The Longitudinal Association of Lifestyle with Cognitive Health and Dementia Risk: Findings from the HELIAD Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Sample and Procedures
2.2. Dietary Assessment
2.3. Physical Activity Assessment
2.4. Sleep Assessment
2.5. Assessment of Engagement in Activities of Daily Living
2.6. Neuropsychological Evaluation and Clinical Diagnoses
2.7. Total Lifestyle Index Calculation
2.8. Outcomes
2.9. Statistical Analyses
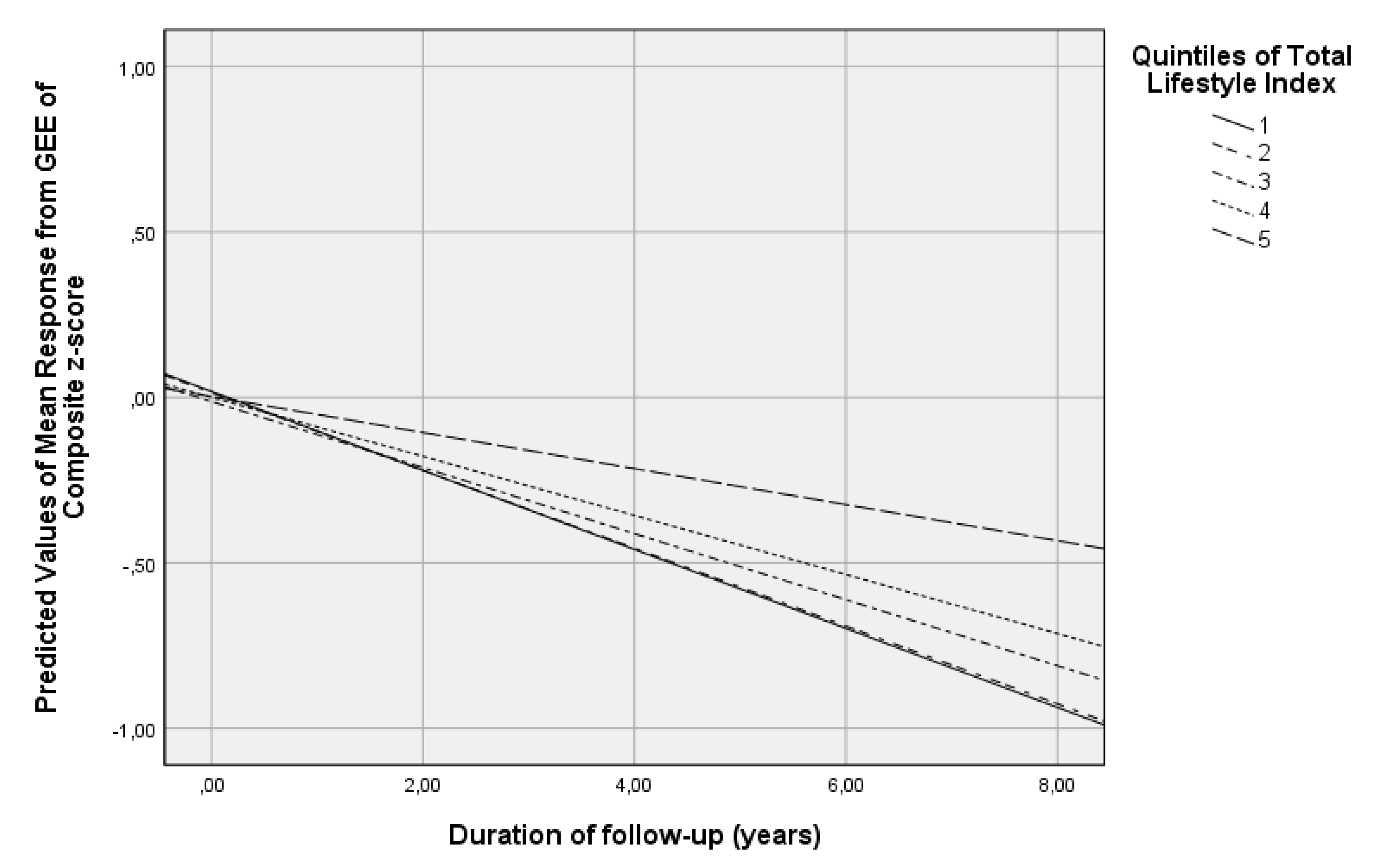
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Alzheimer’s Disease International. World Alzheimer Report 2015. 2015. Available online: https://www.alzint.org/resource/world-alzheimer-report-2015/ (accessed on 7 September 2021).
- O’Brien, J.T.; Holmes, C.; Jones, M.; Jones, R.; Livingston, G.; McKeith, I.; Mittler, P.; Passmore, P.; Ritchie, C.; Robinson, L.; et al. Clinical practice with anti-dementia drugs: A revised (third) consensus statement from the British Association for Psychopharmacology. J. Psychopharmacol. 2017, 31, 147–168. [Google Scholar] [CrossRef] [PubMed]
- Hardman, R.J.; Kennedy, G.; Macpherson, H.; Scholey, A.B.; Pipingas, A. Adherence to a Mediterranean-Style Diet and Effects on Cognition in Adults: A Qualitative Evaluation and Systematic Review of Longitudinal and Prospective Trials. Front. Nutr. 2016, 3, 22. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Scarmeas, N.; Anastasiou, C.A.; Yannakoulia, M. Nutrition and prevention of cognitive impairment. Lancet. Neurol. 2018, 17, 1006–1015. [Google Scholar] [CrossRef]
- Pace-Schott, E.F.; Spencer, R.M. Age-related changes in the cognitive function of sleep. Prog. Brain Res. 2011, 191, 75–89. [Google Scholar] [CrossRef] [PubMed]
- Angevaren, M.; Aufdemkampe, G.; Verhaar, H.J.; Aleman, A.; Vanhees, L. Physical activity and enhanced fitness to improve cognitive function in older people without known cognitive impairment. Cochrane Database Syst. Rev. 2008, 3, CD005381. [Google Scholar] [CrossRef]
- Hamer, M.; Chida, Y. Physical activity and risk of neurodegenerative disease: A systematic review of prospective evidence. Psychol. Med. 2009, 39, 3–11. [Google Scholar] [CrossRef]
- Sofi, F.; Valecchi, D.; Bacci, D.; Abbate, R.; Gensini, G.F.; Casini, A.; Macchi, C. Physical activity and risk of cognitive decline: A meta-analysis of prospective studies. J. Intern. Med. 2011, 269, 107–117. [Google Scholar] [CrossRef]
- Scarmeas, N.; Luchsinger, J.A.; Schupf, N.; Brickman, A.M.; Cosentino, S.; Tang, M.X.; Stern, Y. Physical Activity, Diet, and Risk of Alzheimer Disease. JAMA J. Am. Med. Assoc. 2009, 302, 627–637. [Google Scholar] [CrossRef] [Green Version]
- Anastasiou, C.A.; Yannakoulia, M.; Kontogianni, M.D.; Kosmidis, M.H.; Mamalaki, E.; Dardiotis, E.; Hadjigeorgiou, G.; Sakka, P.; Tsapanou, A.; Lykou, A.; et al. Mediterranean Lifestyle in Relation to Cognitive Health: Results from the HELIAD Study. Nutrients 2018, 10, 1557. [Google Scholar] [CrossRef] [Green Version]
- Dhana, K.; Evans, D.A.; Rajan, K.B.; Bennett, D.A.; Morris, M.C. Healthy lifestyle and the risk of Alzheimer dementia: Findings from 2 longitudinal studies. Neurology 2020, 95, e374–e383. [Google Scholar] [CrossRef]
- Lourida, I.; Hannon, E.; Littlejohns, T.J.; Langa, K.M.; Hyppönen, E.; Kuzma, E.; Llewellyn, D.J. Association of Lifestyle and Genetic Risk With Incidence of Dementia. Jama 2019, 322, 430–437. [Google Scholar] [CrossRef] [PubMed]
- Weng, P.H.; Chen, J.H.; Chiou, J.M.; Tu, Y.K.; Chen, T.F.; Chiu, M.J.; Tang, S.C.; Yeh, S.J.; Chen, Y.C. The effect of lifestyle on late-life cognitive change under different socioeconomic status. PLoS ONE 2018, 13, e0197676. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ngandu, T.; Lehtisalo, J.; Solomon, A.; Levalahti, E.; Ahtiluoto, S.; Antikainen, R.; Backman, L.; Hanninen, T.; Jula, A.; Laatikainen, T.; et al. A 2 year multidomain intervention of diet, exercise, cognitive training, and vascular risk monitoring versus control to prevent cognitive decline in at-risk elderly people (FINGER): A randomised controlled trial. Lancet 2015, 385, 2255–2263. [Google Scholar] [CrossRef]
- Lee, K.S.; Lee, Y.; Back, J.H.; Son, S.J.; Choi, S.H.; Chung, Y.K.; Lim, K.Y.; Noh, J.S.; Koh, S.H.; Oh, B.H.; et al. Effects of a multidomain lifestyle modification on cognitive function in older adults: An eighteen-month community-based cluster randomized controlled trial. Psychother. Psychosom. 2014, 83, 270–278. [Google Scholar] [CrossRef]
- Andrieu, S.; Guyonnet, S.; Coley, N.; Cantet, C.; Bonnefoy, M.; Bordes, S.; Bories, L.; Cufi, M.N.; Dantoine, T.; Dartigues, J.F.; et al. Effect of long-term omega 3 polyunsaturated fatty acid supplementation with or without multidomain intervention on cognitive function in elderly adults with memory complaints (MAPT): A randomised, placebo-controlled trial. Lancet Neurol. 2017, 16, 377–389. [Google Scholar] [CrossRef] [PubMed]
- Moll van Charante, E.P.; Richard, E.; Eurelings, L.S.; van Dalen, J.-W.; Ligthart, S.A.; van Bussel, E.F.; Hoevenaar-Blom, M.P.; Vermeulen, M.; van Gool, W.A. Effectiveness of a 6-year multidomain vascular care intervention to prevent dementia (preDIVA): A cluster-randomised controlled trial. Lancet 2016, 388, 797–805. [Google Scholar] [CrossRef] [Green Version]
- Elwood, P.; Galante, J.; Pickering, J.; Palmer, S.; Bayer, A.; Ben-Shlomo, Y.; Longley, M.; Gallacher, J. Healthy lifestyles reduce the incidence of chronic diseases and dementia: Evidence from the Caerphilly cohort study. PLoS ONE 2013, 8, e81877. [Google Scholar] [CrossRef]
- Anastasiou, C.A.; Yannakoulia, M.; Kosmidis, M.H.; Dardiotis, E.; Hadjigeorgiou, G.M.; Sakka, P.; Arampatzi, X.; Bougea, A.; Labropoulos, I.; Scarmeas, N. Mediterranean diet and cognitive health: Initial results from the Hellenic Longitudinal Investigation of Ageing and Diet. PLoS ONE 2017, 12, e0182048. [Google Scholar] [CrossRef] [Green Version]
- Mamalaki, E.; Anastasiou, C.A.; Ntanasi, E.; Tsapanou, A.; Kosmidis, M.H.; Dardiotis, E.; Hadjigeorgiou, G.M.; Sakka, P.; Scarmeas, N.; Yannakoulia, M. Associations between the mediterranean diet and sleep in older adults: Results from the hellenic longitudinal investigation of aging and diet study. Geriatr. Gerontol. Int. 2018, 18, 1543–1548. [Google Scholar] [CrossRef] [Green Version]
- Ntanasi, E.; Yannakoulia, M.; Kosmidis, M.H.; Anastasiou, C.A.; Dardiotis, E.; Hadjigeorgiou, G.; Sakka, P.; Scarmeas, N. Adherence to Mediterranean Diet and Frailty. J. Am. Med. Dir. Assoc. 2018, 19, 315–322.e2. [Google Scholar] [CrossRef]
- Bountziouka, V.; Bathrellou, E.; Giotopoulou, A.; Katsagoni, C.; Bonou, M.; Vallianou, N.; Barbetseas, J.; Avgerinos, P.C.; Panagiotakos, D.B. Development, repeatability and validity regarding energy and macronutrient intake of a semi-quantitative food frequency questionnaire: Methodological considerations. Nutr. Metab. Cardiovasc. Dis. NMCD 2012, 22, 659–667. [Google Scholar] [CrossRef] [PubMed]
- Panagiotakos, D.B.; Pitsavos, C.; Stefanadis, C. Dietary patterns: A Mediterranean diet score and its relation to clinical and biological markers of cardiovascular disease risk. Nutr. Metab. Cardiovasc. Dis. 2006, 16, 559–568. [Google Scholar] [CrossRef] [PubMed]
- Kavouras, S.A.; Maraki, M.I.; Kollia, M.; Gioxari, A.; Jansen, L.T.; Sidossis, L.S. Development, reliability and validity of a physical activity questionnaire for estimating energy expenditure in Greek adults. Sci. Sports 2016, 31, e47–e53. [Google Scholar] [CrossRef]
- Spritzer, K.L.; Hays, R.D. MOS Sleep Scale: A Manual for Use and Scoring, Version 1.0; RAND Corporation: Los Angeles, CA, USA, 2003. [Google Scholar]
- Fieo, R.; Manly, J.J.; Schupf, N.; Stern, Y. Functional status in the young-old: Establishing a working prototype of an extended-instrumental activities of daily living scale. J. Gerontol. A Biol. Sci. Med. Sci. 2014, 69, 766–772. [Google Scholar] [CrossRef] [Green Version]
- Folstein, M.F.; Folstein, S.E.; McHugh, P.R. “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J. Psychiatr. Res. 1975, 12, 189–198. [Google Scholar] [CrossRef]
- Vlahou, C.H.; Kosmidis, M.H.; Dardagani, A.; Tsotsi, S.; Giannakou, M.; Giazkoulidou, A.; Zervoudakis, E.; Pontikakis, N. Development of the Greek Verbal Learning Test: Reliability, construct validity, and normative standards. Arch. Clin. Neuropsychol. 2013, 28, 52–64. [Google Scholar] [CrossRef] [Green Version]
- Lezak, M.D. Neuropsychological Assessment; Oxford University Press: New York, NY, USA, 2004. [Google Scholar]
- Kosmidis, M.H.; Vlahou, C.H.; Panagiotaki, P.; Kiosseoglou, G. The verbal fluency task in the Greek population: Normative data, and clustering and switching strategies. J. Int. Neuropsychol. Soc. 2004, 10, 164–172. [Google Scholar] [CrossRef]
- Tsapkini, K.; Vlahou, C.H.; Potagas, C. Adaptation and validation of standardized aphasia tests in different languages: Lessons from the Boston Diagnostic Aphasia Examination—Short Form in Greek. Behav. Neurol. 2010, 22, 111–119. [Google Scholar] [CrossRef]
- Vlahou, C.H.; Kosmidis, M.H. The Greek Trail Making Test: Preliminary norms for clinical and research use. Psychol. J. Hell. Psychol. Soc. 2002, 9, 336–352. [Google Scholar]
- Kosmidis, M.H.; Tsotsi, S.; Karambela, O.; Takou, E.; Vlahou, C.H. Cultural factors influencing performance on visuoperceptual neuropsychological tasks. Behav. Neurol. 2010, 23, 245–247. [Google Scholar] [CrossRef]
- Bozikas, V.P.; Giazkoulidou, A.; Hatzigeorgiadou, M.; Karavatos, A.; Kosmidis, M.H. Do age and education contribute to performance on the clock drawing test? Normative data for the Greek population. J. Clin. Exp. Neuropsychol. 2008, 30, 199–203. [Google Scholar] [CrossRef]
- Guze, S.B. Diagnostic and Statistical Manual of Mental Disorders, 4th ed. (DSM-IV). Am. J. Psychiatry 1995, 152, 1228. [Google Scholar] [CrossRef]
- McKhann, G.; Drachman, D.; Folstein, M.; Katzman, R.; Price, D.; Stadlan, E.M. Clinical diagnosis of Alzheimer’s disease: Report of the NINCDS-ADRDA Work Group under the auspices of Department of Health and Human Services Task Force on Alzheimer’s Disease. Neurology 1984, 34, 939–944. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Harrell, F.E. Regression Modeling Strategies: With Applications to Linear Models, Logistic Regression, and Survival Analysis; Springer: New York, NY, USA, 2001. [Google Scholar]
- Mamalaki, E.; Poulimeneas, D.; Kosmidis, M.H.; Yannakoulia, M. Mediterranean lifestyle patterns are associated with cognition in older adults. Lifestyle Med. 2021, 2, e30. [Google Scholar] [CrossRef]
- Charisis, S.; Ntanasi, E.; Yannakoulia, M.; Anastasiou, C.A.; Kosmidis, M.H.; Dardiotis, E.; Hadjigeorgiou, G.; Sakka, P.; Scarmeas, N. Mediterranean diet and risk for dementia and cognitive decline in a Mediterranean population. J. Am. Geriatr. Soc. 2021, 69, 1548–1559. [Google Scholar] [CrossRef]
- Petersson, S.D.; Philippou, E. Mediterranean Diet, Cognitive Function, and Dementia: A Systematic Review of the Evidence. Adv. Nutr. 2016, 7, 889–904. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Demurtas, J.; Schoene, D.; Torbahn, G.; Marengoni, A.; Grande, G.; Zou, L.; Petrovic, M.; Maggi, S.; Cesari, M.; Lamb, S.; et al. Physical Activity and Exercise in Mild Cognitive Impairment and Dementia: An Umbrella Review of Intervention and Observational Studies. J. Am. Med. Dir. Assoc. 2020, 21, 1415–1422.e6. [Google Scholar] [CrossRef] [PubMed]
- Jia, R.X.; Liang, J.H.; Xu, Y.; Wang, Y.Q. Effects of physical activity and exercise on the cognitive function of patients with Alzheimer disease: A meta-analysis. BMC Geriatr. 2019, 19, 181. [Google Scholar] [CrossRef]
- Ma, Y.; Liang, L.; Zheng, F.; Shi, L.; Zhong, B.; Xie, W. Association between Sleep Duration and Cognitive Decline. JAMA Netw. Open 2020, 3, e2013573. [Google Scholar] [CrossRef]
- Lindbergh, C.A.; Dishman, R.K.; Miller, L.S. Functional Disability in Mild Cognitive Impairment: A Systematic Review and Meta-Analysis. Neuropsychol. Rev. 2016, 26, 129–159. [Google Scholar] [CrossRef]
- Cummings, J.L. Alzheimer’s disease. N. Engl. J. Med. 2004, 351, 56–67. [Google Scholar] [CrossRef] [PubMed]
- Steele, M.; Stuchbury, G.; Munch, G. The molecular basis of the prevention of Alzheimer’s disease through healthy nutrition. Exp. Gerontol. 2007, 42, 28–36. [Google Scholar] [CrossRef] [PubMed]
- Ju, Y.E.; Lucey, B.P.; Holtzman, D.M. Sleep and Alzheimer disease pathology—A bidirectional relationship. Nat. Reviews. Neurol. 2014, 10, 115–119. [Google Scholar] [CrossRef] [PubMed]
- Kennedy, G.; Hardman, R.J.; Macpherson, H.; Scholey, A.B.; Pipingas, A. How Does Exercise Reduce the Rate of Age-Associated Cognitive Decline? A Review of Potential Mechanisms. J. Alzheimer’s Dis. JAD 2017, 55, 1–18. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fitzgerald, K.N.; Hodges, R.; Hanes, D.; Stack, E.; Cheishvili, D.; Szyf, M.; Henkel, J.; Twedt, M.W.; Giannopoulou, D.; Herdell, J.; et al. Potential reversal of epigenetic age using a diet and lifestyle intervention: A pilot randomized clinical trial. Aging 2021, 13, 9419–9432. [Google Scholar] [CrossRef] [PubMed]
- Gure, T.R.; Kabeto, M.U.; Plassman, B.L.; Piette, J.D.; Langa, K.M. Differences in functional impairment across subtypes of dementia. J. Gerontol. Ser. A Biol. Sci. Med. Sci. 2010, 65, 434–441. [Google Scholar] [CrossRef] [Green Version]
| All Participants n = 1018 | Participants with Normal Cognition at Follow Up n = 957 | Participants with Dementia at Follow-Up n = 61 | p-Value * | |
|---|---|---|---|---|
| Age (years) | 73.1 ± 5.0 | 72.7 ± 4.9 | 77.4 ± 4.7 | <0.001 |
| Sex (% women) | 59.7 | 59.9 | 57.1 | 0.692 |
| Education (years) | 8.2 ± 4.9 | 8.3 ± 4.9 | 6.0 ± 4.8 * | <0.001 |
| Duration of follow-up (years) | 3.0 ± 0.8 | 3.0 ± 0.9 | 3.0 ± 0.8 | 0.975 |
| MedDietScore (0–55) | 33.6 ± 4.5 | 33.7 ± 4.6 | 32.1 ± 3.5 | 0.011 |
| Physical Activity (/ 200 MET-min/day) | 7.5 ± 1.4 | 7.6 ± 1.4 | 7.0 ± 1.2 | 0.002 |
| Sleep Duration (hours) | 6.5 ± 1.4 | 6.5 ± 1.4 | 6.7 ± 2.0 | 0.501 |
| Engagement in activities of daily living (0–9) | 4.6 ± 1.3 | 4.7 ± 1.2 | 3.8 ± 1.4 | <0.001 |
| Total Lifestyle Index (0–12) | 6.0 ± 4.4 | 6.2 ± 4.4 | 2.9 ± 3.8 | <0.001 |
| Total Lifestyle Index as a Continuous Variable | Total Lifestyle Index as Quintiles | |||||
|---|---|---|---|---|---|---|
| β (95% CI) | p | Quartiles | β (95%CI) | p | p for Trend | |
| Global Cognition score | 0.005 (0.003–0.007) | <0.001 | 1st (ref) | <0.001 | ||
| 2nd | −0.002 (−0.0034–0.029) | 0.881 | ||||
| 3rd | −0.002 (−0.0040–0.036) | 0.917 | ||||
| 4th | 0.017 (−0.015–0.048) | 0.301 | ||||
| 5th | 0.058 (0.032–0.084) | <0.001 | ||||
| Total Lifestyle Index as a Continuous Variable | Total Lifestyle Index as Quintiles | |||||
|---|---|---|---|---|---|---|
| RR (95% CI) | p | Quartiles | RR (95% CI) | p | p for Trend | |
| Dementia incidence | 0.998 (0.997–0.999) | <0.001 | 1st (ref) | <0.001 | ||
| 2nd | 0.974 (0.956–0.992) | 0.004 | ||||
| 3rd | 0.965 (0.948–0.982) | <0.001 | ||||
| 4th | 0.981 (0.962–1.000) | 0.049 | ||||
| 5th | 0.963 (0.949–0.978) | <0.001 | ||||
| Adherence to the Mediterranean Diet | Sleep Duration | Physical Activity | Engagement in Activities of Daily Living | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Quartiles | β (95% CI) | p | p for Trend | Quartiles | β (95% CI) | p | p for Trend | Quartiles | β (95% CI) | p | p for Trend | Quartiles | β (95% CI) | p | p for Trend | |
| Global Cognition score | 1st (ref) | <0.001 | 1st (ref) | <0.001 | 1st (ref) | <0.001 | 1st (ref) | <0.001 | ||||||||
| 2nd | −0.010 (−0.040–0.021) | 0.534 | 2nd | −0.005 (−0.035–0.025) | 0.739 | 2nd | −0.002 (−0.032–0.028) | 0.917 | 2nd | 0.009 (−0.021–0.039) | 0.576 | |||||
| 3rd | 0.018 (−0.010–0.047) | 0.208 | 3rd | 0.015 (−0.014–0.044) | 0.313 | 3rd | 0.012 (−0.017–0.042) | 0.409 | 3rd | 0.018 (−0.012–0.047) | 0.238 | |||||
| 4th | 0.054 (0.030–0.078) | <0.001 | 4th | 0.055 (0.031–0.079) | <0.001 | 4th | 0.057 (0.032–0.081) | <0.001 | 4th | 0.059 (0.035–0.084) | <0.001 | |||||
| Adherence to the Mediterranean Diet | Sleep Duration | Physical Activity | Engagement in Activities of Daily Living | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Quartiles | RR (95%CI) | p | p for Trend | Quartiles | RR (95% CI) | p | p for Trend | Quartiles | RR (95% CI) | p | p for Trend | Quartiles | RR (95% CI) | p | p for Trend | |
| Dementia incidence | 1st (ref) | <0.001 | 1st (ref) | <0.001 | 1st (ref) | <0.001 | 1st (ref) | <0.001 | ||||||||
| 2nd | 0.977 (0.961–0.994) | 0.007 | 2nd | 0.975 (0.958–0.992) | 0.004 | 2nd | 0.974 (0.957–0.991) | 0.003 | 2nd | 0.977 (0.960–0.994) | 0.007 | |||||
| 3rd | 0.984 (0.967–1.001) | 0.065 | 3rd | 0.980 (0.963–0.997) | 0.025 | 3rd | 0.979 (0.962–0.997) | 0.021 | 3rd | 0.981 (0.964–0.998) | 0.031 | |||||
| 4th | 0.968 (0.955–0.982) | <0.001 | 4th | 0.966 (0.952–0.980) | <0.001 | 4th | 0.965 (0.952–0.980) | <0.001 | 4th | 0.967 (0.954–0.981) | <0.001 | |||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mamalaki, E.; Charisis, S.; Anastasiou, C.A.; Ntanasi, E.; Georgiadi, K.; Balomenos, V.; Kosmidis, M.H.; Dardiotis, E.; Hadjigeorgiou, G.; Sakka, P.; et al. The Longitudinal Association of Lifestyle with Cognitive Health and Dementia Risk: Findings from the HELIAD Study. Nutrients 2022, 14, 2818. https://doi.org/10.3390/nu14142818
Mamalaki E, Charisis S, Anastasiou CA, Ntanasi E, Georgiadi K, Balomenos V, Kosmidis MH, Dardiotis E, Hadjigeorgiou G, Sakka P, et al. The Longitudinal Association of Lifestyle with Cognitive Health and Dementia Risk: Findings from the HELIAD Study. Nutrients. 2022; 14(14):2818. https://doi.org/10.3390/nu14142818
Chicago/Turabian StyleMamalaki, Eirini, Sokratis Charisis, Costas A. Anastasiou, Eva Ntanasi, Kyriaki Georgiadi, Vassilis Balomenos, Mary H. Kosmidis, Efthimios Dardiotis, Georgios Hadjigeorgiou, Paraskevi Sakka, and et al. 2022. "The Longitudinal Association of Lifestyle with Cognitive Health and Dementia Risk: Findings from the HELIAD Study" Nutrients 14, no. 14: 2818. https://doi.org/10.3390/nu14142818
APA StyleMamalaki, E., Charisis, S., Anastasiou, C. A., Ntanasi, E., Georgiadi, K., Balomenos, V., Kosmidis, M. H., Dardiotis, E., Hadjigeorgiou, G., Sakka, P., Scarmeas, N., & Yannakoulia, M. (2022). The Longitudinal Association of Lifestyle with Cognitive Health and Dementia Risk: Findings from the HELIAD Study. Nutrients, 14(14), 2818. https://doi.org/10.3390/nu14142818







