | N/S |
| 45–65% | 18 (90%) | 37 (93%) | 52 (95%) | ||
| >65% | 2 (10%) | 1 (2%) | 1 (2%) | ||
| Carbohydrates PolDiab | <45% | 0 (0%) | 2 (5%) | 2 (4%) | N/S |
| 45–60% | 16 (80%) | 31 (78%) | 39 (71%) | ||
| >60% | 4 (20%) | 7 (17%) | 14 (25%) | ||
| Carbohydrates ISPAD | <45% | 0 (0%) | 2 (5%) | 2 (4%) | N/S |
| 45–50% | 5 (25%) | 9 (22%) | 9 (16%) | ||
| >50% | 15 (75%) | 29 (73%) | 44 (80%) | ||
| Fatty acids | |||||
| SFA | <10% | 13 (65%) | 29 (73%) | 49 (89%) | <0.05 |
| ≥10% | 7 (35%) | 11 (27%) | 6 (11%) | ||
| MUFA | <10% | 15 (75%) | 29 (73%) | 15 (27%) | <0.001 |
| 10–20% | 5 (25%) | 11 (27%) | 38 (69%) | ||
| >20% | 0 (0%) | 0 (0%) | 2 (4%) | ||
| LA | <3.5% | 19 (95%) | 31 (78%) | 26 (47%) | <0.001 |
| 3.5–4.5% | 1 (5%) | 7 (18%) | 16 (29%) | ||
| >4.5% | 0 (0%) | 2 (4%) | 13 (24%) | ||
| ALA | ≤0.5% | 17 (85%) | 33 (83%) | 23 (42%) | <0.01 |
| >0.5% | 3 (15%) | 7 (17%) | 32 (58%) | ||
| EPA + DHA | ≤250 mg | 17 (85%) | 37 (93%) | 44 (80%) | N/S |
| >250 mg | 3 (15%) | 7 (3%) | 11 (20%) | ||
| PUFA | <6% | 18 (90%) | 39 (97%) | 45 (82%) | N/S |
| 6–10% | 2 (10%) | 1 (2%) | 9 (16%) | ||
| >10% | 0 (0%) | 0 (0%) | 1 (2%) | ||
| Carbohydrates | |||||
| Saccharose | ≤10% | 12 (60%) | 30 (75%) | 30 (55%) | N/S |
| >10% | 8 (40%) | 10 (25%) | 25 (45%) | ||
| Dietary fiber | >19 g | 13 (65%) | 27 (68%) | 26 (47%) | N/S |
| ≥19 g | 7 (35%) | 13 (32%) | 29 (53%) | ||
| Dietary fiber PolDiab | <25 g | 18 (90%) | 39 (98%) | 46 (83%) | N/S |
| ≥25 g | 2 (10%) | 1 (2%) | 9 (17%) | ||
| Food Products | Never | 1–3 Times a Month | Once a Week | Several Times a Week | Once a Day | Several Times a Day | |
|---|---|---|---|---|---|---|---|
| Wheat bread | MetS+ | 0 (0%) | 1 (5%) | 1 (5%) | 5 (25%) | 5 (25%) | 8 (40%) |
| MetS− | 2 (5%) | 2 (5%) | 3 (8%) | 8 (20%) | 6 (15%) | 19 (47%) | |
| Control | 6 (11%) | 2 (4%) | 4 (7%) | 21 (38%) | 15 (27%) | 7 (13%) | |
| Wholemeal bread | MetS+ | 2 (10%) | 3 (15%) | 6 (30%) | 5 (25%) | 1 (5%) | 3 (15%) |
| MetS− | 3 (8%) | 2 (5%) | 8 (20%) | 11 (27%) | 10 (25%) | 6 (15%) | |
| Control | 6 (11%) | 3 (5%) | 6 (11%) | 25 (45%) | 12 (22%) | 3 (6%) | |
| Groats, pasta, rice | MetS+ | 0 (0%) | 2 (10%) | 10 (50%) | 7 (35%) | 1 (5%) | 0 (0%) |
| MetS− | 0 (0%) | 7 (17%) | 12 (30%) | 20 (50%) | 1 (3%) | 0 (0%) | |
| Control | 0 (0%) | 8 (15%) | 9 (16%) | 35 (63%) | 2 (4%) | 1 (2%) | |
| Potatoes | MetS+ | 0 (0%) | 0 (0%) | 0 (0%) | 9 (45%) | 11 (55%) | 0 (0%) |
| MetS− | 0 (0%) | 2 (5%) | 2 (5%) | 21 (52%) | 15 (38%) | 0 (0%) | |
| Control | 0 (0%) | 11 (20%) | 13 (23%) | 25 (46%) | 4 (7%) | 2 (4%) | |
| Red meat | MetS+ | 1 (5%) | 7 (35%) | 6 (30%) | 6 (30%) | 0 (0%) | 0 (0%) |
| MetS− | 6 (15%) | 6 (15%) | 5 (12%) | 19 (48%) | 2 (5%) | 2 (5%) | |
| Control | 3 (5%) | 5 (9%) | 15 (27%) | 30 (55%) | 2 (4%) | 0 (0%) | |
| White meat | MetS+ | 0 (0%) | 2 (10%) | 6 (30%) | 11 (55%) | 1 (5%) | 0 (0%) |
| MetS− | 1 (2%) | 3 (7%) | 5 (13%) | 27 (68%) | 2 (5%) | 2 (5%) | |
| Control | 0 (0%) | 2 (4%) | 7 (13%) | 43 (78%) | 3 (5%) | 0 (0%) | |
| Fried products | MetS+ | 1 (5%) | 3 (15%) | 6 (30%) | 5 (25%) | 5 (25%) | 0 (0%) |
| MetS− | 1 (3%) | 4 (10%) | 16 (40%) | 18 (44%) | 0 (0%) | 1 (3%) | |
| Control | 1 (2%) | 6 (11%) | 14 (25%) | 30 (55%) | 4 (7%) | 0 (0%) | |
| Fast-food | MetS+ | 2 (10%) | 11 (55%) | 5 (25%) | 2 (10%) | 0 (0%) | 0 (0%) |
| MetS− | 4 (10%) | 25 (63%) | 10 (25%) | 1 (2%) | 0 (0%) | 0 (0%) | |
| Control | 9 (16%) | 37 (67%) | 8 (15%) | 1 (2%) | 0 (0%) | 0 (0%) | |
| Fruit | MetS+ | 0 (0%) | 0 (0%) | 1 (5%) | 6 (30%) | 9 (45%) | 4 (20%) |
| MetS− | 0 (0%) | 3 (8%) | 0 (0%) | 13 (32%) | 11 (28%) | 13 (32%) | |
| Control | 0 (0%) | 0 (0%) | 2 (3%) | 18 (33%) | 17 (31%) | 18 (33%) | |
| Vegetables | MetS+ | 0 (0%) | 0 (0%) | 2 (10%) | 8 (40%) | 5 (25%) | 5 (25%) |
| MetS− | 0 (0%) | 0 (0%) | 2 (5%) | 13 (33%) | 8 (20%) | 17 (42%) | |
| Control | 0 (0%) | 0 (0%) | 3 (6%) | 17 (31%) | 19 (35%) | 16 (28%) | |
| Beverages with sweeteners | MetS+ | 2 (10%) | 3 (15%) | 3 (15%) | 10 (50%) | 2 (10%) | 0 (0%) |
| MetS− | 9 (22%) | 4 (10%) | 12 (30%) | 9 (22%) | 5 (13%) | 1 (3%) | |
| Control | 13 (24%) | 8 (14%) | 11 (20%) | 12 (22%) | 10 (18%) | 1 (2%) | |
| Energy drink | MetS+ | 13 (65%) | 2 (10%) | 4 (20%) | 1 (5%) | 0 (0%) | 0 (0%) |
| MetS− | 30 (75%) | 3 (7%) | 6 (15%) | 1 (3%) | 0 (0%) | 0 (0%) | |
| Control | 47 (85%) | 5 (9%) | 3 (6%) | 0 (0%) | 0 (0%) | 0 (0%) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Grabia, M.; Markiewicz-Żukowska, R.; Socha, K.; Polkowska, A.; Zasim, A.; Boruch, K.; Bossowski, A. Prevalence of Metabolic Syndrome in Relation to Cardiovascular Biomarkers and Dietary Factors among Adolescents with Type 1 Diabetes Mellitus. Nutrients 2022, 14, 2435. https://doi.org/10.3390/nu14122435
Grabia M, Markiewicz-Żukowska R, Socha K, Polkowska A, Zasim A, Boruch K, Bossowski A. Prevalence of Metabolic Syndrome in Relation to Cardiovascular Biomarkers and Dietary Factors among Adolescents with Type 1 Diabetes Mellitus. Nutrients. 2022; 14(12):2435. https://doi.org/10.3390/nu14122435
Chicago/Turabian StyleGrabia, Monika, Renata Markiewicz-Żukowska, Katarzyna Socha, Agnieszka Polkowska, Aneta Zasim, Karolina Boruch, and Artur Bossowski. 2022. "Prevalence of Metabolic Syndrome in Relation to Cardiovascular Biomarkers and Dietary Factors among Adolescents with Type 1 Diabetes Mellitus" Nutrients 14, no. 12: 2435. https://doi.org/10.3390/nu14122435
APA StyleGrabia, M., Markiewicz-Żukowska, R., Socha, K., Polkowska, A., Zasim, A., Boruch, K., & Bossowski, A. (2022). Prevalence of Metabolic Syndrome in Relation to Cardiovascular Biomarkers and Dietary Factors among Adolescents with Type 1 Diabetes Mellitus. Nutrients, 14(12), 2435. https://doi.org/10.3390/nu14122435