Placing a Well-Designed Vegan Diet for Slovenes
Abstract
1. Introduction
2. The Definition of a Vegan Diet
3. Health Effects of a Vegan Diet
3.1. In Adults
3.1.1. Body Mass and Body Composition
3.1.2. Cardiovascular Health
3.1.3. Diabetes Type 2
3.1.4. Other Health Benefits
3.1.5. Sport and Exercise Performance
3.2. During Pregnancy, Breastfeeding, Infancy and Childhood
4. Vegan Diet and Environmental Footprint
5. Nutrients of Concern in Vegan Diet
- sufficient intake of energy and protein;
- nutrients that should be obtained from dietary supplements or enriched foods (i.e., vitamin B12, vitamin D, omega-3 fatty acids); and
- micronutrients of concern (i.e., calcium, iron, zinc, iodine and selenium).
5.1. Energy and Protein Intake Concerns
5.2. Nutrients That Should Be Obtained from Dietary Supplements or Enriched Foods
5.2.1. Vitamin B12
5.2.2. Vitamin D
5.2.3. Omega-3 Fatty Acids
5.3. Micronutrients of Concern (i.e., Calcium, Iron, Zinc, Iodine and Selenium)
5.3.1. Calcium
5.3.2. Iron and Zinc
5.3.3. Iodine and Selenium
6. Practical Recommendations for Implementing Vegan Diet
- unprocessed or minimally processed plant-based foods, especially whole grains, legumes, fruits and vegetables, can be eaten ad libitum (i.e., moderate to full satiety) [197];
- whole grains (e.g., oats, buckwheat, rice, millet, quinoa, corn, rye), legumes (e.g., beans, lentils, soy foods, peas, chickpeas) and fruits (e.g., all types but preferably berries) should provide the majority of energy intake and should be included in most meals [41];
- tubers (e.g., white and sweet potatoes), colorful, green leafy and cruciferous vegetables, fresh/dry herbs, spices and aromatics are encouraged on a daily basis [41];
- nuts (e.g., walnuts, hazelnuts, almonds, peanuts) and seeds (e.g., flaxseeds, chia, sesame and hemp seeds) should be consumed daily but sparingly within a meal and in a natural form (without added salt or oil and, if possible, unroasted) [282];
- plant-based or non-dairy milk alternatives (with vitamin D, B12 and calcium when possible): (a) cereal based: oat milk, rice milk, corn milk, spelt milk; (b) legume based: soy milk, peanut milk, lupin milk, cowpea milk; (c) nut based: almond milk, coconut milk, hazelnut milk, pistachio milk, walnut milk; (d) seed based: sesame milk, flax milk, hemp milk, sunflower milk; and (e) pseudo-cereal based: quinoa milk, teff milk and amaranth milk are optional and, whenever possible, should have no free sugars, added vegetable oil or salt [283,284];
- to enhance the aroma and flavor as well as the antioxidative potential of dishes, culturally inspired spice combinations are recommended: fresh and/or dried herbs, spices and aromatics, such as Mediterranean, which is comprised of basil, garlic, leek, marjoram, onion, oregano, rosemary, sage, thyme and white pepper. Other options are Thai (i.e., chili, ginger), Mexican and Spanish (i.e., chili, coriander, cumin, parsley), Moroccan and African (i.e., cardamom, clove, saffron), Japanese and Chinese (i.e., wasabi), Turkish and Greek (i.e., anise, cilantro, chili, thyme) and Indian (i.e., curry, turmeric) [285];
- primary liquids should be water and herbal teas (e.g., green, black and hibiscus), and to a lesser extent fresh green smoothies, whereas other liquids (e.g., sports drinks, plant-based protein supplements in connection with PA, plant-based meal replacements) may be used in cases of increased energy and nutritional requirements (e.g., with the precondition of maintaining an intake of 45–80 g fiber/day, which is considered for a well-designed vegan diet [71,187,191,199,289,290], the recommended daily intake of protein and micronutrients [196]) and with as low as possible an intake of free sugars [280] and saturated fats [291];
- to meet higher energy requirements, individuals may incorporate carbohydrate-rich foods (e.g., dry fruits, whole grain spaghetti, polenta, whole grain bread) in smaller amounts of fat-rich foods (e.g., nuts, seeds and avocado) or mixed sources (e.g., burgers, spreads and dressings, ideally without free sugars and fat);
- the main appropriate cooking methods are moist heat (such as poaching, simmering, boiling, steaming), combination cooking (braising, stewing, pressure cooking), no heat (curing, culturing, fermenting, acidifying, sprouting, soaking, high-speed blending, pureeing, vacuum sealing, juicing (in rare cases, small amounts only), dehydrating) and dry heat (air drying/dehydrating, sweating, searing, stir-frying, griddle cooking, baking, roasting, grilling, broiling, sauntering) [292].
7. Barriers to the Implementation of the Vegan Diet/Lifestyle
7.1. Lack of Education in the Vegan Field of Nutrition by Physicians and Dietitians
7.2. Lack of Financial Interest in Research on the Vegan Diet
7.3. Obesogenic Food Environment That Poses an Increasing Challenge
7.4. Believing That a Vegan Diet Is Expensive
7.5. Specific Characteristics of a Vegan Diet/Lifestyle
7.6. Animal-Based Analogues/Alternatives
8. Conclusions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Willett, W.; Rockström, J.; Loken, B.; Springmann, M.; Lang, T.; Vermeulen, S.; Garnett, T.; Tilman, D.; DeClerck, F.; Wood, A.; et al. Food in the Anthropocene: The EAT–Lancet Commission on healthy diets from sustainable food systems. Lancet 2019, 393, 447–492. [Google Scholar] [CrossRef]
- Greger, M. Primary Pandemic Prevention. Am. J. Lifestyle Med. 2021, 15, 498–505. [Google Scholar] [CrossRef]
- Springmann, M.; Spajic, L.; Clark, M.A.; Poore, J.; Herforth, A.; Webb, P.; Rayner, M.; Scarborough, P. The healthiness and sustainability of national and global food based dietary guidelines: Modelling study. BMJ 2020, 370, 2322. [Google Scholar] [CrossRef] [PubMed]
- Storz, M.A. Lifestyle Adjustments in Long-COVID Management: Potential Benefits of Plant-Based Diets. Curr. Nutr. Rep. 2021, 1, 1–12. [Google Scholar] [CrossRef]
- Kim, H.; Rebholz, C.M.; Hegde, S.; LaFiura, C.; Raghavan, M.; Lloyd, J.F.; Cheng, S.; Seidelmann, S.B. Plant-based diets, pescatarian diets and COVID-19 severity: A population-based case–control study in six countries. BMJ Nutr. Prev. Heal. 2021, 4. [Google Scholar] [CrossRef] [PubMed]
- Stancic, S.; Cullimore, J.; Barnard, N.D. Shoring Up Vaccine Efficacy. Am. J. Med. 2021. [Google Scholar] [CrossRef] [PubMed]
- Petersen, K.S.; Freeman, A.M.; Kris-Etherton, P.M.; Williams, K.A.W., Sr.; Reddy, K.R.; Aggarwal, M.; Barnard, N.D.; Ornish, D.; Esselstyn, C.B.E., Jr.; Allen, K.; et al. The Importance of a Healthy Lifestyle in the Era of COVID-19. Int. J. Dis. Reversal Prev. 2021, 3, 16. [Google Scholar] [CrossRef]
- United Nation. UN Task Forces Battle Misconceptions of Avian Flu, Mount Indonesian Campaign||UN News. Available online: https://news.un.org/en/story/2005/10/157792-un-task-forces-battle-misconceptions-avian-flu-mount-indonesian-campaign (accessed on 16 October 2021).
- Sakkas, H.; Bozidis, P.; Touzios, C.; Kolios, D.; Athanasiou, G.; Athanasopoulou, E.; Gerou, I.; Gartzonika, C. Nutritional Status and the Influence of the Vegan Diet on the Gut Microbiota and Human Health. Medicina 2020, 56, 88. [Google Scholar] [CrossRef] [PubMed]
- Bailey, P. What Does It Mean to Consumers? An Exploration into Diets around the World; Ipsos: Paris, France, 2018. [Google Scholar]
- Hargreaves, S.M.; Nakano, E.Y.; Zandonadi, R.P. Brazilian Vegetarian Population-Influence of Type of Diet, Motivation and Sociodemographic Variables on Quality of Life Measured by Specific Tool (VEGQOL). Nutrients 2020, 12, 1406. [Google Scholar] [CrossRef]
- Dyett, P.A.; Sabaté, J.; Haddad, E.; Rajaram, S.; Shavlik, D. Vegan lifestyle behaviors. An exploration of congruence with health-related beliefs and assessed health indices. Appetite 2013, 67, 119–124. [Google Scholar] [CrossRef]
- Radnitz, C.; Beezhold, B.; DiMatteo, J. Investigation of lifestyle choices of individuals following a vegan diet for health and ethical reasons. Appetite 2015, 90, 31–36. [Google Scholar] [CrossRef] [PubMed]
- Janssen, M.; Busch, C.; Rödiger, M.; Hamm, U. Motives of consumers following a vegan diet and their attitudes towards animal agriculture. Appetite 2016, 105, 643–651. [Google Scholar] [CrossRef] [PubMed]
- Pribis, P.; Pencak, R.C.; Grajales, T. Beliefs and attitudes toward vegetarian lifestyle across generations. Nutrients 2010, 2, 523–531. [Google Scholar] [CrossRef] [PubMed]
- Jakše, B.; Jakše, B.; Pinter, S.; Pajek, J.; Mis, N.F. Characteristics of Slovenian Adults in Community-Based Whole-Food Plant-Based Lifestyle Program. J. Nutr. Metab. 2020, 2020, 6950530. [Google Scholar] [CrossRef]
- Tso, R.; Forde, C.G. Unintended Consequences: Nutritional Impact and Potential Pitfalls of Switching from Animal- to Plant-Based Foods. Nutrients 2021, 13, 2527. [Google Scholar] [CrossRef]
- Davey, D.; Malone, S.; Egan, B. Case Study: Transition to a Vegan Diet in an Elite Male Gaelic Football Player. Sport 2021, 9, 6. [Google Scholar] [CrossRef] [PubMed]
- Van Vliet, S.; Burd, N.A.; van Loon, L.J.C. The skeletal muscle anabolic response to plant- versus animal-based protein consumption. J. Nutr. 2015, 145, 1981–1991. [Google Scholar] [CrossRef]
- Bailey, H.M.; Stein, H.H. Can the digestible indispensable amino acid score methodology decrease protein malnutrition. Anim. Front. 2019, 9, 18–23. [Google Scholar] [CrossRef]
- Chef’s Pencil Staff. Most Popular Countries and Cities for Vegans in 2020 (Jan-2021 Update)—Chef’s Pencil. Available online: https://www.chefspencil.com/most-popular-countries-and-cities-for-vegans-in-2020-jan-2021-update/ (accessed on 16 October 2021).
- Loh, H.C.; Hoo, F.K.; Kwan, J.N.; Lim, Y.F.; Looi, I. A Bibliometric Analysis of Global Trends in Vegan-Related Research. Int. J. Dis. Reversal Prev. 2021, 3, 12. [Google Scholar] [CrossRef]
- Melina, V.; Craig, W.; Levin, S. Position of the Academy of Nutrition and Dietetics: Vegetarian Diets. J. Acad. Nutr. Diet. 2016, 116, 1970–1980. [Google Scholar] [CrossRef]
- Agnoli, C.; Baroni, L.; Bertini, I.; Ciappellano, S.; Fabbri, A.; Papa, M.; Pellegrini, N.; Sbarbati, R.; Scarino, M.L.; Siani, V.; et al. Position paper on vegetarian diets from the working group of the Italian Society of Human Nutrition. Nutr. Metab. Cardiovasc. Dis. 2017, 27, 1037–1052. [Google Scholar] [CrossRef]
- British Dietetic Association. British Dietetic Association Confirms Well-Planned Vegan Diets can Support Healthy Living in People of All Ages; The Association of UK Dietitians: Birmingham, UK, 2017. [Google Scholar]
- Dietitians of Canada. What You Need to Know About Following a Vegan Eating Plan; Dietitians of Canada: Toronto, ON, Canada, 2020. [Google Scholar]
- National Health and Medical Council of Australia. Australian Dietary Guidelines; National Health and Medical Research Council: Canberra, Australia, 2013; ISBN 1864965754.
- Gomes, S.C.; João, S.; Pinho, P.; Borges, C.; Santos, C.T.; Santos, A.; Design, P.G. National Programme for the Promotion of Healthy Eating Guidelines for a Healthy Vegetarian Diet; National Programme for the Promotions of Healthy Eating: Lisboa, Portugal, 2015; ISBN 978-972-675-228-8. [Google Scholar]
- Anderson, L. U.S. Doctors Blast Belgian Misinformation on Vegan Diets; Physicians Committee for Responsible Medicine: Washington, DC, USA, 2019. [Google Scholar]
- National Institute of Public Health of Slovenia. Strokovno Mnenje Glede Vegetarijanstva in Kitajske Študije; National Institute of Public Health of Slovenia: Ljubljana, Slovenia, 2011. [Google Scholar]
- Richter, M.; Boeing, H.; Grünewald-Funk, D.; Heseker, H.; Kroke, A.; Leschik-Bonnet, E.; Oberritter, H.; Strohm, D.; Watzl, B. Vegane Ernährung Position der Deutschen Gesellschaft für Ernährung e. V. (DGE). Ernaehrungs Umschau 2016, 63, M262. [Google Scholar]
- Gorenc, A. Znanost nad Mite o Prehrani: Ni Dokazov, da bi bil Veganski način Prehranjevanja Bolj Zdrav; Slovenska Tiskovna Agencija—STAznanost: Ljubljana, Slovenia, 2021. [Google Scholar]
- Novljan, N.; Boštjančič, V. Res Sprejeti? Vegani, Dokumentarna Oddaja; Televizija Slovenija—RTVSLO.si.: Ljubljana, Slovenia, 2021. [Google Scholar]
- Zgonc, D. Prof. Dr. Tadej Battelino: Hlastanje po Zdravju je Tudi Nasilje! Available online: https://www.viva.si/Intervju/15623/prof-dr-Tadej-Battelino-Hlastanje-po-zdravju-je-tudi-nasilje (accessed on 10 December 2021).
- Zupan, Š. Zato Morajo Dojenčki in Otroci Jesti Meso. Available online: https://www.bibaleze.si/dojencek/prehrana-za-dojencke/vegetarijanska-prehrana-starsi-otroci-dojencek-otrok-vegetarijanci-vegani-meso-ribe-jajca-mleko.html (accessed on 10 December 2021).
- Lorenčič, M. Rok Orel: Človek je po Naravi Vsejeda Živalska Vrsta. Dnevnik. Available online: https://www.dnevnik.si/1042466254 (accessed on 11 December 2021).
- Kozjek Rotovnik, N. Nada Rotovnik Kozjek: Veganstvo ni za Vsakogar. Delo. Available online: https://www.delo.si/polet/nada-rotovnik-kozjek-veganstvo-ni-za-vsakogar/ (accessed on 11 December 2021).
- Dinu, M.; Abbate, R.; Gensini, G.F.; Casini, A.; Sofi, F. Vegetarian, vegan diets and multiple health outcomes: A systematic review with meta-analysis of observational studies. Crit. Rev. Food Sci. Nutr. 2017, 57, 3640–3649. [Google Scholar] [CrossRef]
- Hever, J.; Cronise, R.J. Plant-based nutrition for healthcare professionals: Implementing diet as a primary modality in the prevention and treatment of chronic disease. J. Geriatr. Cardiol. 2017, 14, 355–368. [Google Scholar] [PubMed]
- Tuso, P.; Ismail, M.H.; Ha, B.P.; Bartolotto, C. Nutritional Update for Physicians: Plant-Based Diets. Perm. J. 2013, 17, 61–66. [Google Scholar] [CrossRef] [PubMed]
- Hever, J. Plant-Based Diets: A Physician’s Guide. Perm. J. 2016, 20, 15–082. [Google Scholar] [CrossRef]
- Storz, M.A. What makes a plant-based diet? a review of current concepts and proposal for a standardized plant-based dietary intervention checklist. Eur. J. Clin. Nutr. 2021. [Google Scholar] [CrossRef]
- Robbins, R.; Quan, S.F.; Weaver, M.D.; Bormes, G.; Barger, L.K.; Czeisler, C.A. Examining sleep deficiency and disturbance and their risk for incident dementia and all-cause mortality in older adults across 5 years in the United States. Aging 2021, 13, 3254–3268. [Google Scholar] [CrossRef]
- Li, Y.; Schoufour, J.; Wang, D.D.; Dhana, K.; Pan, A.; Liu, X.; Song, M.; Liu, G.; Shin, H.J.; Sun, Q.; et al. Healthy lifestyle and life expectancy free of cancer, cardiovascular disease, and type 2 diabetes: Prospective cohort study. BMJ 2020, 368, I6669. [Google Scholar] [CrossRef]
- Rezende, L.F.M.; Sá, T.H.; Mielke, G.I.; Viscondi, J.Y.K.; Rey-López, J.P.; Garcia, L.M.T. All-Cause Mortality Attributable to Sitting Time. Am. J. Prev. Med. 2016, 51, 253–263. [Google Scholar] [CrossRef]
- Finucane, M.M.; Stevens, G.A.; Cowan, M.J.; Danaei, G.; Lin, J.K.; Paciorek, C.J.; Singh, G.M.; Gutierrez, H.R.; Lu, Y.; Bahalim, A.N.; et al. National, regional, and global trends in body-mass index since 1980: Systematic analysis of health examination surveys and epidemiological studies with 960 country-years and 9·1 million participants. Lancet 2011, 377, 557–567. [Google Scholar] [CrossRef]
- Bentham, J.; Di Cesare, M.; Bilano, V.; Bixby, H.; Zhou, B.; Stevens, G.A.; Riley, L.M.; Taddei, C.; Hajifathalian, K.; Lu, Y.; et al. Worldwide trends in body-mass index, underweight, overweight, and obesity from 1975 to 2016: A pooled analysis of 2416 population-based measurement studies in 128·9 million children, adolescents, and adults. Lancet 2017, 390, 2627–2642. [Google Scholar]
- Ng, M.; Fleming, T.; Robinson, M.; Thomson, B.; Graetz, N.; Margono, C.; Mullany, E.C.; Biryukov, S.; Abbafati, C.; Abera, S.F.; et al. Global, regional, and national prevalence of overweight and obesity in children and adults during 1980–2013: A systematic analysis for the Global Burden of Disease Study 2013. Lancet 2014, 384, 766–781. [Google Scholar] [CrossRef]
- Leyden, E.; Hanson, P.; Halder, L.; Rout, L.; Cherry, I.; Shuttlewood, E.; Poole, D.; Loveder, M.; Abraham, J.; Kyrou, I.; et al. Older age does not influence the success of weight loss through the implementation of lifestyle modification. Clin. Endocrinol. 2020, 94, 204–209. [Google Scholar] [CrossRef]
- Li, Z.; Heber, D. Sarcopenic obesity in the elderly and strategies for weight management. Nutr. Rev. 2012, 70, 57–64. [Google Scholar] [CrossRef] [PubMed]
- Cava, E.; Yeat, N.C.; Mittendorfer, B. Preserving Healthy Muscle during Weight Loss. Adv. Nutr. Int. Rev. J. 2017, 8, 511–519. [Google Scholar] [CrossRef] [PubMed]
- Roh, E.; Choi, K.M. Health Consequences of Sarcopenic Obesity: A Narrative Review. Front. Endocrinol. 2020, 11, 332. [Google Scholar] [CrossRef]
- Polyzos, S.A.; Margioris, A.N. Sarcopenic obesity. Hormones 2018, 17, 321–331. [Google Scholar] [CrossRef] [PubMed]
- Seljak, B.K.; Valenčič, E.; Hristov, H.; Hribar, M.; Lavriša, Ž.; Kušar, A.; Žmitek, K.; Krušič, S.; Gregorič, M.; Blaznik, U.; et al. Inadequate Intake of Dietary Fibre in Adolescents, Adults, and Elderlies: Results of Slovenian Representative SI. Menu Study. Nutrients 2021, 13, 3826. [Google Scholar] [CrossRef] [PubMed]
- Gregorič, M.; Blaznik, U.; Turk, V.F.; Delfar, N.; Korošec, A.; Lavtar, D.; Zaletel, M.; Seljak, B.K.; Golja, P.; Kotnik, K.Z.; et al. Različni Vidiki Prehranjevanja Prebivalcev Slovenije (v Starosti od 3 Mesecev do 74 let); Nacionalni Inštitut za Javno Zdravje: Ljubljana, Slovenia, 2020; ISBN 978-961-6945-03-5. [Google Scholar]
- Wright, N.; Wilson, L.; Smith, M.; Duncan, B.; McHugh, P. The BROAD study: A randomised controlled trial using a whole food plant-based diet in the community for obesity, ischaemic heart disease or diabetes. Nutr. Diabetes 2017, 7, e256. [Google Scholar] [CrossRef]
- Mishra, S.; Xu, J.; Agarwal, U.; Gonzales, J.; Levin, S.; Barnard, N.D. A multicenter randomized controlled trial of a plant-based nutrition program to reduce body weight and cardiovascular risk in the corporate setting: The GEICO study. Eur. J. Clin. Nutr. 2013, 67, 718–724. [Google Scholar] [CrossRef]
- Tran, E.; Dale, H.F.; Jensen, C.; Lied, G.A. Effects of Plant-Based Diets on Weight Status: A Systematic Review. Diabetes Metab. Syndr. Obes. Targets Ther. 2020, 13, 3433–3448. [Google Scholar] [CrossRef]
- Jakše, B.; Pinter, S.; Jakše, B.; Bučar Pajek, M.; Pajek, J. Effects of an Ad Libitum Consumed Low-Fat Plant-Based Diet Supplemented with Plant-Based Meal Replacements on Body Composition Indices. Biomed Res. Int. 2017, 2017, 9626390. [Google Scholar] [CrossRef]
- Barnard, N.D.; Alwarith, J.; Rembert, E.; Brandon, L.; Nguyen, M.; Goergen, A.; Horne, T.; do Nascimento, G.F.; Lakkadi, K.; Tura, A.; et al. A Mediterranean Diet and Low-Fat Vegan Diet to Improve Body Weight and Cardiometabolic Risk Factors: A Randomized, Cross-over Trial. J. Am. Coll. Nutr. 2021, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Barnard, N.D.; Rembert, E.; Freeman, A.; Bradshaw, M.; Holubkov, R.; Kahleova, H. Blood Type Is Not Associated with Changes in Cardiometabolic Outcomes in Response to a Plant-Based Dietary Intervention. J. Acad. Nutr. Diet. 2020, 121, 1080–1086. [Google Scholar] [CrossRef] [PubMed]
- Kent, L.; Morton, D.; Hurlow, T.; Rankin, P.; Hanna, A.; Diehl, H. Long-term effectiveness of the community-based Complete Health Improvement Program (CHIP) lifestyle intervention: A cohort study. BMJ Open 2013, 3, e003751. [Google Scholar] [CrossRef]
- Benatar, J.R.; Stewart, R.A.H. Cardiometabolic risk factors in vegans; A meta-analysis of observational studies. PLoS ONE 2018, 13, e0209086. [Google Scholar] [CrossRef] [PubMed]
- Schick, A.; Boring, J.; Courville, A.; Gallagher, I.; Guo, J.; Howard, R.; Milley, L.; Raisinger, K.; Rozga, I.; Stagliano, M.; et al. Effects of Ad Libitum Low Carbohydrate Versus Low Fat Diets on Body Weight and Fat Mass. Curr. Dev. Nutr. 2020, 4, 658. [Google Scholar] [CrossRef]
- Koertge, J.; Weidner, G.; Elliott-Eller, M.; Scherwitz, L.; Merritt-Worden, T.A.; Marlin, R.; Lipsenthal, L.; Guarneri, M.; Finkel, R.; Saunders, D.E.; et al. Improvement in medical risk factors and quality of life in women and men with coronary artery disease in the Multicenter Lifestyle Demonstration Project. Am. J. Cardiol. 2003, 91, 1316–1322. [Google Scholar] [CrossRef]
- Nugent, S.J.; Rogerson, D.; Ranchordas, M.K.; Broom, D.R. Vegan diet for adults with overweight or obesity. Cochrane Database Syst. Rev. 2020, 19. [Google Scholar] [CrossRef]
- Kahleova, H.; Petersen, K.F.; Shulman, G.I.; Alwarith, J.; Rembert, E.; Tura, A.; Hill, M.; Holubkov, R.; Barnard, N.D. Effect of a Low-Fat Vegan Diet on Body Weight, Insulin Sensitivity, Postprandial Metabolism, and Intramyocellular and Hepatocellular Lipid Levels in Overweight Adults. JAMA Netw. Open 2020, 3, e2025454. [Google Scholar] [CrossRef] [PubMed]
- Jakše, B.; Jakše, B.; Pajek, J.; Pajek, M. Effects of ad libitum consumed, low-fat, high-fiber plant-based diet supplemented with plant-based meal replacements on cardiovascular risk factors. Food Nutr. Res. 2019, 63. [Google Scholar] [CrossRef]
- Jakše, B.; Jakše, B.; Pinter, S.; Pajek, J.; Fidler Mis, N. Whole-Food Plant-Based Lifestyle Program and Decreased Obesity. Am. J. Lifestyle Med. 2020, 155982762094920. [Google Scholar] [CrossRef]
- Losasso, C.; Eckert, E.M.; Mastrorilli, E.; Villiger, J.; Mancin, M.; Patuzzi, I.; Di Cesare, A.; Cibin, V.; Barrucci, F.; Pernthaler, J.; et al. Assessing the Influence of Vegan, Vegetarian and Omnivore Oriented Westernized Dietary Styles on Human Gut Microbiota: A Cross Sectional Study. Front. Microbiol. 2018, 9, 317. [Google Scholar] [CrossRef]
- Jakše, B.; Jakše, B.; Godnov, U.; Pinter, S. Nutritional, Cardiovascular Health and Lifestyle Status of ‘Health Conscious’ Adult Vegans and Non-Vegans from Slovenia: A Cross-Sectional Self-Reported Survey. Int. J. Environ. Res. Public Health 2021, 18, 5968. [Google Scholar] [CrossRef] [PubMed]
- Kahleova, H.; Rembert, E.; Alwarith, J.; Yonas, W.N.; Tura, A.; Holubkov, R.; Agnello, M.; Chutkan, R.; Barnard, N.D. Effects of a Low-Fat Vegan Diet on Gut Microbiota in Overweight Individuals and Relationships with Body Weight, Body Composition, and Insulin Sensitivity. A Randomized Clinical Trial. Nutrients 2020, 12, 2917. [Google Scholar] [CrossRef]
- Hall, K.D.; Guo, J.; Courville, A.B.; Boring, J.; Brychta, R.; Chen, K.Y.; Darcey, V.; Forde, C.G.; Gharib, A.M.; Gallagher, I.; et al. Effect of a plant-based, low-fat diet versus an animal-based, ketogenic diet on ad libitum energy intake. Nat. Med. 2021, 27, 344–353. [Google Scholar] [CrossRef]
- Stiegler, P.; Cunliffe, A. The role of diet and exercise for the maintenance of fat-free mass and resting metabolic rate during weight loss. Sports Med. 2006, 36, 239–262. [Google Scholar] [CrossRef] [PubMed]
- Odegaard, A.O.; Manson, J.E. Weight and mortality: Why body composition matters. Am. J. Clin. Nutr. 2021, nqaa409. [Google Scholar] [CrossRef]
- Bouzas, C.; Bibiloni, M.D.M.; Tur, J.A. Relationship between body image and body weight control in overweight ≥55-year-old adults: A systematic review. Int. J. Environ. Res. Public Health 2019, 16, 1622. [Google Scholar] [CrossRef]
- Hausenblas, H.A.; Fallon, E.A. Exercise and body image: A meta-analysis. Psychol. Heal. 2006, 21, 33–47. [Google Scholar] [CrossRef]
- Grannell, A.; De Vito, G.; Murphy, J.C.; le Roux, C.W. The influence of skeletal muscle on appetite regulation. Expert Rev. Endocrinol. Metab. 2019, 14, 267–282. [Google Scholar] [CrossRef] [PubMed]
- Hall, K.D.; Kahan, S. Maintenance of Lost Weight and Long-Term Management of Obesity. Med. Clin. N. Am. 2018, 102, 183–197. [Google Scholar] [CrossRef]
- Turicchi, J.; O’Driscoll, R.; Finlayson, G.; Duarte, C.; Hopkins, M.; Martins, N.; Michalowska, J.; Larsen, T.M.; Van Baak, M.A.; Astrup, A.; et al. Associations between the proportion of fat-free mass loss during weight loss, changes in appetite, and subsequent weight change: Results from a randomized 2-stage dietary intervention trial. Am. J. Clin. Nutr. 2020, 111, 536–544. [Google Scholar] [CrossRef] [PubMed]
- Dwyer-Lindgren, L.; Freedman, G.; Engell, R.E.; Fleming, T.D.; Lim, S.S.; Murray, C.J.; Mokdad, A.H. Prevalence of physical activity and obesity in US counties, 2001–2011: A road map for action. Popul. Health Metr. 2013, 11, 7. [Google Scholar] [CrossRef]
- Samitz, G.; Egger, M.; Zwahlen, M. Domains of physical activity and all-cause mortality: Systematic review and dose-response meta-analysis of cohort studies. Int. J. Epidemiol. 2011, 40, 1382–1400. [Google Scholar] [CrossRef]
- Johns, D.J.; Hartmann-Boyce, J.; Jebb, S.A.; Aveyard, P. Diet or Exercise Interventions vs Combined Behavioral Weight Management Programs: A Systematic Review and Meta-Analysis of Direct Comparisons. J. Acad. Nutr. Diet. 2014, 114, 1557–1568. [Google Scholar] [CrossRef]
- Shaw, K.A.; Gennat, H.C.; O’Rourke, P.; Del Mar, C. Exercise for overweight or obesity. Cochrane Database Syst. Rev. 2006, CD003817. [Google Scholar] [CrossRef]
- Bull, F.C.; Al-Ansari, S.S.; Biddle, S.; Borodulin, K.; Buman, M.P.; Cardon, G.; Carty, C.; Chaput, J.P.; Chastin, S.; Chou, R.; et al. World Health Organization 2020 guidelines on physical activity and sedentary behaviour. Br. J. Sports Med. 2020, 54, 1451–1462. [Google Scholar] [CrossRef]
- Roth, G.A.; Johnson, C.; Abajobir, A.; Abd-Allah, F.; Abera, S.F.; Abyu, G.; Ahmed, M.; Aksut, B.; Alam, T.; Alam, K.; et al. Global, Regional, and National Burden of Cardiovascular Diseases for 10 Causes, 1990 to 2015. J. Am. Coll. Cardiol. 2017, 70, 1–25. [Google Scholar] [CrossRef]
- Meier, T.; Gräfe, K.; Senn, F.; Sur, P.; Stangl, G.I.; Dawczynski, C.; März, W.; Kleber, M.E.; Lorkowski, S. Cardiovascular mortality attributable to dietary risk factors in 51 countries in the WHO European Region from 1990 to 2016: A systematic analysis of the Global Burden of Disease Study. Eur. J. Epidemiol. 2019, 34, 37–55. [Google Scholar] [CrossRef] [PubMed]
- American Diabetes Association 8. Cardiovascular Disease and Risk Management. Diabetes Care 2015, 38, S49–S57. [Google Scholar] [CrossRef]
- Flora, G.D.; Nayak, M.K. A Brief Review of Cardiovascular Diseases, Associated Risk Factors and Current Treatment Regimes. Curr. Pharm. Des. 2019, 25, 4063–4084. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Hu, G. Dietary Pattern, Lifestyle Factors, and Cardiovascular Diseases. Curr. Nutr. Rep. 2012, 1, 64–72. [Google Scholar] [CrossRef][Green Version]
- Piepoli, M.F.; Hoes, A.W.; Agewall, S.; Albus, C.; Brotons, C.; Catapano, A.L.; Cooney, M.-T.; Corrà, U.; Cosyns, B.; Deaton, C.; et al. 2016 European Guidelines on cardiovascular disease prevention in clinical practice. Eur. Heart J. 2016, 37, 2315–2381. [Google Scholar] [CrossRef]
- Murray, C.J.L.; Abraham, J.; Ali, M.K.; Alvarado, M.; Atkinson, C.; Baddour, L.M.; Bartels, D.H.; Benjamin, E.J.; Bhalla, K.; Birbeck, G.; et al. The State of US health, 1990-2010: Burden of diseases, injuries, and risk factors. JAMA 2013, 310, 591–608. [Google Scholar] [CrossRef]
- National Institute of Public Health of the Republic of Slovenia. Nacionalni Program Primarne Preventive Srčno-Žilnih Bolezni; National Institute of Public Health of the Republic of Slovenia: Ljubljana, Slovenia, 2006. [Google Scholar]
- National Institute of Public Health of the Republic of Slovenia. 17. maj: Svetovni dan Hipertenzije; National Institute of Public Health: Ljubljana, Slovenia, 2017. [Google Scholar]
- Petek Šter, M.; Bulc, M.; Accetto, R.; Petek, D.; Salobir, B.; Žontar, T. Združenje za Arterijsko Hipertenzijo—Slovensko Zdravniško Društvo. In Proceedings of the Protokol Vodenja Arterijske Hipertenzije v Ambulanti Družinske Medicine; Dolenc, P., Ed.; Slovensko Zdravniško Društvo. Sekcija za Hipertenzijo: Ljubljana, Slovenia, 2011; pp. 63–80. [Google Scholar]
- Chareonrungrueangchai, K.; Wongkawinwoot, K.; Anothaisintawee, T.; Reutrakul, S. Dietary factors and risks of cardiovascular diseases: An umbrella review. Nutrients 2020, 12, 1088. [Google Scholar] [CrossRef]
- Kahleova, H.; Levin, S.; Barnard, N.D. Vegetarian Dietary Patterns and Cardiovascular Disease. Prog. Cardiovasc. Dis. 2018, 61, 54–61. [Google Scholar] [CrossRef] [PubMed]
- Jakše, B.; Jakše, B.; Pinter, S.; Jug, B.; Godnov, U.; Pajek, J.; Mis, N.F. Dietary Intakes and Cardiovascular Health of Healthy Adults in Short-, Medium-, and Long-Term Whole-Food Plant-Based Lifestyle Program. Nutrients 2019, 12, 55. [Google Scholar] [CrossRef]
- Ornish, D.; Scherwitz, L.W.; Billings, J.H.; Brown, S.E.; Gould, K.L.; Merritt, T.A.; Sparler, S.; Armstrong, W.T.; Ports, T.A.; Kirkeeide, R.L.; et al. Intensive lifestyle changes for reversal of coronary heart disease. JAMA 1998, 280, 2001–2007. [Google Scholar] [CrossRef] [PubMed]
- Esselstyn, C.B.; Gendy, G.; Doyle, J.; Golubic, M.; Roizen, M.F. A way to reverse CAD? J. Fam. Pract. 2014, 63, 356–364. [Google Scholar]
- Esselstyn, C.B. Updating a 12-year experience with arrest and reversal therapy for coronary heart disease (an overdue requiem for palliative cardiology). Am. J. Cardiol. 1999, 84, 339–341. [Google Scholar] [CrossRef]
- Esselstyn, C.B.; Ellis, S.G.; Edendorp, S.V.M.; Crowe, T.D. A Strategy to Arrest and Reverse Coronary Artery Disease: A 5-Year Longitudinal Study of a Single Physician’s Practice. J. Fam. Pract. 1995, 41, 560–568. [Google Scholar] [PubMed]
- Silberman, A.; Banthia, R.; Estay, I.S.; Kemp, C.; Studley, J.; Hareras, D.; Ornish, D. The effectiveness and efficacy of an intensive cardiac rehabilitation program in 24 sites. Am. J. Health Promot. 2010, 24, 260–266. [Google Scholar] [CrossRef]
- Dovč, A.; Mlinšek, G.; Arnol, M.; Oblak, M.; Jakše, B.; Pajek, J. Nutrition intervention for managing dyslipidemia in kidney transplant recipients: Preliminary results of a clinical trial. In Proceedings of the Book of Abstracts: 7th Slovenian Congress of Nephrology, Virtual Congress, 11–14 March 2021; p. 141. [Google Scholar]
- Kahleova, H.; Levin, S.; Barnard, N. Cardio-Metabolic Benefits of Plant-Based Diets. Nutrients 2017, 9, 848. [Google Scholar] [CrossRef] [PubMed]
- Lee, K.W.; Loh, H.C.; Ching, S.M.; Devaraj, N.K.; Hoo, F.K. Effects of Vegetarian Diets on Blood Pressure Lowering: A Systematic Review with Meta-Analysis and Trial Sequential Analysis. Nutrients 2020, 12, 1604. [Google Scholar] [CrossRef]
- Yokoyama, Y.; Nishimura, K.; Barnard, N.D.; Takegami, M.; Watanabe, M.; Sekikawa, A.; Okamura, T.; Miyamoto, Y. Vegetarian Diets and Blood Pressure. JAMA Intern. Med. 2014, 174, 577. [Google Scholar] [CrossRef] [PubMed]
- Yokoyama, Y.; Levin, S.M.; Barnard, N.D. Association between plant-based diets and plasma lipids: A systematic review and meta-analysis. Nutr. Rev. 2017, 75, 683–698. [Google Scholar] [CrossRef]
- Ornish, D.; Brown, S.E.; Billings, J.H.; Scherwitz, L.W.; Armstrong, W.T.; Ports, T.A.; McLanahan, S.M.; Kirkeeide, R.L.; Gould, K.L.; Brand, R.J. Can lifestyle changes reverse coronary heart disease? The Lifestyle Heart Trial. Lancet 1990, 336, 129–133. [Google Scholar] [CrossRef]
- International Diabetes Federation Facts & Figures. Available online: https://idf.org/aboutdiabetes/what-is-diabetes/facts-figures.html (accessed on 13 March 2021).
- National Institute of Public Health of Slovenia Sladkorna bolezen v Sloveniji: Kje smo in Kam Gremo? Available online: https://www.nijz.si/sl/sladkorna-bolezen-v-sloveniji-kje-smo-in-kam-gremo (accessed on 13 March 2021).
- National Institute of Public Health Of Slovenia 14. November 2020—Svetovni dan Sladkorne Bolezni. Available online: https://www.nijz.si/sl/14-november-2020-svetovni-dan-sladkorne-bolezni (accessed on 17 October 2021).
- Kelly, J.; Karlsen, M.; Steinke, G. Type 2 Diabetes Remission and Lifestyle Medicine: A Position Statement From the American College of Lifestyle Medicine. Am. J. Lifestyle Med. 2020, 14, 406–419. [Google Scholar] [CrossRef]
- Barnard, N.D.; Cohen, J.; Jenkins, D.J.A.; Turner-McGrievy, G.; Gloede, L.; Green, A.; Ferdowsian, H. A low-fat vegan diet and a conventional diabetes diet in the treatment of type 2 diabetes: A randomized, controlled, 74-wk clinical trial. Am. J. Clin. Nutr. 2009, 89, 1588S–1596S. [Google Scholar] [CrossRef] [PubMed]
- Anderson, J.W.; Ward, K. High-carbohydrate, high-fiber diets for insulin-treated men with diabetes mellitus. Am. J. Clin. Nutr. 1979, 32, 2312–2321. [Google Scholar] [CrossRef] [PubMed]
- Dunaief, D.M.; Fuhrman, J.; Dunaief, J.L.; Ying, G. Glycemic and cardiovascular parameters improved in type 2 diabetes with the high nutrient density (HND) diet. Open J. Prev. Med. 2012, 02, 364–371. [Google Scholar] [CrossRef]
- Pischke, C.R.; Weidner, G.; Elliott-Eller, M.; Scherwitz, L.; Merritt-Worden, T.A.; Marlin, R.; Lipsenthal, L.; Finkel, R.; Saunders, D.; McCormac, P.; et al. Comparison of Coronary Risk Factors and Quality of Life in Coronary Artery Disease Patients with Versus without Diabetes Mellitus. Am. J. Cardiol. 2006, 97, 1267–1273. [Google Scholar] [CrossRef]
- Kahleova, H.; Tura, A.; Hill, M.; Holubkov, R.; Barnard, N. A Plant-Based Dietary Intervention Improves Beta-Cell Function and Insulin Resistance in Overweight Adults: A 16-Week Randomized Clinical Trial. Nutrients 2018, 10, 189. [Google Scholar] [CrossRef]
- Sarver, J.; Khambatta, C.; Barbaro, R.; Chavan, B.; Drozek, D. Retrospective Evaluation of an Online Diabetes Health Coaching Program: A Pilot Study. Am. J. Lifestyle Med. 2019, 15, 466–474. [Google Scholar] [CrossRef]
- Rinaldi, S.; Campbell, E.E.; Fournier, J.; O’Connor, C.; Madill, J. A Comprehensive Review of the Literature Supporting Recommendations From the Canadian Diabetes Association for the Use of a Plant-Based Diet for Management of Type 2 Diabetes. Can. J. Diabetes 2016, 40, 471–477. [Google Scholar] [CrossRef]
- Barnard, N.D.; Katcher, H.I.; Jenkins, D.J.A.; Cohen, J.; Turner-McGrievy, G. Vegetarian and vegan diets in type 2 diabetes management. Nutr. Rev. 2009, 67, 255–263. [Google Scholar] [CrossRef]
- Toumpanakis, A.; Turnbull, T.; Alba-Barba, I. Effectiveness of plant-based diets in promoting well-being in the management of type 2 diabetes: A systematic review. BMJ Open Diabetes Res. Care 2018, 6, e000534. [Google Scholar] [CrossRef] [PubMed]
- Barnard, N.D.; Scialli, A.R.; Hurlock, D.; Bertron, P. Diet and sex-hormone binding globulin, dysmenorrhea, and premenstrual symptoms. Obstet. Gynecol. 2000, 95, 245–250. [Google Scholar]
- Ornish, D.; Weidner, G.; Fair, W.R.; Marlin, R.; Pettengill, E.B.; Raisin, C.J.; Dunn-Emke, S.; Crutchfield, L.; Jacobs, F.N.; Barnard, R.J.; et al. Intensive lifestyle changes may affect the progression of prostate cancer. J. Urol. 2005, 174, 1065–1070. [Google Scholar] [CrossRef] [PubMed]
- Beezhold, B.; Radnitz, C.; Rinne, A.; Di Matteo, J. Vegans report less stress and anxiety than omnivores. Nutr. Neurosci. 2015, 18, 289–296. [Google Scholar] [CrossRef]
- Kahleova, H.; McCann, J.; Alwarith, J.; Rembert, E.; Tura, A.; Holubkov, R.; Barnard, N.D. A plant-based diet in overweight adults in a 16-week randomized clinical trial: The role of dietary acid load. Clin. Nutr. ESPEN 2021, 44, 150–158. [Google Scholar] [CrossRef]
- Barnard, N.D.; Kahleova, H.; Holtz, D.N.; del Aguila, F.; Neola, M.; Crosby, L.M.; Holubkov, R. The Women’s Study for the Alleviation of Vasomotor Symptoms (WAVS): A randomized, controlled trial of a plant-based diet and whole soybeans for postmenopausal women. Menopause 2021, 28, 1150–1156. [Google Scholar] [CrossRef] [PubMed]
- Bunner, A.E.; Agarwal, U.; Gonzales, J.F.; Valente, F.; Barnard, N.D. Nutrition intervention for migraine: A randomized crossover trial. J. Headache Pain 2014, 15, 69. [Google Scholar] [CrossRef]
- Goldner, B. Six Week Raw Vegan Nutrition Protocol Rapidly Reverses Lupus Nephritis: A Case Series. Int. J. Dis. Reversal Prev. 2019, 1, 11. [Google Scholar] [CrossRef]
- Campbell, T.M.; Liebman, S.E. Plant-based dietary approach to stage 3 chronic kidney disease with hyperphosphataemia. BMJ Case Rep. 2019, 12, 232080. [Google Scholar] [CrossRef]
- Chiarioni, G.; Popa, S.L.; Dalbeni, A.; Senore, C.; Leucuta, D.C.; Baroni, L.; Fantin, A. Vegan Diet Advice Might Benefit Liver Enzymes in Nonalcoholic Fatty Liver Disease: An Open Observational Pilot Study. J. Gastrointest. Liver Dis. 2021, 30, 81–87. [Google Scholar] [CrossRef] [PubMed]
- McDougall, J.; Bruce, B.; Spiller, G.; Westerdahl, J.; McDougall, M. Effects of a very low-fat, vegan diet in subjects with rheumatoid arthritis. J. Altern. Complement. Med. 2002, 8, 71–75. [Google Scholar] [CrossRef]
- Fuhrman, J.H.; Ferreri, D.M. Treatment and Remission of Symptoms in Type 1 Diabetes with a Nutrient-Dense, Plant-Rich (NDPR) Diet: Case Studies. Int. J. Dis. Reversal Prev. 2019, 1, 13. [Google Scholar] [CrossRef]
- Goldhamer, A.C.; Klaper, M.; Foorohar, A.; Myers, T.R. Water-only fasting and an exclusively plant foods diet in the management of. BMJ Case Rep. 2015, 2015, bcr2015211582. [Google Scholar] [CrossRef]
- Anderson, J.W.; Zeigler, J.A.; Deakins, D.A.; Floore, T.L.; Dillon, D.W.; Wood, C.L.; Oeltgen, P.R.; Whitley, R.J. Metabolic effects of high-carbohydrate, high-fiber diets for insulin-dependent diabetic individuals. Am. J. Clin. Nutr. 1991, 54, 936–943. [Google Scholar] [CrossRef]
- Giem, P.; Beeson, W.L.; Fraser, G.E. The incidence of dementia and intake of animal products: Preliminary findings from the Adventist Health Study. Neuroepidemiology 1993, 12, 28–36. [Google Scholar] [CrossRef] [PubMed]
- Wirnitzer, K.C. Vegan Diet in Sports and Exercise—Health Benefits and Advantages to Athletes and Physically Active People: A Narrative Review. Int. J. Sport. Exerc. Med. 2020, 6, 166. [Google Scholar]
- Longo, U.G.; Spiezia, F.; Maffulli, N.; Denaro, V. The Best Athletes in Ancient Rome were Vegetarian! J. Sports Sci. Med. 2008, 7, 565. [Google Scholar] [PubMed]
- Nebl, J.; Haufe, S.; Eigendorf, J.; Wasserfurth, P.; Tegtbur, U.; Hahn, A. Exercise capacity of vegan, lacto-ovo-vegetarian and omnivorous recreational runners. J. Int. Soc. Sports Nutr. 2019, 16, 23. [Google Scholar] [CrossRef] [PubMed]
- Hevia-Larraín, V.; Gualano, B.; Longobardi, I.; Gil, S.; Fernandes, A.L.; Costa, L.A.R.; Pereira, R.M.R.; Artioli, G.G.; Phillips, S.M.; Roschel, H. High-Protein Plant-Based Diet Versus a Protein-Matched Omnivorous Diet to Support Resistance Training Adaptations: A Comparison Between Habitual Vegans and Omnivores. Sports Med. 2021, 51, 1317–1330. [Google Scholar] [CrossRef]
- Król, W.; Price, S.; Sliz, D.; Parol, D.; Konopka, M.; Mamcarz, A.; Welnicki, M.; Braksator, W. A Vegan Athlete’s Heart-Is It Different? Morphology and Function in Echocardiography. Diagnostics 2020, 10, 477. [Google Scholar] [CrossRef]
- Lynch, H.; Johnston, C.; Wharton, C. Plant-Based Diets: Considerations for Environmental Impact, Protein Quality, and Exercise Performance. Nutrients 2018, 10, 1841. [Google Scholar] [CrossRef]
- Boutros, G.H.; Landry-Duval, M.A.; Garzon, M.; Karelis, A.D. Is a vegan diet detrimental to endurance and muscle strength? Eur. J. Clin. Nutr. 2020, 74, 1550–1555. [Google Scholar] [CrossRef]
- Wirnitzer, K.; Boldt, P.; Lechleitner, C.; Wirnitzer, G.; Leitzmann, C.; Rosemann, T.; Knechtle, B. Health status of female and male vegetarian and vegan endurance runners compared to omnivores—Results from the NURMI study (Step 2). Nutrients 2019, 11, 29. [Google Scholar] [CrossRef]
- Monteyne, A.J.; Dunlop, M.V.; Machin, D.J.; Coelho, M.O.C.; Pavis, G.F.; Porter, C.; Murton, A.J.; Abdelrahman, D.R.; Dirks, M.L.; Stephens, F.B.; et al. A mycoprotein based high-protein vegan diet supports equivalent daily myofibrillar protein synthesis rates compared with an isonitrogenous omnivorous diet in older adults: A randomized controlled trial. Br. J. Nutr. 2020, 126, 674–684. [Google Scholar] [CrossRef]
- Messina, M.J.; Lynch, H.; Dickinson, J.M.; Reed, K.E. No Difference Between the Effects of Supplementing with Soy Protein Versus Animal Protein on Gains in Muscle Mass and Strength in Response to Resistance Exercise. Int. J. Sport Nutr. Exerc. Metab. 2018, 28, 674–685. [Google Scholar] [CrossRef]
- Hernández-Martínez, C.; Fernández-Rodríguez, L.; Soriano, M.A.; Martínez-Sanz, J.M. Case Study: Body Composition Changes Resulting from a Nutritional Intervention on a Professional Vegan Powerlifter. Appl. Sci. 2020, 10, 8675. [Google Scholar] [CrossRef]
- Rogerson, D. Vegan diets: Practical advice for athletes and exercisers. J. Int. Soc. Sports Nutr. 2017, 14, 36. [Google Scholar] [CrossRef]
- Kaviani, M.; Shaw, K.; Chilibeck, P.D. Benefits of Creatine Supplementation for Vegetarians Compared to Omnivorous Athletes: A Systematic Review. Int. J. Environ. Res. Public Health 2020, 17, 3041. [Google Scholar] [CrossRef] [PubMed]
- Great Vegan Athletes All Athletes. Available online: https://www.greatveganathletes.com/all-athletes/ (accessed on 18 March 2021).
- Bivi, D.; Di Chio, T.; Geri, F.; Morganti, R.; Goggi, S.; Baroni, L.; Mumolo, M.G.; de Bortoli, N.; Peroni, D.G.; Marchi, S.; et al. Raising Children on a Vegan Diet: Parents’ Opinion on Problems in Everyday Life. Nutrients 2021, 13, 1796. [Google Scholar] [CrossRef] [PubMed]
- Orel, R.; Sedmak, M.; Fidler Mis, N. Vegetarijanska prehrana pri otrocih-praktična navodila. Zdrav. Vestn. 2014, 83, 169–181. [Google Scholar]
- Fewtrell, M.; Bronsky, J.; Campoy, C.; Domellöf, M.; Embleton, N.; Fidler Mis, N.; Hojsak, I.; Hulst, J.M.; Indrio, F.; Lapillonne, A.; et al. Complementary Feeding: A Position Paper by the European Society for Paediatric Gastroenterology, Hepatology, and Nutrition (ESPGHAN) Committee on Nutrition. J. Pediatr. Gastroenterol. Nutr. 2017, 64, 119–132. [Google Scholar] [CrossRef]
- Merritt, R.J.; Fleet, S.E.; Fifi, A.; Jump, C.; Schwartz, S.; Sentongo, T.; Duro, D.; Rudolph, J.; Turner, J. North American Society for Pediatric Gastroenterology, Hepatology, and Nutrition Position Paper: Plant-based Milks. J. Pediatr. Gastroenterol. Nutr. 2020, 71, 276–281. [Google Scholar] [CrossRef] [PubMed]
- De Cosmi, V.; Scaglioni, S.; Agostoni, C. Early taste experiences and later food choices. Nutrients 2017, 9, 107. [Google Scholar] [CrossRef]
- Waterland, R.A.; Garza, C. Potential mechanisms of metabolic imprinting that lead to chronic disease. Am. J. Clin. Nutr. 1999, 69, 179–197. [Google Scholar] [CrossRef] [PubMed]
- Mangels, A.R.; Messina, V. Considerations in planning vegan diets: Infants. J. Am. Diet. Assoc. 2001, 101, 670–677. [Google Scholar] [CrossRef]
- Mahase, E. What does the evidence say about vegan diets in children? BMJ 2021, 375, n2792. [Google Scholar] [CrossRef]
- Baroni, L.; Goggi, S.; Battaglino, R.; Berveglieri, M.; Fasan, I.; Filippin, D.; Griffith, P.; Rizzo, G.; Tomasini, C.; Tosatti, M.; et al. Vegan Nutrition for Mothers and Children: Practical Tools for Healthcare Providers. Nutrients 2018, 11, 5. [Google Scholar] [CrossRef]
- Sebastiani, G.; Barbero, A.H.; Borrás-Novel, C.; Casanova, M.A.; Aldecoa-Bilbao, V.; Andreu-Fernández, V.; Tutusaus, M.P.; Martínez, S.F.; Roig, M.D.G.; García-Algar, O. The effects of vegetarian and vegan diet during pregnancy on the health of mothers and offspring. Nutrients 2019, 11, 557. [Google Scholar] [CrossRef]
- Sutter, D.O.; Bender, N. Nutrient status and growth in vegan children. Nutr. Res. 2021, 91, 13–25. [Google Scholar] [CrossRef]
- Tran, B.X.; Dang, K.A.; Le, H.T.; Ha, G.H.; Nguyen, L.H.; Nguyen, T.H.; Tran, T.H.; Latkin, C.A.; Ho, C.S.H.; Ho, R.C.M. Global evolution of obesity research in children and youths: Setting priorities for interventions and policies. Obes. Facts 2019, 12, 137–149. [Google Scholar] [CrossRef]
- Weder, S.; Hoffmann, M.; Becker, K.; Alexy, U.; Keller, M. Energy, macronutrient intake, and anthropometrics of vegetarian, vegan, and omnivorous children (1–3 years) in Germany (VeChi diet study). Nutrients 2019, 11, 832. [Google Scholar] [CrossRef] [PubMed]
- Bailey, A.D.L.; Fulgoni, V.L., III; Shah, N.; Patterson, A.C.; Gutierrez-Orozco, F.; Mathews, R.S.; Walsh, K.R. Nutrient Intake Adequacy from Food and Beverage Intake of US Children Aged 1–6 Years from NHANES 2001–2016. Nutrients 2021, 13, 827. [Google Scholar] [CrossRef]
- Hovinen, T.; Korkalo, L.; Freese, R.; Skaffari, E.; Isohanni, P.; Niemi, M.; Nevalainen, J.; Gylling, H.; Zamboni, N.; Erkkola, M.; et al. Vegan diet in young children remodels metabolism and challenges the statuses of essential nutrients. EMBO Mol. Med. 2021, 13, e13492. [Google Scholar] [CrossRef] [PubMed]
- Desmond, M.A.; Sobiecki, J.G.; Jaworski, M.; Płudowski, P.; Antoniewicz, J.; Shirley, M.K.; Eaton, S.; Ksiązyk, J.; Cortina-Borja, M.; De Stavola, B.; et al. Growth, body composition, and cardiovascular and nutritional risk of 5- to 10-y-old children consuming vegetarian, vegan, or omnivore diets. Am. J. Clin. Nutr. 2021, 113, 1565–1577. [Google Scholar] [CrossRef]
- McGill, H.C.; Herderick, E.E.; McMahan, C.A.; Zieske, A.W.; Malcom, G.T.; Tracy, R.E.; Strong, J.P. Atherosclerosis in youth. Minerva Pediatr. 2002, 54, 437–447. [Google Scholar] [PubMed]
- Strong, J.P.; Malcom, G.T.; McMahan, C.A.; Tracy, R.E.; Newman, W.P.; Herderick, E.E.; Cornhill, J.F. Prevalence and extent of atherosclerosis in adolescents and young adults: Implications for prevention from the pathobiological determinants of atherosclerosis in youth study. J. Am. Med. Assoc. 1999, 281, 727–735. [Google Scholar] [CrossRef] [PubMed]
- Jing, L.; Pulenthiran, A.; Nevius, C.D.; Mejia-Spiegeler, A.; Suever, J.D.; Wehner, G.J.; Kirchner, H.L.; Haggerty, C.M.; Fornwalt, B.K. Impaired right ventricular contractile function in childhood obesity and its association with right and left ventricular changes: A cine DENSE cardiac magnetic resonance study. J. Cardiovasc. Magn. Reson. 2017, 19, 49. [Google Scholar] [CrossRef]
- Napoli, C.; D’Armiento, F.P.; Mancini, F.P.; Postiglione, A.; Witztum, J.L.; Palumbo, G.; Palinski, W. Fatty streak formation occurs in human fetal aortas and is greatly enhanced maternal, hypercholesterolemia. Intimal accumulation of low density lipoprotein and its oxidation precede monocyte recruitment into early atheroeclerotic lesions. J. Clin. Investig. 1997, 100, 2680–2690. [Google Scholar] [CrossRef]
- Skilton, M.R.; Siitonen, N.; Würtz, P.; Viikari, J.S.A.; Juonala, M.; Seppälä, I.; Laitinen, T.; Lehtimäki, T.; Taittonen, L.; Kähönen, M.; et al. High birth weight is associated with obesity and increased carotid wall thickness in young adults: The cardiovascular risk in young finns study. Arterioscler. Thromb. Vasc. Biol. 2014, 34, 1064–1068. [Google Scholar] [CrossRef]
- Macknin, M.; Kong, T.; Weier, A.; Worley, S.; Tang, A.S.; Alkhouri, N.; Golubic, M. Plant-Based, No-Added-Fat or American Heart Association Diets: Impact on Cardiovascular Risk in Obese Children with Hypercholesterolemia and Their Parents. J. Pediatr. 2015, 166, 953–959.e3. [Google Scholar] [CrossRef]
- Hall, K.D. Did the Food Environment Cause the Obesity Epidemic? Obesity 2018, 26, 11–13. [Google Scholar] [CrossRef]
- Gearhardt, A.N.; Hebebrand, J. The concept of “food addiction” helps inform the understanding of overeating and obesity: Debate Consensus. Am. J. Clin. Nutr. 2021, 113, 274–276. [Google Scholar] [CrossRef] [PubMed]
- Amit, M.; Cummings, C.; Grueger, B.; Feldman, M.; Lang, M.; Grabowski, J.; Wong, D.; Greig, A.; Patel, H. Vegetarian diets in children and adolescents. Paediatr. Child Health 2010, 15, 303–314. [Google Scholar] [PubMed]
- Redecilla Ferreiro, S.; Moráis López, A.; Moreno Villares, J.M.; Leis Trabazo, R.; José Díaz, J.; Sáenz de Pipaón, M.; Blesa, L.; Campoy, C.; Ángel Sanjosé, M.; Gil Campos, M.; et al. Position paper on vegetarian diets in infants and children. Committee on Nutrition and Breastfeeding of the Spanish Paediatric Association. An. Pediatr. 2019, 92, 306.e1–306.e6. [Google Scholar] [CrossRef]
- Lucas, A. Programming by early nutrition: An experimental approach. J. Nutr. 1998, 128, 401S–406S. [Google Scholar] [CrossRef]
- Ripple, W.J.; Wolf, C.; Newsome, T.M.; Barnard, P.; Moomaw, W.R. World Scientists’ Warning of a Climate Emergency. Bioscience 2019, 70, 8–12. [Google Scholar] [CrossRef]
- Crippa, M.; Solazzo, E.; Guizzardi, D.; Monforti-Ferrario, F.; Tubiello, F.N.; Leip, A. Food systems are responsible for a third of global anthropogenic GHG emissions. Nat. Food 2021, 2, 198–209. [Google Scholar] [CrossRef]
- Aleksandrowicz, L.; Green, R.; Joy, E.J.M.; Smith, P.; Haines, A. The Impacts of Dietary Change on Greenhouse Gas Emissions, Land Use, Water Use, and Health: A Systematic Review. PLoS ONE 2016, 11, e0165797. [Google Scholar] [CrossRef]
- Pieper, M.; Michalke, A.; Gaugler, T. Calculation of external climate costs for food highlights inadequate pricing of animal products. Nat. Commun. 2020, 11, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Chai, B.C.; van der Voort, J.R.; Grofelnik, K.; Eliasdottir, H.G.; Klöss, I.; Perez-Cueto, F.J.A. Which Diet Has the Least Environmental Impact on Our Planet? A Systematic Review of Vegan, Vegetarian and Omnivorous Diets. Sustainability 2019, 11, 4110. [Google Scholar] [CrossRef]
- Bakaloudi, D.R.; Halloran, A.; Rippin, H.L.; Oikonomidou, A.C.; Dardavesis, T.I.; Williams, J.; Wickramasinghe, K.; Breda, J.; Chourdakis, M. Intake and adequacy of the vegan diet. A systematic review of the evidence. Clin. Nutr. 2020, 40, 3503–3521. [Google Scholar] [CrossRef]
- German Nutrition Society; Austrian Nutrition Society; Swiss Society of Nutrition Research the SA for N. Ergaenzlieferung D-A-CH Referenzwerte für die Nährstoffzufuhr [Reference Values for Nutrient Intake], 4th ed.; German Nutrition Society; Austrian Nutrition Society; Swiss Society of Nutrition Research the SA for N: Frankfurt, Germany, 2018; pp. 1–56. [Google Scholar]
- EFSA. Dietary Reference Values for nutrients Summary report. EFSA Support. Publ. 2017, 14. [Google Scholar] [CrossRef]
- National Institut for Public Health of Slovenia. Referenčne Vrednosti za Energijski vnos ter vnos Hranil. Tabelarična Priporočila za Otroke (od 1. Leta Starosti Naprej), Mladostnike, Odrasle, Starejše Odrasle, Nosečnice ter Doječe Matere; National Institut for Public Health of Slovenia: Ljubljana, Slovenia, 2020. [Google Scholar]
- Dunn-Emke, S.R.; Weidner, G.; Pettengill, E.B.; Marlin, R.O.; Chi, C.; Ornish, D.M. Nutrient Adequacy of a Very Low-Fat Vegan Diet. J. Am. Diet. Assoc. 2005, 105, 1442–1446. [Google Scholar] [CrossRef]
- Clarys, P.; Deliens, T.; Huybrechts, I.; Deriemaeker, P.; Vanaelst, B.; De Keyzer, W.; Hebbelinck, M.; Mullie, P. Comparison of nutritional quality of the vegan, vegetarian, semi-vegetarian, pesco-vegetarian and omnivorous diet. Nutrients 2014, 6, 1318–1332. [Google Scholar] [CrossRef]
- Schüpbach, R.; Wegmüller, R.; Berguerand, C.; Bui, M.; Herter-Aeberli, I. Micronutrient status and intake in omnivores, vegetarians and vegans in Switzerland. Eur. J. Nutr. 2017, 56, 283–293. [Google Scholar] [CrossRef] [PubMed]
- Elorinne, A.L.; Alfthan, G.; Erlund, I.; Kivimäki, H.; Paju, A.; Salminen, I.; Turpeinen, U.; Voutilainen, S.; Laakso, J. Food and nutrient intake and nutritional status of Finnish vegans and non-vegetarians. PLoS ONE 2016, 11, e0148235. [Google Scholar] [CrossRef]
- Rizzo, N.S.; Jaceldo-Siegl, K.; Sabate, J.; Fraser, G.E. Nutrient Profiles of Vegetarian and Nonvegetarian Dietary Patterns. J. Acad. Nutr. Diet. 2013, 113, 1610–1619. [Google Scholar] [CrossRef]
- Schmidt, J.A.; Crowe, F.L.; Appleby, P.N.; Key, T.J.; Travis, R.C. Serum Uric Acid Concentrations in Meat Eaters, Fish Eaters, Vegetarians and Vegans: A Cross-Sectional Analysis in the EPIC-Oxford Cohort. PLoS ONE 2013, 8, e56339. [Google Scholar] [CrossRef] [PubMed]
- Weikert, C.; Trefflich, I.; Menzel, J.; Obeid, R.; Longree, A.; Dierkes, J.; Meyer, K.; Herter-Aeberli, I.; Mai, K.; Stangl, G.I.; et al. Versorgungsstatus mit Vitaminen und Mineralstoffen bei veganer Ernährungsweise. Dtsch. Arztebl. Int. 2020, 117, 575–582. [Google Scholar]
- Jeran, M. Evaluation of Diet Quality of Vegans and Omnivores with a Web-Based Application. Master’s Thesis, Biotehniška Fakulteta, Univerza v Ljubljani, Ljubljana, Slovenia, 2018. [Google Scholar]
- Kristensen, N.B.; Madsen, M.L.; Hansen, T.H.; Allin, K.H.; Hoppe, C.; Fagt, S.; Lausten, M.S.; Gøbel, R.J.; Vestergaard, H.; Hansen, T.; et al. Intake of macro- and micronutrients in Danish vegans. Nutr. J. 2015, 14, 115. [Google Scholar] [CrossRef]
- National Institute of Public Health of Slovenia. Referenčne Vrednosti za Energijski vnos ter Vnos Hranil; National Institute of Public: Ljubljana, Slovenia, 2020. [Google Scholar]
- Greger, M. A Whole Food Plant-Based Diet Is Effective for Weight Loss: The Evidence. Am. J. Lifestyle Med. 2020, 14, 500–510. [Google Scholar] [CrossRef] [PubMed]
- Mariotti, F.; Gardner, C.D. Dietary protein and amino acids in vegetarian diets—A review. Nutrients 2019, 11, 2661. [Google Scholar] [CrossRef] [PubMed]
- Karlsen, M.; Rogers, G.; Miki, A.; Lichtenstein, A.; Folta, S.; Economos, C.; Jacques, P.; Livingston, K.; McKeown, N.; Karlsen, M.C.; et al. Theoretical Food and Nutrient Composition of Whole-Food Plant-Based and Vegan Diets Compared to Current Dietary Recommendations. Nutrients 2019, 11, 625. [Google Scholar] [CrossRef]
- Green, C.L.; Lamming, D.W.; Fontana, L. Molecular mechanisms of dietary restriction promoting health and longevity. Nat. Rev. Mol. Cell Biol. 2021. [Google Scholar] [CrossRef] [PubMed]
- McCarty, M.F. The moderate essential amino acid restriction entailed by low-protein vegan diets may promote vascular health by stimulating FGF21 secretion. Horm. Mol. Biol. Clin. Investig. 2016, 30. [Google Scholar] [CrossRef] [PubMed]
- Schoenfeld, B.J.; Aragon, A.A. How much protein can the body use in a single meal for muscle-building? Implications for daily protein distribution. J. Int. Soc. Sports Nutr. 2018, 15, 10. [Google Scholar] [CrossRef]
- OPKP Computer Web-Based Software: The Open Platform for Clinical Nutrition (OPEN). Available online: http://www.opkp.si/sl_SI/fooddiary/diary (accessed on 28 July 2019).
- Herreman, L.; Nommensen, P.; Pennings, B.; Laus, M.C. Comprehensive overview of the quality of plant- And animal-sourced proteins based on the digestible indispensable amino acid score. Food Sci. Nutr. 2020, 8, 5379. [Google Scholar] [CrossRef]
- Craddock, J.C.; Genoni, A.; Strutt, E.F.; Goldman, D.M. Limitations with the Digestible Indispensable Amino Acid Score (DIAAS) with Special Attention to Plant-Based Diets: A Review. Curr. Nutr. Rep. 2021, 10, 93–98. [Google Scholar] [CrossRef] [PubMed]
- Reidy, P.T.; Borack, M.S.; Markofski, M.M.; Dickinson, J.M.; Deer, R.R.; Husaini, S.H.; Walker, D.K.; Igbinigie, S.; Robertson, S.M.; Cope, M.B.; et al. Protein supplementation has minimal effects on muscle adaptations during resistance exercise training in young men: A double-blind randomized clinical trial. J. Nutr. 2016, 146, 1660–1669. [Google Scholar] [CrossRef]
- Samal, J.R.K.; Samal, I.R. Protein Supplements: Pros and Cons. J. Diet. Suppl. 2018, 15, 365–371. [Google Scholar] [CrossRef] [PubMed]
- Morton, R.W.; Murphy, K.T.; McKellar, S.R.; Schoenfeld, B.J.; Henselmans, M.; Helms, E.; Aragon, A.A.; Devries, M.C.; Banfield, L.; Krieger, J.W.; et al. A systematic review, meta-analysis and meta-regression of the effect of protein supplementation on resistance training-induced gains in muscle mass and strength in healthy adults. Br. J. Sports Med. 2018, 52, 376–384. [Google Scholar] [CrossRef]
- Young, V.R.; Pellett, P.L. Plant proteins in relation to human protein and amino acid nutrition. Am. J. Clin. Nutr. 1994, 59, 1203S–1212S. [Google Scholar] [CrossRef] [PubMed]
- Moughan, P.J.; Rutherfurd, S.M. Gut luminal endogenous protein: Implications for the determination of ileal amino acid digestibility in humans. Br. J. Nutr. 2012, 108, S258–S263. [Google Scholar] [CrossRef] [PubMed]
- Munro, H.N. Regulation of protein metabolism. Acta Anaesthesiol. Scand. 1974, 55, 66–73. [Google Scholar] [CrossRef] [PubMed]
- Wu, G. Important roles of dietary taurine, creatine, carnosine, anserine and 4-hydroxyproline in human nutrition and health. Amino Acids 2020, 52, 329–360. [Google Scholar] [CrossRef] [PubMed]
- Hou, Y.; He, W.; Hu, S.; Wu, G. Composition of polyamines and amino acids in plant-source foods for human consumption. Amino Acids 2019, 51, 1153–1165. [Google Scholar] [CrossRef] [PubMed]
- Kreider, R.B.; Stout, J.R. Creatine in Health and Disease. Nutrients 2021, 13, 447. [Google Scholar] [CrossRef]
- Jäger, R.; Purpura, M.; Shao, A.; Inoue, T.; Kreider, R.B. Analysis of the efficacy, safety, and regulatory status of novel forms of creatine. Amino Acids 2011, 40, 1369. [Google Scholar] [CrossRef]
- Blancquaert, L.; Baguet, A.; Bex, T.; Volkaert, A.; Everaert, I.; Delanghe, J.; Petrovic, M.; Vervaet, C.; De Henauw, S.; Constantin-Teodosiu, D.; et al. Changing to a vegetarian diet reduces the body creatine pool in omnivorous women, but appears not to affect carnitine and carnosine homeostasis: A randomised trial. Br. J. Nutr. 2018, 119, 759–770. [Google Scholar] [CrossRef]
- Lourenço, R.; Camilo, M.E. Taurine: A conditionally essential amino acid in humans? An overview in health and disease. Nutr. Hosp. 2002, 17, 262–270. [Google Scholar]
- Stabler, S.P.; Allen, R.H. Vitamin B12 deficiency as a worldwide problem. Annu. Rev. Nutr. 2004, 24, 299–326. [Google Scholar] [CrossRef]
- Obeid, R.; Murphy, M.; Solé-Navais, P.; Yajnik, C. Cobalamin status from pregnancy to early childhood: Lessons from global experience. Adv. Nutr. 2017, 8, 971–979. [Google Scholar] [CrossRef] [PubMed]
- Allen, L.H. How common is vitamin B-12 deficiency? Am. J. Clin. Nutr. 2009, 89, 693S–696S. [Google Scholar] [CrossRef] [PubMed]
- Mariotti, F. Vegetarian and Plant-Based Diets in Health and Disease Prevention, 1st ed.; Academic Press: London, UK, 2019; ISBN 9780128039687. [Google Scholar]
- Hankey, G.J. B vitamins for stroke prevention. Stroke Vasc. Neurol. 2018, 3, 51–58. [Google Scholar] [CrossRef]
- Paul, C.; Brady, D.M. Comparative Bioavailability and Utilization of Particular Forms of B12 Supplements with Potential to Mitigate B12-related Genetic Polymorphisms. Integr. Med. 2017, 16, 42–49. [Google Scholar]
- Ströhle, A.; Richter, M.; González-Gross, M.; Neuhäuser-Berthold, M.; Wagner, K.H.; Leschik-Bonnet, E.; Egert, S. The Revised D-A-CH-Reference Values for the Intake of Vitamin B 12: Prevention of Deficiency and Beyond. Mol. Nutr. Food Res. 2019, 63, e1801178. [Google Scholar] [CrossRef]
- Palacios, C.; Gonzalez, L. Is vitamin D deficiency a major global public health problem? J. Steroid Biochem. Mol. Biol. 2014, 144, 138–145. [Google Scholar] [CrossRef] [PubMed]
- Hribar, M.; Hristov, H.; Lavriša, Ž.; Seljak, B.K.; Gregorič, M.; Blaznik, U.; Žmitek, K.; Pravst, I. Vitamin D Intake in Slovenian Adolescents, Adults, and the Elderly Population. Nutrients 2021, 13, 3528. [Google Scholar] [CrossRef]
- Hribar, M.; Hristov, H.; Gregorič, M.; Blaznik, U.; Zaletel, K.; Oblak, A.; Osredkar, J.; Kušar, A.; Žmitek, K.; Rogelj, I.; et al. Nutrihealth Study: Seasonal Variation in Vitamin D Status Among the Slovenian Adult and Elderly Population. Nutrients 2020, 12, 1838. [Google Scholar] [CrossRef]
- Charoenngam, N.; Holick, M.F. Immunologic effects of vitamin d on human health and disease. Nutrients 2020, 12, 2097. [Google Scholar] [CrossRef] [PubMed]
- Roth, D.E.; Abrams, S.A.; Aloia, J.; Bergeron, G.; Bourassa, M.W.; Brown, K.H.; Calvo, M.S.; Cashman, K.D.; Combs, G.; De-Regil, L.M.; et al. Global prevalence and disease burden of vitamin D deficiency: A roadmap for action in low- and middle-income countries. Ann. N. Y. Acad. Sci. 2018, 1430, 44. [Google Scholar] [CrossRef]
- Crowe, F.L.; Steur, M.; Allen, N.E.; Appleby, P.N.; Travis, R.C.; Key, T.J. Plasma concentrations of 25-hydroxyvitamin D in meat eaters, fish eaters, vegetarians and vegans: Results from the EPIC-Oxford study. Public Health Nutr. 2011, 14, 340–346. [Google Scholar] [CrossRef]
- Allès, B.; Baudry, J.; Méjean, C.; Touvier, M.; Péneau, S.; Hercberg, S.; Kesse-Guyot, E. Comparison of Sociodemographic and Nutritional Characteristics between Self-Reported Vegetarians, Vegans, and Meat-Eaters from the NutriNet-Santé Study. Nutrients 2017, 9, 1023. [Google Scholar] [CrossRef]
- Jakše, B.; Jakše, B.; Mis, N.F.; Jug, B.; Šajber, D.; Godnov, U.; Čuk, I. Nutritional Status and Cardiovascular Health in Female Adolescent Elite-Level Artistic Gymnasts and Swimmers: A Cross-Sectional Study of 31 Athletes. J. Nutr. Metab. 2021, 8810548, 15. [Google Scholar] [CrossRef] [PubMed]
- Chan, J.; Jaceldo-Siegl, K.; Fraser, G.E. Serum 25-hydroxyvitamin D status of vegetarians, partial vegetarians, and nonvegetarians: The Adventist Health Study-2. Am. J. Clin. Nutr. 2009, 89, 1686S. [Google Scholar] [CrossRef] [PubMed]
- Pfeifer, M.; Siuka, D.; Pravst, I. Priporočila za Nadomeščanje Holekalciferola (vitamina D3) v Obdobjih Respiratornih Okužb in za Nadomeščanje Holekalciferola pri Posameznikih s COVID-19; University Medical Centre Ljubljana: Ljubljana, Slovenia, 2020. [Google Scholar]
- Ekwaru, J.P.; Zwicker, J.D.; Holick, M.F.; Giovannucci, E.; Veugelers, P.J. The importance of body weight for the dose response relationship of oral vitamin D supplementation and serum 25-hydroxyvitamin D in healthy volunteers. PLoS ONE 2014, 9, e111265. [Google Scholar] [CrossRef]
- American Geriatrics Society Workgroup on Vitamin D Supplementation for Older Adults. American Geriatrics Society Workgroup on Vitamin D Supplementation for Older Adults Recommendations abstracted from the american geriatrics society consensus statement on vitamin D for prevention of falls and their consequences. J. Am. Geriatr. Soc. 2014, 62, 147–152. [Google Scholar] [CrossRef] [PubMed]
- Saunders, A.V.; Davis, B.C.; Garg, M.L. Omega-3 polyunsaturated fatty acids and vegetarian diets. Med. J. Aust. 2013, 199, S22–S26. [Google Scholar] [CrossRef]
- Raatz, S.K.; Bibus, D.; Thomas, W.; Kris-Etherton, P. Human Nutrition and Metabolism: Total fat intake modifies plasma fatty acid composition in humans. J. Nutr. 2001, 131, 231–234. [Google Scholar] [CrossRef] [PubMed]
- Welch, A.A.; Shakya-Shrestha, S.; Lentjes, M.A.H.; Wareham, N.J.; Khaw, K.T. Dietary intake and status of n-3 polyunsaturated fatty acids in a population of fish-eating and non-fish-eating meat-eaters, vegetarians, and vegans and the precursor-product ratio of α-linolenic acid to long-chain n-3 polyunsaturated fatty acids: Results from the EPIC-Norfolk cohort. Am. J. Clin. Nutr. 2010, 92, 1040–1051. [Google Scholar]
- Burns-Whitmore, B.; Froyen, E.; Heskey, C.; Parker, T.; Pablo, G.S. Alpha-linolenic and linoleic fatty acids in the vegan diet: Do they require dietary reference intake/adequate intake special consideration? Nutrients 2019, 11, 2365. [Google Scholar] [CrossRef]
- Koletzko, B.; Reischl, E.; Tanjung, C.; Gonzalez-Casanova, I.; Ramakrishnan, U.; Meldrum, S.; Simmer, K.; Heinrich, J.; Demmelmair, H. FADS1 and FADS2 Polymorphisms Modulate Fatty Acid Metabolism and Dietary Impact on Health. Annu. Rev. Nutr. 2019, 39, 21–44. [Google Scholar] [CrossRef]
- Koletzko, B.; Godfrey, K.M.; Poston, L.; Szajewska, H.; van Goudoever, J.B.; de Waard, M.; Brands, B.; Grivell, R.M.; Deussen, A.R.; Dodd, J.M.; et al. Nutrition During Pregnancy, Lactation and Early Childhood and its Implications for Maternal and Long-Term Child Health: The Early Nutrition Project Recommendations. Ann. Nutr. Metab. 2019, 74, 93–106. [Google Scholar] [CrossRef] [PubMed]
- Ågren, J.J.; Törmälä, M.L.; Nenonen, M.T.; Hänninen, O.O. Fatty acid composition of erythrocyte, platelet, and serum lipids in strict vegans. Lipids 1995, 30, 365–369. [Google Scholar] [CrossRef]
- Vannice, G.; Rasmussen, H. Position of the academy of nutrition and dietetics: Dietary fatty acids for healthy adults. J. Acad. Nutr. Diet. 2014, 114, 136–153. [Google Scholar] [CrossRef]
- Tan, Z.S.; Harris, W.S.; Beiser, A.S.; Au, R.; Himali, J.J.; Debette, S.; Pikula, A.; DeCarli, C.; Wolf, P.A.; Vasan, R.S.; et al. Red blood cell omega-3 fatty acid levels and markers of accelerated brain aging. Neurology 2012, 78, 658–664. [Google Scholar] [CrossRef]
- Witte, A.V.; Kerti, L.; Hermannstädter, H.M.; Fiebach, J.B.; Schreiber, S.J.; Schuchardt, J.P.; Hahn, A.; Flöel, A. Long-chain omega-3 fatty acids improve brain function and structure in older adults. Cereb. Cortex 2014, 24, 3059–3068. [Google Scholar] [CrossRef]
- Sobiecki, J.G.; Appleby, P.N.; Bradbury, K.E.; Key, T.J. High compliance with dietary recommendations in a cohort of meat eaters, fish eaters, vegetarians, and vegans: Results from the European Prospective Investigation into Cancer and Nutrition–Oxford study. Nutr. Res. 2016, 36, 464–477. [Google Scholar] [CrossRef]
- Fallon, N.; Dillon, S.A. Low Intakes of Iodine and Selenium Amongst Vegan and Vegetarian Women Highlight a Potential Nutritional Vulnerability. Front. Nutr. 2020, 0, 72. [Google Scholar] [CrossRef] [PubMed]
- Balk, E.M.; Adam, G.P.; Langberg, V.N.; Earley, A.; Clark, P.; Ebeling, P.R.; Mithal, A.; Rizzoli, R.; Zerbini, C.A.F.; Pierroz, D.D.; et al. Global dietary calcium intake among adults: A systematic review. Osteoporos. Int. 2017, 28, 3315–3324. [Google Scholar] [CrossRef]
- Willett, W.C.; Ludwig, D.S. Milk and Health. N. Engl. J. Med. 2020, 127, 2542–2545. [Google Scholar] [CrossRef] [PubMed]
- Menzel, J.; Abraham, K.; Stangl, G.I.; Ueland, P.M.; Obeid, R.; Schulze, M.B.; Herter-Aeberli, I.; Schwerdtle, T.; Weikert, C. Vegan Diet and Bone Health—Results from the Cross-Sectional RBVD Study. Nutrients 2021, 13, 685. [Google Scholar] [CrossRef] [PubMed]
- Hsu, E. Plant-based diets and bone health: Sorting through the evidence. Curr. Opin. Endocrinol. Diabetes. Obes. 2020, 27, 248–252. [Google Scholar] [CrossRef] [PubMed]
- Tong, T.Y.N.; Appleby, P.N.; Armstrong, M.E.G.; Fensom, G.K.; Knuppel, A.; Papier, K.; Perez-Cornago, A.; Travis, R.C.; Key, T.J. Vegetarian and vegan diets and risks of total and site-specific fractures: Results from the prospective EPIC-Oxford study. BMC Med. 2020, 18, 353. [Google Scholar] [CrossRef] [PubMed]
- Li, T.; Li, Y.; Wu, S. Comparison of human bone mineral densities in subjects on plant-based and omnivorous diets: A systematic review and meta-analysis. Arch. Osteoporos. 2021, 16, 95. [Google Scholar] [CrossRef]
- Jakse, B.; Sekulic, D.; Jakse, B.; Cuk, I.; Sajber, D. Bone health among indoor female athletes and associated factors; a cross-sectional study. Res. Sport. Med. 2019, 28, 314–323. [Google Scholar] [CrossRef] [PubMed]
- Burckhardt, P. Calcium revisited, part III: Effect of dietary calcium on BMD and fracture risk. Bonekey Rep. 2015, 4, 708. [Google Scholar] [CrossRef]
- Melse-Boonstra, A. Bioavailability of Micronutrients From Nutrient-Dense Whole Foods: Zooming in on Dairy, Vegetables, and Fruits. Front. Nutr. 2020, 7, 101. [Google Scholar] [CrossRef]
- Heaney, R.P.; Weaver, C.M.; Hinders, S.; Martin, B.; Packard, P.T. Absorbability of Calcium from Brassica Vegetables: Broccoli, Bok Choy, and Kale. J. Food Sci. 1993, 58, 1378–1380. [Google Scholar] [CrossRef]
- Yang, W.; Li, B.; Dong, X.; Zhang, X.Q.; Zeng, Y.; Zhou, J.L.; Tang, Y.H.; Xu, J.J. Is heme iron intake associated with risk of coronary heart disease? A meta-analysis of prospective studies. Eur. J. Nutr. 2014, 53, 395–400. [Google Scholar] [CrossRef] [PubMed]
- Bao, W.; Rong, Y.; Rong, S.; Liu, L. Dietary iron intake, body iron stores, and the risk of type 2 diabetes: A systematic review and meta-analysis. BMC Med. 2012, 10, 119. [Google Scholar] [CrossRef]
- Fonseca-Nunes, A.; Jakszyn, P.; Agudo, A. Iron and cancer risk-a systematic review and meta-analysis of the epidemiological evidence. Cancer Epidemiol. Biomarkers Prev. 2014, 23, 12–31. [Google Scholar] [CrossRef]
- Posen, J.S. Iron and vegetarian diets. Med. J. Aust. 2013, 199, S11–S16. [Google Scholar]
- Diaz, M.; Rosado, J.L.; Allen, L.H.; Abrams, S.; García, O.P. The efficacy of a local ascorbic acid-rich food in improving iron absorption from Mexican diets: A field study using stable isotopes. Am. J. Clin. Nutr. 2003, 78, 436–440. [Google Scholar] [CrossRef]
- Gautam, S.; Platel, K.; Srinivasan, K. Higher Bioaccessibility of iron and zinc from food grains in the presence of garlic and onion. J. Agric. Food Chem. 2010, 58, 8426–8429. [Google Scholar] [CrossRef]
- Thankachan, P.; Walczyk, T.; Muthayya, S.; Kurpad, A.V.; Hurrell, R.F. Iron absorption in young Indian women: The interaction of iron status with the influence of tea and ascorbic acid 1–3. Am. J. Clin. Nutr. 2008, 87, 881–886. [Google Scholar] [CrossRef]
- Schlemmer, U.; Frølich, W.; Prieto, R.M.; Grases, F. Phytate in foods and significance for humans: Food sources, intake, processing, bioavailability, protective role and analysis. Mol. Nutr. Food Res. 2009, 53, S330–S375. [Google Scholar] [CrossRef] [PubMed]
- Lönnerdal, B. Dietary factors influencing zinc absorption. J. Nutr. 2000, 130, 1378S–1383S. [Google Scholar] [CrossRef]
- Biban, B.G.; Lichiardopol, C. Iodine Deficiency, Still a Global Problem? Curr. Heal. Sci. J. 2017, 43, 103–111. [Google Scholar]
- Eveleigh, E.R.; Coneyworth, L.J.; Avery, A.; Welham, S.J.M. Vegans, vegetarians, and omnivores: How does dietary choice influence iodine intake? A systematic review. Nutrients 2020, 12, 1606. [Google Scholar] [CrossRef] [PubMed]
- Štimec, M.; Kobe, H.; Smole, K.; Kotnik, P.; Širca-Čampa, A.; Zupančič, M.; Battelino, T.; Kržišnik, C.; Fidler Mis, N. Adequate iodine intake of Slovenian adolescents is primarily attributed to excessive salt intake. Nutr. Res. 2009, 29, 888–896. [Google Scholar] [CrossRef]
- World Health Organization. Nutrition, Physical Activity and Obesity Slovenia; World Health Organization, Regional Office for Europe: Copenhagen, Denmark, 2013. [Google Scholar]
- Andersson, M.; Karumbunathan, V.; Zimmermann, M.B. Global iodine status in 2011 and trends over the past decade. J. Nutr. 2012, 142, 744–750. [Google Scholar] [CrossRef] [PubMed]
- Zimmermann, M.B.; Andersson, M. Update on iodine status worldwide. Curr. Opin. Endocrinol. Diabetes. Obes. 2012, 19, 382–387. [Google Scholar] [CrossRef]
- Afshin, A.; Sur, P.J.; Fay, K.A.; Cornaby, L.; Ferrara, G.; Salama, J.S.; Mullany, E.C.; Abate, K.H.; Abbafati, C.; Abebe, Z.; et al. Health effects of dietary risks in 195 countries, 1990–2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet 2019, 393, 1958–1972. [Google Scholar] [CrossRef]
- Partearroyo, T.; de Samaniego-Vaesken, M.L.; Ruiz, E.; Aranceta-Bartrina, J.; Gil, Á.; González-Gross, M.; Ortega, R.M.; Serra-Majem, L.; Varela-Moreiras, G. Sodium intake from foods exceeds recommended limits in the spanish population: The ANIBES study. Nutrients 2019, 11, 2451. [Google Scholar] [CrossRef] [PubMed]
- Monteiro, C.A.; Cannon, G.; Moubarac, J.C.; Levy, R.B.; Louzada, M.L.C.; Jaime, P.C. The UN Decade of Nutrition, the NOVA food classification and the trouble with ultra-processing. Public Health Nutr. 2018, 21, 5–17. [Google Scholar] [CrossRef]
- Meinhardt, A.K.; Müller, A.; Burcza, A.; Greiner, R. Influence of cooking on the iodine content in potatoes, pasta and rice using iodized salt. Food Chem. 2019, 301, 125293. [Google Scholar] [CrossRef] [PubMed]
- Hu, W.; Zhao, C.; Hu, H.; Yin, S. Food Sources of Selenium and Its Relationship with Chronic Diseases. Nutrients 2021, 13, 1739. [Google Scholar] [CrossRef] [PubMed]
- Scientific Advisory Committee on Nutrition. Carbohydrates and Health; The Stationery Office: London, UK, 2015. [Google Scholar]
- Fidler Mis, N.; Braegger, C.; Bronsky, J.; Campoy, C.; Domellöf, M.; Embleton, N.D.; Hojsak, I.; Hulst, J.; Indrio, F.; Lapillonne, A.; et al. Sugar in Infants, Children and Adolescents: A Position Paper of the European Society for Paediatric Gastroenterology, Hepatology and Nutrition Committee on Nutrition. J. Pediatr. Gastroenterol. Nutr. 2017, 65, 681–696. [Google Scholar] [CrossRef]
- Śliż, D.; Parol, D.; Wełnicki, M.; Chomiuk, T.; Grabowska, I.; Dąbrowska, D.; Król, W.; Price, S.; Braksator, W.; Mamcarz, A. Macronutrient intake, carbohydrate metabolism and cholesterol in Polish male amateur athletes on a vegan diet. Nutr. Bull. 2021, 46, 120–127. [Google Scholar] [CrossRef]
- Fuhrman, J.H.; Ferreri, D.M. Nuts And Seeds For Heart Disease Prevention. Int. J. Dis. Reversal Prev. 2020, 2, 8. [Google Scholar] [CrossRef]
- Sethi, S.; Tyagi, S.K.; Anurag, R.K. Plant-based milk alternatives an emerging segment of functional beverages: A review. J. Food Sci. Technol. 2016, 53, 3408–3423. [Google Scholar] [CrossRef]
- Craig, W.J.; Fresán, U. International Analysis of the Nutritional Content and a Review of Health Benefits of Non-Dairy Plant-Based Beverages. Nutrients 2021, 13, 842. [Google Scholar] [CrossRef] [PubMed]
- Carlsen, M.H.; Halvorsen, B.L.; Holte, K.; Bøhn, S.K.; Dragland, S.; Sampson, L.; Willey, C.; Senoo, H.; Umezono, Y.; Sanada, C.; et al. The total antioxidant content of more than 3100 foods, beverages, spices, herbs and supplements used worldwide. Nutr. J. 2010, 9, 3. [Google Scholar] [CrossRef]
- Estruch, R.; Ros, E.; Salas-Salvadó, J.; Covas, M.-I.; Corella, D.; Arós, F.; Gómez-Gracia, E.; Ruiz-Gutiérrez, V.; Fiol, M.; Lapetra, J.; et al. Primary Prevention of Cardiovascular Disease with a Mediterranean Diet. N. Engl. J. Med. 2013, 368, 1279–1290. [Google Scholar] [CrossRef] [PubMed]
- Esselstyn, C.B., Jr. Is Oil Healthy? Int. J. Dis. Reversal Prev. 2019, 1, 3. [Google Scholar] [CrossRef]
- Neelakantan, N.; Seah, J.Y.H.; Van Dam, R.M. The Effect of Coconut Oil Consumption on Cardiovascular Risk Factors: A Systematic Review and Meta-Analysis of Clinical Trials. Circulation 2020, 141, 803–814. [Google Scholar] [CrossRef] [PubMed]
- Jakše, B.; Jakše, B.; Pinter, S.; Pajek, J.; Godnov, U.; Fidler Mis, N. Nutrient and Food Intake of Participants in a Whole-Food Plant-Based Lifestyle Program. J. Am. Coll. Nutr. 2020, 40, 333–348. [Google Scholar] [CrossRef]
- Dewell, A.; Weidner, G.; Sumner, M.D.; Chi, C.S.; Ornish, D. A Very-Low-Fat Vegan Diet Increases Intake of Protective Dietary Factors and Decreases Intake of Pathogenic Dietary Factors. J. Am. Diet. Assoc. 2008, 108, 347–356. [Google Scholar] [CrossRef] [PubMed]
- Kris-Etherton, P.M.; Krauss, R.M. Public health guidelines should recommend reducing saturated fat consumption as much as possible: YES. Am. J. Clin. Nutr. 2020, 112, 13–18. [Google Scholar] [CrossRef]
- Rouxbe Online Culinary School. Available online: https://rouxbe.com/ (accessed on 18 October 2021).
- Moore, W.J.; McGrievy, M.E.; Turner-McGrievy, G.M. Dietary adherence and acceptability of five different diets, including vegan and vegetarian diets, for weight loss: The New DIETs study. Eat. Behav. 2015, 19, 33–38. [Google Scholar] [CrossRef]
- Cruwys, T.; Norwood, R.; Chachay, V.S.; Ntontis, E.; Sheffield, J. “An Important Part of Who I am”: The Predictors of Dietary Adherence among Weight-Loss, Vegetarian, Vegan, Paleo, and Gluten-Free Dietary Groups. Nutrients 2020, 12, 970. [Google Scholar] [CrossRef]
- Brandt, C.J.; Clemensen, J.; Nielsen, J.B.; Søndergaard, J. Drivers for successful long-term lifestyle change, the role of e-health: A qualitative interview study. BMJ Open 2018, 8, 17466. [Google Scholar] [CrossRef]
- Turner-McGrievy, G.M.; Barnard, N.D.; Scialli, A.R. A two-year randomized weight loss trial comparing a vegan diet to a more moderate low-fat diet. Obesity 2007, 15, 2276–2281. [Google Scholar] [CrossRef] [PubMed]
- Fuhrman, J.; Sarter, B.; Glaser, D.; Acocella, S. Changing perceptions of hunger on a high nutrient density diet. Nutr. J. 2010, 9. [Google Scholar] [CrossRef]
- Fuhrman, J. The Hidden Dangers of Fast and Processed Food*. Am. J. Lifestyle Med. 2018, 12, 375–381. [Google Scholar] [CrossRef] [PubMed]
- Chung, M.; Van Buul, V.J.; Wilms, E.; Nellessen, N.; Brouns, F.J.P.H. Nutrition education in European medical schools: Results of an international survey. Eur. J. Clin. Nutr. 2014, 68, 844–846. [Google Scholar] [CrossRef] [PubMed]
- Dumic, A.; Miskulin, M.; Pavlovic, N.; Orkic, Z.; Bilic-Kirin, V.; Miskulin, I. The Nutrition Knowledge of Croatian General Practitioners. J. Clin. Med. 2018, 7, 178. [Google Scholar] [CrossRef] [PubMed]
- Grammatikopoulou, M.G.; Katsouda, A.; Lekka, K.; Tsantekidis, K.; Bouras, E.; Kasapidou, E.; Poulia, K.A.; Chourdakis, M. Is continuing medical education sufficient? Assessing the clinical nutrition knowledge of medical doctors. Nutrition 2019, 57, 69–73. [Google Scholar] [CrossRef]
- Hyska, J.; Mersini, E.; Mone, I.; Bushi, E.; Sadiku, E.; Hoti, K.; Bregu, A. Assessment of knowledge, attitudes and practices about public health nutrition among students of the University of Medicine in Tirana, Albania. South East. Eur. J. Public Heal. 2014. [Google Scholar] [CrossRef]
- Devries, S.; Dalen, J.E.; Eisenberg, D.M.; Maizes, V.; Ornish, D.; Prasad, A.; Sierpina, V.; Weil, A.T.; Willett, W. A deficiency of nutrition education in medical training. Am. J. Med. 2014, 127, 804–806. [Google Scholar] [CrossRef]
- Crowley, J.; Ball, L.; Hiddink, G.J. Nutrition in medical education: A systematic review. Lancet Planet. Health 2019, 3, e379–e389. [Google Scholar] [CrossRef]
- Devries, S.; Agatston, A.; Aggarwal, M.; Aspry, K.E.; Esselstyn, C.B.; Kris-Etherton, P.; Miller, M.; O’Keefe, J.H.; Ros, E.; Rzeszut, A.K.; et al. A Deficiency of Nutrition Education and Practice in Cardiology. Am. J. Med. 2017, 130, 1298–1305. [Google Scholar] [CrossRef] [PubMed]
- Sanne, I.; Bjørke-Monsen, A.L. Lack of nutritional knowledge among Norwegian medical students concerning vegetarian diets. J. Public Health 2020, 7. [Google Scholar] [CrossRef]
- Bettinelli, M.E.; Bezze, E.; Morasca, L.; Plevani, L.; Sorrentino, G.; Morniroli, D.; Giannì, M.L.; Mosca, F. Knowledge of health professionals regarding vegetarian diets from pregnancy to adolescence: An observational study. Nutrients 2019, 11, 1149. [Google Scholar] [CrossRef] [PubMed]
- Hamiel, U.; Landau, N.; Eshel Fuhrer, A.; Shalem, T.; Goldman, M. The Knowledge and Attitudes of Pediatricians in Israel Towards Vegetarianism. J. Pediatr. Gastroenterol. Nutr. 2020, 71, 119–124. [Google Scholar] [CrossRef]
- Ha, B. The Power of Plants: Is a Whole-Foods, Plant-Based Diet the Answer to Health, Health Care, and Physician Wellness? Perm. J. 2019, 23. [Google Scholar] [CrossRef]
- Nestle, M.; Baron, R.B. Nutrition in medical education: From counting hours to measuring competence. JAMA Intern. Med. 2014, 174, 843–844. [Google Scholar] [CrossRef]
- Mulpuri, L.; Allen, N.; Lunde, A.; Thomas, S.; Ray, M.; Polanco, E.; Cret, N.; Molinari, J.; Dowell, L. Rooting for Wellness: An Initiative Introducing Plant-Based Nutrition to First Year Medical Students. Int. J. Dis. Reversal Prev. 2021, 3, 12. [Google Scholar] [CrossRef]
- Saldivar, B.; Al-Turk, B.; Brown, M.; Aggarwal, M. Successful Incorporation of a Plant-Based Menu Into a Large Academic Hospital. Am. J. Lifestyle Med. 2021, 7. [Google Scholar] [CrossRef]
- Aggarwal, M.; Grady, A.; Desai, D.; Hartog, K.; Correa, L.; Ostfeld, R.J.; Freeman, A.M.; McMacken, M.; Gianos, E.; Reddy, K.; et al. Successful Implementation of Healthful Nutrition Initiatives into Hospitals. Am. J. Med. 2020, 133, 19–25. [Google Scholar] [CrossRef]
- Aggarwal, M.; Singh Ospina, N.; Kazory, A.; Joseph, I.; Zaidi, Z.; Ataya, A.; Agito, M.; Bubb, M.; Hahn, P.; Sattari, M. The Mismatch of Nutrition and Lifestyle Beliefs and Actions Among Physicians: A Wake-Up Call. Am. J. Lifestyle Med. 2020, 14, 304–315. [Google Scholar] [CrossRef]
- Storz, M. Barriers to the Plant-Based Movement: A Physician’s Perspective. Int. J. Dis. Reversal Prev. 2020, 2, 4. [Google Scholar] [CrossRef]
- Storz, M.A. Is There a Lack of Support for Whole-Food, Plant-Based Diets in the Medical Community? Perm. J. 2018, 23, 18–068. [Google Scholar] [CrossRef]
- U.S. National Library of Medicine. National Library of Medicine; US National Institutes of Health: Bethesda, MD, USA, 2021. Available online: ClinicalTrials.gov (accessed on 1 December 2021).
- Medawar, E.; Huhn, S.; Villringer, A.; Veronica Witte, A. The effects of plant-based diets on the body and the brain: A systematic review. Transl. Psychiatry 2019, 9, 226. [Google Scholar] [CrossRef] [PubMed]
- Katcher, H.I.; Ferdowsian, H.R.; Hoover, V.J.; Cohen, J.L.; Barnard, N.D. A worksite vegan nutrition program is well-accepted and improves health-related quality of life and work productivity. Ann. Nutr. Metab. 2010, 56, 245–252. [Google Scholar] [CrossRef]
- Spar SPAR Online Grocery Shop, Spar Slovenija Trgovsko Podjetje d. o. o., Ljubljana, Slovenia. 2021. Available online: https://www.sparindia.com/ (accessed on 1 December 2021).
- Mercator Mercator Online Grocery Shop, Družba Poslovni Sistem Mercator, d. d., Ljubljana, Slovenia. 2021. Available online: https://www.mercatorgroup.si/en/home-en-us/ (accessed on 1 December 2021).
- MÜLLER MÜLLER Online Grocery Shop, Müeller Drogerija d. o. o., Ljubljana, Slovenia. 2021. Available online: https://www.mueller.si/letaki-in-revije/ (accessed on 1 December 2021).
- Hofer HOFER Online Grocery Shop, Hofer Trgovina d. o. o., Ljubljana, Slovenia. 2021. Available online: https://www.hofer.at/de/onlineshop/onlineshop-aktionsartikel.html (accessed on 1 December 2021).
- Hiti Dvoršak, A.; Bele, S. Stopnja Samooskrbe s Hrano; Slovenian Environment Agency—ARSO: Ljubljana, Slovenia, 2020.
- Bredač, M.; Bele, S.; Brečko, J.; Hiti, A.; Kožar, M.; Moljk, B.; Travnikar, T.; Zagorc, B. Poročilo o Stanju Kmetijstva, živilstva, Gozdarstva in Ribištva; Agricultural Institute of Slovenia: Ljubljana, Slovenia, 2020. [Google Scholar]
- Slavich, G.M. Life Stress and Health: A Review of Conceptual Issues and Recent Findings. Teach. Psychol. 2016, 43, 346–355. [Google Scholar] [CrossRef] [PubMed]
- Karlsen, M.C.; Pollard, K.J. Strategies for practitioners to support patients in plant-based eating. J. Geriatr. Cardiol. 2017, 14, 338–341. [Google Scholar] [PubMed]
- Reipurth, M.F.S.; Hørby, L.; Gregersen, C.G.; Bonke, A.; Perez Cueto, F.J.A. Barriers and facilitators towards adopting a more plant-based diet in a sample of Danish consumers. Food Qual. Prefer. 2019, 73, 288–292. [Google Scholar] [CrossRef]
- Fresán, U.; Rippin, H. Nutritional Quality of Plant-Based Cheese Available in Spanish Supermarkets: How Do They Compare to Dairy Cheese? Nutrients 2021, 13, 3291. [Google Scholar] [CrossRef]
- Alcorta, A.; Porta, A.; Tárrega, A.; Alvarez, M.D.; Pilar Vaquero, M. Foods for Plant-Based Diets: Challenges and Innovations. Foods 2021, 10, 293. [Google Scholar] [CrossRef]
- Crimarco, A.; Springfield, S.; Petlura, C.; Streaty, T.; Cunanan, K.; Lee, J.; Fielding-Singh, P.; Carter, M.M.; Topf, M.A.; Wastyk, H.C.; et al. A randomized crossover trial on the effect of plant-based compared with animal-based meat on trimethylamine-N-oxide and cardiovascular disease risk factors in generally healthy adults: Study with Appetizing Plantfood-Meat Eating Alternative Trial (SWAP-MEAT). Am. J. Clin. Nutr. 2020, 112, 1188–1199. [Google Scholar]
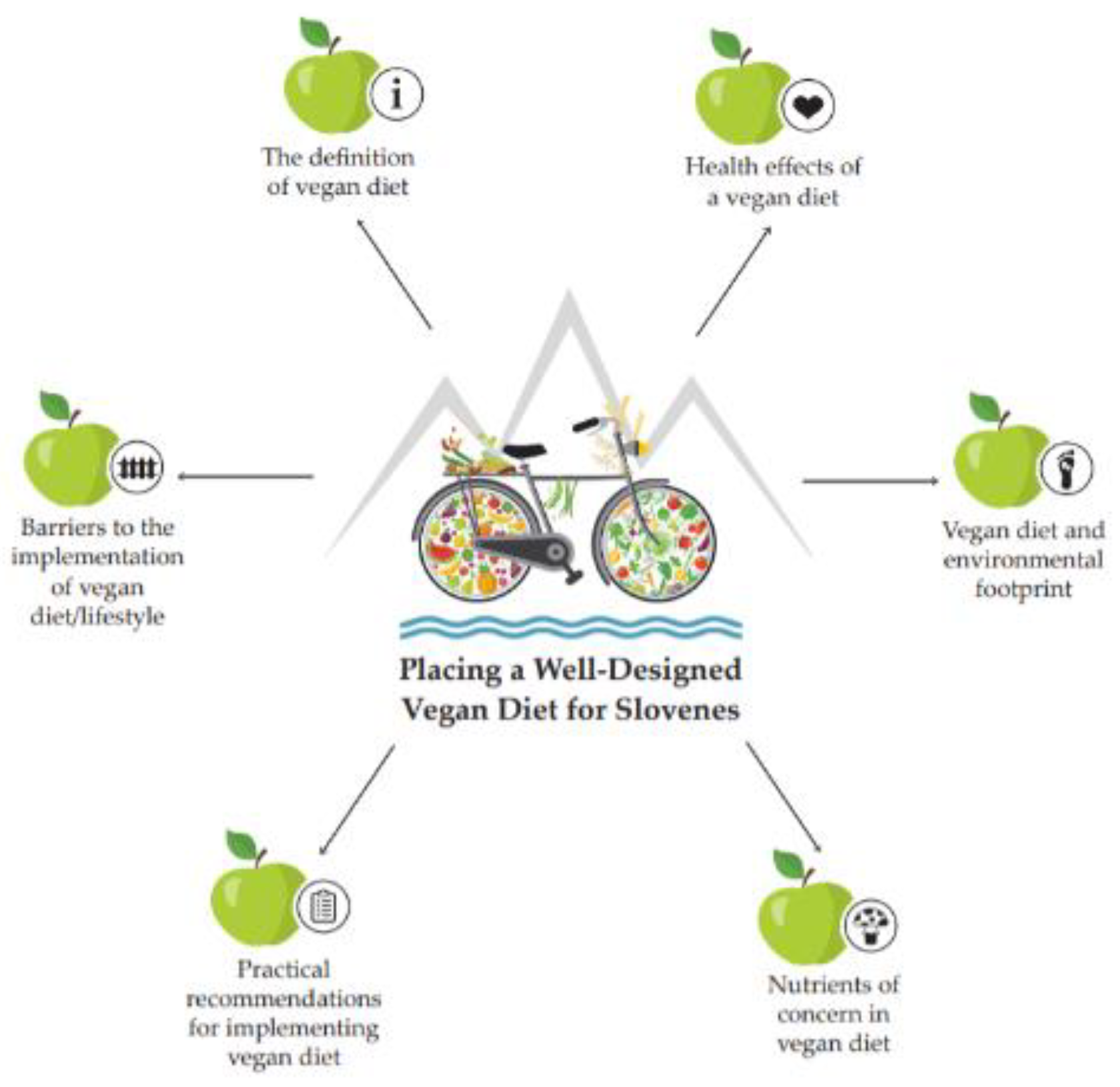
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jakše, B. Placing a Well-Designed Vegan Diet for Slovenes. Nutrients 2021, 13, 4545. https://doi.org/10.3390/nu13124545
Jakše B. Placing a Well-Designed Vegan Diet for Slovenes. Nutrients. 2021; 13(12):4545. https://doi.org/10.3390/nu13124545
Chicago/Turabian StyleJakše, Boštjan. 2021. "Placing a Well-Designed Vegan Diet for Slovenes" Nutrients 13, no. 12: 4545. https://doi.org/10.3390/nu13124545
APA StyleJakše, B. (2021). Placing a Well-Designed Vegan Diet for Slovenes. Nutrients, 13(12), 4545. https://doi.org/10.3390/nu13124545





