1. Introduction
Lung cancer is the second most commonly diagnosed type of cancer, after breast cancer, with a global incidence of around 11.4% [
1]. It represents the leading cause of cancer death worldwide (18.0%) [
1]. According to the latest cancer statistics, it is estimated that there will be more than 235,760 new cases and 131,880 deaths in the United States in 2021 [
2].
Non-small-cell lung cancer (NSCLC) represents around 80–85% of all lung cancers [
3]. Survival of lung cancer patients 5 years after diagnosis is between 10% and 20% in most countries, even after surgery, chemotherapy, and radiotherapy [
4]. There is therefore a need to look for new prognostic biomarkers that will improve survival in these patients [
5]. The main factor influencing disease prognosis is the initial tumor stage [
6,
7,
8]. However, studies in patients diagnosed with the same stage have shown variability in survival, which suggests that other factors may influence the prognosis of NSCLC [
9,
10,
11,
12]. It should be emphasized that genetic alterations such as single nucleotide polymorphisms (SNPs) may be the cause of this interindividual variability in survival of patients with NSCLC [
5,
13,
14,
15].
Vitamin D is notable for its wide-ranging biological functions, which involve, among other things, suppressing metastasis by inhibiting tumor progression, angiogenesis, and cell proliferation, or by apoptosis promotion in cancer cells [
5,
16,
17,
18,
19,
20]. In lung cancer, specifically, in vivo and in vitro studies have been carried out, showing that 1,25-dihydroxycholecalciferol inhibits growth of lung cancerous cell lines and affects cell cycle regulation in squamous cell carcinoma models [
21,
22,
23]. In mouse models, calcitriol proved to inhibit growth of lung tumors and metastases [
24,
25]. Furthermore, observational studies have found that lung cancer mortality is lower during the autumn and summer months, the times of year associated with the highest vitamin D levels [
26,
27]. Risk, development, and growth of solid and non-solid tumors have been associated with vitamin D low levels [
19].
Vitamin D has two basic isoforms: vitamin D2 (ergocalciferol) and vitamin D3 (cholecalciferol). Both are produced endogenously following sun exposure and by direct consumption through diet or supplements [
27,
28,
29,
30]. The two isoforms of vitamin D (D2 and D3) bind to the vitamin D binding protein (VDBP), encoded by the group-specific component (vitamin D binding protein) gene (
GC), facilitating their transport [
29,
31,
32,
33]. Both forms are subsequently metabolized in the liver to 25-hydroxycholecalciferol, by 25-hydroxylases (encoded by
CYP2R1 and
CYP27A1), this being its main circulating form [
29,
31,
34,
35]; 1α-hydroxylase (encoded by
CYP27B1) converts it to 1,25-dihydroxycholecalciferol, either in the kidney (where it is released into circulation) or in specific target organs, converting it to its biologically active form [
16,
27,
28,
29,
31]. In the target tissues, 1,25-dihydroxycholecalciferol binds to the vitamin D receptor (VDR) and interacts with the retinoid X receptor (RXR), forming a heterodimer complex (VDR-RXR), which is translocated to the nucleus, binding to the VDR response elements in numerous genomic loci, some of which have anticancer properties [
16,
31,
36,
37]. Finally, circulating 1,25-dihydroxycholecalciferol and 25-hydroxycholecalciferol are degraded by 24-hydroxylase (encoded by
CYP24A1) to calcitroic acid and other hydrosoluble products which are inactive and are excreted in bile or urine [
27,
29,
31,
36].
The genes that encode the enzymes involved in the vitamin D pathway are highly polymorphic [
27]. These genetic alterations may influence the expression of those genes in lung tumor tissue, modifying the activity of vitamin D [
15,
28,
36,
38,
39,
40,
41]. Therefore, they may play a vital part in the development, progression, and prognosis of NSCLC [
5]. In this context, polymorphisms in the genes that mediate the metabolic pathway of vitamin D (
CYP27B1,
CYP24A1,
CYP2R1,
GC, and
VDR) may have a crucial role in the survival of patients with NSCLC [
5,
14,
15,
31,
42,
43].
On the basis of the foregoing, this study was design to evaluate the association of SNP-type polymorphisms in the genes implicated in the vitamin D metabolic pathway with progression-free survival (PFS) and overall survival (OS) in Caucasian patients (from Spain) with NSCLC.
4. Discussion
Cancer survival may be influenced by vitamin D through the suppression of cell proliferation, angiogenesis, cell proliferation, and metastasis which means the inhibition of tumor progression. Furthermore, the promotion of apoptosis in cancerous cells could be triggered by vitamin D [
5,
16]. Survival rates in patients diagnosed with NSCLC vary, even among patients diagnosed with the same stage [
9,
10,
11,
12]. Genetic factors may explain these interindividual differences. Several polymorphisms in various genes involved in the vitamin D metabolic pathway have been suggested as possible causes of this variability [
5,
14,
15,
31,
42,
43].
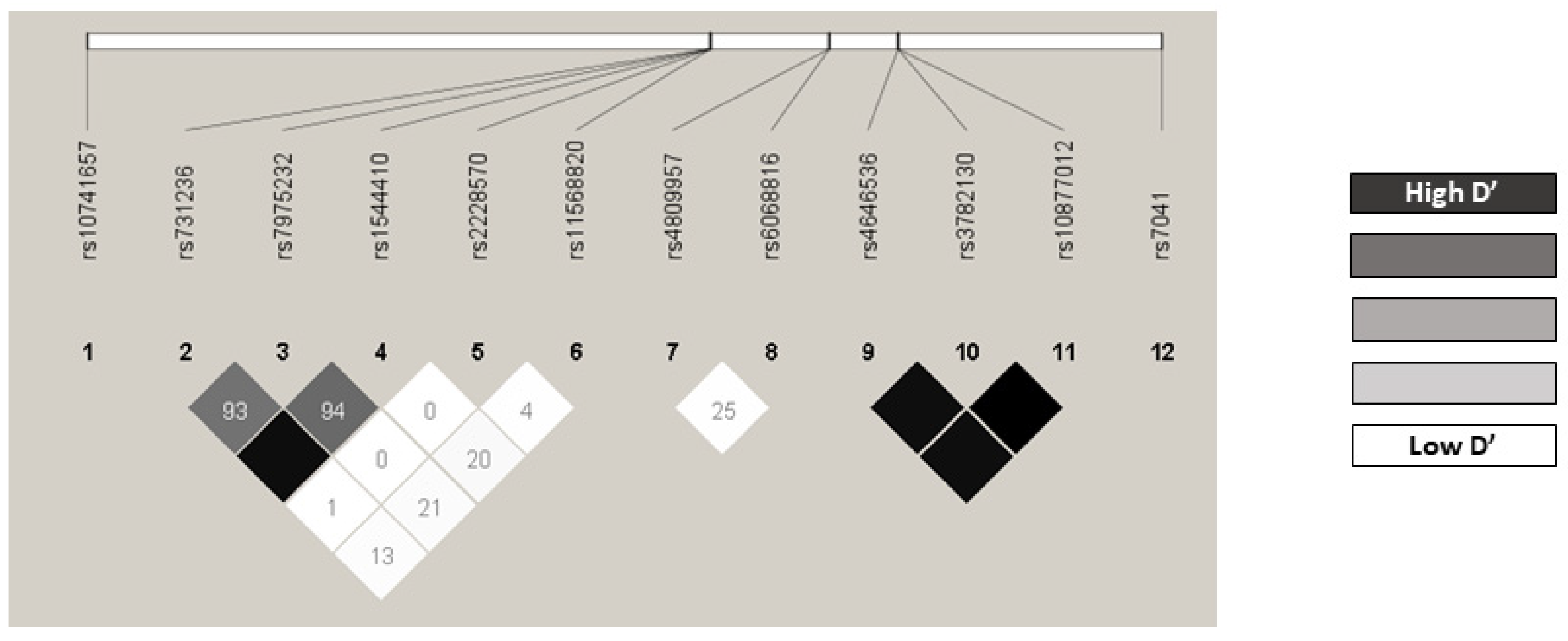
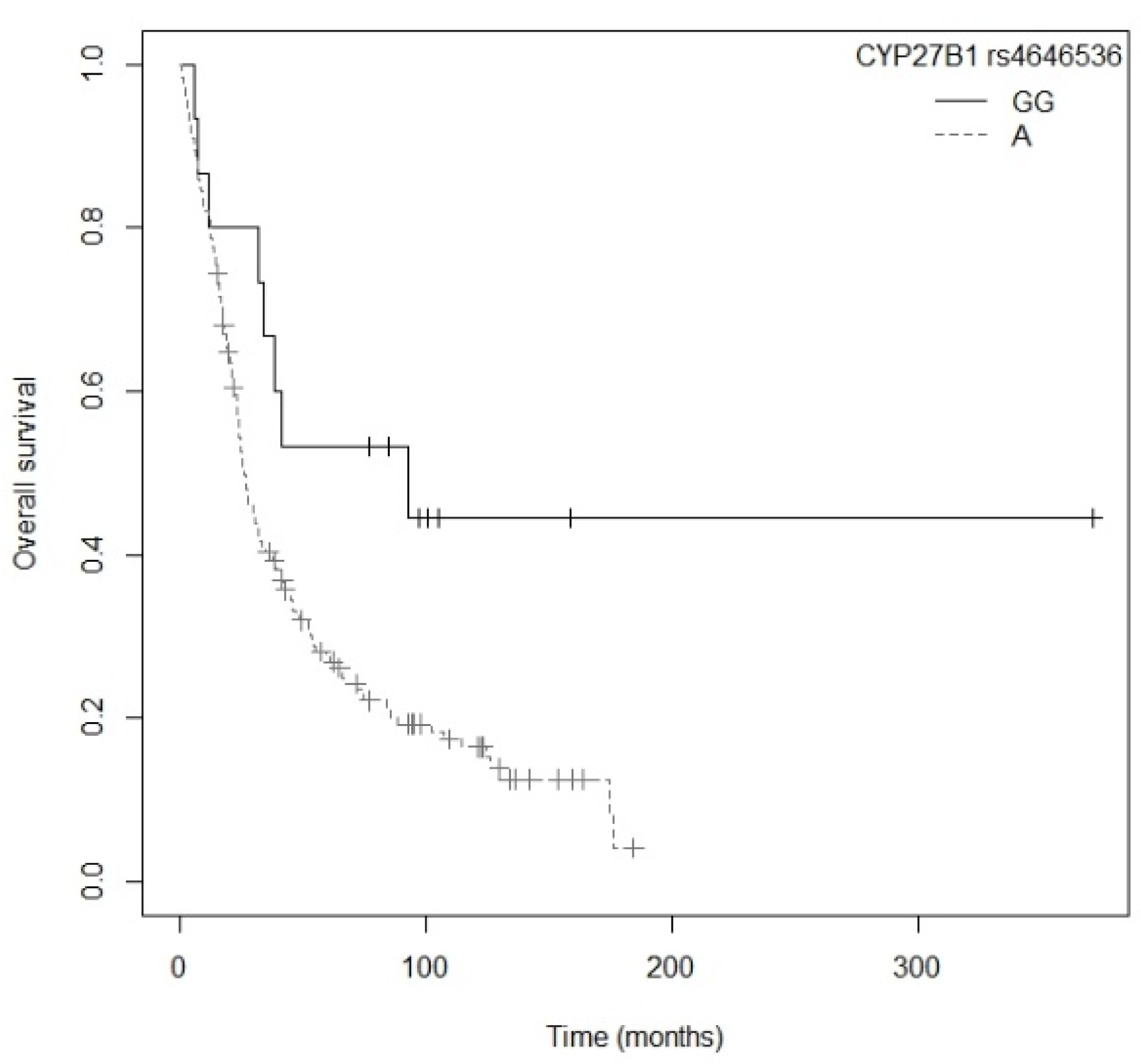
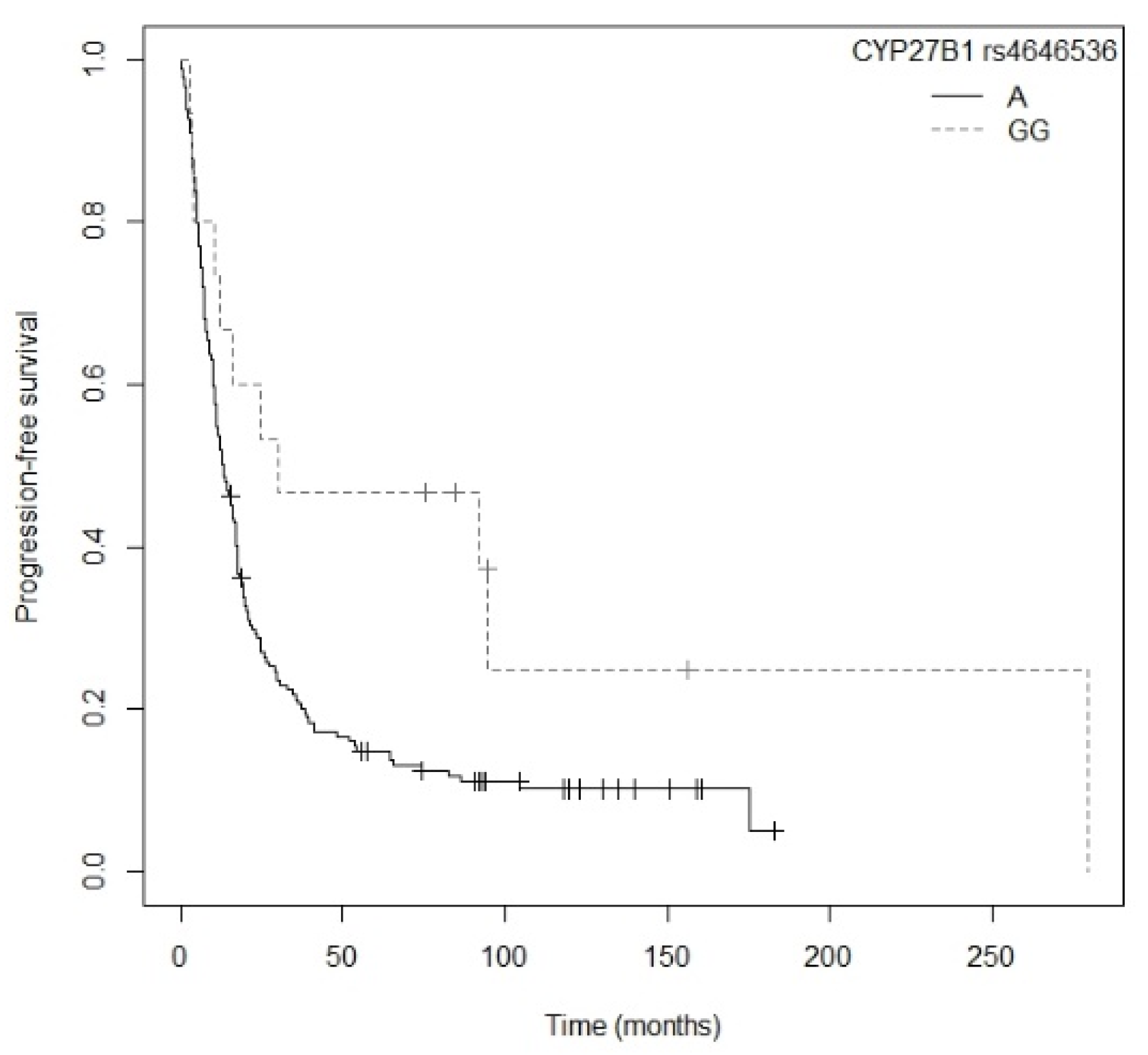
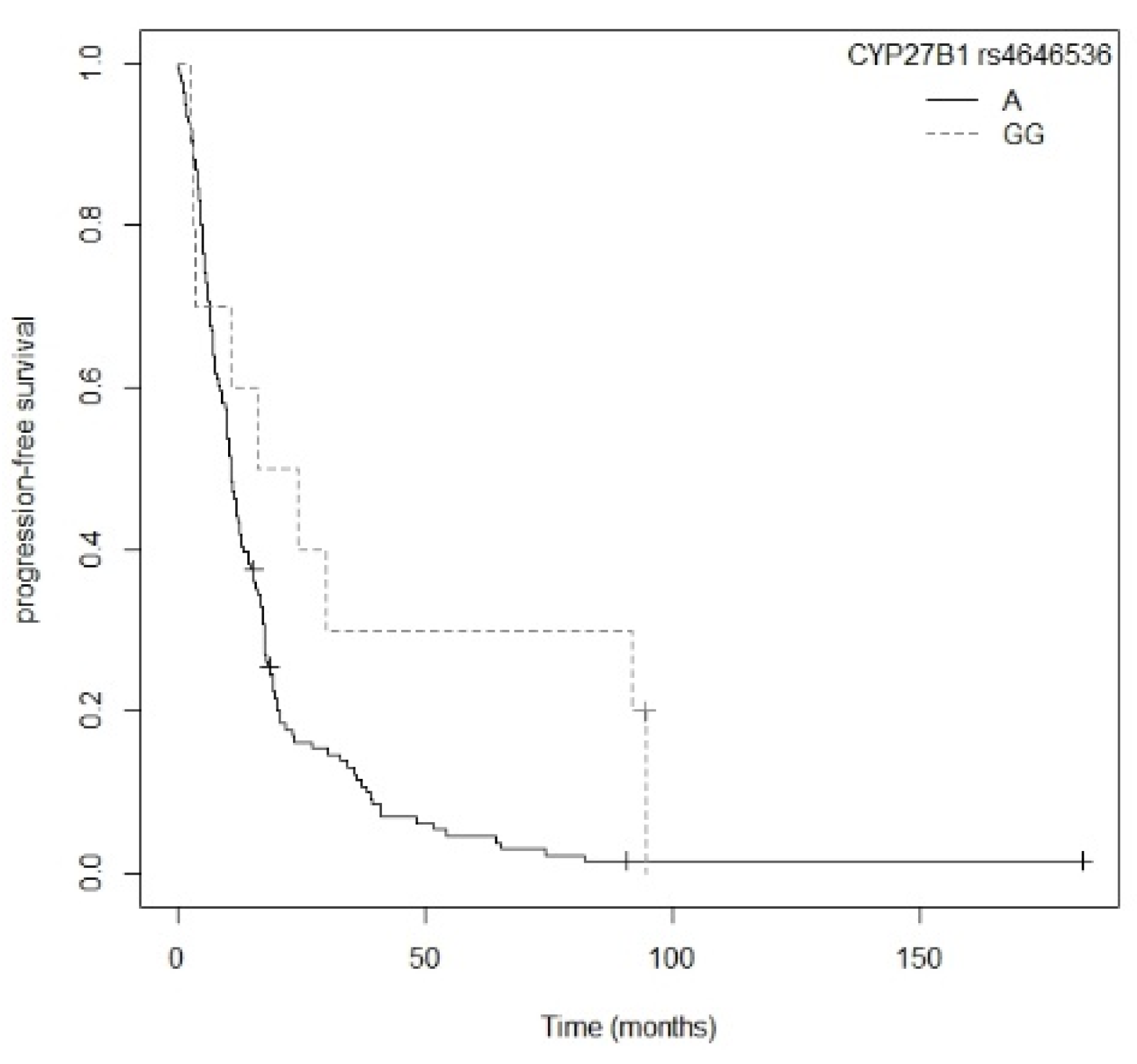
After investigating the potential of the gene polymorphisms involved in the vitamin D metabolic pathway in 194 Caucasian patients (from Spain) with NSCLC, we found that for the general population, patients carrying the A allele for the
CYP27B1 rs4545636 polymorphism had a higher risk of progression and tended to have a higher risk of death than bearers of the GG genotype. Additionally,
CYP27B1 rs4646536 maintained its associated with PFS in the subgroup of non-resected patients. To date there is only one other study, conducted in an Asian population (from China) with 542 NSCLC patients, that has evaluated the influence of
CYP27B1 rs4646536 on survival. However, no statistically significant association was found (
p = 0.625) [
5]. On the other hand, another study carried out in an Asian population (from China), with 153 (NSCLC) tumor samples, where a better overall survival (
p = 0.018) was associated with a high
CYP27B1 expression. It also found that alteration in gene expression may be due to SNPs, and specifically that the differences in expression were statistically significant in the
CYP27B1 rs3782130 polymorphism (
p = 0.028) [
31]. The importance of expression of
CYP27B1 lies in the fact that it is the only gene capable of converting vitamin D to its active form (1,25-dihydroxycholecalciferol) and it is this product that triggers all the biological functions of vitamin D, after binding to VDR [
16]. In our study, the
CYP27B1 rs3782130 polymorphism was associated with PFS in the non-resected patient subgroup in the univariate Cox regression model.
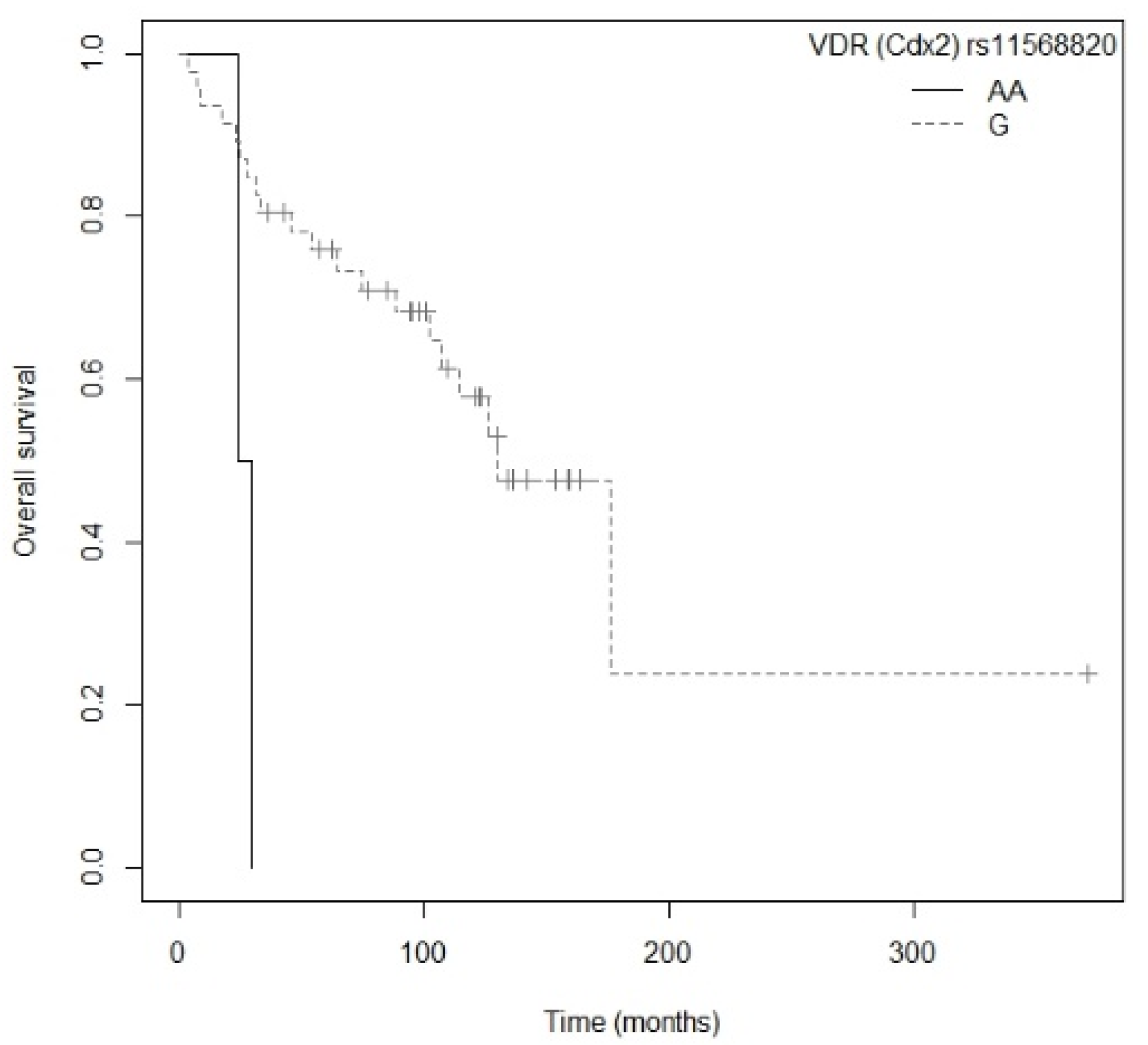
In the resected patient subgroup, the multivariate analysis revealed that patients carrying the AA genotype for
VDR rs11568820 had a higher risk of death than those with the GG genotype. Previous studies have shown contradictory results. Akiba et al., in a study with 155 Asian NSCLC patients (from Japan), found that the A allele of
VDR rs11568820 was associated with better overall survival (
p = 0.04; HR = 0.39; CI
95% = 0.16–0.97 for GA/AA vs. GG) [
43]. Similarly, another study with 376 patients of Caucasian origin (from the United States) with early stage NSCLC showed that the AA/AG genotypes of
VDR rs11568820 had better overall survival that the GG genotype (
p = 0.04; HR = 0.56; CI
95% = 0.33–0.95 for GA/AA vs. GG) [
15]. However, a study involving 294 Caucasian patients (from the United States) with advanced NSCLC found no association between
VDR rs11568820 polymorphisms and overall survival (
p = 0.82) [
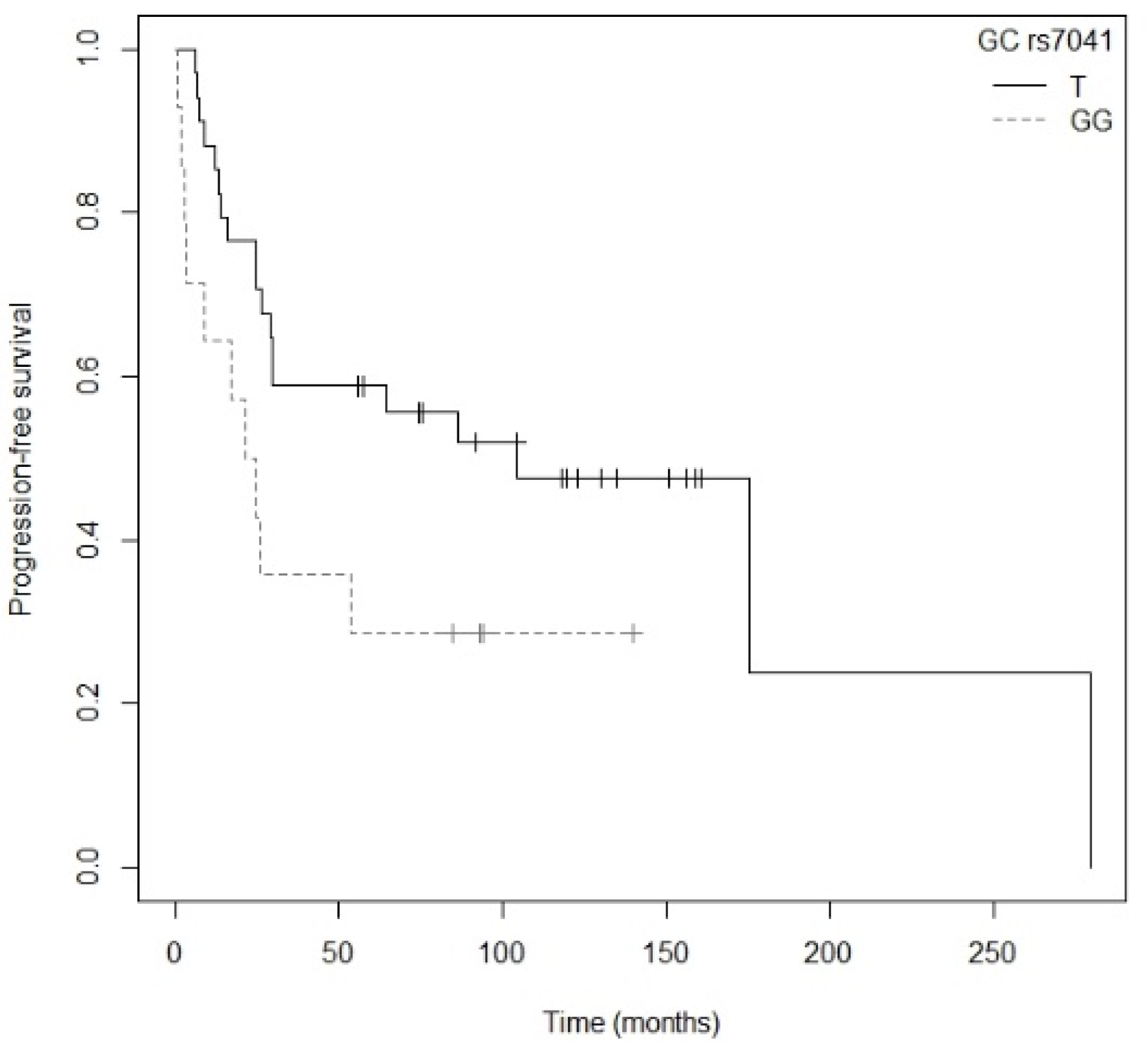
14]. Moreover, in our study patients bearing the G allele of the
GC rs7041 polymorphism showed a higher risk of progression than those with the TT genotype. Our findings are in line with the above-mentioned study by Akiba et al., in which the TT genotype of
GC rs7041 was associated with better PFS (
p = 0.045; HR = 0.51; CI
95% = 0.26–0.99; TT vs. TG/GG) and better OS (
p = 0.003; HR = 0.21; CI
95% = 0.07–0.59; TT vs. TG/GG) [
43]. Subsequently, another study was carried out with 542 Asian patients (from China), evaluating the relationship between
GC rs7041 and survival in NSCLC. However, the results were not statistically significant (
p = 0.693) [
5].
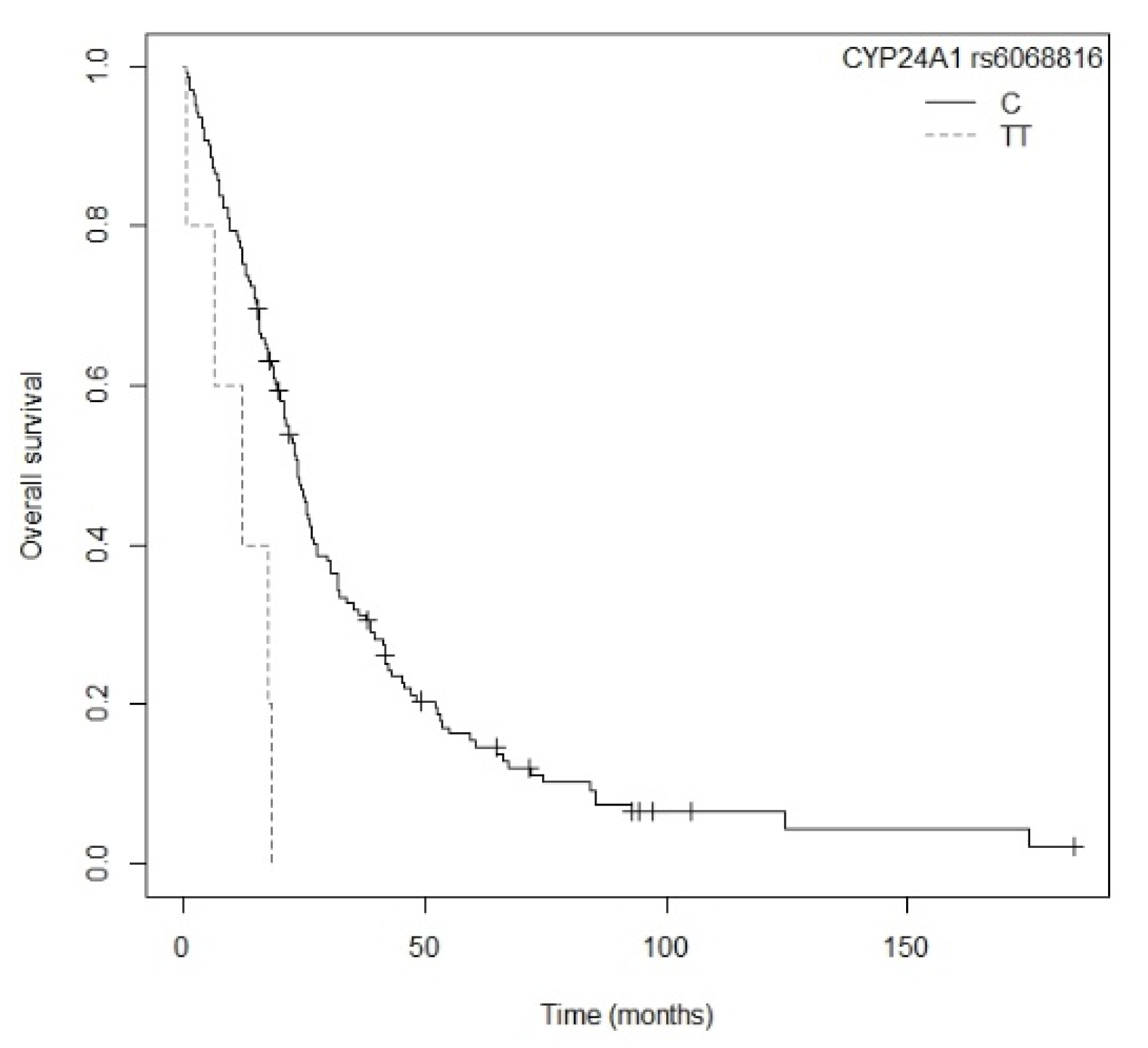
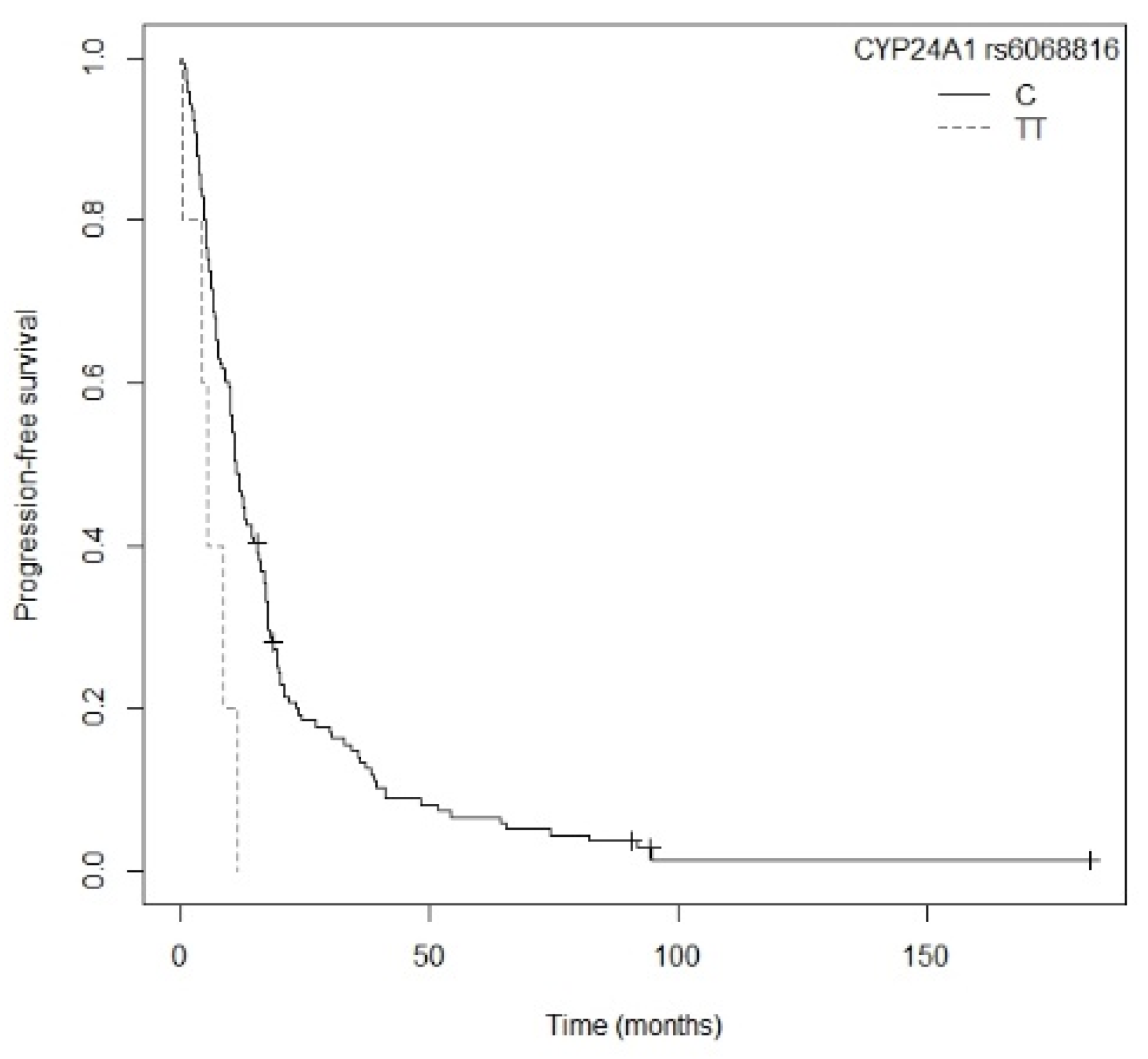
With regard to the subgroup of non-resected patients, our study revealed that a higher risk of death and of progression was associated with the TT genotype for the
CYP24A1 rs6068816 polymorphism in comparison to those carrying the C allele. Only one other study of the relationship between
CYP24A1 rs6068816 and survival has been conducted to date, in 542 Asian patients (from China) with NSCLC. However, it did not find a statistically significant association (
p = 0.072) [
5].
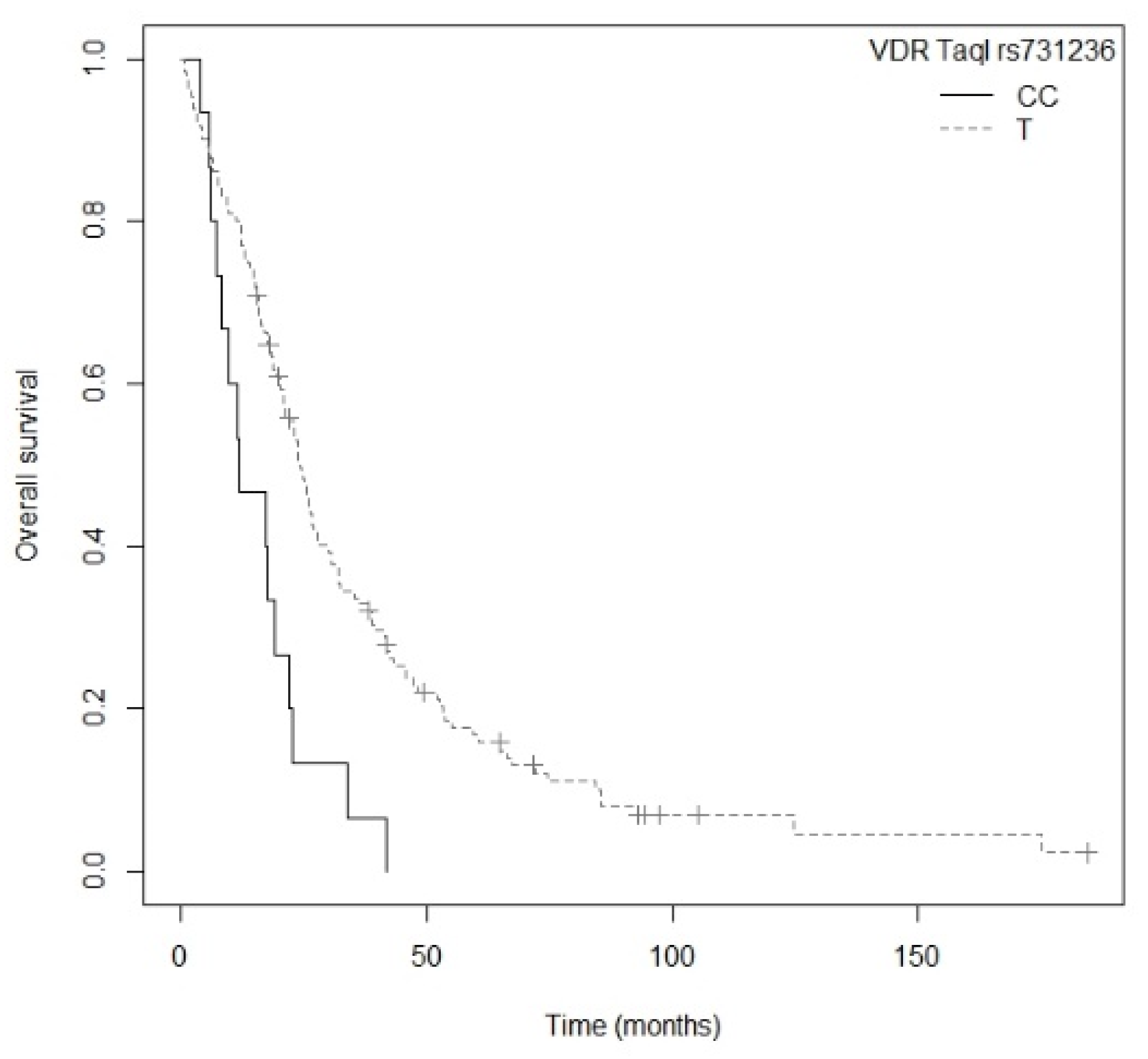
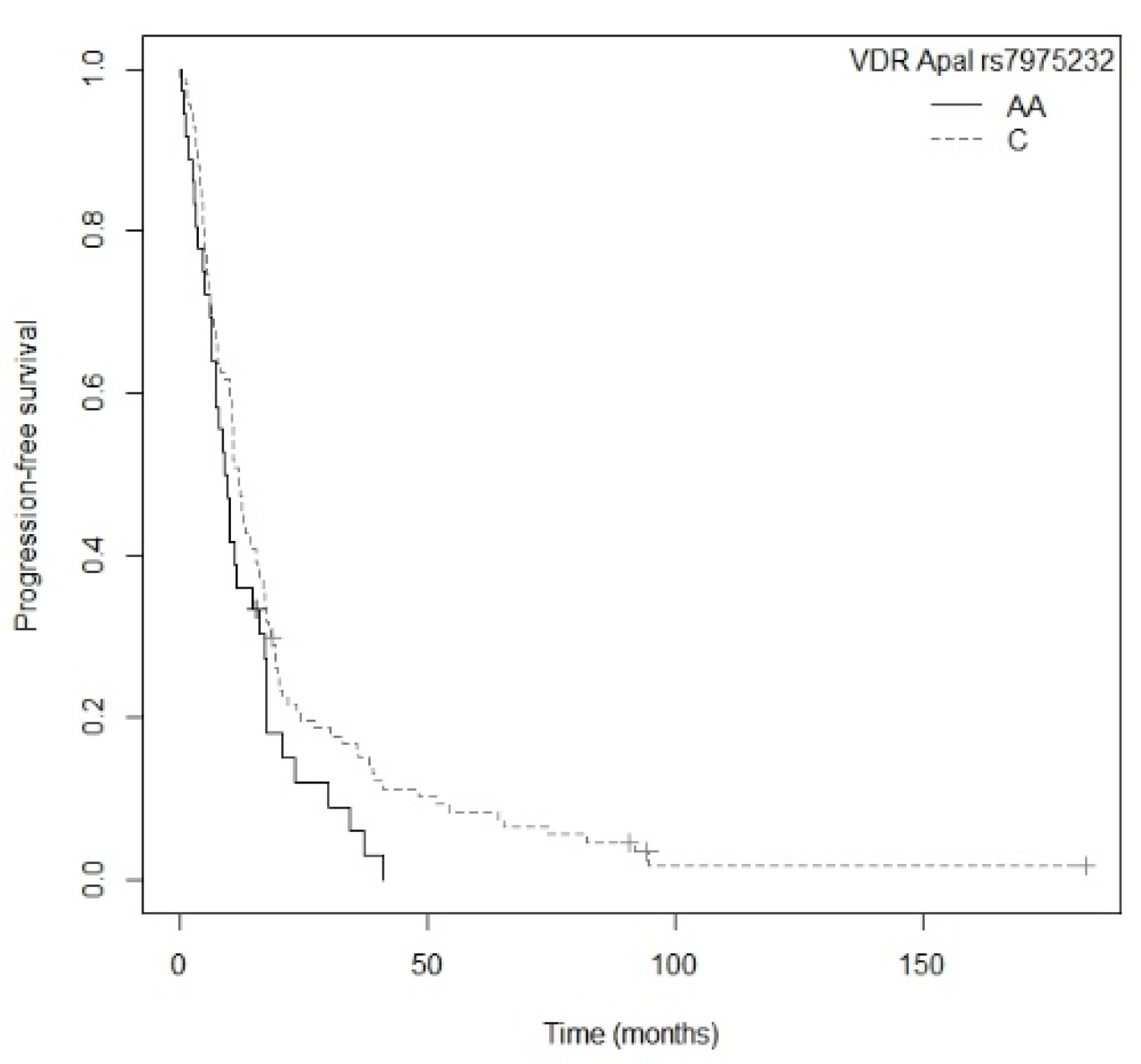
In our study, we also found that in the non-resected patient subgroup the rs7975232 and rs731236 polymorphisms of the
VDR gene were associated with progression-free survival and overall survival, respectively. Firstly, patients in our study carrying the CC genotype for
VDR rs731236 had a higher risk of death that those bearing the T allele. Previous studies have reported contradictory results. A study involving 62 patients of Asian origin (from Turkey) with NSCLC showed that the combined TT-CC/TT-TC genotypes for rs731236 and rs2228570, respectively, were associated with worse overall survival (HR = 1.81; CI
95% = 1.23–3.48;
p = 0.04) [
51]. However, another later study with 155 Asian patients (from Japan) with NSCLC did not find a statistically significant association between
VDR rs731236 and overall survival (
p = 0.26) [
43]. The
VDR rs7975232 polymorphism was associated in our study with a higher risk of death and progression. Specifically, patients carrying the AA genotype showed worse OS and greater progression than those with the C allele. Our results are in line with a previous study in 321 Asian patients (from China) with advanced NSCLC [
52]. This found an association between the AA genotype of
VDR rs7975232 and worse OS (
p < 0.001; HR = 2.84; CI
95% = 2.63–3.94) as well as a strong tendency toward a higher risk of progression (
p = 0.053; HR = 1.43; CI
95% = 0.99–2.78) than with the CC genotype [
52]. Moreover, this association has been confirmed in a multiethnic meta-analysis with 3.199 cases in five studies of various types of cancer (prostate, renal, colorectal, lung, and head and neck), which revealed that the AA genotype of
VDR rs7975232was associated with worse PFS (HR = 1.29; CI
95% = 1.02–1.56) [
53].
The CYP2R1 rs10741657 polymorphism has been studied recently. A study in an Asian population (from China) with 542 cases of NSCLC found that patients with the GG and AG genotypes had better OS than those with the AA genotype (
p = 0.033; HR = 0.69; CI
95% = 0.46–0.97), particularly elderly patients not receiving chemotherapy [
5]. In our patients this effect could not be confirmed. However, we did observe a strong tendency in the univariate Cox regression model toward OS in the general population.
Finally, a multiethnic meta-analysis of various types of cancer with 9926 cases in 10 studies (prostate, lung, colorectal, skin, glioma, and head and neck) for
VDR rs1544410 and 11,334 cases in 12 studies (breast, prostate, lung, colorectal, skin, glioma, ovarian, and head and neck) for
VDR rs2228570 evaluated the association of these two polymorphisms with OS. In particular, the AA/AG genotypes of
VDR rs1544410 were associated with worse OS (HR = 1.40; CI
95% = 1.05–1.75; AA/AG vs. GG) [
53]. In our study, the univariate Cox regression model showed that the AA genotype for the
VDR rs1544410 polymorphism was associated with worse OS in non-resected patients compared to the G allele. However, after the multivariate Cox regression this association was not sustained. The
VDR rs2228570 polymorphism was not associated with OS in the meta-analysis described above (HR = 1.26; CI
95% = 0.96–1.56) [
53]. Our study is in agreement with those results, since we did not obtain statistically significant associations for
VDR rs2228570 in any of the subgroups analyzed.
Vitamin D is strongly related to survival and risk of NSCLC. There is therefore a presumption that alterations in the genes involved in the metabolic pathway of vitamin D may affect their expression and functionality [
15,
28,
36,
37,
38,
39,
40]. Each of the genes fulfills a unique and characteristic function within the metabolic process of vitamin D. We can therefore surmise that variations in one or more genes may entail a worse prognosis. Thus far, we know that the genetic expression of
CYP24A1,
CYP27B1, and
VDR in lung cancer is affected by tumor differentiation and characterization. When the tumor is poorly differentiated, there is greater expression of
CYP24A1 and reduced expression of
CYP27B1 [
36,
38]. Increased expression of
VDR in lung cancer is associated with better survival [
40,
54]. This may be related to a lower proliferative state and G1-phase arrest of high VDR-expressing tumor cells [
40,
54]. Continued research is needed on the mechanism by which the SNPs associated with the vitamin D metabolic pathway affect overall survival and progression-free survival in patients with NSCLC.
This study presents a cohort of patients diagnosed with NSCLC from the same institution and treated under the same therapeutic protocol, ensuring the uniformity of the sample in the measurement of the survival variables analyzed. Although the sample size in our study is limited and it was not possible to detect some associations, the effect of the polymorphisms in the CYP27B1, CYP24A1, GC y VDR genes was clear.