Global, Regional, and National Burden of Protein–Energy Malnutrition: A Systematic Analysis for the Global Burden of Disease Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Data Source
2.2. Statistical Analysis
3. Results
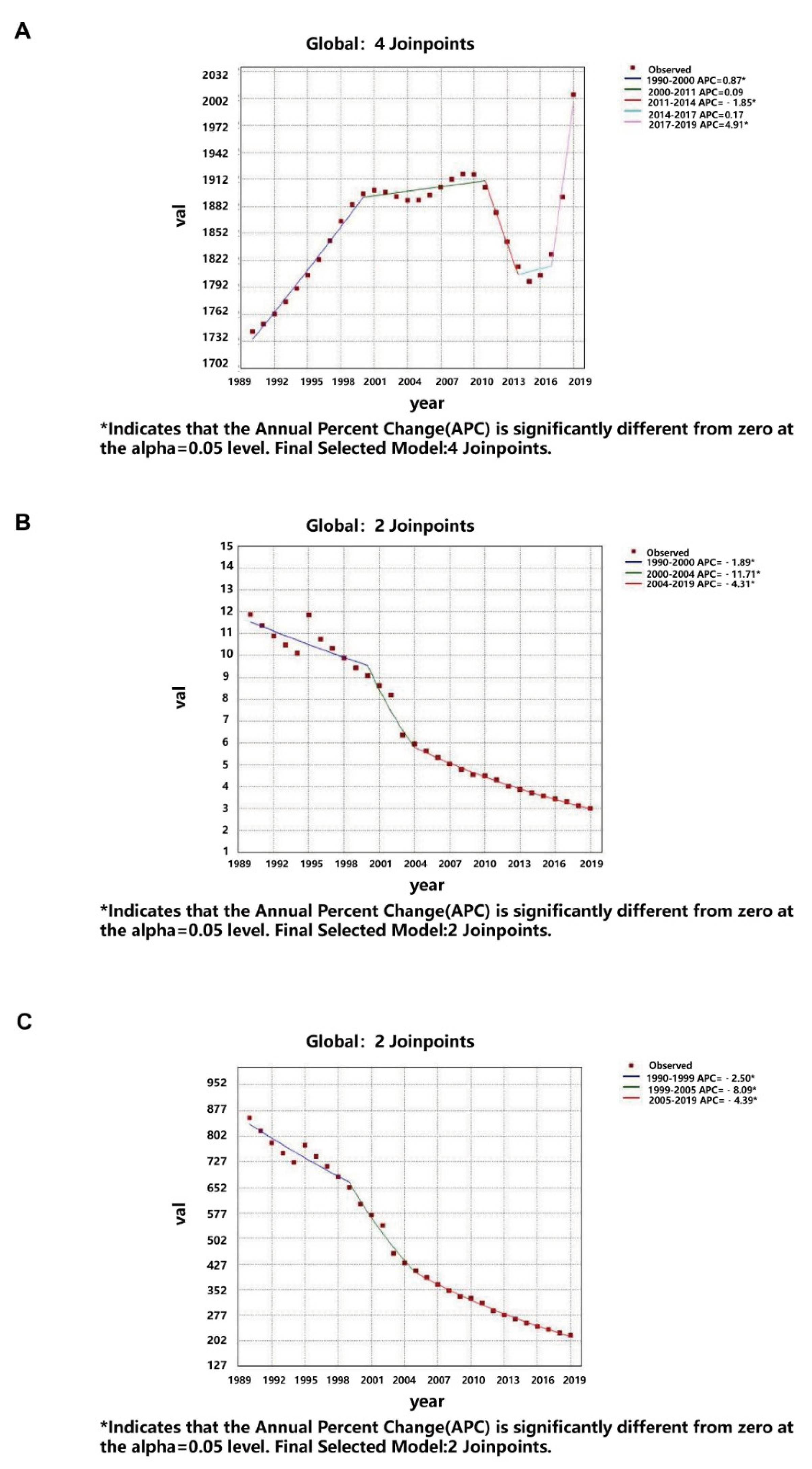
3.1. Global Burden of Protein–Energy Malnutrition
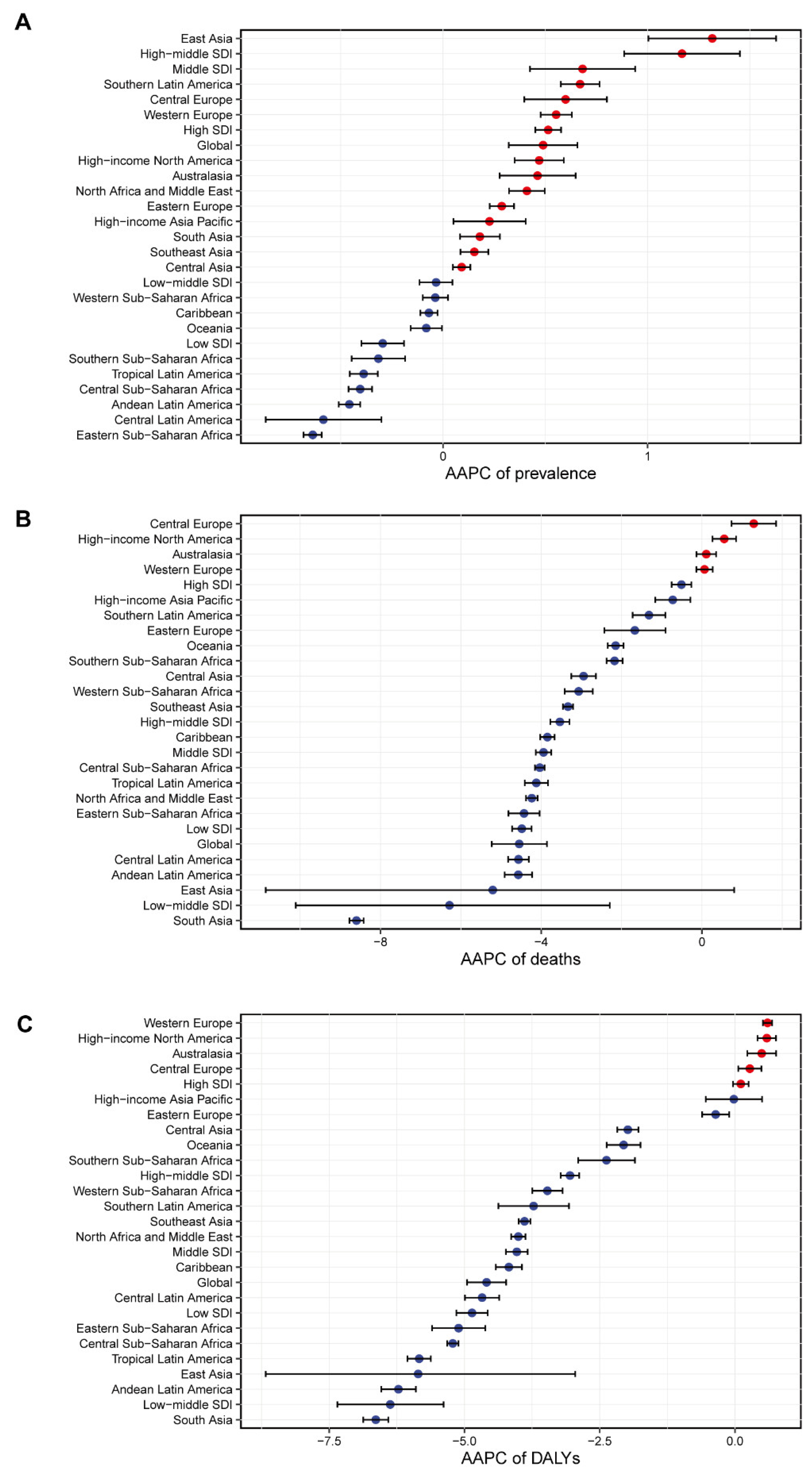
3.2. Regional Burden of Protein–Energy Malnutrition
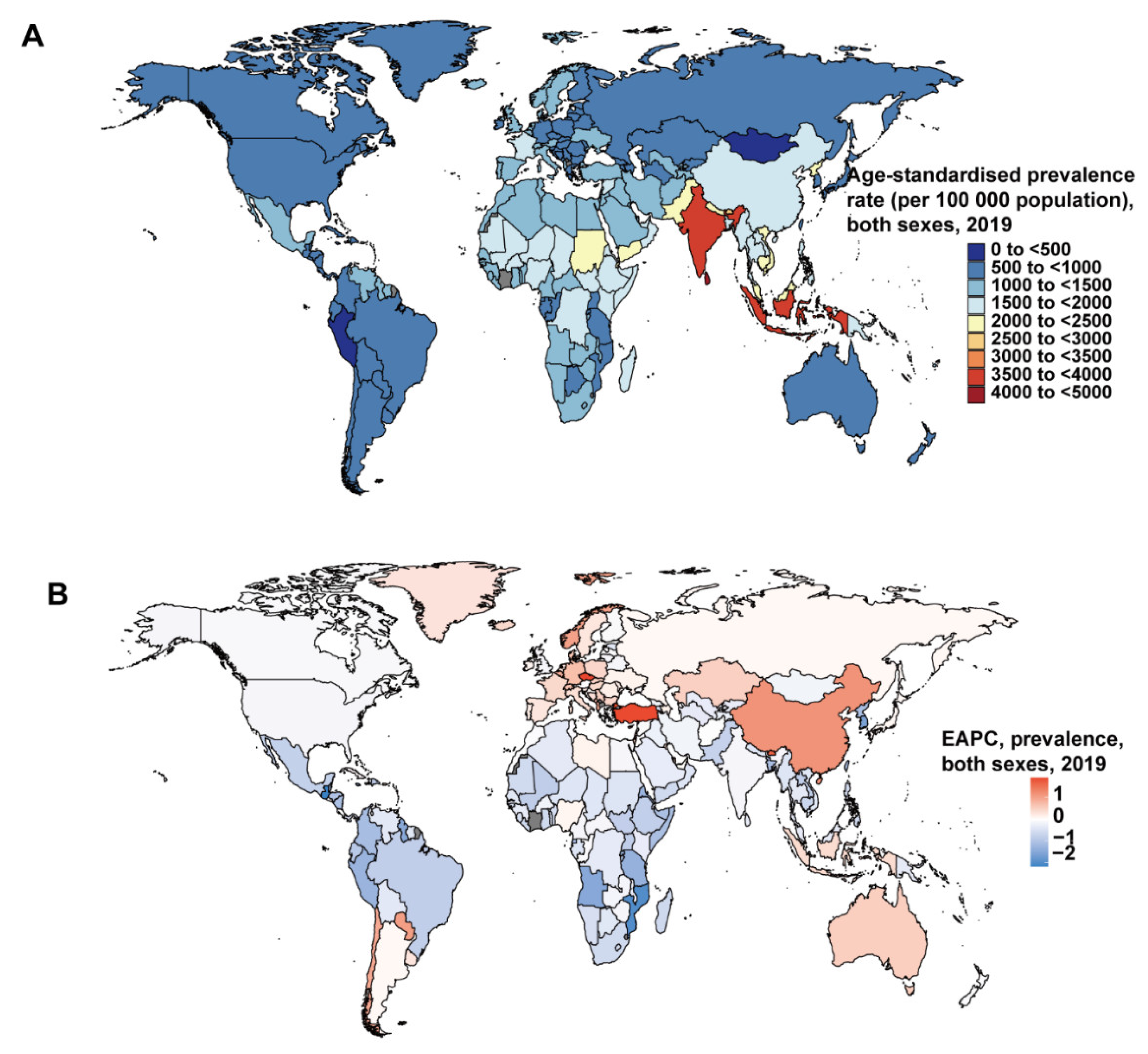
3.3. National Burden of Protein–Energy Malnutrition
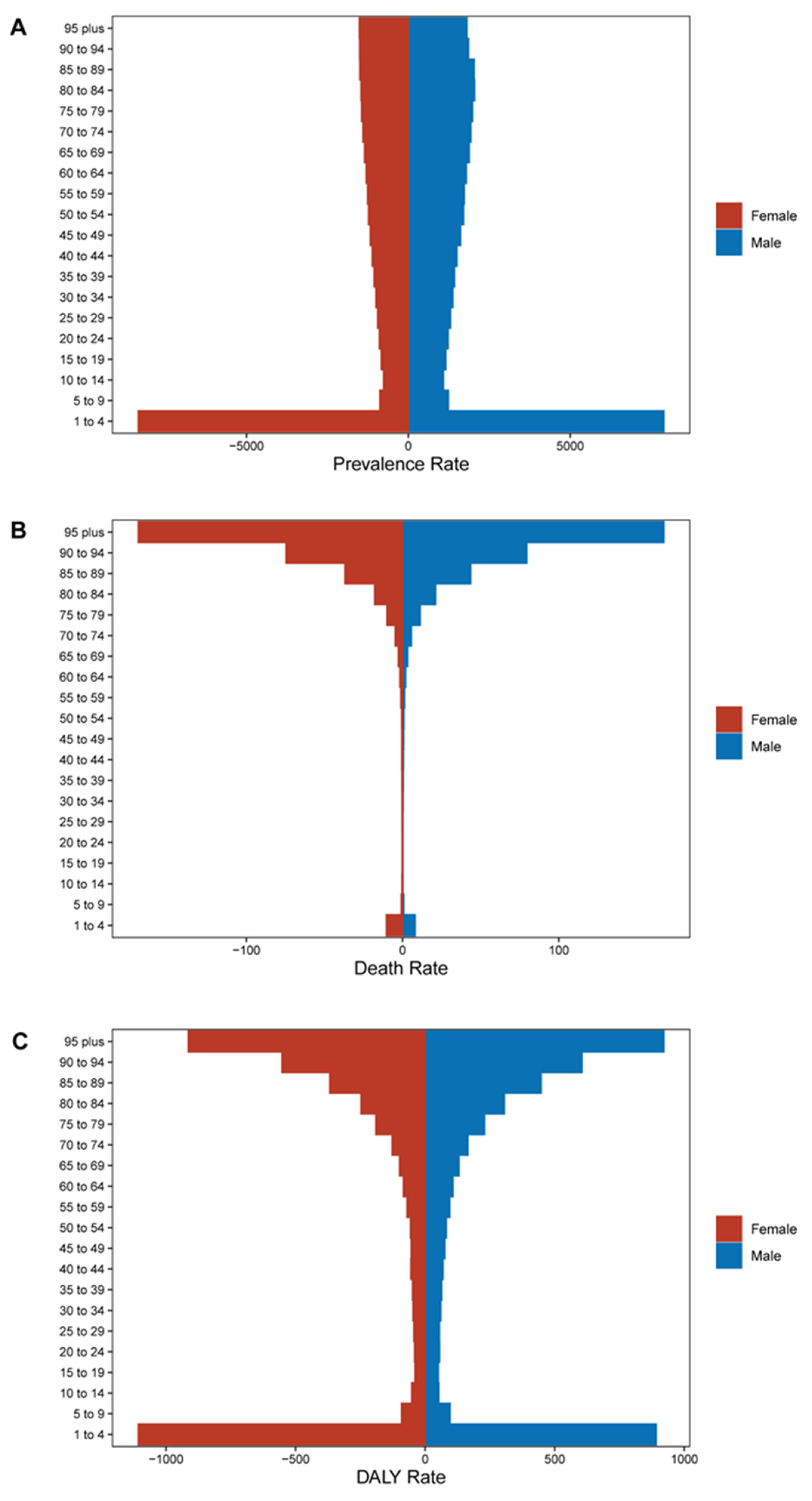
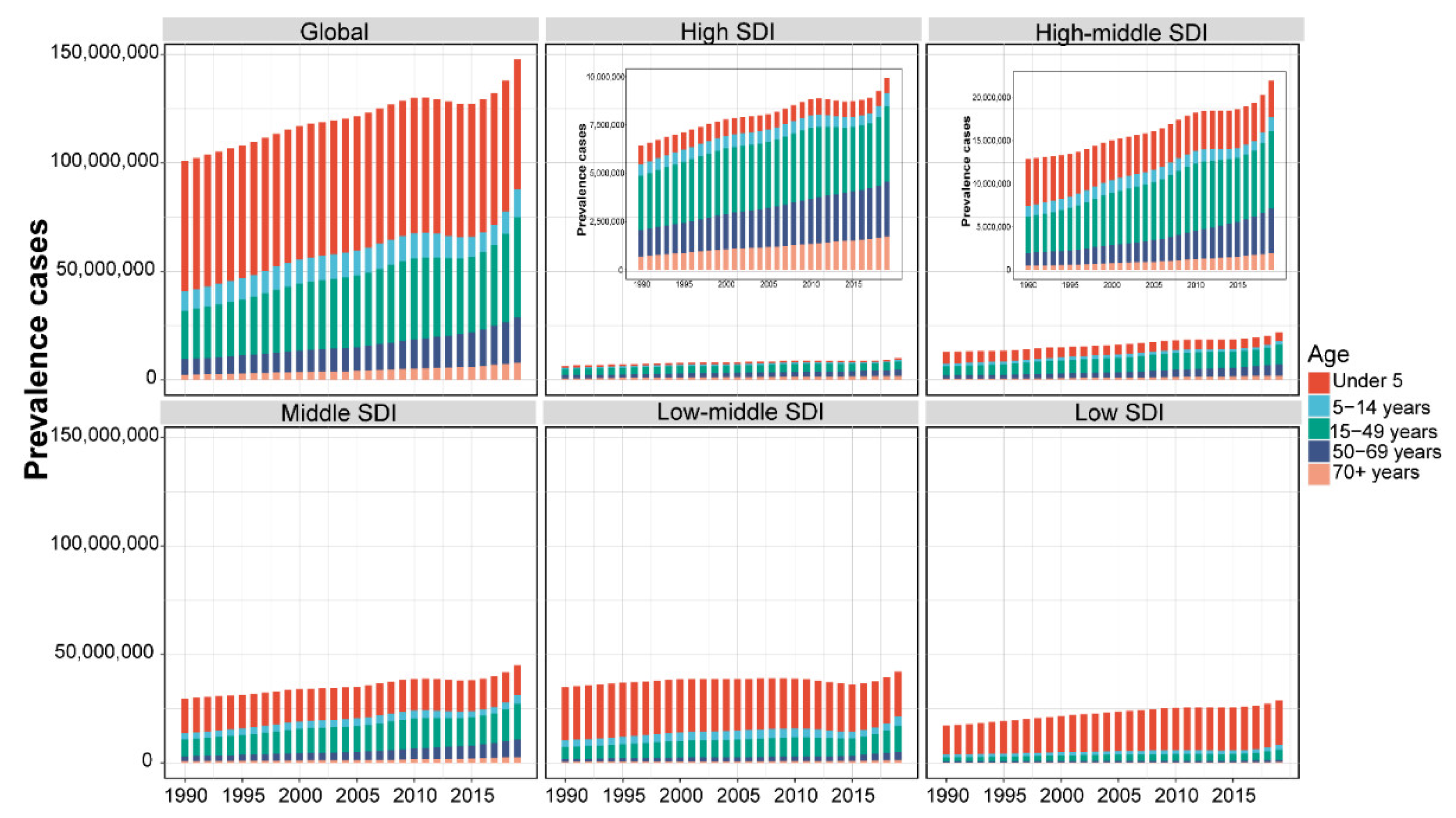
3.4. Age and Sex
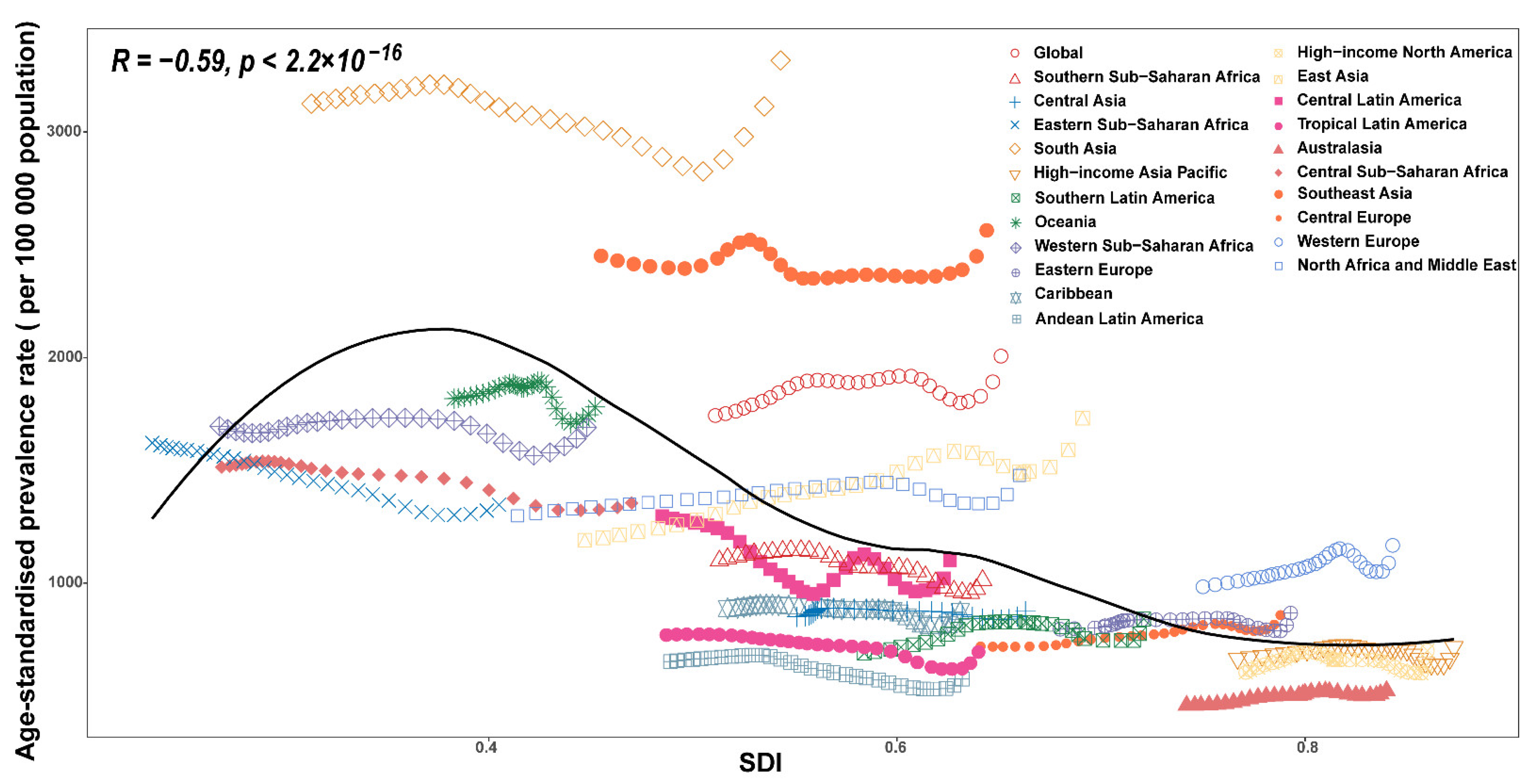
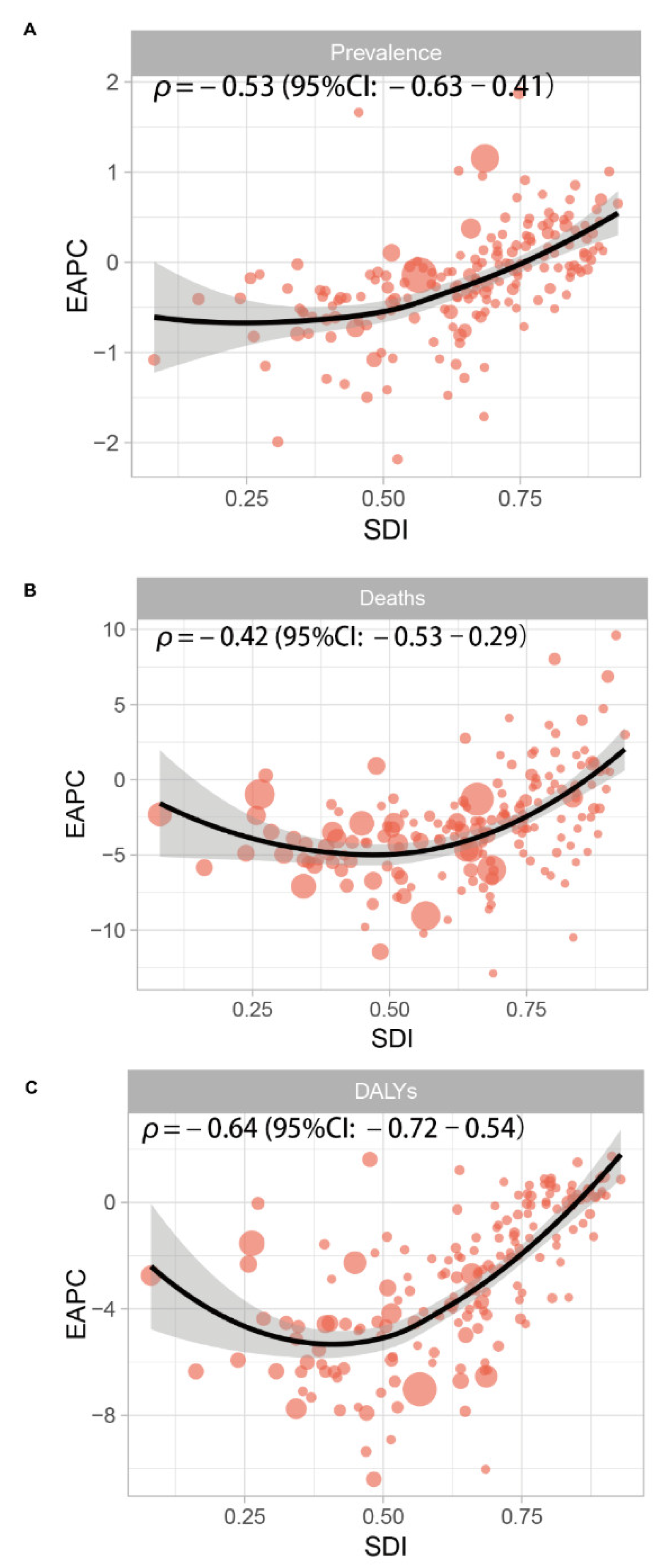
3.5. The Socio-Demographic Index (SDI) and Human Development Index (HDI)
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
References
- Cederholm, T.; Jensen, G.L.; Correia, M.I.T.D.; Gonzalez, M.C.; Fukushima, R.; Higashiguchi, T.; Baptista, G.; Barazzoni, R.; Blaauw, R.; Coats, A.; et al. GLIM criteria for the diagnosis of malnutrition—A consensus report from the global clinical nutrition community. Clin. Nutr. 2019, 38, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Soeters, P.; Bozzetti, F.; Cynober, L.; Forbes, A.; Shenkin, A.; Sobotka, L. Defining malnutrition: A plea to rethink. Clin. Nutr. 2017, 36, 896–901. [Google Scholar] [CrossRef] [PubMed]
- Crichton, M.; Craven, D.; Mackay, H.; Marx, W.; de van der Schueren, M.; Marshall, S. A systematic review, meta-analysis and meta-regression of the prevalence of protein-energy malnutrition: Associations with geographical region and sex. Age Ageing 2019, 48, 38–48. [Google Scholar] [CrossRef]
- Levels and Trends in Child Malnutrition: UNICEF/WHO/The World Bank Group Joint Child Malnutrition Estimates: Key findings of the 2021 Edition. Available online: https://www.who.int/publications-detail-redirect/9789240025257 (accessed on 25 April 2022).
- Raynaud-Simon, A.; Revel-Delhom, C.; Hébuterne, X. Clinical practice guidelines from the French health high authority: Nutritional support strategy in protein-energy malnutrition in the elderly. Clin. Nutr. 2011, 30, 312–319. [Google Scholar] [CrossRef] [PubMed]
- Bray, F.; Ferlay, J.; Soerjomataram, I.; Siegel, R.L.; Torre, L.A.; Jemal, A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 2018, 68, 394–424. [Google Scholar] [CrossRef] [PubMed]
- Lozano, R.; Naghavi, M.; Foreman, K.; Lim, S.; Shibuya, K.; Aboyans, V.; Abraham, J.; Adair, T.; Aggarwal, R.; Ahn, S.Y.; et al. Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: A systematic analysis for the Global Burden of Disease Study 2010. Lancet 2012, 380, 2095–2128. [Google Scholar] [CrossRef]
- Yusuf, S.; Hawken, S.; Ôunpuu, S.; Dans, T.; Avezum, A.; Lanas, F.; McQueen, M.; Budaj, A.; Pais, P.; Varigos, J.; et al. Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): Case-control study. Lancet 2004, 364, 937–952. [Google Scholar] [CrossRef]
- GBD 2019 Diseases and Injuries Collaborators. Global Burden of 369 Diseases and Injuries in 204 Countries and Territories, 1990–2019: A systematic analysis for the Global Burden of Disease Study 2019. Lancet 2020, 17, 1204–1222. [Google Scholar] [CrossRef]
- Webb, P.; Stordalen, G.A.; Singh, S.; Wijesinha-Bettoni, R.; Shetty, P.; Lartey, A. Hunger and malnutrition in the 21st century. BMJ 2018, 361, k2238. [Google Scholar] [CrossRef]
- Micha, R.; Mannar, V.; Afshin, A.; Allemandi, L.; Baker, P.; Battersby, J.; Bhutta, Z.; Chen, K.; Corvalan, C.; Di Cesare, M.; et al. 2020 Global Nutrition Report: Action on Equity to end Malnutrition. 2020. Available online: https://globalnutritionreport.org/reports/2020-global-nutrition-report/ (accessed on 7 May 2022).
- Soeters, P.B.; Reijven, P.L.M.; van der Schueren, M.A.E.va.; Schols, J.M.G.A.; Halfens, R.J.G.; Meijers, J.M.M.; van Gemert, W.G. A rational approach to nutritional assessment. Clin. Nutr. 2008, 27, 706–716. [Google Scholar] [CrossRef]
- Cederholm, T.; Barazzoni, R.; Austin, P.; Ballmer, P.; Biolo, G.; Bischoff, S.C.; Compher, C.; Correia, I.; Higashiguchi, T.; Holst, M.; et al. ESPEN guidelines on definitions and terminology of clinical nutrition. Clin. Nutr. 2017, 36, 49–64. [Google Scholar] [CrossRef]
- Perspective: The Potential Role of Essential Amino Acids and the Mechanistic Target of Rapamycin Complex 1 (mTORC1) Pathway in the Pathogenesis of Child Stunting | Advances in Nutrition | Oxford Academic. Available online: https://academic.oup.com/advances/article/7/5/853/4616731?login=true (accessed on 7 May 2022).
- Laplante, M.; Sabatini, D.M. mTOR Signaling in Growth Control and Disease. Cell 2012, 149, 274–293. [Google Scholar] [CrossRef]
- Nova, E.; Samartín, S.; Gómez, S.; Morandé, G.; Marcos, A. The adaptive response of the immune system to the particular malnutrition of eating disorders. Eur. J. Clin. Nutr. 2002, 56 (Suppl. S3), S34–S37. [Google Scholar] [CrossRef]
- Walker, A.F. The Contribution of Weaning Foods to Protein–Energy Malnutrition. Nutr. Res. Rev. 1990, 3, 25–47. [Google Scholar] [CrossRef][Green Version]
- Bhutia, D.T. Protein Energy Malnutrition in India: The Plight of Our Under Five Children. J. Fam. Med. Prim. Care 2014, 3, 63–67. [Google Scholar] [CrossRef]
- Sharghi, A.; Kamran, A.; Faridan, M. Evaluating risk factors for protein-energy malnutrition in children under the age of six years: A case-control study from Iran. Int. J. Gen. Med. 2011, 4, 607–611. [Google Scholar] [CrossRef][Green Version]
- Getaneh, T.; Assefa, A.; Tadesse, Z. Protein-energy malnutrition in urban children: Prevalence and determinants. Ethiop. Med. J. 1998, 36, 153–166. [Google Scholar]
- Raja, R.; Lim, A.V.; Lim, Y.P.; Lim, G.; Chan, S.P.; Vu, C.K.F. Malnutrition screening in hospitalised patients and its implication on reimbursement. Intern. Med. J. 2004, 34, 176–181. [Google Scholar] [CrossRef]
- Dj, M.; Aa, J. Protein/energy ratios of current diets in developed and developing countries compared with a safe protein/energy ratio: Implications for recommended protein and amino acid intakes. Public Health Nutr. 2004, 7, 387–405. [Google Scholar] [CrossRef]
- Castel, H.; Shahar, D.; Harman-Boehm, I. Gender Differences in Factors Associated with Nutritional Status of Older Medical Patients. J. Am. Coll. Nutr. 2006, 25, 128–134. [Google Scholar] [CrossRef]
- Heersink, J.T.; Brown, C.J.; Dimaria-Ghalili, R.A.; Locher, J.L. Undernutrition in Hospitalized Older Adults: Patterns and Correlates, Outcomes, and Opportunities for Intervention with a Focus on Processes of Care. J. Nutr. Elder. 2010, 29, 4–41. [Google Scholar] [CrossRef]
- Fuster, V. Changing Demographics. J. Am. Coll. Cardiol. 2017, 69, 3002–3005. [Google Scholar] [CrossRef]
- Li, F. Physical activity and health in the presence of China’s economic growth: Meeting the public health challenges of the aging population. J. Sport Health Sci. 2016, 5, 258–269. [Google Scholar] [CrossRef]
- Walton, E.; Allen, S. Malnutrition in developing countries. Paediatr. Child Health 2011, 21, 418–424. [Google Scholar] [CrossRef]
- FAO. The State of Food Insecurity in the World, 2005: Eradicating World Hunger-Key to Achieving the Millennium Development Goals; Food & Agriculture Organization: Rome, Italy, 2005.
- High Level Panel of Experts. 2nd Note on critical and emerging issues for food security and nutrition. A note by the High Level Panel of Experts on Food Security and Nutrition of the Committee on World Food Security. Available online: https://www.fao.org/fileadmin/user_upload/hlpe/hlpe_documents/Critical-Emerging-Issues-2016/HLPE_Note-to-CFS_Critical-and-Emerging-Issues-2nd-Edition__27-April-2017_.pdf (accessed on 25 April 2022).
- Ashworth, A.; Chopra, M.; McCoy, D.; Sanders, D.; Jackson, D.; Karaolis, N.; Sogaula, N.; Schofield, C. WHO guidelines for management of severe malnutrition in rural South African hospitals: Effect on case fatality and the influence of operational factors. Lancet 2004, 363, 1110–1115. [Google Scholar] [CrossRef]
- Nuss, E.T.; Tanumihardjo, S.A. Quality Protein Maize for Africa: Closing the Protein Inadequacy Gap in Vulnerable Populations. Adv. Nutr. 2011, 2, 217–224. [Google Scholar] [CrossRef]
| 1990 | 2019 | 1990–2019 | |||
|---|---|---|---|---|---|
| Prevalence Cases No. (95% UI) | ASR per 100,000 No. (95% UI) | Prevalence Cases No. (95% UI) | ASR per 100,000 No. (95% UI) | EAPC No. (95% CI) | |
| Global | 100,977,331.3 (92,783,224.2–110,877,370.1) | 1743.1 (1587.1–1928.7) | 147,672,757.9 (130,405,923.7–167,471,359.5) | 2006.4 (1786–2261.3) | 0.19 (0.08–0.31) |
| Social-demographic index | |||||
| Low SDI | 17,156,823.7 (16,449,965.2–18,031,793.4) | 2218.2 (2076.1–2387.2) | 28,682,621.5 (26,973,402.2–30,794,848.6) | 2030.2 (1872.4–2221.8) | −0.61 (−0.72–0.51) |
| Low-middle SDI | 34,823,174.6 (32,775,266.5–37,362,791.2) | 2445.7 (2262.2–2670.4) | 42,123,907.2 (37,747,744.6–47,459,684) | 2429.1 (2186.2–2723.2) | −0.45 (−0.58–0.32) |
| Middle SDI | 29,621,821.1 (26,779,018.9–33,164,070.2) | 1648.3 (1479.7–1848.9) | 44,926,275.8 (38,798,928.9–52,033,671.7) | 1996.2 (1748.7–2288.2) | 0.42 (0.31–0.52) |
| High-middle SDI | 12,900,075.5 (11,312,222.2–14,908,449.5) | 1166 (1029.2–1337.5) | 21,951,415 (18,393,911.9–26,054,900.4) | 1638 (1401.6–1919.3) | 0.98 (0.85–1.1) |
| High SDI | 6,429,788.8 (5,347,783.1–7,673,702.3) | 788.6 (661.2–944.7) | 9,921,037.9 (8,203,301.8–11,768,169.2) | 923.1 (765.9–1105.5) | 0.2 (0.08–0.33) |
| Region | |||||
| Central Asia | 745,903.7 (702,157.8–794,880.2) | 849.7 (789.3–920) | 825,914 (754,870–909,758.1) | 874.5 (799.9–962.6) | −0.07 (−0.15–0) |
| Central Europe | 760,858.2 (641,646.6–908,940.9) | 718.7 (621.9–839.5) | 826,696.3 (689,623.4–991,992.1) | 858 (734.7–1012) | 0.53 (0.45–0.61) |
| Eastern Europe | 1,514,453.3 (1,325,633.1–1,750,709.8) | 795.2 (708.8–899.2) | 1,374,636.6 (1,171,915.8–1,626,208.8) | 866.9 (764.9–997.1) | 0.04 (−0.06–0.14) |
| Australasia | 86,161.7 (71,127.9–102,835.3) | 457.8 (384.1–541.3) | 147,972.6 (123,728.6–176,502.4) | 522.9 (444.9–618.2) | 0.41 (0.32–0.51) |
| High-income Asia Pacific | 1,021,487.4 (853,742.1–1,224,002.9) | 664.5 (571.2–779.4) | 1,218,063 (1,003,598.5–1,453,380.1) | 716.6 (607.3–850) | −0.15 (−0.31–0.01) |
| High-income North America | 1,747,931 (1,392,721.8–2,150,830.2) | 603.5 (481.9–748.9) | 2,819,995.5 (2,271,045.4–3,422,009.3) | 699.6 (558.7–863.1) | −0.09 (−0.27–0.1) |
| Southern Latin America | 338,303.3 (293,896.6–390,650.5) | 688.6 (596.8–795.6) | 564,920.9 (477,318.1–666,322.6) | 840.5 (715.9–985.5) | 0.29 (0.06–0.52) |
| Western Europe | 3,851,175.4 (3,163,177.4–4,659,506) | 983.4 (811.4–1201) | 5,681,745.9 (4,686,331.5–6,704,396.3) | 1167.2 (959.1–1407.5) | 0.39 (0.26–0.52) |
| Andean Latin America | 240,068.3 (218,594.8–261,646.9) | 652.1 (583.5–720) | 355,853.7 (318,216.1–396,580.6) | 573.8 (513.2–638.7) | −0.92 (−1.08–0.75) |
| Caribbean | 325,151.1 (298,094.6–356,433.9) | 887.2 (805.6–976.6) | 390,393.7 (347,659.3–436,540.6) | 873.3 (785.8–970.6) | −0.32 (−0.41–0.23) |
| Central Latin America | 2,025,781.6 (1,806,272–2,281,193.9) | 1296.3 (1134.6–1475) | 2,681,644.3 (2,293,249.8–3,139,277.2) | 1102.6 (948.2–1282.6) | −0.84 (−1.14–0.55) |
| Tropical Latin America | 1,159,104.5 (1,044,944.5–1,292,708.6) | 769.7 (687.3–864.7) | 1,415,034.7 (1,225,954.6–1,634,539.4) | 694.2 (613.7–790) | −0.76 (−0.9–0.63) |
| North Africa and Middle East | 5,892,716.2 (5,553,048.4–6,340,665.1) | 1298 (1199.3–1424.7) | 8,814,709.6 (7,949,141.2–9,906,526.1) | 1477.4 (1335.7–1649.6) | 0.23 (0.12–0.34) |
| South Asia | 43,696,425.7 (40,926,199.5–47,183,646.5) | 3125 (2874.5–3435.9) | 57,490,327.3 (50,908,475.1–65,795,679.3) | 3316.7 (2961.3–3752.9) | −0.27 (−0.4–0.13) |
| East Asia | 14,029,975.9 (11,926,576.9–16,629,041.4) | 1190 (1013–1403.5) | 26,118,724.4 (21,263,244.6–31,657,526) | 1731.3 (1425.6–2098) | 1.05 (0.91–1.19) |
| Oceania | 147,114.8 (139,460.9–155,676) | 1817.8 (1690.5–1947.6) | 283,672.2 (266,582.1–302,257.4) | 1780.8 (1647.1–1922.7) | −0.18 (−0.3–0.06) |
| Southeast Asia | 12,093,977.1 (11,147,165.8–13,222,689.6) | 2450.7 (2227.3–2707.1) | 16,142,385.4 (14,315,450.9–18,265,959.5) | 2563.6 (2297.1–2876.1) | −0.07 (−0.17–0.03) |
| Central Sub-Saharan Africa | 1,332,271.9 (1,282,265.5–1,387,876.2) | 1514.5 (1434.8–1600.2) | 2,394,812.8 (2,282,754.9–2,514,402.1) | 1355.2 (1274.6–1440.8) | −0.54 (−0.65–0.44) |
| Eastern Sub-Saharan Africa | 4,387,305.3 (4,215,311.8–4,574,173) | 1621.8 (1513.8–1740) | 7,009,047.6 (6,721,523.8–7,341,028.7) | 1347.4 (1266–1438.5) | −0.84 (−0.91–0.76) |
| Southern Sub-Saharan Africa | 647,947.4 (603,654.8–699,495) | 1098.7 (1006.1–1202.6) | 789,790.3 (724,192.5–864,048) | 1012.4 (925.9–1107.4) | −0.59 (−0.71–0.47) |
| Western Sub-Saharan Africa | 4,933,217.4 (4,750,330.9–5,167,049) | 1695.9 (1592.7–1819) | 10,326,417 (9,839,148.9–10,911,512.6) | 1690.4 (1572.9–1821.5) | −0.12 (−0.24–0.01) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zhang, X.; Zhang, L.; Pu, Y.; Sun, M.; Zhao, Y.; Zhang, D.; Wang, X.; Li, Y.; Guo, D.; He, S. Global, Regional, and National Burden of Protein–Energy Malnutrition: A Systematic Analysis for the Global Burden of Disease Study. Nutrients 2022, 14, 2592. https://doi.org/10.3390/nu14132592
Zhang X, Zhang L, Pu Y, Sun M, Zhao Y, Zhang D, Wang X, Li Y, Guo D, He S. Global, Regional, and National Burden of Protein–Energy Malnutrition: A Systematic Analysis for the Global Burden of Disease Study. Nutrients. 2022; 14(13):2592. https://doi.org/10.3390/nu14132592
Chicago/Turabian StyleZhang, Xu, Lu Zhang, Yuanchun Pu, Min Sun, Yan Zhao, Dan Zhang, Xin Wang, Yarui Li, Dan Guo, and Shuixiang He. 2022. "Global, Regional, and National Burden of Protein–Energy Malnutrition: A Systematic Analysis for the Global Burden of Disease Study" Nutrients 14, no. 13: 2592. https://doi.org/10.3390/nu14132592
APA StyleZhang, X., Zhang, L., Pu, Y., Sun, M., Zhao, Y., Zhang, D., Wang, X., Li, Y., Guo, D., & He, S. (2022). Global, Regional, and National Burden of Protein–Energy Malnutrition: A Systematic Analysis for the Global Burden of Disease Study. Nutrients, 14(13), 2592. https://doi.org/10.3390/nu14132592






