Fat–Fit Patterns, Drug Consumption, and Polypharmacy in Older Adults: The EXERNET Multi-Center Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Participants
2.2. Ethics
2.3. Measurements
2.3.1. Physical Fitness and Body Composition
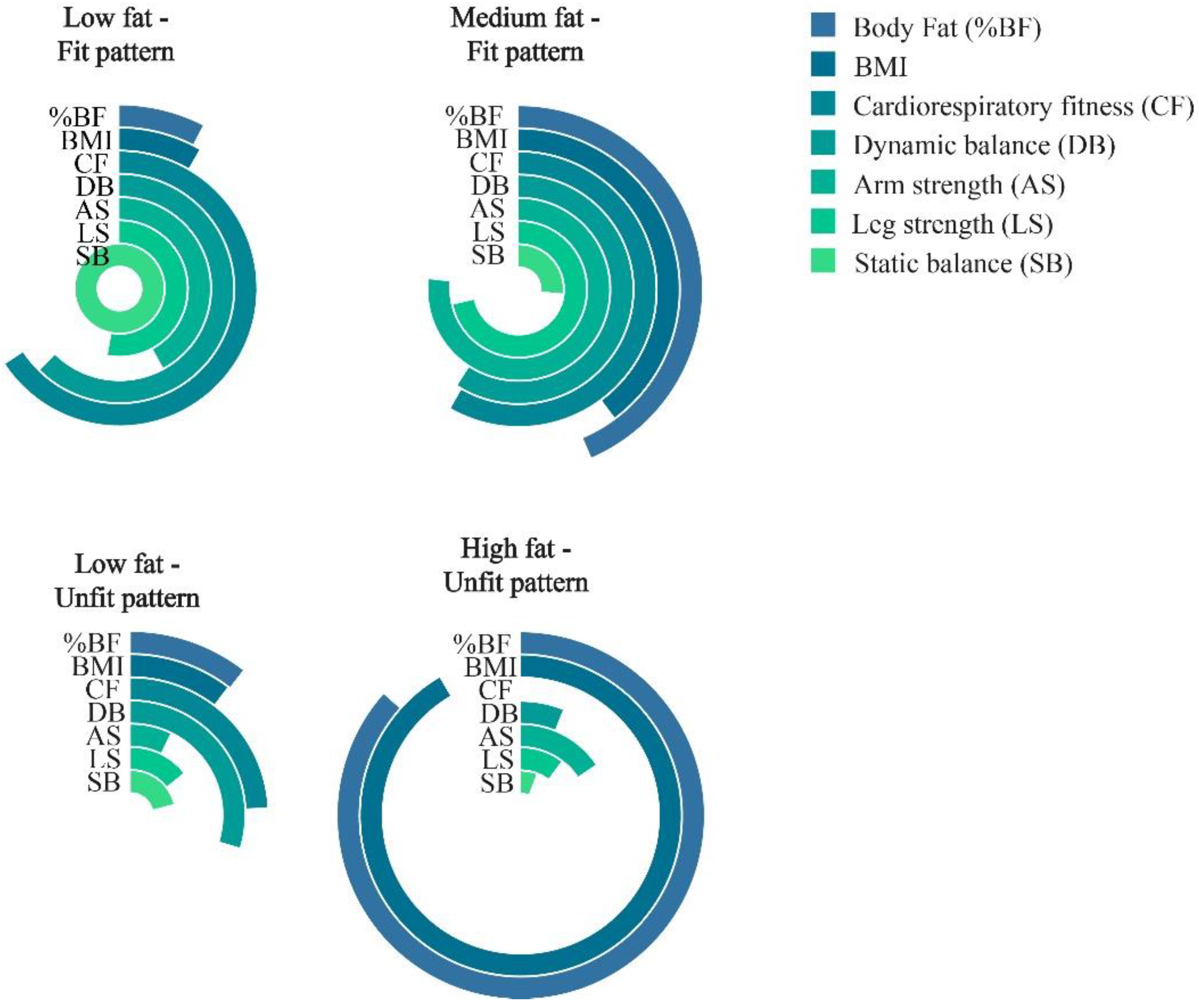
2.3.2. Fat–Fit Patterns
- -
- Low-Fat–Fit pattern (LFat-Fit), which was characterized by high levels of fitness, especially for the balance test, and the lowest levels of BMI and %BF.
- -
- Medium-Fat–Fit pattern (MFat-Fit), which included the subjects with the highest values for strength, high levels of dynamic balance and CRF, and the presence of medium values for both of the body composition variables studied.
- -
- High Fat–Unfit pattern (HFat-Unfit), which included subjects with the lowest values for physical fitness and the highest values for BMI and %BF.
- -
- Low-Fat–Unfit pattern (LFat-Unfit), which included subjects with low values for the physical fitness variables and low values for both the BMI and %BF in comparison with the other groups.
2.3.3. Demographic Characteristics
2.3.4. Polypharmacy and Medicine Consumption
2.4. Statistical Analyses
3. Results
3.1. Participants’ Characteristics
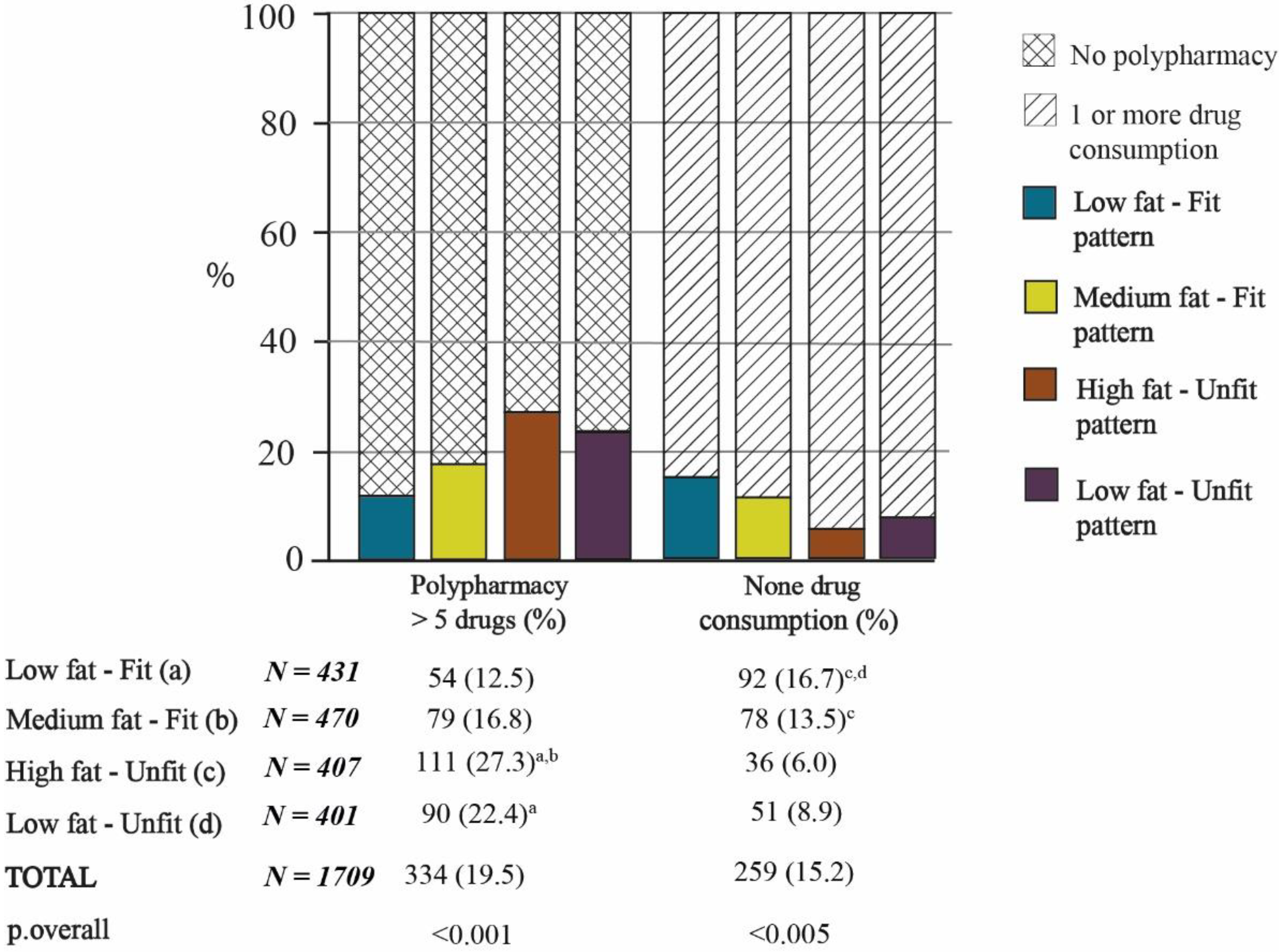
3.2. Relationships between Fat–Fit Patterns, Number of Medications Consumed, and Polypharmacy
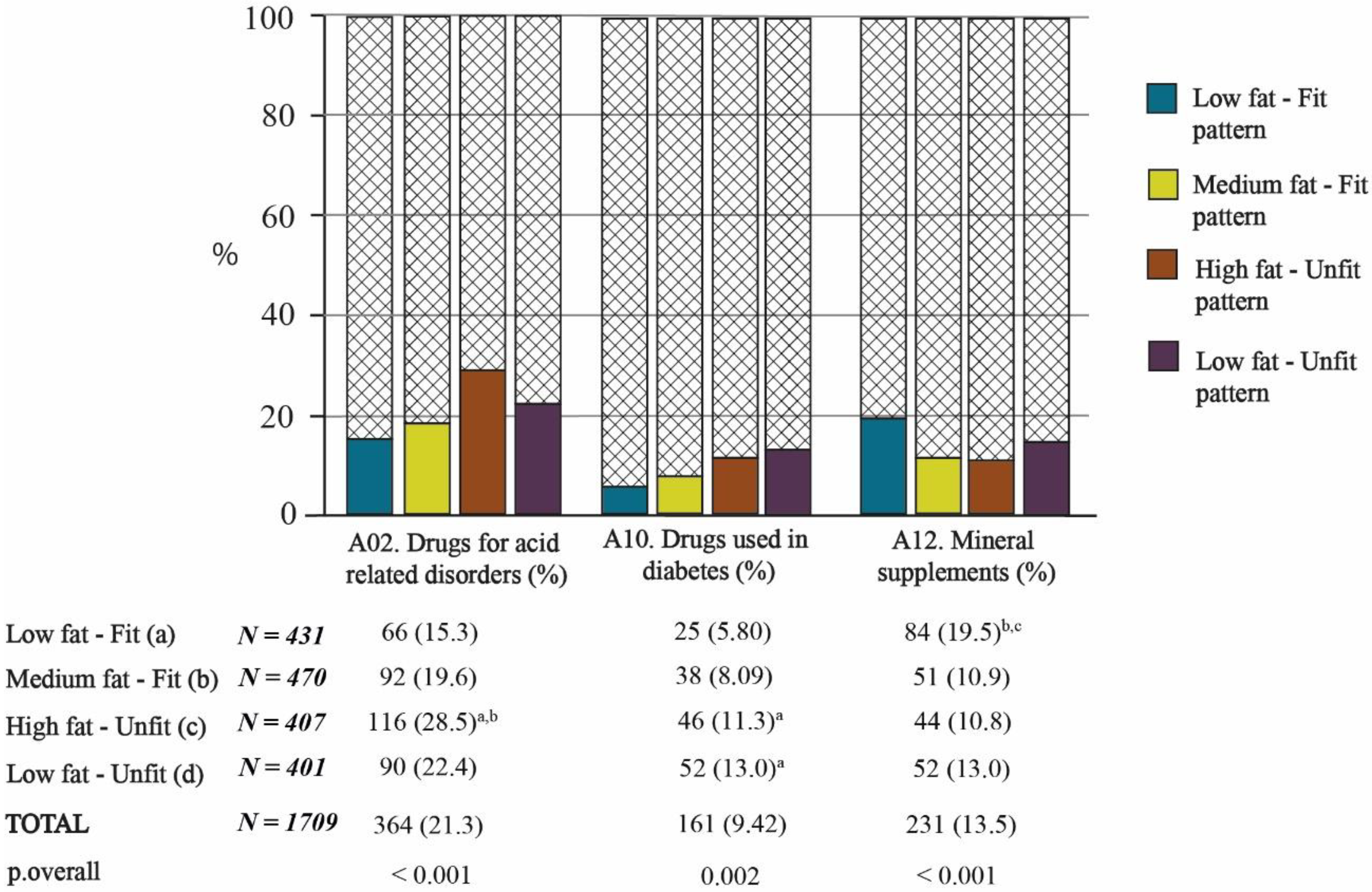
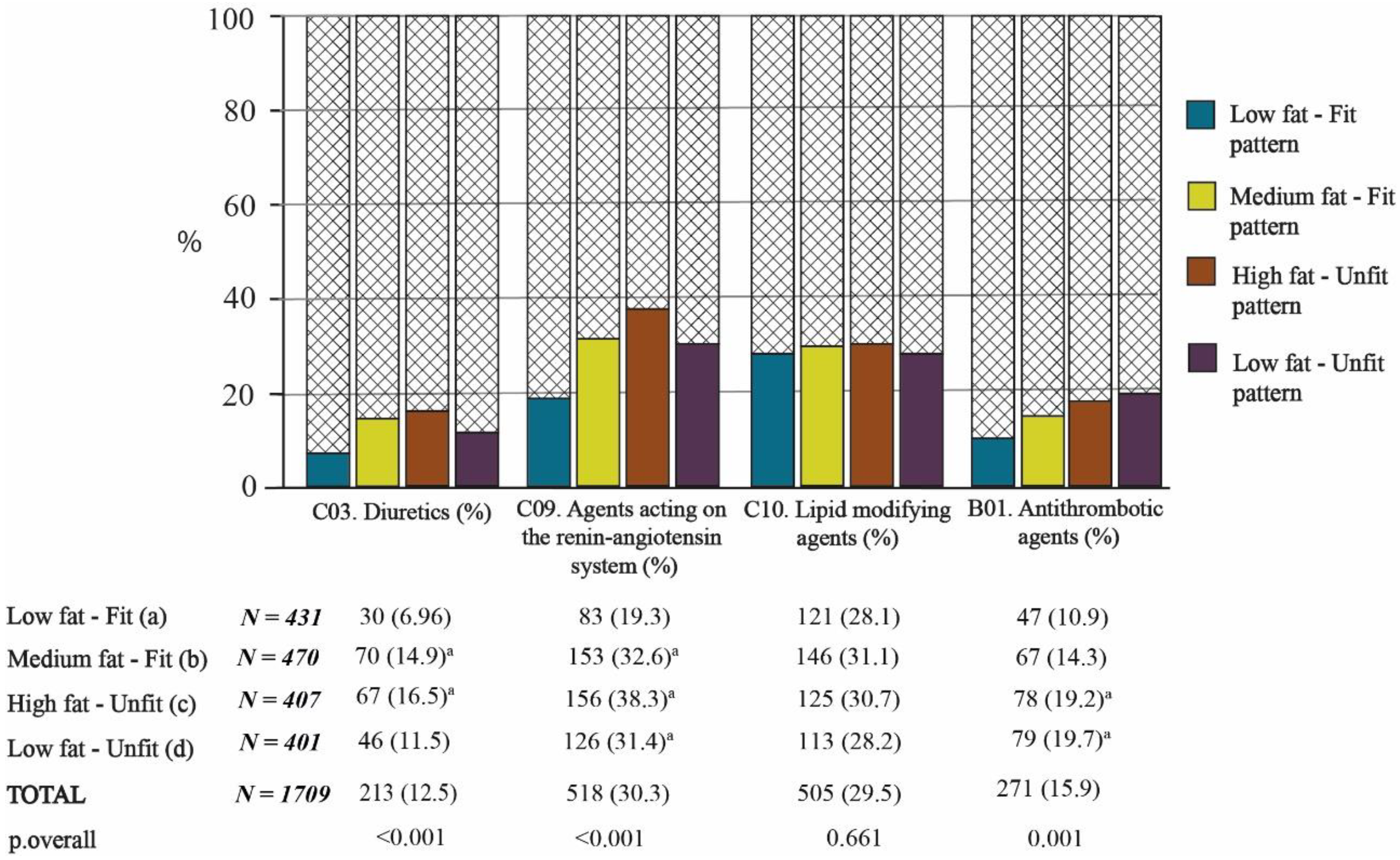
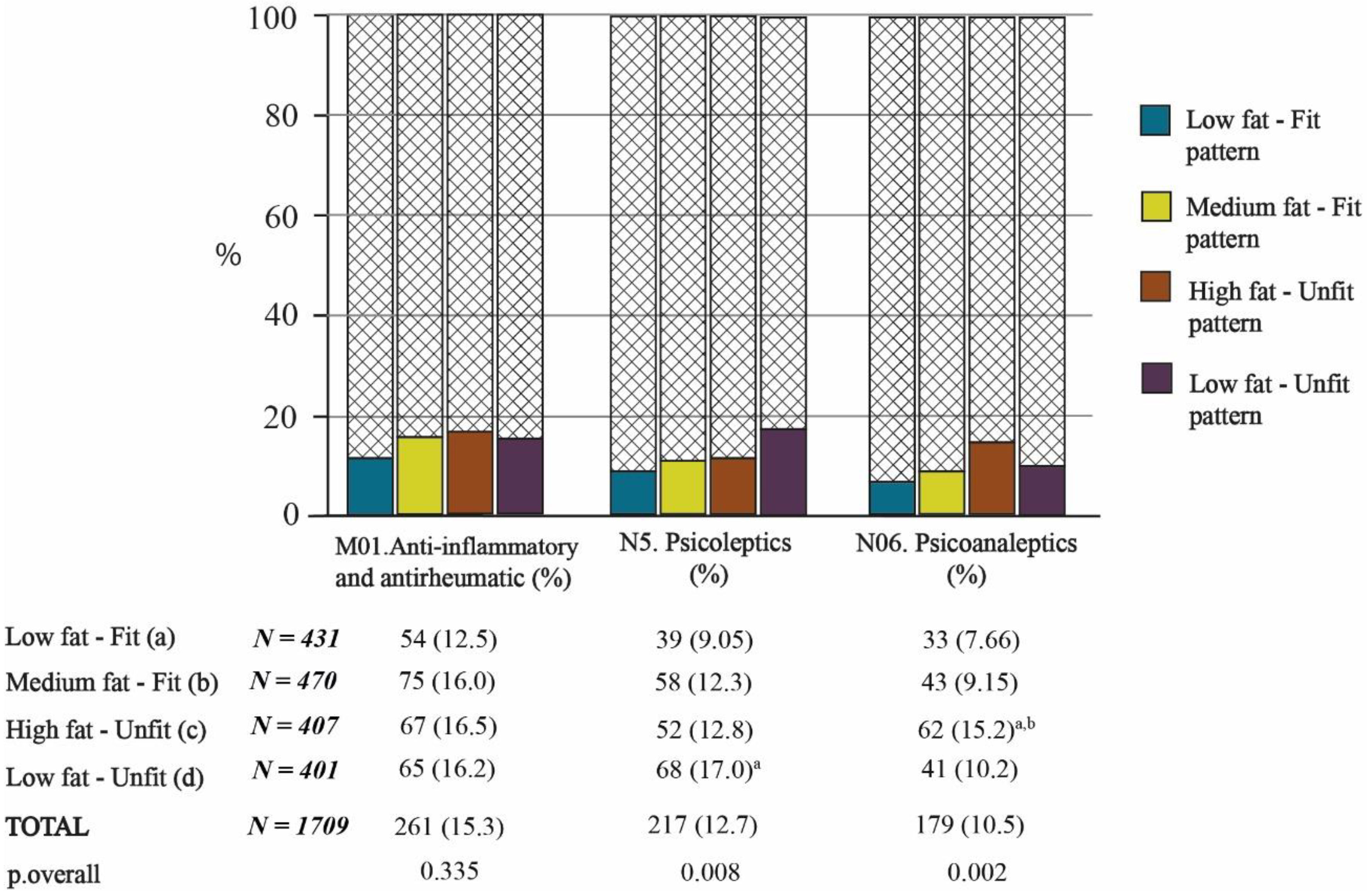
3.3. Relationships between Fat–Fit Patterns and Drug Groups
3.3.1. Fat–Fit Patterns and Drugs Related to the Alimentary Tract and Metabolism
3.3.2. Fat–Fit Patterns and Drugs Related to the Cardiovascular System and Blood
3.3.3. Fat–Fit Patterns and Drugs Related to the Musculoskeletal and Nervous Systems
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Ortega, F.B.; Cadenas-Sanchez, C.; Lee, D.-C.; Ruiz, J.R.; Blair, S.N.; Sui, X. Fitness and Fatness as Health Markers through the Lifespan: An Overview of Current Knowledge. Prog. Prev. Med. 2018, 3, e0013. [Google Scholar] [CrossRef] [PubMed]
- Wagner, K.-H.; Cameron-Smith, D.; Wessner, B.; Franzke, B. Biomarkers of Aging: From Function to Molecular Biology. Nutrients 2016, 8, 338. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Veronese, N.; Stubbs, B.; Fontana, L.; Trevisan, C.; Bolzetta, F.; De Rui, M.; Sartori, L.; Musacchio, E.; Zambon, S.; Maggi, S.; et al. A Comparison of Objective Physical Performance Tests and Future Mortality in the Elderly People. J. Gerontol. Ser. A Boil. Sci. Med. Sci. 2016, 72, 362–368. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mertz, K.J.; Lee, D.-C.; Sui, X.; Powell, K.E.; Blair, S.N. Falls among Adults: The Association of Cardiorespiratory Fitness and Physical Activity with Walking-Related Falls. Am. J. Prev. Med. 2010, 39, 15–24. [Google Scholar] [CrossRef]
- World Health Organization (WHO). World Report on Ageing and Health; WHO Library Cataloguing-in-Publication Data: Luxembourg, 2015. [Google Scholar]
- Barnett, K.; Mercer, S.; Norbury, M.; Watt, G.; Wyke, S.; Guthrie, B. Epidemiology of multimorbidity and implications for health care, research, and medical education: A cross-sectional study. Lancet 2012, 380, 37–43. [Google Scholar] [CrossRef] [Green Version]
- Marengoni, A.; Angleman, S.; Melis, R.; Mangialasche, F.; Karp, A.; Garmen, A.; Meinow, B.; Fratiglioni, L. Aging with multimorbidity: A systematic review of the literature. Ageing Res. Rev. 2011, 10, 430–439. [Google Scholar] [CrossRef]
- Katsimpris, A.; Linseisen, J.; Meisinger, C.; Volaklis, K. The Association Between Polypharmacy and Physical Function in Older Adults: A Systematic Review. J. Gen. Intern. Med. 2019, 34, 1865–1873. [Google Scholar] [CrossRef]
- Masnoon, N.; Shakib, S.; Kalisch-Ellett, L.; Caughey, G.E. What is polypharmacy? A systematic review of definitions. BMC Geriatr. 2017, 17, 1–10. [Google Scholar] [CrossRef] [Green Version]
- Nguyen, T.; Wong, E.; Ciummo, F. Polypharmacy in Older Adults: Practical Applications alongside a Patient Case. J. Nurse Pract. 2020, 16, 205–209. [Google Scholar] [CrossRef] [Green Version]
- Fried, T.R.; O’Leary, J.; Towle, V.; Goldstein, M.K.; Trentalange, M.; Martin, D.K. Health Outcomes Associated with Polypharmacy in Community-Dwelling Older Adults: A Systematic Review. J. Am. Geriatr. Soc. 2014, 62, 2261–2272. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pazan, F.; Wehling, M. Polypharmacy in older adults: A narrative review of definitions, epidemiology and consequences. Eur. Geriatr. Med. 2021, 12, 443–452. [Google Scholar] [CrossRef]
- Midão, L.; Giardini, A.; Menditto, E.; Kardas, P.; Costa, E. Polypharmacy prevalence among older adults based on the survey of health, ageing and retirement in Europe. Arch. Gerontol. Geriatr. 2018, 78, 213–220. [Google Scholar] [CrossRef]
- Assari, S.; Wisseh, C.; Bazargan, M. Obesity and Polypharmacy among African American Older Adults: Gender as the Moderator and Multimorbidity as the Mediator. Int. J. Environ. Res. Public Health 2019, 16, 2181. [Google Scholar] [CrossRef] [Green Version]
- Laureano, M.L.M.; Martins, R.A.; Sousa, N.M.; Machado-Rodrigues, A.M.; Valente-Santos, J.; Coelho-E-Silva, M. Relationship between functional fitness, medication costs and mood in elderly people. Rev. Assoc. Méd. Bras. 2014, 60, 200–207. [Google Scholar] [CrossRef] [Green Version]
- Gomez-Cabello, A.; Pedrero-Chamizo, R.; Olivares, P.R.; Luzardo, L.; Juez-Bengoechea, A.; Mata, E.; Albers, U.; Aznar, S.; Villa, G.; Espino, L.; et al. Prevalence of overweight and obesity in non-institutionalized people aged 65 or over from Spain: The elderly EXERNET multi-centre study. Obes. Rev. 2011, 12, 583–592. [Google Scholar] [CrossRef]
- Sui, X.; LaMonte, M.J.; Laditka, J.N.; Hardin, J.W.; Chase, N.; Hooker, S.P.; Blair, S.N. Cardiorespiratory Fitness and Adiposity as Mortality Predictors in Older Adults. JAMA 2007, 298, 2507–2516. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ortega, F.B.; Ruiz, J.R.; Labayen, I.; Lavie, C.J.; Blair, S.N. The Fat but Fit paradox: What we know and don’t know about it. Br. J. Sports Med. 2017, 52, 151–153. [Google Scholar] [CrossRef] [PubMed]
- Gómez-Cabello, A.; Vicente-Rodríguez, G.; Albers, U.; Mata, E.; Royo, I.A.; Olivares, P.R.; Gusi, N.; Villa, G.; Aznar, S.; Gonzalez-Gross, M.; et al. Harmonization Process and Reliability Assessment of Anthropometric Measurements in the Elderly EXERNET Multi-Centre Study. PLoS ONE 2012, 7, e41752. [Google Scholar] [CrossRef] [PubMed]
- Stewat, A.; Marfell-Jones, M.J.; Olds, T.; de Ridder, H. Protocolo Internacional para la Valoración Antropométrica. ISAK; Sociedad Internacional para el Avance de la Cineantropometría: Portsmouth, UK, 2011. [Google Scholar]
- Rikli, R.E.; Jones, C.J. Development and Validation of Criterion-Referenced Clinically Relevant Fitness Standards for Maintaining Physical Independence in Later Years. Gerontologist 2013, 53, 255–267. [Google Scholar] [CrossRef]
- Johnson, B.L.; Nelson, J.K. Practical Measurements for Evaluation in Physical Education, 2nd ed.; Burgess Publishing Company: Minneapolis, MN, USA, 1969. [Google Scholar]
- Pedrero-Chamizo, R.; Gómez-Cabello, A.; Delgado, S.; Rodríguez-Llarena, S.; Royo, I.A.; Cabanillas, E.; Meléndez, A.; Vicente-Rodríguez, G.; Aznar, S.; Villa, G.; et al. Physical fitness levels among independent non-institutionalized Spanish elderly: The elderly EXERNET multi-center study. Arch. Gerontol. Geriatr. 2012, 55, 406–416. [Google Scholar] [CrossRef] [PubMed]
- Navarrete-Villanueva, D.; Gómez-Cabello, A.; Gómez-Bruton, A.; Gesteiro, E.; Rodríguez-Gómez, I.; Pérez-Gómez, J.; Villa-Vicente, J.G.; Espino-Toron, L.; Gusi, N.; González-Gross, M.; et al. Fitness vs. fatness as determinants of survival in non-institutionalized older adults: The EXERNET multi-center study. J. Gerontol. Ser. A Boil. Sci. Med. Sci. 2021, glab179. [Google Scholar] [CrossRef]
- López-Rodríguez, C.; Laguna, M.; Gómez-Cabello, A.; Gusi, N.; Espino, L.; Villa, G.; Pedrero-Chamizo, R.; Casajus, J.; Ara, I.; Aznar, S. Validation of the self-report EXERNET questionnaire for measuring physical activity and sedentary behavior in elderly. Arch. Gerontol. Geriatr. 2017, 69, 156–161. [Google Scholar] [CrossRef] [PubMed]
- WHO Collaborating Centre for Drug Statistics Methodology. Available online: https://www.whocc.no/ (accessed on 7 July 2021).
- Albers, U.; Palacios, G.; Pedrero-Chamizo, R.; Meléndez, A.; Pietrzik, K.; González-Gross, M. Polymedication in institutionalized elderly and its effect on vitamin B12, folate, and homocysteine levels. Nutr. Hosp. 2012, 27, 298–302. [Google Scholar] [PubMed]
- George, C.; Verghese, J. Polypharmacy and Gait Performance in Community-dwelling Older Adults. J. Am. Geriatr. Soc. 2017, 65, 2082–2087. [Google Scholar] [CrossRef]
- Sganga, F.; Vetrano, D.L.; Volpato, S.; Cherubini, A.; Ruggiero, C.; Corsonello, A.; Fabbietti, P.; Lattanzio, F.; Bernabei, R.; Onder, G. Physical performance measures and polypharmacy among hospitalized older adults: Results from the crime study. J. Nutr. Health Aging 2014, 18, 616–621. [Google Scholar] [CrossRef] [PubMed]
- Rawle, M.J.; Cooper, R.; Kuh, D.; Richards, M. Associations between Polypharmacy and Cognitive and Physical Capability: A British Birth Cohort Study. J. Am. Geriatr. Soc. 2018, 66, 916–923. [Google Scholar] [CrossRef] [Green Version]
- Volaklis, K.A.; Thorand, B.; Peters, A.; Halle, M.; Heier, M.; Strasser, B.; Amann, U.; Ladwig, K.H.; Schulz, H.; Koenig, W.; et al. Physical activity, muscular strength, and polypharmacy among older multimorbid persons: Results from the KORA-Age study. Scand. J. Med. Sci. Sports 2017, 28, 604–612. [Google Scholar] [CrossRef]
- Verde, Z.; De Diego, L.G.; Chicharro, L.M.; Bandrés, F.; Velasco, V.; Mingo, T.; Fernández-Araque, A.; De Diego, G.; Araque, F.-. Physical Performance and Quality of Life in Older Adults: Is There Any Association between Them and Potential Drug Interactions in Polymedicated Octogenarians. Int. J. Environ. Res. Public Health 2019, 16, 4190. [Google Scholar] [CrossRef] [Green Version]
- Frith, E.; Loprinzi, P.D. The protective effects of a novel fitness-fatness index on all-cause mortality among adults with cardiovascular disease. Clin. Cardiol. 2017, 40, 469–473. [Google Scholar] [CrossRef] [Green Version]
- Frith, E.; Loprinzi, P.D. Fitness Fatness Index and Alzheimer-specific mortality. Eur. J. Intern. Med. 2017, 42, 51–53. [Google Scholar] [CrossRef] [PubMed]
- Gómez-Cabello, A.; Rodríguez, G.V.; Vila-Maldonado, S.; Casajús, J.A.; Ara, I. Aging and body composition: The sarcopenic obesity in Spain. Nutr. Hosp. 2012, 27, 22–30. [Google Scholar] [CrossRef]
- Gomez-Bruton, A.; Navarrete-Villanueva, D.; Pérez-Gómez, J.; Vila-Maldonado, S.; Gesteiro, E.; Gusi, N.; Villa-Vicente, J.G.; Espino, L.; Gonzalez-Gross, M.; Casajus, J.A.; et al. The effects of Age, Organized Physical Activity and Sedentarism on Fitness in Older Adults: An 8-Year Longitudinal Study. Int. J. Environ. Res. Public Health 2020, 17, 4312. [Google Scholar] [CrossRef]
- Lee, Y.Y.; McColl, K.E.L. Disruption of the gastroesophageal junction by central obesity and waist belt: Role of raised intra-abdominal pressure. Dis. Esophagus 2014, 28, 318–325. [Google Scholar] [CrossRef]
- Loggia, G.; Attoh-Mensah, E.; Pothier, K.; Morello, R.; Lescure, P.; Bocca, M.-L.; Marcelli, C.; Chavoix, C. Psychotropic Polypharmacy in Adults 55 Years or Older: A Risk for Impaired Global Cognition, Executive Function, and Mobility. Front. Pharmacol. 2020, 10, 1659. [Google Scholar] [CrossRef] [Green Version]
- Baena-Díez, J.M.; Byram, A.O.; Grau, M.; Gómez-Fernández, C.; Vidal-Solsona, M.; Ledesma-Ulloa, G.; González-Casafont, I.; Vasquez-Lazo, J.; Subirana, I.; Schroder, H. Obesity Is an Independent Risk Factor for Heart Failure: Zona Franca Cohort Study. Clin. Cardiol. 2010, 33, 760–764. [Google Scholar] [CrossRef] [PubMed]
- Ponce, S.; Allison, M.A.; Swett, K.; Cai, J.; Desai, A.; Hurwitz, B.E.; Ni, A.; Schneiderman, N.; Shah, S.J.; Spevack, D.M.; et al. The associations between anthropometric measurements and left ventricular structure and function: The Echo-SOL Study. Obes. Sci. Pract. 2018, 4, 387–395. [Google Scholar] [CrossRef] [PubMed]
- Russo, C.; Sera, F.; Jin, Z.; Palmieri, V.; Homma, S.; Rundek, T.; Elkind, M.S.; Sacco, R.L.; Di Tullio, M.R. Abdominal adiposity, general obesity, and subclinical systolic dysfunction in the elderly: A population-based cohort study. Eur. J. Hear. Fail. 2016, 18, 537–544. [Google Scholar] [CrossRef] [PubMed]
- INE (Instituto Nacional de Estadística). Estudio de Consumo de Medicamentos en España. 2012. Available online: https://www.ine.es/jaxi/tabla.do?path=/t15/p419/p03/a2003/l1/&file=03001.px&type=pcaxis&L=1 (accessed on 7 July 2021).
- Ferri, N.; Corsini, A. Clinical Pharmacology of Statins: An Update. Curr. Atheroscler. Rep. 2020, 22, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Aparicio-Ugarriza, R.; Luzardo-Socorro, R.; Palácios, G.; Bibiloni, M.M.; Argelich, E.; Tur, J.A.; González-Gross, M. What is the relationship between physical fitness level and macro- and micronutrient intake in Spanish older adults? Eur. J. Nutr. 2018, 58, 1579–1590. [Google Scholar] [CrossRef]
| First-Level Group | Second-Level Group | |
|---|---|---|
| 1 | A. Alimentary tract and metabolism | A02. Drugs for acid-related disorders |
| 2 | A10. Drugs used in diabetes | |
| 3 | A12. Mineral supplements | |
| 4 | B. Blood and blood-forming organs | B01. Antithrombotic agents |
| 5 | C. Cardiovascular system | C03. Diuretics |
| 6 | C09. Agents acting on the renin–angiotensin system | |
| 7 | C10. Blood-lipid-modifying agents | |
| 8 | M. Musculoskeletal system | M01. Anti-inflammatory and antirheumatic products |
| 9 | N. Nervous system | N05. Psycholeptics |
| 10 | N06. Psychoanaleptics |
| TOTAL | Low-Fat–Fit Pattern | Medium-Fat–Fit Pattern | High-Fat–Unfit Pattern | Low-Fat–Unfit Pattern | p.overall | |
|---|---|---|---|---|---|---|
| N = 1709 | N = 431 | N = 470 | N = 407 | N = 401 | ||
| Age (year) (mean (SD)) | 72.1 (5.20) | 71.1 (4.87) | 72.7 (5.39) | 72.1 (5.04) | 72.4 (5.35) | 0.001 |
| Sex (female) | 1300 (76.1%) | 317 (73.5%) | 361 (76.8%) | 310 (76.2%) | 312 (77.8%) | 0.5 |
| OPA (yes) | 1487 (88.2%) | 385 (90.6%) | 424 (92.0%) | 352 (88.0%) | 326 (81.7%) | 0.001 |
| Walking hours per day | 0.004 | |||||
| <1 | 506 (30.5%) | 97 (23.1%) | 132 (29.1%) | 147 (37.7%) | 130 (32.8%) | |
| 1–2 | 882 (53.2%) | 240 (57.1%) | 243 (53.6%) | 191 (49.0%) | 208 (52.5%) | |
| 2–3 | 216 (13.0%) | 68 (16.2%) | 60 (13.2%) | 43 (11.0%) | 45 (11.4%) | |
| 3–4 | 34 (2.05%) | 10 (2.4%) | 11 (2.4%) | 6 (1.5%) | 7 (1.8%) | |
| 4–5 | 10 (0.6%) | 2 (0.5%) | 4 (0.9%) | 2 (0.5%) | 2 (0.5%) | |
| >5 | 11 (0.7%) | 3 (0.7%) | 3 (0.7%) | 1 (0.3%) | 4 (1.0%) | |
| Sitting hours per day | 0.004 | |||||
| <1 | 40 (2.5%) | 12 (2.9%) | 7 (1.6%) | 10 (2.6%) | 11 (2.9%) | |
| 1–2 | 154 (9.6%) | 49 (12.0%) | 40 (9.7%) | 24 (6.3%) | 41 (10.8%) | |
| 2–3 | 449 (28.0%) | 136 (33.3%) | 108 (25.0%) | 95 (24.9%) | 110 (28.9%) | |
| 3–4 | 417 (26.0%) | 94 (23.0%) | 110 (25.5%) | 106 (27.8%) | 107 (28.2%) | |
| 4–5 | 272 (17.0%) | 64 (15.7%) | 89 (20.6%) | 68 (17.8%) | 51 (13.4%) | |
| >5 | 269 (16.8%) | 53 (13.0%) | 78 (18.1%) | 78 (20.5%) | 60 (15.8%) | |
| Smoking (%yes) | 55 (3.3%) | 18 (4.3%) | 8 (1.8%) | 12 (3.1%) | 17 (4.3%) | 0.07 |
| Fat Mass (%) | 37.1 (6.87) | 33.6 (6.4) | 37.9 (5.9) | 42.5 (5.6) | 34.6 (5.9) | <0.001 |
| BMI (kg/m2) | 29.2 (4.1) | 26.5 (2.8) | 29.2 (2.9) | 33.9 (3.5) | 26.9 (2.6) | <0.001 |
| Number of Medicines (mean (SD)) | 2.75 (2.1) | 2.23 (1.9) | 2.61 (2.1) | 3.27 (2.2) a,b,d | 2.96 (2.2) a | <0.001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Navarrete-Villanueva, D.; Gesteiro, E.; Gómez-Cabello, A.; Mañas, A.; Olivares, R.P.; Villa-Vicente, J.-G.; Gusi, N.; González-Gross, M.; Ara, I.; Vicente-Rodríguez, G.; et al. Fat–Fit Patterns, Drug Consumption, and Polypharmacy in Older Adults: The EXERNET Multi-Center Study. Nutrients 2021, 13, 2872. https://doi.org/10.3390/nu13082872
Navarrete-Villanueva D, Gesteiro E, Gómez-Cabello A, Mañas A, Olivares RP, Villa-Vicente J-G, Gusi N, González-Gross M, Ara I, Vicente-Rodríguez G, et al. Fat–Fit Patterns, Drug Consumption, and Polypharmacy in Older Adults: The EXERNET Multi-Center Study. Nutrients. 2021; 13(8):2872. https://doi.org/10.3390/nu13082872
Chicago/Turabian StyleNavarrete-Villanueva, David, Eva Gesteiro, Alba Gómez-Cabello, Asier Mañas, Rufino Pedro Olivares, José-Gerardo Villa-Vicente, Narcís Gusi, Marcela González-Gross, Ignacio Ara, Germán Vicente-Rodríguez, and et al. 2021. "Fat–Fit Patterns, Drug Consumption, and Polypharmacy in Older Adults: The EXERNET Multi-Center Study" Nutrients 13, no. 8: 2872. https://doi.org/10.3390/nu13082872
APA StyleNavarrete-Villanueva, D., Gesteiro, E., Gómez-Cabello, A., Mañas, A., Olivares, R. P., Villa-Vicente, J.-G., Gusi, N., González-Gross, M., Ara, I., Vicente-Rodríguez, G., & Casajús, J. A. (2021). Fat–Fit Patterns, Drug Consumption, and Polypharmacy in Older Adults: The EXERNET Multi-Center Study. Nutrients, 13(8), 2872. https://doi.org/10.3390/nu13082872











