The Polish Version of the Avoidant/Restrictive Food Intake Disorder Questionnaire—Parents Report (ARFID-Q-PR) and the Nine Items Avoidant/Restrictive Food Intake Disorder Screen—Parents Report (NIAS-PR): Maternal Perspective
Abstract
:1. Introduction
1.1. ARFID Incidence, Prevalence, and Diagnostic Considerations
- (A)
- An eating or feeding disturbance (e.g., apparent lack of interest in eating or food; avoidance based on the sensory characteristics of food; concern about aversive consequences of eating) associated with one (or more) of the following:
- Significant weight loss (or failure to achieve expected weight gain or faltering growth in children).
- Significant nutritional deficiency.
- Dependence on enteral feeding or oral nutritional supplements.
- Marked interference with psychosocial functioning.
- (B)
- The disturbance is not better explained by lack of available food or by an associated culturally sanctioned practice.
- (C)
- The eating disturbance does not occur exclusively during the course of anorexia nervosa or bulimia nervosa, and there is no evidence of a disturbance in the way in which one’s body weight or shape is experienced.
- (D)
- The eating disturbance is not attributable to a concurrent medical condition or not better explained by another mental disorder. When the eating disturbance occurs in the context of another condition or disorder, the severity of the eating disturbance exceeds that routinely associated with the condition or disorder and warrants additional clinical attention.
1.2. Objective of the Study
2. Methods
2.1. Participants and Procedure
2.2. Measures
2.2.1. Demographic Schedule
2.2.2. Nine Items Avoidant/Restrictive Food Intake Disorder Screen—Parent Report (NIAS-PR)
2.2.3. ARFID Questionnaire—Parent Report (ARFID-Q-PR)
3. Results
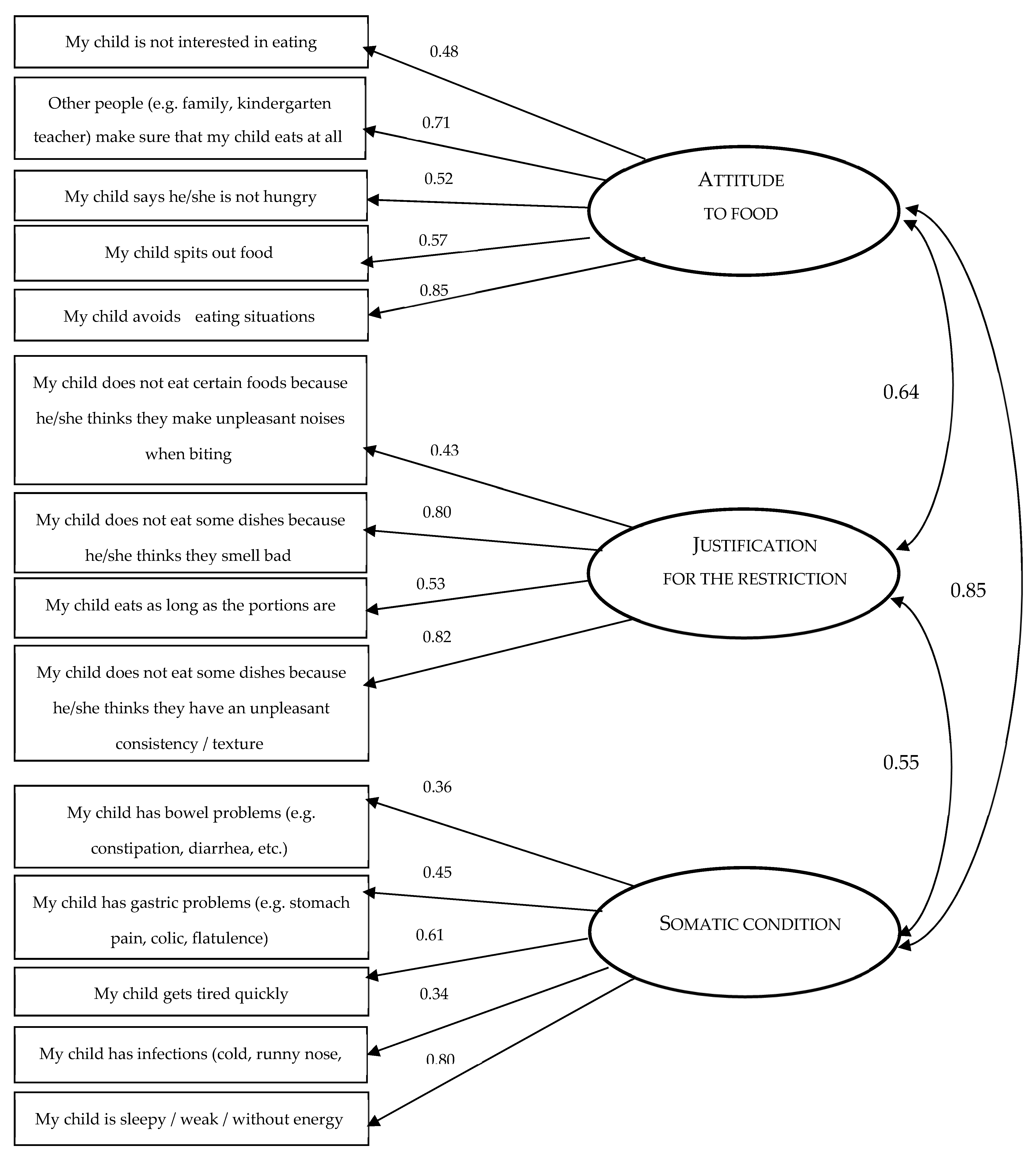
3.1. Factor Structure of Research Tools
3.2. Structural Modeling for Research Tools
- (a)
- criterion for the sum of the subscales “attitude to food” and “justification for restriction”: the mean for the sum of these subscales was M = 18.26 (SD = 6.00). The score indicating symptoms of ARFID was determined by summing up the mean value and 1 SD (25 points). There were 23 people who achieved this result in the sample (13.77%).
- (b)
- criterion for the ARFID-Q-PR overall score (sum of the subscales “attitude to food, justification for restriction” and “somatic condition”): the mean for the overall ARFID-Q-PR score was M = 23.83 (SD = 5.72). The score that indicates symptoms of ARFID was determined by summing up the mean value and 2 SD (35 points). There were 6 (3.59%) people in the sample who achieved this result.
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th ed.; American Psychiatric Publishing: Arlington, VA, USA, 2013. [Google Scholar]
- Fisher, M.M.; Rosen, D.S.; Ornstein, R. Characteristics of avoidant/restrictive food intake disorder in children and adolescents: A “new disorder” in DSM-5. J. Adolesc. Health 2014, 55, 49–52. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nicely, T.A.; Lane-Loney, S.; Masciulli, E. Prevalence and characteristics of avoidant/restrictive food intake disorder in a cohort of young patients in day treatment for eating disorders. J. Eat. Disord. 2014, 2, 21–25. [Google Scholar] [CrossRef] [PubMed]
- Thomas, J.J.; Brigham, K.S.; Sally, S.T.; Hazen, E.P.; Eddy, K.T. Case 18-2017: An 11-year-old girl with difficulty eating after a choking incident. N. Engl. J. Med. 2017, 376, 2377–2386. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kurz, S.; van Dyck, Z.; Dremmel, D. Early-onset restrictive eating disturbances in primary school boys and girls. Eur. Child Adolesc. Psychiatry 2015, 24, 779–785. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zickgraf, H.F.; Murray, H.B.; Kratz, H.E.; Franklin, M.E. Characteristics of outpatients diagnosed with the selective/neophobic presentation of avoidant/restrictive food intake disorder. Int. J. Eat. Disord. 2019, 52, 367–377. [Google Scholar] [CrossRef] [PubMed]
- Sdravou, K.; Fotoulaki, M.; Emmanouilidou-Fotoulaki, E.; Andreoulakis, E.; Makris, G.; Sotiriadou, F.; Printza, A. Feeding Problems in Typically Developing Young Children, a Population-Based Study. Children 2021, 8, 388. [Google Scholar] [CrossRef] [PubMed]
- Katzman, D.K.; Spettigue, W.; Agostino, H.; Couturier, J.; Dominic, A.; Findlay, S.M.; Lam, P.-Y.; Lane, M.; Maguire, B.; Mawjee, K.; et al. Incidence and Age- and Sex-Specific Differences in the Clinical Presentation of Children and Adolescents with Avoidant Restrictive Food Intake Disorder. JAMA Pediatr. 2021, 175, e213861. [Google Scholar] [CrossRef]
- Sdravou, K.; Emmanouilidou-Fotoulaki, E.; Printza, A.; Andreoulakis, E.; Beropouli, S.; Makris, G.; Fotoulaki, M. Factors Associated with Feeding Problems in Young Children with Gastrointestinal Diseases. Healthcare 2021, 9, 741. [Google Scholar] [CrossRef]
- Sysko, R.; Glasofer, D.R.; Hildebrandt, T.; Klimek, P.; Mitchell, J.E.; Berg, K.C.; Peterson, C.B.; Wonderlich, S.A.; Walsh, B.T. The eating disorder assessment for DSM-5 (EDA-5): Development and validation of a structured interview for feeding and eating disorders. Int. J. Eat. Disord. 2015, 48, 452–463. [Google Scholar] [CrossRef] [Green Version]
- Bermudez, O. ARFID: Some New Twists and Some Old Themes. Available online: https://iaedp.confex.com/iaedp/2017/webprogram/Session3406.html (accessed on 15 June 2022).
- Brigham, K.S.; Manzo, L.D.; Eddy, K.T.; Thomas, J. Evaluation and Treatment of Avoidant/Restrictive Food Intake Disorder (ARFID) in Adolescents. Curr. Pediatr. Rep. 2018, 6, 107–113. [Google Scholar] [CrossRef]
- Coglan, L.; Otasowie, J. Avoidant/restrictive food intake disorder: What do we know so far? BJPsych Adv. 2019, 25, 90–98. [Google Scholar] [CrossRef]
- Leonidas, C.; Souza, A.; Azevedo, L.; Ferreira, I.; Pessa, R.; Santos, M. Emotional and feeding aspects of avoidant/restrictive food intake disorder (ARFID): A case report. Int. J. Psychiatry 2020, 5, 21, ISSN: 2475-5435. [Google Scholar]
- Forman, S.F.; McKenzie, N.; Hehn, R. Predictors of outcome at 1 year in adolescents with DSM-5 restrictive eating disorders: Report of the national eating disorders quality improvement collaborative. J. Adolesc. Health 2014, 5, 750–756. [Google Scholar] [CrossRef] [PubMed]
- Zickgraf, H.F.; Lane-Loney, S.; Essayli, J.H.; Ornstein, R.M. Further support for diagnostically meaningful ARFID symptom presentations in an adolescent medicine partial hospitalization program. Int. J. Eat. Disord. 2019, 52, 402–409. [Google Scholar] [CrossRef]
- Norris, M.L.; Spettigue, W.J.; Katzman, D.K. Update on eating disorders: Current perspectives on avoidant/restrictive food intake disorder in children and youth. Neuropsychiatr. Dis. Treat. 2016, 12, 213–218. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Duncombe Lowe, K.; Barnes, T.L.; Martell, C.; Keery, H.; Eckhardt, S.; Peterson, C.B.; Lesser, J.; Le Grange, D. Youth with Avoidant/Restrictive Food Intake Disorder: Examining Differences by Age, Weight Status, and Symptom Duration. Nutrients 2019, 11, 1955. [Google Scholar] [CrossRef] [Green Version]
- Iron-Segev, S.; Best, D.; Arad-Rubinstein, S.; Efron, M.; Serur, Y.; Dickstein, H.; Stein, D. Feeding, Eating, and Emotional Disturbances in Children with Avoidant/Restrictive Food Intake Disorder (ARFID). Nutrients 2020, 12, 3385. [Google Scholar] [CrossRef] [PubMed]
- Kurz, S.; Van Dyck, Z.; Dremmel, D.; Munsch, S.; Hilbert, A. Variants of early-onset restrictive eating disturbances in middle childhood. Int. J. Eat. Disord. 2016, 49, 102–106. [Google Scholar] [CrossRef] [Green Version]
- Mairs, R.; Nicholls, D. Assessment and treatment of eating disorders in children and adolescents. Arch. Dis. Child. 2016, 101, 1168–1175. [Google Scholar] [CrossRef]
- Zickgraf, H.; Franklin, M.; Rozin, P. Adult picky eaters with symptoms of avoidant/restrictive food intake disorder: Comparable distress and comorbidity but different eating behaviors compared to those with disordered eating symptoms. J. Eat. Disord. 2016, 4, 1–11. [Google Scholar] [CrossRef] [Green Version]
- Chandran, J.J.; Anderson, G.; Kennedy, A.; Kohn, M.; Clarke, S. Subacute degeneration of the spinal cord in an adolescent male with avoidant/restrictive food intake disorder: A clinical case report. Int. J. Eat. Disord. 2015, 48, 1176–1179. [Google Scholar] [CrossRef] [PubMed]
- Tsai, K.; Singh, D.; Pinkhasov, A. Pudendal nerve entrapment leading to avoidant/restrictive food intake disorder (ARFID): A Case report. Int. J. Eat. Disord. 2017, 50, 84–87. [Google Scholar] [CrossRef] [Green Version]
- Sharp, W.; Stubbs, K. Avoidant/restrictive food intake disorder: A diagnosis at the intersection of feeding and eating disorders necessitating subtype differentiation. Int. J. Eat. Disord. 2019, 52, 77. [Google Scholar] [CrossRef] [PubMed]
- Sdravou, K.; Emmanouilidou-Fotoulaki, E.; Printza, A.; Andreoulakis, E.; Evangeliou, A.; Fotoulaki, M. Mealtime Environment and Control of Food Intake in Healthy Children and in Children with Gastrointestinal Diseases. Children 2021, 8, 77. [Google Scholar] [CrossRef]
- Ornstein, R.M.; Rosen, D.S.; Mammel, K.A. Distribution of eating disorders in children and adolescents using the proposed DSM-5 criteria for feeding and eating disorders. J. Adolesc. Health 2013, 53, 303–305. [Google Scholar] [CrossRef]
- Norris, M.L.; Robinson, A.; Obeid, N.; Harrison, M.; Spettigue, W.; Henderson, K. Exploring avoidant/restrictive food intake disorder in eating disordered patients: A descriptive study. Int. J. Eat. Disord. 2014, 47, 495–499. [Google Scholar] [CrossRef]
- Williams, K.; Hendy, H.M.; Field, D.G.; Belousov, Y.; Riegel, K.; Harclerode, W. Implications of Avoidant/Restrictive Food Intake Disorder (ARFID) on Children with Feed. Probl. Child. Health Care 2015, 44, 307–321. [Google Scholar] [CrossRef]
- Eddy, K.T.; Thomas, J.J.; Hastings, E.; Edkins, K.; Lamont, E.; Nevins, C.; Patterson, R.; Murray, H.; Bryant-Waugh, R.; Becker, A. Prevalence of DSM-5 avoidant/restrictive food intake disorder in a pediatric gastroenterology healthcare network. Int. J. Eat. Disord. 2015, 48, 464–470. [Google Scholar] [CrossRef] [PubMed]
- Cooney, M.; Lieberman, M.; Guimond, T.; Katzman, D.K. Clinical and psychological features of children and adolescents diagnosed with avoidant/restrictive food intake disorder in a pediatric tertiary care eating disorder program: A descriptive study. J. Eat. Disord. 2018, 6, 7. [Google Scholar] [CrossRef] [PubMed]
- Murray, H.; Rao, F.; Baker, C.; Silvernale, C.; Staller, K.; Harshman, S.; Thomas, J.; Kuo, B.; Zar-Kessler, C. Prevalence and Characteristics of Avoidant/Restrictive Food Intake Disorder in Pediatric Neurogastroenterology Patients. J. Pediatr. Gastroenterol. Nutr. 2022, 74, 588–592. [Google Scholar] [CrossRef] [PubMed]
- Dinkler, L.; Yasumitsu-Lovell, K.; Eitoku, M.; Fujieda, M.; Suganuma, N.; Hatakenaka, Y.; Hadjikhani, N.; Bryant-Waugh, R.; Råstam, M.; Gillberg, C. Development of a parent-reported screening tool for avoidant/restrictive food intake disorder (ARFID): Initial validation and prevalence in 4–7-year-old Japanese children. Appetite 2022, 168, 105735. [Google Scholar] [CrossRef] [PubMed]
- Hay, P.; Mitchison, D.; Collado, A.E.L.; González-Chica, D.A.; Stocks, N.; Touyz, S. Burden and health-related quality of life of eating disorders, including Avoidant/Restrictive Food Intake Disorder (ARFID), in the Australian population. J. Eat. Disord. 2017, 5, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Mokkink, L.B.; Terwee, C.B.; Patrick, D.L.; Alonso, J.; Stratford, P.W.; Knol, D.L.; Bouter, L.M.; de Vet, H.C. The COSMIN study reached international consensus on taxonomy, terminology, and definitions of meas-urement properties for health-related patient-reported outcomes. J. Clin. Epidemiol. 2010, 63, 737–745. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Burton Murray, B.; Dreier, M.; Zickgraf, H.; Becker, K.; Breithaupt, L. Validation of the nine item ARFID screen (NIAS) subscales for distinguishing ARFID presentations and screening for ARFID. Int. J. Eat. Disord. 2021, 54, 1782–1792. [Google Scholar] [CrossRef]
- Zickgraf, H.; Ellis, J. Initial validation of the Nine Item Avoidant/Restrictive Food Intake disorder screen (NIAS): A measure of 588 three restrictive eating patterns. Appetite 2018, 123, 32–42. [Google Scholar] [CrossRef]
- Nkechi Theresa, E. Procedures for the Construction and Development of Psychological Test. Eur. J. Sci. Res. 2017, 145, 146–151. [Google Scholar]
- Kaiser, H.F. The varimax criterion for analytic rotation in factor analysis. Pyrometrical 1958, 23, 187–200. [Google Scholar] [CrossRef]
- Li-tze, H.; Bentler, P. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Struct. Equ. Modeling A Multidiscip. J. 1999, 6, 1–55. [Google Scholar] [CrossRef]
- Bedyńska, S.; Cypryańska, M. Statystyczny Drogowskaz. Praktyczne Wprowadzenie Do Wnioskowania Statystycznego; Wydawnictwo Akademickie SEDNO: Warszawa, Poland, 2012; ISBN 978-83-63354-17-6. [Google Scholar]
- Eddy, K.T.; Thomas, J.J. Introduction to a special issue on child and adolescent feeding and eating disorders and avoidant/restrictive food intake disorder. Int. J. Eat. Disord. 2019, 52, 327–330. [Google Scholar] [CrossRef]
- Strandjord, S.E.; Sieke, E.H.; Richmond, M.; Rome, E.S. Avoidant/restrictive food intake disorder: Illness and hospital course in 578 patients hospitalized for nutritional insufficiency. J. Adolesc. Health 2015, 57, 673–678. [Google Scholar] [CrossRef]
- Bourne, K.; Stiles, L.; Raj, S.; Shibao, C. Do meals affect heart rate and symptoms in postural orthostatic tachycardia syndrome? Clin. Auton. Res. 2021, 22, 207–214. [Google Scholar] [CrossRef] [PubMed]
- Strand, M.; Hausswolff-Juhlin, Y.; Welch, E. A systematic scoping review of diagnostic validity in avoidant/restrictive food intake disorder. Int. J. Eat. Disord. 2019, 52, 331–360. [Google Scholar] [CrossRef] [PubMed]
- Nitsch, A.; Knopf, E.; Manwaring, J.; Mehler, P. Avoidant/Restrictive Food Intake Disorder (ARFID): Its Medical Complications and Their Treatment—an Emerging Area. Curr. Pediatr. Rep. 2021, 9, 21–29. [Google Scholar] [CrossRef]
- Yule, S.; Wanik, J.; Holm, E.M.; Bruder, M.B.; Shanley, E.; Sherman, C.Q.; Fitterman, M.; Lerner, J.; Marcello, M.; Parenchuck, N.; et al. Nutritional Deficiency Disease Secondary to ARFID Symptoms Associated with Autism and the Broad Autism Phenotype: A Qualitative Systematic Review of Case Reports and Case Series. J. Acad. Nutr. Diet. 2021, 121, 467–492. [Google Scholar] [CrossRef]
- Krom, H.; van Oers, H.A.; van der Sluijs Veer, L.; van Zundert, S.; Otten, M.; Haverman, L.; Benninga, M.A.; Kindermann, A. Health-Related Quality of Life and Distress of Parents of Children with Avoidant Restrictive Food Intake Disorder. J. Pediatric Gastroenterol. Nutr. 2021, 73, 115–124. [Google Scholar] [CrossRef] [PubMed]
- Kennedy, G.A.; Wick, M.R.; Keel, P.K. Eating disorders in children: Is avoidant-restrictive food intake disorder a feeding disorder or an eating disorder and what are the implications for treatment? F1000Research 2018, 7, 88. [Google Scholar] [CrossRef] [PubMed]

| Assessment Tool | Authors | Sample | Symptoms | Reliability |
|---|---|---|---|---|
| Eating Disorder Assessment for DSM-5 (EDA-5) | Sysko et al., 2015 [10] | Adults | Pica, RD ARFID (all presentations) | κ = 0.87 |
| Pica, ARFID, and Rumination Disorder Interview (PARDI) | Bryant-Waugh et al., 2018, 2019 | 2 years—adult | Pica, RD ARFID (all presentations) | α (for subscales) = 0.77 to 0.89 |
| Eating Disturbances in Youth-Questionnaire (EDY-Q) | Hilbert & van Dyck, 2016 | 8–13 years | Pica, RD ARFID (all presentations) | α = 0.62 |
| Nine-item ARFID Screen (NIAS) | Zickgraf & Ellis, 2018 | Adults | ARFID (all presentations) | α = 0.79 |
| English Version of the NIAS-PR | Polish Version of the NIA-PR | |
|---|---|---|
| 1 | My child is a picky eater | Moje dziecko jest wybredne |
| 2 | My child doesn’t like many of the foods that other kids his or her age eat easily | Moje dziecko nie lubi większości potraw, które jedzą jego rówieśnicy |
| 3 | My child refuses to eat everything but a short list of preferred foods | Lista produktów, które lubi i zjada moje dziecko jest krótsza, niż lista produktów, których nie zjada |
| 4 | My child does not appear very interested in eating; s/he has a smaller appetite than other kids the same age | Moje dziecko nie jest bardzo zainteresowane jedzeniem; Wydaje mi się, że ma mniejszy apetyt niż jego rówieśnicy |
| 5 | Left to his/her own devices, my child would not eat a large enough volume of food | Pozostawione samemu sobie, moje dziecko nie zjadłoby wystarczająco dużej ilości jedzenia |
| 6 | It is difficult to get my child to eat a large enough volume, even when I offer foods that s/he really likes | Pozostawione samemu sobie, moje dziecko nie zjadłoby wystarczająco dużej ilości jedzenia |
| 7 | My child refuses to eat because s/he is afraid of discomfort, choking, or vomiting | Moje dziecko unika jedzenia, ponieważ boi się dyskomfortu w żołądku, duszenia się lub wymiotów |
| 8 | My child restricts him/herself to certain foods because s/he is afraid that other foods will cause discomfort, choking, or vomiting | Mojemu dziecku trudno jest jeść wystarczająco dużą objętość pokarmu, nawet gdy oferuję mu produkty, które naprawdę lubi |
| 9 | My child does not eat enough food because s/he is afraid of discomfort, choking, or vomiting | Moje dziecko nie je wystarczającej ilości jedzenia, ponieważ boi się dyskomfortu, zadławienia lub wymiotów |
| Polish Version of the ARFID-Q-PR | English Version of the ARFID-Q-PR | |
|---|---|---|
| 1 | Moje dziecko nie jest zainteresowane jedzeniem | My child is not interested in eating |
| 2 | Moje dziecko nie je niektórych potraw, bo jego zdaniem wydają nieprzyjemne dźwięki podczas gryzienia | My child does not eat certain foods because he thinks they make unpleasant noises when biting |
| 3 | Moje dziecko ma problemy jelitowe (np. zaparcia, biegunki, itp.) | My child has intestinal problems (e.g., constipation, diarrhea, etc.) |
| 4 | Inne osoby (np. rodzina, wychowawca w przedszkolu) pilnują, aby moje dziecko w ogóle jadło | Other people (e.g., family, kindergarten teacher) make sure that my child eats at all |
| 5 | Moje dziecko nie je niektórych potraw, bo jego zdaniem brzydko pachną | My child does not eat some foods because he thinks they smell bad |
| 6 | Moje dziecko ma problemy gastryczne (np. bóle żołądka, kolki, wzdęcia) | My child has gastric problems (e.g., stomach pain, colic, flatulence) |
| 7 | Moje dziecko je, o ile porcje są małe | My child eats if the portions are small |
| 8 | Moje dziecko nie je niektórych potraw, bo jego zdaniem mają nieprzyjemną konsystencję/fakturę | My child does not eat some dishes because he thinks they have an unpleasant consistency/texture |
| 9 | Moje dziecko szybko się męczy | My child gets tired quickly |
| 10 | Moje dziecko twierdzi, że nie czuje głodu/nie jest głodne | My child says he is not hungry |
| 11 | Moje dziecko zapada na infekcje (przeziębienie, katar itp.) | My child has infections (colds, runny nose, etc.) |
| 12 | Moje dziecko wypluwa jedzenie | My child spits out food |
| 13 | Moje dziecko unika sytuacji związanych z jedzeniem | My child avoids eating situations |
| 14 | Moje dziecko jest senne/słabe/bez energii | My child is sleepy/weak/without energy |
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. ARFID-Q-PR Attitude to food | - | |||||||||||
| 2. ARFID-Q-PR Justification for restriction | 0.58 *** | - | ||||||||||
| 3. ARFID-Q-PR Somatic condition | −0.26 ** | −0.28 *** | - | |||||||||
| 4. ARFID-Q-PR Total | 0.81 *** | 0.77 *** | 0.17 * | - | ||||||||
| 5. NIAS-PR Selective eating | 0.61 *** | 0.58 *** | −0.18 * | 0.61 *** | - | |||||||
| 6. NIAS-PR Poor appetite | 0.64 *** | 0.56 *** | −0.20 * | 0.60 *** | 0.67 *** | - | ||||||
| 7. NIAS-PR Fear of negative consequences from eating | 0.28 *** | 0.25 ** | −0.37 *** | 0.13 | 0.13 | 0.37 *** | - | |||||
| 8. NIAS-PR Total | 0.68 *** | 0.62 *** | −0.30 *** | 0.61 *** | 0.84 *** | 0.90 *** | 0.55 *** | - | ||||
| 9. Age | −0.12 | 0.15 | −0.13 | −0.05 | <0.01 | 0.10 | 0.13 | 0.09 | - | |||
| 10. Gender | −0.17 * | −0.04 | 0.16 * | −0.05 | −0.09 | −0.04 | −0.03 | −0.07 | 0.19 * | - | ||
| 11. Chronic diseases | −0.01 | 0.05 | −0.11 | −0.03 | 0.14 | −0.03 | 0.19 * | 0.12 | 0.17 * | −0.06 | - | |
| 12. BMI | −0.10 | −0.08 | −0.07 | −0.14 | −0.07 | <0.01 | 0.07 | −0.01 | 0.15 | 0.08 | 0.09 | - |
| M. | 9.75 | 8.51 | 5.56 | 23.83 | 6.01 | 4.17 | 1.20 | 11.38 | 5.77 | - | - | 15.83 |
| SD | 3.63 | 3.11 | 2.81 | 5.72 | 4.19 | 3.73 | 2.70 | 8.40 | 2.47 | - | - | 2.26 |
| Item | Factor 1: Attitude to Food | Factor 2: Justification Restrictions | Factor 3: Fitness Somatic |
|---|---|---|---|
| 1. My child is not interested in eating | 0.65 | −0.07 | 0.19 |
| 2. My child does not eat certain foods because he/she thinks they make unpleasant noises when biting | 0.00 | 0.32 | 0.52 |
| 3. My child has intestinal problems (e.g., constipation, diarrhea, etc.) | 0.24 | 0.64 | 0.00 |
| 4. Other people (e.g., family, kindergarten teacher) make sure that my child eats at all) | 0.70 | 0.16 | 0.26 |
| 5. My child does not eat some dishes because he/she thinks they smell bad | 0.27 | 0.22 | 0.72 |
| 8. My child does not eat some dishes because he/she thinks they have an unpleasant consistency/texture | 0.24 | 0.16 | 0.80 |
| 9. My child gets tired quickly | 0.00 | 0.57 | 0.27 |
| 10. My child says he or she is not hungry/hungry | 0.52 | 0.05 | 0.45 |
| 11. My child has infections (cold, runny nose, etc.) | 0.37 | 0.44 | −0.09 |
| 12. My child spits out food | 0.60 | 0.40 | −0.03 |
| 13. My child avoids eating situations | 0.76 | 0.23 | 0.19 |
| 14. My child is sleepy/weak/without energy | 0.14 | 0.66 | 0.27 |
| 6. My child has gastric problems (e.g., stomach pain, colic, flatulence) | −0.03 | 0.71 | 0.25 |
| 7. My child eats as long as the portions are small | 0.51 | −0.01 | 0.54 |
| Out condition | 20.72 | 20.30 | 20.28 |
| Participation | 0.19 | 0.16 | 0.16 |
| Item | Factor 1 Selective Eating | Factor 2 Poor Appetite | Factor 3 Fear of Negative Consequences from Eating |
|---|---|---|---|
| 0.83 | −0.04 | 0.28 |
| 0.84 | 0.04 | 0.18 |
| 0.77 | 0.14 | 0.39 |
| 0.48 | 0.22 | 0.73 |
| 0.41 | 0.24 | 0.76 |
| 0.16 | 0.18 | 0.90 |
| 0.05 | 0.98 | 0.14 |
| 0.04 | 0.99 | 0.14 |
| 0.04 | 0.99 | 0.14 |
| Out condition | 2.44 | 3.07 | 2.25 |
| Participation | 0.27 | 0.34 | 0.25 |
| Factor | Item | Correlation | Alpha When Removed |
|---|---|---|---|
| Attitude to food Cronbach’s alpha = 0.76 | 1. My child is not interested in eating | 0.46 | 0.74 |
| 4. Other people (e.g., family, kindergarten teacher) make sure that my child eats at all | 0.58 | 0.69 | |
| 10. My child says he or she is not hungry/hungry | 0.48 | 0.73 | |
| 12. My child spits out food | 0.45 | 0.74 | |
| 13. My child avoids eating situations | 0.71 | 0.66 | |
| Justification for the restriction Cronbach’s alpha = 0.73 | 2. My child does not eat certain foods because he/she thinks they make unpleasant noises when biting | 0.34 | 0.77 |
| 5. My child does not eat some dishes because he/she thinks they smell bad | 0.64 | 0.61 | |
| 8. My child does not eat some dishes because he/she thinks they have an unpleasant consistency/texture | 0.70 | 0.57 | |
| 7. My child eats as long as the portions are small | 0.46 | 0.72 | |
| Somatic condition Cronbach’s alpha = 0.67 | 3. My child has bowel problems (e.g., constipation, diarrhea, etc.) | 0.42 | 0.60 |
| 6. My child has gastric problems (e.g., stomach pain, colic, flatulence) | 0.48 | 0.57 | |
| 9. My child gets tired quickly | 0.39 | 0.62 | |
| 11. My child has infections (cold, runny nose, etc.) | 0.30 | 0.66 | |
| 14. My child is sleepy/weak/without energy | 0.52 | 0.57 |
| Factor | Item | Correlation |
|---|---|---|
| Selective eating Cronbach’s alpha = 0.84 | 1. My child is a picky eater | 0.84 |
| 2. My child doesn’t like many of the foods that other kids his or her age eat easily | 0.85 | |
| 3. My child refuses to eat everything but a short list of preferred foods | 0.78 | |
| Poor appetite Cronbach’s alpha = 0.88… | 4. My child does not appear very interested in eating; s/he has a smaller appetite than other kids the same age | 0.72 |
| 5. Left to his/her own devices, my child would not eat a large enough volume of food | 0.76 | |
| 6. It is difficult to get my child to eat a large enough volume, even when I offer foods that’s/he really likes | 0.90 | |
| Fear of negative consequences from eating Cronbach’s alpha = 0.99… | 7. My child refuses to eat because s/he is afraid of discomfort, choking, or vomiting | 0.98 |
| 8. My child restricts him/herself to certain foods because s/he is afraid that other foods will cause discomfort, choking, or vomiting | 0.97 | |
| 9. My child does not eat enough food because s/he is afraid of discomfort, choking, or vomiting | 0.98 |
| CMIN | p | CMIN/df | RMSEA | AGFI | TLI | CFI | |
|---|---|---|---|---|---|---|---|
| ARFID-Q-PR (three factor model) | 81.22 | 0.114 | 1.21 | 0.036 | 0.902 | 0.971 | 0.978 |
| NIAS-PR (three factor model) | 29.63 | 0.197 | 1.24 | 0.038 | 0.930 | 0.995 | 0.997 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ziółkowska, B.; Ocalewski, J.; Zickgraf, H.; Brytek-Matera, A. The Polish Version of the Avoidant/Restrictive Food Intake Disorder Questionnaire—Parents Report (ARFID-Q-PR) and the Nine Items Avoidant/Restrictive Food Intake Disorder Screen—Parents Report (NIAS-PR): Maternal Perspective. Nutrients 2022, 14, 3175. https://doi.org/10.3390/nu14153175
Ziółkowska B, Ocalewski J, Zickgraf H, Brytek-Matera A. The Polish Version of the Avoidant/Restrictive Food Intake Disorder Questionnaire—Parents Report (ARFID-Q-PR) and the Nine Items Avoidant/Restrictive Food Intake Disorder Screen—Parents Report (NIAS-PR): Maternal Perspective. Nutrients. 2022; 14(15):3175. https://doi.org/10.3390/nu14153175
Chicago/Turabian StyleZiółkowska, Beata, Jarosław Ocalewski, Hana Zickgraf, and Anna Brytek-Matera. 2022. "The Polish Version of the Avoidant/Restrictive Food Intake Disorder Questionnaire—Parents Report (ARFID-Q-PR) and the Nine Items Avoidant/Restrictive Food Intake Disorder Screen—Parents Report (NIAS-PR): Maternal Perspective" Nutrients 14, no. 15: 3175. https://doi.org/10.3390/nu14153175
APA StyleZiółkowska, B., Ocalewski, J., Zickgraf, H., & Brytek-Matera, A. (2022). The Polish Version of the Avoidant/Restrictive Food Intake Disorder Questionnaire—Parents Report (ARFID-Q-PR) and the Nine Items Avoidant/Restrictive Food Intake Disorder Screen—Parents Report (NIAS-PR): Maternal Perspective. Nutrients, 14(15), 3175. https://doi.org/10.3390/nu14153175






