Establishing Postnatal Growth Monitoring Curves of Preterm Infants in China: Allowing for Continuous Use from 24 Weeks of Preterm Birth to 50 Weeks
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Data Source
2.2. Process of Establishing Postnatal Growth Monitoring Curves
2.2.1. Selecting Seven Main Percentile Curves
2.2.2. Selecting Age Target Points of Initial Percentile Curves
2.2.3. Obtaining Preliminarily Smoothed Percentile Values
2.2.4. Obtaining Smoothed L, M and S Parameters
2.2.5. Obtaining Standardized Smoothed Percentile Values
2.2.6. Assessing the Fitted Performance of the Standardized Smoothed Percentile Curves
2.3. Fenton 2013 Growth Monitoring Curves and INTERGROWTH Growth Curves
2.4. Statistical Analysis
3. Results
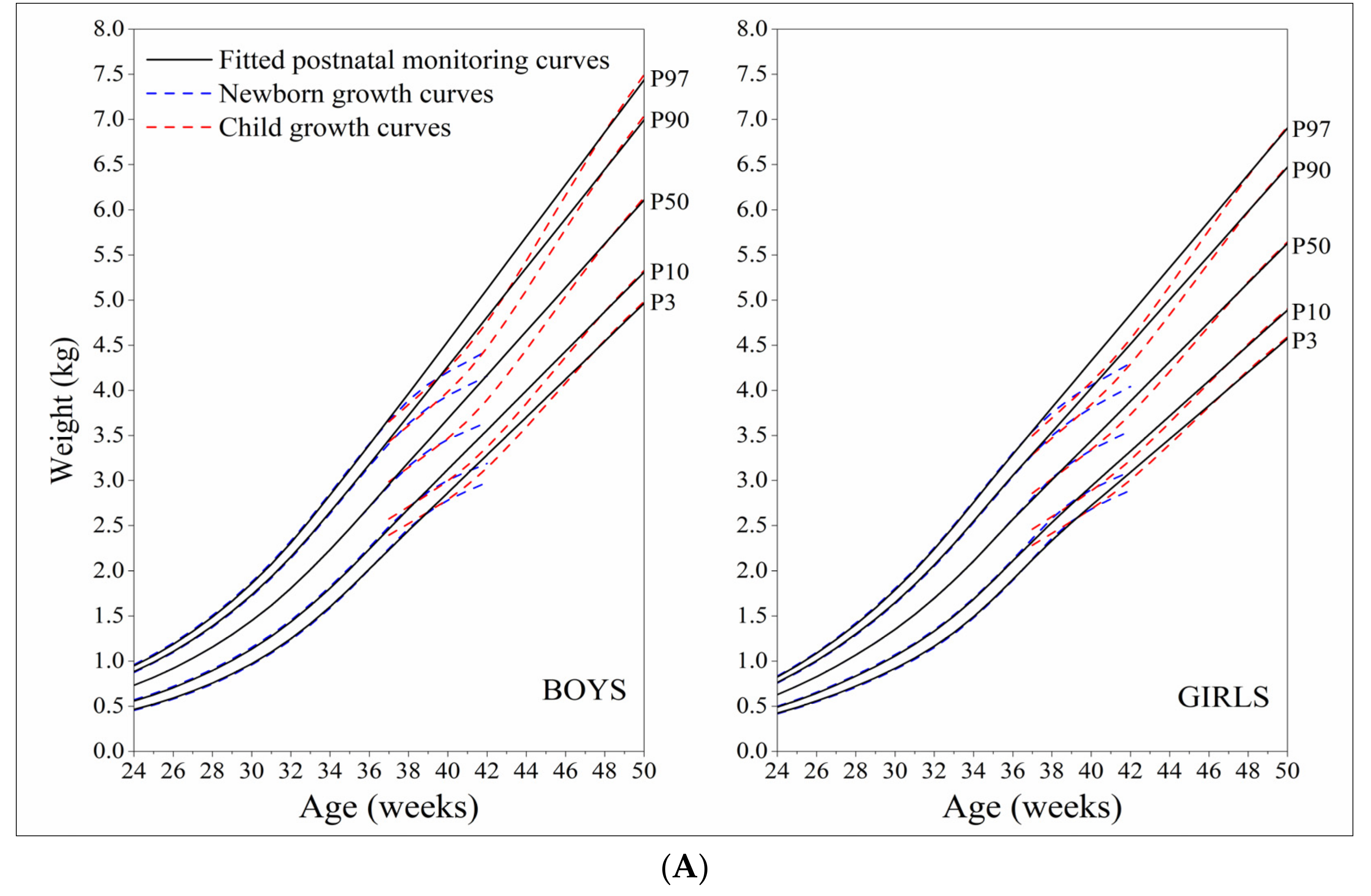
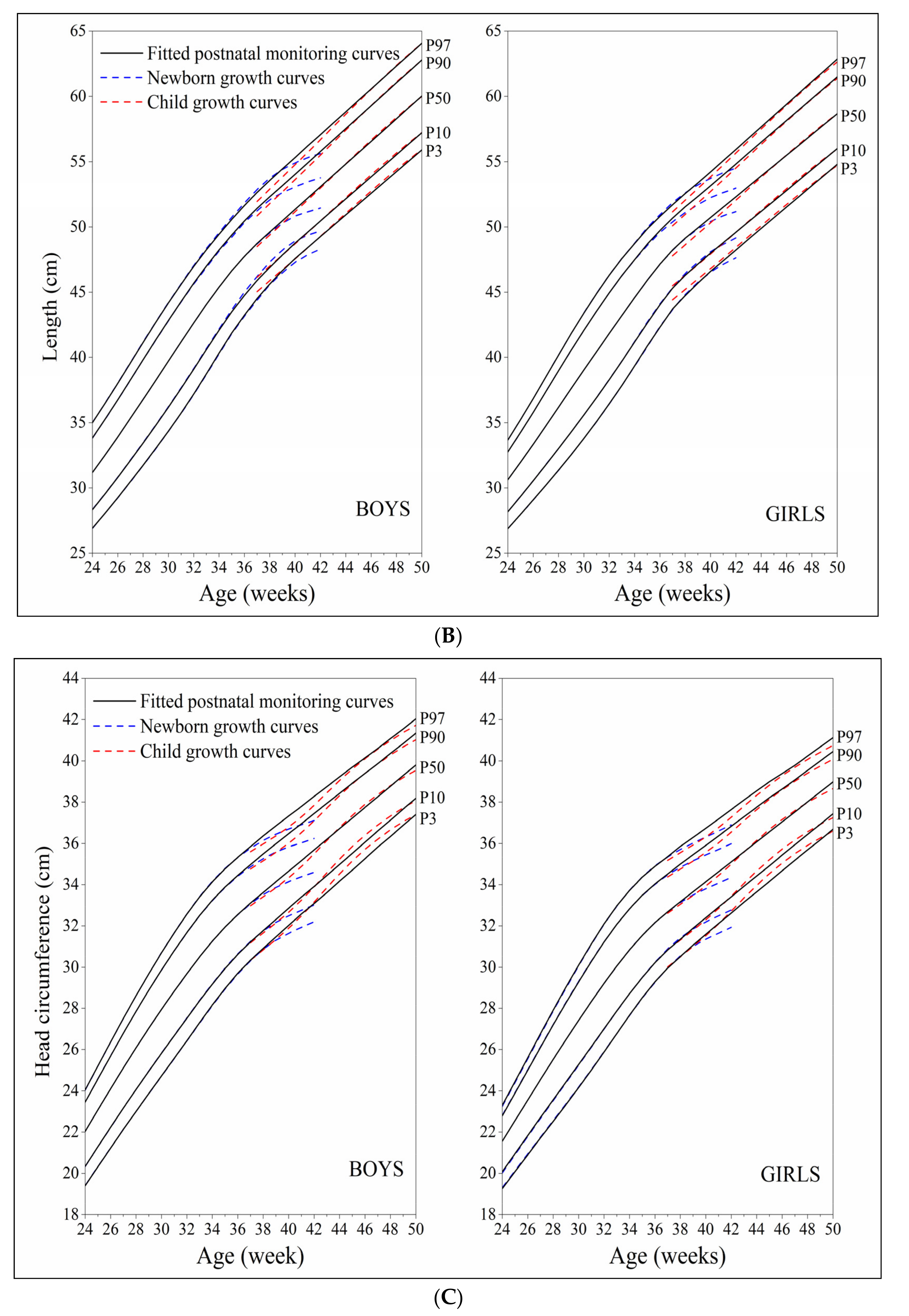
3.1. Established Postnatal Growth Monitoring Curves and their Comparison with Newborn Growth Curves and the Child Growth Curves
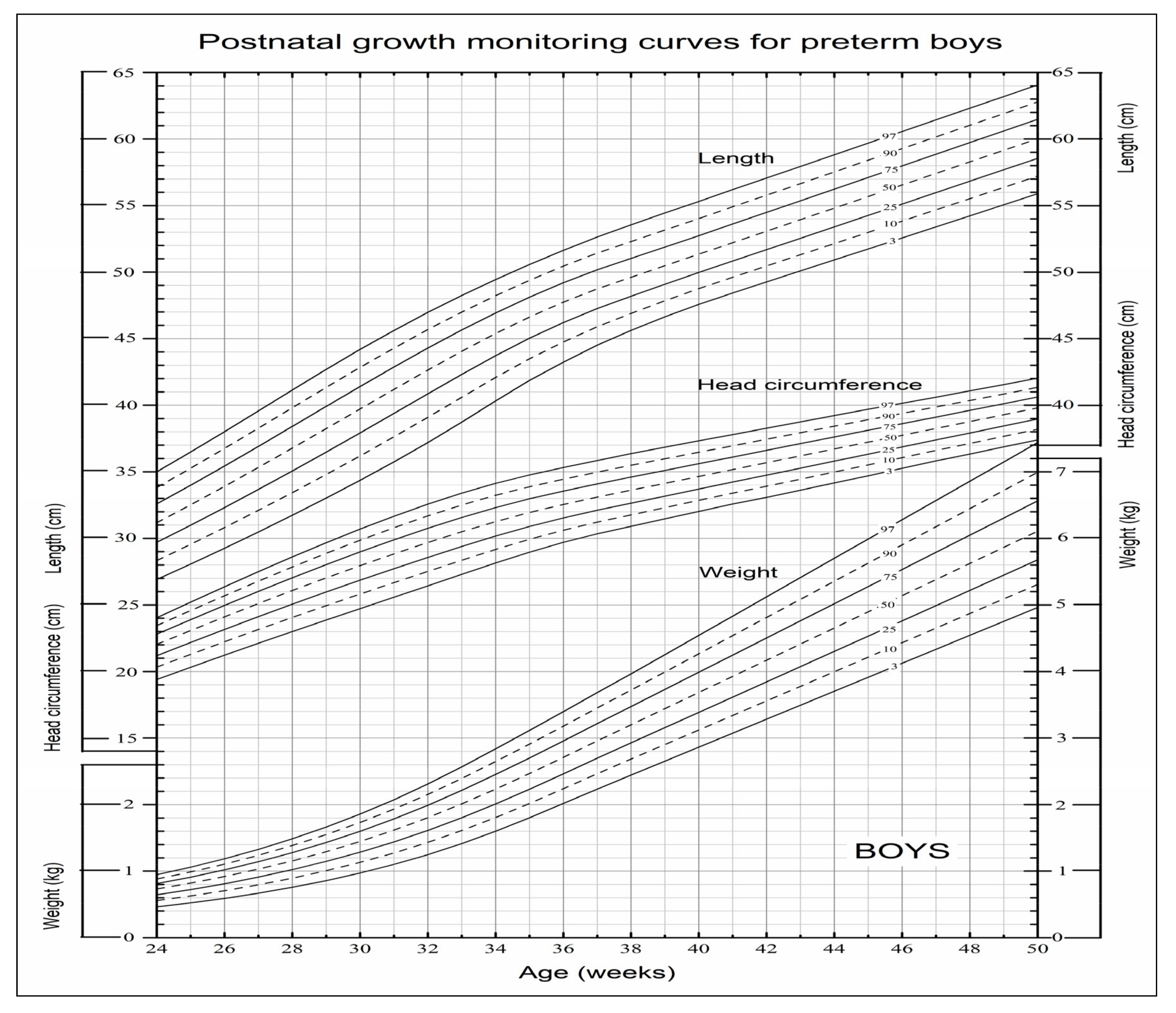
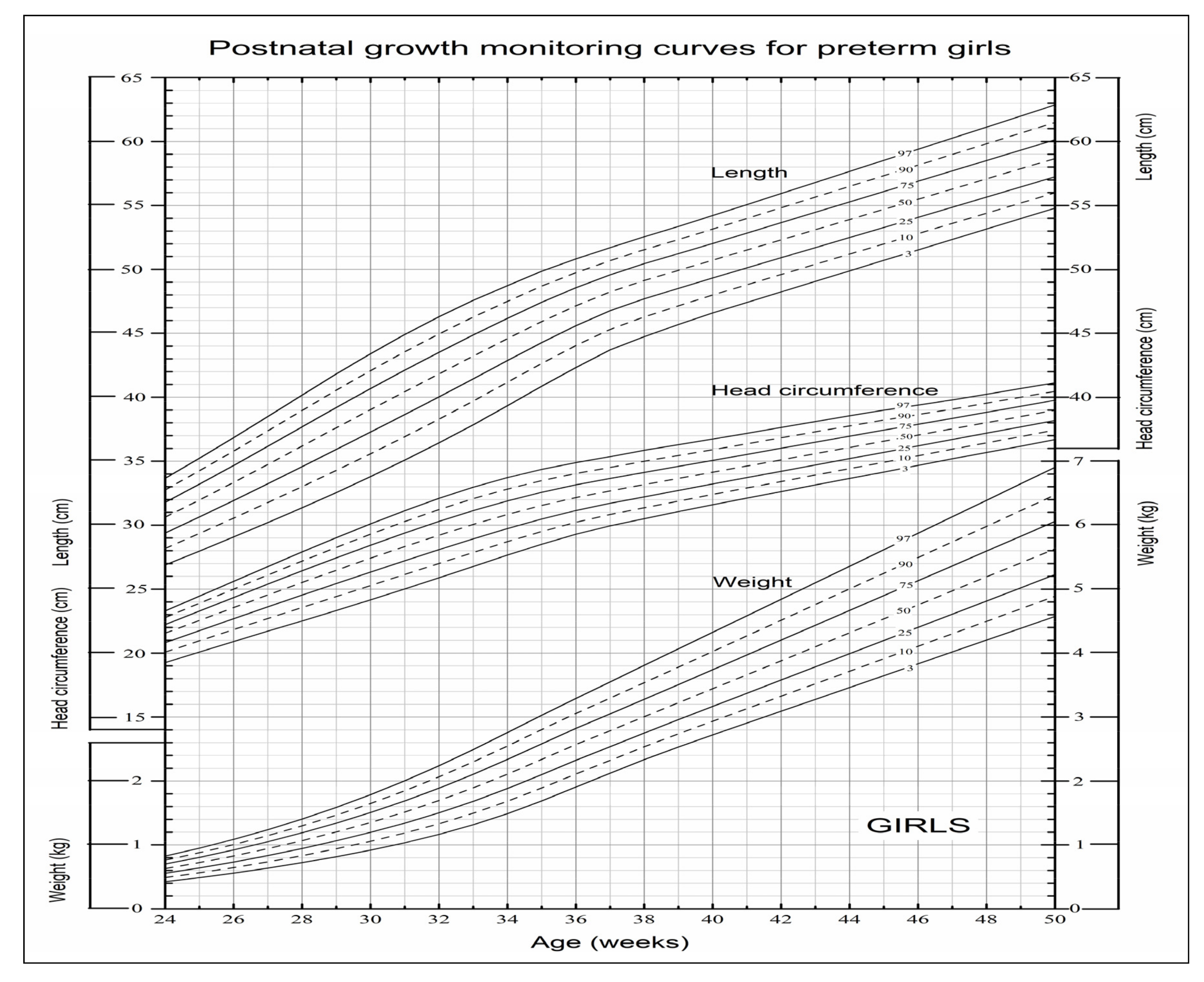
3.2. Postnatal Growth Monitoring Curve Allowing for Continuous Use from 24 Weeks of Preterm Birth to 50 Weeks
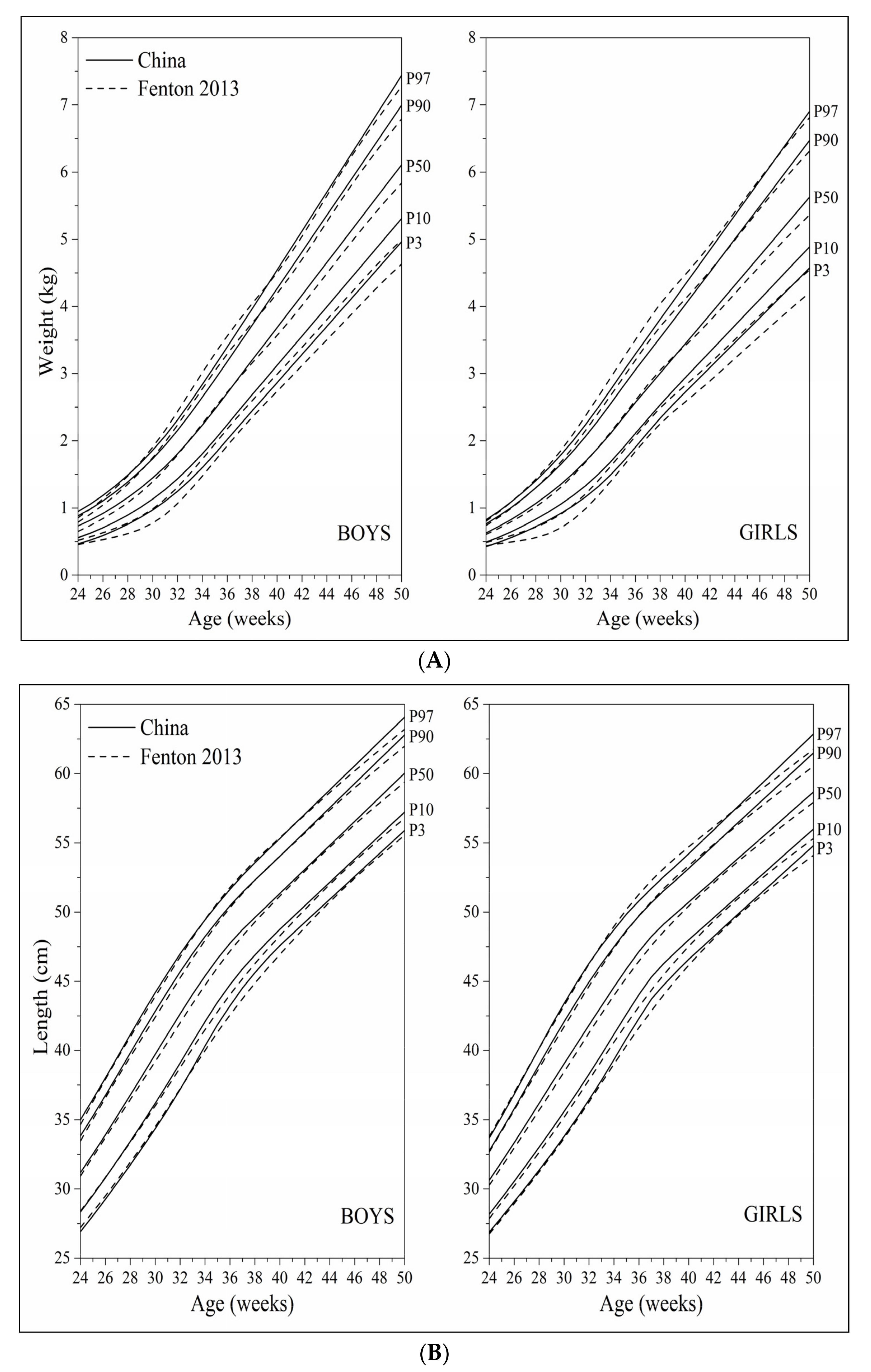
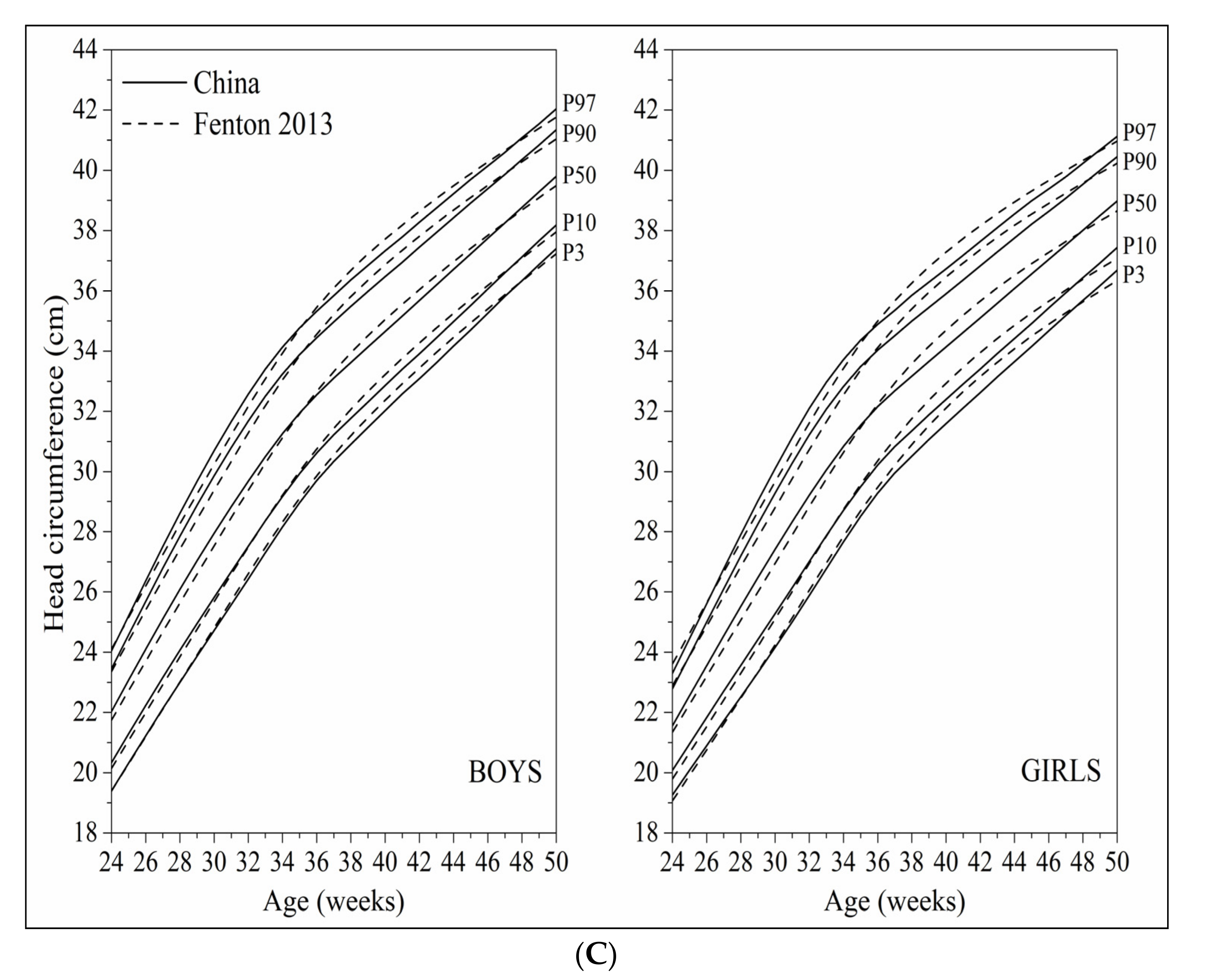
3.3. Comparison of the Established Postnatal Growth Monitoring Curves with the Fenton 2013 Growth Curves
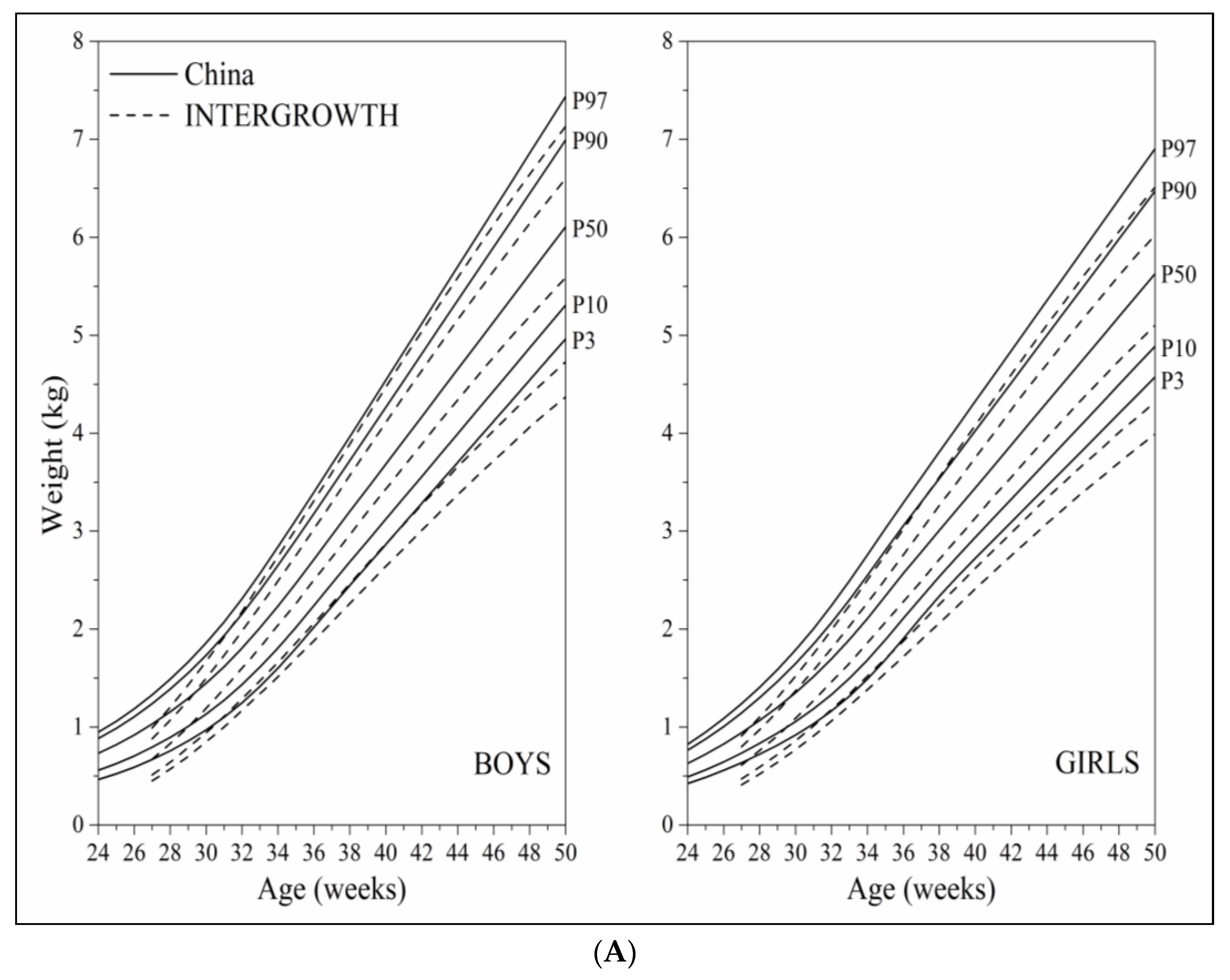
3.4. Comparison of Established Postnatal Growth Monitoring Curves with the INTERGROWTH Growth Curves
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Fenton, T.R.; Kim, J.H. A systematic review and meta-analysis to revise the Fenton growth chart for preterm infants. BMC Pediatr. 2013, 13, 59. [Google Scholar] [CrossRef] [Green Version]
- Villar, J.; Giuliani, F.; Bhutta, Z.A.; Bertino, E.; Ohuma, E.O.; Ismail, L.C.; Barros, F.C.; Altman, D.G.; Victora, C.; Noble, J.A.; et al. Postnatal growth standards for preterm infants: The Preterm Postnatal Follow-up Study of the INTERGROWTH-21(st) Project. Lancet Glob. Health 2015, 3, e681–e691. [Google Scholar] [CrossRef] [Green Version]
- Clark, R.H.; Olsen, I.E.; Spitzer, A.R. Assessment of neonatal growth in prematurely born infants. Clin. Perinatol. 2014, 41, 295–307. [Google Scholar] [CrossRef] [PubMed]
- Sankilampi, U. One size may not fit all when it comes to growth references for preterm infants. Acta Paediatr. 2016, 105, 228–229. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Natale, V.; Rajagopalan, A. Worldwide variation in human growth and the World Health Organization growth standards: A systematic review. BMJ Open 2014, 4, e003735. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhang, L.; Li, Y.; Liang, S.; Liu, X.J.; Kang, F.L.; Li, G.M. Postnatal length and weight growth velocities according to Fenton reference and their associated perinatal factors in healthy late preterm infants during birth to term-corrected age: An observational study. Ital. J. Pediatr. 2019, 45, 1. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Song, Q.Y.; Zhao, X.L.; Guo, Y.Q.; Ding, B.L.; Peng, Q.L.; Ma, L.Y. Assessment of growth pattern of preterm infants up to a corrected age of 24 months. Chin. J. Contemp. Pediatr. 2021, 23, 1200–1207. [Google Scholar]
- Fenton, T.R. A new growth chart for preterm babies: Babson and Benda’s chart updated with recent data and a new format. BMC Pediatr. 2003, 3, 13. [Google Scholar] [CrossRef] [Green Version]
- Capital Institute of Pediatrics; Coordinating Study Group of Nine Cities on the Physical Growth and Development of Children. Growth standard curves of birth weight, length and head circumference of Chinese newborns of different gestation. Zhonghua Er Ke Za Zhi 2020, 58, 738–746. [Google Scholar]
- Capital Institute of Pediatrics; Coordinating Study Group of Nine Cities on the Physical Growth and Development of Children. A national survey on physical growth and development of children under seven years of age in nine cities of China in 2015. Zhonghua Er Ke Za Zhi 2018, 56, 192–199. [Google Scholar]
- Zong, X.N.; Li, H. Establishment of growth standards for Chinese newborns by gestational ages: Study design and statistical methods. Chin. J. Evid.-Based Pediatr. 2020, 15, 254–263. [Google Scholar]
- Zong, X.N.; Li, H.; Zhang, Y.Q.; Wu, H.H.; Zhao, G.L.; Working Committee of the China National Newborn Growth Standards Project. Construction of China national newborn growth standards based on a large low-risk sample. Sci. Rep. 2021, 11, 16093. [Google Scholar] [CrossRef]
- Zhang, Y.Q.; Li, H.; Wu, H.H.; Zong, X.N.; Zhu, Z.H.; Pan, Y.; Li, J.; Zheng, X.R.; Wei, M.; Tong, M.L.; et al. The 5th national survey on the physical growth and development of children in the nine cities of China: Anthropometric measurements of Chinese children under 7 years in 2015. Am. J. Phys. Anthropol. 2017, 163, 497–509. [Google Scholar] [CrossRef]
- Kuczmarski, R.J.; Ogden, C.L.; Guo, S.S.; Grummer-Strawn, L.M.; Flegal, K.M.; Mei, Z.; Wei, R.; Curtin, L.R.; Roche, A.F.; Johnson, C.L. 2000 CDC Growth Charts for the United States: Methods and development. Vital Health Stat. 11 2002, 246, 1–190. [Google Scholar]
- Cole, T.J. The British, American NCHS, and Dutch weight standards compared using the LMS method. Am. J. Hum. Biol. 1989, 1, 397–408. [Google Scholar] [CrossRef]
- Cole, T.J. The LMS method for constructing normalized growth standards. Eur. J. Clin. Nutr. 1990, 44, 45–60. [Google Scholar]
- WHO Multicentre Growth Reference Study Group. WHO Child Growth Standards: Length/Height-for-Age, Weight-for-Age, Weight-for-Length, Weight-for-Height and Body Mass Index-for-Age: Methods and Development; World Health Organization: Geneva, Swithzerland, 2006. [Google Scholar]
- Reddy, K.V.; Sharma, D.; Vardhelli, V.; Bashir, T.; Deshbotla, S.K.; Murki, S. Comparison of Fenton 2013 growth curves and Intergrowth-21 growth standards to assess the incidence of intrauterine growth restriction and extrauterine growth restriction in preterm neonates ≤32 weeks. J. Matern. Fetal Neonatal Med. 2021, 34, 2634–2641. [Google Scholar] [CrossRef]
- Tuzun, F.; Yucesoy, E.; Baysal, B.; Kumral, A.; Duman, N.; Ozkan, H. Comparison of INTERGROWTH-21 and Fenton growth standards to assess size at birth and extrauterine growth in very preterm infants. J. Matern. Fetal Neonatal Med. 2018, 31, 2252–2257. [Google Scholar] [CrossRef]
- Kim, Y.J.; Shin, S.H.; Cho, H.; Shin, S.H.; Kim, S.H.; Song, I.G.; Kim, E.K.; Kim, H.S. Extrauterine growth restriction in extremely preterm infants based on the Intergrowth-21st Project Preterm Postnatal Follow-up Study growth charts and the Fenton growth charts. Eur. J. Pediatr. 2021, 180, 817–824. [Google Scholar] [CrossRef]
- Fenton, T.R.; Nasser, R.; Eliasziw, M.; Kim, J.H.; Bilan, D.; Sauve, R. Validating the weight gain of preterm infants between the reference growth curve of the fetus and the term infant. BMC Pediatr. 2013, 13, 92. [Google Scholar] [CrossRef] [Green Version]
- Boghossian, N.S.; Geraci, M.; Edwards, E.M.; Morrow, K.A.; Horbar, J.D. Anthropometric Charts for Infants Born Between 22 and 29 Weeks’ Gestation. Pediatrics 2016, 138, e20161641. [Google Scholar] [CrossRef] [PubMed]
- Giuliani, F.; Cheikh Ismail, L.; Bertino, E.; Bhutta, Z.A.; Ohuma, E.O.; Rovelli, I.; Conde-Agudelo, A.; Villar, J.; Kennedy, S.H. Monitoring postnatal growth of preterm infants: Present and future. Am. J. Clin. Nutr. 2016, 103, 635S–647S. [Google Scholar] [CrossRef] [PubMed] [Green Version]

Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zong, X.; Li, H.; Zhang, Y. Establishing Postnatal Growth Monitoring Curves of Preterm Infants in China: Allowing for Continuous Use from 24 Weeks of Preterm Birth to 50 Weeks. Nutrients 2022, 14, 2232. https://doi.org/10.3390/nu14112232
Zong X, Li H, Zhang Y. Establishing Postnatal Growth Monitoring Curves of Preterm Infants in China: Allowing for Continuous Use from 24 Weeks of Preterm Birth to 50 Weeks. Nutrients. 2022; 14(11):2232. https://doi.org/10.3390/nu14112232
Chicago/Turabian StyleZong, Xin’nan, Hui Li, and Yaqin Zhang. 2022. "Establishing Postnatal Growth Monitoring Curves of Preterm Infants in China: Allowing for Continuous Use from 24 Weeks of Preterm Birth to 50 Weeks" Nutrients 14, no. 11: 2232. https://doi.org/10.3390/nu14112232
APA StyleZong, X., Li, H., & Zhang, Y. (2022). Establishing Postnatal Growth Monitoring Curves of Preterm Infants in China: Allowing for Continuous Use from 24 Weeks of Preterm Birth to 50 Weeks. Nutrients, 14(11), 2232. https://doi.org/10.3390/nu14112232




