The Current Findings on the Impact of Prenatal BPA Exposure on Metabolic Parameters: In Vivo and Epidemiological Evidence
Abstract
:1. Introduction
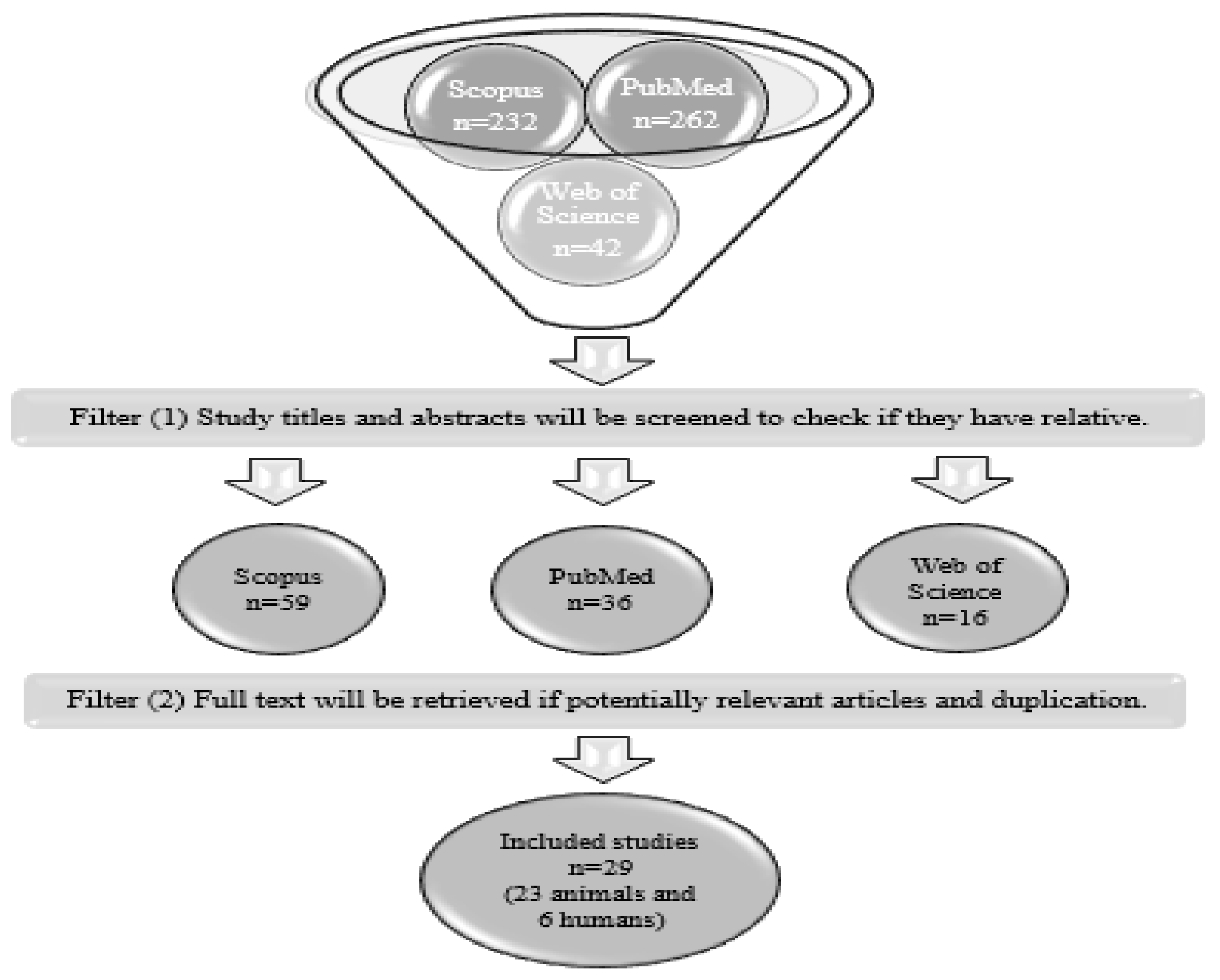
2. Search Strategy
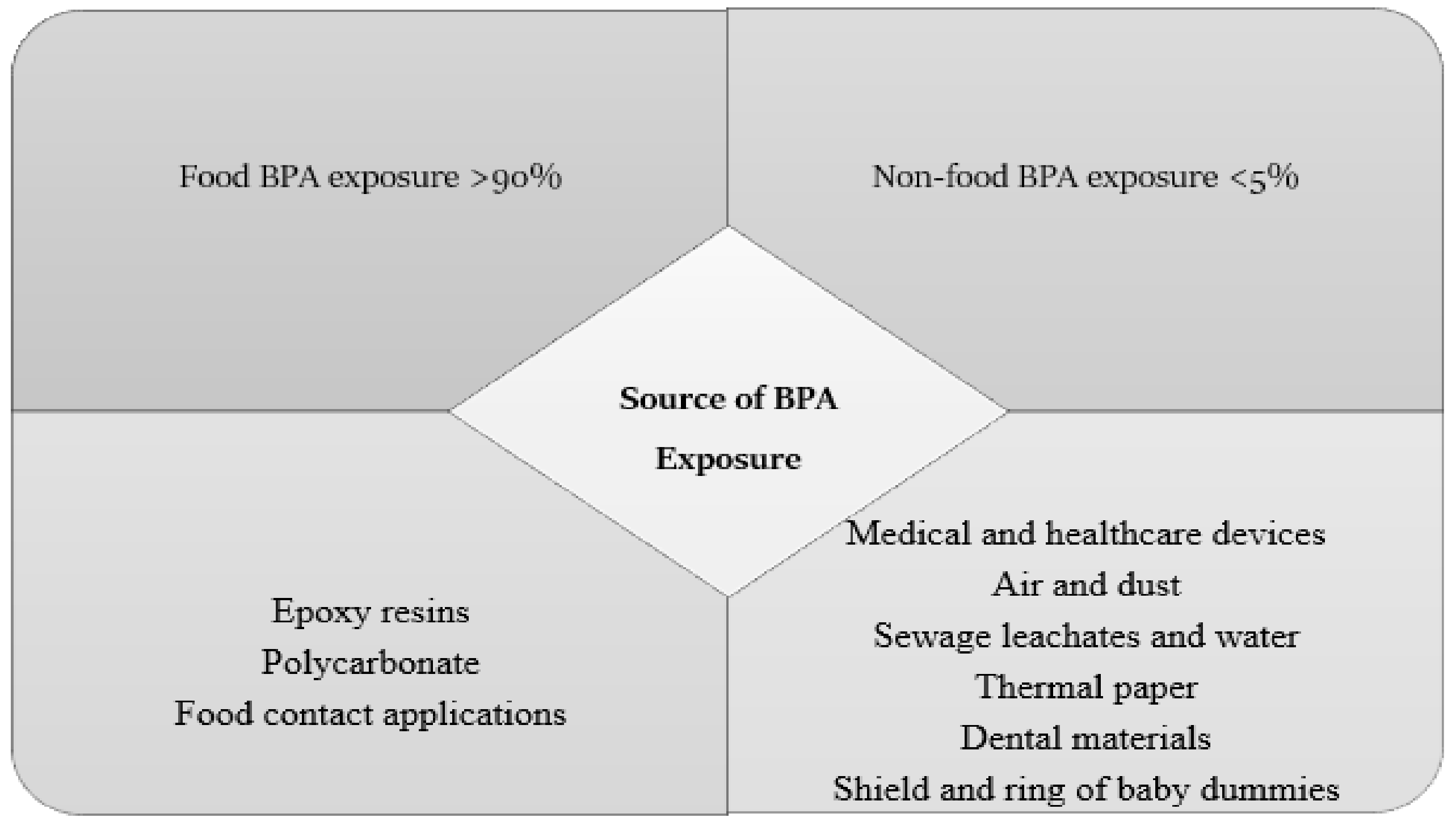
3. Sources of BPA Exposure and BPA Metabolism
4. Different Doses of BPA Exposure
5. The Mechanisms of Action of BPA and Its Deleterious Effects
6. Discussion
6.1. Metabolic Effect of Prenatal BPA Exposure in Animal Studies
6.1.1. High and Low Doses of Prenatal BPA Exposure and Glucose Parameters in the Animal Models
6.1.2. High and Low Doses of Developmental BPA Exposure and Lipid Parameters in the Animal Models
| Reference | Dose | Low/High Dose | Route of Exposure | Exposure Window | Strain, Species | Sex | Outcomes |
|---|---|---|---|---|---|---|---|
| [51] | 2.5 µg/kg/day | Very low | Drinking water | 30 days before mating and continued until GD 20 | SD rats | M (male) and F (female) | No effect on parameters of lipid metabolism on pregnant rats. No effect on foetus hepatic TG or TC content. |
| [43] | 1, 10, 100, and 1000 µg/kg/day | Very low, low, and high | Gavage | GD 7.5–GD 16.5 | C57BL/6J mice | M and F | In male offspring (14 weeks of age), the hepatic TG content increased significantly at 1 and 1000 µg/kg/day (very low and high doses, respectively) and liver weight increased at very low BPA dose (1 µg/kg/day). In female offspring, the hepatic TG content increased significantly at 1000 µg/kg/day (high dose). |
| [43] | 1 µg/kg/day | Very low | Gavage | GD 7.5–GD 16.5 | C57BL/6J mice | M and F | In ♂ (14 weeks) offspring, gestational exposure to low-dose BPA caused increased hepatic TG and glycogen levels and significantly elevated fasting blood glucose and insulin levels, as well as the blood glucose levels, in IPGTT and IPITT analysis. Low-dose gestational exposure to BPA did not impair glucose or lipid metabolism in adult female offspring. |
| [44] | 5 μg/kg/day | Low | Pipette | GD 19–GD 21 | C57BL/6J mice | M and F | Low gestational BPA exposure (♀) significantly increased BW (at 13, 14, 20, and 22 weeks), significantly decreased hepatic TG content, and had no effect on plasma lipid parameters, plasma insulin level, or glucose tolerance at 10 and 21 weeks. Low gestational BPA exposure (♂) significantly decreased BW (at 4 weeks), showed faster glucose clearance at 10 and 21 weeks, and significantly decreased plasma TG, FFA, UC, and VLDL, but not TC, HDL, or LDL; there was a significant increase in hepatic TC content. |
| [52] | 100 μg/kg/day | High | Gavage | GD 6–PND 21 | SD rats | M and F | High BPA did not significantly alter maternal weight gain or birth weight. ♂ BPA only increased body weight at PND 97 and energy intake (but not significant) and had no effect on body composition (fat/lean mass ratio) at birth or weaning. However, during the post-weaning to adulthood period, BPA significantly increased the fat/lean mass ratio (PND 60–90). ♂ High BPA significantly increased the amount of both hepatic TG and FFAs (PND 1). |
| [55] | 2.5, 25, or 250 µg/Kg/day | Very low, low, and high | Diet | Month virgin state plus 20 days during pregnancy | SD rats | M and F | During pregnancy, the mother’s weight in the third week of pregnancy was significantly lower in the 2.5 µg/Kg/day BPA group. Foetal weight at birth was significantly increased in rats treated with 2.5 µg/kg/day BPA. |
| [45] | 0.5 or 50 µg/Kg/day | Very low and low | Drinking water | GD 3.5–PND 22 | Fischer 344 rats | M and F | (♀, ♂) A very low BPA dose (0.5 µg BPA/kg) was correlated with insulin hypersecretion, while 50 µg BPA/kg was associated with reduced insulin secretion from both rat offspring and dams (5 and 52 weeks, respectively). |
| [56] | 0.05, 0.5, or 5 mg/Kg/day | Very low, low, and high | Subcutaneous | GD 30–90 | Sheep | F | (♀ at ∼21 months) No effect on plasma TG content for all BPA doses. Significantly increased both hepatic and muscular TG content at 0.5 and 5 mg/Kg/day doses. The plasma LMW ADP levels were significantly reduced only in the BPA high-dose (5 mg/Kg/day) group. |
| [57] | 10 μg/kg/day and 10 mg/kg/day | Low and high | Diet | 2 weeks prior to mating (preconception) until weaning | C57BL/6 mice | M and F | ♂ Low BPA doses in the male offspring were associated with lower birth weights (PND 1) and the development of obesity in adulthood (PND 98 and117). ♂ Glucose tolerance test results (GTTs) were greater in high-dose (10 mg/kg/day) BPA male offspring than in control male offspring, consistent with the phenotype of glucose intolerance (PND 98 and 117). ♂ significantly increased insulin levels in the low-dose BPA group (PND 98 and 117). ♀ and ♂ Low and high doses of BPA had no effect on fasting glucose levels. Low- and high-dose BPA-exposed male but not female offspring had impaired glucose homeostasis and developed obesity in adulthood. |
| [53] | 50 µg/kg/day | Low | Oral gavage | GD 15–PND 21 | C3H/HeN mice | M | Low doses decreased gWAT at PND 45 and increased BW (PND 70 until PND 170). However, there was no effect on food intake, and it was associated with glucose intolerance (at PND 35) and decreased insulin sensitivity (at PND 125). |
| [54] | 0.5 or 50 µg/kg/day | Very low and low | Drinking water | GD 3.5–PND 22 | F344 rats | M and F | No effect on maternal parameters, including BW, food, and water intake. Increase in plasma TG with 50 µg/kg/day (♀) at 5 weeks and slightly increased BW at 52 weeks. Increase in plasma TG at 5 weeks in ♂ with 0.5 µg/kg BW/day offspring and low BW at 52 weeks. No effect on ♂ or ♀ offspring parameters, plasma TG, cholesterol, leptin, or ADP in BPA-exposed 52-week rat offspring. 5-week-old ♂ exposed to low doses (0.5 µg/kg /day) were linked with insulin resistance. |
| [46] | 10 μg/kg/day | Low | Subcutaneous injection | GD 9–GD 16 | OF-1 mice | M | Increased fasting blood glucose and higher insulin level (28 weeks), increased hepatic TG levels, and increased BW (PND 196). Increase in perigonadal fat pad weight at 28 weeks. |
| [48] | 1 and 10 µg/mL | Low | Drinking water | GD 6–PND 21 | SD rats | M | 1 µg/mL or 10 µg/mL BPA in water had no significant effect on maternal weight gain, food intake, or water consumption during pregnancy. For ♂ PND 7–PND 100, low-dose BPA (1 and 10 µg/mL) exposure increased BW. ♂ At puberty stage, a low dose (10 µg/mL BPA) increased blood glucose and insulin and decreased serum ADP. ♂At adult stage, both low doses increased blood glucose and insulin and significantly decreased the level of serum ADP. |
| [58] | 50 μg/kg/day | Low | Oral gavage | GD 0 until weaning at 3 weeks | Wistar rats | M | At week 3, a low dose had no effect on BW or blood glucose but increased the serum insulin level. At week 21, a low dose increased BW and insulin resistance and impaired glucose tolerance in rat’s hepatic tissue. |
| [26] | 1 and 20 µg/kg diet BPA | Very low and low | Diet | Pregnant and lactating | CD-1 mice | M and F | Both low doses of BPA had no effect on maternal body weight or food intake or on the BW of 3-month-old (♂ and ♀) offspring. ♂ For adults, a low dose (20 µg/kg) impaired glucose tolerance and increased plasma insulin. However, no effect on leptin level was found. ♀ No effect on glucose tolerance and increased plasma leptin. |
| [59] | 10 or 100 µg/kg/day | Low and high | Subcutaneous | GD 9–GD 16 | OF-1 mice | M | A low BPA dose (10 µg/kg/day) displayed maternal glucose intolerance, and a high dose of BPA (100 µg/kg/day) showed a tendency to increase insulin sensitivity (but not statistically significant). Pregnant mice at GD 18 with exposure to BPA (100 µg/kg/day) showed significantly increased leptin, TG, and glycerol. At 3 months of age, for ♂ and ♀, both BPA doses had no effect on insulin resistance or glucose intolerance. At 6 months of age, male offspring exposed in utero had reduced glucose tolerance and increased insulin resistance (10 µg/kg/day). A low BPA (10µg/kg/day) dose decreased BW in the offspring. BPA (100 µg/kg/day) mice had higher levels of leptin than F0-BPA 10µg/kg/day mice. |
| [49] | 25 mg BPA/kg diet | High | Diet | GD 7.5–GD 18.5 | C57BL/6 mice | Foetus | A high dose of BPA (25 mg/kg) did not alter the expression of insulin in the foetal pancreatic islets. However, there was an increase in glucagon expression in BPA-exposed foetal pancreatic islets. |
| [60] | 100 µg/kg/day | High | Subcutaneous | GD 6–PND 0 PND 0–PND 21 GD 6–PND 21 | C57BL6 mice | M and F | No effect on birth weight. ♂ and ♀ Showed significant decreases in the body weight of pups in the GD 6–PND 0 group. ♀ No differences in body weight were observed among the GD 6–PND 0, PND 0–PND 21, or GD 6–PND 21 groups from 3 to 35 weeks. However, GD 6–PND 0 mice started gaining less weight than controls from weaning until 35 weeks. ♂ The GD 6–PND 0 and PND 0–PND 21 groups increased BW, but the GD 6–PND 0 group had deceased BW. ♀ No effect on glucose tolerance in the PND 0–PND 21 or GD 6–PND 21 groups from 3 months to 8 months. PND 0–PND 21 male mice showed glucose intolerance. |
| [61] | 10 μg/kg/day and 10 mg/kg/day | Low and high | Diet | 2 weeks prior to mating until weaning | C57BL/6J mice | M and F | High and low doses of BPA significantly impaired insulin secretion in male but not in female offspring. |
| [62] | 50 ng, 50 µg, or 50 mg BPA/kg | Very low, low, and high | Diet | 2 weeks prior to mating, pregnancy, and lactation | Mice | M and F | ♀ 50 ng and 50 mg of BPA/kg in the diet increased serum ADP levels in female adult offspring. ♂ Males exposed to 50 µg BPA/kg had marginally significant lower levels of ADP. ♀ 50 mg of BPA/kg in the diet decreased the mean baseline glucose and insulin levels. ♀ Significant decrease in insulin and the homeostasis assessment model of insulin resistance (HOMA-IR) levels but mildly lower serum glucose levels with 50 mg/kg in the diet in the female offspring. ♀ Significantly decreased serum leptin (50 mg BPA) but no effect in ♂. ♀ At 6 and 9 months of age, 50 ng BPA/kg-exposed females had an increase in fat mass and body weight compared with controls. ♂ No significant changes were found in fat mass in males. |
| [63] | 50 µg/kg/day | Low | Drinking water | GD 9–PND 21 | Wistar rats | M | Exposure to BPA (50 µg/kg/d) significantly increased BW with significantly greater amounts of epididymal and perirenal fat pads and increased food intake. BPA alone had no effect on fasting glucose or the glucose tolerance test, but BPA exposure of 50 µg/kg/day increased insulin and leptin levels. BPA impaired glucose homeostasis, induced obesity, and increased food intake in adult male rats. |
| [64] | 0.1 mg/L | Low | Drinking water | GD 11–PND 21 | SD rats | M | A low BPA dose had no effect on the food intake or water consumption of dams. BPA had no effect on BW of either dams or pups. A low BPA dose led to decreased glucose metabolism in rats. |
| [65] | 0.05, 0.5, or 5 mg/kg/day | Very low, low, and high | Subcutaneous injections | GD 30–GD 90 147 days | Sheep | F | Prenatal-BPA-treated adult females were hyperglycaemic and had IR only at low BPA doses. |
| [66] | 2.5, 25, and 250 µg/kg/day | Very low, low, and high | Drinking water | Month virgin state plus 20 days during pregnancy | SD rats | M and F | BPA had no effect on the weight of pregnant rats or their plasma lipid profile (TC, TG, LDL, and HDL); sacrificed at GD 20. |
| [67] | 20 and 40 µg/kg/day | Low | Orally by gastric intubation | GD 1 to GD 20 | Rats | Foetus | Increase in foetal serum leptin and insulin levels in both treated groups compared to controls. However, there was a decrease in maternal and foetal body weight in both treated groups compared to the control group. |
6.2. Metabolic Effect of Prenatal BPA Exposure in Children (Epidemiological Studies)
| Author (Year) Reference | Country | Study Design (N) | LOD | %>LOD | BPA Assessment | Collection Year(s) | Outcome Time Window | Results |
|---|---|---|---|---|---|---|---|---|
| Huang Y et al., (2021) [68] | Taiwan | Cohort study: 162 mother–infant pairs | 0.16 ng/mL | - | Ultra-performance liquid chromatography coupled with time-of-flight mass spectrometry | 2010 | Mothers: three spot urine samples and three blood samples at approximately 11 and 26 weeks gestation and at admission for delivery Children: cord blood samples | Exposure to BPA in the second trimester was associated with low birth weight. |
| Ouyang F et al., (2020) [69] | China | Birth cohort study: 218 pregnant women | 0.1 µg/L = (0.1ng/mL) | Mothers = 98.2% children = 99.4% | HPLC-MS/MS | 2012–2013 | Spot urine samples Mothers: third trimester Children: 2 years | In boys, a medium maternal prenatal BPA level (1.14 µg/L) was associated with higher plasma glucose. No associations were found between prenatal BPA and child body weight, BMI, skinfold thicknesses, serum lipids, or insulin in children, either girls or boys. |
| Yang T et al., (2017) [70] | Mexico | Cross-sectional: 250 mother–child pairs | 0.4 ng/mL | Prenatal = 70% Children = 85% | Isotope dilution-liquid chromatography-tandem mass spectrometry | 2012 | A single spot urine sample for both Mothers: third trimester Children: 8–14 years | Increased BPA exposure was positively associated with the sum of skinfold thicknesses and BMI z-score in girls but not in boys. |
| Vafeiadi M et al., (2016) [71] | Greece | Cohort study: 500 mother–child pairs | 0.01 ng/mL | Mothers = 99.6% Children at 2.5 years = 99.6% Children at 4 years = 98.8% | OLYMPUS 2700 immunoassay system | 2007 | A spot urine sample for mothers in the first trimester of pregnancy Children: two spot urine samples at 2.5 and 4 years of age | Prenatal BPA concentrations were associated with lower BMI and adiposity measures in girls and higher measures in boys at 1–4 years of age. Maternal BPA was not significantly associated with birth weight. |
| Martin J et al., (2014) [72] | Canada | Cohort study: 2001 women | 0.2ng/mL | 86.6% | GC-MS-MS instrument with a GC Agilent 6890 N (Agilent Technologies; Mississauga, ON, Canada) coupled with a tandem mass spectrometer Quattro Micro GC | 2008–2011 | Urine samples Mothers: first trimester | In males, there was an inverse relationship between maternal urinary BPA and ADP levels. Female infants were shown to have higher leptin levels than male infants. |
| Volberg V (2013) [73] | Mexico/USA | Birth cohort study: 537 mother–child pairs | 5 0.4 µg/L = 0.4ng/mL | Mothers at 13-week gestation = 79% and mothers at 26-week gestation = 83% Children = 91% | Online solid-phase extraction coupled with isotope-dilution high-performance liquid chromatography tandem mass spectrometry with peak focusing | 1999–2000 | Two urine spot samples Mothers at 13 and 26 weeks gestation Children at 9 years | No differences were observed comparing maternal and child anthropometric measures, including BMI, food consumption, and child birth size. Late-pregnancy urinary BPA levels were associated with increased leptin levels in boys, while early-pregnancy BPA levels were positively related to ADP levels in 9-year-old girls. |
6.3. Why do Low Doses Have More Effect Than High Doses?
7. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
| Reference | Effective Dose | Pregnant Mothers | Offspring Childhood | Offspring Adulthood | ||
|---|---|---|---|---|---|---|
| Male | Female | Male | Female | |||
| [51] | 2.5 µg/kg/day | No effect on lipid metabolism | NS foetus hepatic TG and TC content | |||
| [43] | 1 and 100 µg/kg/day | Week 14 | ||||
| ↑ hepatic TG (1 and 1000 BPA) ↑ liver weight (1 BPA) | ↑ hepatic TG (1000 BPA) ↑ liver weight (1000 BPA) | |||||
| [43] | 1 µg/kg/day | Week 14 | ||||
| ↑ hepatic TG ↑ glucagon ↑ fasting glucose ↑ insulin levels ↑ IPGTT ↑ IPITT | NS hepatic TG NS glucagon NS fasting glucose NS insulin levels NS IPGTT NS IPITT | |||||
| [44] | 5 μg/kg/day | 4 weeks | 10 and 21 weeks | |||
| ↓ BW | NS BW | ↑ glucose clearance ↑ plasma ↑ TG ↑ FFA ↑ UC ↑ VLDL ↑ hepatic TC content NS TC NS HDL NS LDL | ↑ BW (13, 14, 20, and 22 weeks) ↓ hepatic TG NS lipid parameters NS insulin NS glucose tolerance | |||
| [52] | 100 μg/kg/day | NS BW | NS birth weight ↑ hepatic TG ↑ FFA NS body composition (fat/lean mass ratio) | ↑ BW but NS ↑ energy intake but NS ↑ body composition (fat/lean mass ratio) | ||
| [55] | 2.5 µg/Kg/day | ↓ BW third week | ↑ birth weight | |||
| [45] | 0.5 or 50 µg/Kg/day | 5 and 52 weeks | ||||
| ↑ insulin secretion (0.5 BPA) ↓ insulin secretion (50 BPA) | ||||||
| [56] | 0.5 and 5 mg /Kg/day | 21 Months | ||||
| NS plasma triglyceride (0.5 and 5 mg/Kg/day) ↑ hepatic and muscular TG content (0.5 and 5 mg/Kg/day) ↓ plasma LMW adiponectin levels (5 mg/Kg/day) | ||||||
| [57] | 10 μg/kg/day and 10 mg/kg/day | ↓ Birth weight ↓ BW (PND 14 and PND 21) | NS birth weight | PND 98 to PND 117 | ||
| ↑ BW and body fat content (PND 98 and PND 117)↑ insulin levels (10 μg/kg/day) NS fasting glucose level in both doses ↑ IPGTT (10 mg/kg/day) ↓ maximal glucose stimulated insulin release | NS fasting glucose level NS IPGTT | |||||
| [53] | 50 µg/ kg/day | ↓ gWAT at PND 45 glucose intolerance at PND 35 | ↑ BW PND 70-170 NS food intake IR at PND 125 | |||
| [54] | 0.5 or 50 µg/kg/day | NS BW NS water and food intake | 5 Weeks | |||
| ↑ plasma TG (0.5 µg/kg/day) | ↑ plasma TG (50 µg/kg/day) | |||||
| 52 Weeks | ||||||
| ↓ BW (0.5 µg/kg/day) IR (0.5 µg/kg/day) NS plasma TG NS cholesterol NS leptin NS adiponectin | ↑ BW (50 µg/kg/day) NS plasma TG NS cholesterol NS leptin NS adiponectin | |||||
| [47] | 10 μg/kg/day | ↑ hepatic TG levels at PND 196 ↑ BW at PND 196 ↑ insulin level at 28 weeks ↑ perigonadal fat pad weight at 28 weeks ↑ fasting blood glucose at 17 weeks but NS impaired glucose tolerance | ||||
| [48] | 1 and 10 µg/mL | NS BW NS food and water intake | ↑ BW both doses (PND 7-100) ↑ Blood glucose ↑ insulin ↓ serum adiponectin at (10 µg/mL BPA) PND 50 | ↑ BW both doses (PND 7-100) ↑ blood glucose ↑ insulin ↓ serum adiponectin IR at (1 and 10 µg/mL BPA) PND 100 | ||
| [58] | 50 μg/kg/day | 3 weeks NS BW NS blood glucose ↑ serum insulin 21 weeks ↑ BW ↑ insulin resistance impaired glucose tolerance in rats’ hepatic tissue | ||||
| [26] | 1 or 20 µg/kg diet BPA | Both low doses NS BW NS food intake | NS BW Impaired glucose tolerance ↑ plasma insulin NS leptin level | NS BW NS glucose tolerance ↑ plasma leptin | ||
| [59] | 10 or 100 µg/kg/day | Glucose intolerance (10 µg/kg/day) ↑ insulin sensitivity ↑ leptin ↑ TG ↑ glycerol (100 µg/kg/day) | 3 months NS insulin resistance NS glucose intolerance 6 months ↓ glucose tolerance ↑ insulin resistance ↓ BW (10 µg/kg/day) ↑ leptin (100 µg/kg/day) | 3 months NS insulin resistance NS glucose intolerance | ||
| [49] | 25 mg BPA/kg diet | Did not alter the expression of insulin or increase in glucagon expression in BPA-exposed foetal pancreatic islets | ||||
| [60] | 100 µg/kg/day | NS birth weight | NS birth weight | ↓ BW 3-8 months impaired glucose tolerance 3 months glucose intolerance | ↓ BW NS glucose tolerance | |
| [61] | 10 μg/kg/day and 10 mg/kg/day | 16 to 21 weeks Both doses of BPA significantly impaired insulin secretion | ||||
| [62] | 50ng, 50µg, or 50mg BPA/kg | ↓ ADP at 50 µg BPA/kg NS fat mass and body weight | ↑ ADP ♀ (50 ng and 50 mg of BPA/kg diet) ↓ the mean baseline glucose and insulin levels (50 mg of BPA/kg diet) ↑ fat mass and body weight ↓ serum leptin ↓ insulin and HOMA-IR (50 mg of BPA/kg diet) | |||
| [63] | 50 µg/kg/day | 20 weeks ↑ BW ↑ epididymal and perirenal fat pads ↑ food intake NS fasting glucose and glucose tolerance test ↑ insulin and leptin levels impaired glucose homeostasis ↑ food intake | ||||
| [64] | 0.1 mg/L | NS BW NS food intake NS water intake | NS BW ↓ glucose metabolism | |||
| [65] | 0.05mg/kg/day | ↑ glucose level IR | ||||
| [66] | 2.5, 25, and 250µg/kg/day | NS BW NS plasma lipid profile (cholesterol, HDL, LDL, and TG) | ||||
| [67] | 20 and 40 µg/kg/day | ↓ BW | ↓ BW ↑ foetal serum leptin ↑ insulin levels in both treated groups | |||
References
- Talsness, C.E.; Andrade, A.J.M.; Kuriyama, S.N.; Taylor, J.A.; Saal, F.S.V. Components of plastic: Experimental studies in animals and relevance for human health. Philos. Trans. R. Soc. B Biol. Sci. 2009, 364, 2079–2096. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kloukos, D.; Pandis, N.; Eliades, T. In vivo bisphenol-A release from dental pit and fissure sealants: A systematic review. J. Dent. 2013, 41, 659–667. [Google Scholar] [CrossRef] [PubMed]
- Valentino, R.; D’Esposito, V.; Ariemma, F.; Cimmino, I.; Beguinot, F.; Formisano, P. Bisphenol A environmental exposure and the detrimental effects on human metabolic health: Is it necessary to revise the risk assessment in vulnerable population? J. Endocrinol. Investig. 2016, 39, 259–263. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lorber, M.; Schecter, A.; Paepke, O.; Shropshire, W.; Christensen, K.; Birnbaum, L. Exposure assessment of adult intake of bisphenol A (BPA) with emphasis on canned food dietary exposures. Environ. Int. 2015, 77, 55–62. [Google Scholar] [CrossRef] [Green Version]
- Barker, D.J.P. The developmental origins of adult disease. Curr. Opin. Pediatr. 2009, 21, 230–234. [Google Scholar] [CrossRef]
- Farahani, M.; Rezaei-Tavirani, M. A systematic review of microRNA expression studies with exposure to bisphenol A. J. Appl. Toxicol. 2020, 41, 4–19. [Google Scholar] [CrossRef]
- Almeida, S.; Raposo, A.; Almeida-González, M.; Carrascosa, C. Bisphenol A: Food Exposure and Impact on Human Health. Compr. Rev. Food Sci. Food Saf. 2018, 17, 1503–1517. [Google Scholar] [CrossRef] [Green Version]
- Lejonklou, M.H.; Dunder, L.; Bladin, E.; Pettersson, V.; Rönn, M.; Lind, L.; Waldén, T.B.; Lind, P.M. Effects of low-dose developmental bisphenol a exposure on metabolic parameters and gene expression in male and female fischer 344 rat offspring. Environ. Health Perspect. 2017, 125, 067018. [Google Scholar] [CrossRef]
- Rochester, J.R. Bisphenol A and human health: A review of the literature. Reprod. Toxicol. 2013, 42, 132–155. [Google Scholar] [CrossRef]
- Richter, C.A.; Birnbaum, L.S.; Farabollini, F.; Newbold, R.R.; Rubin, B.S.; Talsness, C.E.; Vandenbergh, J.G.; Walser-Kuntz, D.R.; vom Saal, F.S. In vivo effects of bisphenol A in laboratory rodent studies. Reprod. Toxicol. 2007, 24, 199–224. [Google Scholar] [CrossRef] [Green Version]
- Zhang, B.; He, Y.; Zhu, H.; Huang, X.; Bai, X.; Kannan, K.; Zhang, T. Concentrations of bisphenol A and its alternatives in paired maternal–fetal urine, serum and amniotic fluid from an e-waste dismantling area in China. Environ. Int. 2020, 136, 105407. [Google Scholar] [CrossRef] [PubMed]
- Han, C.; Hong, Y. Bisphenol A, Hypertension, and Cardiovascular Diseases: Epidemiological, Laboratory, and Clinical Trial Evidence. Curr. Hypertens. Rep. 2016, 18, 11. [Google Scholar] [CrossRef] [PubMed]
- Moon, S.; Hoon, S.; Beom, C.; Joo, Y.; Joon, H.; Sun, D. Science of the Total Environment Effects of bisphenol A on cardiovascular disease: An epidemiological study using National Health and Nutrition Examination Survey 2003–2016 and meta-analysis. Sci. Total Environ. 2020, 763, 142941. [Google Scholar] [CrossRef] [PubMed]
- Legeay, S.; Sébastien, F. Is bisphenol A an environmental obesogen? Fundam. Clin. Pharmacol. 2017, 31, 594–609. [Google Scholar] [CrossRef] [Green Version]
- Jain, J.; Gupta, N.; Mathur, R.; Nimesh, S.; Mathur, S.K. A Study on Impact of BPA in the Adipose Tissue Dysfunction (Adiposopathy) in Asian Indian Type 2 Diabetes Mellitus Subjects. Indian J. Clin. Biochem. 2020, 35, 451–457. [Google Scholar] [CrossRef]
- Silver, M.K.; O’Neill, M.S.; Sowers, M.F.R.; Park, S.K. Urinary Bisphenol a and type-2 diabetes in U.S. Adults: Data from NHANES 2003–2008. PLoS ONE 2011, 6, e26868. [Google Scholar] [CrossRef] [Green Version]
- Kim, M.E.; Park, H.R.; Gong, E.J.; Choi, S.Y.; Kim, H.S.; Lee, J. Exposure to bisphenol A appears to impair hippocampal neurogenesis and spatial learning and memory. Food Chem. Toxicol. 2011, 49, 3383–3389. [Google Scholar] [CrossRef]
- Negashi, T.; Kawasaki, K.; Suzaki, S.; Maeda, H.; Ishii, Y.; Kyuwa, S.; Kuroda, Y.; Yoshikawa, Y. Behavioral alterations in response to fear-provoking stimuli and tranylcypromine induced by perinatal exposure to bisphenol A and nonylphenol in male rats. Environ. Health Perspect. 2004, 112, 1159–1164. [Google Scholar] [CrossRef] [Green Version]
- Salian, S.; Doshi, T.; Vanage, G. Perinatal exposure of rats to Bisphenol A affects fertility of male offspring-An overview. Reprod. Toxicol. 2011, 31, 359–362. [Google Scholar] [CrossRef]
- Bhosale, V.V.; Singh, S.; Srivastava, M.; Pathak, P.; Prakash, S.; Sonkar, S.; Misra, A.K.; Ghatak, A. A case control study of clinical and biochemical parameters of metabolic syndrome with special attention among young and middle aged population. Diabetes Metab. Syndr. Clin. Res. Rev. 2019, 13, 2653–2659. [Google Scholar] [CrossRef]
- Nicolaas, P.; Wassenaar, H.; Trasande, L.; Legler, J. Systematic Review and Meta-Analysis of Early-Life Exposure to Bisphenol A and Obesity-Related Outcomes in Rodents. Environ. Health Perspect. 2015, 125, 106001. [Google Scholar]
- Tang-Péronard, J.L.; Andersen, H.R.; Jensen, T.K.; Heitmann, B.L. Endocrine-disrupting chemicals and obesity development in humans: A review. Obes. Rev. 2011, 12, 622–636. [Google Scholar] [CrossRef]
- Vom Saal, F.S.; Nagel, S.C.; Coe, B.L.; Angle, B.M.; Taylor, J.A. The estrogenic endocrine disrupting chemical bisphenol A (BPA) and obesity. Mol. Cell. Endocrinol. 2012, 354, 74–84. [Google Scholar] [CrossRef] [Green Version]
- Boudalia, S.; Bousbia, A.; Boumaaza, B.; Oudir, M.; Chantal, M.; Lavier, C. Relationship between endocrine disruptors and obesity with a focus on bisphenol A: A narrative review. Tabriz Univ. Med. Sci. 2021, 11, 289–300. [Google Scholar] [CrossRef] [PubMed]
- Zulkifli, S.; Rahman, A.A.; Kadir, S.H.S.A.; Nor, N.S.M. Bisphenol A and its effects on the systemic organs of children. Eur. J. Pediatr. 2021, 180, 3111–3127. [Google Scholar] [CrossRef] [PubMed]
- Mackay, H.; Patterson, Z.R.; Khazall, R.; Patel, S.; Tsirlin, D.; Abizaid, A. Organizational Effects of Perinatal Exposure to Bisphenol-A and Diethylstilbestrol on Arcuate Nucleus Circuitry Controlling Food Intake and Energy Expenditure in Male and Female CD-1 Mice. Endocrinology 2013, 154, 1465–1475. [Google Scholar] [CrossRef]
- Mouneimne, Y.; Nasrallah, M.; Khoueiry-Zgheib, N.; Nasreddine, L.; Nakhoul, N.; Ismail, H.; Abiad, M.; Koleilat, L.; Tamim, H. Bisphenol A urinary level, its correlates, and association with cardiometabolic risks in Lebanese urban adults. Environ. Monit. Assess. 2017, 189, 517. [Google Scholar] [CrossRef]
- Bertoli, S.; Leone, A.; Battezzati, A. Human Bisphenol A Exposure and the “Diabesity Phenotype”. Dose Response 2015, 13, 26858585. [Google Scholar] [CrossRef] [Green Version]
- Chooi, Y.C.; Ding, C.; Magkos, F. The epidemiology of obesity. Metabolism 2019, 92, 6–10. [Google Scholar] [CrossRef] [Green Version]
- Geens, T.; Aerts, D.; Berthot, C.; Bourguignon, J.-P.; Goeyens, L.; Lecomte, P.; Maghuin-Rogister, G.; Pironnet, A.-M.; Pussemier, L.; Scippo, M.-L.; et al. A review of dietary and non-dietary exposure to bisphenol-A. Food Chem. Toxicol. 2012, 50, 3725–3740. [Google Scholar] [CrossRef]
- Vandenberg, L.N.; Hauser, R.; Marcus, M.; Olea, N.; Welshons, W.V. Human exposure to bisphenol A (BPA). Reprod. Toxicol. 2007, 24, 139–177. [Google Scholar] [CrossRef] [PubMed]
- Nishikawa, M.; Iwano, H.; Yanagisawa, R.; Koike, N.; Inoue, H.; Yokota, H. Placental Transfer of Conjugated Bisphenol A and Subsequent Reactivation in the Rat Fetus. Environ. Health Perspect. 2010, 118, 1196–1203. [Google Scholar] [CrossRef] [PubMed]
- BBalakrishnan, B.; Henare, K.; Thorstensen, E.B.; Ponnampalam, A.P.; Mitchell, M.D. Transfer of bisphenol A across the human placenta. Am. J. Obstet. Gynecol. 2010, 202, 393.e1–393.e7. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.; Choi, K.; Park, J.; Moon, H.-B.; Choi, G.; Lee, J.J.; Suh, E.; Kim, H.-J.; Eun, S.-H.; Kim, G.-H.; et al. Bisphenol A distribution in serum, urine, placenta, breast milk, and umbilical cord serum in a birth panel of mother–neonate pairs. Sci. Total Environ. 2017, 626, 1494–1501. [Google Scholar] [CrossRef] [PubMed]
- EFSA (European Food Safety Authority). Scientific Opinion on the risks to public health related to the presence of bisphenol A (BPA) in foodstuffs. EFSA J. 2015, 13, 3978. [Google Scholar] [CrossRef]
- Cimmino, I.; Fiory, F.; Perruolo, G.; Miele, C.; Beguinot, F.; Formisano, P.; Oriente, F. Potential Mechanisms of Bisphenol A (BPA) Contributing to Human Disease. Int. J. Mol. Sci. 2020, 21, 5761. [Google Scholar] [CrossRef]
- Delfosse, V.; Grimaldi, M.; Pons, J.-L.; Boulahtouf, A.; le Maire, A.; Cavailles, V.; Labesse, G.; Bourguet, W.; Balaguer, P. Structural and mechanistic insights into bisphenols action provide guidelines for risk assessment and discovery of bisphenol A substitutes. Proc. Natl. Acad. Sci. USA 2012, 109, 14930–14935. [Google Scholar] [CrossRef] [Green Version]
- Ben-Jonathan, N.; Hugo, E.R.; Brandebourg, T.D. Effects of bisphenol A on adipokine release from human adipose tissue: Implications for the metabolic syndrome. Mol. Cell. Endocrinol. 2010, 304, 49–54. [Google Scholar] [CrossRef] [Green Version]
- Rubin, B.S.; Paranjpe, M.; DaFonte, T.; Schaeberle, C.; Soto, A.M.; Obin, M.; Greenberg, A.S. Perinatal BPA exposure alters body weight and composition in a dose specific and sex specific manner: The addition of peripubertal exposure exacerbates adverse effects in female mice. Reprod. Toxicol. 2016, 68, 130–144. [Google Scholar] [CrossRef] [Green Version]
- Wang, A.; Luo, J.; Moore, W.; Alkhalidy, H.; Wu, L.; Zhang, J.; Zhen, W.; Wang, Y.; Clegg, D.J.; Xu, B.; et al. GPR30 regulates diet-induced adiposity in female mice and adipogenesis in vitro. Sci. Rep. 2016, 6, srep34302. [Google Scholar] [CrossRef] [Green Version]
- Cimmino, I.; Oriente, F.; D’Esposito, V.; Liguoro, D.; Liguoro, P.; Ambrosio, M.R.; Cabaro, S.; D’Andrea, F.; Beguinot, F.; Formisano, P.; et al. Low-dose Bisphenol-A regulates inflammatory cytokines through GPR30 in mammary adipose cells. J. Mol. Endocrinol. 2019, 63, 273–283. [Google Scholar] [CrossRef] [PubMed]
- Caporossi, L.; Papaleo, B. Exposure to Bisphenol A and Gender Differences: From Rodents to Humans Evidences and Hypothesis about the Health Effects. J. Xenobiot. 2015, 5, 15–19. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Long, Z.; Fan, J.; Wu, G.; Liu, X.; Wu, H.; Liu, J.; Chen, Y.; Su, S.; Cheng, X.; Xu, Z.; et al. Gestational bisphenol A exposure induces fatty liver development in male offspring mice through the inhibition of HNF1b and upregulation of PPARγ. Cell Biol. Toxicol. 2020, 37, 65–84. [Google Scholar] [CrossRef]
- Diamante, G.; Cely, I.; Zamora, Z.; Ding, J.; Blencowe, M.; Lang, J.; Bline, A.; Singh, M.; Lusis, A.J.; Yang, X. Systems toxicogenomics of prenatal low-dose BPA exposure on liver metabolic pathways, gut microbiota, and metabolic health in mice. Environ. Int. 2020, 146, 106260. [Google Scholar] [CrossRef] [PubMed]
- Manukyan, L.; Dunder, L.; Lind, P.M.; Bergsten, P.; Lejonklou, M.H. Developmental exposure to a very low dose of bisphenol A induces persistent islet insulin hypersecretion in Fischer 344 rat offspring. Environ. Res. 2019, 172, 127–136. [Google Scholar] [CrossRef]
- García-Arevalo, M.; Magdalena, P.A.; Dos Santos, J.R.; Quesada, I.; Carneiro, E.M.; Nadal, A. Exposure to Bisphenol-A during Pregnancy Partially Mimics the Effects of a High-Fat Diet Altering Glucose Homeostasis and Gene Expression in Adult Male Mice. PLoS ONE 2014, 9, e100214. [Google Scholar] [CrossRef] [Green Version]
- Wang, D.; Zhu, W.; Yan, S.; Meng, Z.; Yan, J.; Teng, M.; Jia, M.; Li, R.; Zhou, Z. Impaired lipid and glucose homeostasis in male mice offspring after combined exposure to low-dose bisphenol A and arsenic during the second half of gestation. Chemosphere 2018, 210, 998–1005. [Google Scholar] [CrossRef]
- Song, S.; Zhang, L.; Zhang, H.; Wei, W.; Jia, L. Perinatal BPA Exposure Induces Hyperglycemia, Oxidative Stress and Decreased Adiponectin Production in Later Life of Male Rat Offspring. Int. J. Environ. Res. Public Health 2014, 11, 3728–3742. [Google Scholar] [CrossRef] [Green Version]
- Whitehead, R.; Guan, H.; Arany, E.; Cernea, M.; Yang, K. Prenatal exposure to bisphenol A alters mouse fetal pancreatic morphology and islet composition. Horm. Mol. Biol. Clin. Investig. 2016, 25, 171–179. [Google Scholar] [CrossRef]
- WHO. Obesity and Overweight; WHO: Geneva, Switzerland, 2021; Available online: https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight (accessed on 6 June 2022).
- Tonini, C.; Segatto, M.; Bertoli, S.; Leone, A.; Mazzoli, A.; Cigliano, L.; Barberio, L.; Mandalà, M.; Pallottini, V. Prenatal Exposure to BPA: The Effects on Hepatic Lipid Metabolism in Male and Female Rat Fetuses. Nutrients 2021, 13, 1970. [Google Scholar] [CrossRef]
- Strakovsky, R.S.; Wang, H.; Engeseth, N.J.; Flaws, J.A.; Helferich, W.G.; Pan, Y.-X.; Lezmi, S. Developmental bisphenol A (BPA) exposure leads to sex-specific modification of hepatic gene expression and epigenome at birth that may exacerbate high-fat diet-induced hepatic steatosis. Toxicol. Appl. Pharmacol. 2015, 284, 101–112. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Malaisé, Y.; Menard, S.; Cartier, C.; Gaultier, E.; Lasserre, F.; Lencina, C.; Harkat, C.; Geoffre, N.; Lakhal, L.; Castan, I.; et al. Gut dysbiosis and impairment of immune system homeostasis in perinatally-exposed mice to Bisphenol A precede obese phenotype development. Sci. Rep. 2017, 7, 14472. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dunder, L.; Lejonklou, M.H.; Lind, L.; Risérus, U.; Lind, P.M. Low-dose developmental bisphenol A exposure alters fatty acid metabolism in Fischer 344 rat offspring. Environ. Res. 2018, 166, 117–129. [Google Scholar] [CrossRef]
- Benincasa, L.; Mandalà, M.; Paulesu, L.; Barberio, L.; Ietta, F. Prenatal Nutrition Containing Bisphenol A Affects Placenta Glucose Transfer: Evidence in Rats and Human Trophoblast. Nutrients 2020, 12, 1375. [Google Scholar] [CrossRef] [PubMed]
- Puttabyatappa, M.; Martin, J.D.; Andriessen, V.; Stevenson, M.; Zeng, L.; Pennathur, S.; Padmanabhan, V. Developmental programming: Changes in mediators of insulin sensitivity in prenatal bisphenol A-treated female sheep. Reprod. Toxicol. 2019, 85, 110–122. [Google Scholar] [CrossRef]
- Susiarjo, M.; Xin, F.; Bansal, A.; Stefaniak, M.; Li, C.; Simmons, R.A.; Bartolomei, M.S. Bisphenol A Exposure Disrupts Metabolic Health Across Multiple Generations in the Mouse. Endocrinology 2015, 156, 2049–2058. [Google Scholar] [CrossRef]
- Ma, Y.; Xia, W.; Wang, D.Q.; Wan, Y.J.; Xu, B.; Chen, X.; Li, Y.Y.; Xu, S.Q. Hepatic DNA methylation modifications in early development of rats resulting from perinatal BPA exposure contribute to insulin resistance in adulthood. Diabetologia 2013, 56, 2059–2067. [Google Scholar] [CrossRef]
- Magdalena, P.A.; Vieira, E.; Soriano, S.; Menes, L.; Burks, D.; Quesada, I.; Nadal, A. Bisphenol a exposure during pregnancy disrupts glucose homeostasis in mothers and adult male offspring. Environ. Health Perspect. 2010, 118, 1243–1250. [Google Scholar] [CrossRef] [Green Version]
- Liu, J.; Yu, P.; Qian, W.; Li, Y.; Zhao, J.; Huan, F.; Wang, J.; Xiao, H. Perinatal Bisphenol A Exposure and Adult Glucose Homeostasis: Identifying Critical Windows of Exposure. PLoS ONE 2013, 8, e64143. [Google Scholar] [CrossRef]
- Bansal, A.; Rashid, C.; Xin, F.; Li, C.; Polyak, E.; Duemler, A.; van der Meer, T.; Stefaniak, M.; Wajid, S.; Doliba, N.; et al. Sex- and Dose-Specific Effects of Maternal Bisphenol A Exposure on Pancreatic Islets of First- and Second-Generation Adult Mice Offspring. Environ. Health Perspect. 2017, 125, 097022. [Google Scholar] [CrossRef]
- Anderson, O.S.; Peterson, K.E.; Sanchez, B.N.; Zhang, Z.; Mancuso, P.; Dolinoy, D.C. Perinatal bisphenol A exposure promotes hyperactivity, lean body composition, and hormonal responses across the murine life course. FASEB J. 2012, 27, 1784–1792. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Stoker, C.; Andreoli, M.F.; Kass, L.; Bosquiazzo, V.L.; Rossetti, M.F.; Canesini, G.; Luque, E.H.; Ramos, J.G. Perinatal exposure to bisphenol A (BPA) impairs neuroendocrine mechanisms regulating food intake and kisspetin system in adult male rats. Evidences of metabolic disruptor hypothesis. Mol. Cell. Endocrinol. 2019, 499, 110614. [Google Scholar] [CrossRef] [PubMed]
- Xu, X.; Fan, S.; Guo, Y.; Tan, R.; Zhang, J.; Zhang, W.; Pan, B.-X.; Kato, N. The effects of perinatal bisphenol A exposure on thyroid hormone homeostasis and glucose metabolism in the prefrontal cortex and hippocampus of rats. Brain Behav. 2019, 9, e01225. [Google Scholar] [CrossRef] [Green Version]
- Veiga-Lopez, A.; Moeller, J.; Sreedharan, R.; Singer, K.; Lumeng, C.; Ye, W.; Pease, A.; Padmanabhan, V. Developmental programming: Interaction between prenatal BPA exposure and postnatal adiposity on metabolic variables in female sheep. Am. J. Physiol. Metab. 2016, 310, E238–E247. [Google Scholar] [CrossRef] [Green Version]
- Tonini, C.; Segatto, M.; Gagliardi, S.; Bertoli, S.; Leone, A.; Barberio, L.; Mandalà, M.; Pallottini, V. Maternal Dietary Exposure to Low-Dose Bisphenol A Affects Metabolic and Signaling Pathways in the Brain of Rat Fetuses. Nutrients 2020, 12, 1448. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, R. Maternal bisphenol A alters fetal endocrine system: Thyroid adipokine dysfunction. Food Chem. Toxicol. 2016, 95, 168–174. [Google Scholar] [CrossRef]
- Huang, Y.F.; Chang, C.H.; Chen, P.J.; Lin, I.H.; Tsai, Y.A.; Chen, C.F.; Wang, Y.C.; Huang, W.Y.; Tsai, M.S.; Chen, M.L. Prenatal Bisphenol a Exposure, DNA Methylation, and Low Birth Weight: A Pilot Study in Taiwan. Int. J. Environ. Res. Public Health 2021, 18, 6144. [Google Scholar] [CrossRef]
- Ouyang, F.; Zhang, G.H.; Du, K.; Shen, L.; Ma, R.; Wang, X.; Wang, X.; Zhang, J. Maternal prenatal urinary bisphenol A level and child cardio-metabolic risk factors: A prospective cohort study. Environ. Pollut. 2020, 265, 115008. [Google Scholar] [CrossRef]
- Yang, T.; Peterson, K.E.; Meeker, J.D.; Sánchez, B.N.; Zhang, Z.; Cantoral, A.; Solano, M.; Tellez-Rojo, M.M. Bisphenol A and phthalates in utero and in childhood: Association with child BMI z-score and adiposity. Environ. Res. 2017, 156, 326–333. [Google Scholar] [CrossRef] [Green Version]
- Vafeiadi, M.; Roumeliotaki, T.; Myridakis, A.; Chalkiadaki, G.; Fthenou, E.; Dermitzaki, E.; Karachaliou, M.; Sarri, K.; Vassilaki, M.; Stephanou, E.G.; et al. Association of early life exposure to bisphenol A with obesity and cardiometabolic traits in childhood. Environ. Res. 2016, 146, 379–387. [Google Scholar] [CrossRef]
- Ashley-Martin, J.; Dodds, L.; E Arbuckle, T.; Ettinger, A.S.; Shapiro, G.D.; Fisher, M.; Morisset, A.S.; Taback, S.; Bouchard, M.F.; Monnier, P.; et al. A birth cohort study to investigate the association between prenatal phthalate and bisphenol A exposures and fetal markers of metabolic dysfunction. Environ. Health 2014, 13, 84. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Volberg, V.; Harley, K.; Calafat, A.M.; Davé, V.; McFadden, J.; Eskenazi, B.; Holland, N. Maternal Bisphenol A Exposure During Pregnancy and Its Association With Adipokines in Mexican-American Children. Environ. Mol. Mutagenesis 2013, 54, 621–628. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Welshons, W.V.; Thayer, K.A.; Judy, B.M.; Taylor, J.A.; Curran, E.M.; von Saal, F.S. Large effects from small exposures. I. Mechanisms for endocrine-disrupting chemicals with estrogenic activity. Environ. Heal. Perspect. 2003, 111, 994–1006. [Google Scholar] [CrossRef] [PubMed] [Green Version]
| Included Criteria | Excluded Criteria | |
|---|---|---|
| Population | Experiment in animals and humans | All non-human and non-animal studies |
| Intervention | Prenatal BPA exposure | Non-BPA exposure in mixed chemical treatments, transgenerational studies, or direct exposure |
| Comparator | Low and high doses relative to control | |
| Outcome | Metabolic syndrome, glucose homeostasis distribution, lipid homeostasis distribution, diabetes mellitus, disrupted insulin release and level | All other non-metabolic complications or no determination of metabolic parameter outcomes |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Abulehia, H.F.S.; Mohd Nor, N.S.; Sheikh Abdul Kadir, S.H. The Current Findings on the Impact of Prenatal BPA Exposure on Metabolic Parameters: In Vivo and Epidemiological Evidence. Nutrients 2022, 14, 2766. https://doi.org/10.3390/nu14132766
Abulehia HFS, Mohd Nor NS, Sheikh Abdul Kadir SH. The Current Findings on the Impact of Prenatal BPA Exposure on Metabolic Parameters: In Vivo and Epidemiological Evidence. Nutrients. 2022; 14(13):2766. https://doi.org/10.3390/nu14132766
Chicago/Turabian StyleAbulehia, Hala F. S., Noor Shafina Mohd Nor, and Siti Hamimah Sheikh Abdul Kadir. 2022. "The Current Findings on the Impact of Prenatal BPA Exposure on Metabolic Parameters: In Vivo and Epidemiological Evidence" Nutrients 14, no. 13: 2766. https://doi.org/10.3390/nu14132766
APA StyleAbulehia, H. F. S., Mohd Nor, N. S., & Sheikh Abdul Kadir, S. H. (2022). The Current Findings on the Impact of Prenatal BPA Exposure on Metabolic Parameters: In Vivo and Epidemiological Evidence. Nutrients, 14(13), 2766. https://doi.org/10.3390/nu14132766






