Risk of Incident Stroke among Vegetarians Compared to Nonvegetarians: A Systematic Review and Meta-Analysis of Prospective Cohort Studies
Abstract
:1. Introduction
2. Materials and Methods
2.1. Data Sources and Literature Search
2.2. Study Selection and Outcomes
2.3. Data Extraction and Risk of Bias Assessment
2.4. Data Synthesis and Statistical Analyses
2.5. Certainty of Evidence Assessment
3. Results
3.1. Search Results
3.2. Characteristics of Included Studies
3.3. Risk of Bias Assessment
3.4. Vegetarian Diet and Risk of Total Stroke
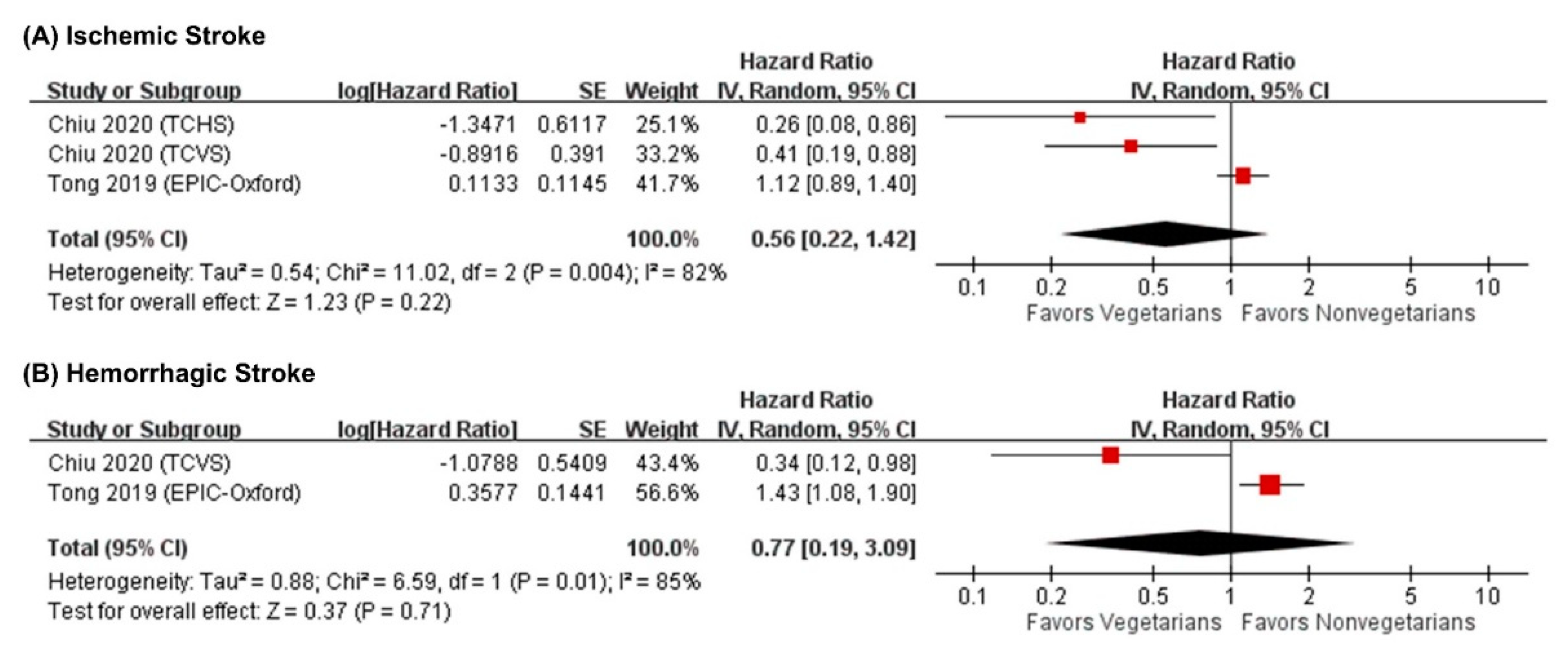
3.5. Vegetarian Diet and Risk of Ischemic and Hemorrhagic Stroke
3.6. Subgroup Analysis
3.7. Sensitivity Analysis and Publication Bias
3.8. Certainty of Evidence
4. Discussion
Strength and Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Sacco, R.L.; Kasner, S.E.; Broderick, J.P.; Caplan, L.R.; Connors, J.J.; Culebras, A.; Elkind, M.S.; George, M.G.; Hamdan, A.D.; Higashida, R.T. An updated definition of stroke for the 21st century: A statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 2013, 44, 2064–2089. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- World Health Organization (WHO). Global Health Estimates 2020: Deaths by Cause, Age, Sex, by Country and by Region, 2000–2019; WHO: Geneva, Switzerland, 2020; Available online: http://who.int/data/gho/data/themes/mortality-and-global-health-estimates/ghe-leading-causes-of-death (accessed on 31 May 2021).
- Ahmad, F.B.; Anderson, R.N. The Leading Causes of Death in the US for 2020. JAMA 2021, 325, 1829–1830. [Google Scholar] [CrossRef]
- Virani, S.S.; Alonso, A.; Aparicio, H.J.; Benjamin, E.J.; Bittencourt, M.S.; Callaway, C.W.; Carson, A.P.; Chamberlain, A.M.; Cheng, S.; Delling, F.N. American Heart Association Council on Epidemiology and Prevention Statistics. Heart disease and stroke statistics-2021 update: A report from the American Heart Association. Circulation 2021, 143, e254–e743. [Google Scholar] [CrossRef]
- GBD 2016 Stroke collaborators. Global, regional, and national burden of stroke, 1990–2016: A systematic analysis for the Global Burden of Disease Study 2016. Lancet Neurol. 2016, 18, 439–458. [Google Scholar]
- Larsson, S.C. Dietary approaches for stroke prevention. Stroke 2017, 48, 2905–2911. [Google Scholar] [CrossRef] [PubMed]
- Larsson, S.C.; Wallin, A.; Wolk, A. Dietary approaches to stop hypertension diet and incidence of stroke: Results from 2 prospective cohorts. Stroke 2016, 47, 986–990. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Springmann, M.; Wiebe, K.; Mason-D’Croz, D.; Sulser, T.B.; Rayner, M.; Scarborough, P. Health and nutritional aspects of sustainable diet strategies and their association with environmental impacts: A global modelling analysis with country-level detail. Lancet Planet. Health 2018, 2, e451–e461. [Google Scholar] [CrossRef] [Green Version]
- Arnett, D.K.; Blumenthal, R.S.; Albert, M.A.; Buroker, A.B.; Goldberger, Z.D.; Hahn, E.J.; Himmelfarb, C.D.; Khera, A.; Lloyd-Jones, D.; McEvoy, J.W. 2019 ACC/AHA guideline on the primary prevention of cardiovascular disease: A report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation 2019, 140, e596–e646. [Google Scholar] [CrossRef] [PubMed]
- Pearson, G.J.; Thanassoulis, G.; Anderson, T.J.; Barry, A.R.; Couture, P.; Dayan, N.; Francis, G.A.; Genest, J.; Grégoire, J.; Grover, S.A. 2021 Canadian Cardiovascular Society guidelines for the management of dyslipidemia for the prevention of cardiovascular disease in the adult. Can. J. Cardiol. 2021, S0828-282X (21)00165-3. [Google Scholar] [CrossRef]
- Campbell, T. A plant-based diet and stroke. J. Geriatr. Cardiol. 2017, 14, 321–326. [Google Scholar] [PubMed]
- Spence, J.D. Diet for stroke prevention. Stroke Vasc. Neurol. 2018, 3, 44–50. [Google Scholar] [CrossRef] [Green Version]
- Aune, D.; Giovannucci, E.; Boffetta, P.; Fadnes, L.T.; Keum, N.; Norat, T.; Greenwood, D.C.; Riboli, E.; Vatten, L.J.; Tonstad, S. Fruit and vegetable intake and the risk of cardiovascular disease, total cancer and all-cause mortality-a systematic review and dose–response meta-analysis of prospective studies. Int. J. Epidemiol. 2017, 46, 1029–1056. [Google Scholar] [CrossRef]
- Baden, M.Y.; Shan, Z.; Wang, F.; Li, Y.; Manson, J.E.; Rimm, E.B.; Willett, W.C.; Hu, F.B.; Rexrode, K.M. Quality of plant-based diet and risk of total, ischemic, and hemorrhagic stroke. Neurology 2021, 96, e1940–e1953. [Google Scholar] [CrossRef] [PubMed]
- Petermann-Rocha, F.; Parra-Soto, S.; Gray, S.; Anderson, J.; Welsh, P.; Gill, J.; Sattar, N.; Ho, F.K.; Celis-Morales, C.; Pell, J.P. Vegetarians, fish, poultry, and meat-eaters: Who has higher risk of cardiovascular disease incidence and mortality? A prospective study from UK Biobank. Eur. Heart J. 2021, 42, 1136–1143. [Google Scholar] [CrossRef] [PubMed]
- Tong, T.; Appleby, P.N.; Bradbury, K.E.; Perez-Cornago, A.; Travis, R.C.; Clarke, R.; Key, T.J. Risks of ischaemic heart disease and stroke in meat eaters, fish eaters, and vegetarians over 18 years of follow-up: Results from the prospective EPIC-Oxford study. BMJ 2019, 366, l4897. [Google Scholar] [CrossRef] [Green Version]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- Stroup, D.F.; Berlin, J.A.; Morton, S.C.; Olkin, I.; Williamson, G.D.; Rennie, D.; Moher, D.; Becker, B.J.; Sipe, T.A.; Thacker, S.B. Meta-analysis of observational studies in epidemiology: A proposal for reporting. Meta-analysis Of Observational Studies in Epidemiology (MOOSE) group. JAMA 2000, 283, 2008–2012. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.; Kattan, M.W. Cohort studies: Design, analysis, and reporting. Chest 2020, 158, S72–S78. [Google Scholar] [CrossRef]
- Wells, G.A.; Shea, B.; O’Connell, D.; Peterson, J.; Welch, V.; Loso, M.; Tugwell, P. The Newcastle–Ottawa Scale (NOS) for Assessing the Quality of Non Randomised Studies in Meta-Analyses. Available online: http://www.ohri.ca/programs/clinical_epidemiology/oxford.htm (accessed on 2 May 2021).
- Higgins, J.; Thomas, J.; Chandler, J.; Cumpston, M.; Li, T.; Page, M.; Welch, V.A. Cochrane Handbook for Systematic, Reviews of Interventions version 6.2; updated 2021; Cochrane Collaboration: London, UK, 2021; Available online: http://www.training.cochrane.org/handbook (accessed on 2 May 2021).
- Higgins, J.P.T.; Thompson, S.G.; Deeks, J.J.; Altman, D.G. Measuring inconsistency in meta-analyses. BMJ 2003, 327, 557–560. [Google Scholar] [CrossRef] [Green Version]
- Schwingshackl, L.; Knüppel, S.; Schwedhelm, C.; Hoffmann, G.; Missbach, B.; Stelmach-Mardas, M.; Dietrich, S.; Eichelmann, F.; Kontopantelis, E.; Iqbal, K. Perspective: NutriGrade: A Scoring System to Assess and Judge the Meta-Evidence of Randomized Controlled Trials and Cohort Studies in Nutrition Research. Adv. Nutr. 2016, 7, 994–1004. [Google Scholar] [CrossRef] [PubMed]
- Chiu, T.H.T.; Chang, H.R.; Wang, L.Y.; Chang, C.C.; Lin, M.N.; Lin, C.L. Vegetarian diet and incidence of total, ischemic, and hemorrhagic stroke in 2 cohorts in Taiwan. Neurology 2020, 94, e1112–e1121. [Google Scholar] [CrossRef] [Green Version]
- Oussalah, A.; Levy, J.; Berthezène, C.; Alpers, D.H.; Guéant, J.L. Health outcomes associated with vegetarian diets: An umbrella review of systematic reviews and meta-analyses. Clin. Nutr. 2020, 39, 3283–3307. [Google Scholar] [CrossRef] [PubMed]
- Dinu, M.; Abbate, R.; Gensini, G.F.; Casini, A.; Sofi, F. Vegetarian, vegan diets and multiple health outcomes: A systematic review with meta-analysis of observational studies. Crit. Rev. Food Sci. Nutr. 2017, 57, 3640–3649. [Google Scholar] [CrossRef] [PubMed]
- Glenn, A.J.; Viguiliouk, E.; Seider, M.; Boucher, B.A.; Khan, T.A.; Blanco Mejia, S.; Jenkins, D.J.A.; Kahleova, H.; Rahelic, D.; Salas-Salvado, J.; et al. Relation of vegetarian dietary patterns with major cardiovascular outcomes: A systematic review and meta-analysis of prospective cohort studies. Front. Nutr. 2019, 6, 80. [Google Scholar] [CrossRef] [Green Version]
- Archundia Herrera, M.C.; Subhan, F.B.; Chan, C.B. Dietary patterns and cardiovascular disease risk in people with type 2 diabetes. Curr. Obes. Rep. 2017, 6, 405–413. [Google Scholar] [CrossRef] [PubMed]
- Le, L.T.; Sabaté, J. Beyond meatless, the health effects of vegan diets: Findings from the Adventist cohorts. Nutrients 2014, 6, 2131–2147. [Google Scholar] [CrossRef] [Green Version]
- Fresán, U.; Sabaté, J. Vegetarian diets: Planetary health and its alignment with human health. Adv. Nutr. 2019, 10 (Suppl. 4), S380–S388. [Google Scholar] [CrossRef] [Green Version]
- Satija, A.; Hu, F.B. Plant-based diets and cardiovascular health. Trends Cardiovasc. Med. 2018, 28, 437–441. [Google Scholar] [CrossRef]
- Aune, D. Plant foods, antioxidant biomarkers, and the risk of cardiovascular disease, cancer, and mortality: A review of the evidence. Adv. Nutr. 2019, 10 (Suppl 4), S404–S421. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kahleova, H.; Levin, S.; Barnard, N. Cardio-metabolic benefits of plant-based diets. Nutrients 2017, 9, 848. [Google Scholar] [CrossRef]
- Wang, F.; Zheng, J.; Yang, B.; Jiang, J.; Fu, Y.; Li, D. Effects of vegetarian diets on blood lipids: A systematic review and meta-analysis of randomized controlled trials. J. Am. Heart Assoc. 2015, 4, e002408. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yokoyama, Y.; Barnard, N.D.; Levin, S.M.; Watanabe, M. Vegetarian diets and glycemic control in diabetes: A systematic review and meta-analysis. Cardiovasc. Diagn Ther. 2014, 4, 373–382. [Google Scholar] [PubMed]
- Yokoyama, Y.; Nishimura, K.; Barnard, N.D.; Takegami, M.; Watanabe, M.; Sekikawa, A.; Okamura, T.; Miyamoto, Y. Vegetarian diets and blood pressure: A meta-analysis. JAMA Intern. Med. 2014, 174, 577–587. [Google Scholar] [CrossRef] [PubMed]
- Bechthold, A.; Boeing, H.; Schwedhelm, C.; Hoffmann, G.; Knüppel, S.; Iqbal, K.; De Henauw, S.; Michels, N.; Devleesschauwer, B.; Schlesinger, S. Food groups and risk of coronary heart disease, stroke and heart failure: A systematic review and dose-response meta-analysis of prospective studies. Crit. Rev. Food Sci. Nutr. 2019, 59, 1071–1090. [Google Scholar] [CrossRef] [Green Version]
- Schwingshackl, L.; Schwedhelm, C.; Hoffmann, G.; Knüppel, S.; Iqbal, K.; Andriolo, V.; Bechthold, A.; Schlesinger, S.; Boeing, H. Food Groups and Risk of Hypertension: A Systematic Review and Dose-Response Meta-Analysis of Prospective Studies. Adv. Nutr. 2017, 8, 793–803. [Google Scholar] [CrossRef]
- Borude, S. Which is a good diet-veg or non-veg? Faith-based vegetarianism for protection from obesity-a myth or actuality? Obes. Surg. 2019, 29, 1276–1280. [Google Scholar] [CrossRef]
- Hever, J.; Cronise, R.J. Plant-based nutrition for healthcare professionals: Implementing diet as a primary modality in the prevention and treatment of chronic disease. J. Geriatr. Cardiol. 2017, 14, 355–368. [Google Scholar]
- Judd, S.E.; Gutiérrez, O.M.; Newby, P.K.; Howard, G.; Howard, V.J.; Locher, J.L.; Kissela, B.M.; Shikany, J.M. Dietary patterns are associated with incident stroke and contribute to excess risk of stroke in black Americans. Stroke 2013, 44, 3305–3311. [Google Scholar] [CrossRef]
- Heianza, Y.; Zhou, T.; Sun, D.; Hu, F.B.; Manson, J.E.; Qi, L. Genetic susceptibility, plant-based dietary patterns, and risk of cardiovascular disease. Am. J. Clin. Nutr. 2020, 112, 220–228. [Google Scholar] [CrossRef]
- Estruch, R.; Ros, E.; Salas-Salvadó, J.; Covas, M.I.; Corella, D.; Arós, F.; Gomez-Gracia, E.; Ruiz-Gutierrez, V.; Fiol, M.; Lapetra, J.; et al. Primary prevention of cardiovascular disease with a Mediterranean diet supplemented with extra-virgin olive oil or nuts. N. Engl. J. Med. 2018, 378, e34. [Google Scholar] [CrossRef]
- Tektonidis, T.G.; Åkesson, A.; Gigante, B.; Wolk, A.; Larsson, S.C. A Mediterranean diet and risk of myocardial infarction, heart failure and stroke: A population-based cohort study. Atherosclerosis 2015, 243, 93–98. [Google Scholar] [CrossRef]
- Fung, T.T.; Chiuve, S.E.; McCullough, M.L.; Rexrode, K.M.; Logroscino, G.; Hu, F.B. Adherence to a DASH-style diet and risk of coronary heart disease and stroke in women. Arch. Intern. Med. 2008, 168, 713–720. [Google Scholar] [CrossRef] [Green Version]
- Morze, J.; Danielewicz, A.; Hoffmann, G.; Schwingshackl, L. Diet Quality as Assessed by the Healthy Eating Index, Alternate Healthy Eating Index, Dietary Approaches to Stop Hypertension Score, and Health Outcomes: A Second Update of a Systematic Review and Meta-Analysis of Cohort Studies. J. Acad. Nutr. Diet. 2020, 120, 1998–2031.e15. [Google Scholar] [CrossRef]
- Rizzo, N.S.; Jaceldo-Siegl, K.; Sabate, J.; Fraser, G.E. Nutrient profiles of vegetarian and nonvegetarian dietary patterns. J. Acad. Nutr. Diet. 2013, 113, 1610–1619. [Google Scholar] [CrossRef] [Green Version]
- Putaala, J.; Metso, A.J.; Metso, T.M.; Konkola, N.; Kraemer, Y.; Haapaniemi, E.; Kaste, M.; Tatlisumak, T. Analysis of 1008 consecutive patients aged 15 to 49 with first-ever ischemic stroke: The Helsinki young stroke registry. Stroke 2009, 40, 1195–1203. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Schwamm, J.R.; Pervez, M.A.; Singhal, A.B. Ischemic stroke and transient ischemic attack in young adults: Risk factors, diagnostic yield, neuroimaging, and thrombolysis. JAMA Neurol. 2013, 70, 51–57. [Google Scholar]
- Kittner, S.J.; Stern, B.J.; Feeser, B.R.; Hebel, R.; Nagey, D.A.; Buchholz, D.W.; Earley, C.J.; Johnson, C.J.; Macko, R.F.; Sloan, M.A. Pregnancy and the risk of stroke. N. Engl. J. Med. 1996, 335, 768–774. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- de los Ríos, F.; Kleindorfer, D.O.; Khoury, J.; Broderick, J.P.; Moomaw, C.J.; Adeoye, O.; Flaherty, M.L.; Khatri, P.; Woo, D.; Alwell, K. Trends in substance abuse preceding stroke among young adults: A population-based study. Stroke 2012, 43, 3179–3183. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- von Sarnowski, B.; Schminke, U.; Tatlisumak, T.; Putaala, J.; Grittner, U.; Kaps, M.; Tobin, W.O.; Kinsella, J.A.; McCabe, D.J.; Hennerici, M.G. Prevalence of stenoses and occlusions of brain-supplying arteries in young stroke patients. Neurology 2013, 80, 1287–1294. [Google Scholar] [CrossRef]
- Aigner, A.; Grittner, U.; Rolfs, A.; Norrving, B.; Siegerink, B.; Busch, M.A. Contribution of established stroke risk factors to the burden of stroke in young adults. Stroke 2017, 48, 1744–1751. [Google Scholar] [CrossRef]
- Rasura, M.; Spalloni, A.; Ferrari, M.; De Castro, S.; Patella, R.; Lisi, F.; Beccia, M. A case series of young stroke in Rome. Eur. J. Neurol. 2006, 13, 146–152. [Google Scholar] [CrossRef]
- Weikert, C.; Dierkes, J.; Hoffmann, K.; Berger, K.; Drogan, D.; Klipstein-Grobusch, K.; Spranger, J.; Möhlig, M.; Luley, C.; Boeing, H. B vitamin plasma levels and the risk of ischemic stroke and transient ischemic attack in a German cohort. Stroke 2007, 38, 2912–2918. [Google Scholar] [CrossRef] [Green Version]
- Homocysteine Studies Collaboration. Homocysteine and risk of ischemic heart disease and stroke: A meta-analysis. JAMA 2002, 288, 2015–2022. [Google Scholar]
- Rizzo, G.; Laganà, A.S.; Rapisarda, A.M.; La Ferrera, G.M.; Buscema, M.; Rossetti, P.; Nigro, A.; Muscia, V.; Valenti, G.; Sapia, F. Vitamin B12 among vegetarians: Status, assessment and supplementation. Nutrients 2016, 8, 767. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pawlak, R. Is vitamin B12 deficiency a risk factor for cardiovascular disease in vegetarians? Am. J. Prev. Med. 2015, 48, e11–e26. [Google Scholar] [CrossRef]
- Ghai, N.R.; Jacobsen, S.J.; Van Den Eeden, S.K.; Ahmed, A.T.; Haque, R.; Rhoads, G.G.; Quinn, V.P. A comparison of lifestyle and behavioral cardiovascular disease risk factors between Asian Indian and White non-Hispanic men. Ethn. Dis. 2012, 22, 168–174. [Google Scholar] [PubMed]

| First Author, Year | Study Name (Country) | N of Participants | N of Cases (Absolute Rate of Stroke, %) | Age, Years, Mean (SD) | Female (%) | BMI, Mean (SD) | Ethanol Intake, g/day, Mean (SD) | Incidence of DM | Incidence of HTN | Average Follow-Up Length, Years (Date) | Dietary Assessment | Definition of Vegetarian/non-Vegetarians | Stroke Assessment | Covariate Adjustment Set | Risk Estimates, HR (95% CI) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Baden et al., 2021 [14] | NHS (US) | 473 of vegetarians/65,987 of non-vegetarians | 29 in vegetarians (6.1)/3575 in non-vegetarians | 69 (7) | 100 | 24.9 (5.2) | 2.3 (7.2) | 7% | 42% | 31.4 (1984–2016) | 110-item FFQ, updated every 2–4 years | Lacto-ovo-vegetarians (meat and/or fish intakes were 0 or <1 serving per month)/meat and/or fish intakes were ≥1 serving per month | Hospital-based records | Age, race, smoking, alcohol intake, physical activity, total energy intake, DM, HTN, dyslipidemia, BMI, medication use | 1.07 (0.74–1.55) |
| Baden et al., 2021 [14] | NHS II (US) | 978 of vegetarians/90,539 of non-vegetarians | 6 in vegetarians (0.6)/734 in non-vegetarians | 48 (5) | 100 | 24.8 (5.2) | 3.1 (7.3) | 2% | 14% | 25.8 (1991–2017) | 110-item FFQ, updated every 2–4 years | Lacto-ovo-vegetarians (meat and/or fish intakes were 0 or <1 serving per month)/meat and/or fish intakes were ≥1 serving per month | Hospital-based records | Age, race, smoking, alcohol intake, physical activity, total energy intake, DM, HTN, hypercholesterolemia, BMI, medication use | 0.75 (0.33–1.67) |
| Baden et al., 2021 [14] | HPFS (US) | 320 of vegetarians/37,095 of non-vegetarians | 16 in vegetarians (5)/1881 in non-vegetarians | 68 (9) | 0 | 25.0 (4.7) | 4.5 (10.8) | 8% | 36% | 26.0 (1986–2012) | 110-item FFQ, updated every 2–4 years | Lacto-ovo-vegetarians (meat and/or fish intakes were 0 or <1 serving per month)/meat and/or fish intakes were ≥1 serving per month | Hospital-based records | Age, race, smoking, alcohol intake, physical activity, total energy intake, DM, HTN, hypercholesterolemia, BMI, medication use | 0.98 (0.60–1.62) |
| Chiu et al., 2020 [15] | TCHS (Taiwan) | 1424 of vegetarians/3626 of non-vegetarians | 10 in vegetarians (0.7)/44 in non-vegetarians | 53.8 (9.0) | 59 | 23.0 (3.1) | 8.1% ever drink alcohol | 4.6% | 14.2% | 6.1 (2007–2014) | 64-item FFQ, baseline | Lacto-ovo-vegetarians (consuming no meat and fish)/any consumption of meat or fish | ICD 9: 430–438 | Age, sex, smoking, alcohol intake, betel nut, physical activity, education, DM, HTN, dyslipidemia, ischemic heart disease, and BMI | 0.51 (0.25–1.06) |
| Chiu et al., 2020 [15] | TCVS (Taiwan) | 2719 of vegetarians/5583 of non-vegetarians | 24 in vegetarians (0.9)/97 in non-vegetarians | 50.1 (9.3) | 64 | NA | 11% ever drink alcohol | 11.8% | 9.4% | 9.3 (2005–2014) | 57-item FFQ, baseline | Lacto-ovo-vegetarians (consuming no meat and fish)/any consumption of meat or fish | ICD 9: 430–438 | Age, sex, smoking, alcohol intake, betel nut, physical activity, education, DM, HTN, dyslipidemia, and ischemic heart disease | 0.52 (0.33–0.82) |
| Petermann-Rocha et al., 2021 [16] | UK Biobank (UK) | 7537 of vegetarians/415,304 of non-vegetarians | 65 in vegetarians (0.9)/5881 in non-vegetarians | 53.1 (7.9) | 55 | 25.6 (4.6) | 77.9% ever drink alcohol | NA | NA | 8.5 (2006–2020) | 24-hr recall questionnaire via Oxford WebQ, baseline | Lacto-ovo-vegetarians excluding vegans (consuming cheese and/or milk but not fish, poultry, or red meat)/meat-eaters (consumption of cheese, milk, fish, poultry, and red meat) | ICD 10: I60, I61, I63, I64 | Age, sex, deprivation, race, smoking, alcohol intake, physical activity, and BMI | 0.84 (0.66–1.07) |
| Tong et al., 2019 [24] | EPIC-Oxford (UK) | 16,254 of vegetarians/31,934 of non-vegetarians | 258 in vegetarians/814 in non-vegetarians | 39.4 (13.1) | 77 | 23 | 9.3 (12.8) | 0.6% | 5.8% | 14 (1993–2016) | 130-item FFQ, baseline and a follow-up 2010 | Lacto-ovo-vegetarians including vegans (consuming no meat and fish)/meat-eaters (consumption of meat and fish) | ICD-9: 430–431, 433–434, 436ICD-10: I60–I61, I63–I64 | Age, sex, smoking, alcohol intake, region, education, deprivation, physical activity, medication use | 1.20 (1.02–1.40) |
| Subgroups | No. of Studies | Hazard Ratio (95% CI) | I2 (%) |
|---|---|---|---|
| Overall | 7 | 0.86 (0.67–1.11) | 68 |
| Mean age | |||
| Age < 50 y | 2 | 1.13 (0.83–1.54) | 20 |
| 50 y ≦ Age < 65 y | 3 | 0.66 (0.45–0.95) * | 54 |
| Age ≥ 65 y | 2 | 1.04 (0.77–1.40) | 0 |
| Geographic locations | |||
| America | 3 | 1.00 (0.76–1.32) | 0 |
| Asia | 2 | 0.52 (0.35–0.76) * | 0 |
| Europe | 2 | 1.02 (0.72–1.44) | 83 |
| Sex | |||
| Men | 1 | 0.98 (0.60–1.61) | NA |
| Women | 2 | 1.01 (0.72–1.41) | 0 |
| Body mass index (BMI) category | |||
| Normal (18.5 ≦ BMI < 24.9) | 4 | 0.98 (0.72–1.33) | 52 |
| Overweight (BMI ≥ 25.0) | 2 | 0.87 (0.70–1.08) | 0 |
| Dietary assessment | |||
| Baseline intake | 3 | 0.66 (0.45–0.95) * | 54 |
| Longitudinal follow-up | 4 | 1.15 (1.00–1.32) * | 0 |
| Nutri Grade Items a | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Comparison | Item 1 b | Item 2 c | Item 3 d | Item 4 e | Item 5 f | Item 6 g | Item 7 h | Item 8 i | Total Score | Certainty of Evidence |
| Total stroke | 2 | 0 | 0.1 | 1 | 0 | 1 | 0 | 0 | 4.1 | Low |
| Ischemic stroke | 2 | 0 | 0.1 | 1 | 0 | 1 | 0 | 0 | 4.1 | Low |
| Hemorrhage stroke | 2 | 0 | 0.1 | 1 | 0 | 1 | 0 | 0 | 4.1 | Low |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lu, J.-W.; Yu, L.-H.; Tu, Y.-K.; Cheng, H.-Y.; Chen, L.-Y.; Loh, C.-H.; Chen, T.-L. Risk of Incident Stroke among Vegetarians Compared to Nonvegetarians: A Systematic Review and Meta-Analysis of Prospective Cohort Studies. Nutrients 2021, 13, 3019. https://doi.org/10.3390/nu13093019
Lu J-W, Yu L-H, Tu Y-K, Cheng H-Y, Chen L-Y, Loh C-H, Chen T-L. Risk of Incident Stroke among Vegetarians Compared to Nonvegetarians: A Systematic Review and Meta-Analysis of Prospective Cohort Studies. Nutrients. 2021; 13(9):3019. https://doi.org/10.3390/nu13093019
Chicago/Turabian StyleLu, Jing-Wun, Luo-Hua Yu, Yu-Kang Tu, Hung-Yu Cheng, Li-Yu Chen, Ching-Hui Loh, and Tai-Li Chen. 2021. "Risk of Incident Stroke among Vegetarians Compared to Nonvegetarians: A Systematic Review and Meta-Analysis of Prospective Cohort Studies" Nutrients 13, no. 9: 3019. https://doi.org/10.3390/nu13093019
APA StyleLu, J.-W., Yu, L.-H., Tu, Y.-K., Cheng, H.-Y., Chen, L.-Y., Loh, C.-H., & Chen, T.-L. (2021). Risk of Incident Stroke among Vegetarians Compared to Nonvegetarians: A Systematic Review and Meta-Analysis of Prospective Cohort Studies. Nutrients, 13(9), 3019. https://doi.org/10.3390/nu13093019







