Increasing Access to Healthy Foods through Improving Food Environment: A Review of Mixed Methods Intervention Studies with Residents of Low-Income Communities
Abstract
:1. Introduction
2. Materials and Methods
3. Food Insecurity and Risk for Diet-Related Chronic Disease
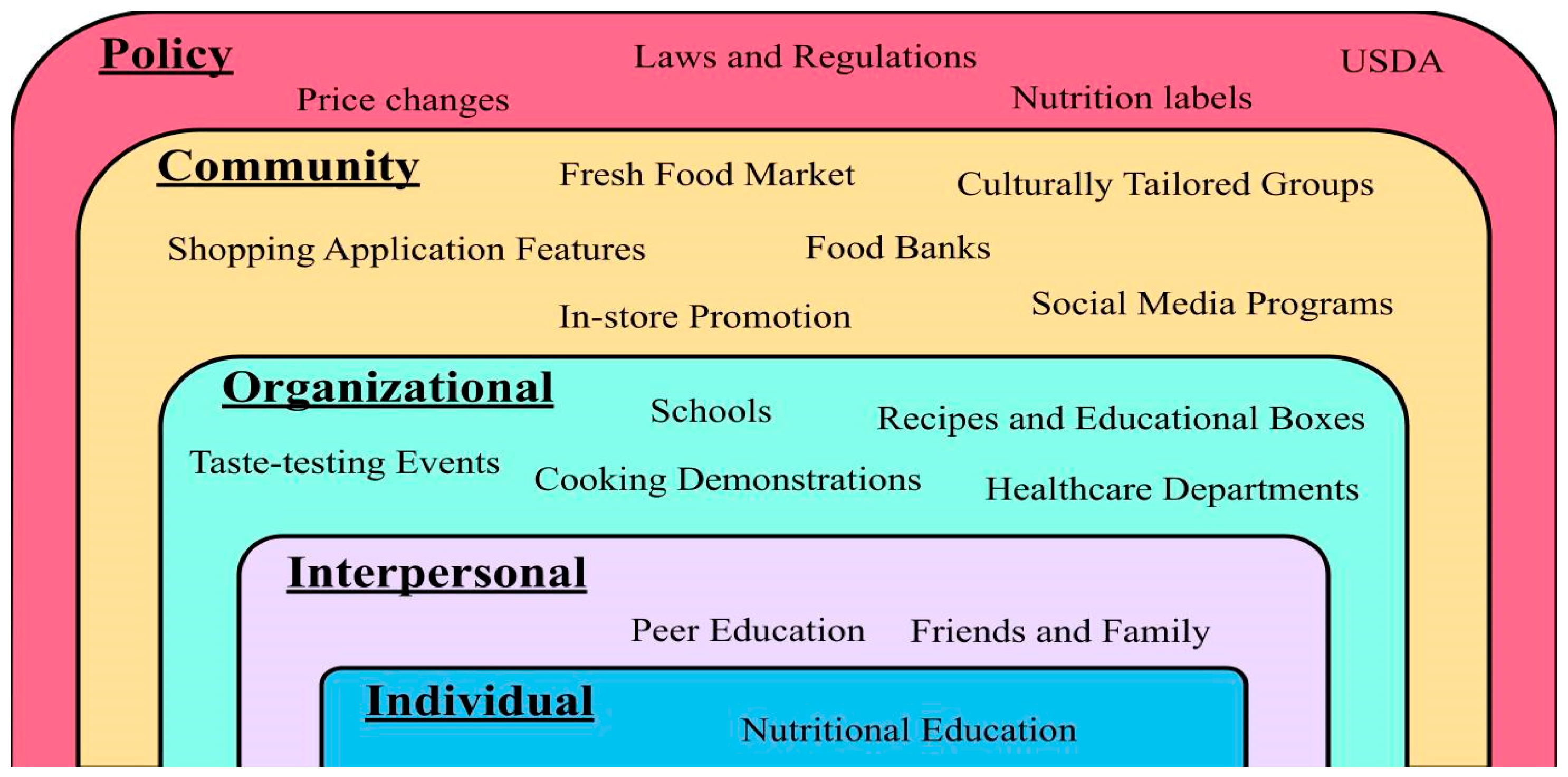
3.1. Obesity
3.2. Cardiovascular Diseases
3.3. Diabetes Mellitus
4. The Impact of Food Environment on Access to Healthy Food Choices
5. Environmental Approaches to Improve Food Security and Nutritional Status: Multilevel Intervention Studies with Residents of Low-Income Communities
5.1. Individual Nutrition Education and Peer Education
5.2. Community-Based Participatory Research
| Author | Type of Study | Target Population | Sample Size | Type of Approach | Outcome Measure | Results |
|---|---|---|---|---|---|---|
| Gans. et al. [37] | RCT | Western adults | 1587 | Individual, community, policy Changes | Fruit and vegetable consumption measured by National Cancer Institute’s “Eating at America’s Table All Day Screener” | -↑ total intake F & V by 0.44 c/day with the control group ↓ by 0.08 c/day (p < 0.02). -↑ F&V frequency (p = 0.01) |
| Trude. et al. [40] | RCT | Obese children (9–15 years old) in 30 areas of Baltimore. | 401 | Individual, interpersonal, organizational, community, policy | -Purchase and consumption of low-sugar foods and beverages. | -↑ healthier purchases by 1.4 more items per week compared to the control group. -There was a 3.5% ↓ in kcal from sweets for older intervention youths. |
| Weber. et al. [44] | Review and analysis of features | WIC participants | 17 app features | Organizational and community | -Reviewing app stores and their benefits to users. | App features were classified into categories for shopping management, WIC required nutrition education modules and others. The app was rated with 4–5/5 stars |
| White et al. [52] | Multicenter randomized intervention trial | Children | 53 | Community and policy | -Increasing food access based on availability, accessibility, affordability, acceptability, and accommodation. | Availability was enhanced for those who could select their own produce items. Flexible pick-up times and locations. ↑ access to F&V. |
| McGuirt et al. [54] | Qualitative Study | Women of child-bearing age | 37 | Individual, organizational, and policy | -Examine willingness to shop at farmers’ markets. | More likely to shop at farmers’ market when price saving ↑ at least 20%. |
5.3. Policy Changes in Supplemental Nutrition Programs
6. Discussion and Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Anderson, S.A. Core Indicators of Nutritional State for Difficult-to-Sample Populations. J. Nutr. 1990, 120 (Suppl. 11), 1555–1600. [Google Scholar] [CrossRef] [PubMed]
- The Prevalence of Food Insecurity in 2020 is Unchanged from 2019. Available online: http://www.ers.usda.gov/data-products/chart-gallery/gallery/chart-detail/?chartId=58378 (accessed on 9 February 2022).
- Robaina, K.A.; Martin, K.S. Food Insecurity, Poor Diet Quality, and Obesity among Food Pantry Participants in Hartford, CT. J. Nutr. Educ. Behav. 2013, 45, 159–164. [Google Scholar] [CrossRef] [PubMed]
- Drewnowski, A.; Specter, S.E. Poverty and obesity: The role of energy density and energy costs. Am. J. Clin. Nutr. 2004, 79, 6–16. [Google Scholar] [CrossRef] [PubMed]
- Champagne, C.M.; Casey, P.H.; Connell, C.L.; Stuff, J.E.; Gossett, J.M.; Harsha, D.W.; McCabe-Sellers, B.; Robbins, J.; Simpson, P.M.; Weber, J.L.; et al. Poverty and Food Intake in Rural America: Diet Quality Is Lower in Food Insecure Adults in the Mississippi Delta. J. Am. Diet. Assoc. 2007, 107, 1886–1894. [Google Scholar] [CrossRef] [PubMed]
- Kendall, A.; Olson, C.M.; Frongillo, E.A. Relationship of Hunger and Food Insecurity to Food Availability and Consumption. J. Am. Diet. Assoc. 1996, 96, 1019–1024. [Google Scholar] [CrossRef]
- Belon, A.P.; Nieuwendyk, L.M.; Vallianatos, H.; Nykiforuk, C.I. Perceived community environmental influences on eating behaviors: A Photovoice analysis. Soc. Sci. Med. 2016, 171, 18–29. [Google Scholar] [CrossRef] [Green Version]
- Drewnowski, A.; Darmon, N. Food Choices and Diet Costs: An Economic Analysis. J. Nutr. 2005, 135, 900–904. [Google Scholar] [CrossRef]
- Paeratakul, S.; Lovejoy, J.; Ryan, D.; Bray, G. The relation of gender, race and socioeconomic status to obesity and obesity comorbidities in a sample of US adults. Int. J. Obes. 2002, 26, 1205–1210. [Google Scholar] [CrossRef] [Green Version]
- Moradi, S.; Mirzababaei, A.; Dadfarma, A.; Rezaei, S.; Mohammadi, H.; Jannat, B.; Mirzaei, K. Food insecurity and adult weight abnormality risk: A systematic review and meta-analysis. Eur. J. Nutr. 2019, 58, 45–61. [Google Scholar] [CrossRef]
- Duffy, P.; Zizza, C.; Jacoby, J.; Tayie, F.A. Diet Quality is Low among Female Food Pantry Clients in Eastern Alabama. J. Nutr. Educ. Behav. 2009, 41, 414–419. [Google Scholar] [CrossRef]
- Kaur, J.; Lamb, M.M.; Ogden, C.L. The Association between Food Insecurity and Obesity in Children—The National Health and Nutrition Examination Survey. J. Acad. Nutr. Diet. 2015, 115, 751–758. [Google Scholar] [CrossRef]
- Walker, R.J.; Grusnick, J.; Garacci, E.; Mendez, C.; Egede, L.E. Trends in Food Insecurity in the USA for Individuals with Prediabetes, Undiagnosed Diabetes, and Diagnosed Diabetes. J. Gen. Intern. Med. 2018, 34, 33–35. [Google Scholar] [CrossRef] [Green Version]
- Dammann, K.W.; Smith, C. Factors Affecting Low-income Women’s Food Choices and the Perceived Impact of Dietary Intake and Socioeconomic Status on Their Health and Weight. J. Nutr. Educ. Behav. 2009, 41, 242–253. [Google Scholar] [CrossRef]
- Jung, S.E.; Shin, Y.H.; Kim, S.; Hermann, J.; Bice, C. Identifying Underlying Beliefs About Fruit and Vegetable Consumption Among Low-Income Older Adults: An Elicitation Study Based on the Theory of Planned Behavior. J. Nutr. Educ. Behav. 2017, 49, 717–723. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.; Chang, Y.; Cho, J.; Hong, Y.S.; Zhao, D.; Kang, J.; Jung, H.-S.; Yun, K.E.; Guallar, E.; Ryu, S.; et al. Life’s Simple 7 Cardiovascular Health Metrics and Progression of Coronary Artery Calcium in a Low-Risk Population. Arter. Thromb. Vasc. Biol. 2019, 39, 826–833. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Leung, C.; Tester, J.; Laraia, B. Household Food Insecurity and Ideal Cardiovascular Health Factors in US Adults. JAMA Intern. Med. 2017, 177, 730–732. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Marmash, D.; Ha, K.; Sakaki, J.R.; Gorski, I.; Rule, B.; Puglisi, M.; Chun, O.K. The Association between Diet Quality and Health Status in Mobile Food Pantry Users in Northeastern Connecticut. Nutrients 2022, 14, 1302. [Google Scholar] [CrossRef] [PubMed]
- Seligman, H.K.; Laraia, B.A.; Kushel, M.B. Food Insecurity Is Associated with Chronic Disease among Low-Income NHANES Participants. J. Nutr. 2009, 140, 304–310. [Google Scholar] [CrossRef] [Green Version]
- Beltrán, S.; Pharel, M.; Montgomery, C.T.; López-Hinojosa, I.J.; Arenas, D.J.; Delisser, H.M. Food insecurity and hypertension: A systematic review and meta-analysis. PLoS ONE 2020, 15, e0241628. [Google Scholar] [CrossRef]
- Thomas, M.K.; Lammert, L.J.; Beverly, E.A. Food Insecurity and its Impact on Body Weight, Type 2 Diabetes, Cardiovascular Disease, and Mental Health. Curr. Cardiovasc. Risk Rep. 2021, 15, 15. [Google Scholar] [CrossRef]
- Liu, Y.; Eicher-Miller, H.A. Food Insecurity and Cardiovascular Disease Risk. Curr. Atheroscler. Rep. 2021, 23, 24. [Google Scholar] [CrossRef] [PubMed]
- Sun, Y.; Liu, B.; Rong, S.; Du, Y.; Xu, G.; Snetselaar, L.G.; Wallace, R.B.; Bao, W. Food Insecurity Is Associated with Cardiovascular and All-Cause Mortality Among Adults in the United States. J. Am. Heart Assoc. 2020, 9, e014629. [Google Scholar] [CrossRef] [PubMed]
- Bazzano, L.A.; He, J.; Ogden, L.G.; Loria, C.M.; Vupputuri, S.; Myers, L.; Whelton, P.K. Fruit and vegetable intake and risk of cardiovascular disease in US adults: The first National Health and Nutrition Examination Survey Epidemiologic Follow-up Study. Am. J. Clin. Nutr. 2002, 76, 93–99. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Haynes-Maslow, L.; Parsons, S.E.; Wheeler, S.B.; Leone, L.A. A Qualitative Study of Perceived Barriers to Fruit and Vegetable Consumption Among Low-Income Populations, North Carolina, 2011. Prev. Chronic Dis. 2013, 10, E34. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wright, L.; Stallings-Smith, S.; Arikawa, A.Y. Associations between food insecurity and prediabetes in a representative sample of U.S. Adults (NHANES 2005–2014). Diabetes Res. Clin. Pract. 2018, 148, 130–136. [Google Scholar] [CrossRef]
- Ippolito, M.M.; Lyles, C.R.; Prendergast, K.; Marshall, M.B.; Waxman, E.; Seligman, H.K. Food insecurity and diabetes self-management among food pantry clients. Public Health Nutr. 2016, 20, 183–189. [Google Scholar] [CrossRef] [Green Version]
- Urbszat, D.; Herman, C.P.; Polivy, J. Eat, drink, and be merry, for tomorrow we diet: Effects of anticipated deprivation on food intake in restrained and unrestrained eaters. J. Abnorm. Psychol. 2002, 111, 396–401. [Google Scholar] [CrossRef]
- Duska, F.; Andel, M.; Kubena, A.; Macdonald, I. Effects of acute starvation on insulin resistance in obese patients with and without type 2 diabetes mellitus. Clin. Nutr. 2005, 24, 1056–1064. [Google Scholar] [CrossRef]
- Abdurahman, A.A.; Chaka, E.E.; Nedjat, S.; Dorosty, A.R.; Majdzadeh, R. The association of household food insecurity with the risk of type 2 diabetes mellitus in adults: A systematic review and meta-analysis. Eur. J. Nutr. 2018, 58, 1341–1350. [Google Scholar] [CrossRef]
- Beltrán, S.; Arenas, D.J.; Pharel, M.; Montgomery, C.; Lopez-Hinojosa, I.; DeLisser, H.M. Food insecurity, type 2 diabetes, and hyperglycaemia: A systematic review and meta-analysis. Endocrinol. Diabetes Metab. 2021, 5, e00315. [Google Scholar] [CrossRef]
- Liese, A.D.; Weis, K.E.; Pluto, D.; Smith, E.; Lawson, A. Food Store Types, Availability, and Cost of Foods in a Rural Environment. J. Am. Diet. Assoc. 2007, 107, 1916–1923. [Google Scholar] [CrossRef] [PubMed]
- Algert, S.J.; Agrawal, A.; Lewis, D.S. Disparities in Access to Fresh Produce in Low-Income Neighborhoods in Los Angeles. Am. J. Prev. Med. 2006, 30, 365–370. [Google Scholar] [CrossRef] [PubMed]
- Martin, K.S.; Havens, E.; Boyle, K.E.; Matthews, G.; Schilling, E.A.; Harel, O.; Ferris, A.M. If you stock it, will they buy it? Healthy food availability and customer purchasing behaviour within corner stores in Hartford, CT, USA. Public Health Nutr. 2012, 15, 1973–1978. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Monsivais, P.; Drewnowski, A. The Rising Cost of Low-Energy-Density Foods. J. Am. Diet. Assoc. 2007, 107, 2071–2076. [Google Scholar] [CrossRef]
- Social Ecological Model. CDC-Social Ecological Model-CRCCP. (27 October 2015). Available online: http://medbox.iiab.me/modules/encdc/www.cdc.gov/cancer/crccp/sem.htm#:~:text=CDC%20adapted%20the%20social%20ecological,five%20bands%20represents%20the%20SEM (accessed on 27 May 2022).
- Gans, K.M.; Risica, P.M.; Keita, A.D.; Dionne, L.; Mello, J.; Stowers, K.C.; Papandonatos, G.; Whittaker, S.; Gorham, G. Multilevel approaches to increase fruit and vegetable intake in low-income housing communities: Final results of the ‘Live Well, Viva Bien’ cluster-randomized trial. Int. J. Behav. Nutr. Phys. Act. 2018, 15, 80. [Google Scholar] [CrossRef] [Green Version]
- Hammons, A.J.; Hannon, B.; Teran-Garcia, M.; Barragan, M.; Villegas, E.; Wiley, A.; Fiese, B. Effects of Culturally Tailored Nutrition Education on Dietary Quality of Hispanic Mothers: A Randomized Control Trial. J. Nutr. Educ. Behav. 2019, 51, 1168–1176. [Google Scholar] [CrossRef] [Green Version]
- Flynn, M.M.; Reinert, S.; Schiff, A.R. A Six-Week Cooking Program of Plant-Based Recipes Improves Food Security, Body Weight, and Food Purchases for Food Pantry Clients. J. Hunger Environ. Nutr. 2013, 8, 73–84. [Google Scholar] [CrossRef]
- Trude, A.C.B.; Surkan, P.J.; Cheskin, L.J.; Gittelsohn, J. A multilevel, multicomponent childhood obesity prevention group-randomized controlled trial improves healthier food purchasing and reduces sweet-snack consumption among low-income African-American youth. Nutr. J. 2018, 17, 96. [Google Scholar] [CrossRef] [Green Version]
- Hoelscher, D.M.; Springer, A.E.; Ranjit, N.; Perry, C.L.; Evans, A.E.; Stigler, M.; Kelder, S.H. Reductions in Child Obesity Among Disadvantaged School Children with Community Involvement: The Travis County CATCH Trial. Obesity 2010, 18 (Suppl. 1), S36–S44. [Google Scholar] [CrossRef]
- Wetherill, M.S.; White, K.C.; Seligman, H.K. Nutrition-Focused Food Banking in the United States: A Qualitative Study of Healthy Food Distribution Initiatives. J. Acad. Nutr. Diet. 2019, 119, 1653–1665. [Google Scholar] [CrossRef]
- Rustad, C.; Smith, C. Nutrition Knowledge and Associated Behavior Changes in a Holistic, Short-term Nutrition Education Intervention with Low-income Women. J. Nutr. Educ. Behav. 2013, 45, 490–498. [Google Scholar] [CrossRef] [PubMed]
- Weber, S.J.; Dawson, D.; Greene, H.; Hull, P.C. Mobile Phone Apps for Low-Income Participants in a Public Health Nutrition Program for Women, Infants, and Children (WIC): Review and Analysis of Features. JMIR mHealth uHealth 2018, 6, e12261. [Google Scholar] [CrossRef] [PubMed]
- Marmash, D.; Ha, K.; Sakaki, J.R.; Hair, R.; Morales, E.; Duffy, V.B.; Puglisi, M.; Chun, O.K. A Feasibility and Pilot Study of a Personalized Nutrition Intervention in Mobile Food Pantry Users in Northeastern Connecticut. Nutrients 2021, 13, 2939. [Google Scholar] [CrossRef] [PubMed]
- Ayala, G.X.; Baquero, B.; Laraia, B.A.; Ji, M.; Linnan, L. Efficacy of a store-based environmental change intervention compared with a delayed treatment control condition on store customers’ intake of fruits and vegetables. Public Health Nutr. 2013, 16, 1953–1960. [Google Scholar] [CrossRef]
- Gatto, N.; Martinez, L.; Spruijt-Metz, D.; Davis, J. LA sprouts randomized controlled nutrition, cooking and gardening programme reduces obesity and metabolic risk in Hispanic/Latino youth. Pediatr. Obes. 2016, 12, 28–37. [Google Scholar] [CrossRef] [Green Version]
- Flores-Luevano, S.; Pacheco, M.; Shokar, G.S.; Dwivedi, A.K.; Shokar, N.K. Impact of a Culturally Tailored Diabetes Education and Empowerment Program in a Mexican American Population Along the US/Mexico Border: A Pragmatic Study. J. Clin. Med. Res. 2020, 12, 517–529. [Google Scholar] [CrossRef]
- Marshall, A.N.; Markham, C.; Ranjit, N.; Bounds, G.; Chow, J.; Sharma, S.V. Long-term impact of a school-based nutrition intervention on home nutrition environment and family fruit and vegetable intake: A two-year follow-up study. Prev. Med. Rep. 2020, 20, 101247. [Google Scholar] [CrossRef]
- What Is CBPR? Detroit Urban Research Center Web Site. Available online: https://www.detroiturc.org/about-cbpr/what-is-cbpr (accessed on 12 January 2022).
- Martinez, L.C.; Gatto, N.M.; Spruijt-Metz, D.; Davis, J.N. Design and methodology of the LA Sprouts nutrition, cooking and gardening program for Latino youth: A randomized controlled intervention. Contemp. Clin. Trials 2015, 42, 219–227. [Google Scholar] [CrossRef] [Green Version]
- White, M.J.; Pitts, S.B.J.; McGuirt, J.T.; Hanson, K.L.; Morgan, E.H.; Kolodinsky, J.; Wang, W.; Sitaker, M.; Ammerman, A.S.; Seguin, R.A. The perceived influence of cost-offset community-supported agriculture on food access among low-income families. Public Health Nutr. 2018, 21, 2866–2874. [Google Scholar] [CrossRef] [Green Version]
- Seguin, R.A.; Morgan, E.H.; Hanson, K.L.; Ammerman, A.S.; Pitts, S.B.J.; Kolodinsky, J.; Sitaker, M.; Becot, F.A.; Connor, L.M.; Garner, J.A.; et al. Farm Fresh Foods for Healthy Kids (F3HK): An innovative community supported agriculture intervention to prevent childhood obesity in low-income families and strengthen local agricultural economies. BMC Public Health 2017, 17, 306. [Google Scholar] [CrossRef] [Green Version]
- McGuirt, J.T.; Pitts, S.B.J.; Ward, R.; Crawford, T.W.; Keyserling, T.C.; Ammerman, A.S. Examining the Influence of Price and Accessibility on Willingness to Shop at Farmers’ Markets Among Low-income Eastern North Carolina Women. J. Nutr. Educ. Behav. 2013, 46, 26–33. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- French, S.A.; Story, M.; Jeffery, R.W.; Snyder, P.; Eisenberg, M.; Sidebottom, A.; Murray, D. Pricing Strategy to Promote Fruit and Vegetable Purchase in High School Cafeterias. J. Am. Diet. Assoc. 1997, 97, 1008–1010. [Google Scholar] [CrossRef]
- Brownson, R.C.; Haire-Joshu, D.; Luke, D.A. Shaping the context of health: A Review of Environmental and Policy Approaches in the Prevention of Chronic Diseases. Annu. Rev. Public Health 2006, 27, 341–370. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bersamin, A.; Izumi, B.T.; Nu, J.; O’Brien, D.; Paschall, M. Strengthening adolescents’ connection to their traditional food system improves diet quality in remote Alaska Native communities: Results from the Neqa Elicarvigmun Pilot Study. Transl. Behav. Med. 2019, 9, 952–961. [Google Scholar] [CrossRef]
- Beresford, S.A.; Thompson, B.; Feng, Z.; Christianson, A.; McLerran, D.; Patrick, D.L. Seattle 5 a Day Worksite Program to Increase Fruit and Vegetable Consumption. Prev. Med. 2001, 32, 230–238. [Google Scholar] [CrossRef]
- French, S.A.; Jeffery, R.W.; Story, M.; Breitlow, K.K.; Baxter, J.S.; Hannan, P.; Snyder, M.P. Pricing and promotion effects on low-fat vending snack purchases: The CHIPS Study. Am. J. Public Health 2001, 91, 112–117. [Google Scholar] [CrossRef] [Green Version]
- Barnes, T.L.; Lenk, K.; Caspi, C.E.; Erickson, D.J.; Laska, M.N. Perceptions of a Healthier Neighborhood Food Environment Linked to Greater Fruit and Vegetable Purchases at Small and Non-Traditional Food Stores. J. Hunger Environ. Nutr. 2018, 14, 741–761. [Google Scholar] [CrossRef]
| Parameter | Criteria | Exclusion |
|---|---|---|
| Search terms included | Food insecurity, chronic disease, multilevel approaches, low-income, food environment. | N/A |
| Criteria for study design | RCT, clinical trials, comparative studies, multicenter studies, cohort studies, qualitative studies, books. | Review articles, notes, comments, editorials. |
| Criteria for subject population | Low-income populations, all age ranges. | Other populations, low-income population not living in US. |
| Criteria for outcomes | Improved dietary behavior, weight status, improved lifestyle, educating the community on healthier choices when on a budget. | N/A |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ziso, D.; Chun, O.K.; Puglisi, M.J. Increasing Access to Healthy Foods through Improving Food Environment: A Review of Mixed Methods Intervention Studies with Residents of Low-Income Communities. Nutrients 2022, 14, 2278. https://doi.org/10.3390/nu14112278
Ziso D, Chun OK, Puglisi MJ. Increasing Access to Healthy Foods through Improving Food Environment: A Review of Mixed Methods Intervention Studies with Residents of Low-Income Communities. Nutrients. 2022; 14(11):2278. https://doi.org/10.3390/nu14112278
Chicago/Turabian StyleZiso, Dea, Ock K. Chun, and Michael J. Puglisi. 2022. "Increasing Access to Healthy Foods through Improving Food Environment: A Review of Mixed Methods Intervention Studies with Residents of Low-Income Communities" Nutrients 14, no. 11: 2278. https://doi.org/10.3390/nu14112278
APA StyleZiso, D., Chun, O. K., & Puglisi, M. J. (2022). Increasing Access to Healthy Foods through Improving Food Environment: A Review of Mixed Methods Intervention Studies with Residents of Low-Income Communities. Nutrients, 14(11), 2278. https://doi.org/10.3390/nu14112278








