The Relationship between Low Serum Vitamin D Levels and Altered Intestinal Barrier Function in Patients with IBS Diarrhoea Undergoing a Long-Term Low-FODMAP Diet: Novel Observations from a Clinical Trial
Abstract
1. Introduction
2. Materials and Methods
2.1. Patient Recruitment
2.2. Study Design
2.3. Symptom Profile
2.4. Assessment of Nutrient Intake
2.5. Intervention Diet
2.6. Sugar Absorption Test
2.7. Biochemical Assays
2.8. Indican and Skatole Evaluation
2.9. Statistical Analysis
3. Results
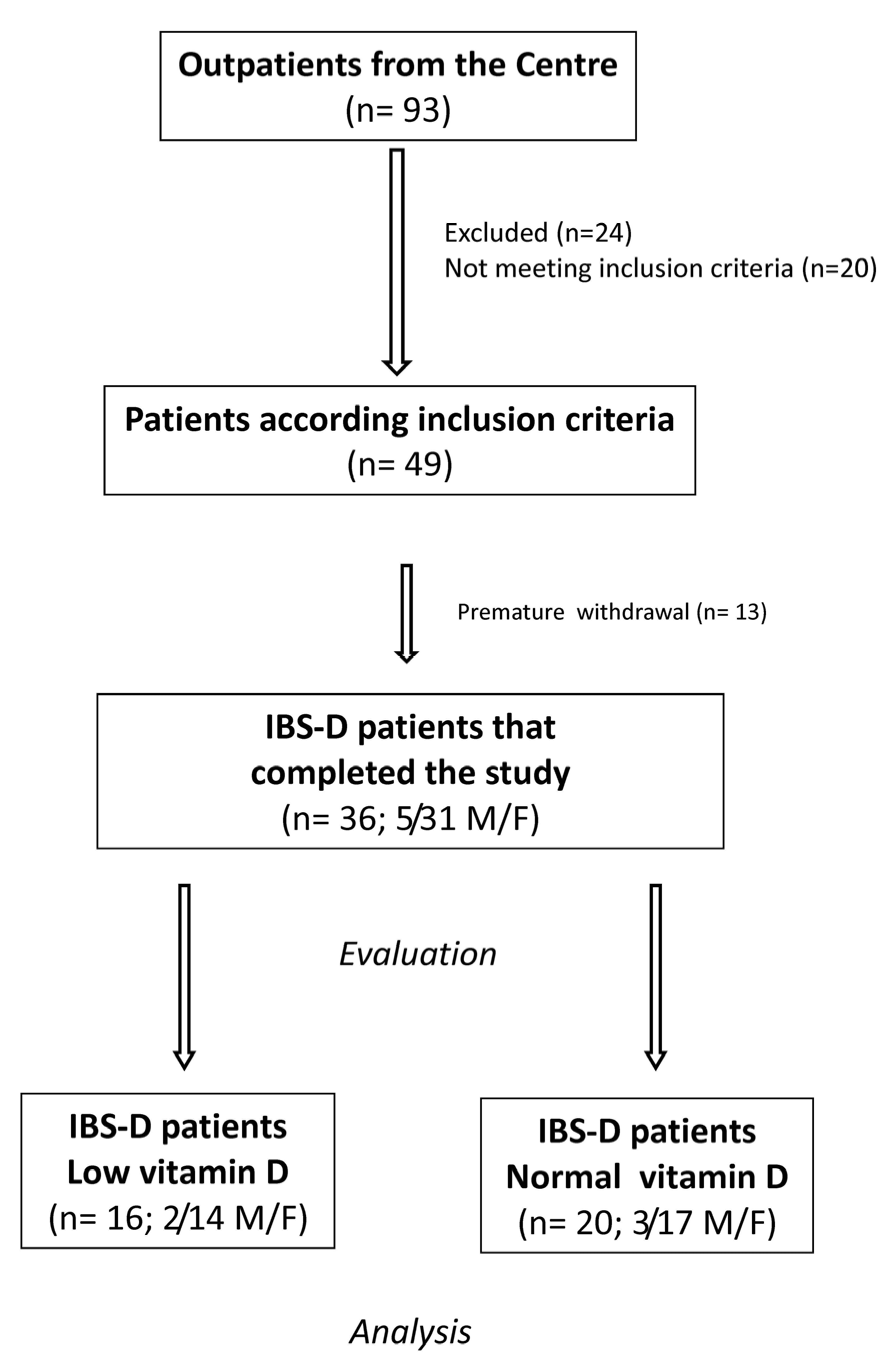
3.1. Number, Anthropometric Characteristics of the Patients, and Intervention Diet
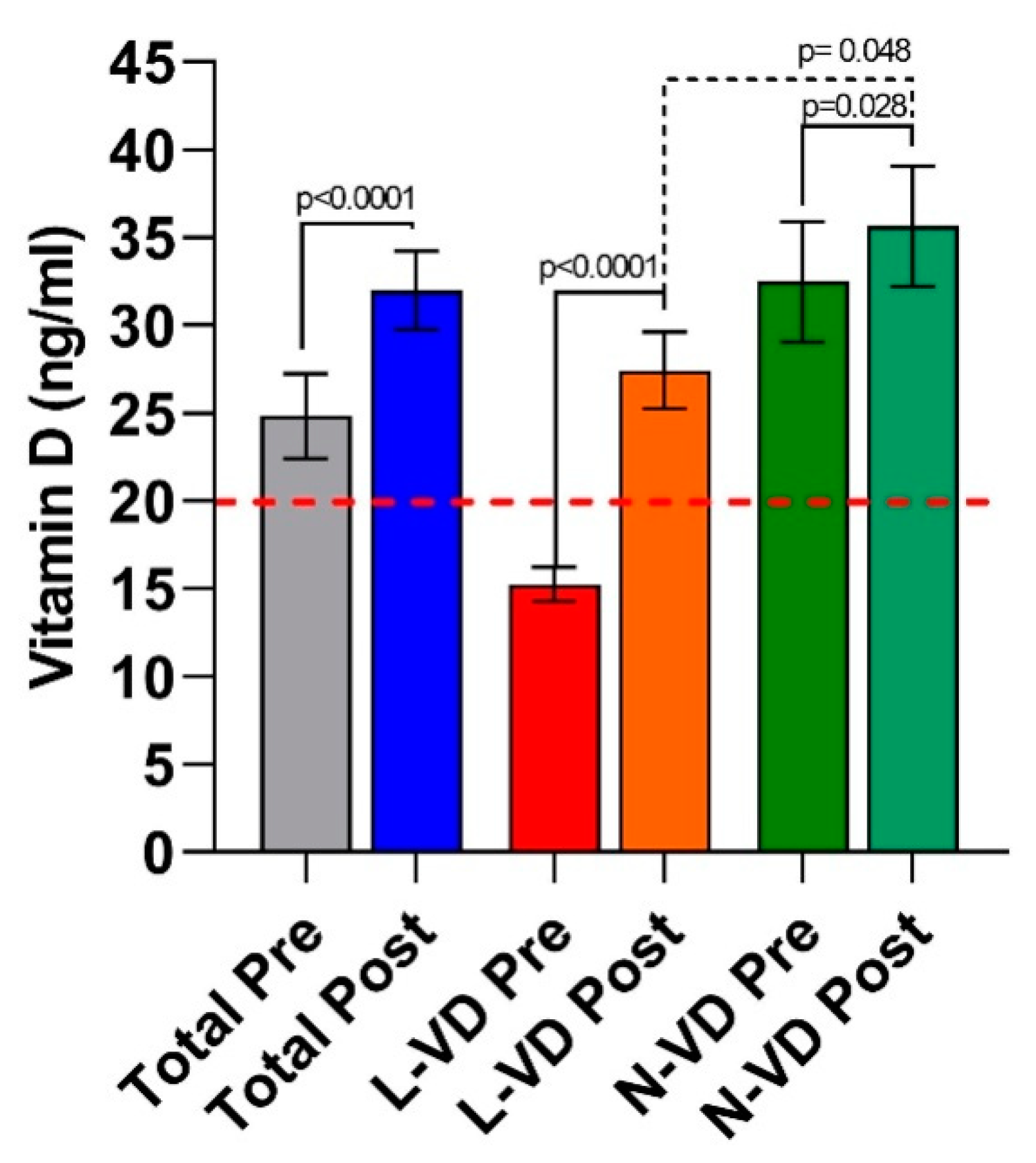
3.2. Circulating VD Levels in IBS-D Patients
3.3. The Symptom Profile in IBS-D Patients
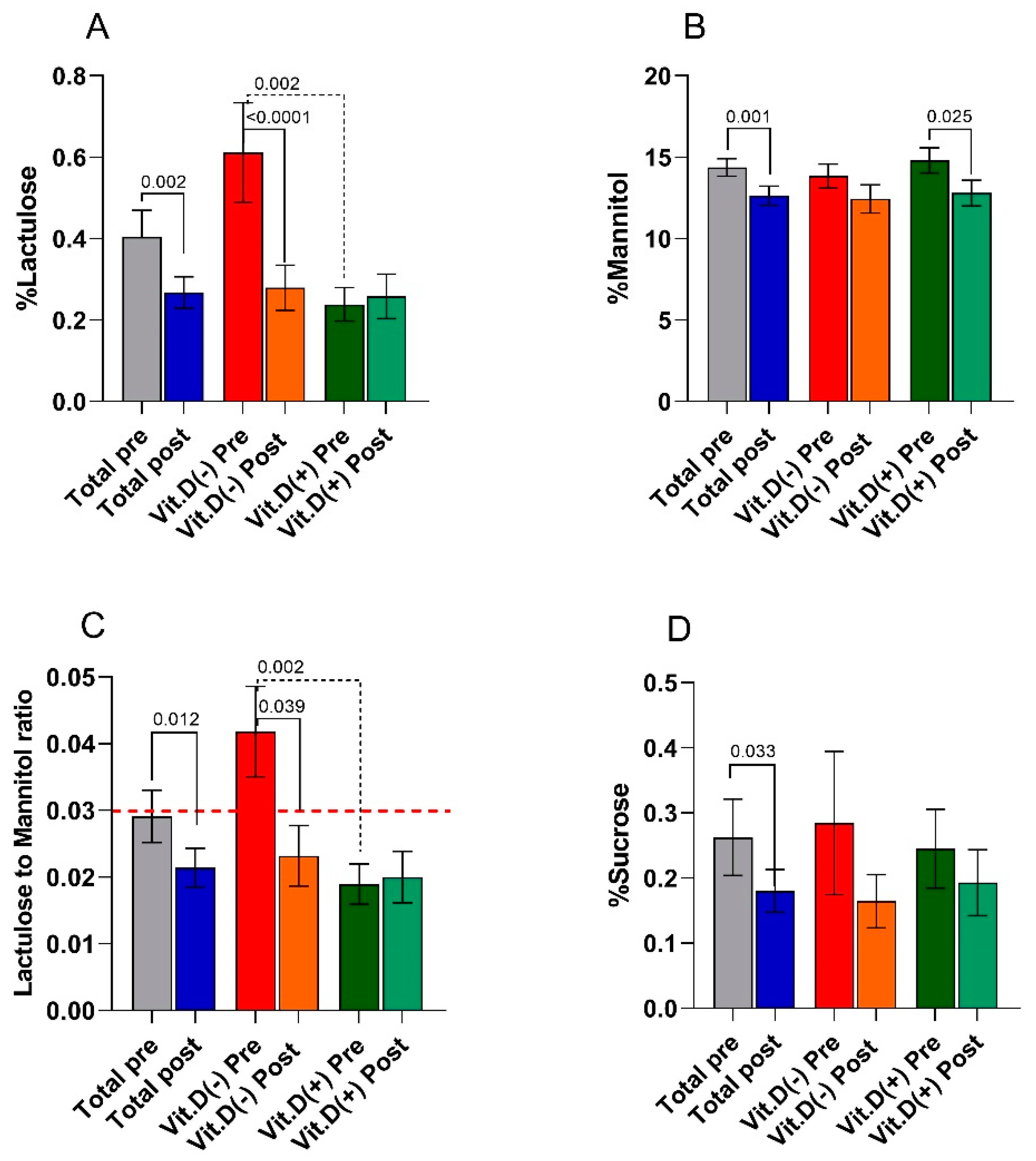
3.4. The Small Intestinal Permeability (s-IP)
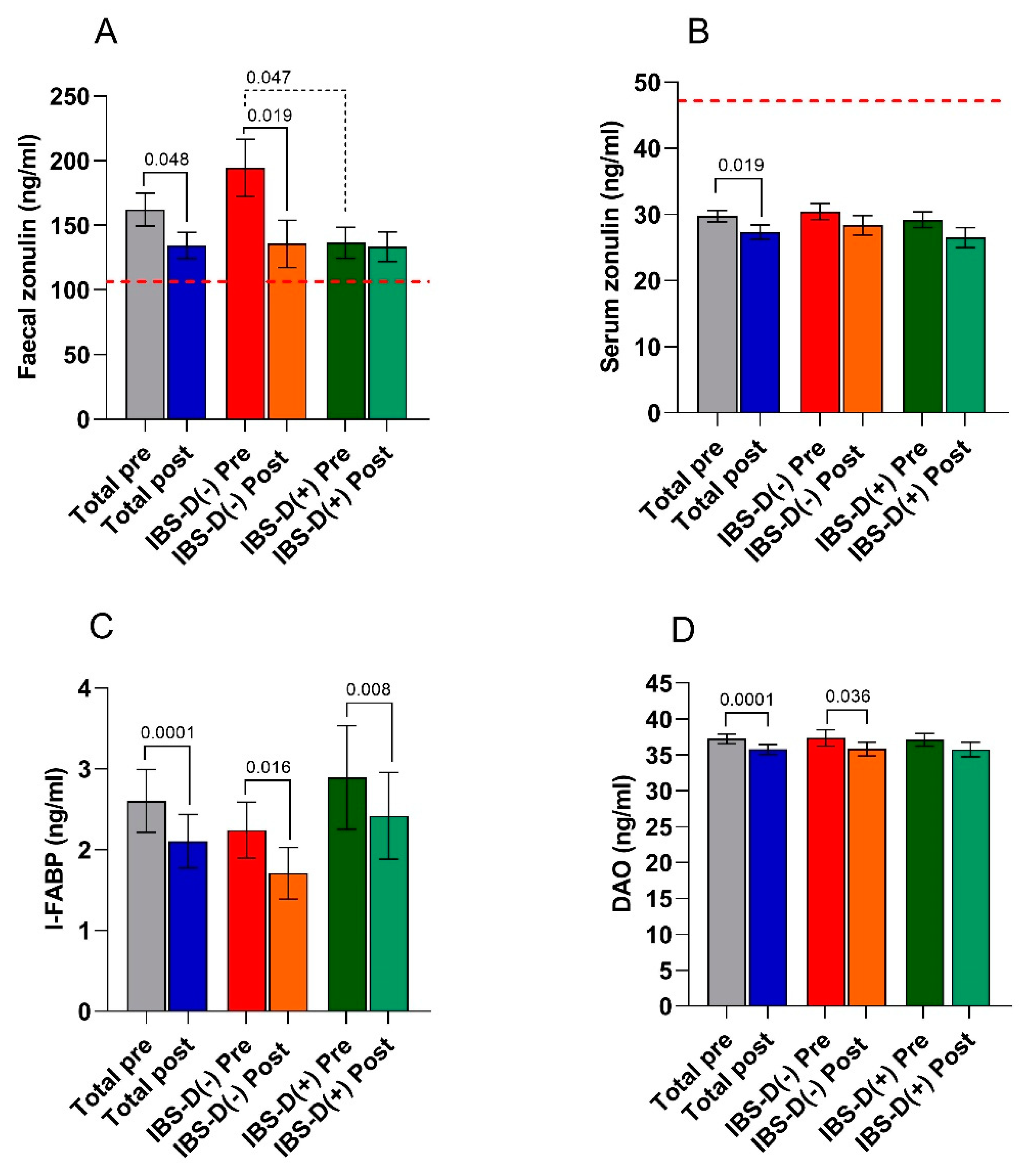
3.5. Biomarkers of Intestinal Barrier Function and Integrity
3.6. Indices of Inflammation
3.7. The Markers of Intestinal Dysbiosis and Bacterial Translocation
3.8. Correlation and Regression Analyses
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Brett, N.R.; Lavery, P.; Agellon, S.; Vanstone, C.A.; Goruk, S.; Field, C.J.; Weiler, H.A. Vitamin D Status and Immune Health Outcomes in a Cross-Sectional Study and a Randomized Trial of Healthy Young Children. Nutrients 2018, 10, 680. [Google Scholar] [CrossRef] [PubMed]
- Sassi, F.; Tamone, C.; D’Amelio, P. Vitamin D: Nutrient, Hormone, and Immunomodulator. Nutrients 2018, 10, 1656. [Google Scholar] [CrossRef]
- Panarese, A.; Pesce, F.; Porcelli, P.; Riezzo, G.; Iacovazzi, P.A.; Leone, C.M.; De Carne, M.; Rinaldi, C.M.; Shahini, E. Chronic functional constipation is strongly linked to vitamin D deficiency. World J. Gastroenterol. 2019, 25, 1729–1740. [Google Scholar] [CrossRef]
- Tazzyman, S.; Richards, N.; Trueman, A.R.; Evans, A.L.; Grant, V.A.; Garaiova, I.; Plummer, S.F.; Williams, E.A.; Corfe, B.M. Vitamin D associates with improved quality of life in participants with irritable bowel syndrome: Outcomes from a pilot trial. BMJ Open Gastroenterol. 2015, 2, e000052. [Google Scholar] [CrossRef] [PubMed]
- Abbasnezhad, A.; Amani, R.; Hajiani, E.; Alavinejad, P.; Cheraghian, B.; Ghadiri, A. Effect of vitamin D on gastrointestinal symptoms and health-related quality of life in irritable bowel syndrome patients: A randomized double-blind clinical trial. Neurogastroenterol. Motil. 2016, 28, 1533–1544. [Google Scholar] [CrossRef]
- Gil, A.; Plaza-Diaz, J.; Mesa, M.D. Vitamin D: Classic and Novel Actions. Ann. Nutr. Metab. 2018, 72, 87–95. [Google Scholar] [CrossRef] [PubMed]
- Williams, C.E.; Williams, E.A.; Corfe, B.M. Vitamin D status in irritable bowel syndrome and the impact of supplementation on symptoms: What do we know and what do we need to know? Eur. J. Clin. Nutr. 2018, 72, 1358–1363. [Google Scholar] [CrossRef]
- Katrinaki, M.; Kampa, M.; Margioris, A.; Castanas, E.; Malliaraki, N. Vitamin D levels in a large Mediterranean cohort: Reconsidering normal cut-off values. Hormones (Athens) 2016, 15, 205–223. [Google Scholar] [CrossRef]
- Khalighi Sikaroudi, M.; Mokhtare, M.; Janani, L.; Faghihi Kashani, A.H.; Masoodi, M.; Agah, S.; Abbaspour, N.; Dehnad, A.; Shidfar, F. Vitamin d3 supplementation in diarrhea-predominant irritable bowel syndrome patients: The effects on symptoms improvement, serum corticotropin-releasing hormone, and interleukin-6—A randomized clinical trial. Complementary Med. Res. 2020, 27, 302–309. [Google Scholar] [CrossRef] [PubMed]
- Silva, M.C.; Furlanetto, T.W. Intestinal absorption of vitamin D: A systematic review. Nutr. Rev. 2018, 76, 60–76. [Google Scholar] [CrossRef]
- Assa, A.; Vong, L.; Pinnell, L.J.; Avitzur, N.; Johnson-Henry, K.C.; Sherman, P.M. Vitamin d deficiency promotes epithelial barrier dysfunction and intestinal inflammation. J. Infect. Dis. 2014, 210, 1296–1305. [Google Scholar] [CrossRef]
- Fakhoury, H.M.A.; Kvietys, P.R.; Al Kattan, W.; Anouti, F.A.; Elahi, M.A.; Karras, S.N.; Grant, W.B. Vitamin D and intestinal homeostasis: Barrier, microbiota, and immune modulation. J. Steroid Biochem. Mol. Biol. 2020, 200, 105663. [Google Scholar] [CrossRef] [PubMed]
- Akimbekov, N.S.; Digel, I.; Sherelkhan, D.K.; Lutfor, A.B.; Razzaque, M.S. Vitamin D and the Host-Gut Microbiome: A Brief Overview. Acta Histochem. Cytochem. 2020, 53, 33–42. [Google Scholar] [CrossRef] [PubMed]
- Linsalata, M.; Riezzo, G.; D’Attoma, B.; Clemente, C.; Orlando, A.; Russo, F. Noninvasive biomarkers of gut barrier function identify two subtypes of patients suffering from diarrhoea predominant-ibs: A case-control study. BMC Gastroenterol. 2018, 18, 167. [Google Scholar] [CrossRef] [PubMed]
- Wells, J.M.; Brummer, R.J.; Derrien, M.; MacDonald, T.T.; Troost, F.; Cani, P.D.; Theodorou, V.; Dekker, J.; Meheust, A.; de Vos, W.M.; et al. Homeostasis of the gut barrier and potential biomarkers. Am. J. Physiol. Gastrointest. Liver Physiol. 2017, 312, G171–G193. [Google Scholar] [CrossRef]
- Linsalata, M.; Riezzo, G.; Clemente, C.; D’Attoma, B.; Russo, F. Noninvasive biomarkers of gut barrier function in patients suffering from diarrhea predominant-ibs: An update. Dis. Markers 2020, 2020, 2886268. [Google Scholar] [CrossRef] [PubMed]
- Camilleri, M. Leaky gut: Mechanisms, measurement and clinical implications in humans. Gut 2019, 68, 1516–1526. [Google Scholar] [CrossRef]
- Fasano, A. Zonulin and its regulation of intestinal barrier function: The biological door to inflammation, autoimmunity, and cancer. Physiol. Rev. 2011, 91, 151–175. [Google Scholar] [CrossRef]
- Pelsers, M.M.; Hermens, W.T.; Glatz, J.F. Fatty acid-binding proteins as plasma markers of tissue injury. Clin. Chim. Acta 2005, 352, 15–35. [Google Scholar] [CrossRef] [PubMed]
- Song, W.B.; Lv, Y.H.; Zhang, Z.S.; Li, Y.N.; Xiao, L.P.; Yu, X.P.; Wang, Y.Y.; Ji, H.L.; Ma, L. Soluble intercellular adhesion molecule-1, D-lactate and diamine oxidase in patients with inflammatory bowel disease. World J. Gastroenterol. 2009, 15, 3916–3919. [Google Scholar] [CrossRef] [PubMed]
- Zhang, L.; Fan, X.; Zhong, Z.; Xu, G.; Shen, J. Association of plasma diamine oxidase and intestinal fatty acid-binding protein with severity of disease in patient with heat stroke. Am. J. Emerg. Med. 2015, 33, 867–871. [Google Scholar] [CrossRef]
- Tuck, C.J.; Reed, D.E.; Muir, J.G.; Vanner, S.J. Implementation of the low FODMAP diet in functional gastrointestinal symptoms: A real-world experience. Neurogastroenterol. Motil. 2020, 32, e13730. [Google Scholar] [CrossRef] [PubMed]
- Orlando, A.; Tutino, V.; Notarnicola, M.; Riezzo, G.; Linsalata, M.; Clemente, C.; Prospero, L.; Martulli, M.; D’Attoma, B.; De Nunzio, V.; et al. Improved Symptom Profiles and Minimal Inflammation in IBS-D Patients Undergoing a Long-Term Low-FODMAP Diet: A Lipidomic Perspective. Nutrients 2020, 12, 1652. [Google Scholar] [CrossRef] [PubMed]
- Francis, C.Y.; Morris, J.; Whorwell, P.J. The irritable bowel severity scoring system: A simple method of monitoring irritable bowel syndrome and its progress. Aliment. Pharmacol. Ther. 1997, 11, 395–402. [Google Scholar] [CrossRef] [PubMed]
- Kulich, K.R.; Madisch, A.; Pacini, F.; Pique, J.M.; Regula, J.; Van Rensburg, C.J.; Ujszaszy, L.; Carlsson, J.; Halling, K.; Wiklund, I.K. Reliability and validity of the Gastrointestinal Symptom Rating Scale (GSRS) and Quality of Life in Reflux and Dyspepsia (QOLRAD) questionnaire in dyspepsia: A six-country study. Health Qual. Life Outcomes 2008, 6, 12. [Google Scholar] [CrossRef]
- Schmulson, M.J.; Drossman, D.A. What Is New in Rome IV. J. Neurogastroenterol. Motil. 2017, 23, 151–163. [Google Scholar] [CrossRef]
- Verdu, E.F.; Armstrong, D.; Murray, J.A. Between celiac disease and irritable bowel syndrome: The “no man’s land” of gluten sensitivity. Am. J. Gastroenterol. 2009, 104, 1587–1594. [Google Scholar] [CrossRef] [PubMed]
- Blake, M.R.; Raker, J.M.; Whelan, K. Validity and reliability of the Bristol Stool Form Scale in healthy adults and patients with diarrhoea-predominant irritable bowel syndrome. Aliment Pharmacol. Ther. 2016, 44, 693–703. [Google Scholar] [CrossRef]
- Maagaard, L.; Ankersen, D.V.; Vegh, Z.; Burisch, J.; Jensen, L.; Pedersen, N.; Munkholm, P. Follow-up of patients with functional bowel symptoms treated with a low FODMAP diet. World J. Gastroenterol. 2016, 22, 4009–4019. [Google Scholar] [CrossRef] [PubMed]
- MonashUniversity (2017) The Monash University Low FODMAP App. Available online: https://www.monashfodmap.com/ibs-central/i-have-ibs/get-the-app/ (accessed on 4 September 2019).
- Linsalata, M.; D’Attoma, B.; Orlando, A.; Guerra, V.; Russo, F. Comparison of an enzymatic assay with liquid chromatography-pulsed amperometric detection for the determination of lactulose and mannitol in urine of healthy subjects and patients with active celiac disease. Clin. Chem. Lab. Med. 2014, 52, e61–e64. [Google Scholar] [CrossRef] [PubMed]
- Hilsden, R.J.; Meddings, J.B.; Sutherland, L.R. Intestinal permeability changes in response to acetylsalicylic acid in relatives of patients with Crohn’s disease. Gastroenterology 1996, 110, 1395–1403. [Google Scholar] [CrossRef]
- Simeoni, M.; Citraro, M.L.; Cerantonio, A.; Deodato, F.; Provenzano, M.; Cianfrone, P.; Capria, M.; Corrado, S.; Libri, E.; Comi, A.; et al. An open-label, randomized, placebo-controlled study on the effectiveness of a novel probiotics administration protocol (ProbiotiCKD) in patients with mild renal insufficiency (stage 3a of CKD). Eur. J. Nutr. 2019, 58, 2145–2156. [Google Scholar] [CrossRef]
- Meeker, S.; Seamons, A.; Maggio-Price, L.; Paik, J. Protective links between vitamin D, inflammatory bowel disease and colon cancer. World J. Gastroenterol. 2016, 22, 933–948. [Google Scholar] [CrossRef] [PubMed]
- Barbalho, S.M.; Goulart, R.A.; Araujo, A.C.; Guiguer, E.L.; Bechara, M.D. Irritable bowel syndrome: A review of the general aspects and the potential role of vitamin D. Expert Rev. Gastroenterol. Hepatol. 2019, 13, 345–359. [Google Scholar] [CrossRef]
- Eslamian, G.; Ardehali, S.H.; Hajimohammadebrahim-Ketabforoush, M.; Vahdat Shariatpanahi, Z. Association of intestinal permeability with admission vitamin D deficiency in patients who are critically ill. J. Investig. Med. 2020, 68, 397–402. [Google Scholar] [CrossRef]
- Kong, J.; Zhang, Z.; Musch, M.W.; Ning, G.; Sun, J.; Hart, J.; Bissonnette, M.; Li, Y.C. Novel role of the vitamin D receptor in maintaining the integrity of the intestinal mucosal barrier. Am. J. Physiol. Gastrointest. Liver Physiol. 2008, 294, G208–G216. [Google Scholar] [CrossRef] [PubMed]
- Zhu, T.; Liu, T.J.; Shi, Y.Y.; Zhao, Q. Vitamin D/VDR signaling pathway ameliorates 2,4,6-trinitrobenzene sulfonic acid-induced colitis by inhibiting intestinal epithelial apoptosis. Int. J. Mol. Med. 2015, 35, 1213–1218. [Google Scholar] [CrossRef] [PubMed]
- Raftery, T.; Martineau, A.R.; Greiller, C.L.; Ghosh, S.; McNamara, D.; Bennett, K.; Meddings, J.; O’Sullivan, M. Effects of vitamin D supplementation on intestinal permeability, cathelicidin and disease markers in Crohn’s disease: Results from a randomised double-blind placebo-controlled study. United Eur. Gastroenterol. J. 2015, 3, 294–302. [Google Scholar] [CrossRef] [PubMed]
- McCabe, P.S.; Pye, S.R.; Beth, J.M.; Lee, D.M.; Tajar, A.; Bartfai, G.; Boonen, S.; Bouillon, R.; Casanueva, F.; Finn, J.D.; et al. Low vitamin D and the risk of developing chronic widespread pain: Results from the European male ageing study. BMC Musculoskelet. Disord. 2016, 17, 32. [Google Scholar] [CrossRef]
- Jalili, M.; Vahedi, H.; Poustchi, H.; Hekmatdoost, A. Effects of Vitamin D Supplementation in Patients with Irritable Bowel Syndrome: A Randomized, Double-Blind, Placebo-Controlled Clinical Trial. Int. J. Prev. Med. 2019, 10, 16. [Google Scholar] [CrossRef]
- Bicikova, M.; Duskova, M.; Vitku, J.; Kalvachova, B.; Ripova, D.; Mohr, P.; Starka, L. Vitamin D in anxiety and affective disorders. Physiol. Res. 2015, 64, S101–S103. [Google Scholar] [CrossRef]
- Ajamian, M.; Rosella, G.; Newnham, E.D.; Biesiekierski, J.R.; Muir, J.G.; Gibson, P.R. Effect of Gluten Ingestion and FODMAP Restriction on Intestinal Epithelial Integrity in Patients with Irritable Bowel Syndrome and Self-Reported Non-Coeliac Gluten Sensitivity. Mol. Nutr. Food Res. 2020, e1901275. [Google Scholar] [CrossRef]
- Zhou, S.Y.; Gillilland, M., III; Wu, X.; Leelasinjaroen, P.; Zhang, G.; Zhou, H.; Ye, B.; Lu, Y.; Owyang, C. FODMAP diet modulates visceral nociception by lipopolysaccharide-mediated intestinal inflammation and barrier dysfunction. J. Clin. Investig. 2018, 128, 267–280. [Google Scholar] [CrossRef]
- Harvie, R.M.; Chisholm, A.W.; Bisanz, J.E.; Burton, J.P.; Herbison, P.; Schultz, K.; Schultz, M. Long-term irritable bowel syndrome symptom control with reintroduction of selected FODMAPs. World J. Gastroenterol. 2017, 23, 4632–4643. [Google Scholar] [CrossRef] [PubMed]
- Gibson, P.R.; Shepherd, S.J. Evidence-based dietary management of functional gastrointestinal symptoms: The FODMAP approach. J. Gastroenterol. Hepatol. 2010, 25, 252–258. [Google Scholar] [CrossRef] [PubMed]
- Bascunan, K.A.; Elli, L.; Pellegrini, N.; Scricciolo, A.; Lombardo, V.; Doneda, L.; Vecchi, M.; Scarpa, C.; Araya, M.; Roncoroni, L. Impact of FODMAP Content Restrictions on the Quality of Diet for Patients with Celiac Disease on a Gluten-Free Diet. Nutrients 2019, 11, 2220. [Google Scholar] [CrossRef] [PubMed]
- Vincenzi, M.; Del Ciondolo, I.; Pasquini, E.; Gennai, K.; Paolini, B. Effects of a Low FODMAP Diet and Specific Carbohydrate Diet on Symptoms and Nutritional Adequacy of Patients with Irritable Bowel Syndrome: Preliminary Results of a Single-blinded Randomized Trial. J. Transl. Int. Med. 2017, 5, 120–126. [Google Scholar] [CrossRef] [PubMed]
- Maes, M.; Kubera, M.; Leunis, J.C. The gut-brain barrier in major depression: Intestinal mucosal dysfunction with an increased translocation of LPS from gram negative enterobacteria (leaky gut) plays a role in the inflammatory pathophysiology of depression. Neuro Endocrinol. Lett. 2008, 29, 117–124. [Google Scholar]

| Total Pre (n = 36) | Total Post (n = 36) | Rank-Sum Test p | L-VD Pre (n = 16) | L-VD Post (n = 16) | Rank-Sum Test p | N-VD Pre (n = 20) | N-VD Post (n = 20) | Rank-Sum Test p | |
|---|---|---|---|---|---|---|---|---|---|
| Age (Years) | 43.10 ± 1.70 | // | // | 43.90 ± 2.90 | // | // | 42.50 ± 2.00 | // | // |
| Height (cm) | 1.60 ± 0.01 | // | // | 1.60 ± 0.10 | // | // | 1.60 ± 0.020 | // | // |
| Weight (kg) | 65.50 ± 2.10 | 62.00 ± 1.90 | <0.001 | 66.70 ± 3.70 | 63.50 ± 3.60 | <0.001 | 64.60 ± 2.30 | 60.80 ± 2.10 | <0.001 |
| BMI (kg/m2) | 25.10 ± 0.80 | 23.80 ± 0.80 | <0.001 | 25.90 ± 1.40 | 24.70 ± 1.40 | <0.001 | 24.50 ± 0.80 | 23.20 ± 0.80 | <0.001 |
| Abdominal circumference (cm) | 88.90 ± 1.80 | 86.20 ± 1.80 | <0.001 | 89.10 ± 3.30 | 86.40 ± 3.20 | 0.034 | 88.90 ± 1.90 | 86.00 ± 2.10 | <0.001 |
| Waist circumference (cm) | 79.10 ± 2.00 | 76.30 ± 1.90 | <0.001 | 79.80 ± 3.80 | 77.70 ± 3.50 | 0.011 | 78.60 ± 2.20 | 75.30 ± 1.90 | <0.001 |
| Creatinine (mg/dL) | 0.76 ± 0.04 | 0.75 ± 0.04 | 0.85 | 0.73 ± 0.05 | 0.74 ± 0.05 | 0.68 | 0.78 ± 0.05 | 0.76 ± 0.05 | 0.63 |
| Urea (mg/dL) | 32.64 ± 1.38 | 33.91 ± 1.20 | 0.31 | 33.25 ± 2.15 | 33.87 ± 1.50 | 0.93 | 32.16 ± 1.83 | 33.84 ± 1.75 | 0.33 |
| Calcium (mg/dL) | 9.42 ± 0.07 | 8.84 ± 0.06 | <0.001 | 9.46 ± 0.10 | 8.84 ± 0.07 | <0.001 | 9.39 ± 0.10 | 8.84 ± 0.10 | <0.001 |
| Phosphorous (mg/dL) | 3.64 ± 0.13 | 3.65 ± 0.12 | 0.83 | 3.45 ± 0.19 | 3.45 ± 0.18 | 0.79 | 3.79 ± 0.17 | 3.80 ± 0.16 | 0.95 |
| PTH (pg/mL) | 42.37 ± 2.31 | 42.85 ± 2.32 | <0.001 | 43.45 ± 3.30 | 43.93 ± 3.33 | <0.001 | 41.50 ± 3.28 | 41.99 ± 3.28 | <0.001 |
| Total Pre (n = 36) | Total Post (n = 36) | p | |
|---|---|---|---|
| Energy consumption (kcal) | 2062 ± 68.54 | 2058 ± 67.55 | 0.967 |
| Energy intake (kcal) | 2054 ± 129.30 | 1811 ± 92.22 | 0.058 |
| Basal metabolism (kcal) | 1485 ± 29.86 | 1502 ± 32.80 | 0.056 |
| Proteins (g) | 78.81 ± 4.60 | 86.81 ± 3.97 | 0.783 |
| Proteins (%) | 15.91 ± 0.31 | 19.50 ± 0.16 | <0.0001 |
| Lipids (g) | 87.28 ± 7.36 | 59.09 ± 3.12 | 0.0011 |
| Lipids (%) | 36.35 ± 0.88 | 29.67 ± 0.17 | <0.0001 |
| Carbohydrates (g) | 236.40 ± 11.75 | 242.40 ± 12.94 | 0.237 |
| Carbohydrates (%) | 47.24 ± 0.88 | 50.54 ± 0.24 | 0.002 |
| Alcohol (%) | 0.74 ± 0.21 | 0.29 ± 0.12 | 0.178 |
| Dietary fiber (g) | 18.05 ± 0.76 | 16.97 ± 0.92 | 0.060 |
| Total FODMAPs (g/day) | 20.71 ± 0.80 | 3.26 ± 0.08 | <0.0001 |
| Calcium (mg) | 813.80 ± 6.17 | 789.10 ± 11.18 | 0.061 |
| Chloride (mg) | 3.97 ± 0.03 | 3.89 ± 0.06 | 0.118 |
| Copper (mg) | 1.30 ± 0.01 | 1.25 ± 0.02 | 0.104 |
| Iodine (µg) | 117.7 ± 0.98 | 122.6 ± 2.81 | 0.056 |
| Iron (mg) | 11.54 ± 0.07 | 10.94 ± 0.27 | 0.064 |
| Magnesium (mg) | 279.3 ± 1.87 | 275.6 ± 2.13 | 0.072 |
| Potassium (mg) | 2.82 ± 0.01 | 2.87 ± 0.04 | 0.133 |
| Phosphorous (mg) | 1.25 ± 0.01 | 1.24 ± 0.01 | 0.064 |
| Selenium (µg) | 45.31 ± 0.40 | 47.17 ± 1.05 | 0.119 |
| Sodium (mg) | 2.74 ± 0.01 | 2.68 ± 0.05 | 0.120 |
| Zinc (mg) | 8.51 ± 0.05 | 8.34 ± 0.07 | 0.060 |
| Vitamin A (µg) | 1.04 ± 0.03 | 1.11 ± 0.03 | 0.089 |
| Vitamin B6 (mg) | 1.92 ± 0.05 | 2.01 ± 0.02 | 0.217 |
| Vitamin B12 (µg) | 5.14 ± 0.12 | 5.47 ± 0.11 | 0.074 |
| Vitamin C (mg) | 95.64 ± 1.54 | 98.50 ± 1.70 | 0.070 |
| Niacin (mg) | 19.98 ± 0.13 | 20.46 ± 0.20 | 0.060 |
| Riboflavin (mg) | 1.51 ± 0.01 | 1.45 ± 0.02 | 0.077 |
| Thiamin (mg) | 1.50 ± 0.02 | 1.44 ± 0.02 | 0.078 |
| Folate (µg) | 231.60 ± 1.99 | 227.0 ± 2.30 | 0.118 |
| Total Pre (n = 36) | Total Post (n = 36) | Rank-Sum Test p | L-VD Pre (n = 16) | L-VD Post (n = 16) | Rank-Sum Test p | N-VD Pre (n = 20) | N-VD Post (n = 20) | Rank-Sum Test p | |
|---|---|---|---|---|---|---|---|---|---|
| Abdominal pain intensity | 48.3 ±3.7 | 22.9 ± 3.5 | <0.001 | 59.0 ± 4.6 a | 30.0 ± 6.3 | 0.003 | 40.0 ± 4.8 a | 17.1 ± 3.4 | <0.001 |
| Abdominal pain frequency | 43.3 ± 4.5 | 22.6 ± 4.2 | <0.001 | 58.0 ± 6.2 b | 26.9 ± 7.2 | 0.002 | 38.0 ± 5.5 b | 19.1 ± 5.0 | 0.014 |
| Abdominal distension | 55.9 ± 3.7 | 26.3 ± 3.6 | <0.001 | 54.2 ± 6.7 | 28.7 ± 5.8 | 0.005 | 57.1 ± 4.2 | 24.4 ± 4.5 | <0.001 |
| Dissatisfaction of bowel habit | 67.8 ± 3.7 | 35,7 ± 3.9 | <0.001 | 72.3 ± 4.3 | 40.4 ± 6.3 | 0.002 | 64.2 ± 5.8 | 31.8 ± 4.8 | <0.001 |
| Interference on life in general | 57.8 ± 3.2 | 34.5 ± 4.2 | <0.001 | 65.0 ± 4.4 c | 40.3 ± 6.8 | 0.005 | 48.0 ± 5.2 c | 29.8 ± 5.1 | 0.003 |
| Stool frequency | 1.9 ± 0.2 | 1.3 ± 0.1 | <0.001 | 2.3 ± 0.2 d | 1.5 ± 0.2 | 0.014 | 1.7 ± 0.2 d | 1.22 ± 0.2 | 0.008 |
| Total score | 273.1 ± 12.6 | 141.9 ± 15.1 | <0.001 | 308.0 ± 14.0 e | 166.4 ± 25.5 | <0.001 | 246.0 ± 15.0 e | 122.3 ± 17.2 | <0.001 |
| Total Pre (n = 36) | Total Post (n = 36) | Rank-Sum Test p | L-VD Pre (n = 16) | L-VD Post (n = 16) | Rank-Sum Test p | N-VD Pre (n = 20) | N-VD Post (n = 20) | Rank-Sum Test p | |
|---|---|---|---|---|---|---|---|---|---|
| IL-6 (pg/mL) | 5.3 ± 0.13 | 5.1 ± 0.13 | 0.020 | 5.4 ± 0.24 | 5.1 ± 0.21 | 0.232 | 5.3 ± 0.2 | 5.1 ± 0.2 | 0.052 |
| IL-8 (pg/mL) | 4.5 ± 0.40 | 4.0 ± 0.16 | 0.019 | 4.0 ± 0.18 | 3.8 ± 0.14 | 0.109 | 4.9 ± 0.71 | 4.2 ± 0.26 | 0.113 |
| Parameters | β | Std. Error (β) | p | 95% CI |
|---|---|---|---|---|
| IBS-SSS tot | −0.047 | 0.015 | 0.002 | −0.075–−0.018 |
| Fecal zonulin | −0.065 | 0.022 | 0.004 | −0.108–−0.022 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Linsalata, M.; Riezzo, G.; Orlando, A.; D’Attoma, B.; Prospero, L.; Tutino, V.; Notarnicola, M.; Russo, F. The Relationship between Low Serum Vitamin D Levels and Altered Intestinal Barrier Function in Patients with IBS Diarrhoea Undergoing a Long-Term Low-FODMAP Diet: Novel Observations from a Clinical Trial. Nutrients 2021, 13, 1011. https://doi.org/10.3390/nu13031011
Linsalata M, Riezzo G, Orlando A, D’Attoma B, Prospero L, Tutino V, Notarnicola M, Russo F. The Relationship between Low Serum Vitamin D Levels and Altered Intestinal Barrier Function in Patients with IBS Diarrhoea Undergoing a Long-Term Low-FODMAP Diet: Novel Observations from a Clinical Trial. Nutrients. 2021; 13(3):1011. https://doi.org/10.3390/nu13031011
Chicago/Turabian StyleLinsalata, Michele, Giuseppe Riezzo, Antonella Orlando, Benedetta D’Attoma, Laura Prospero, Valeria Tutino, Maria Notarnicola, and Francesco Russo. 2021. "The Relationship between Low Serum Vitamin D Levels and Altered Intestinal Barrier Function in Patients with IBS Diarrhoea Undergoing a Long-Term Low-FODMAP Diet: Novel Observations from a Clinical Trial" Nutrients 13, no. 3: 1011. https://doi.org/10.3390/nu13031011
APA StyleLinsalata, M., Riezzo, G., Orlando, A., D’Attoma, B., Prospero, L., Tutino, V., Notarnicola, M., & Russo, F. (2021). The Relationship between Low Serum Vitamin D Levels and Altered Intestinal Barrier Function in Patients with IBS Diarrhoea Undergoing a Long-Term Low-FODMAP Diet: Novel Observations from a Clinical Trial. Nutrients, 13(3), 1011. https://doi.org/10.3390/nu13031011







