Effects of Sarcopenic Obesity and Its Confounders on Knee Range of Motion Outcome after Total Knee Replacement in Older Adults with Knee Osteoarthritis: A Retrospective Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
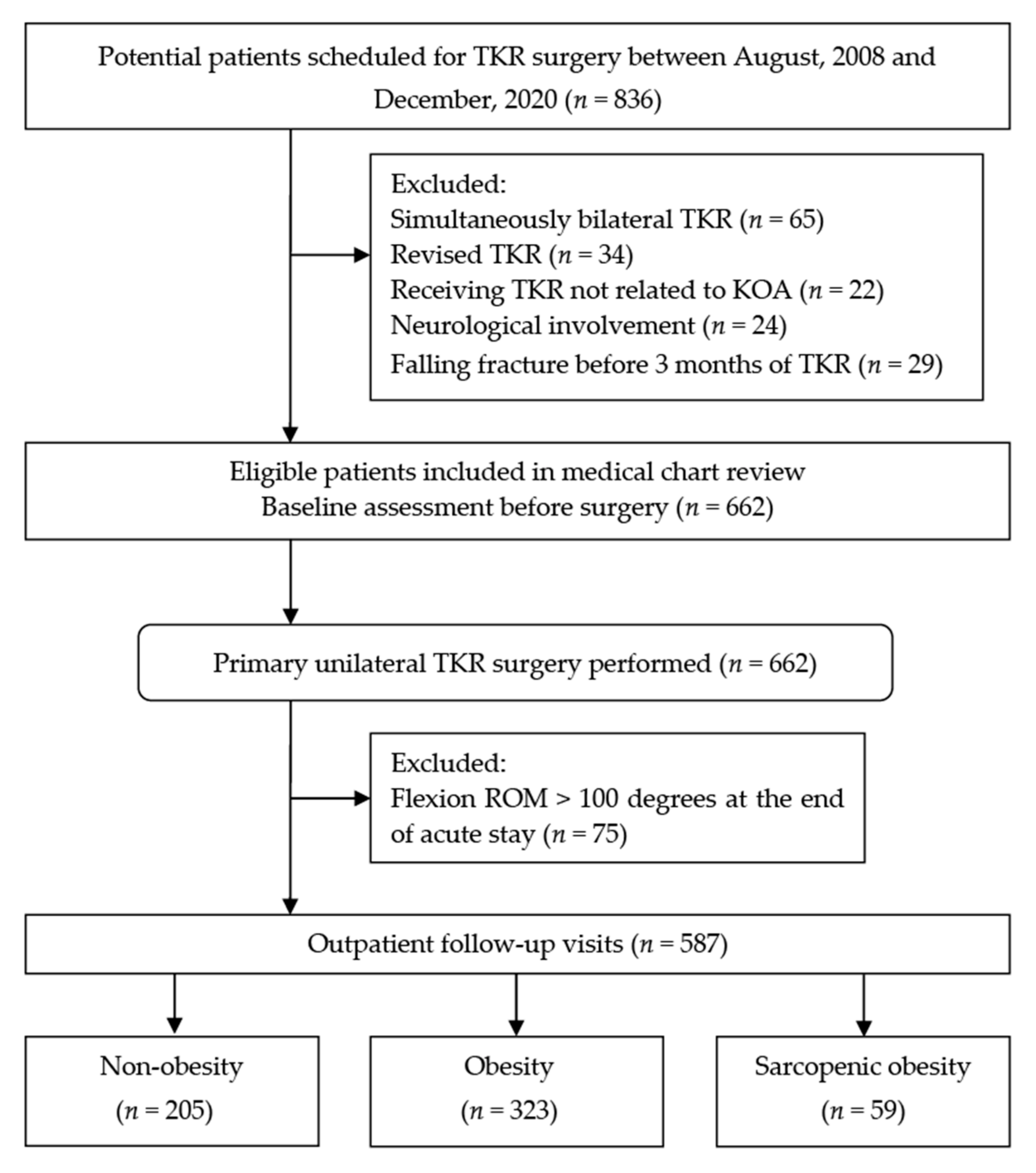
2.2. Participants
2.3. Assessment of Nutritional Status and Risk of Undernutrition
2.4. Identification of Sarcopenic Obesity
female = 2) − 0.037 × age (year) − 2.631
2.5. Measurement and Follow up of Knee Flexion Range of Motion
2.6. Identification of Poor Surgical Outcome
2.7. Statistical Analysis
3. Results
3.1. Patient Demographics and Clinical Characteristics
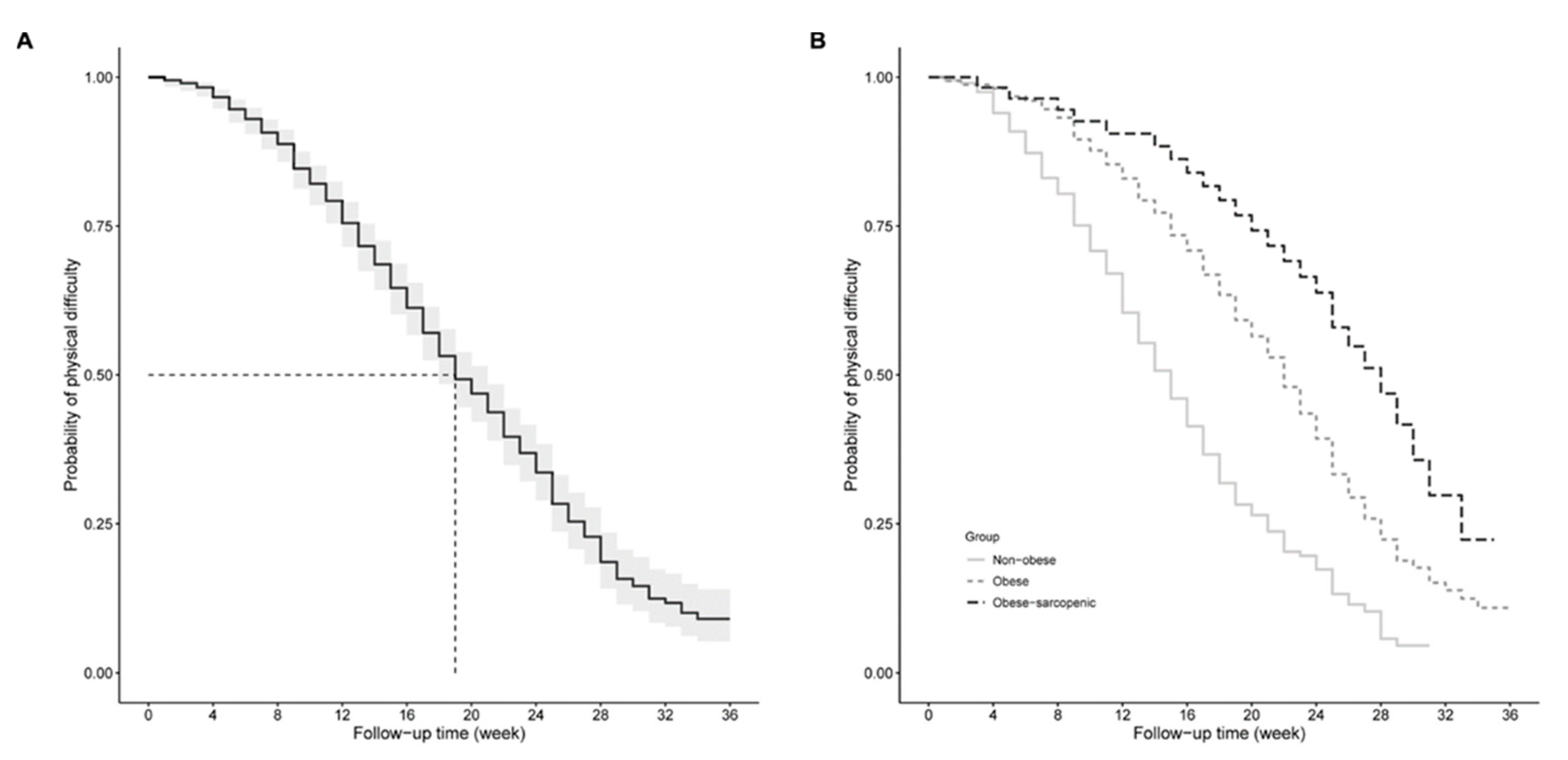
3.2. Survival Time for ROM Recovery after TKR
3.3. Associations of Sarcopenic Obesity with ROM Restoration following TKR
4. Discussion
4.1. Summary of the Main Findings
4.2. Demographics and Characteristics in the Study Cohort
4.3. Prevalence of Sarcopenic Obesity and Nutritional Status in End-Stage Knee Osteoarthritis
4.4. Obesity and Range of Motion in Knee Osteoarthritis
4.5. Sarcopenic Obesity and Its Risk of Poor Recovery in Range of Motion after Total Knee Replacement
4.6. Study Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Jester, R.; Rodney, A. The relationship between obesity and primary Total Knee Replacement: A scoping review of the literature. Int. J. Orthop. Trauma Nurs. 2021, 42, 100850. [Google Scholar] [CrossRef] [PubMed]
- Pishgar, F.; Guermazi, A.; Ashraf-Ganjouei, A.; Haj-Mirzaian, A.; Roemer, F.W.; Zikria, B.; Sereni, C.; Hakky, M.; Demehri, S. Association between Patellofemoral and medial Tibiofemoral compartment osteoarthritis progression: Exploring the effect of body weight using longitudinal data from osteoarthritis initiative (OAI). Skelet. Radiol. 2021, 1–10. [Google Scholar] [CrossRef]
- Haase, C.L.; Eriksen, K.T.; Lopes, S.; Satylganova, A.; Schnecke, V.; McEwan, P. Body mass index and risk of obesity-related conditions in a cohort of 2.9 million people: Evidence from a UK primary care database. Obes Sci Pract. 2021, 7, 137–147. [Google Scholar] [CrossRef]
- Munugoda, I.; Wills, K.; Cicuttini, F.; Graves, S.; Lorimer, M.; Jones, G.; Callisaya, M.; Aitken, D. The association between ambulatory activity, body composition and hip or knee joint replacement due to osteoarthritis: A prospective cohort study. Osteoarthr. Cartil. 2018, 26, 671–679. [Google Scholar] [CrossRef] [PubMed]
- Lim, Y.Z.; Wang, Y.; Cicuttini, F.M.; Giles, G.G.; Graves, S.; Wluka, A.E.; Hussain, S.M. Obesity defined by body mass index and waist circumference and risk of total knee arthroplasty for osteoarthritis: A prospective cohort study. PLoS ONE 2021, 16, e0245002. [Google Scholar] [CrossRef]
- Vasarhelyi, E.M.; Macdonald, S.J. Obesity and Total Joint Arthroplast. Semin. Arthroplast. 2012, 23, 10–12. [Google Scholar] [CrossRef]
- Liao, C.-D.; Huang, Y.-C.; Chiu, Y.-S.; Liou, T.-H. Effect of body mass index on knee function outcomes following continuous passive motion in patients with osteoarthritis after total knee replacement: A retrospective study. Physiotherapy 2017, 103, 266–275. [Google Scholar] [CrossRef]
- Xu, S.; Chen, J.Y.; Lo, N.N.; Chia, S.L.; Tay, D.K.J.; Pang, H.N.; Hao, Y.; Yeo, S.J. The influence of obesity on functional outcome and quality of life after total knee arthroplasty: A ten-year follow-up study. Bone Joint, J. 2018, 100, 579–583. [Google Scholar] [CrossRef]
- Kornuijt, A.; De Kort, G.J.L.; Das, D.; Lenssen, A.F.; Van Der Weegen, W. Recovery of knee range of motion after total knee arthroplasty in the first postoperative weeks: Poor recovery can be detected early. Musculoskelet. Surg. 2019, 103, 289–297. [Google Scholar] [CrossRef]
- Wimmer, M.A.; Nechtow, W.; Schwenke, T.; Moisio, K.C. Knee Flexion and Daily Activities in Patients following Total Knee Replacement: A Comparison with ISO Standard 14243. BioMed Res. Int. 2015, 2015, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Ito, H.; Ichihara, K.; Tamari, K.; Amano, T.; Tanaka, S.; Uchida, S.; Morikawa, S. Determination of reference intervals for knee motor functions specific to patients undergoing knee Arthroplast. PLoS ONE 2021, 16, e0249564. [Google Scholar] [CrossRef]
- Miner, A.L.; Lingard, E.A.; Wright, E.A.; Sledge, C.B.; Katz, J.N. Knee range of motion after total knee arthroplasty: How important is this as an outcome measure? J. Arthroplast. 2003, 18, 286–294. [Google Scholar] [CrossRef]
- Stratford, P.; Kennedy, D.M.; Robarts, S.F. Modelling Knee Range of Motion Post Arthroplasty: Clinical Applications. Physiother. Can. 2010, 62, 378–387. [Google Scholar] [CrossRef]
- Razak, H.R.B.A.; Chong, H.C.; Tan, A.H.C. Obesity Does Not Imply Poor Outcomes in Asians after Total Knee Arthroplast. Clin. Orthop. Relat. Res. 2013, 471, 1957–1963. [Google Scholar] [CrossRef]
- Bonnefoy-Mazure, A.; Martz, P.; Armand, S.; Sagawa, Y.; Suva, D.; Turcot, K.; Miozzari, H.H.; Lübbeke, A. Influence of Body Mass Index on Sagittal Knee Range of Motion and Gait Speed Recovery 1-Year After Total Knee Arthroplast. J. Arthroplast. 2017, 32, 2404–2410. [Google Scholar] [CrossRef] [PubMed]
- Vasarhelyi, E.M.; Macdonald, S.J.; Munro, J.T.; Garbuz, D.S.; Masri, B.A.; Duncan, C.P. The influence of obesity on total joint Arthroplast. J. Bone Jt. Surg. Br. Vol. 2012, 94, 100–102. [Google Scholar] [CrossRef] [PubMed]
- Gillespie, G.; Porteous, A. Obesity and knee Arthroplast. Knee 2007, 14, 81–86. [Google Scholar] [CrossRef] [PubMed]
- Zeni, J.A.; Snyder-Mackler, L. Early Postoperative Measures Predict 1- and 2-Year Outcomes After Unilateral Total Knee Arthroplasty: Importance of Contralateral Limb Strength. Phys. Ther. 2010, 90, 43–54. [Google Scholar] [CrossRef]
- Park, K.K.; Chang, C.B.; Kang, Y.G.; Seong, S.C.; Kim, T.K. Correlation of maximum flexion with clinical outcome after total knee replacement in Asian patients. J. Bone Jt. Surg. Br. Vol. 2007, 89, 604–608. [Google Scholar] [CrossRef]
- Meneghini, R.M.; Pierson, J.L.; Bagsby, D.; Ziemba-Davis, M.; Berend, M.E.; Ritter, M.A. Is there a functional benefit to obtaining high flexion after total knee arthroplasty? J Arthroplast. 2007, 22, 43–46. [Google Scholar] [CrossRef]
- Devers, B.N.; Conditt, M.A.; Jamieson, M.L.; Driscoll, M.D.; Noble, P.C.; Parsley, B.S. Does greater knee flexion increase patient function and satisfaction after total knee arthroplasty? J Arthroplast. 2011, 26, 178–186. [Google Scholar] [CrossRef] [PubMed]
- Papalia, R.; Zampogna, B.; Torre, G.; Lanotte, A.; Vasta, S.; Albo, E.; Tecame, A.; Denaro, V. Sarcopenia and its relationship with osteoarthritis: Risk factor or direct consequence? Musculoskelet Surg. 2014, 98, 9–14. [Google Scholar] [CrossRef] [PubMed]
- Karlsson, M.; Magnusson, H.; Cöster, M.; Karlsson, C.; Rosengren, B. Patients With Knee Osteoarthritis Have a Phenotype With Higher Bone Mass, Higher Fat Mass, and Lower Lean Body Mass. Clin. Orthop. Relat. Res. 2015, 473, 258–264. [Google Scholar] [CrossRef]
- Kemnitz, J.; Wirth, W.; Eckstein, F.; Culvenor, A. The role of thigh muscle and adipose tissue in knee osteoarthritis progression in women: Data from the Osteoarthritis Initiative. Osteoarthr. Cartil. 2018, 26, 1190–1195. [Google Scholar] [CrossRef] [PubMed]
- Jin, W.S.; Choi, E.J.; Lee, S.Y.; Bae, E.J.; Lee, T.H.; Park, J. Relationships among Obesity, Sarcopenia, and Osteoarthritis in the Elderly. J. Obes. Metab. Syndr. 2017, 26, 36–44. [Google Scholar] [CrossRef]
- Kim, B.S.; Lee, S.Y.; Kim, B.R.; Choi, J.H.; Kim, S.R.; Lee, H.J.; Lee, S.J. Associations Between Obesity with Low Muscle Mass and Physical Function in Patients with End-Stage Knee Osteoarthritis. Geriatr. Orthop. Surg. Rehabil. 2021, 12, 21514593211020700. [Google Scholar] [CrossRef]
- Godziuk, K.; Prado, C.; Woodhouse, L.; Forhan, M. Prevalence of sarcopenic obesity in adults with end-stage knee osteoarthritis. Osteoarthr. Cartil. 2019, 27, 1735–1745. [Google Scholar] [CrossRef]
- Rossi, A.P.; Urbani, S.; Fantin, F.; Nori, N.; Brandimarte, P.; Martini, A.; Zoico, E.; Mazzali, G.; Babbanini, A.; Muollo, V.; et al. Worsening Disability and Hospitalization Risk in Sarcopenic Obese and Dynapenic Abdominal Obese: A 5.5 Years Follow-Up Study in Elderly Men and Women. Front. Endocrinol. 2020, 11, 314. [Google Scholar] [CrossRef]
- Gao, Q.; Mei, F.; Shang, Y.; Hu, K.; Chen, F.; Zhao, L.; Ma, B. Global prevalence of sarcopenic obesity in older adults: A systematic review and meta-analysis. Clin. Nutr. 2021, 40, 4633–4641. [Google Scholar] [CrossRef]
- Misra, D.; Fielding, R.A.; Felson, D.T.; Niu, J.; Brown, C.; Nevitt, M.; Lewis, C.E.; Torner, J.; Neogi, T.; the MOST study. Risk of Knee Osteoarthritis with Obesity, Sarcopenic Obesity, and Sarcopenia. Arthritis Rheumatol. 2019, 71, 232–237. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.; Kim, T.N.; Kim, S.-H. Sarcopenic obesity is more closely associated with knee osteoarthritis than is nonsarcopenic obesity: A cross-sectional study. Arthritis Rheum. 2012, 64, 3947–3954. [Google Scholar] [CrossRef]
- Jeanmaire, C.; Mazières, B.; Verrouil, E.; Bernard, L.; Guillemin, F.; Rat, A.-C. Body composition and clinical symptoms in patients with hip or knee osteoarthritis: Results from the KHOALA cohort. Semin. Arthritis Rheum. 2018, 47, 797–804. [Google Scholar] [CrossRef] [PubMed]
- Kennedy, D.M.; Hanna, S.E.; Stratford, P.; Wessel, J.; Gollish, J.D. Preoperative Function and Gender Predict Pattern of Functional Recovery After Hip and Knee Arthroplast. J. Arthroplast. 2006, 21, 559–566. [Google Scholar] [CrossRef] [PubMed]
- Fortin, P.R.; Clarke, A.E.; Joseph, L.; Liang, M.H.; Tanzer, M.; Ferland, D.; Phillips, C.; Partridge, A.J.; Fossel, A.H.; Mahomed, N.; et al. Outcomes of total hip and knee replacement: Preoperative functional status predicts outcomes at six months after surgery. Arthritis Rheum. 1999, 42, 1722–1728. [Google Scholar] [CrossRef]
- Parent, É.; Moffet, H. Preoperative predictors of locomotor ability two months after total knee arthroplasty for severe osteoarthritis. Arthritis Rheum. 2003, 49, 36–50. [Google Scholar] [CrossRef]
- Hopkins, S.J.; Toms, A.D.; Brown, M.; Welsman, J.R.; Ukoumunne, O.C.; Knapp, K.M. A study investigating short- and medium-term effects on function, bone mineral density and lean tissue mass post-total knee replacement in a Caucasian female post-menopausal population: Implications for hip fracture risk. Osteoporos. Int. 2016, 27, 2567–2576. [Google Scholar] [CrossRef]
- Kitsuda, Y.; Tanimura, C.; Inoue, K.; Park, D.; Osaki, M.; Hagino, H. Effectiveness of ultrasonographic skeletal muscle assessment in patients after total knee arthroplast. Osteoporos. Sarcopenia 2019, 5, 94–101. [Google Scholar] [CrossRef] [PubMed]
- Mizner, R.L.; Petterson, S.C.; Stevens, J.E.; Vandenborne, K.; Snyder-Mackler, L. Early quadriceps strength loss after total knee Arthroplast. The contributions of muscle atrophy and failure of voluntary muscle activation. J. Bone Jt. Surg. Am. 2005, 87, 1047–1053. [Google Scholar] [CrossRef] [PubMed]
- Petterson, S.C.; Barrance, P.; Marmon, A.R.; Handling, T.; Buchanan, T.S.; Snyder-Mackler, L. Time Course of Quad Strength, Area, and Activation after Knee Arthroplasty and Strength Training. Med. Sci. Sports Exerc. 2011, 43, 225–231. [Google Scholar] [CrossRef] [PubMed]
- Rasch, A.; Byström, A.H.; Dalén, N.; Martinez-Carranza, N.; Berg, H.E. Persisting muscle atrophy two years after replacement of the hip. J. Bone Jt. Surgy. Br. Vol. 2009, 91, 583–588. [Google Scholar] [CrossRef]
- Reardon, K.; Galea, M.; Dennett, X.; Choong, P.; Byrne, E. Quadriceps muscle wasting persists 5 months after total hip arthroplasty for osteoarthritis of the hip: A pilot study. Intern. Med. J. 2001, 31, 7–14. [Google Scholar] [CrossRef]
- Godziuk, K.; Prado, C.M.; Woodhouse, L.J.; Forhan, M. The impact of sarcopenic obesity on knee and hip osteoarthritis: A scoping review. BMC Musculoskelet Disord. 2018, 19, 271. [Google Scholar] [CrossRef]
- Wanaratna, K.; Muangpaisan, W.; Kuptniratsaikul, V.; Chalermsri, C.; Nuttamonwarakul, A. Prevalence and Factors Associated with Frailty and Cognitive Frailty among Community-Dwelling Elderly with Knee Osteoarthritis. J. Community Health 2019, 44, 587–595. [Google Scholar] [CrossRef]
- Courtney, P.M.; Boniello, A.J.; Berger, R.A. Complications Following Outpatient Total Joint Arthroplasty: An Analysis of a National Database. J. Arthroplast. 2017, 32, 1426–1430. [Google Scholar] [CrossRef] [PubMed]
- Gu, A.; Malahias, M.-A.; Strigelli, V.; Nocon, A.A.; Sculco, T.P.; Sculco, P.K. Preoperative Malnutrition Negatively Correlates With Postoperative Wound Complications and Infection after Total Joint Arthroplasty: A Systematic Review and Meta-Analysis. J. Arthroplast. 2019, 34, 1013–1024. [Google Scholar] [CrossRef] [PubMed]
- Hanada, M.; Hotta, K.; Matsuyama, Y. Prognostic nutritional index as a risk factor for aseptic wound complications after total knee arthroplast. J. Orthop. Sci. 2020, 26, 827–830. [Google Scholar] [CrossRef]
- Liao, C.-D.; Huang, Y.-C.; Lin, L.-F.; Huang, S.-W.; Liou, T.-H. Body Mass Index and Functional Mobility Outcome Following Early Rehabilitation after a Total Knee Replacement: A Retrospective Study in Taiwan. Arthritis Rheum. 2015, 67, 799–808. [Google Scholar] [CrossRef]
- Von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gøtzsche, P.C.; Vandenbroucke, J.P. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: Guidelines for reporting observational studies. Lancet 2007, 370, 1453–1457. [Google Scholar] [CrossRef]
- Abizanda Soler, P.; Paterna Mellinas, G.; Martinez Sanchez, E.; Lopez Jimenez, E. Comorbidity in the elderly: Utility and validity of assessment tools. Rev. Espanola. Geriatr. Gerontol. 2010, 45, 219–228. [Google Scholar] [CrossRef] [PubMed]
- Valderas, J.M.; Starfield, B.; Sibbald, B.; Salisbury, C.; Roland, M. Defining Comorbidity: Implications for Understanding Health and Health Services. Ann. Fam. Med. 2009, 7, 357–363. [Google Scholar] [CrossRef] [PubMed]
- Sinclair, S.T.; Emara, A.K.; Orr, M.N.; McConaghy, K.M.; Klika, A.K.; Piuzzi, N.S. Comorbidity indices in orthopaedic surgery: A narrative review focused on hip and knee Arthroplast. EFORT Open Rev. 2021, 6, 629–640. [Google Scholar] [CrossRef] [PubMed]
- Kaiser, M.J.; MNA-International Group; Bauer, J.M.; Ramsch, C.; Uter, W.; Guigoz, Y.; Cederholm, T.; Thomas, D.R.; Anthony, P.; Charlton, K.; et al. Validation of the Mini Nutritional Assessment short-form (MNA®-SF): A practical tool for identification of nutritional status. J. Nutr. Health Aging 2009, 13, 782–788. [Google Scholar] [CrossRef]
- Rubenstein, L.Z.; Harker, J.O.; Salvà, A.; Guigoz, Y.; Vellas, B. Screening for Undernutrition in Geriatric Practice: Developing the Short-Form Mini-Nutritional Assessment (MNA-SF). J. Gerontol. Ser. A Boil. Sci. Med. Sci. 2001, 56, M366–M372. [Google Scholar] [CrossRef]
- Zhang, X.; Zhang, X.; Zhu, Y.; Tao, J.; Zhang, Z.; Zhang, Y.; Wang, Y.; Ke, Y.; Ren, C.; Xu, J. Predictive Value of Nutritional Risk Screening 2002 and Mini Nutritional Assessment Short Form in Mortality in Chinese Hospitalized Geriatric Patients. Clin. Interv. Aging 2020, 15, 441–449. [Google Scholar] [CrossRef]
- Lilamand, M.; The Toulouse Frailty Platform Team; Kelaiditi, E.; Cesari, M.; Raynaud-Simon, A.; Ghisolfi, A.; Guyonnet, S.; Vellas, B.; Van Kan, G.A. Validation of the Mini Nutritional Assessment-Short Form in a population of frail elders without disability. Analysis of the Toulouse Frailty Platform population in 2013. J. Nutr. Health Aging 2015, 19, 570–574. [Google Scholar] [CrossRef] [PubMed]
- Soysal, P.; Veronese, N.; Arik, F.; Kalan, U.; Smith, L.; Isik, A.T. Mini Nutritional Assessment Scale-Short Form can be useful for frailty screening in older adults. Clin. Interv. Aging 2019, 14, 693–699. [Google Scholar] [CrossRef]
- Weir, C.B.; Jan, A. BMI Classification Percentile and Cut off Points; StatPearls Publishing LLC.: Treasure Island, FL, USA, 2021. [Google Scholar]
- Wen, X.; Wang, M.; Jiang, C.-M.; Zhang, Y.-M. Anthropometric equation for estimation of appendicular skeletal muscle mass in Chinese adults. Asia Pac. J. Clin. Nutr. 2011, 20, 551–556. [Google Scholar]
- Wu, X.; Li, X.; Xu, M.; Zhang, Z.; He, L.; Li, Y. Sarcopenia prevalence and associated factors among older Chinese population: Findings from the China Health and Retirement Longitudinal Study. PLoS ONE 2021, 16, e0247617. [Google Scholar] [CrossRef]
- Yang, M.; Hu, X.; Wang, H.; Zhang, L.; Hao, Q.; Dong, B. Sarcopenia predicts readmission and mortality in elderly patients in acute care wards: A prospective study. J. Cachex-Sarcopenia Muscle 2016, 8, 251–258. [Google Scholar] [CrossRef] [PubMed]
- Chen, L.-K.; Woo, J.; Assantachai, P.; Auyeung, T.-W.; Chou, M.-Y.; Iijima, K.; Jang, H.C.; Kang, L.; Kim, M.; Kim, S.; et al. Asian Working Group for Sarcopenia: 2019 Consensus Update on Sarcopenia Diagnosis and Treatment. J. Am. Med Dir. Assoc. 2020, 21, 300–307.e2. [Google Scholar] [CrossRef]
- Mehta, S.; Rigney, A.; Webb, K.; Wesney, J.; Stratford, P.W.; Shuler, F.D.; Oliashirazi, A. Characterizing the recovery trajectories of knee range of motion for one year after total knee replacement. Physiother. Theory Pr. 2018, 36, 176–185. [Google Scholar] [CrossRef] [PubMed]
- McClure, G.; Frisch, N.B. Range of Motion (ROM) after Knee Replacement Surgery: The Basics. Available online: https://peerwell.co/blog/range-of-motion-after-knee-replacement/ (accessed on 5 July 2017).
- Lenssen, A.F.; Van Dam, E.M.; Crijns, Y.H.; Verhey, M.; Geesink, R.J.; Brandt, P.A.V.D.; De Bie, R.A. Reproducibility of goniometric measurement of the knee in the in-hospital phase following total knee Arthroplast. BMC Musculoskelet Disord. 2007, 8, 83. [Google Scholar] [CrossRef]
- Hyodo, K.; Masuda, T.; Aizawa, J.; Jinno, T.; Morita, S. Hip, knee, and ankle kinematics during activities of daily living: A cross-sectional study. Braz. J. Phys. Ther. 2017, 21, 159–166. [Google Scholar] [CrossRef]
- Pfeiffer, J.L.; Zhang, S.; Milner, C.E. Knee biomechanics during popular recreational and daily activities in older men. Knee 2014, 21, 683–687. [Google Scholar] [CrossRef] [PubMed]
- Rowe, P.J.; Myles, C.M.; Walker, C.; Nutton, R. Knee joint kinematics in gait and other functional activities measured using flexible electrogoniometry: How much knee motion is sufficient for normal daily life? Gait Posture 2000, 12, 143–155. [Google Scholar] [CrossRef]
- Hoogeboom, T.J.; Van Meeteren, N.L.U.; Kim, R.H.; Stevens-Lapsley, J.E. Linear and Curvilinear Relationship between Knee Range of Motion and Physical Functioning in People with Knee Osteoarthritis: A Cross-Sectional Study. PLoS ONE 2013, 8, e76173. [Google Scholar] [CrossRef] [PubMed]
- Farahini, H.; Moghtadaei, M.; Bagheri, A.; Akbarian, E. Factors Influencing Range of Motion after Total Knee Arthroplast. Iran. Red Crescent Med. J. 2012, 14, 417–421. [Google Scholar]
- Hewlett-Smith, N.A.; Pope, R.P.; Hing, W.A.; Simas, V.P.; Furness, J.W. Patient and surgical prognostic factors for inpatient functional recovery following THA and TKA: A prospective cohort study. J. Orthop. Surg. Res. 2020, 15, 1–19. [Google Scholar] [CrossRef]
- Alzahrani, K.; Gandhi, R.; Debeer, J.; Petruccelli, D.; Mahomed, N. Prevalence of Clinically Significant Improvement Following Total Knee Replacement. J. Rheumatol. 2011, 38, 753–759. [Google Scholar] [CrossRef]
- Ritter, M.A.; Harty, L.D.; Davis, K.E.; Meding, J.B.; Berend, M.E. Predicting range of motion after total knee arthroplast. JBJS 2003, 85, 1278–1285. [Google Scholar] [CrossRef]
- Parsley, B.S.; Bertolusso, R.; Harrington, M.; Brekke, A.; Noble, P.C. Influence of Gender on Age of Treatment with TKA and Functional Outcome. Clin. Orthop. Relat. Res. 2010, 468, 1759–1764. [Google Scholar] [CrossRef] [PubMed]
- Naylor, J.M.; Ko, V.; Rougellis, S.; Green, N.; Mittal, R.; Heard, R.; Yeo, A.E.T.; Barnett, A.; Hackett, D.; Saliba, C.; et al. Is discharge knee range of motion a useful and relevant clinical indicator after total knee replacement? Part 2. J. Eval. Clin. Pr. 2011, 18, 652–658. [Google Scholar] [CrossRef]
- Elmallah, R.D.K.; Cherian, J.J.; Robinson, K.; Harwin, S.F.; Mont, M.A. The Effect of Comorbidities on Outcomes following Total Knee Arthroplast. J. Knee Surg. 2015, 28, 411–416. [Google Scholar] [CrossRef] [PubMed]
- Podmore, B.; Hutchings, A.; Van Der Meulen, J.; Aggarwal, A.; Konan, S. Impact of comorbid conditions on outcomes of hip and knee replacement surgery: A systematic review and meta-analysis. BMJ Open 2018, 8, e021784. [Google Scholar] [CrossRef] [PubMed]
- Harvey, I.A.; Barry, K.; Kirby, S.P.; Johnson, R.; Elloy, M.A. Factors affecting the range of movement of total knee Arthroplast. J. Bone Jt. Surg. 1993, 75, 950–955. [Google Scholar] [CrossRef]
- Kawamura, H.; Bourne, R.B. Factors affecting range of flexion after total knee Arthroplast. J. Orthop. Sci. 2001, 6, 248–252. [Google Scholar] [CrossRef] [PubMed]
- Fatima, M.; Scholes, C.; Tutty, A.; Ebrahimi, M.; Genon, M.; Martin, S.J. Outcomes following short hospital stay after total knee replacement in a regional setting: A prospective analysis of an observational cohort in a public hospital treated 2018–2019. medRxiv 2020. medRxiv: 2020.2003.2008.20031989. [Google Scholar]
- Font-Vizcarra, L.; Lozano, L.; Ríos, J.; Forga, M.T.; Soriano, A. Preoperative Nutritional Status and Post-Operative Infection in Total Knee Replacements: A Prospective Study of 213 Patients. Int. J. Artif. Organs 2011, 34, 876–881. [Google Scholar] [CrossRef]
- Alfargieny, R.; Bodalal, Z.; Bendardaf, R.; El-Fadli, M.; Langhi, S. Nutritional status as a predictive marker for surgical site infection in total joint Arthroplast. Avicenna J. Med. 2015, 5, 117–122. [Google Scholar] [CrossRef] [PubMed]
- Lavernia, C.J.; Sierra, R.J.; Baerga, L. Nutritional parameters and short term outcome in Arthroplast. J. Am. Coll. Nutr. 1999, 18, 274–278. [Google Scholar] [CrossRef]
- Cheng, Q.; Zhu, X.; Zhang, X.; Li, H.; Du, Y.; Hong, W.; Xue, S.; Zhu, H. A cross-sectional study of loss of muscle mass corresponding to sarcopenia in healthy Chinese men and women: Reference values, prevalence, and association with bone mass. J. Bone Miner. Metab. 2013, 32, 78–88. [Google Scholar] [CrossRef] [PubMed]
- Liu, L.-K.; Lee, W.-J.; Liu, C.-L.; Chen, L.-Y.; Lin, M.-H.; Peng, L.-N. Age-related skeletal muscle mass loss and physical performance in Taiwan: Implications to diagnostic strategy of sarcopenia in Asia. Geriatr. Gerontol. Int. 2013, 13, 964–971. [Google Scholar] [CrossRef] [PubMed]
- Singh, V.; Yeroushalmi, D.; Lygrisse, K.A.; Simcox, T.; Long, W.J.; Schwarzkopf, R. The influence of obesity on achievement of a ‘forgotten joint’ following total knee Arthroplast. Arch. Orthop. Trauma Surg. 2021, 1–9. [Google Scholar] [CrossRef]
- Singh, V.; Yeroushalmi, D.; Lygrisse, K.A.; Schwarzkopf, R.; Davidovitch, R.I. Impact of Obesity on the Forgotten Joint Score Following Primary Total Hip Arthroplast. J. Arthroplast. 2020, 36, 1342–1347. [Google Scholar] [CrossRef] [PubMed]
- Husted, H.; Jørgensen, C.C.; Gromov, K.; Kehlet, H. Does BMI influence hospital stay and morbidity after fast-track hip and knee arthroplasty? Acta Orthop. 2016, 87, 466–472. [Google Scholar] [CrossRef]
- Raut, S.; Mertes, S.C.; Muniz-Terrera, G.; Khanduja, V. Factors associated with prolonged length of stay following a total knee replacement in patients aged over 75. Int. Orthop. 2012, 36, 1601–1608. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Kemmler, W.; Teschler, M.; Goisser, S.; Bebenek, M.; Von Stengel, S.; Bollheimer, L.C.; Sieber, C.C.; Freiberger, E. Prevalence of sarcopenia in Germany and the corresponding effect of osteoarthritis in females 70 years and older living in the community: Results of the FORMoSA study. Clin. Interv. Aging 2015, 10, 1565–1573. [Google Scholar] [CrossRef] [PubMed]
- Erturk, C.; Altay, M.A.; Sert, C.; Levent, A.; Yaptı, M.; Yüce, K. The body composition of patients with knee osteoarthritis: Relationship with clinical parameters and radiographic severity. Aging Clin. Exp. Res. 2015, 27, 673–679. [Google Scholar] [CrossRef] [PubMed]
- Ho, K.K.-W.; Lau, L.C.-M.; Chau, W.-W.; Poon, Q.; Chung, K.-Y.; Wong, R.M.-Y. End-stage knee osteoarthritis with and without sarcopenia and the effect of knee arthroplasty—A prospective cohort study. BMC Geriatr. 2021, 21, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Shyam, A.K.; Joshi, R.; Patil, K.; Jain, A.; Sancheti, K.H.; Sancheti, P.K. Factors affecting range of motion in total knee arthroplasty using high flexion prosthesis: A prospective study. Indian J. Orthop. 2013, 47, 50–56. [Google Scholar] [CrossRef] [PubMed]
- Järvenpää, J.; Kettunen, J.; Kröger, H.; Miettinen, H. Obesity May Impair the Early Outcome of Total Knee Arthroplasty a Prospective Study of 100 Patients. Scand. J. Surg. 2010, 99, 45–49. [Google Scholar] [CrossRef] [PubMed]
- Gadinsky, N.E.; Ehrhardt, J.K.; Urband, C.; Westrich, G.H. Effect of Body Mass Index on Range of Motion and Manipulation After Total Knee Arthroplast. J. Arthroplast. 2011, 26, 1194–1197. [Google Scholar] [CrossRef] [PubMed]
- Shoji, H.; Solomonow, M.; Yoshino, S.; D’Ambrosia, R.; Dabezies, E. Factors affecting postoperative flexion in total knee arthroplast. Orthopedics 1990, 13, 643–649. [Google Scholar] [CrossRef] [PubMed]
- Järvenpää, J.; Kettunen, J.; Soininvaara, T.; Miettinen, H.; Kröger, H. Obesity Has a Negative Impact on Clinical Outcome after Total Knee Arthroplast. Scand. J. Surg. 2012, 101, 198–203. [Google Scholar] [CrossRef] [PubMed]
- Lizaur, A.; Marco, L.; Cebrian, R.; Lizaur-Utrilla, A. Preoperative factors influencing the range of movement after total knee arthroplasty for severe osteoarthritis. J. Bone Jt. Surg. Br. Vol. 1997, 79, 626–629. [Google Scholar] [CrossRef]
- Liao, C.-D.; Chen, H.-C.; Huang, S.-W.; Liou, T.-H. Impact of sarcopenia on rehabilitation outcomes after total knee replacement in older adults with knee osteoarthritis. Ther. Adv. Musculoskelet Dis. 2021, 13, 1759720X21998508. [Google Scholar] [CrossRef]
- Bell, J.; Bauer, J.; Capra, S.; Pulle, R.C. Concurrent and predictive evaluation of malnutrition diagnostic measures in hip fracture inpatients: A diagnostic accuracy study. Eur. J. Clin. Nutr. 2014, 68, 358–362. [Google Scholar] [CrossRef]
- Bell, J.J.; Bauer, J.; Capra, S.; Pulle, R.C. Quick and Easy Is Not without Cost: Implications of Poorly Performing Nutrition Screening Tools in Hip Fracture. J. Am. Geriatr. Soc. 2014, 62, 237–243. [Google Scholar] [CrossRef]
- Aghdam, A.R.M.; Kolahi, S.; Hasankhani, H.; Behshid, M.; Varmaziar, Z. The relationship between pain and physical function in adults with Knee Osteoarthritis. Int. Res. J. Appl. Basic Sci. 2013, 4, 1102–1106. [Google Scholar]
- Pisters, M.; Veenhof, C.; van Dijk, G.; Heymans, M.; Twisk, J.; Dekker, J. The course of limitations in activities over 5 years in patients with knee and hip osteoarthritis with moderate functional limitations: Risk factors for future functional decline. Osteoarthr. Cartil. 2012, 20, 503–510. [Google Scholar] [CrossRef] [PubMed]
| Items | Non-Obese | Obese | Obese-Sarcopenic | p Value | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| mean | ± | SD | mean | ± | SD | mean | ± | SD | ||
| n | 205 | 323 | 59 | |||||||
| Women, n (%) | 160 | (78.0) | 249 | (77.1) | 39 | (66.1) | 0.15 d | |||
| Age (years) | 70.9 | ± | 6.9 | 67.8 | ± | 6.3a | 75.1 | ± | 6.1 a | <0.001 b |
| Age category, n (%) | <0.001 d | |||||||||
| <65 years | 44 | (21.5) | 156 | (48.3) | 10 | (16.9) | ||||
| 70−74.9 years | 101 | (17.1) | 105 | (32.5) | 21 | (35.6) | ||||
| ≥75 years | 60 | (29.2) | 62 | (19.2) | 28 | (47.5) | ||||
| BMI (kg/m2) | 22.9 | ± | 1.8 | 30.6 | ± | 3.9 a | 27.0 | ± | 2.1 a | <0.001 c |
| ALM (kg) | 16.0 | ± | 3.2 | 17.9 | ± | 3.6 a | 13.8 | ± | 2.8 a | <0.001 c |
| AMI (kg/m2) | 6.64 | ± | 0.91 | 7.56 | ± | 0.98 a | 5.96 | ± | 0.75 a | <0.001 c |
| CIRS score | 8.4 | ± | 5.7 | 10.1 | ± | 5.5 a | 10.9 | ± | 6.2 a | 0.001 c |
| Surgical time (min) | 149 | ± | 35 | 152 | ± | 39 | 155 | ± | 33 | 0.35 b |
| LOS (day) | 5.3 | ± | 1.6 | 6.5 | ± | 2.4 a | 6.2 | ± | 1.9 a | <0.001 c |
| Follow-up time (week) | 13.7 | ± | 7.3 | 16.4 | ± | 7.7 a | 19.5 | ± | 8.9 a | <0.001 c |
| TKR leg, Right, n (%) | 123 | (60.0) | 181 | (56.0) | 31 | (52.5) | 0.51 d | |||
| KL grade, TKR leg, n (%) | 0.33 d | |||||||||
| 3 | 103 | (50.2) | 165 | (51.1) | 24 | (40.7) | ||||
| 4 | 102 | (49.8) | 158 | (48.9) | 35 | (59.3) | ||||
| MNA-SF <12 points | 76 | (37.1) | 92 | (28.5) | 27 | (45.8) | 0.01 d | |||
| Number of comorbidities, n (%) | ||||||||||
| Hypertension | 129 | (62.9) | 228 | (70.6) | 40 | (67.8) | 0.19 d | |||
| DM | 37 | (18.0) | 139 | (43.0) | 22 | (37.3) | <0.001 d | |||
| Cardiopulmonary disease | 94 | (45.9) | 174 | (53.9) | 29 | (49.2) | 0.19 d | |||
| Leg fracture | 12 | (5.9) | 15 | (4.6) | 3 | (5.1) | 0.83 d | |||
| Knee flexion ROM (degree) | ||||||||||
| Presurgery | 118 | ± | 14 | 108 | ± | 13 a | 101 | ± | 15 a | <0.001 b |
| Inpatient discharge | 102 | ± | 10 | 95 | ± | 10 a | 94 | ± | 10 a | <0.001 b |
| Body-Composition Group | Crude Model | Adjusted Model a | ||||
|---|---|---|---|---|---|---|
| HR | (95% CI) | p | HR | (95% CI) | p | |
| Non-obesity | Reference | Reference | ||||
| Obesity | 2.10 | (1.68, 2.62) | <0.001 | 1.35 | (1.04, 1.75) | 0.02 |
| Sarcopenic obesity | 3.63 | (2.37, 5.56) | <0.001 | 1.68 | (1.06, 2.66) | 0.03 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Liao, C.-D.; Huang, S.-W.; Huang, Y.-Y.; Lin, C.-L. Effects of Sarcopenic Obesity and Its Confounders on Knee Range of Motion Outcome after Total Knee Replacement in Older Adults with Knee Osteoarthritis: A Retrospective Study. Nutrients 2021, 13, 3817. https://doi.org/10.3390/nu13113817
Liao C-D, Huang S-W, Huang Y-Y, Lin C-L. Effects of Sarcopenic Obesity and Its Confounders on Knee Range of Motion Outcome after Total Knee Replacement in Older Adults with Knee Osteoarthritis: A Retrospective Study. Nutrients. 2021; 13(11):3817. https://doi.org/10.3390/nu13113817
Chicago/Turabian StyleLiao, Chun-De, Shih-Wei Huang, Yu-Yun Huang, and Che-Li Lin. 2021. "Effects of Sarcopenic Obesity and Its Confounders on Knee Range of Motion Outcome after Total Knee Replacement in Older Adults with Knee Osteoarthritis: A Retrospective Study" Nutrients 13, no. 11: 3817. https://doi.org/10.3390/nu13113817
APA StyleLiao, C.-D., Huang, S.-W., Huang, Y.-Y., & Lin, C.-L. (2021). Effects of Sarcopenic Obesity and Its Confounders on Knee Range of Motion Outcome after Total Knee Replacement in Older Adults with Knee Osteoarthritis: A Retrospective Study. Nutrients, 13(11), 3817. https://doi.org/10.3390/nu13113817






