Abstract
Physical inactivity is a major public health problem, and there are concerns this might have increased during the COVID-19 pandemic. We aimed to identify distinct trajectories of physical activity over a 6-week period after the first restrictive measures and to explore determinants of these trajectories in a population-based cohort of middle-aged and elderly in the Netherlands (n = 5777). We observed that at least 59% of participants did not meet the World Health Organization recommendations for physical activity. Using latent class trajectory analyses over three time points, we identified five distinct trajectories, including four steady trajectories at different levels (very low, low, medium and high) and one increasing trajectory. Using multinomial logistic regression analyses, we observed that, compared to the ‘steadily high’ trajectory, participants in the ‘steadily very low’ trajectory were more often older, lower educated, reporting poorer physical health, more depressive symptoms, consuming a less healthy diet, smoking, and lower alcohol use, and were less often retired. A similar pattern of determinants was seen for those in the increasing trajectory, albeit with smaller effect sizes. Concluding, we observed low levels of physical activity that generally remained during the pandemic. The determinants we described can help identify groups that require additional preventive interventions.
1. Introduction
In March 2020, the World Health Organization (WHO) declared COVID-19 to be a pandemic. To curb the pandemic, several regional and national governments responded by encouraging people to stay at home and keep distance from each other. Due to these restrictive measures many health behaviors may have changed, among which physical activity levels [1].
The health benefits of physical activity are indisputable [2,3]. However, more than half of the European population does not meet the WHO guidelines of at least 150 min of moderate or 75 min of vigorous physical activity per week [4]. Several studies have shown a further decrease in physical activity during the COVID-19 pandemic after the first restrictive measures were implemented [5,6,7]. This is a major public health concern as physical activity may lessen the burden or impact of COVID-19 [8], and potentially also of various physical and mental health consequences of the restrictive measures [9,10]. Encouraging individuals to remain physically active during the pandemic should therefore be a public health priority, calling for the identification of determinants reflecting participants who need specific attention for preventive interventions.
So far, only a few studies have identified changes in physical activity during the pandemic. These studies have found that average physical activity levels remained stable or increased within a few weeks after the start of restrictive measures [5,6]. However, these studies mainly focused on average changes on a population-level, while individuals within a population may show different patterns. Different subgroups of the population, e.g., those with different ages, or different statuses of physical and psychosocial health, may have responded differently to the restrictive measures in their behaviors of physical activity.
Therefore, we determined distinct trajectories of physical activity over a 6-week period after the first restrictive measures were announced and explored determinants of these trajectories in a middle-aged and elderly population in the Netherlands.
2. Materials and Methods
2.1. Study Design and Participants
This study was embedded within the Rotterdam Study, a large ongoing population-based cohort study among residents of the Ommoord area, a suburb in Rotterdam, the Netherlands. The initial cohort started in 1989 and comprised 7983 participants aged 55 years and older. The cohort was subsequently expanded three times with 3011 participants in 2000 (≥55 years), 3932 participants in 2005 (≥45 years), and 3368 participants in 2016 (≥40 years), resulting in a study population of 18,924 participants [11].
On 8 April 2020, 9008 of the 18,924 participants were still alive and participating in the Rotterdam Study. Among those, 8732 participants were not hospitalized or living in a nursing home and were invited to fill out multiple questionnaires during the COVID-19 pandemic [12].
For the current analyses, we used data from the first three questionnaires. The response rate was 71.5% (N = 6242 out of 8732) for the first questionnaire, 64.6% (N = 5640 out of 8.732) for the second questionnaire and 88.2% (N = 4956 out of 5618) for the third questionnaire. For the current study, we excluded participants with no physical activity data from the first questionnaire (N = 465), leaving 5777 participants for analyses.
2.2. Measurements
2.2.1. COVID-19 Questionnaire
The COVID-19 questionnaire was sent out three times between 20 April 2020 and 22 May 2020, with an interval of two weeks. The first two questionnaires were sent on paper to all participants. The third questionnaire was sent both digitally and on paper, only to participants who actively agreed to participate. This questionnaire included questions on the following categories: COVID-19 related symptoms and risk factors, mental health and health care utilization during the pandemic. Questions were based on the COVID-19 questionnaire of the Lifelines COVID-19 cohort, which was designed to compare results among similar projects within Europe and including similar questions as used in studies in Denmark and France at that time [13].
2.2.2. Physical Activity
At each time point, participants answered the question how many minutes they spent in moderate-to-vigorous physical activity (e.g., walking, cycling, running) in total in the previous 14 days. Answer options, in line with the LifeLines COVID-19 cohort questionnaire [13], were “less than 50 min”, “50–100 min”, “100–150 min”, “150–180 min”, and “more than 180 min”.
2.2.3. Determinants
For information on potential determinants, we used data from the first COVID-19 questionnaire (time point 1). We included determinants based on the intrapersonal domain of the socio-ecological model, referring to an individuals’ demographic, biological and psychological characteristics [14,15,16].
1. Demographics
Self-report data were available for sex, age, education, and occupation. Educational level was categorized into primary, lower, intermediate and higher education according to the UNESCO classification. Occupational status was categorized into ‘employed’, ‘not employed’, and ‘retired’ [13,17].
2. Physical Health
Participants were asked how they would self-report their overall health status with answer options ‘excellent’, ‘very good’, ‘good’, ‘fair’, and ‘poor’ [13,17].
3. Psychosocial Health
Depressive symptoms were assessed using a shortened version of the Dutch Center for Epidemiological Studies Depression (CES-D) scale [18,19]. The sum score, based on 10 items of the questionnaire, ranges from 0 to 30, with higher scores indicating more depressive symptoms. To assess symptoms of anxiety, the subscale for anxiety of the Hospital Anxiety and Depression Scale (HADS-A) was used [20,21]. The subscale consists of seven items resulting in a total score ranging from 0 to 21, a higher score reflects more symptoms of anxiety. Participants were also asked how worried they have been in the past 14 days about the pandemic. Answer options were on a 10-point Likert scale, with higher scores reflecting more worries about the pandemic [13,22,23].
4. Lifestyle
Participants were asked how healthy their eating behaviour was compared to before the pandemic. Answer options were on a 5-point Likert scale: “much less healthy”, “less healthy”, “just as healthy”, “more healthy” and “much more healthy” [13,24]. Smoking was asked by a single question: “Have you smoked in the last 14 days?”, which could be answered with ‘yes’ or ‘no’. Alcohol use was asked by the question: “Have you used alcohol in the last 14 days? If so, how many glasses per day on average?”. This question could be answered by ‘no’ or ‘yes’, with the number of glasses [13].
2.3. Statistical Analysis
The study population was characterized using descriptive statistics. Missing information on potential determinants of activity (<3%, except for worries about the pandemic: 4.3%, and occupational status: 9.1%) was imputed using 10 folded multiple imputation using the mice package in R.
To determine distinct trajectories of physical activity, latent class trajectory analyses were performed using the lcmm package in R. Due to the ordinal nature of the physical activity variable, threshold models were used (using the ‘thresholds’ link function) with fixed effects for time. Models from two to seven latent classes were constructed to investigate which of these best fitted our data. Models of five, six or seven classes were almost equal in terms of fit measures (e.g., Bayesian Information Criterion (BIC) and relative entropy). As the solution with six classes showed one class with a small number of participants (N = 167, 2.9%), we continued our analyses with a parsimonious model of five distinct trajectories of physical activity (BIC: 38615.3, relative entropy: 0.71).
Subsequently, we investigated the associations of potential determinants with the five different trajectories of physical activity using multinomial logistic regression. As potential determinants we included: sex, age, educational level, occupational status, self-perceived health, depressive symptoms, anxiety symptoms, worries related to the pandemic, diet, smoking and alcohol use. Class membership (which trajectory the participant belongs to) was used as the outcome variable. First, analyses were performed using sex- and age adjusted models. Secondly, models were adjusted for all other potential determinants in order to study associations of determinants independent of each other. For sensitivity analyses, we repeated the analyses excluding participants who got infected with COVID-19 during the study period.
Data analyses were performed using R version 4.0.2 (The R Foundation for Statistical Computing, Vienna, Austria) using the mice, lcmm and nnet packages.
3. Results
Characteristics of the study population are presented in Table 1. Mean age of the population was 69.4 (standard deviation (SD): 11.5) years and 58% was female. Physical activity levels at baseline were generally low: 3434 participants (59.4%) reported less than 150 min of moderate-to-vigorous physical activity in the past 14 days, of which 1323 (22.9%) participants reported even less than 50 min. Only 1673 (29.0%) reported more than 180 min. Descriptive information on physical activity at all three time points is presented in Supplementary Table S1.

Table 1.
Study sample characteristics.
3.1. Physical Activity Trajectories
Five distinct trajectories were defined (Figure 1, Supplementary Table S2). Four trajectories were steady over time, although a slight increase was shown in each group. A total of 1837 (32%) participants belonged to the trajectory that reported ‘steadily high’ physical activity. Another 1277 (22%) participants reported ‘steadily medium’ levels, and 1590 (28%) participants reported ‘steadily low’ levels. A total of 786 (14%) participants reported ‘steadily very low’ levels of physical activity. Finally, 287 (5%) participants increased their physical activity during the pandemic from the level of the ‘steadily low’ to the ‘steadily high’ group, referred to as ‘increasers.
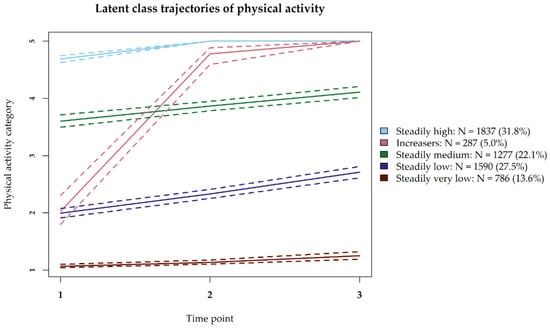
Figure 1.
Trajectories of physical activity during COVID-19 pandemic. Question asked at each time point: “During the past 14 days, how many minutes did you exercise (moderately) intensively in total (walking, cycling, running)?”. Physical activity categories refer to the different answer options: 1 ‘Less than 50 min’, 2 ‘50–100 min’, 3 ‘100–150 min’, 4 ‘150–180 min’, 5 ‘More than 180 min’.
3.2. Determinants of Trajectories
The trajectory of participants who reported ‘steadily high’ physical activity levels over time was used as reference group for all analyses, in order to investigate which determinants were associated with less optimal trajectories. Results of sex- and age adjusted models are presented in Table 2, and of multivariate models in Table 3.

Table 2.
Sex- and age adjusted associations of potential determinants with the latent class of physical activity.

Table 3.
Multivariate adjusted associations of potential determinants with the latent class of physical activity.
3.2.1. Steadily Medium, Low and Very Low Trajectories
Based on multivariate models, participants in the ‘steadily very low’ trajectory were more often older (odds ratio (OR) = 2.22, 95%-confidence interval 1.94–2.54, per 10 years of age increase), lower educated (e.g., OR = 3.64, 2.45–5.40 for primary versus higher education), and less often retired (OR = 0.38, 0.27–0.53, versus employed) (Table 3). Regarding health status, participants with poorer self-perceived health (e.g., OR = 8.56, 6.08–12.08 for poor/fair health versus very good/excellent health) or more depressive symptoms (OR = 1.13, 1.09–1.17, per point increase on CES-D scale) more often belonged to the ‘steadily very low’ trajectory. In contrast, in multivariable models, those with more anxiety symptoms less often belonged to the ‘steadily very low’ trajectory (OR = 0.90, 0.86–0.94, per point increase on HADS scale). Regarding lifestyle factors, participants who reported to eat less healthy during the pandemic also more often reported ‘steadily very low’ physical activity levels (OR = 2.17, 1.44–3.27, versus those who ate as healthy as before), even as participants who smoked (OR = 2.30, 1.73–3.05, versus non-smokers), whereas participants who used more alcohol were less likely to be in the ‘steadily very low’ trajectory (OR = 0.89, 0.82–0.96, per glass of alcohol per day).
Associations of potential determinants with the ‘steadily medium’ and ‘steadily low’ trajectories showed effect estimates in the same direction. Effect sizes were largest for the ‘steadily very low’, followed by the ‘steadily low’ and ‘steadily medium’ trajectory (Table 3).
In sex- and age adjusted models, associations were largely in the same direction (Table 2). However, without adjustment for the other potential determinants, participants with more anxiety symptoms were more likely instead of less likely to be in a trajectory representing lower levels of physical activity (e.g., for the ‘steadily very low’ trajectory, OR = 1.09, 1.06–1.12, per point on HADS scale). The change in direction in multivariate models was mainly explained by mutual adjustment for depressive symptoms. In sex- and age adjusted models, we also observed that women and unemployed participants were more often in trajectories with lower physical activity levels (Table 2), but these associations were explained by other variables in the multivariate analysis.
3.2.2. Increasers
In multivariate models, we observed that lower educated participants (OR = 1.94, 1.13–1.35 for primary, versus higher education), and participants with poorer health (e.g., OR = 1.96, 1.17–3.30 for poor/fair health, versus very good/excellent health) were more likely to be in the ‘increasers’ trajectory, although effect sizes were smaller as compared to the ‘steadily medium’, ‘steadily low’ and ‘steadily very low’ trajectories (Table 3). Moreover, participants with more depressive symptoms (OR = 1.06, 1.01–1.11, per point increase on CES-D scale), and more worries about the pandemic (OR = 1.07, 1.01–1.14, per point on 10-point Likert scale) more often belonged to the ‘increasers’ trajectory, while participants with more anxiety symptoms (OR = 0.93, 0.87–0.99, per point increase on HADS scale) were less often in the ‘increasers’ trajectory.
Again, associations were largely similar to the sex- and age adjusted models, except for anxiety symptoms (Table 2).
In post hoc analyses we additionally compared the ‘increasers’ trajectory with the ‘steadily low’ trajectory as reference, as these trajectories start at the same baseline physical activity level. In multivariate models, we observed that older participants (OR = 0.62, 0.51–0.75, per 10 years of age increase), lower educated participants (e.g., OR = 0.62, 0.44–0.88 for lower education, versus higher education) and those who reported poor/fair health (OR = 0.50, 0.30–0.84, versus very good/excellent health) were less often in the ‘increasers’ trajectory than in the ‘steadily low’ trajectory (Supplementary Table S3).
3.3. Sensitivity Analysis
After exclusion of participants who reported a COVID-19 infection during the study period (n = 92), results did not change (data not shown).
4. Discussion
In this large population-based cohort of middle-aged and elderly individuals, the majority of participants reported less than 150 min of moderate and vigorous physical activity in the past 14 days, meaning that they did not meet the WHO physical activity guidelines [25]. Five distinct trajectories of physical activity over a 6-week period during the pandemic were identified. Four trajectories were relatively steady over time, although a slight increase was shown in each group. The fifth group started at a low physical activity level, but increased steeply over time. We identified determinants of these trajectories relating to demographics, physical health, psychosocial health and lifestyle.
Various studies have found a significant drop in physical activity levels during the pandemic compared to before [5,6,26]. We could not directly make this comparison due to lack of information on physical activity levels before the pandemic from the same study sample. Although, according to national data on physical activity levels in the Netherlands in 2019, 49% of the adult population did not meet physical activity guidelines prior to the pandemic, while at least 59.4% of the participants in our study did not meet these guidelines, which indeed suggests a drop in physical activity levels during the pandemic compared to before [27]. In line with our findings, studies that determined physical activity levels after the start of the pandemic found that average physical activity levels either remained stable or increased over time [5,6,28]. The steady levels of physical activity that we observed could be explained by the fact that the restrictive measures in the Netherlands have not changed during our study period. Also, restrictive measures in the Netherlands were relatively mild, i.e., individuals were allowed to go outside for unlimited time to perform physical activity during the pandemic. Previously, Tison et al. have shown that the severity of restrictive measures was of large impact on physical activity in terms of step counts [6]. For example, in Italy, which had a full lockdown, a decrease of 48.7% was measured while in Sweden, which had less strict restrictive measures, a decrease of only 6.9% was observed. As restrictive measures were fixed during our study period, we assume that participants have been able to maintain their physical activity levels during our study period.
The determinants we identified are largely in line with determinants of physical inactivity in general. Furthermore, as most trajectories in our population were stable over time, we presume that identified determinants are representatives of both baseline physical activity and the trajectories. In line with previous findings, we identified demographic and physical health determinants of physical activity trajectories such as older age, lower socioeconomic status and poorer health/disabilities [25,29]. Also, more depressive symptoms were associated with lower physical activity levels in our study, which is in line with previous findings before and during pandemic [30,31,32]. Remarkably, anxiety symptoms were associated with lower trajectories of physical activity in the sex- and age adjusted model, but with higher trajectories in the multivariate model. This change in direction was mainly explained by mutual adjustment for depressive symptoms. We might speculate that anxiety may have been a trigger to be physically active during the pandemic as a healthy lifestyle was suggested to be protective against severe symptoms of COVID-19. Regarding lifestyle factors, those who reported consuming a (much) less healthy diet compared to before the pandemic were more often in trajectories with lower levels of physical activity. This emphasizes the co-occurrence of unhealthy lifestyle factors and the need for combined lifestyle interventions. Also smoking was associated with lower trajectories of physical activity, while alcohol consumption was associated with higher trajectories of physical activity, which is both in line with previous findings [33,34]. The determinants we could assess were all on the individual level. However, from a social-ecological perspective, determinants on other levels, such as interpersonal, organizational and policy factors, may also affect population physical activity levels [14,15,16]. Future studies are warranted to study the additional and interrelating effects of these higher levels factors on individuals’ physical activity during the pandemic.
Determinants of lower trajectories of physical activity during the pandemic largely overlap with those established before the pandemic, emphasizing that these groups are also more vulnerable under these unusual circumstances. Moreover, many of these determinants may also be direct risk factors for chronic diseases in general and specifically to the severity of COVID-19 symptoms. This could lead to enhanced health inequities due to the pandemic. Also, we have shown again that other poor lifestyle factors relate to lower levels of physical activity, which emphasizes the urge for combined interventions to these groups at higher risk of poorer health and lifestyle.
Strengths of this study include the relatively large sample size, repeated measures of physical activity during the pandemic, and the embeddedness within a population-based cohort which might enhance the representativeness of the sample. However, several limitations should be taken into account when interpreting the results. First, physical activity levels could not be directly compared to levels before the pandemic. Second, physical activity was self-reported and measured based on a single question with categorical answer options. Therefore, estimates of physical activity levels may be inaccurate due to e.g., recall bias and categorical answer options may have led to loss of information. Lastly, over the 6-week period that physical activity levels were assessed in this study, restrictive measures in the Netherlands have not changed substantially. Therefore, we could not report on physical activity levels when the restrictions were lifted. This is of particular importance and should be investigated by future studies, as it would give information on whether individuals are able to return to their physical activity levels as they were before the pandemic, or whether it is difficult for people to get back to these levels which might be a call for public health strategies.
5. Conclusions
In this population-based study in the Netherlands, we observed low physical activity levels during the COVID-19 pandemic, with most subjects not adhering to physical activity guidelines. For most individuals, the trajectories over a 6-week period after the first restrictive measures were announced remained relatively stable over time during the pandemic, except for a small group of participants that increased their physical activity levels. Determinants of these trajectories included demographics, physical and psychosocial health, and lifestyle factors. More specifically, older, lower educated, and those reporting poorer physical health and lifestyle, and more depressive symptoms were more often in trajectories representing lower levels of physical activity. These groups may therefore require additional preventive interventions to promote physical activity.
Supplementary Materials
The following are available online at https://www.mdpi.com/article/10.3390/nu13113832/s1, Table S1: Descriptive information on physical activity of each time point, Table S2: Study sample characteristics per trajectory of physical activity, Table S3: Multivariate adjusted associations of potential determinants for the ‘increasers’ trajectory.
Author Contributions
Conceptualization, A.H., M.A.M.L., T.O.E.d.C., A.I.L. and T.V.; Formal analysis, A.H., M.A.M.L., T.O.E.d.C., A.I.L. and T.V.; Writing—Original Draft Preparation, A.H., M.A.M.L. and T.O.E.d.C.; Writing—Review & Editing, A.I.L., M.A.I. and T.V., Supervision, A.I.L., M.A.I. and T.V. All authors have read and agreed to the published version of the manuscript.
Funding
The Rotterdam Study is funded by Erasmus Medical Center and Erasmus University, Rotterdam, Netherlands Organization for the Health Research and Development (ZonMw), the Research Institute for Diseases in the Elderly (RIDE), the Ministry of Education, Culture and Science, the Ministry for Health, Welfare and Sports, the European Commission (DG XII), and the Municipality of Rotterdam.
Institutional Review Board Statement
The Rotterdam Study has been approved by the Medical Ethics Committee of the Erasmus MC (registration number MEC 02.1015) and by the Dutch Ministry of Health, Welfare and Sport (Population Screening Act WBO, license number 1071272-159521-PG). The Rotterdam Study Personal Registration Data collection is filed with the Erasmus MC Data Protection Officer under registration number EMC1712001. The Rotterdam Study has been entered into the Netherlands National Trial Register (NTR; www.trialregister.nl) and into the WHO International Clinical Trials Registry Platform (ICTRP; www.who.int/ictrp/network/primary/en/) under shared catalogue number NTR6831.
Informed Consent Statement
All participants provided written informed consent to participate in the study and to have their information obtained from treating physicians.
Data Availability Statement
Data can be obtained upon request. Requests should be directed towards the management team of the Rotterdam Study (secretariat.epi@erasmusmc.nl), which has a protocol for approving data requests. Because of restrictions based on privacy regulations and informed consent of the participants, data cannot be made freely available in a public repository.
Acknowledgments
We acknowledge the dedication, commitment, and contribution of inhabitants, general practitioners, and pharmacists of the Ommoord district who took part in the Rotterdam Study. We thank the research staff for organizing the COVID-19 substudy. We thank Sven Geurts, Maud F. de Feijter, Michelle M.J. Mens, Niels van der Schaft and Frank J. Wolters for their valuable contribution to cleaning of the data.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Freiberg, A.; Schubert, M.; Starke, K.R.; Hegewald, J.; Seidler, A. A rapid review on the influence of COVID-19 lockdown and quarantine measures on modifiable cardiovascular risk factors in the general population. Int. J. Environ. Res. Public Health 2021, 18, 8567. [Google Scholar] [CrossRef]
- Ekelund, U.; Tarp, J.; Steene-Johannessen, J.; Hansen, B.H.; Jefferis, B.; Fagerland, M.W.; Whincup, P.; Diaz, K.M.; Hooker, S.P.; Chernofsky, A.; et al. Dose-response associations between accelerometry measured physical activity and sedentary time and all cause mortality: Systematic review and harmonised meta-analysis. BMJ 2019, 366, l4570. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Warburton, D.E.R.; Bredin, S.S.D. Health benefits of physical activity: A systematic review of current systematic reviews. Curr. Opin. Cardiol. 2017, 32, 541–556. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Physical Activity Strategy for the Who European Region 2016–2025; World Health Organization: Geneva, Switzerland, 2016. [Google Scholar]
- McCarthy, H.; Potts, H.W.W.; Fisher, A. Physical activity behavior before, during, and after COVID-19 restrictions: Longitudinal smartphone-tracking study of adults in the united kingdom. J. Med. Internet Res. 2021, 23, e23701. [Google Scholar] [CrossRef] [PubMed]
- Tison, G.H.; Avram, R.; Kuhar, P.; Abreau, S.; Marcus, G.M.; Pletcher, M.J.; Olgin, J.E. Worldwide effect of COVID-19 on physical activity: A descriptive study. Ann. Intern. Med. 2020, 173, 767–770. [Google Scholar] [CrossRef]
- Caputo, E.L.; Reichert, F.F. Studies of physical activity and COVID-19 during the pandemic: A scoping review. J. Phys. Act. Health 2020, 17, 1275–1284. [Google Scholar] [CrossRef] [PubMed]
- Hamer, M.; Kivimäki, M.; Gale, C.R.; Batty, G.D. Lifestyle risk factors, inflammatory mechanisms, and COVID-19 hospitalization: A community-based cohort study of 387,109 adults in uk. Brain Behav. Immun. 2020, 87, 184–187. [Google Scholar] [CrossRef] [PubMed]
- Callow, D.D.; Arnold-Nedimala, N.A.; Jordan, L.S.; Pena, G.S.; Won, J.; Woodard, J.L.; Smith, J.C. The mental health benefits of physical activity in older adults survive the COVID-19 pandemic. Am. J. Geriatr. Psychiatry 2020, 28, 1046–1057. [Google Scholar] [CrossRef] [PubMed]
- Faulkner, J.; O’Brien, W.J.; McGrane, B.; Wadsworth, D.; Batten, J.; Askew, C.D.; Badenhorst, C.; Byrd, E.; Coulter, M.; Draper, N.; et al. Physical activity, mental health and well-being of adults during initial COVID-19 containment strategies: A multi-country cross-sectional analysis. J. Sci. Med. Sport 2021, 24, 320–326. [Google Scholar] [CrossRef]
- Ikram, M.A.; Brusselle, G.; Ghanbari, M.; Goedegebure, A.; Ikram, M.K.; Kavousi, M.; Kieboom, B.C.T.; Klaver, C.C.W.; de Knegt, R.J.; Luik, A.I.; et al. Objectives, design and main findings until 2020 from the rotterdam study. Eur. J. Epidemiol. 2020, 35, 483–517. [Google Scholar] [CrossRef] [PubMed]
- Licher, S.; Terzikhan, N.; Splinter, M.J.; Velek, P.; van Rooij, F.J.A.; Heemst, J.V.; Haarman, A.E.G.; Thee, E.F.; Geurts, S.; Mens, M.M.J.; et al. Design, implementation and initial findings of COVID-19 research in the rotterdam study: Leveraging existing infrastructure for population-based investigations on an emerging disease. Eur. J. Epidemiol. 2021, 36, 649–654. [Google Scholar] [CrossRef]
- Mc Intyre, K.; Lanting, P.; Deelen, P.; Wiersma, H.H.; Vonk, J.M.; Ori, A.P.S.; Jankipersadsing, S.A.; Warmerdam, R.; van Blokland, I.; Boulogne, F.; et al. Lifelines COVID-19 cohort: Investigating COVID-19 infection and its health and societal impacts in a dutch population-based cohort. BMJ Open 2021, 11, e044474. [Google Scholar] [CrossRef] [PubMed]
- Sallis, J.F.; Cervero, R.B.; Ascher, W.; Henderson, K.A.; Kraft, M.K.; Kerr, J. An ecological approach to creating active living communities. Annu. Rev. Public Health 2006, 27, 297–322. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sallis, J.F.; Owen, N.; Fisher, E. Ecological models of health behavior. In Health Behavior: Theory, Research, and Practice, 5th ed.; John Wiley & Sons: Hoboken, NJ, USA, 2015. [Google Scholar]
- Yen, H.Y.; Li, C. Determinants of physical activity: A path model based on an ecological model of active living. PLoS ONE 2019, 14, e0220314. [Google Scholar] [CrossRef] [Green Version]
- Brandão, M.P.; Fonseca Cardoso, M. Associations between depressive symptoms and being employed or retired in older adults with type 2 diabetes. Prim. Care Diabetes 2020, 14, 464–468. [Google Scholar] [CrossRef] [PubMed]
- Beekman, A.T.; Deeg, D.J.; Van Limbeek, J.; Braam, A.W.; De Vries, M.Z.; Van Tilburg, W. Criterion validity of the center for epidemiologic studies depression scale (ces-d): Results from a community-based sample of older subjects in the netherlands. Psychol. Med. 1997, 27, 231–235. [Google Scholar] [CrossRef] [Green Version]
- Radloff, L.S. The ces-d scale: A self-report depression scale for research in the general population. Appl. Psychol. Meas. 1977, 1, 385–401. [Google Scholar] [CrossRef]
- Herrmann, C. International experiences with the hospital anxiety and depression scale-a review of validation data and clinical results. J. Psychosom. Res. 1997, 42, 17–41. [Google Scholar] [CrossRef]
- Zigmond, A.S.; Snaith, R.P. The hospital anxiety and depression scale. Acta Psychiatr. Scand. 1983, 67, 361–370. [Google Scholar] [CrossRef] [Green Version]
- Clotworthy, A.; Dissing, A.S.; Nguyen, T.-L.; Jensen, A.K.; Andersen, T.O.; Bilsteen, J.F.; Elsenburg, L.K.; Keller, A.; Kusumastuti, S.; Mathisen, J.; et al. ‘Standing together—At a distance’: Documenting changes in mental-health indicators in denmark during the COVID-19 pandemic. Scand. J. Public Health 2021, 49, 79–87. [Google Scholar] [CrossRef] [PubMed]
- Varga, T.V.; Bu, F.; Dissing, A.S.; Elsenburg, L.K.; Bustamante, J.J.H.; Matta, J.; van Zon, S.K.R.; Brouwer, S.; Bültmann, U.; Fancourt, D.; et al. Loneliness, worries, anxiety, and precautionary behaviours in response to the COVID-19 pandemic: A longitudinal analysis of 200,000 western and northern europeans. Lancet Reg. Health—Eur. 2021, 2, 100020. [Google Scholar] [CrossRef] [PubMed]
- Ingram, J.; Maciejewski, G.; Hand, C.J. Changes in diet, sleep, and physical activity are associated with differences in negative mood during COVID-19 lockdown. Front. Psychol. 2020, 11, 588604. [Google Scholar] [CrossRef] [PubMed]
- Bull, F.C.; Al-Ansari, S.S.; Biddle, S.; Borodulin, K.; Buman, M.P.; Cardon, G.; Carty, C.; Chaput, J.-P.; Chastin, S.; Chou, R.; et al. World health organization 2020 guidelines on physical activity and sedentary behaviour. Br. J. Sports Med. 2020, 54, 1451. [Google Scholar] [CrossRef]
- López-Bueno, R.; Calatayud, J.; Andersen, L.L.; Balsalobre-Fernández, C.; Casaña, J.; Casajús, J.A.; Smith, L.; López-Sánchez, G.F. Immediate impact of the COVID-19 confinement on physical activity levels in spanish adults. Sustainability 2020, 12, 5708. [Google Scholar] [CrossRef]
- CBS; RIVM. Gezondheidsenquete/Leefstijlmonitor. Available online: https://www.rivm.nl/leefstijlmonitor/bewegen (accessed on 14 October 2021).
- Castañeda-Babarro, A.; Arbillaga-Etxarri, A.; Gutiérrez-Santamaría, B.; Coca, A. Physical activity change during COVID-19 confinement. Int. J. Environ. Res. Public Health 2020, 17, 6878. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Global Action Plan on Physical Activity 2018–2030: More Active People for a Healthier World; World Health Organization: Geneva, Switzerland, 2019. [Google Scholar]
- Rebar, A.L.; Stanton, R.; Geard, D.; Short, C.; Duncan, M.J.; Vandelanotte, C. A meta-meta-analysis of the effect of physical activity on depression and anxiety in non-clinical adult populations. Health Psychol. Rev. 2015, 9, 366–378. [Google Scholar] [CrossRef]
- Robinson, E.; Boyland, E.; Chisholm, A.; Harrold, J.; Maloney, N.G.; Marty, L.; Mead, B.R.; Noonan, R.; Hardman, C.A. Obesity, eating behavior and physical activity during COVID-19 lockdown: A study of uk adults. Appetite 2021, 156, 104853. [Google Scholar] [CrossRef] [PubMed]
- Schuch, F.B.; Vancampfort, D.; Firth, J.; Rosenbaum, S.; Ward, P.B.; Silva, E.S.; Hallgren, M.; Ponce De Leon, A.; Dunn, A.L.; Deslandes, A.C.; et al. Physical activity and incident depression: A meta-analysis of prospective cohort studies. Am. J. Psychiatry 2018, 175, 631–648. [Google Scholar] [CrossRef] [PubMed]
- Dodge, T.; Clarke, P.; Dwan, R. The relationship between physical activity and alcohol use among adults in the united states: A systematic review of the literature. Am. J. Health Promot. 2017, 31, 97–108. [Google Scholar] [CrossRef] [PubMed]
- Kaczynski, A.T.; Manske, S.R.; Mannell, R.C.; Grewal, K. Smoking and physical activity: A systematic review. Am. J. Health Behav. 2008, 32, 93–110. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).