Effectiveness of a Lifestyle Modification Program Delivered under Real-World Conditions in a Rural Setting
Abstract
:1. Introduction
2. Materials and Methods
2.1. Design
2.2. Participants and Procedure
2.3. Intervention
2.4. Measures
2.5. Statistical Analysis
3. Results
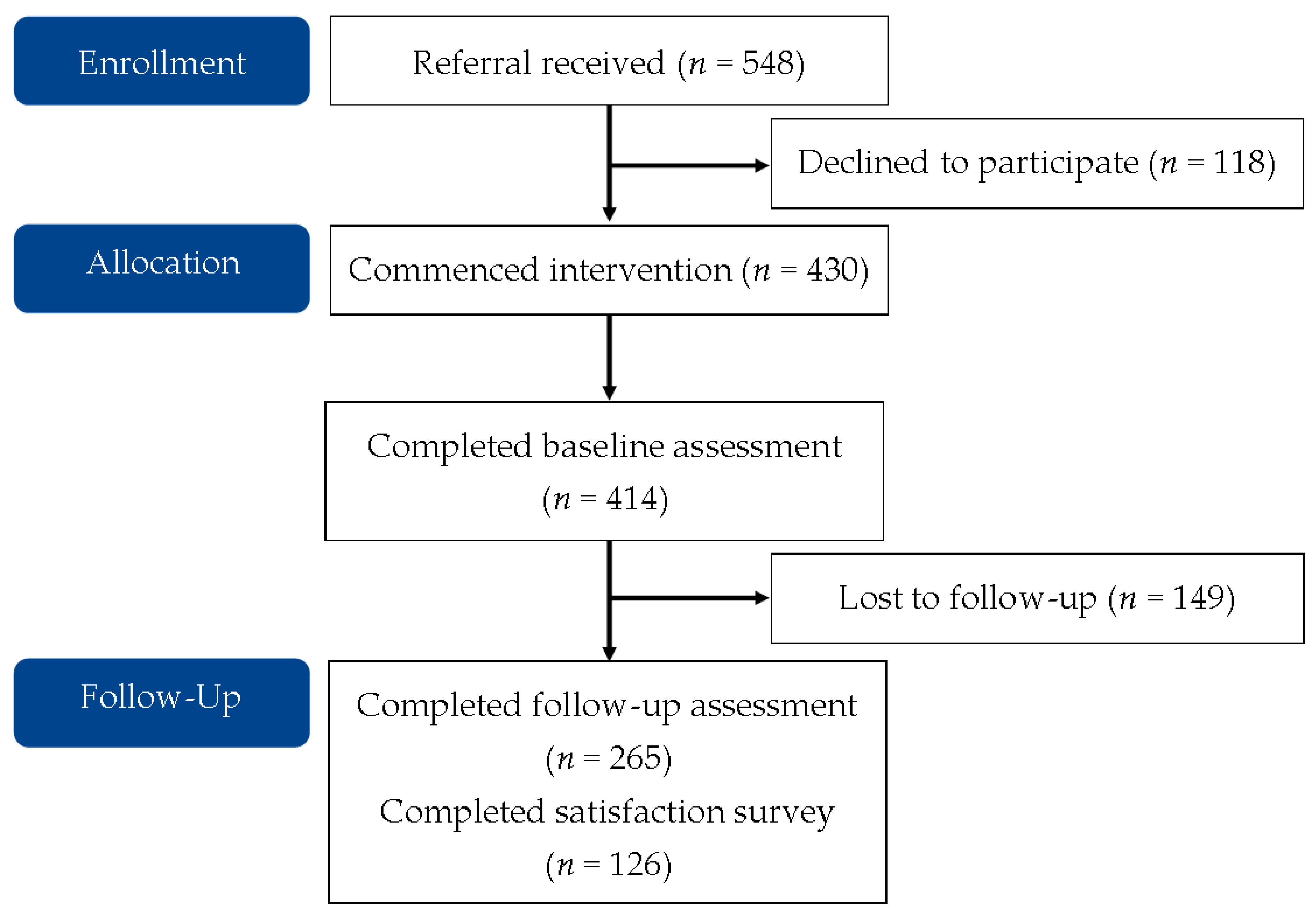
3.1. Uptake and Retention
3.2. Program Effectiveness
3.3. Satisfaction
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Australian Institute of Health and Welfare. Australia’s Health 2014; Australia’s health series no. 14. Cat. no. AUS 178; Australian Institute of Health and Welfare: Canberra, Australia, 2014.
- Crowley, S.; Antioch, K.; Carter, R.; Waters, A.M.; Conway, L.; Mathers, C. The Cost of Diet-Related Disease in Australia: A Discussion Paper; AIHW: Canberra, Australia, 1992.
- Australian Bureau of Statistics. Daily Intake of Fruit and Vegetables. Australian Health Survey: Updated Results, 2011–2012. 2013. Available online: https://www.abs.gov.au/ausstats/abs@.nsf/Lookup/C549D4433F6B74D7CA257B8200179569?opendocument (accessed on 1 September 2021).
- Australian Bureau of Statistics. Australian Health Survey: First Results, 2011–12. Available online: https://www.abs.gov.au/ausstats/abs@.nsf/lookup/1DA0C56919DE176BCA257AA30014BFB7?opendocument (accessed on 1 September 2021).
- Welfare, A. Australia’s Health 2016; Australia’s Health Series No. 15. Cat. No. AUS 199; AIHW: Canberra, Australia, 2016.
- Ball, K.; Lamb, K.E.; Costa, C.; Cutumisu, N.; Ellaway, A.; Kamphuis, C.B.M.; Mentz, G.; Pearce, J.; Santana, P.; Santos, R.; et al. Neighbourhood Socioeconomic Disadvantage and Fruit and Vegetable Consumption: A Seven Countries Comparison. Int. J. Behav. Nutr. Phys. Act. 2015, 12, 1–13. [Google Scholar] [CrossRef] [Green Version]
- Beenackers, M.A.; Kamphuis, C.B.M.; Giskes, K.; Brug, J.; Kunst, A.E.; Burdorf, A.; Van Lenthe, F.J. Socioeconomic Inequalities in Occupational, Leisure-Time, and Transport Related Physical Activity among European Adults: A systematic review. Int. J. Behav. Nutr. Phys. Act. 2012, 9, 116. [Google Scholar] [CrossRef] [Green Version]
- Andrade-Gómez, E.; García-Esquinas, E.; Ortolá, R.; Martinez-Gomez, D.; Rodríguez-Artalejo, F. Watching TV has a Distinct Sociodemographic and Lifestyle Profile Compared with Other Sedentary Behaviors: A nationwide population-based study. PLoS ONE 2017, 12, e0188836. [Google Scholar] [CrossRef] [Green Version]
- Australian Institute of Health and Welfare. Rural and Remote Health. Available online: https://www.aihw.gov.au/reports/rural-health/rural-remote-health (accessed on 3 October 2019).
- Australian Institute of Health and Welfare. Australian Burden of Disease Study: Impact and Causes of Illness and Death in Aboriginal and Torres Strait Islander People 2011; Cat. no. BOD 7.; AIHW: Canberra, Australia, 2016.
- Reading, J. The Crisis of Chronic Disease among Aboriginal Peoples: A Challenge for Public Health, Population Health and Social Policy; Centre for Aboriginal Health Research: Victoria, BC, Canada, 2009. [Google Scholar]
- Hefford, M.; Crampton, P.; Foley, J. Reducing Health Disparities through Primary Care Reform: The New Zealand Experiment. Health Policy 2005, 72, 9–23. [Google Scholar] [CrossRef] [PubMed]
- Cleland, V.; Squibb, K.; Stephens, L.; Dalby, J.; Timperio, A.; Winzenberg, T.; Ball, K.; Dollman, J. Effectiveness of Interventions to Promote Physical Activity and/or Decrease Sedentary Behaviour among Rural Adults: A Systematic Review and Meta-Analysis. Obes. Rev. 2017, 18, 727–741. [Google Scholar] [CrossRef]
- Rhodes, R.E.; Janssen, I.; Bredin, S.; Warburton, D.; Bauman, A. Physical Activity: Health Impact, Prevalence, Correlates and Interventions. Psychol. Health 2017, 32, 942–975. [Google Scholar] [CrossRef]
- Greaves, C.J.; Sheppard, K.E.; Abraham, C.; Hardeman, W.; Roden, M.; Evans, P.H.; Schwarz, P. The IMAGE STUDY Group. Systematic Review of Reviews of Intervention Components Associated with Increased Effectiveness in Dietary and Physical Activity Interventions. BMC Public Health 2011, 11, 119. [Google Scholar] [CrossRef]
- Pignone, M.P.; Ammerman, A.; Fernandez, L.; Orleans, C.; Pender, N.; Woolf, S.; Lohr, K.N.; Sutton, S. Counseling to promote a healthy diet in adults: A summary of the evidence for the U.S. Preventive Services Task Force. Am. J. Prev. Med. 2003, 24, 75–92. [Google Scholar] [CrossRef]
- Conn, V.S.; Hafdahl, A.R.; Brown, S.A.; Brown, L.M. Meta-analysis of patient education interventions to increase physical activity among chronically ill adults. Patient Educ. Couns. 2008, 70, 157–172. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shelton, R.C.; Lee, M. Sustaining Evidence-Based Interventions and Policies: Recent Innovations and Future Directions in Implementation Science. Am. Public Health Assoc. 2019, 109, S132–S134. [Google Scholar] [CrossRef] [PubMed]
- Bell, K.J.L.; McCullough, A.; Del Mar, C.; Glasziou, P. What’s the uptake? Pragmatic RCTs may be used to estimate uptake, and thereby population impact of interventions, but better reporting of trial recruitment processes is needed. BMC Med. Res. Methodol. 2017, 17, 174. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kerner, J.; Rimer, B.; Emmons, K. Introduction to the Special Section on Dissemination: Dissemination Research and Research Dissemination: How Can We Close the Gap? Health Psychol. 2005, 24, 443–446. [Google Scholar] [CrossRef] [PubMed]
- Brownson, R.C.; Jones, E. Bridging the gap: Translating research into policy and practice. Prev. Med. 2009, 49, 313–315. [Google Scholar] [CrossRef]
- Ali, M.K.; Echouffo-Tcheugui, J.B.; Williamson, D.F. How Effective Were Lifestyle Interventions in Real-World Settings That Were Modeled on The Diabetes Prevention Program? Health Aff. 2012, 31, 67–75. [Google Scholar] [CrossRef] [Green Version]
- Hetherington, S.A.; Borodzicz, J.A.; Shing, C.M. Assessing the real world effectiveness of the Healthy Eating Activity and Lifestyle (HEAL™) program. Health Promot. J. Aust. 2015, 26, 93–98. [Google Scholar] [CrossRef] [PubMed]
- Norton, K.; Norton, L. Pre-Exercise Screening. Guide to the Australian Adult Pre-Exercise Screening System; Exercise and Sports Science Australia: Adelaide, Australia, 2011. [Google Scholar]
- Australian Bureau of Statistics. Table 3 Correspondence 1270.0.55.005—Australian Statistical Geography Standard (ASGS): Volume 5—Remoteness Structure, July 2016; Australian Bureau of Statistics: Canberra, Australia, 2018.
- Australian Bureau of Statistics. Table 2 Postal Area (POA) Index of Relative Socio-Economic Disadvantage, 2016. 2033.0.55.001—Census of Population and Housing: Socio-Economic Indexes for Areas (SEIFA) Australia, 2016; Australian Bureau of Statistics: Canberra, Australia, 2018.
- Australian Institute of Health Welfare. The Active Australia Survey: A Guide and Manual for Implementation, Analysis and Reporting; AIHW: Canberra, Australis, 2003.
- Brown, W.J.; Burton, N.; Marshall, A.; Miller, Y.D. Reliability and Validity of a Modified Self-Administered Version of the Active Australia Physical Activity Survey in a Sample of Mid-Age Women. Aust. N. Z. J. Public Health 2008, 32, 535–541. [Google Scholar] [CrossRef]
- Brown, W.; Bauman, A.; Chey, T.; Trost, S.; Mummery, K. Method: Comparison of Surveys Used to Measure Physical Activity. Aust. N. Z. J. Public Health 2004, 28, 128–134. [Google Scholar] [CrossRef]
- Cora, C.L.; Marshall, A.L.; Sjostrom, M.; Bauman, A.E.; Booth, M.L.; Ainsworth, B.E.; Pratt, M.; Ekelund, U.; Yngve, A.; Sallis, J.F.; et al. International Physical Activity Questionnaire: 12-Country Reliability and Validity. Med. Sci. Sports Exerc. 2003, 35, 1381–1395. [Google Scholar] [CrossRef] [Green Version]
- Wright, J.L.; Scott, J.A. The Fat and Fibre Barometer, a Short Food Behaviour Questionnaire: Reliability, Relative Validity and Utility. Aust. J. Nutr. Diet. 2000, 57, 33–39. [Google Scholar]
- Harada, N.D.; Chiu, V.; Stewart, A.L. Mobility-related function in older adults: Assessment with a 6-minute walk test. Arch. Phys. Med. Rehabil. 1999, 80, 837–841. [Google Scholar] [CrossRef]
- Rikli, R.E.; Jones, C.J. Development and Validation of a Functional Fitness Test for Community-Residing Older Adults. J. Aging Phys. Act. 1999, 7, 129–161. [Google Scholar] [CrossRef]
- Gupta, S.K. Intention-to-Treat Concept: A Review. Perspect. Clin. Res. 2011, 2, 109–112. [Google Scholar] [CrossRef] [PubMed]
- National Health and Medical Research Council. Australian Dietary Guidelines (Reference N55a); National Health and Medical Research Council: Canberra, Australia, 2013.
- Australian Institute of Health and Welfare. Towards National Indicators for Food and Nutrition: An AIHW View. Reporting against the Dietary Guidelines for Australian Adults; Cat. No. PHE 70; AIHW: Canberra, Australia, 2005.
- Adams, S.A. The Effect of Social Desirability and Social Approval on Self-Reports of Physical Activity. Am. J. Epidemiol. 2005, 161, 389–398. [Google Scholar] [CrossRef] [PubMed]
- Edney, S.M.; Olds, T.; Ryan, J.C.; Vandelanotte, C.; Plotnikoff, R.C.; Curtis, R.; Maher, C.A. A Social Networking and Gamified App to Increase Physical Activity: Cluster RCT. Am. J. Prev. Med. 2020, 58, e51–e62. [Google Scholar] [CrossRef]
- Australian Institute of Health and Welfare. Profile of Indigenous Australians. Available online: https://www.aihw.gov.au/reports/australias-welfare/profile-of-indigenous-australians (accessed on 5 September 2021).
- Ness, R.B.; Nelson, D.B.; Kumanyika, S.K.; Grisso, J.A. Evaluating Minority Recruitment into Clinical Studies: How Good are the Data? Ann. Epidemiol. 1997, 7, 472–478. [Google Scholar] [CrossRef]
- Moreno-John, G.; Gachie, A.; Fleming, C.M.; Nápoles-Springer, A.; Mutran, E.; Manson, S.M.; Pérez-Stable, E.J. Ethnic Minority Older Adults Participating in Clinical Research. J. Aging Health 2004, 16, 93S–123S. [Google Scholar] [CrossRef] [PubMed]
- Gavarkovs, A.G.; Burke, S.M.; Petrella, R.J. Engaging Men in Chronic Disease Prevention and Management Programs. Am. J. Men’s Health 2016, 10, NP145–NP154. [Google Scholar] [CrossRef] [PubMed]
- Brown, C.H.; Curran, G.; Palinkas, L.A.; Aarons, G.A.; Wells, K.B.; Jones, L.; Collins, L.M.; Duan, N.; Mittman, B.S.; Wallace, A.; et al. An Overview of Research and Evaluation Designs for Dissemination and Implementation. Annu. Rev. Public Health 2017, 38, 1–22. [Google Scholar] [CrossRef] [Green Version]
| n | Males (n = 102) | Females (n = 300) | All (n = 414) a | |
|---|---|---|---|---|
| Age (years), M (SD) | 383 | 55.3 (12.55) | 53.2 (14.4) | 53.7 (13.9) |
| Aboriginal, n (%) | 380 | 12 (12.2) | 30 (10.6) | 42 (11.1) |
| Health care card (yes), n (%) | 362 | 53 (55.8) | 113 (49.8) | 186 (51.4) |
| Remoteness, n (%) | 399 | |||
| Major Cities | 3 (2.9) | 5 (1.7) | 8 (2.0) | |
| Inner Regional | 30 (29.4) | 93 (31.5) | 123 (30.8) | |
| Outer Regional | 47 (46.1) | 99 (33.6) | 147 (36.8) | |
| Remote | 18 (17.6) | 87 (29.5) | 106 (26.6) | |
| Very Remote | 4 (3.9) | 11 (3.7) | 15 (3.8) | |
| SES decile, n (%) | 399 | |||
| 1–2 | 36 (35.3) | 71 (24.1) | 107 (26.8) | |
| 3–4 | 26 (25.5) | 119 (40.3) | 146 (36.6) | |
| 5–6 | 28 (27.5) | 70 (23.7) | 98 (24.6) | |
| 7–8 | 5 (4.9) | 28 (9.5) | 34 (8.5) | |
| 9–10 | 5 (6.9) | 7 (2.4) | 14 (3.5) | |
| Completed sessions, M (SD) | 290 | 6.2 (2.3) | 6.1 (2.0) | 6.1 (2.1) |
| Walking (min/week), M (SD) | 394 | 91.8 (118.9) | 71.6 (99.3) | 75.7 (103.9) |
| Planned PA (min/week), M (SD) | 397 | 66.7 (112.2) | 56.1 (96.7) | 59.1 (100.2) |
| Incidental PA (min/week), M (SD) | 378 | 119.7 (170.9) | 116.6 (170.5) | 116.9 (169.0) |
| Total PA (min/week), M (SD) | 358 | 277.0 (282.6) | 230.2 (227.7) | 240.7 (241.5) |
| Sitting time (h/day), M (SD) | 400 | 6.7 (3.8) | 5.8 (2.9) | 6.03 (3.15) |
| Fruit (servings/day), M (SD) | 409 | 1.5 (1.1) | 1.6 (1.2) | 1.6 (1.1) |
| Vegetables (servings/day), M (SD) | 411 | 2.4 (1.3) | 2.6 (1.4) | 2.6 (1.4) |
| Weight (kg), M (SD) | 413 | 109.9 (26.8) | 95.6 (22.3) | 99.3 (24.2) |
| Waist circumference (cm), M (SD) | 404 | 120.4 (16.9) | 111.5 (16.8) | 113.8 (17.2) |
| BMI, M (SD) | 412 | 35.8 (7.8) | 36.6 (8.0) | 36.4 (7.9) |
| Systolic BP (mmHg), M (SD) | 384 | 139.8 (14.8) | 133.3 (15.8) | 135.1 (15.7) |
| Diastolic BP (mmHg), M (SD) | 377 | 81.0 (10.0) | 79.0 (10.4) | 79.5 (10.3) |
| 30 s chair stand (n), M (SD) | 396 | 10.9 (3.8) | 10.9 (3.5) | 10.9 (3.5) |
| 30 s arm curl (n), M (SD) | 403 | 23.0 (9.5) | 22.2 (9.5) | 22.3 (9.4) |
| 6 min walk (m), M (SD) | 377 | 380.0 (127.6) | 375.0 (127.8) | 376.6 (130.2) |
| Baseline | 8 Weeks | Estimated Difference | |||
|---|---|---|---|---|---|
| n | M (SD) | n | M (SD) | B [95% CI] | |
| Walking (min/week) | 394 | 75.7 (103.9) | 250 | 110.7 (116.7) | 31.66 [20.77, 42.56] *** |
| Planned PA (min/week) | 397 | 59.1 (100.2) | 251 | 115.4 (99.9) | 58.09 [45.88, 70.30] *** |
| Incidental PA (min/week) | 378 | 116.9 (169.0) | 239 | 157.2 (204.4) | 46.17 [24.24, 68.11] *** |
| Total PA (min/week) | 358 | 277.0 (282.6) | 292 | 387.5 (277.3) | 140.98 [112.87, 169.09] *** |
| Sitting time (h/day) | 400 | 6.03 (3.15) | 252 | 5.5 (2.7) | −0.36 [−0.59, −0.12] ** |
| Fruit (servings/day) | 409 | 1.6 (1.1) | 255 | 2.0 (1.0) | 0.38 [0.27, 0.48] *** |
| Vegetables (servings/day) | 411 | 2.6 (1.4) | 256 | 3.4 (1.4) | 0.81 [0.66, 0.96] *** |
| Weight (kg) | 413 | 99.27 (24.17) | 263 | 94.45 (22.05) | −1.43 [−2.44, −0.41] ** |
| Waist circumference (cm) | 404 | 113.8 (17.2) | 257 | 110.3 (17.8) | −1.61 [−2.50, −0.72] *** |
| Systolic BP (mmHg) | 384 | 135.1 (15.7) | 245 | 133.4 (15.4) | −1.63 [−3.42, 0.17] |
| Diastolic BP (mmHg) | 377 | 79.5 (10.3) | 239 | 78.3 (10.4) | −1.10 [−2.15, −0.05] * |
| 30 s chair stand (n) | 396 | 10.9 (3.5) | 250 | 13.1 (4.9) | 2.01 [1.61, 2.42] *** |
| 30 s arm curl (n) | 403 | 22.3 (9.4) | 255 | 24.6 (10.0) | 2.61 [2.03, 3.19] *** |
| 6 min walk (m) | 377 | 376.6 (130.2) | 234 | 402.0 (146.9) | 24.68 [12.70, 36.66] *** |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jennings, C.; Patterson, E.; Curtis, R.G.; Mazzacano, A.; Maher, C.A. Effectiveness of a Lifestyle Modification Program Delivered under Real-World Conditions in a Rural Setting. Nutrients 2021, 13, 4040. https://doi.org/10.3390/nu13114040
Jennings C, Patterson E, Curtis RG, Mazzacano A, Maher CA. Effectiveness of a Lifestyle Modification Program Delivered under Real-World Conditions in a Rural Setting. Nutrients. 2021; 13(11):4040. https://doi.org/10.3390/nu13114040
Chicago/Turabian StyleJennings, Cally, Elsie Patterson, Rachel G. Curtis, Anna Mazzacano, and Carol A. Maher. 2021. "Effectiveness of a Lifestyle Modification Program Delivered under Real-World Conditions in a Rural Setting" Nutrients 13, no. 11: 4040. https://doi.org/10.3390/nu13114040
APA StyleJennings, C., Patterson, E., Curtis, R. G., Mazzacano, A., & Maher, C. A. (2021). Effectiveness of a Lifestyle Modification Program Delivered under Real-World Conditions in a Rural Setting. Nutrients, 13(11), 4040. https://doi.org/10.3390/nu13114040






