Abstract
Alzheimer’s disease (AD) is the most common type of dementia leading to progressive memory loss and cognitive impairment. Considering that pharmacological treatment options for AD are few and not satisfactory, increasing attention is being paid to dietary components that may affect the development of the disease. Such a dietary component may be caffeine contained in coffee, tea or energy drinks. Although epidemiological data suggest that caffeine intake may counteract the development of cognitive impairment, results of those studies are not conclusive. The aim of the present study is to review the existing experimental studies on the efficacy of caffeine against AD and AD-related cognitive impairment, focusing on the proposed protective mechanisms of action. In conclusion, the reports of studies on experimental AD models generally supported the notion that caffeine may exert some beneficial effects in AD. However, further studies are necessary to elucidate the role of caffeine in the effects of its sources on cognition and possibly AD risk.
1. Introduction
Alzheimer’s disease (AD) is the most common type of dementia, accounting for 50–70% of neurodegenerative dementia cases. AD leads to a progressive loss of memory and cognitive abilities [1].
It is believed, especially taking into account very limited therapeutic options, that dietary interventions or nutraceuticals may be promising in the prophylaxis and treatment of cognitive impairment of ageing, including AD [2,3,4,5,6,7]. The effects of dietary components are usually evaluated based on dietary questionnaires, and the results of those studies, as well as the results of their meta-analyses are often not conclusive. The number of randomized controlled trials concerning phytochemicals is low [4]. On the other hand, numerous experimental studies indicated phytochemicals as potentially useful in the prophylaxis of AD, including flavonoids, phenolic acids, carotenoids, curcumin, resveratrol, and some alkaloids (for comprehensive review—see [4,6]). From among those phytochemicals, the effects of caffeine seem to be the most thoroughly examined and best documented.
Caffeine (1,3,7-trimethylxanthine) is a purine alkaloid, commonly consumed on a daily basis. Caffeine is probably the most commonly used psychoactive substance/psychostimulant [8,9,10]. It is found in coffee (Coffea L.) beans, cola (Cola acuminata (P. Beauv.) Schott and Endl.) nuts, tea (Camellia sinensis (L.) Kuntze) leaves and yerba mate (Ilex paraguariensis A.St.-Hil.) leaves, as well as guarana (Paullinia cupana Kunth) seeds and cocoa (Theobroma cacao L.) beans [4,10]. The main dietary source of caffeine is coffee, tea and yerba mate [11]. Caffeine is also present in soft drinks (cola-type) and energy drinks, used mainly by younger individuals [8]. The mean caffeine intake varies between countries, however it has remained stable in adults in the last 10–15 years [12]. According to the recommendations of the European Food Safety Authority (EFSA), the daily caffeine intake up to 400 mg is considered safe for healthy adults [13,14].
Numerous health-promoting activities are attributed to coffee and caffeine. A recent umbrella review of meta-analyses indicated, among others, beneficial role of coffee in reducing risk of type 2 diabetes mellitus (T2D), cardiovascular diseases, some cancers and Parkinson’s disease [15,16]. The results of epidemiological and experimental studies suggest also a possible beneficial effect of caffeine in the prevention of AD [17,18,19,20]. However, human studies concerned caffeine contained in the diet and cannot isolate caffeine’s effects from countless lifestyle choices people make.
Here we would like to focus on the results of experimental studies of caffeine, carried out in order to evaluate its potential in the prophylaxis and treatment of AD. A literature search was conducted on the PubMed electronic database. Articles presented in languages other than English were excluded. Results of all studies on caffeine effects in different AD experimental models, published until December 2020, and found in the PubMed electronic database, were referred to in the present review.
2. Caffeine—Main Mechanisms of Action
The mechanism of action of caffeine is complex. Caffeine is a non-selective antagonist of adenosine receptors (mainly A1 and A2A), demonstrating a structural similarity to adenosine. The blocking of these receptors modulates glutamatergic, cholinergic, dopaminergic, serotoninergic and noradrenergic neurotransmission [8,21,22]. The blockade of adenosine receptors is observed in lower concentrations of caffeine (<250 µM) [22]. Moreover, caffeine is an agonist of ryanodine receptors (RyRs), stimulation of which increases the release of Ca2+ from the endoplasmic reticulum [23,24]. Caffeine is also a non-selective competitive inhibitor of phosphodiesterases (PDEs), the enzymes degrading cyclic adenosine monophosphate (cAMP), which leads to increases in the cell cAMP concentration [8,23]. However, the effect of caffeine through the signaling pathways associated with the stimulation of RyRs and the blocking of PDEs is only possible at higher doses (plasma concentration >250 µM) [22,23,25]. Caffeine also interferes with γ-aminobutyric acid type A (GABAA) receptors [24,26,27]. Caffeine protects against cell damage, exerts antioxidant effects, reducing oxidative stress markers [23,28]. Caffeine may exert also anti-inflammatory activity, decreasing proinflammatory (C-reactive protein, interleukin (IL)-1β, IL-6, IL-18, tumor necrosis factor α—TNF-α) and increasing anti-inflammatory (IL-10, adiponectin) marker levels [23,29,30].
3. Alzheimer’s Disease (AD)
AD is characterized by personality disorders, amnesia, dementia and cognitive impairment [31]. Brain atrophy observed in AD results from the synaptic degeneration and neuronal cell death. Dysfunctions occur mainly in the brain regions that play a major role in memory and spatial orientation, i.e., in the hippocampus, striatum, cerebral cortex, thalamus and amygdala [32,33]. Besides cognitive dysfunctions, the majority of patients with AD suffer from behavioral and psychological symptoms of dementia (BPSD). BPSD include depression, apathy, anxiety, sleep changes, hallucinations, delusions and agitation [34,35,36].
There are two major forms of AD—familial (or early-onset) and sporadic. Familial AD (FAD), 5% of AD cases [35,37], is caused by mutations in genes encoding three proteins—amyloid precursor protein (APP), presenilin 1 (PS1) and presenilin 2 (PS2) [38]. The cause of the sporadic forms of AD is unknown; the majority of them develop after 65 years of age [39]. The ε-4 allele of the apolipoprotein E (APOE) is a risk factor in the pathogenesis of late-onset of AD, playing an important role in amyloid β (Aβ) brain metabolism (APOE ε-4 exacerbates deposition of Aβ in the brain and tau-mediated neurodegeneration) [40,41,42]. Among various risk factors associated with AD, T2D, traumatic brain injury, cerebrovascular disease, hypertension, dyslipidemia, obesity and metabolic syndrome have been demonstrated [43,44]. There is a hypothesis that the sporadic type of AD is triggered by dysfunctional insulin signaling in the brain; it has been proposed that sporadic AD may be considered the brain type of diabetes [45] or type 3 diabetes [46,47].
The most popular hypothesis on the pathogenesis of AD is the amyloid hypothesis, which assumes an important role of Aβ deposits in the form of senile plaques [48,49]. In fact, the neuropathological hallmarks of AD are the presence of extracellular neuritic plaques, consisting of deposits of Aβ peptides and intraneuronal neurofibrillary tangles (NFTs) composed of aggregated and often truncated, and hyperphosphorylated tau protein [1,50,51].
Aβ is formed as a result of incorrect fragmentation of the amyloid precursor protein (APP) processed by β-secretases (β-site amyloid-precursor-protein-cleaving enzyme-1—BACE-1 and BACE-2) and γ-secretases [52]. Senile plaques activate microglial cells and induce inflammation [49,52,53]. In AD, the tau protein uncouples from microtubules, aggregates into tangles and inhibits microtubular transport [50]. Hyperphosphorylation of tau protein causes dysregulation of the neuronal system and axon damage [52]. Also, neuroinflammation is considered to be involved in the pathogenesis of AD [53]. Proinflammatory cytokines (TNF-α, IL-1 and IL-6), reactive oxygen species (ROS) and NO production leads to dysfunction of the blood–brain barrier (BBB) and the influx of immunocompetent cells [32]. The associated oxidative stress causes lipid and neuronal protein oxidation [48,52]. Inflammation-related biomarkers are present in the cerebrospinal fluid, peripheral blood and brain in AD patients [49,53,54].
Neurodegenerative disorders in AD lead to decreases in the levels of neurotransmitters. An important role in the pathogenesis of AD is a reduction of acetylcholine (ACh) content. The dysfunction of cholinergic system is related to degeneration of the nucleus basalis of Meynert cholinergic neurons caused by NFTs formation. The presence of NFTs and Aβ plaques leads to cholinergic synapse loss. Moreover, despite the preservation of postsynaptic M1 muscarinic receptors (the level of presynaptic M2 receptors is decreased) in the cerebral cortex, their functions are impaired. Also, progressive decrease in the number of nicotinic receptors in the cerebral cortex is observed. Deficits in cholinergic neurotransmission contribute to the learning, memory and attention impairment [55,56]. Moreover, it has been demonstrated that interaction between cholinergic and glutamatergic transmission is involved in Ca2+-dependent neuroprotection [56]. The glutamatergic system is controlled by various mediators, including adenosine and ACh [56,57,58]. In AD, there is a decrease in the number of the N-methyl-D-aspartate (NMDA) receptors resulting in an imbalance between synaptic and extrasynaptic NMDA receptors [59,60]. Malfunctioning glutamatergic neurons release too much glutamate, which over-stimulates the extrasynaptic NMDA receptors leading to the neuronal cell death and synaptic loss [59]. Moreover, cholinergic neuronal loss leads to dopaminergic transmission dysfunction which is correlated with psychiatric symptoms of AD (BPSD) [55,56]. Also, the loss of noradrenergic neurons in the locus coeruleus caused by the tau protein accumulation results in the progression of AD. Noradrenergic receptors (mainly α2 receptor activation or β receptor blockade) are involved in the Aβ-related neuropathology. Upregulation of adenosine receptors (A1R and A2AR) is also observed in AD. Activation of adenosine receptors affects synaptic neurotransmission and various neurotransmitters release (ACh, glutamate) [58]. Moreover, it disrupts learning and memory processes and leads to cognitive disorders [58,61]. Also, dysregulated signaling by other purinergic receptors may be involved in the pathomechanism of AD. Activation of P2X7 receptors by high levels of adenosine triphosphate—ATP or its metabolites (Aβ accumulation induces increased release of ATP) leads to neuroinflammation, i.e., increased level of IL-1, IL-6, IL-18, TNF-α and interferon-γ, and neurodegeneration [62].
Summing up, cholinergic and glutamatergic transmission disorders are associated with impaired cognitive processes, while disorders of dopaminergic, serotonergic and noradrenergic transmission are responsible for the symptoms associated with dementia, such as depression, apathy, anxiety and psychotic symptoms [63].
Epidemiological studies demonstrated higher occurrence of AD (2:1 women to men ratio) and risk of developing AD in women compared to men. It is probably related to the longer life expectancy for women. In addition, faster cognitive decline and longer life span after diagnosis of mild cognitive impairment or AD dementia is observed in elderly women in comparison to men [64,65,66]. More aggressive behaviors and higher mortality is demonstrated in men, whereas women suffer from more severe symptoms of affective disorders [67].
The treatment options of AD are very limited. Currently, only four drugs are approved by Food and Drug Administration (FDA) and European Medicines Agency (EMA) for AD treatment. These include three drugs from the group of acetylcholinesterase (AChE) inhibitors (donepezil, rivastigmine and galantamine) and memantine, a selective and non-competitive NMDA receptor antagonist [68,69]. AChE inhibitors increase ACh levels in the synaptic cleft and partially improve cognitive function and the quality of a patient’s life [55]. Memantine restores NMDA receptor function and exerts neuroprotective effects, reducing the intracellular influx of calcium ions [70,71]. There is a great need to search for new therapeutic and prophylactic approaches to AD.
Taking into account the postulated pathomechanism of AD, it is believed that antioxidant nutraceuticals may have beneficial effects in the prevention of AD. The best-known antioxidants include plant polyphenols such as curcumin, flavonoids and phenolic acids. Experimental studies and/or population studies suggest the possibility of beneficial effects of curcumin [3,72,73,74], ferulic acid [3,75,76,77], epigallocatechin 3-gallate (EGCG) [3,78,79,80] and caffeine [18,19,20,21,23,81,82,83] in AD treatment and prevention.
4. Caffeine in Alzheimer’s Disease
The studies on the effects of caffeine consumption (coffee, tea, other sources) on the cognitive impairment, mild cognitive impairment, dementia and AD led to differential conclusions. Although the review articles and meta-analyses indicated rather favorable effects of caffeine-containing dietary sources on those disorders, their conclusions were not unequivocal [84,85,86,87,88,89,90]. For example, a latest systematic review supported the notion that green tea intake might reduce the risk of those disorders [86], but the meta-analysis of observational studies did not demonstrate the effect of tea drinking on AD specifically [87]. Similarly, the meta-analyses concerning coffee intake led to differential conclusions. A meta-analysis of prospective cohort studies demonstrated a “J-shaped” association between coffee intake and the occurrence of cognitive disorders (the lowest risk with daily consumption level of 1–2 cups of coffee) [88]. On the other hand, another analysis of prospective cohort studies found that higher coffee consumption was associated with reduced risk for AD [89]. The most recent meta-analysis of prospective studies did not support an association between coffee consumption and a risk of AD and overall dementia [90]. Moreover, it seems worth mentioning that studies using Mendelian randomization, which is a genetic epidemiological method, did not provide the evidence for a causal effect of habitual coffee consumption on global cognition or memory [91]. In fact, surprisingly, one study even suggested an association between genetically predicted higher consumption of coffee and higher risk of AD (the report concerned analysis of genome-wide association studies of the potentially modifiable risk factors of AD) [92].
It should be emphasized that other than caffeine active constituents of coffee or tea (like phenolic acids, EGCG, trigonelline) may contribute to their effects on cognition/AD risk [4,93]. Decaffeinated coffee constituents have been demonstrated to exert potential beneficial effects in neurodegenerative diseases [94]. However, decaffeinated coffee was not associated with a protective effect on cognitive performance in older people [95]. The data from the human studies do not allow to conclude on the role of caffeine itself in the modulation of AD risk. However, there is growing evidence on the effects of caffeine on cognition and AD development coming from numerous experimental studies.
5. Experimental Models of AD
It is crucial to use experimental models faithfully mimicking the pathologies of investigated diseases. In case of AD, it is problematic. None of the experimental AD animal models fully reflects complete disorders and cognitive impairments characteristic for human AD. Although FAD accounts for about 5% of all disease cases only, the majority of potential therapies has been investigated in transgenic mouse models of AD [42].
Transgenic technologies allowed mouse and rat models to be created, based on the mutations of APP, presenilin (PS), APOE and tau protein genes [37,42,96]. Mouse models are the most commonly used in the experimental studies on AD, due to their low prices, relatively short life span and similar AD symptoms to the human disease [96]. Histopathological changes in the brain tissue, depending on the mutation used, are characterized by the presence of Aβ plaques, tau protein deposits and hippocampus atrophy [1,56,97].
APP mutations causing cognitive deficits in mice and rats are related to an increased Aβ production, increased Aβ accumulation (in the blood or cerebral vessels, in neurons of the cortex and hippocampus), promotion of fibrillogenic and toxic Aβ1-42 form or modification of the Aβ1-42/Aβ1-40 ratio, depending on the type of mutation [96,98,99,100]. Pathogenic PS1 or PS2 mutations increase the levels of Aβ1-42 form in vitro, but do not promote Aβ plaques aggregation in vivo in mice. Several double-transgenic (2xTg) mouse models have been developed by crossing APP and PS1 transgenic mice, demonstrating accelerated Aβ accumulation leading to the impairment of cognitive functions [98,100,101].
In the human tau protein (h-tau) transgenic model, the mice tau gene is replaced by the human gene correlating with NFTs development and neurodegeneration [37,42,100,102,103]. The most commonly used tau transgenic model is THY-Tau22 model in which progressive development of the hippocampal tau pathology is observed. Hyperphosphorylated hippocampal tau protein and neuroinflammation results in an age-dependent memory impairment [103,104,105].
A triple-transgenic mice model of AD (3xTg-AD) is a combination of three mutations resulting in the age-related progressive neuropathy including accumulation of Aβ plaques and NFTs, resulting in the cognitive deficits [98,106,107], whereas the 5xFAD transgenic model concerns five mutations exhibiting severe pathology with accelerated Aβ accumulation, senile plaques formation and neuronal loss [37,98,108].
The number of rat genetic models is much lower (for example TgF344-AD, single Tg UKUR28, double Tg UKUR25). In the TgF344-AD rat model (human APPswe and human PS1ΔE9 mutations) accumulation of Aβ plaques, presence of NFTs, gliosis, increased tau protein level and decreased basal hippocampal synaptic transmission was observed [109,110]. Aβ accumulation in the hippocampus and cortex, and increased levels of phosphorylated mitogen-activated protein kinase/extracellular signal-regulated kinase 2 (MAPK/ERK2) were observed in UKUR28 (human APPswe mutation) and UKUR25 (human APPswe and human PS1 Finn mutations) transgenic rat models [97,99,111].
Moreover, several non-mammalian species, including nematode (Caenorhabditis elegans), zebrafish (Danio rerio) and fruit fly (Drosophila melanogaster) and have been used to create transgenic models of AD [112].
In spite of a large number transgenic animal models of AD, it should be pointed out that results of the preclinical studies on those models have been rather not satisfactorily translated into clinical outcomes [37].
Several pharmacological models of sporadic AD have been used. Those models included: administration of aluminum chloride per os (p.o.) [113], intraperitoneal (i.p.) administration of scopolamine [114,115], intracerebroventricular (i.c.v.) injections or infusions of Aβ [116,117], i.c.v. injections of streptozotocin (STZ) [47,118], subcutaneous (s.c.) injections of d-galactose [78,119], i.p. injections of MK-801 (a non-competitive NMDA receptor antagonist) [120], olfactory bulbectomy (OBE) [121] and i.c.v. injections of lipopolysaccharide (LPS) [116,122,123,124] or colchicine [116]. A model of senescence-accelerated rodents (OXYS rats) is also used as a model of sporadic AD [125,126]. It is a non-transgenic model established by inbreeding of highly susceptible rats with spontaneously developing cataract and accelerated senescence syndrome. OXYS rats demonstrate learning and memory deficits, decreased locomotor activity and progressive cognitive impairment [121,125,126].
To summarize, it should be pointed out that sophisticated transgenic experimental models of AD are used in preclinical in vitro and in vivo studies on novel drugs or compounds potentially useful in the prevention or treatment of AD. However, those models reflect only genetic changes present in familial AD, whereas the sporadic form of AD is much more common. On the other hand, mostly rather simplistic models of sporadic AD are currently being used in the experimental studies. Some of them are controversial, for example the scopolamine model [112,127]. It seems that there is a need for development of new, reliable models of sporadic AD.
5.1. Effects of Caffeine in Experimental Animal Models of AD
5.1.1. Transgenic Rodent Models
The effects of caffeine have been studied in various transgenic models of AD, including APPswe, double transgenic (2xTg) APPswe/PS1, THY-Tau22 and 3xTg models (Table 1) [104,105,128,129,130,131,132,133,134,135,136].

Table 1.
Transgenic models.
The most commonly used transgenic models of AD in animals is the APPswe mouse model. In the APPswe model, mice develop cognitive deficits, learning impairment and age-dependent spatial memory dysfunction [37,98,129,130,131]. Expression of human APP in transgenic mice model enable Aβ plaques deposition and synaptic and neuritic dystrophy [130,131,137].
In studies on the APPswe transgenic mice model, caffeine intake prevented cognitive impairment, memory deficits and exerted neuroprotective activity [128,129,130,131,133]. The neuroprotective caffeine activity associated with reduced Aβ production resulted from the inhibition of BACE-1 and γ-secretase [129], suppressed neuronal cell death, reduced caspase-3 activity [131], activation of cAMP/PKA (cyclic adenosine monophosphate/phosphokinase A) signaling pathway and stimulation of cAMP response element-binding protein (CREB) phosphorylation in the striatum [128]. Two-week caffeine treatment in APPswe mice exerted antiapoptotic activity (decreased the expression of phosphorylated c-Jun N-terminal kinase (JNK) and phosphorylated extracellular signal-regulated kinase (ERK) in the striatum and frontal cortex) [128]. Long-term treatment with caffeine improved mitochondrial functions in the hippocampus, cerebral cortex and striatum in APPswe transgenic mice [133]. No effect on A1R and A2AR hippocampal density was observed in APPswe transgenic mice treated with caffeine [129]. Caffeine treatment in N2a neuroblastoma cells transfected with mutant APPswe indicated slight antioxidant activity associated with reduced ROS production [133].
Chronic intake of crude (containing 95.95% caffeine) and pure caffeine prevented memory disorders in APPswe mice model. However, only crude caffeine reduced the level of Aβ and formation of Aβ plaques in the hippocampus. Crude caffeine increased the level of ATP (an indicator of cell survival), reduced caspase-3 activity and reduced Aβ-induced neuronal cell death [131]. Crude and pure caffeine increased the number of cholinergic neurons in Aβ-treated cultures [131]. Greater effects of crude caffeine may result from the activity of other than caffeine components. Phenolic substances (about 1%) may be responsible for antioxidant activity of crude caffeine which exhibited much higher values than pure caffeine in the oxygen radical absorbance capacity (ORAC) assay [131,138]. Moreover crude caffeine strongly inhibited cyclooxygenase-2 (COX-2), whereas pure caffeine did not inhibit the enzyme [138]. The authors concluded that substantial antioxidant and anti-inflammatory effects of crude caffeine are crucial in preventing cognitive and memory impairment in APPswe transgenic mice [131].
Studies on caffeine were also performed on 2xTg and 3xTg animal models. Double transgenic mice indicate rapid rate and early onset of AD associated with cognitive impairment [98]. For example, the double transgenic APPswe/PS1 mice model is related to Aβ plaque formation in the cortex and hippocampus [37,98]. In those mice spatial learning and memory assessed in the water maze test worsened [132].
Acute intake of caffeine by APPswe/PS1 transgenic mice resulted in a reduced Aβ production (by inhibiting γ-secretase and BACE-1) and reduced Aβ1-40 and Aβ1-42 levels in plasma (the same effects were observed in transgenic APPswe mice). Similarly, long-term caffeine administration to APPswe/PS1 transgenic mice was related to a permanent and sustained decrease in the Aβ1-40 and Aβ1-42 levels in plasma and reduced Aβ accumulation in the brain. Chronic caffeine administration enhanced cognitive performance in the transgenic mice [134].
Acute caffeine use (administered as a coffee constituent) increased the levels of granulocyte-colony stimulating factor—G-CSF, IL-6 and IL-10 in plasma in APPswe/PS1 double transgenic mice and in non-transgenic mice. Higher levels of plasma caffeine were related to lower levels of plasma Aβ in APPswe/PS1 transgenic mice. Chronic intake of concentrated coffee improved cognitive performance and increased the level of G-CSF in plasma in APPswe transgenic mice. The authors concluded that coffee (as a source of caffeine) may protect against AD and that elevated G-CSF levels may contribute to favorable effects of coffee [136].
Also chronic treatment with caffeine in double transgenic APPswe/PS1 mice reversed memory impairment [132]. Caffeine improved spatial learning and memory, which was demonstrated by a decrease of escape latency time and longer time spent in the target quadrant assessed in the water maze test. The effects of caffeine were dose dependent. The mechanism of changes could involve the effect on the brain-derived neurotrophic factor (BDNF)—tropomyosin-related kinase receptor B (TrkB) signaling pathway, taking part in the learning and memory processes, since caffeine exerted dose-dependent increase in the expression of hippocampal BDNF and TrkB [132].
In a transgenic model of tau disorders, THY-Tau22 mice, progressively developing memory dysfunction is associated with hippocampal neuroinflammation that promotes tau protein hyperphosphorylation and aggregation [104,105,139]. Chronic administration of caffeine to THY-Tau22 transgenic mice prevented behavioral disorders and spatial memory deficits. The beneficial activity of caffeine on memory was associated with reduced hyperphosphorylated tau protein level in the hippocampus [104]. The deletion of A2AR improved memory, prevented spatial memory deficits and hippocampal long-term depression in THY-Tau22 transgenic mice [139]. It did not affect the tau protein level and the number of proteolytic tau fragments, which were reduced by caffeine intake in the previous study [104]. It may indicate that mechanism of caffeine in the regulation of tau-related pathology was more complex than only blockade of A2AR in THY-Tau22 transgenic mice [139].
Moreover, caffeine exerted anti-inflammatory activity (reduced level of proinflammatory cytokines: chemokine ligand factor 4—CCl4, chemokine ligand factor 5—CCl5 and TNF-α) and antioxidant activity (decreased activity of manganese superoxide dismutase—MnSOD and excitatory amino acid transporter 3—EAAT3 involved in the glutathione synthesis) in THY-Tau22 transgenic mice [104]. However, when caffeine was administered to pregnant THY-Tau22 transgenic rats, accelerated physiological and cognitive disorders in offspring were observed. Those results indicate that exposure to caffeine during pregnancy in rats may be a risk factor for early stages of AD [105].
Effects of caffeine were also studied in 3xTg-AD mice (carrying APPswe, PS1/M146V and tau P301L transgenes). The effects of long-term intake of caffeine in 3xTg-AD mice were assessed in multiple behavioral tests (lasting 21 days) to evaluate sensorimotor functions, exploratory activity, bizarre movements, emotional and anxiety-like behaviors, risk assessment, visual perceptual learning and reference spatial learning and memory in comparison with normal non-transgenic mice. Some of the tests were interpreted as tests concerning BPSD-like behaviors [135]. The effects of caffeine treatment in the two models were differential. Caffeine in control non-transgenic mice improved some behavioral parameters connected with cognition, exploratory and locomotor activity. Caffeine did not counteract any of behavioral disorders observed in 3xTg-AD mice, moreover some of the behavioral parameters even worsened (mostly those related to the anxiety-like behaviors). Caffeine increased horizontal locomotor activity in the open field test in non-transgenic mice and reduced it in 3xTg-AD mice; increased emotionality in the open field test, elevated plus maze and hole-board test in non-transgenic mice and reduced these parameters in 3xTg-AD mice; increased total horizontal activity in the open field test in non-transgenic mice and reduced it in 3xTg-AD mice. Caffeine increased overall spontaneous motor activity (to a greater extent at night) in circadian motor activity test only in 3xTg-AD mice [135]. The authors interpreted their results that anxiogenic effect (associated with anxiety and neophobia) induced by caffeine interfered with beneficial effects of caffeine consumption on cognition (improved visual perceptive learning, spatial learning and memory) in 3xTg-AD mice [135].
5.1.2. Non-Transgenic Rodent Models
Several non-transgenic models of AD have been used to evaluate the effects of caffeine (Table 2). In a model of AD induced by i.c.v. administration of Aβ25-35, in which cognitive dysfunction is observed (Y-maze test and inhibitory avoidance task), acute caffeine administration at a higher i.p. dose or combined 12-day administration in drinking water, followed by acute administration at a lower i.p. dose, prevented Aβ-induced disorders in mice. There was no beneficial effect of the 12-day treatment with caffeine alone [117]. It was concluded that mechanism of caffeine action resulted from the blockade of A2AR rather than A1R, because similar effects were observed after a selective A2AR antagonist—SCH58261 administration [117]. In other studies, selective A2AR antagonists also prevented Aβ-induced progressive cognitive impairment and synaptic deterioration in rats [120,140].

Table 2.
Non-transgenic models.
Long-term administration of d-galactose to rats is associated with increased oxidative stress resulting in memory impairment, neuroinflammation and neurodegeneration. Concurrent caffeine intake improved memory functions and attenuated cognitive decline in the d-galactose-treated aging rats as demonstrated in the Y-maze behavioral test. Caffeine administration exerted anti-inflammatory activity (reduced level of COX-2, nitric oxide synthase-2 (NOS-2), TNF-α and IL-1β), antioxidant activity (decreased level of oxidative stress marker—8-oxoguanine) and antiapoptotic activity (decreased B-cell lymphoma 2-associated X protein/B-cell lymphoma protein-2 (BAX/Bcl-2) ratio and reduced caspase-3 and caspase-9 expression) in rats with accelerated aging induced by d-galactose administration. Caffeine treatment alleviated synaptic dysfunction (increasing the level of presynaptic proteins synaptophysin and post-synaptic protein PSD95 in the hippocampus) in d-galactose-treated rats [119].
The STZ-induced AD model is associated with impaired brain glucose metabolism, Aβ accumulation and tau hyperphosphorylation. STZ i.c.v. administration increase oxidative stress, AChE activity and neuroinflammation in the hippocampus and cortex [35,96,116,144]. Chronic caffeine administration prevented STZ-induced progressive memory loss, sporadic dementia and neurodegeneration. It also decreased the expression and density of A2AR in the hippocampus (not affecting A1R density) in rats [141]. Moreover, caffeine administered to rodents with diabetes mellitus induced by i.p. STZ injections prevented learning and memory deficits [145,146].
In the AlCl3-induced AD model, administration of aluminum chloride increases level of Aβ, BACE-1, hyperphosphorylated tau protein, proinflammatory cytokines (TNF-α, IL-6) and oxidative stress markers in the hippocampus and cortex [35,147]. Chronic caffeine intake exerted neuroprotective activity demonstrated by improvement of the histological hippocampus picture (decreased neuronal apoptosis observed in CA1 and CA3 hippocampal regions) in AlCl3 treated rats. Moreover, increased proliferation marker protein—Ki-67 immunoreactivity, decreased glial fibrillary acidic protein (GFAP) immunoreactivity, and increased expression of BDNF and TrkB were observed after caffeine intake [142]. Further studies on caffeine showed that neuroprotective activity may have resulted from reduced oxidative stress (reduced levels of NO in the cerebral cortex, hippocampus and striatum and increased level of reduced glutathione—GSH in the hippocampus) and attenuated AlCl3-induced lipid peroxidation (reduced level of malondialdehyde—MDA in the cerebral cortex, hippocampus and striatum). Caffeine decreased activity of Na+/K+-ATPase in the cerebral cortex, hippocampus and striatum, and reduced activity of AChE in the cerebral cortex and hippocampus. Also anti-inflammatory properties of caffeine were demonstrated (decreased TNF-α level in the hippocampus and striatum) in AlCl3-induced neurotoxicity in rats [143].
LPS administration induces chronic neuroinflammation and amyloidosis leading to cognitive deficits and memory impairment, reflecting processes specific for sporadic type of AD [124]. Increased BACE-1 and γ-secretase activity leading to Aβ hippocampal accumulation, elevated proinflammatory cytokines level (IL-1β, IL-6, IL-12, TNF-α), mitochondrial dysfunction, and increased ROS production is observed in LPS-induced model of AD in rats [124]. Caffeine exerted protective effect against LPS-induced and age-related neuroinflammation associated with microglia activation in rats [122]. It has been demonstrated that caffeine may decrease neuroinflammation by a reduction in the number of activated microglial cells in the CA3 hippocampus region and regulation of glutamate neurotransmission [122]. Caffeine administration inhibited LPS-induced oxidative stress, neuroinflammation and synaptic dysfunctions (increasing expression of nuclear factor erythroid 2-related factor 2 (Nrf2), hemeoxygenase 1 (HO-1) and Bcl-2, reducing expression of toll-like receptor 4 (TLR-4), phosphorylated nuclear factor-κB (p-NF-κB), phosphorylated c-Jun N-terminal kinase (p-JNK), BAX, caspase-3, TNF-α, COX-2 and NOS-2) in mice [123].
Intraperitoneal administration of scopolamine, a non-selective, competitive muscarinic receptor antagonist, is associated with acute memory and attention deficits through cholinergic system blockade [112,115]. Long-term cholinergic dysfunction results in a reduced number of cholinergic neurons, decreased ACh level in the brain, increased AChE activity and suppressed choline acetyltransferase activity. Moreover, scopolamine increases oxidative stress, apoptosis, mitochondrial dysfunction and neuroinflammation in animal AD models [148,149,150]. Although the scopolamine-induced amnesia/memory impairment as a model of AD was widely used in the past, the relevance of scopolamine in current experimental AD studies is very limited [112,114]. Cholinergic dysfunction observed after acute scopolamine administration is not related to the hallmarks of AD (Aβ or hyperphosphorylated tau protein) and disease progression [112]. The effects of caffeine (or selective adenosine receptors antagonists) were studied only after acute scopolamine administration. In scopolamine-treated mice, caffeine administration prevented short-term and long-term memory deficits assessed in the behavioral tests (novel object recognition task and inhibitory avoidance task), indicating possible beneficial effect in cholinergic-induced memory disruption [115]. Caffeine ameliorated also scopolamine-induced memory impairment in humans [151]. The beneficial effect of caffeine probably resulted from its dual ability to blockade of A1R and A2AR [115]. Studies conducted in scopolamine-treated rats showed that A1R and A2AR antagonists prevented scopolamine-induced memory impairment [61,152,153].
5.1.3. Rabbit Cholesterol-Induced Model
A high cholesterol diet-induced rabbit model of AD is characterized by an elevated Aβ level in the brain, increased tau protein hyperphosphorylation and disturbed BBB integrity (associated with a disrupted brain cholesterol homeostasis) leading to the learning impairment [154]. Chronic caffeine administration to rabbits fed a cholesterol-enriched diet prevented dysfunction of BBB, decreased activation of astrocytes and decreased density of microglia [155] (Table 3). In another study, caffeine intake decreased Aβ level, Aβ production and Aβ deposition in the hippocampus, reduced hyperphosphorylated tau protein level in the hippocampus (probably associated with the reduction of phosphorylated glycogen synthase kinase-3β (pGSK-3β) enzyme level which is involved in the tau protein phosphorylation), decreased oxidative stress (reduced ROS generation and H2O2 production, and increased reduced/oxidized glutathione (GSH/GSSG) ratio) and restored A1R level, reduced by cholesterol. There was no caffeine effect on the cholesterol concentration in plasma in rabbits [156].

Table 3.
Rabbit model.
5.1.4. Nematode Models
Nematodes are suitable for experimental studies on AD due to their short lifespan, short generation time, transparent body and simple creation of new transgenic lines. Many human genes associated with AD have orthologues in nematodes Caenorhabditis elegans [112,157]. Various strains of the nematode Caenorhabditis elegans with human neurotoxic proteins (Aβ1-42, APP, tau protein) expression are used to investigate the cellular and molecular mechanisms of neurodegenerative diseases [112,158,159,160]. Expression of the human Aβ1-42 in muscles causes, among other things, development of paralysis, whereas its expression in neurons results in their neurodegeneration, and odor preference learning disruption [96,159]. After expression of the human APP in Caenorhabditis elegans, only products of α-secretase or γ-secretase cleavage (but not β-secretase) are detected, and APP-induced cholinergic neurodegeneration is observed [159]. Expression of the h-tau protein in Caenorhabditis elegans leads to tau aggregate formation and accumulation, neuronal degeneration and synaptic abnormalities resulting in locomotion defects and behavioral impairment [96,159].
In studies conducted on the nematode AD models, plant extracts containing caffeine were investigated, including the extracts from Ilex paraguariensis leaves [161], Paullinia cupana (guarana) seeds [158], Coffea beans [160], and Zijuan Pu’er tea [162] (Table 4). All studied extracts prevented Aβ-induced toxicity in transgenic models of AD in Caenorhabditis elegans, delaying the paralysis progression in worms and extending their lifespan [158,160,161,162]. However, coffee extract (10% v/v, containing 3.6 mM caffeine) treatment did not reduce Aβ aggregation and Aβ distribution. The authors concluded that beneficial effect of coffee probably resulted from skn-1/Nrf2 signaling pathway activation; similar effects were observed after treatment with decaffeinated coffee (0.032 mM caffeine) [160]. A mixture of Zijuan Pu’er tea water extract ingredients (MCCP), containing (+)-catechins, caffeine and procyanidins, decreased Aβ aggregation and activated the DAF-16 signaling pathway, which was associated with lifespan extension and oxidative stress reduction in Caenorhabditis elegans, and could be mediated by a heat shock factor 1 (HSF-1) and skn-1 [162]. Guarana hydroalcoholic extract and decaffeinated guarana extract treatments were also associated with antioxidant activity and protein degradation pathways, partially through skn-1 and DAF-16 activation [158].

Table 4.
Nematode models.
Caffeine alone was investigated only in one study on nematodes [161]. The effect of caffeine treatment in higher concentrations (0.2 mM or 0.4 mM) was weaker than the effect of Ilex paraguariensis hydroalcoholic extract (IPHE) containing lower concentrations of caffeine (41 or 87 μM). IPHE and caffeine reduced Aβ mRNA levels, decreased AChE activity, increased expression of hsp-16.2 (chaperone protein which overexpression causes suppression of Aβ-toxicity), but also activated DAF-16 signaling (IPHE also HSF-1). It may suggest that beneficial neuroprotective effects may result from different than caffeine constituents of IPHE [161]. Decaffeinated extracts from coffee [160] and guarana [158] also induced some favorable effects in Caenorhabditis elegans.
In conclusion, the studies on nematode models of AD did not allow the effects of caffeine to be distinguished from those of other constituents of plant extracts [158,160,161].
5.2. In Vitro Studies
Caffeine administered to the culture medium caused an enhanced release of stored Ca2+ in the in vitro culture of the cortical neurons of 3xTg-AD mice (Table 5). The effect was not associated with a change in the endoplasmic reticulum store size, defects in the Ca2+ extrusion mechanism or expression of Ca2+-binding/buffering proteins, but probably with an increased expression of the RyR [107]. Similar results were obtained in later studies showing increased calcium signals within dendritic processes induced by RyRs stimulation by caffeine. The proper regulation of calcium signaling may be important in the prevention of synapse loss and further cognitive impairment [163]. Beneficial effect of caffeine treatment was demonstrated in vitro in cultures of human neuroblastoma SH-SY5Y cells, to which Aβ was added in order to induce neurotoxicity [164,165]. Caffeine increased expression of antiapoptotic protein Bcl-2 and reduced expression of proapoptotic protein BAX in the AlCl3-induced and Aβ25–35-induced neurotoxicity in human neuroblastoma SH-SY5Y cells. Caffeine inhibited also the increase of AD-related proteins (APP and BACE-1) expression in cells exposed to both AlCl3 and Aβ25–35. The effects of caffeine were similar to those induced by selective A1R or A2AR antagonists, indicating the role of blockade of both A1R and A2AR. Caffeine reduced also oxidative stress (reducing NF-κB activity, reducing ROS production, increasing superoxide dismutase (SOD) activity and decreasing MDA concentration) induced by AlCl3 and Aβ25–35. The authors proposed that combined involvement of A1R and A2AR blockade by caffeine in the neuronal cell protection is associated with the restoration of Ca2+ homeostasis [164]. In another study, the neuroprotective activity of caffeine against Aβ-induced neurotoxicity was confirmed in a neuronal cell line. The effects were shown to result from complex mechanism of caffeine action—the blockade of A1R and A2AR, direct or indirect blockade of NMDA receptors and activation of RyRs [165].

Table 5.
In vitro models.
Viral delivery of mutated human APP and tau protein to primary rat hippocampal neurons and rat dorsal root ganglion (DRG) caused accelerated neuronal cell death and morphological damage (more severe effects were observed in tau transduced cultures). Also, calcium homeostasis dysregulation was observed in APP-EGFP and tau-DsRed2 transduced hippocampal neurons. Moreover, a neurite impairment was demonstrated in APP-EGFP and tau-DsRed2 transduced DRG neurons. Caffeine treatment prevented morphological neuronal damage increasing the number of healthy neurons in APP-induced and tau-induced models [166].
5.3. In Silico Studies
In silico studies indicated that caffeine may be useful as an anti-amyloidogenic agent in the prevention of AD [167]. Caffeine was studied in silico as a potential molecule that destabilizes preformed Aβ protofilaments. The molecular dynamics simulations and calculations indicated that the mechanism of caffeine action may be associated with the disruption of inter-chain hydrogen bonds and disorganization of secondary structure conformation of Aβ [167]. In another study, molecular dynamic simulations demonstrated that caffeine inhibited the self-assembly of Aβ oligomerization by interference with the hydrophobic interaction between Aβ16-22 peptides; the effect was greater when caffeine concentration in the water solution was higher [168]. In silico studies predicted caffeine to be a potential AChE inhibitor [169]. An improvement of cholinergic system transmission was also revealed in silico molecular docking study, where a coffee and green tea constituent—EGCG inhibited AChE and butyrylcholinesterase [170].
6. Discussion
So far no drugs have been proven to be effective in reversing or stopping AD. Despite numerous studies having been conducted in recent years, no new drugs have been registered by the FDA for almost 20 years [171]. Due to the not fully understood, complex pathomechanism of AD and numerous clinical failures of anti-amyloid and anti-tau drugs, it is necessary to look at strategies involving modifying factors connected with the style of life or dietary factors which potentially would counteract the development of neurodegenerative changes or delay AD progression. Caffeine, or rather its sources (coffee, tea, yerba mate), are considered factors which may exert beneficial effects in the AD—prevent the risk of developing AD and/or delay the progression of AD [81,82].
To investigate the effects of caffeine in AD, numerous studies have been undertaken on different experimental models. In those studies, caffeine was administered in different doses. Caffeine was administered in drinking water, in the diet, or once/twice daily p.o. or i.p. The descriptions of the doses (low, moderate, high) used by authors in their reports on in vitro and in vivo studies are not unequivocal. Caffeine consumption in humans differs in a wide range. A low caffeine intake is considered to be below 200 mg/day (<2.86 mg/kg/day), moderate between 200 and 400 mg/day (2.86–5.71 mg/kg/day) and high above 400 mg/day (>5.71 mg/kg/day) [8,172]. Based on the body surface area conversion ratio, the doses administered to humans are converted into animal doses. Thus, based on the calculations [173], the corresponding rat doses are as follows: low (<17.7 mg/kg/day), moderate (17.7–35.4 mg/kg/day) and high (>35.4 mg/kg/day). Equivalent mouse doses under 35.1 mg/kg/day are considered as low, between 35.1 and 70.3 mg/kg/day as moderate and above 70.3 mg/kg/day as high [172,173,174]. In most of the issues discussed in the present article about animal studies, caffeine was administered in doses corresponding to the human doses; the exact doses used in particular experiments are shown in Table 1, Table 2 and Table 3.
Generally, experimental studies on caffeine effects in AD demonstrated some beneficial influence on cognition. Its neuroprotective, antioxidant, anti-inflammatory and antiapoptotic activities in the neuronal tissues, led to alleviation of cognitive impairment [104,119,122,123,128,131,132,133,136,141,142,143,155,156,158,160,161,164,165,166]. Many studies pointed out on favorable effects of caffeine on the hallmarks of the disease: Aβ or hyperphosphorylated tau protein [104,117,129,131,134,156,161,162,164,165,166].
Since the main mechanism of caffeine action is associated with a non-selective blockade of adenosine receptors (mainly A1R and A2AR), this problem was undertaken in many studies. In fact, both adenosine receptors (A1R and A2AR) are present in synapses of glutamatergic, GABAergic, cholinergic, dopaminergic, serotoninergic and noradrenergic system, and adenosine is involved in neuromodulation of the central nervous system (CNS) [175]. Adenosine has been shown to reduce the release of various neurotransmitters including glutamate, ACh, dopamine, serotonin and noradrenaline in CNS in experimental models, whereas caffeine, as an adenosine receptor antagonist, to promote the release [22].
In fact, the favorable effects of caffeine were shown to result from the blockade of A2AR (but probably not A1R) in mice with AD induced by Aβ25–35 i.c.v. administration [117], in Aβ-induced neurotoxicity in the primary cerebral cultures in rats [176] and in STZ-induced AD in rats [141]. However, A1R may be involved in the protective caffeine activity in cholesterol-enriched diet-induced AD in rabbits [156]. Moreover, the blockade of both A1R and A2AR was responsible for beneficial activity of caffeine in in vitro model of combined neurotoxicity induced by AlCl3 and Aβ25–35 in human neuroblastoma SH-SY5Y cells [164] and in scopolamine-induced memory deficit in mice [115]. Dual blockade was also considered a probable mechanism of caffeine neuroprotective activity in Aβ-induced toxicity in human neuroblastoma SH-SY5Y cells [165].
Beneficial effects of caffeine resulting from the blockade of adenosine receptors (A1R and A2AR) have been confirmed by studies with selective A1R and A2AR antagonists. The studies with use of selective A2AR antagonists (MSX-3 and SCH58261) demonstrated that A2AR blockade prevented spatial memory deficits and development of amyloid burden in the double transgenic APPswe/PS1ΔE9 mice [177] and improved synaptic plasticity deficits in double transgenic APPswe/PS1 mice [178]. Similar favorable effects of selective A2AR antagonist administration (SCH58261) were observed also in 3xTg (APPswe, PS1/M146V and tau P301L) mice [179] and in Aβ-induced neurotoxicity and synaptotoxicity in rats [120,140]. Deletion of A2AR prevented memory impairment and reduced tau protein hyperphosphorylation in THY-Tau22 transgenic mice [139]. Similar effects were observed after caffeine treatment in THY-Tau22 mice [104]. However, SCH58261 did not favorably affect scopolamine-induced and MK-801-induced acute memory impairment suggesting that selective A2AR antagonist exerts beneficial effects only in slowly progressing memory impairment related to synaptic deterioration [120]. However, blockade of A2AR (by a selective antagonist—SCH58261), and also A1R (by a selective antagonist—DPCPX) led to beneficial effects in a scopolamine-induced model in mice [153], confirming the effect observed after caffeine treatment in this mice model [115], but inconsistent with conclusions drawn by other authors [180].
It should be pointed out that the effects of caffeine on adenosine transmission were not consistent in all studied models. For example, no influence of caffeine on A1R and A2AR density was observed in APPswe mice [129]. Moreover, chronic caffeine intake did not result in persistent up-regulation of A1AR in rat brains excluding this mechanism of action as the reason for the neuroprotective effect of caffeine in rats [181]. It should be emphasized that the mechanism of caffeine action on adenosine system is dose-dependent, since, for example, in mice, acute caffeine intake at lower doses (<50 mg/kg) blocks mostly A1R and at higher non-toxic doses (<100 mg/kg) A2AR [117].
Although numerous studies indicate that antagonistic effect of caffeine on adenosine receptors may be responsible for alleviation of memory deficits, it is not the only possible mechanism of beneficial caffeine action in AD. From among other caffeine mechanisms, the inhibitory effect on PDEs and agonistic effect on RyRs were investigated in in vitro models of AD disorders. Caffeine inhibited PDE, restoring the mitochondrial functions in vitro in mouse N2a-APPswe cells [133]. Activation of RyRs by caffeine led to an increased Ca2+ release from intracellular stores in the cortical cultures from 3xTg-AD mice [107] and in the hippocampal cultures from normal rats [24]. However, the caffeine doses required to inhibit PDEs and stimulate the RyRs are not achievable in a normal diet and could exert toxic effects in humans [9,23,25,26].
Numerous mechanisms of caffeine action, which may be relevant to its favorable effects in AD models were demonstrated in studies on cell cultures. For example, in vitro caffeine decreased Aβ level and Aβ1-42 deposition, and reduced BACE-1 activity in human neuroblastoma SH-SY5Y cells [182], and inhibited oligomerization of Aβ in N2a/APP cells [183]. Also decreased expression of BACE-1 and APP was demonstrated after caffeine treatment in human neuroblastoma SH-SY5Y cells exposed to AlCl3 and Aβ [164]. In addition, the beneficial effect of caffeine on Aβ could be associated with antagonism of NMDA receptors or agonism of RyRs [165]. Moreover, brewed coffee reduced Aβ production by a decrease in BACE-1 expression (which was not associated with caffeine activity) in human neuroblastoma SH-SY5Y cells [184]. Brewed coffee increased expression of vascular endothelial growth factor (VEGF)in SH-SY5Y cells, indicating possible neuroprotective effect [185]. The effects of brewed coffee treatment suggest that the neuroprotective activity may result not only from caffeine activity, but also from that of other coffee components.
Since AChE inhibitors (donepezil, rivastigmine, galantamine) currently play the main role in the treatment of AD, the effects of caffeine on AChE were also studied. In vivo studies demonstrated weak anticholinesterase activity of caffeine in normal rats [172], in rats with AlCl3-induced neurotoxicity [143] and in a nematode AD model [161]. In vitro studies on caffeine and donepezil effects in the rat brain tissue homogenate demonstrated that both drugs inhibited AChE, whereas the effect was stronger after the combined treatment (with stronger inhibition at higher caffeine concentration). On the other hand, in vivo studies did not confirm the augmentation of donepezil anticholinesterase activity by caffeine, moreover administration of high-dose caffeine with donepezil elevated the AChE activity [172]. This may suggest adverse effects of high caffeine consumption during the treatment of AD with AChE inhibitors.
The mechanism of favorable actions of caffeine on AD may be connected with the reduction of neuroinflammation [5,186]. AD and other neurodegenerative diseases are associated with an increased level of inflammation and oxidative stress parameters. Numerous studies showed that caffeine reduced parameters of oxidative stress. Caffeine exerted antioxidant activity in transgenic [104,131] and non-transgenic rodent models [119,123,143], a rabbit model [156], and nematode models [158,161] of AD.
Neuroprotective, anti-inflammatory and antiapoptotic activity of caffeine demonstrated in different experimental models of AD in vivo was reflected in in vitro studies. Caffeine exerted antiapoptotic activity in APPswe transgenic mice [128,131] and in the d-galactose-treated rats [119]. Anti-inflammatory effect of caffeine administration was associated with the reduced level of proinflammatory cytokines in THY-Tau22 transgenic mice [104], in AlCl3-induced neurotoxicity in rats [143] and in the d-galactose-treated rats [119].
The caffeine effects presented in studies performed in experimental models of AD are presented in Figure 1.
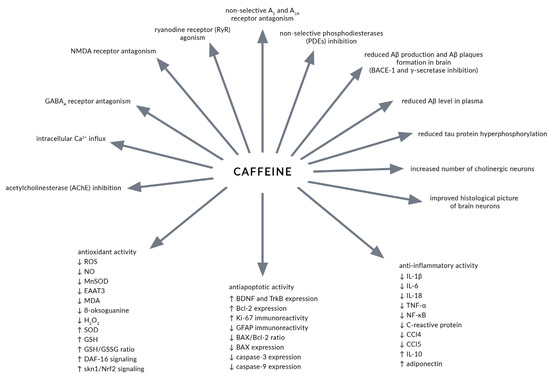
Figure 1.
Caffeine effects reported in studies performed in experimental models of Alzheimer’s disease (AD). Aβ—amyloid β. AChE—acetylcholinesterase. BACE-1—β-site amyloid-precursor-protein-cleaving enzyme-1. BAX—B-cell lymphoma 2-associated X protein. Bcl-2—B-cell lymphoma protein-2. BDNF—brain-derived neurotrophic factor. CCl—chemokine ligand factor. DAF-16—abnormal dauer formation 16. EAAT3—excitatory amino acid transporter 3. GABAA—γ-aminobutyric acid type A receptor. GFAP—glial fibrillary acidic protein. GSH—reduced glutathione. GSH/GSSG ratio—reduced/oxidized glutathione ratio. IL—interleukin. MDA—malondialdehyde. MnSOD—manganese superoxide dismutase. NF-κB—nuclear factor-κB. NMDA—N-methyl-D-aspartate. Nrf2—nuclear factor erythroid 2-related factor 2. PDE—phosphodiesterase. ROS—reactive oxygen species. RyR—ryanodine receptor. skn-1—skinhead 1. SOD—superoxide dismutase. TNF-α—tumor necrosis factor α. TrkB—tropomyosin-related kinase receptor B.
It must be stated that caffeine shares antioxidant and anti-inflammatory effects, leading to neuroprotection, with numerous phenolic compounds, many of them occurring together with caffeine in its dietary sources (coffee, tea, yerba mate). In fact, crude caffeine (containing 1% of phenolic acids) exerted stronger favorable effects than pure caffeine [131]. Also, other substances present in coffee or tea like chlorogenic acid [187,188,189,190], caffeic acid [79,189,191], EGCG [3,79], ferulic acid [76] exerted beneficial effects in experimental models of AD.
It should be pointed out that caffeine did not exert beneficial effects in all experiments on AD experimental models. Caffeine administration did not favorably affect behavioral disorders studied in the behavioral tests in 3xTg-AD mice. Intensification of BPSD-like behaviors and anxiety-related behaviors was demonstrated after caffeine treatment in those mice [135]. The adverse effect of caffeine intake during pregnancy in THY-Tau22 transgenic rats was demonstrated in the behavioral tests in offspring, in which caffeine accelerated the occurrence of cognitive deficits [105]. Detrimental effects of caffeine intake rather than that of other coffee components during pregnancy (low birth weight of infant, increased risk of pregnancy loss and childhood acute leukemia) was also confirmed in an umbrella review on the impact of coffee and caffeine on health outcomes [14,16].
As was mentioned before, caffeine (as a component of coffee, tea, yerba mate, cola) is the most widely used psychostimulant [8,23,192,193]. The safety of caffeine consumption depends on the dose, age, sex and health condition [12,13,194]. Caffeine intake in coffee, tea, yerba mate, cola and other sources at doses up to 400 mg/day is considered safe for healthy adults, except pregnant women (<300 mg/day) [14,194]. In children and adolescents, caffeine consumption up to 2.5 mg/kg/day was not associated with overt adverse effects [14]. Caffeine intake may negatively affect pregnant women, lactating women, children, adolescents, people with cardiovascular disorders, people with gastric and duodenal ulcer disease and smokers [194,195]. Caffeine intake before bedtime is associated with negative impact on sleep condition, although sleep avoidance and increased vigilance and arousal may be desirable [14]. The adverse caffeine effects on the behavior observed at higher doses intake are anxiety, jitteriness and mood disorders [8,13,14,196]. Negative effect of caffeine consumption was demonstrated also in children, including reduced sleep time, impulsiveness, greater emotional lability and depression [197].
Experimental studies, reviewed in the present article, indicate rather favorable effects of caffeine in animal models of AD. However, results of such studies may not be fully relevant to AD in humans. The AD models have been used to investigate many potential drugs that have proven to be effective in the animals, but this has not necessarily been confirmed in the human studies. Multiple potential disease-modifying drug candidates (γ-secretase inhibitors, BACE-1 inhibitors, monoclonal antibodies, anti-Aβ antibodies, tau aggregation inhibitors) failed in the further phases of the trials [36,51,52,171,198,199].
The studies on transgenic models were limited to the mouse models. The rat studies, carried out on non-transgenic models, were less numerous. In many of the experiments caffeine was administered in drinking water or in the diet, the effect of caffeine used in bolus doses at regular time intervals, over a certain period of time may be different.
Another limitation of the experimental studies is that most of them were carried out on male animals (or the animal sex was not stated), whereas human studies indicate that the effect of caffeine on cognition is sex-dependent [95,200,201]. For example, caffeine intake was associated with better cognitive performance in older women, but not in men [202]. On the other hand, the beneficial effects of caffeine consumption were observed in older men but not in women [200]. Moreover, contradictory conclusions have been drawn from the analysis of the relationship between the sex-dependent effects of caffeine consumption on different cognitive outcomes: there was no significant association between caffeine administration and cognitive performance in men; significant interaction between caffeine intake and cognitive performance was observed only in women [95,201]. The sex-dependent effect of caffeine could result from changes in circulating steroid hormones or differences in the caffeine metabolism (probably resulting from higher xanthine oxidase activity in women) in female and male organisms [95,200].
7. Conclusions
In conclusion, the studies carried out on experimental models generally support the notion that dietary caffeine consumption may exert some beneficial effects in AD. However, further studies are necessary to elucidate the role of caffeine in the effects of its sources on cognition and possibly AD risk.
Author Contributions
Conceptualization, J.F. and P.L.; writing—original draft preparation, P.L., M.Z., B.K., A.T. and J.F.; writing—review and editing, P.L. and J.F.; supervision, J.F. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Acknowledgments
The article was partially prepared by the members of Student Scientific Circle in the Department of Pharmacology, Faculty of Pharmaceutical Sciences in Sosnowiec (M.Z., B.K. and A.T.).
Conflicts of Interest
The authors declare no conflict of interest.
References
- Lashley, T.; Schott, J.M.; Weston, P.; Murray, C.E.; Wellington, H.; Keshavan, A.; Foti, S.C.; Foiani, M.; Toombs, J.; Rohrer, J.D.; et al. Molecular biomarkers of Alzheimer’s disease: Progress and prospects. Dis. Model. Mech. 2018, 11, dmm031781. [Google Scholar] [CrossRef]
- Wightman, E.L. Potential benefits of phytochemicals against Alzheimer’s disease. Proc. Nutr. Soc. 2017, 76, 106–112. [Google Scholar] [CrossRef] [PubMed]
- Andrade, S.; Ramalho, M.J.; Loureiro, J.A.; do Carmo Pereira, M. Natural compounds for Alzheimer’s disease therapy: A systematic review of preclinical and clinical studies. Int. J. Mol. Sci. 2019, 20, 2313. [Google Scholar] [CrossRef] [PubMed]
- Howes, M.-J.R.; Perry, N.S.L.; Vásquez-Londoño, C.; Perry, E.K. Role of phytochemicals as nutraceuticals for cognitive functions affected in ageing. Br. J. Pharmacol. 2020, 177, 1294–1315. [Google Scholar] [CrossRef] [PubMed]
- Szczechowiak, K.; Diniz, B.S.; Leszek, J. Diet and Alzheimer’s dementia—Nutritional approach to modulate inflammation. Pharmacol. Biochem. Behav. 2019, 184, 172743. [Google Scholar] [CrossRef]
- Scarmeas, N.; Anastasiou, C.A.; Yannakoulia, M. Nutrition and prevention of cognitive impairment. Lancet Neurol. 2018, 17, 1006–1015. [Google Scholar] [CrossRef]
- Habtemariam, S. Natural products in Alzheimer’s disease therapy: Would old therapeutic approaches fix the broken promise of modern medicines? Molecules 2019, 24, 1519. [Google Scholar] [CrossRef]
- Cappelletti, S.; Piacentino, D.; Sani, G.; Aromatario, M. Caffeine: Cognitive and physical performance enhancer or psychoactive drug? Curr. Neuropharmacol. 2015, 13, 71–88. [Google Scholar] [CrossRef]
- Fredholm, B.B.; Bättig, K.; Holmén, J.; Nehlig, A.; Zvartau, E.E. Actions of caffeine in the brain with special reference to factors that contribute to its widespread use. Pharmacol. Rev. 1999, 51, 83–133. [Google Scholar]
- Ashihara, H.; Kato, M.; Crozier, A. Distribution, biosynthesis and catabolism of methylxanthines in plants. Handb. Exp. Pharmacol. 2011, 200, 11–31. [Google Scholar] [CrossRef]
- Reyes, C.M.; Cornelis, M.C. Caffeine in the diet: Country-level consumption and guidelines. Nutrients 2018, 10, 1772. [Google Scholar] [CrossRef]
- Verster, J.C.; Koenig, J. Caffeine intake and its sources: A review of national representative studies. Crit. Rev. Food Sci. Nutr. 2018, 58, 1250–1259. [Google Scholar] [CrossRef]
- EFSA NDA Panel (EFSA Panel on Dietetic Products, Nutrition and Allergies). Scientific opinion on the safety of caffeine. EFSA J. 2015, 13, 4102. [Google Scholar] [CrossRef]
- Wikoff, D.; Welsh, B.T.; Henderson, R.; Brorby, G.P.; Britt, J.; Myers, E.; Goldberger, J.; Lieberman, H.R.; O’Brien, C.; Peck, J.; et al. Systematic review of the potential adverse effects of caffeine consumption in healthy adults, pregnant women, adolescents, and children. Food Chem. Toxicol. 2017, 109, 585–648. [Google Scholar] [CrossRef]
- Poole, R.; Kennedy, O.J.; Roderick, P.; Fallowfield, J.A.; Hayes, P.C.; Parkes, J. Coffee consumption and health: Umbrella review of meta-analyses of multiple health outcomes. BMJ 2017, 359, j5024. [Google Scholar] [CrossRef] [PubMed]
- Grosso, G.; Godos, J.; Galvano, F.; Giovannucci, E.L. Coffee, caffeine, and health outcomes: An umbrella review. Annu. Rev. Nutr. 2017, 37, 131–156. [Google Scholar] [CrossRef] [PubMed]
- Eskelinen, M.H.; Ngandu, T.; Tuomilehto, J.; Soininen, H.; Kivipelto, M. Midlife coffee and tea drinking and the risk of late-life dementia: A population-based CAIDE study. J. Alzheimers Dis. 2009, 16, 85–91. [Google Scholar] [CrossRef]
- Maia, L.; de Mendonça, A. Does caffeine intake protect from Alzheimer’s disease? Eur. J. Neurol. 2002, 9, 377–382. [Google Scholar] [CrossRef]
- Hussain, A.; Tabrez, E.S.; Mavrych, V.; Bolgova, O.; Peela, J.R. Caffeine: A potential protective agent against cognitive decline in Alzheimer’s disease. Crit. Rev. Eukaryot. Gene Expr. 2018, 28, 67–72. [Google Scholar] [CrossRef]
- Chen, J.-F.; Chern, Y. Impacts of methylxanthines and adenosine receptors on neurodegeneration: Human and experimental studies. Handb. Exp. Pharmacol. 2011, 200, 267–310. [Google Scholar] [CrossRef]
- Alasmari, F. Caffeine induces neurobehavioral effects through modulating neurotransmitters. Saudi Pharm. J. 2020, 28, 445–451. [Google Scholar] [CrossRef] [PubMed]
- McLellan, T.M.; Caldwell, J.A.; Lieberman, H.R. A review of caffeine’s effects on cognitive, physical and occupational performance. Neurosci. Biobehav. Rev. 2016, 71, 294–312. [Google Scholar] [CrossRef] [PubMed]
- Kolahdouzan, M.; Hamadeh, M.J. The neuroprotective effects of caffeine in neurodegenerative diseases. CNS Neurosci. Ther. 2017, 23, 272–290. [Google Scholar] [CrossRef] [PubMed]
- Isokawa, M. Caffeine-induced suppression of GABAergic inhibition and calcium-independent metaplasticity. Neural Plast. 2016, 2016, 1239629. [Google Scholar] [CrossRef]
- Simonin, C.; Duru, C.; Salleron, J.; Hincker, P.; Charles, P.; Delval, A.; Youssov, K.; Burnouf, S.; Azulay, J.-P.; Verny, C.; et al. Association between caffeine intake and age at onset in Huntington’s disease. Neurobiol. Dis. 2013, 58, 179–182. [Google Scholar] [CrossRef] [PubMed]
- Ribeiro, J.A.; Sebastião, A.M. Caffeine and adenosine. J. Alzheimers Dis. 2010, 20, S3–S15. [Google Scholar] [CrossRef]
- Yang, J.Y.; Yang, G.; Ren, J.; Zhao, J.; Li, S. Caffeine suppresses GABA receptor-mediated current in rat primary sensory neurons via inhibition of intracellular phosphodiesterase. Neurophysiology 2015, 47, 108–114. [Google Scholar] [CrossRef]
- Kaczmarczyk-Sedlak, I.; Folwarczna, J.; Sedlak, L.; Zych, M.; Wojnar, W.; Szumińska, I.; Wyględowska-Promieńska, D.; Mrukwa-Kominek, E. Effect of caffeine on biomarkers of oxidative stress in lenses of rats with streptozotocin-induced diabetes. Arch. Med. Sci. 2019, 15, 1073–1080. [Google Scholar] [CrossRef]
- Paiva, C.; Beserra, B.; Reis, C.; Dorea, J.G.; Da Costa, T.; Amato, A.A. Consumption of coffee or caffeine and serum concentration of inflammatory markers: A systematic review. Crit. Rev. Food Sci. Nutr. 2019, 59, 652–663. [Google Scholar] [CrossRef]
- Zampelas, A.; Panagiotakos, D.B.; Pitsavos, C.; Chrysohoou, C.; Stefanadis, C. Associations between coffee consumption and inflammatory markers in healthy persons: The ATTICA study. Am. J. Clin. Nutr. 2004, 80, 862–867. [Google Scholar] [CrossRef]
- Alzheimer’s Association. 2015 Alzheimer’s disease facts and figures. Alzheimers Dement. 2015, 11, 332–384. [Google Scholar] [CrossRef]
- Soto-Rojas, L.O.; de la Cruz-López, F.; Torres, M.A.O.; Viramontes-Pintos, A.; del Cárdenas-Aguayo, M.C.; Meraz-Ríos, M.A.; Salinas-Lara, C.; Florán-Garduño, B.; Luna-Muñoz, J. Neuroinflammation and alteration of the blood-brain barrier in Alzheimer’s disease. In Alzheimer’s Disease—Challenges for the Future; IntechOpen: London, UK, 2015. [Google Scholar]
- Pini, L.; Pievani, M.; Bocchetta, M.; Altomare, D.; Bosco, P.; Cavedo, E.; Galluzzi, S.; Marizzoni, M.; Frisoni, G.B. Brain atrophy in Alzheimer’s disease and aging. Aging Res. Rev. 2016, 30, 25–48. [Google Scholar] [CrossRef] [PubMed]
- Cerejeira, J.; Lagarto, L.; Mukaetova-Ladinska, E.B. Behavioral and psychological symptoms of dementia. Front. Neurol. 2012, 3, 73. [Google Scholar] [CrossRef]
- Zhang, L.; Chen, C.; Mak, M.S.; Lu, J.; Wu, Z.; Chen, Q.; Han, Y.; Li, Y.; Pi, R. Advance of sporadic Alzheimer’s disease animal models. Med. Res. Rev. 2020, 40, 431–458. [Google Scholar] [CrossRef]
- Atri, A. Current and future treatments in Alzheimer’s disease. Semin. Neurol. 2019, 39, 227–240. [Google Scholar] [CrossRef]
- Drummond, E.; Wisniewski, T. Alzheimer’s disease: Experimental models and reality. Acta Neuropathol. 2017, 133, 155–175. [Google Scholar] [CrossRef]
- Morley, J.E.; Farr, S.A.; Nguyen, A.D. Alzheimer disease. Clin. Geriatr. Med. 2018, 34, 591–601. [Google Scholar] [CrossRef] [PubMed]
- Cavanaugh, S.E.; Pippin, J.J.; Barnard, N.D. Animal models of Alzheimer disease: Historical pitfalls and a path forward. ALTEX 2014, 31, 279–302. [Google Scholar] [CrossRef]
- Shi, Y.; Holtzman, D.M. Interplay between innate immunity and Alzheimer disease: APOE and TREM2 in the spotlight. Nat. Rev. Immunol. 2018, 18, 759–772. [Google Scholar] [CrossRef]
- Riphagen, J.M.; Ramakers, I.H.G.M.; Freeze, W.M.; Pagen, L.H.G.; Hanseeuw, B.J.; Verbeek, M.M.; Verhey, F.R.J.; Jacobs, H.I.L. Neurobiology of aging linking APOE-ε4, blood-brain barrier dysfunction, and inflammation to Alzheimer’s pathology. Neurobiol. Aging 2020, 85, 96–103. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.; Strickland, M.R.; Soranno, A.; Holtzman, D.M. Apolipoprotein E: Structural insights and links to Alzheimer disease pathogenesis. Neuron 2020, 109, 205–221. [Google Scholar] [CrossRef]
- Reitz, C.; Brayne, C.; Mayeux, R. Epidemiology of Alzheimer disease. Nat. Rev. Neurol. 2011, 7, 137–152. [Google Scholar] [CrossRef]
- Hickman, R.A.; Faustin, A.; Wisniewski, T. Alzheimer disease and its growing epidemic: Risk factors, biomarkers, and the urgent need for therapeutics. Neurol. Clin. 2016, 34, 941–953. [Google Scholar] [CrossRef]
- Esteves, I.M.; Lopes-Aguiar, C.; Rossignoli, M.T.; Ruggiero, R.N.; Broggini, A.C.S.; Bueno-Junior, L.S.; Kandratavicius, L.; Monteiro, M.R.; Romcy-Pereira, R.N.; Leite, J.P. Chronic nicotine attenuates behavioral and synaptic plasticity impairments in a streptozotocin model of Alzheimer’s disease. Neuroscience 2017, 353, 87–97. [Google Scholar] [CrossRef] [PubMed]
- de la Monte, S.M.; Tong, M.; Wands, J.R. The 20-year voyage aboard the Journal of Alzheimer’s Disease: Docking at “type 3 diabetes”, environmental/exposure factors, pathogenic mechanisms, and potential treatments. J. Alzheimers Dis. 2018, 62, 1381–1390. [Google Scholar] [CrossRef] [PubMed]
- Lester-Coll, N.; Rivera, E.J.; Soscia, S.J.; Doiron, K.; Wands, J.R.; de la Monte, S.M. Intracerebral streptozotocin model of type 3 diabetes: Relevance to sporadic Alzheimer’s disease. J. Alzheimers Dis. 2006, 9, 13–33. [Google Scholar] [CrossRef]
- Cheignon, C.; Tomas, M.; Bonnefont-Rousselot, D.; Faller, P.; Hureau, C.; Collin, F. Oxidative stress and the amyloid beta peptide in Alzheimer’s disease. Redox Biol. 2018, 14, 450–464. [Google Scholar] [CrossRef]
- Sadigh-Eteghad, S.; Sabermarouf, B.; Majdi, A.; Talebi, M.; Farhoudi, M.; Mahmoudi, J. Amyloid-beta: A crucial factor in Alzheimer’s disease. Med. Princ. Pract. 2015, 24, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Anand, A.; Patience, A.A.; Sharma, N.; Khurana, N. The present and future of pharmacotherapy of Alzheimer’s disease: A comprehensive review. Eur. J. Pharmacol. 2017, 815, 364–375. [Google Scholar] [CrossRef] [PubMed]
- Jouanne, M.; Rault, S.; Voisin-Chiret, A.-S. Tau protein aggregation in Alzheimer’s disease: An attractive target for the development of novel therapeutic agents. Eur. J. Med. Chem. 2017, 139, 153–167. [Google Scholar] [CrossRef] [PubMed]
- Du, X.; Wang, X.; Geng, M. Alzheimer’s disease hypothesis and related therapies. Transl. Neurodegener. 2018, 7, 2. [Google Scholar] [CrossRef] [PubMed]
- Heneka, M.T.; Carson, M.J.; El Khoury, J.; Landreth, G.E.; Brosseron, F.; Feinstein, D.L.; Jacobs, A.H.; Wyss-Coray, T.; Vitorica, J.; Ransohoff, R.M.; et al. Neuroinflammation in Alzheimer’s disease. Lancet Neurol. 2015, 14, 388–405. [Google Scholar] [CrossRef]
- Calsolaro, V.; Edison, P. Neuroinflammation in Alzheimer’s disease: Current evidence and future directions. Alzheimers Dement. 2016, 12, 719–732. [Google Scholar] [CrossRef] [PubMed]
- Hampel, H.; Mesulam, M.-M.; Cuello, A.C.; Farlow, M.R.; Giacobini, E.; Grossberg, G.T.; Khachaturian, A.S.; Vergallo, A.; Cavedo, E.; Snyder, P.J.; et al. The cholinergic system in the pathophysiology and treatment of Alzheimer’s disease. Brain 2018, 141, 1917–1933. [Google Scholar] [CrossRef]
- Ferreira-Vieira, T.H.; Guimaraes, I.M.; Silva, F.R.; Ribeiro, F.M. Alzheimer’s disease: Targeting the cholinergic system. Curr. Neuropharmacol. 2016, 14, 101–115. [Google Scholar] [CrossRef]
- Cellai, L.; Carvalho, K.; Faivre, E.; Deleau, A.; Vieau, D.; Buée, L.; Blum, D.; Mériaux, C.; Gomez-Murcia, V. The adenosinergic signaling: A complex but promising therapeutic target for Alzheimer’s disease. Front. Neurosci. 2018, 12, 520. [Google Scholar] [CrossRef] [PubMed]
- Rahman, A. The role of adenosine in Alzheimer’s disease. Curr. Neuropharmacol. 2009, 7, 207–216. [Google Scholar] [CrossRef]
- Wang, R.; Reddy, P.H. Role of glutamate and NMDA receptors in Alzheimer’s disease. J. Alzheimers Dis. 2017, 57, 1041–1048. [Google Scholar] [CrossRef]
- Danysz, W.; Parsons, C.G. Alzheimer’s disease, β-amyloid, glutamate, NMDA receptors and memantine—Searching for the connections. Br. J. Pharmacol. 2012, 167, 324–352. [Google Scholar] [CrossRef]
- Takahashi, R.N.; Pamplona, F.A.; Prediger, R.D.S. Adenosine receptor antagonists for cognitive dysfunction: A review of animal studies. Front. Biosci. 2008, 13, 2614–2632. [Google Scholar] [CrossRef]
- Cieślak, M.; Wojtczak, A. Role of purinergic receptors in the Alzheimer’s disease. Purinergic Signal. 2018, 14, 331–344. [Google Scholar] [CrossRef]
- Liu, K.Y.; Stringer, A.E.; Reeves, S.J.; Howard, R.J. The neurochemistry of agitation in Alzheimer’s disease: A systematic review. Aging Res. Rev. 2018, 43, 99–107. [Google Scholar] [CrossRef] [PubMed]
- Beam, C.R.; Kaneshiro, C.; Jang, J.Y.; Reynolds, C.A.; Pedersen, N.L.; Gatz, M. Differences between women and men in incidence rates of dementia and Alzheimer’s disease. J. Alzheimers Dis. 2018, 64, 1077–1083. [Google Scholar] [CrossRef]
- Podcasy, J.L.; Epperson, C.N. Considering sex and gender in Alzheimer disease and other dementias. Dialogues Clin. Neurosci. 2016, 18, 437–446. [Google Scholar] [CrossRef]
- Ferretti, M.T.; Iulita, M.F.; Cavedo, E.; Chiesa, P.A.; Dimech, A.S.; Chadha, A.S.; Baracchi, F.; Girouard, H.; Misoch, S.; Giacobini, E.; et al. Sex differences in Alzheimer disease—The gateway to precision medicine. Nat. Rev. Neurol. 2018, 14, 457–469. [Google Scholar] [CrossRef]
- Mazure, C.M.; Swendsen, J. Sex differences in Alzheimer’s disease and other dementias. Lancet Neurol. 2016, 15, 451–452. [Google Scholar] [CrossRef]
- Long, J.M.; Holtzman, D.M. Alzheimer disease: An update on pathobiology and treatment strategies. Cell 2019, 179, 312–339. [Google Scholar] [CrossRef]
- Weller, J.; Budson, A. Current understanding of Alzheimer’s disease diagnosis and treatment. F1000Research 2018, 7, F1000 Faculty Rev-1161. [Google Scholar] [CrossRef] [PubMed]
- McShane, R.; Westby, M.J.; Roberts, E.; Minakaran, N.; Schneider, L.; Farrimond, L.E.; Maayan, N.; Ware, J.; Debarros, J. Memantine for dementia. Cochrane Database Syst. Rev. 2019, 3, CD003154. [Google Scholar] [CrossRef]
- Rosini, M.; Simoni, E.; Caporaso, R.; Basagni, F.; Catanzaro, M.; Abu, I.F.; Fagiani, F.; Fusco, F.; Masuzzo, S.; Albani, D.; et al. Merging memantine and ferulic acid to probe connections between NMDA receptors, oxidative stress and amyloid-β peptide in Alzheimer’s disease. Eur. J. Med. Chem. 2019, 180, 111–120. [Google Scholar] [CrossRef] [PubMed]
- Bhat, A.; Mahalakshmi, A.M.; Ray, B.; Tuladhar, S.; Hediyal, T.A.; Manthiannem, E.; Padamati, J.; Chandra, R.; Chidambaram, S.B.; Sakharkar, M.K. Benefits of curcumin in brain disorders. Biofactors 2019, 45, 666–689. [Google Scholar] [CrossRef] [PubMed]
- Farkhondeh, T.; Samarghandian, S.; Pourbagher-Shahri, A.M.; Sedaghat, M. The impact of curcumin and its modified formulations on Alzheimer’s disease. J. Cell. Physiol. 2019, 234, 16953–16965. [Google Scholar] [CrossRef] [PubMed]
- Chen, M.; Du, Z.-Y.; Zheng, X.; Li, D.-L.; Zhou, R.-P.; Zhang, K. Use of curcumin in diagnosis, prevention, and treatment of Alzheimer’s disease. Neural Regen. Res. 2018, 13, 742–752. [Google Scholar] [CrossRef]
- Mori, T.; Koyama, N.; Tan, J.; Segawa, T.; Maeda, M.; Town, T. Combination therapy with octyl gallate and ferulic acid improves cognition and neurodegeneration in a transgenic mouse model of Alzheimer’s disease. J. Biol. Chem. 2017, 292, 11310–11325. [Google Scholar] [CrossRef]
- Sgarbossa, A.; Giacomazza, D.; di Carlo, M. Ferulic acid: A hope for Alzheimer’s disease therapy from plants. Nutrients 2015, 7, 5764–5782. [Google Scholar] [CrossRef] [PubMed]
- Meng, G.; Meng, X.; Ma, X.; Zhang, G.; Hu, X.; Jin, A.; Zhao, Y.; Liu, X. Application of ferulic acid for Alzheimer’s disease: Combination of text mining and experimental validation. Front. Neuroinform. 2018, 12, 31. [Google Scholar] [CrossRef]
- He, M.; Zhao, L.; Wei, M.-J.; Yao, W.-F.; Zhao, H.-S.; Chen, F.-J. Neuroprotective effects of (-)-epigallocatechin-3-gallate on aging mice induced by D-galactose. Biol. Pharm. Bull. 2009, 32, 55–60. [Google Scholar] [CrossRef]
- Polito, C.A.; Cai, Z.-Y.; Shi, Y.-L.; Li, X.-M.; Yang, R.; Shi, M.; Li, Q.-S.; Ma, S.-C.; Xiang, L.-P.; Wang, K.-R.; et al. Association of tea consumption with risk of Alzheimer’s disease and anti-beta-amyloid effects of tea. Nutrients 2018, 10, 655. [Google Scholar] [CrossRef] [PubMed]
- Cascella, M.; Bimonte, S.; Muzio, M.R.; Schiavone, V.; Cuomo, A. The efficacy of Epigallocatechin-3-gallate (green tea) in the treatment of Alzheimer’s disease: An overview of pre-clinical studies and translational perspectives in clinical practice. Infect. Agent. Cancer 2017, 12, 36. [Google Scholar] [CrossRef]
- Oñatibia-Astibia, A.; Franco, R.; Martínez-Pinilla, E. Health benefits of methylxanthines in neurodegenerative diseases. Mol. Nutr. Food Res. 2017, 61, 1600670. [Google Scholar] [CrossRef] [PubMed]
- Panza, F.; Solfrizzi, V.; Barulli, M.R.; Bonfiglio, C.; Guerra, V.; Osella, A.; Seripa, D.; Sabbà, C.; Pilotto, A.; Logroscino, G. Coffee, tea, and caffeine consumption and prevention of late-life cognitive decline and dementia: A systematic review. J. Nutr. Health Aging 2015, 19, 313–328. [Google Scholar] [CrossRef] [PubMed]
- Flaten, V.; Laurent, C.; Coelho, J.E.; Sandau, U.; Batalha, V.L.; Burnouf, S.; Hamdane, M.; Humez, S.; Boison, D.; Lopes, L.V.; et al. From epidemiology to pathophysiology: What about caffeine in Alzheimer’s disease? Biochem. Soc. Trans. 2014, 42, 587–592. [Google Scholar] [CrossRef]
- Kim, Y.-S.; Kwak, S.M.; Myung, S.-K. Caffeine intake from coffee or tea and cognitive disorders: A meta-analysis of observational studies. Neuroepidemiology 2015, 44, 51–63. [Google Scholar] [CrossRef]
- Wierzejska, R. Can coffee consumption lower the risk of Alzheimer’s disease and Parkinson’s disease? A literature review. Arch. Med. Sci. 2017, 13, 507–514. [Google Scholar] [CrossRef] [PubMed]
- Kakutani, S.; Watanabe, H.; Murayama, N. Green tea intake and risks for dementia, Alzheimer’s disease, mild cognitive impairment, and cognitive impairment: A systematic review. Nutrients 2019, 11, 1165. [Google Scholar] [CrossRef]
- Ma, Q.-P.; Huang, C.; Cui, Q.-Y.; Yang, D.-J.; Sun, K.; Chen, X.; Li, X.-H. Meta-analysis of the association between tea intake and the risk of cognitive disorders. PLoS ONE 2016, 11, e0165861. [Google Scholar] [CrossRef]
- Wu, L.; Sun, D.; He, Y. Coffee intake and the incident risk of cognitive disorders: A dose–response meta-analysis of nine prospective cohort studies. Clin. Nutr. 2017, 36, 730–736. [Google Scholar] [CrossRef] [PubMed]
- Liu, Q.-P.; Wu, Y.-F.; Cheng, H.-Y.; Xia, T.; Ding, H.; Wang, H.; Wang, Z.-M.; Xu, Y. Habitual coffee consumption and risk of cognitive decline/dementia: A systematic review and meta-analysis of prospective cohort studies. Nutrition 2016, 32, 628–636. [Google Scholar] [CrossRef] [PubMed]
- Larsson, S.C.; Orsini, N. Coffee consumption and risk of dementia and Alzheimer’s disease: A dose-response meta-analysis of prospective studies. Nutrients 2018, 10, 1501. [Google Scholar] [CrossRef] [PubMed]
- Zhou, A.; Taylor, A.E.; Karhunen, V.; Zhan, Y.; Rovio, S.P.; Lahti, J.; Sjögren, P.; Byberg, L.; Lyall, D.M.; Auvinen, J.; et al. Habitual coffee consumption and cognitive function: A Mendelian randomization meta-analysis in up to 415530 participants. Sci. Rep. 2018, 8, 7526. [Google Scholar] [CrossRef]
- Larsson, S.C.; Traylor, M.; Malik, R.; Dichgans, M.; Burgess, S.; Markus, H.S.; CoSTREAM Consortium, on behalf of the International Genomics of Alzheimer’s Project. Modifiable pathways in Alzheimer’s disease: Mendelian randomisation analysis. BMJ 2017, 359, j5375. [Google Scholar] [CrossRef]
- Schuster, J.; Mitchell, E.S. More than just caffeine: Psychopharmacology of methylxanthine interactions with plant-derived phytochemicals. Prog. Neuropsychopharmacol. Biol. Psychiatry 2019, 89, 263–274. [Google Scholar] [CrossRef] [PubMed]
- Colombo, R.; Papetti, A. An outlook on the role of decaffeinated coffee in neurodegenerative diseases. Crit. Rev. Food Sci. Nutr. 2020, 60, 760–779. [Google Scholar] [CrossRef]
- Dong, X.; Li, S.; Sun, J.; Li, Y.; Zhang, D. Association of coffee, decaffeinated coffee and caffeine intake from coffee with cognitive performance in older adults: National Health and Nutrition Examination Survey (NHANES) 2011–2014. Nutrients 2020, 12, 840. [Google Scholar] [CrossRef]
- Newman, M.; Kretzschmar, D.; Khan, I.; Chen, M.; Verdile, G.; Lardelli, M. Animal models of Alzheimer’s disease. In Animal Models for the Study of Human Disease, 2nd ed.; Michael Conn, P., Ed.; Academic Press: San Diego, CA, USA, 2017; pp. 1031–1085. [Google Scholar]
- Do Carmo, S.; Cuello, A.C. Modeling Alzheimer’s disease in transgenic rats. Mol. Neurodegener. 2013, 8, 37. [Google Scholar] [CrossRef]
- Esquerda-Canals, G.; Montoliu-Gaya, L.; Güell-Bosch, J.; Villegas, S. Mouse models of Alzheimer’s disease. J. Alzheimers Dis. 2017, 57, 1171–1183. [Google Scholar] [CrossRef]
- Echeverria, V.; Ducatenzeiler, A.; Alhonen, L.; Janne, J.; Grant, S.M.; Wandosell, F.; Muro, A.; Baralle, F.; Li, H.; Duff, K.; et al. Rat transgenic models with a phenotype of intracellular Aβ accumulation in hippocampus and cortex. J. Alzheimers Dis. 2004, 6, 209–219. [Google Scholar] [CrossRef] [PubMed]
- Puzzo, D.; Gulisano, W.; Palmeri, A.; Arancio, O. Rodent models for Alzheimer’s disease drug discovery. Expert Opin. Drug Discov. 2015, 10, 703–711. [Google Scholar] [CrossRef] [PubMed]
- Sun, L.; Zhou, R.; Yang, G.; Shi, Y. Analysis of 138 pathogenic mutations in presenilin-1 on the in vitro production of Aβ42 and Aβ40 peptides by γ-secretase. Proc. Natl. Acad. Sci. USA 2017, 114, E476–E485. [Google Scholar] [CrossRef] [PubMed]
- Andorfer, C.; Kress, Y.; Espinoza, M.; de Silva, R.; Tucker, K.L.; Barde, Y.-A.; Duff, K.; Davies, P. Hyperphosphorylation and aggregation of tau in mice expressing normal human tau isoforms. J. Neurochem. 2003, 86, 582–590. [Google Scholar] [CrossRef]
- Van der Jeugd, A.; Vermaercke, B.; Derisbourg, M.; Lo, A.C.; Hamdane, M.; Blum, D.; Buée, L.; D’Hooge, R. Progressive age-related cognitive decline in tau mice. J. Alzheimers Dis. 2013, 37, 777–788. [Google Scholar] [CrossRef]
- Laurent, C.; Eddarkaoui, S.; Derisbourg, M.; Leboucher, A.; Demeyer, D.; Carrier, S.; Schneider, M.; Hamdane, M.; Müller, C.E.; Buée, L.; et al. Beneficial effects of caffeine in a transgenic model of Alzheimer’s disease-like tau pathology. Neurobiol. Aging 2014, 35, 2079–2090. [Google Scholar] [CrossRef] [PubMed]
- Zappettini, S.; Faivre, E.; Ghestem, A.; Carrier, S.; Buée, L.; Blum, D.; Esclapez, M.; Bernard, C. Caffeine consumption during pregnancy accelerates the development of cognitive deficits in offspring in a model of tauopathy. Front. Cell. Neurosci. 2019, 13, 438. [Google Scholar] [CrossRef] [PubMed]
- Stover, K.R.; Campbell, M.A.; Van Winssen, C.M.; Brown, R.E. Early detection of cognitive deficits in the 3xTg-AD mouse model of Alzheimer’s disease. Behav. Brain Res. 2015, 289, 29–38. [Google Scholar] [CrossRef]
- Smith, I.F.; Hitt, B.; Green, K.N.; Oddo, S.; LaFerla, F.M. Enhanced caffeine-induced Ca2+ release in the 3xTg-AD mouse model of Alzheimer’s disease. J. Neurochem. 2005, 94, 1711–1718. [Google Scholar] [CrossRef] [PubMed]
- Oakley, H.; Cole, S.L.; Logan, S.; Maus, E.; Shao, P.; Craft, J.; Guillozet-Bongaarts, A.; Ohno, M.; Disterhoft, J.; Van Eldik, L.; et al. Intraneuronal β-amyloid aggregates, neurodegeneration, and neuron loss in transgenic mice with five familial Alzheimer’s disease mutations: Potential factors in amyloid plaque formation. J. Neurosci. 2006, 26, 10129–10140. [Google Scholar] [CrossRef]
- Cohen, R.M.; Rezai-Zadeh, K.; Weitz, T.M.; Rentsendorj, A.; Gate, D.; Spivak, I.; Bholat, Y.; Vasilevko, V.; Glabe, C.G.; Breunig, J.J.; et al. A transgenic Alzheimer rat with plaques, tau pathology, behavioral impairment, oligomeric aβ, and frank neuronal loss. J. Neurosci. 2013, 33, 6245–6256. [Google Scholar] [CrossRef]
- Smith, L.A.; McMahon, L.L. Deficits in synaptic function occur at medial perforant path-dentate granule cell synapses prior to Schaffer collateral-CA1 pyramidal cell synapses in the novel TgF344-Alzheimer’s disease rat model. Neurobiol. Dis. 2018, 110, 166–179. [Google Scholar] [CrossRef]
- Lopez, E.M.; Bell, K.F.S.; Ribeiro-da-Silva, A.; Cuello, A.C. Early changes in neurons of the hippocampus and neocortex in transgenic rats expressing intracellular human a-β. J. Alzheimers Dis. 2004, 6, 421–431, discussion 443–449. [Google Scholar] [CrossRef]
- Van Dam, D.; De Deyn, P.P. Animal models in the drug discovery pipeline for Alzheimer’s disease. Br. J. Pharmacol. 2011, 164, 1285–1300. [Google Scholar] [CrossRef]
- Cao, Z.; Wang, F.; Xiu, C.; Zhang, J.; Li, Y. Hypericum perforatum extract attenuates behavioral, biochemical, and neurochemical abnormalities in Aluminum chloride-induced Alzheimer’s disease rats. Biomed. Pharmacother. 2017, 91, 931–937. [Google Scholar] [CrossRef]
- McDonald, M.P.; Overmier, J.B. Present imperfect: A critical review of animal models of the mnemonic impairments in Alzheimer’s disease. Neurosci. Biobehav. Rev. 1998, 22, 99–120. [Google Scholar] [CrossRef]
- Botton, P.H.; Costa, M.S.; Ardais, A.P.; Mioranzza, S.; Souza, D.O.; da Rocha, J.B.T.; Porciúncula, L.O. Caffeine prevents disruption of memory consolidation in the inhibitory avoidance and novel object recognition tasks by scopolamine in adult mice. Behav. Brain Res. 2010, 214, 254–259. [Google Scholar] [CrossRef]
- Nazem, A.; Sankowski, R.; Bacher, M.; Al-Abed, Y. Rodent models of neuroinflammation for Alzheimer’s disease. J. Neuroinflamm. 2015, 12, 74. [Google Scholar] [CrossRef] [PubMed]
- Dall’Igna, O.P.; Fett, P.; Gomes, M.W.; Souza, D.O.; Cunha, R.A.; Lara, D.R. Caffeine and adenosine A(2a) receptor antagonists prevent β-amyloid (25–35)-induced cognitive deficits in mice. Exp. Neurol. 2007, 203, 241–245. [Google Scholar] [CrossRef] [PubMed]
- Salkovic-Petrisic, M.; Knezovic, A.; Hoyer, S.; Riederer, P. What have we learned from the streptozotocin-induced animal model of sporadic Alzheimer’s disease, about the therapeutic strategies in Alzheimer’s research. J. Neural Transm. 2013, 120, 233–252. [Google Scholar] [CrossRef]
- Ullah, F.; Ali, T.; Ullah, N.; Kim, M.O. Caffeine prevents d-galactose-induced cognitive deficits, oxidative stress, neuroinflammation and neurodegeneration in the adult rat brain. Neurochem. Int. 2015, 90, 114–124. [Google Scholar] [CrossRef]
- Cunha, G.M.A.; Canas, P.M.; Melo, C.S.; Hockemeyer, J.; Müller, C.E.; Oliveira, C.R.; Cunha, R.A. Adenosine A2A receptor blockade prevents memory dysfunction caused by β-amyloid peptides but not by scopolamine or MK-801. Exp. Neurol. 2008, 210, 776–781. [Google Scholar] [CrossRef]
- Gulyaeva, N.V.; Bobkova, N.V.; Kolosova, N.G.; Samokhin, A.N.; Stepanichev, M.Y.; Stefanova, N.A. Molecular and cellular mechanisms of sporadic Alzheimer’s disease: Studies on rodent models in vivo. Biochemistry 2017, 82, 1088–1102. [Google Scholar] [CrossRef]
- Brothers, H.M.; Marchalant, Y.; Wenk, G.L. Caffeine attenuates lipopolysaccharide-induced neuroinflammation. Neurosci. Lett. 2010, 480, 97–100. [Google Scholar] [CrossRef] [PubMed]
- Badshah, H.; Ikram, M.; Ali, W.; Ahmad, S.; Hahm, J.R.; Kim, M.O. Caffeine may abrogate LPS-induced oxidative stress and neuroinflammation by regulating Nrf2/TLR4 in adult mouse brains. Biomolecules 2019, 9, 719. [Google Scholar] [CrossRef] [PubMed]
- Zakaria, R.; Wan Yaacob, W.M.; Othman, Z.; Long, I.; Ahmad, A.H.; Al-Rahbi, B. Lipopolysaccharide-induced memory impairment in rats: A model of Alzheimer’s disease. Physiol. Res. 2017, 66, 553–565. [Google Scholar] [CrossRef] [PubMed]
- Stefanova, N.A.; Muraleva, N.A.; Korbolina, E.E.; Kiseleva, E.; Maksimova, K.Y.; Kolosova, N.G. Amyloid accumulation is a late event in sporadic Alzheimer’s disease-like pathology in nontransgenic rats. Oncotarget 2015, 6, 1396–1413. [Google Scholar] [CrossRef] [PubMed]
- Stefanova, N.A.; Kozhevnikova, O.S.; Vitovtov, A.O.; Maksimova, K.Y.; Logvinov, S.V.; Rudnitskaya, E.A.; Korbolina, E.E.; Muraleva, N.A.; Kolosova, N.G. Senescence-accelerated OXYS rats: A model of age-related cognitive decline with relevance to abnormalities in Alzheimer disease. Cell Cycle 2014, 13, 898–909. [Google Scholar] [CrossRef]
- Chen, W.N.; Yeong, K.Y. Scopolamine, a toxin-induced experimental model, used for research in Alzheimer’s disease. CNS Neurol. Disord. Drug Targets 2020, 19, 85–93. [Google Scholar] [CrossRef]
- Zeitlin, R.; Patel, S.; Burgess, S.; Arendash, G.W.; Echeverria, V. Caffeine induces beneficial changes in PKA signaling and JNK and ERK activities in the striatum and cortex of Alzheimer’s transgenic mice. Brain Res. 2011, 1417, 127–136. [Google Scholar] [CrossRef] [PubMed]
- Arendash, G.W.; Schleif, W.; Rezai-Zadeh, K.; Jackson, E.K.; Zacharia, L.C.; Cracchiolo, J.R.; Shippy, D.; Tan, J. Caffeine protects Alzheimer’s mice against cognitive impairment and reduces brain β-amyloid production. Neuroscience 2006, 142, 941–952. [Google Scholar] [CrossRef]
- Arendash, G.W.; Mori, T.; Cao, C.; Mamcarz, M.; Runfeldt, M.; Dickson, A.; Rezai-Zadeh, K.; Tan, J.; Citron, B.A.; Lin, X.; et al. Caffeine reverses cognitive impairment and decreases brain amyloid-β levels in aged Alzheimer’s disease mice. J. Alzheimers Dis. 2009, 17, 661–680. [Google Scholar] [CrossRef]
- Chu, Y.-F.; Chang, W.-H.; Black, R.M.; Liu, J.-R.; Sompol, P.; Chen, Y.; Wei, H.; Zhao, Q.; Cheng, I.H. Crude caffeine reduces memory impairment and amyloid β(1–42) levels in an Alzheimer’s mouse model. Food Chem. 2012, 135, 2095–2102. [Google Scholar] [CrossRef]
- Han, K.; Jia, N.; Li, J.; Yang, L.; Min, L.-Q. Chronic caffeine treatment reverses memory impairment and the expression of brain BNDF and TrkB in the PS1/APP double transgenic mouse model of Alzheimer’s disease. Mol. Med. Rep. 2013, 8, 737–740. [Google Scholar] [CrossRef]
- Dragicevic, N.; Delic, V.; Cao, C.; Copes, N.; Lin, X.; Mamcarz, M.; Wang, L.; Arendash, G.W.; Bradshaw, P.C. Caffeine increases mitochondrial function and blocks melatonin signaling to mitochondria in Alzheimer’s mice and cells. Neuropharmacology 2012, 63, 1368–1379. [Google Scholar] [CrossRef]
- Cao, C.; Cirrito, J.R.; Lin, X.; Wang, L.; Verges, D.K.; Dickson, A.; Mamcarz, M.; Zhang, C.; Mori, T.; Arendash, G.W.; et al. Caffeine suppresses β-amyloid levels in plasma and brain of Alzheimer’s transgenic mice. J. Alzheimers Dis. 2009, 17, 681–697. [Google Scholar] [CrossRef]
- Baeta-Corral, R.; Johansson, B.; Giménez-Llort, L. Long-term treatment with low-dose caffeine worsens BPSD-like profile in 3xTg-AD mice model of Alzheimer’s disease and affects mice with normal aging. Front. Pharmacol. 2018, 9, 79. [Google Scholar] [CrossRef] [PubMed]
- Cao, C.; Wang, L.; Lin, X.; Mamcarz, M.; Zhang, C.; Bai, G.; Nong, J.; Sussman, S.; Arendash, G. Caffeine synergizes with another coffee component to increase plasma GCSF: Linkage to cognitive benefits in Alzheimer’s mice. J. Alzheimers Dis. 2011, 25, 323–335. [Google Scholar] [CrossRef] [PubMed]
- Götz, J.; Streffer, J.R.; David, D.; Schild, A.; Hoerndli, F.; Pennanen, L.; Kurosinski, P.; Chen, F. Transgenic animal models of Alzheimer’s disease and related disorders: Histopathology, behavior and therapy. Mol. Psychiatry 2004, 9, 664–683. [Google Scholar] [CrossRef] [PubMed]
- Chu, Y.-F.; Chen, Y.; Brown, P.H.; Lyle, B.J.; Black, R.M.; Cheng, I.H.; Ou, B.; Prior, R.L. Bioactivities of crude caffeine: Antioxidant activity, cyclooxygenase-2 inhibition, and enhanced glucose uptake. Food Chem. 2012, 131, 564–568. [Google Scholar] [CrossRef]
- Laurent, C.; Burnouf, S.; Ferry, B.; Batalha, V.L.; Coelho, J.E.; Baqi, Y.; Malik, E.; Mariciniak, E.; Parrot, S.; Van der Jeugd, A.; et al. A2A adenosine receptor deletion is protective in a mouse model of Tauopathy. Mol. Psychiatry 2016, 21, 97–107. [Google Scholar] [CrossRef]
- Canas, P.M.; Porciúncula, L.O.; Cunha, G.M.A.; Silva, C.G.; Machado, N.J.; Oliveira, J.M.A.; Oliveira, C.R.; Cunha, R.A. Adenosine A2A receptor blockade prevents synaptotoxicity and memory dysfunction caused by β-amyloid peptides via p38 mitogen-activated protein kinase pathway. J. Neurosci. 2009, 29, 14741–14751. [Google Scholar] [CrossRef] [PubMed]
- Espinosa, J.; Rocha, A.; Nunes, F.; Costa, M.S.; Schein, V.; Kazlauckas, V.; Kalinine, E.; Souza, D.O.; Cunha, R.A.; Porciúncula, L.O. Caffeine consumption prevents memory impairment, neuronal damage, and adenosine A2A receptors upregulation in the hippocampus of a rat model of sporadic dementia. J. Alzheimers Dis. 2013, 34, 509–518. [Google Scholar] [CrossRef]
- Ghoneim, F.M.; Khalaf, H.A.; Elsamanoudy, A.Z.; Abo El-Khair, S.M.; Helaly, A.M.N.; Mahmoud, E.-H.M.; Elshafey, S.H. Protective effect of chronic caffeine intake on gene expression of brain derived neurotrophic factor signaling and the immunoreactivity of glial fibrillary acidic protein and Ki-67 in Alzheimer’s disease. Int. J. Clin. Exp. Pathol. 2015, 8, 7710–7728. [Google Scholar]
- Hosny, E.N.; Sawie, H.G.; Elhadidy, M.E.; Khadrawy, Y.A. Evaluation of antioxidant and anti-inflammatory efficacy of caffeine in rat model of neurotoxicity. Nutr. Neurosci. 2019, 22, 789–796. [Google Scholar] [CrossRef] [PubMed]
- Ravelli, K.G.; Rosário, B. dos A.; Camarini, R.; Hernandes, M.S.; Britto, L.R. Intracerebroventricular streptozotocin as a model of Alzheimer’s disease: Neurochemical and behavioral characterization in mice. Neurotox. Res. 2017, 31, 327–333. [Google Scholar] [CrossRef] [PubMed]
- Duarte, J.M.N.; Carvalho, R.A.; Cunha, R.A.; Gruetter, R. Caffeine consumption attenuates neurochemical modifications in the hippocampus of streptozotocin-induced diabetic rats. J. Neurochem. 2009, 111, 368–379. [Google Scholar] [CrossRef]
- Al Marshad, R.; Al Khatib, R.; Amer, H.; Al Shammari, M.; Al Otaibi, A.; Al Otaibi, F.; Behbehani, N.; Al Sayed, A.; Al Hoty, N.; Hassan, Z.; et al. Streptozotocin-induced diabetes mellitus affects the NMDA receptors: Role of caffeine administration in enhancing learning, memory and locomotor deficits. Int. J. Health Sci. 2018, 12, 10–17. [Google Scholar]
- Song, J. Animal model of Aluminum-induced Alzheimer’s disease. Adv. Exp. Med. Biol. 2018, 1091, 113–127. [Google Scholar] [CrossRef] [PubMed]
- Tang, K.S. The cellular and molecular processes associated with scopolamine-induced memory deficit: A model of Alzheimer’s biomarkers. Life Sci. 2019, 233, 116695. [Google Scholar] [CrossRef] [PubMed]
- Klinkenberg, I.; Blokland, A. The validity of scopolamine as a pharmacological model for cognitive impairment: A review of animal behavioral studies. Neurosci. Biobehav. Rev. 2010, 34, 1307–1350. [Google Scholar] [CrossRef] [PubMed]
- More, S.V.; Kumar, H.; Cho, D.-Y.; Yun, Y.-S.; Choi, D.-K. Toxin-induced experimental models of learning and memory impairment. Int. J. Mol. Sci. 2016, 17, 1447. [Google Scholar] [CrossRef]
- Riedel, W.; Hogervorst, E.; Leboux, R.; Verhey, F.; van Praag, H.; Jolles, J. Caffeine attenuates scopolamine-induced memory impairment in humans. Psychopharmacology 1995, 122, 158–168. [Google Scholar] [CrossRef]
- Lee, H.E.; Jeon, S.J.; Ryu, B.; Park, S.J.; Ko, S.Y.; Lee, Y.; Kim, E.; Lee, S.; Kim, H.; Jang, D.S.; et al. Swertisin, a C-glucosylflavone, ameliorates scopolamine-induced memory impairment in mice with its adenosine A1 receptor antagonistic property. Behav. Brain Res. 2016, 306, 137–145. [Google Scholar] [CrossRef]
- Pagnussat, N.; Almeida, A.S.; Marques, D.M.; Nunes, F.; Chenet, G.C.; Botton, P.H.S.; Mioranzza, S.; Loss, C.M.; Cunha, R.A.; Porciúncula, L.O. Adenosine A(2A) receptors are necessary and sufficient to trigger memory impairment in adult mice. Br. J. Pharmacol. 2015, 172, 3831–3845. [Google Scholar] [CrossRef] [PubMed]
- Chen, X.; Ghribi, O.; Geiger, J.D. Caffeine protects against disruptions of the blood-brain barrier in animal models of Alzheimer’s and Parkinson’s disease. J. Alzheimers Dis. 2010, 20, S127–S141. [Google Scholar] [CrossRef]
- Chen, X.; Gawryluk, J.W.; Wagener, J.F.; Ghribi, O.; Geiger, J.D. Caffeine blocks disruption of blood brain barrier in a rabbit model of Alzheimer’s disease. J. Neuroinflamm. 2008, 5, 12. [Google Scholar] [CrossRef]
- Prasanthi, J.R.P.; Dasari, B.; Marwarha, G.; Larson, T.; Chen, X.; Geiger, J.D.; Ghribi, O. Caffeine protects against oxidative stress and Alzheimer’s disease-like pathology in rabbit hippocampus induced by cholesterol-enriched diet. Free Radic. Biol. Med. 2010, 49, 1212–1220. [Google Scholar] [CrossRef]
- Nia, B.V.; Kang, C.; Tran, M.G.; Lee, D.; Murakami, S. Meta analysis of human AlzGene database: Benefits and limitations of using C. elegans for the study of Alzheimer’s disease and co-morbid conditions. Front. Genet. 2017, 8, 55. [Google Scholar] [CrossRef]
- Boasquívis, P.F.; Silva, G.M.M.; Paiva, F.A.; Cavalcanti, R.M.; Nunez, C.V.; de Paula Oliveira, R. Guarana (Paullinia cupana) extract protects Caenorhabditis elegans models for Alzheimer disease and Huntington disease through activation of antioxidant and protein degradation pathways. Oxid. Med. Cell. Longev. 2018, 2018, 9241308. [Google Scholar] [CrossRef]
- Griffin, E.F.; Caldwell, K.A.; Caldwell, G.A. Genetic and pharmacological discovery for Alzheimer’s disease using Caenorhabditis elegans. ACS Chem. Neurosci. 2017, 8, 2596–2606. [Google Scholar] [CrossRef] [PubMed]
- Dostal, V.; Roberts, C.M.; Link, C.D. Genetic mechanisms of coffee extract protection in a Caenorhabditis elegans model of β-amyloid peptide toxicity. Genetics 2010, 186, 857–866. [Google Scholar] [CrossRef]
- Machado, M.L.; Arantes, L.P.; da Silveira, T.L.; Zamberlan, D.C.; Cordeiro, L.M.; Obetine, F.B.B.; da Silva, A.F.; da Cruz, I.B.M.; Soares, F.A.A.; de Oliveira, R.P. Ilex paraguariensis extract provides increased resistance against oxidative stress and protection against Amyloid beta-induced toxicity compared to caffeine in Caenorhabditis elegans. Nutr. Neurosci. 2019, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Du, F.; Zhou, L.; Jiao, Y.; Bai, S.; Wang, L.; Ma, J.; Fu, X. Ingredients in Zijuan Pu’er tea extract alleviate β-amyloid peptide toxicity in a Caenorhabditis elegans model of Alzheimer’s disease likely through DAF-16. Molecules 2019, 24, 729. [Google Scholar] [CrossRef]
- Goussakov, I.; Miller, M.B.; Stutzmann, G.E. NMDA-mediated Ca(2+) influx drives aberrant ryanodine receptor activation in dendrites of young Alzheimer’s disease mice. J. Neurosci. 2010, 30, 12128–12137. [Google Scholar] [CrossRef]
- Giunta, S.; Andriolo, V.; Castorina, A. Dual blockade of the A1 and A2A adenosine receptor prevents amyloid beta toxicity in neuroblastoma cells exposed to aluminum chloride. Int. J. Biochem. Cell Biol. 2014, 54, 122–136. [Google Scholar] [CrossRef]
- Keshavarz, M.; Farrokhi, M.R.; Amiri, A. Caffeine neuroprotective mechanism against β-amyloid neurotoxicity in SHSY5Y cell line: Involvement of adenosine, ryanodine, and N-methyl-D-aspartate receptors. Adv. Pharm. Bull. 2017, 7, 579–584. [Google Scholar] [CrossRef]
- Stoppelkamp, S.; Bell, H.S.; Palacios-Filardo, J.; Shewan, D.A.; Riedel, G.; Platt, B. In vitro modelling of Alzheimer’s disease: Degeneration and cell death induced by viral delivery of amyloid and tau. Exp. Neurol. 2011, 229, 226–237. [Google Scholar] [CrossRef] [PubMed]
- Gupta, S.; Dasmahapatra, A.K. Caffeine destabilizes preformed Aβ protofilaments: Insights from all atom molecular dynamics simulations. Phys. Chem. Chem. Phys. 2019, 21, 22067–22080. [Google Scholar] [CrossRef]
- Sharma, B.; Paul, S. Action of caffeine as an amyloid inhibitor in the aggregation of Aβ16–22 peptides. J. Phys. Chem. B 2016, 120, 9019–9033. [Google Scholar] [CrossRef] [PubMed]
- Kumar, A.; Mehta, V.; Raj, U.; Varadwaj, P.K.; Udayabanu, M.; Yennamalli, R.M.; Singh, T.R. Computational and in-vitro validation of natural molecules as potential acetylcholinesterase inhibitors and neuroprotective agents. Curr. Alzheimer Res. 2019, 16, 116–127. [Google Scholar] [CrossRef]
- Ali, B.; Jamal, Q.M.S.; Shams, S.; Al-Wabel, N.A.; Siddiqui, M.U.; Alzohairy, M.A.; Al Karaawi, M.A.; Kesari, K.K.; Mushtaq, G.; Kamal, M.A. In silico analysis of green tea polyphenols as inhibitors of AChE and BChE enzymes in Alzheimer’s disease treatment. Cns Neurol. Disord. Drug Targets 2016, 15, 624–628. [Google Scholar] [CrossRef] [PubMed]
- Yiannopoulou, K.G.; Anastasiou, A.I.; Zachariou, V.; Pelidou, S.-H. Reasons for failed trials of disease-modifying treatments for Alzheimer disease and their contribution in recent research. Biomedicines 2019, 7, 97. [Google Scholar] [CrossRef]
- Oboh, G.; Ogunsuyi, O.B.; Olonisola, O.E. Does caffeine influence the anticholinesterase and antioxidant properties of donepezil? Evidence from in vitro and in vivo studies. Metab. Brain Dis. 2017, 32, 629–639. [Google Scholar] [CrossRef]
- Nair, A.B.; Jacob, S. A simple practice guide for dose conversion between animals and human. J. Basic Clin. Pharm. 2016, 7, 27–31. [Google Scholar] [CrossRef]
- Reagan-Shaw, S.; Nihal, M.; Ahmad, N. Dose translation from animal to human studies revisited. Faseb J. 2008, 22, 659–661. [Google Scholar] [CrossRef]
- Cunha, R.A. How does adenosine control neuronal dysfunction and neurodegeneration? J. Neurochem. 2016, 139, 1019–1055. [Google Scholar] [CrossRef]
- Dall’lgna, O.P.; Porciúncula, L.O.; Souza, D.O.; Cunha, R.A.; Lara, D.R. Neuroprotection by caffeine and adenosine A2A receptor blockade of β-amyloid neurotoxicity. Br. J. Pharmacol. 2003, 138, 1207–1209. [Google Scholar] [CrossRef] [PubMed]
- Faivre, E.; Coelho, J.E.; Zornbach, K.; Malik, E.; Baqi, Y.; Schneider, M.; Cellai, L.; Carvalho, K.; Sebda, S.; Figeac, M.; et al. Beneficial effect of a selective adenosine A2A receptor antagonist in the APPswe/PS1dE9 mouse model of Alzheimer’s disease. Front. Mol. Neurosci. 2018, 11, 235. [Google Scholar] [CrossRef] [PubMed]
- da Silva, S.V.; Haberl, M.G.; Zhang, P.; Bethge, P.; Lemos, C.; Gonçalves, N.; Gorlewicz, A.; Malezieux, M.; Gonçalves, F.Q.; Grosjean, N.; et al. Early synaptic deficits in the APP/PS1 mouse model of Alzheimer’s disease involve neuronal adenosine A2A receptors. Nat. Commun. 2016, 7, 11915. [Google Scholar] [CrossRef] [PubMed]
- Silva, A.C.; Lemos, C.; Gonçalves, F.Q.; Pliássova, A.V.; Machado, N.J.; Silva, H.B.; Canas, P.M.; Cunha, R.A.; Lopes, J.P.; Agostinho, P. Blockade of adenosine A2A receptors recovers early deficits of memory and plasticity in the triple transgenic mouse model of Alzheimer’s disease. Neurobiol. Dis. 2018, 117, 72–81. [Google Scholar] [CrossRef]
- Cunha, R.A.; Agostinho, P.M. Chronic caffeine consumption prevents memory disturbance in different animal models of memory decline. J. Alzheimers Dis. 2010, 20, S95–S116. [Google Scholar] [CrossRef]
- Nabbi-Schroeter, D.; Elmenhorst, D.; Oskamp, A.; Laskowski, S.; Bauer, A.; Kroll, T. Effects of long-term caffeine consumption on the adenosine A1 receptor in the rat brain: An in vivo PET study with [18F]CPFPX. Mol. Imaging Biol. 2018, 20, 284–291. [Google Scholar] [CrossRef]
- Janitschke, D.; Nelke, C.; Lauer, A.A.; Regner, L.; Winkler, J.; Thiel, A.; Grimm, H.S.; Hartmann, T.; Grimm, M.O.W. Effect of caffeine and other methylxanthines on Aβ-homeostasis in SH-SY5Y cells. Biomolecules 2019, 9, 689. [Google Scholar] [CrossRef]
- Zhang, L.-F.; Zhou, Z.-W.; Wang, Z.-H.; Du, Y.-H.; He, Z.-X.; Cao, C.; Zhou, S.-F. Coffee and caffeine potentiate the antiamyloidogenic activity of melatonin via inhibition of Aβ oligomerization and modulation of the Tau-mediated pathway in N2a/APP cells. Drug Des. Devel. Ther. 2014, 9, 241–272. [Google Scholar] [CrossRef]
- Fukuyama, K.; Kakio, S.; Nakazawa, Y.; Kobata, K.; Funakoshi-Tago, M.; Suzuki, T.; Tamura, H. Roasted coffee reduces β-amyloid production by increasing proteasomal β-secretase degradation in human neuroblastoma SH-SY5Y cells. Mol. Nutr. Food Res. 2018, 62, e1800238. [Google Scholar] [CrossRef] [PubMed]
- Kakio, S.; Funakoshi-Tago, M.; Kobata, K.; Tamura, H. Coffee induces vascular endothelial growth factor (VEGF) expression in human neuroblastama SH-SY5Y cells. Nutr. Neurosci. 2017, 20, 336–342. [Google Scholar] [CrossRef]
- Madeira, M.H.; Boia, R.; Ambrósio, A.F.; Santiago, A.R. Having a coffee break: The impact of caffeine consumption on microglia-mediated inflammation in neurodegenerative diseases. Mediat. Inflamm. 2017, 2017, 4761081. [Google Scholar] [CrossRef] [PubMed]
- Kwon, S.-H.; Lee, H.-K.; Kim, J.-A.; Hong, S.-I.; Kim, H.-C.; Jo, T.-H.; Park, Y.-I.; Lee, C.-K.; Kim, Y.-B.; Lee, S.-Y.; et al. Neuroprotective effects of chlorogenic acid on scopolamine-induced amnesia via anti-acetylcholinesterase and anti-oxidative activities in mice. Eur. J. Pharmacol. 2010, 649, 210–217. [Google Scholar] [CrossRef] [PubMed]
- Lee, C.W.; Won, T.J.; Kim, H.R.; Lee, D.; Hwang, K.W.; Park, S.-Y. Protective effect of chlorogenic acid against Aβ-induced neurotoxicity. Biomol. Ther. 2011, 19, 181–186. [Google Scholar] [CrossRef]
- Oboh, G.; Agunloye, O.M.; Akinyemi, A.J.; Ademiluyi, A.O.; Adefegha, S.A. Comparative study on the inhibitory effect of caffeic and chlorogenic acids on key enzymes linked to Alzheimer’s disease and some pro-oxidant induced oxidative stress in rats’ brain-in vitro. Neurochem. Res. 2013, 38, 413–419. [Google Scholar] [CrossRef]
- Gao, L.; Li, X.; Meng, S.; Ma, T.; Wan, L.; Xu, S. Chlorogenic acid alleviates Aβ25–35-induced autophagy and cognitive impairment via the mTOR/TFEB signaling pathway. Drug Des. Devel. Ther. 2020, 14, 1705–1716. [Google Scholar] [CrossRef]
- Wang, Y.; Wang, Y.; Li, J.; Hua, L.; Han, B.; Zhang, Y.; Yang, X.; Zeng, Z.; Bai, H.; Yin, H.; et al. Effects of caffeic acid on learning deficits in a model of Alzheimer’s disease. Int. J. Mol. Med. 2016, 38, 869–875. [Google Scholar] [CrossRef]
- Fisone, G.; Borgkvist, A.; Usiello, A. Caffeine as a psychomotor stimulant: Mechanism of action. Cell. Mol. Life Sci. 2004, 61, 857–872. [Google Scholar] [CrossRef]
- Cornelis, M.C.; Munafo, M.R. Mendelian randomization studies of coffee and caffeine consumption. Nutrients 2018, 10, 1343. [Google Scholar] [CrossRef] [PubMed]
- Temple, J.L.; Bernard, C.; Lipshultz, S.E.; Czachor, J.D.; Westphal, J.A.; Mestre, M.A. The safety of ingested caffeine: A comprehensive review. Front. Psychiatry 2017, 8, 80. [Google Scholar] [CrossRef]
- van Dam, R.M.; Hu, F.B.; Willett, W.C. Coffee, caffeine, and health. N. Engl. J. Med. 2020, 383, 369–378. [Google Scholar] [CrossRef] [PubMed]
- O’Callaghan, F.; Muurlink, O.; Reid, N. Effects of caffeine on sleep quality and daytime functioning. Risk Manag. Healthc. Policy 2018, 11, 263–271. [Google Scholar] [CrossRef]
- Torres-Ugalde, Y.C.; Romero-Palencia, A.; Román-Gutiérrez, A.D.; Ojeda-Ramírez, D.; Guzmán-Saldaña, R.M.E. Caffeine consumption in children: Innocuous or deleterious? A systematic review. Int. J. Environ. Res. Public Health 2020, 17, 2489. [Google Scholar] [CrossRef]
- Anderson, R.M.; Hadjichrysanthou, C.; Evans, S.; Wong, M.M. Why do so many clinical trials of therapies for Alzheimer’s disease fail? Lancet 2017, 390, 2327–2329. [Google Scholar] [CrossRef]
- Palmqvist, S.; Insel, P.S.; Stomrud, E.; Janelidze, S.; Zetterberg, H.; Brix, B.; Eichenlaub, U.; Dage, J.L.; Chai, X.; Blennow, K.; et al. Cerebrospinal fluid and plasma biomarker trajectories with increasing amyloid deposition in Alzheimer’s disease. EMBO Mol. Med. 2019, 11, e11170. [Google Scholar] [CrossRef]
- Iranpour, S.; Saadati, H.M.; Koohi, F.; Sabour, S. Association between caffeine intake and cognitive function in adults; effect modification by sex: Data from National Health and Nutrition Examination Survey (NHANES) 2013–2014. Clin. Nutr. 2020, 39, 2158–2168. [Google Scholar] [CrossRef]
- Ritchie, K.; Carrière, I.; de Mendonça, A.; Portet, F.; Dartigues, J.F.; Rouaud, O.; Barberger-Gateau, P.; Ancelin, M.L. The neuroprotective effects of caffeine: A prospective population study (the Three City Study). Neurology 2007, 69, 536–545. [Google Scholar] [CrossRef]
- Johnson-Kozlow, M.; Kritz-Silverstein, D.; Barrett-Connor, E.; Morton, D. Coffee consumption and cognitive function among older adults. Am. J. Epidemiol. 2002, 156, 842–850. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).