Effect of COVID-19 Pandemic-Induced Dietary and Lifestyle Changes and Their Associations with Perceived Health Status and Self-Reported Body Weight Changes in India: A Cross-Sectional Survey
Abstract
:1. Introduction
2. Materials and Methods
2.1. Survey
2.2. Statistical Analysis
3. Results
3.1. Respondent Characteristics
3.2. Health and Nutrition Status—Perception and Concerns
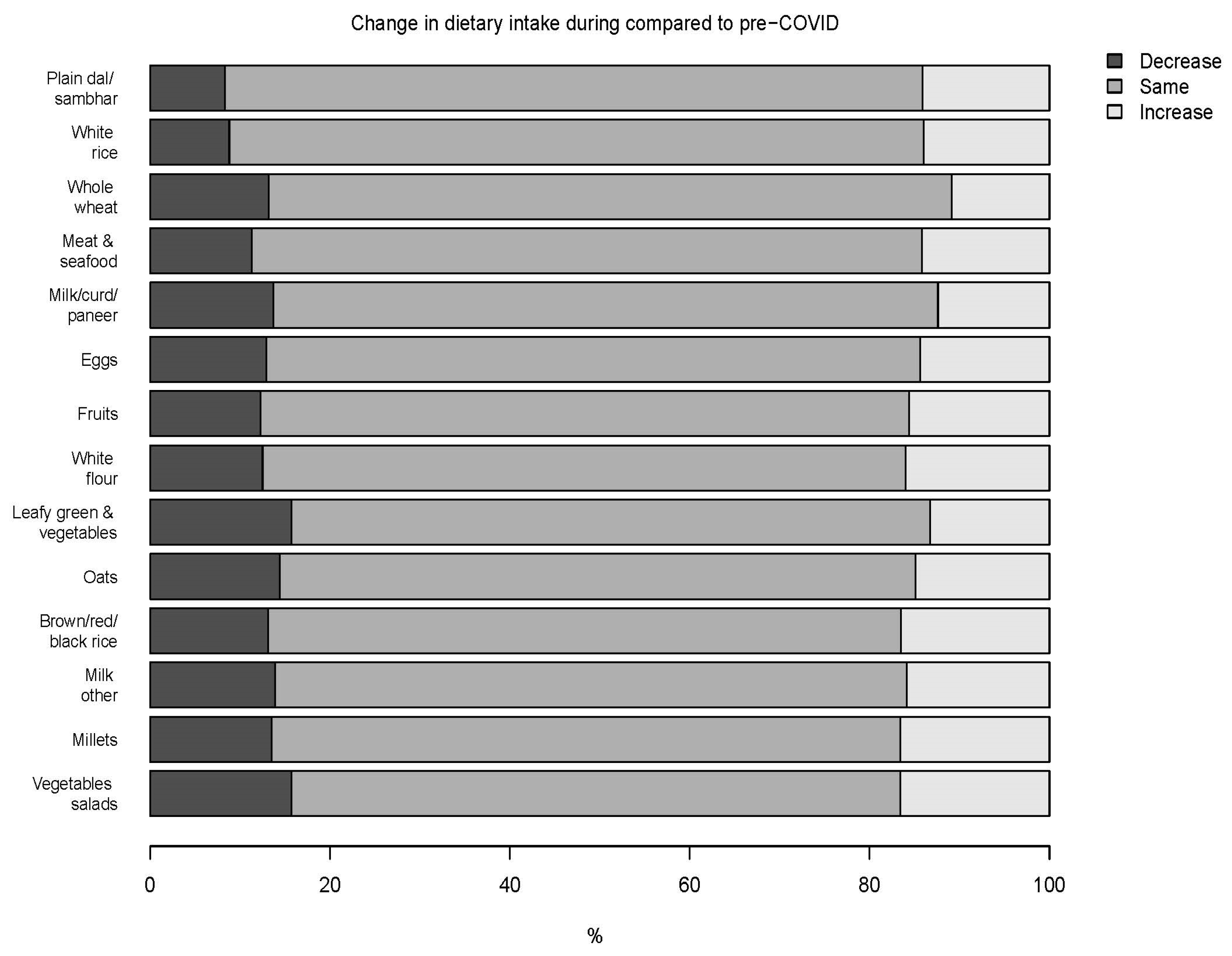
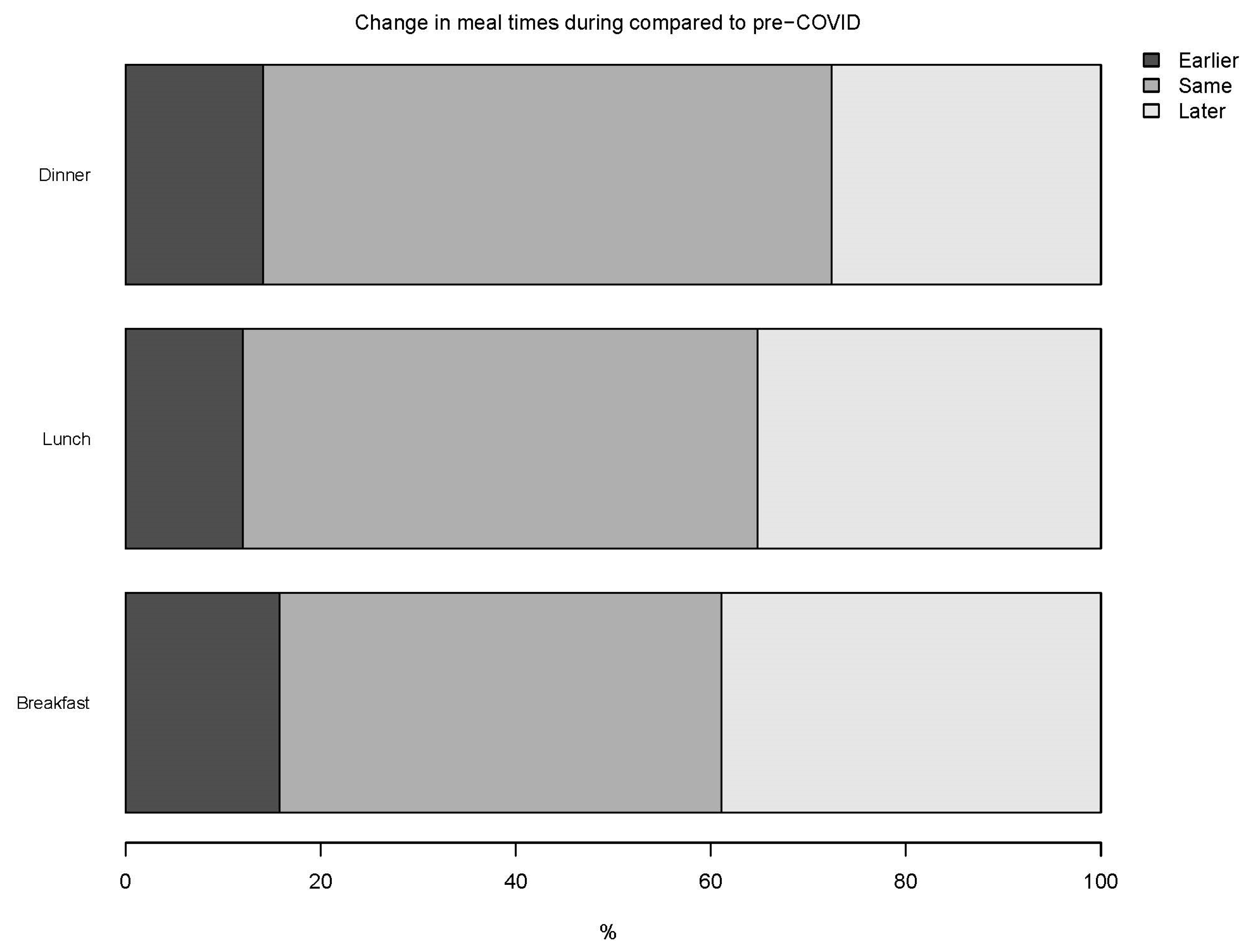
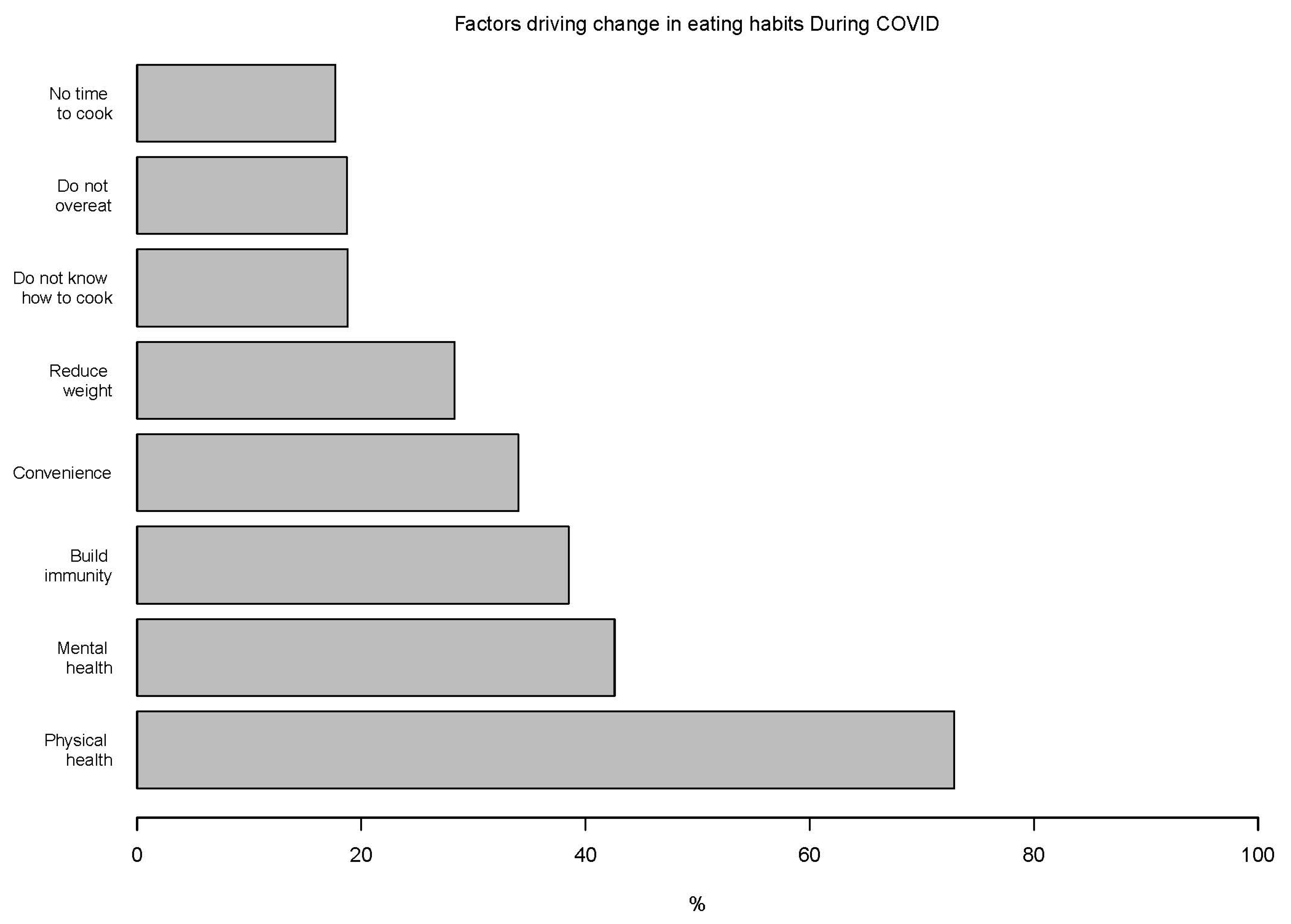
3.3. Dietary Habits
3.4. Oat Consumption
3.5. Lifestyle Behavior
3.6. Associations with Perceived Health and Self-Reported BW Change
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Disclaimer
References
- Hu, Z.; Lin, X.; Chiwanda Kaminga, A.; Xu, H. Impact of the COVID-19 Epidemic on Lifestyle Behaviors and Their Association With Subjective Well-Being Among the General Population in Mainland China: Cross-Sectional Study. J. Med. Internet Res. 2020, 22, e21176. [Google Scholar] [CrossRef]
- Di Renzo, L.; Gualtieri, P.; Pivari, F.; Soldati, L.; Attinà, A.; Cinelli, G.; Leggeri, C.; Caparello, G.; Barrea, L.; Scerbo, F.; et al. Eating habits and lifestyle changes during COVID-19 lockdown: An Italian survey. J. Transl. Med. 2020, 18, 229. [Google Scholar] [CrossRef] [PubMed]
- Lippi, G.; Henry, B.M.; Sanchis-Gomar, F. Physical inactivity and cardiovascular disease at the time of coronavirus disease 2019 (COVID-19). Eur. J. Prev. Cardiol. 2020, 27, 906–908. [Google Scholar] [CrossRef]
- Benedict, C.; Brandão, L.E.M.; Merikanto, I.; Partinen, M.; Bjorvatn, B.; Cedernaes, J. Meal and Sleep Timing before and during the COVID-19 Pandemic: A Cross-Sectional Anonymous Survey Study from Sweden. Clocks Sleep 2021, 3, 251–258. [Google Scholar] [CrossRef]
- Sinha, M.; Pande, B.; Sinha, R. Impact of COVID-19 lockdown on sleep-wake schedule and associated lifestyle related behavior: A national survey. J. Public Health Res. 2020, 9, 1826. [Google Scholar] [CrossRef] [PubMed]
- Thomson, M.; Spence, J.C.; Raine, K.; Laing, L. The association of television viewing with snacking behavior and body weight of young adults. Am. J. Health Promot. AJHP 2008, 22, 329–335. [Google Scholar] [CrossRef] [PubMed]
- Boulos, R.; Vikre, E.K.; Oppenheimer, S.; Chang, H.; Kanarek, R.B. ObesiTV: How television is influencing the obesity epidemic. Physiol. Behav. 2012, 107, 146–153. [Google Scholar] [CrossRef]
- Deschasaux-Tanguy, M.; Druesne-Pecollo, N.; Esseddik, Y.; de Edelenyi, F.S.; Allès, B.; Andreeva, V.A.; Baudry, J.; Charreire, H.; Deschamps, V.; Egnell, M.; et al. Diet and physical activity during the coronavirus disease 2019 (COVID-19) lockdown (March-May 2020): Results from the French NutriNet-Santé cohort study. Am. J. Clin. Nutr. 2021, 113, 924–938. [Google Scholar] [CrossRef]
- Phillipou, A.; Meyer, D.; Neill, E.; Tan, E.J.; Toh, W.L.; Van Rheenen, T.E.; Rossell, S.L. Eating and exercise behaviors in eating disorders and the general population during the COVID-19 pandemic in Australia: Initial results from the COLLATE project. Int. J. Eat. Disord. 2020, 53, 1158–1165. [Google Scholar] [CrossRef] [PubMed]
- Bennett, G.; Young, E.; Butler, I.; Coe, S. The Impact of Lockdown During the COVID-19 Outbreak on Dietary Habits in Various Population Groups: A Scoping Review. Front. Nutr. 2021, 8, 626432. [Google Scholar] [CrossRef] [PubMed]
- Rodríguez-Pérez, C.; Molina-Montes, E.; Verardo, V.; Artacho, R.; García-Villanova, B.; Guerra-Hernández, E.J.; Ruíz-López, M.D. Changes in Dietary Behaviours during the COVID-19 Outbreak Confinement in the Spanish COVIDiet Study. Nutrients 2020, 12, 1730. [Google Scholar] [CrossRef] [PubMed]
- Larsson, S.C.; Kaluza, J.; Wolk, A. Combined impact of healthy lifestyle factors on lifespan: Two prospective cohorts. J. Intern. Med. 2017, 282, 209–219. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Li, Y.; Pan, A.; Wang, D.D.; Liu, X.; Dhana, K.; Franco, O.H.; Kaptoge, S.; Di Angelantonio, E.; Stampfer, M.; Willett, W.C.; et al. Impact of Healthy Lifestyle Factors on Life Expectancies in the US Population. Circulation 2018, 138, 345–355. [Google Scholar] [CrossRef] [PubMed]
- Górnicka, M.; Drywień, M.E.; Zielinska, M.A.; Hamułka, J. Dietary and Lifestyle Changes During COVID-19 and the Subsequent Lockdowns among Polish Adults: A Cross-Sectional Online Survey PLifeCOVID-19 Study. Nutrients 2020, 12, 2324. [Google Scholar] [CrossRef] [PubMed]
- Barkley, G.S. Factors influencing health behaviors in the National Health and Nutritional Examination Survey, III (NHANES III). Soc. Work Health Care 2008, 46, 57–79. [Google Scholar] [CrossRef]
- Rosenstock, I.M.; Strecher, V.J.; Becker, M.H. Social learning theory and the Health Belief Model. Health Educ. Q 1988, 15, 175–183. [Google Scholar] [CrossRef]
- Bombak, A.E. Self-rated health and public health: A critical perspective. Front. Public Health 2013, 1, 15. [Google Scholar] [CrossRef] [Green Version]
- Garre-Olmo, J.; Turró-Garriga, O.; Martí-Lluch, R.; Zacarías-Pons, L.; Alves-Cabratosa, L.; Serrano-Sarbosa, D.; Vilalta-Franch, J.; Ramos, R.; Manté, X.A.; Casedevall, J.B.; et al. Changes in lifestyle resulting from confinement due to COVID-19 and depressive symptomatology: A cross-sectional a population-based study. Compr. Psychiatry 2021, 104, 152214. [Google Scholar] [CrossRef]
- Manjunath, N.K.; Majumdar, V.; Rozzi, A.; Huiru, W.; Mishra, A.; Kimura, K.; Nagarathna, R.; Nagendra, H.R. Health Perceptions and Adopted Lifestyle Behaviors During the COVID-19 Pandemic: Cross-National Survey. JMIR Form. Res. 2021, 5, e23630. [Google Scholar] [CrossRef]
- Bank, T.W. Urban Population (% of Total Population)—India. Available online: https://data.worldbank.org/indicator/SP.URB.TOTL.IN.ZS?locations=IN (accessed on 15 June 2021).
- Trakman, G.L.; Forsyth, A.; Hoye, R.; Belski, R. Developing and validating a nutrition knowledge questionnaire: Key methods and considerations. Public Health Nutr. 2017, 20, 2670–2679. [Google Scholar] [CrossRef] [Green Version]
- Therneau, T.; Atkinson, B. Rpart: Recursive Partitioning and Regression Trees. R Package Version 4.1-15. Available online: https://CRAN.R-project.org/package=rpart (accessed on 6 June 2021).
- Team, R.C. R: A Language and Environment for Statistical Computing. R Foundation for Statistical Computing, Vienna, Austria. Available online: https://www.R-project.org/ (accessed on 7 June 2021).
- Wang, C.; Pan, R.; Wan, X.; Tan, Y.; Xu, L.; McIntyre, R.S.; Choo, F.N.; Tran, B.; Ho, R.; Sharma, V.K.; et al. A longitudinal study on the mental health of general population during the COVID-19 epidemic in China. Brain Behav. Immun. 2020, 87, 40–48. [Google Scholar] [CrossRef] [PubMed]
- Tee, M.L.; Tee, C.A.; Anlacan, J.P.; Aligam, K.J.G.; Reyes, P.W.C.; Kuruchittham, V.; Ho, R.C. Psychological impact of COVID-19 pandemic in the Philippines. J. Affect. Disord. 2020, 277, 379–391. [Google Scholar] [CrossRef]
- Le, X.T.T.; Dang, A.K.; Toweh, J.; Nguyen, Q.N.; Le, H.T.; Do, T.T.T.; Phan, H.B.T.; Nguyen, T.T.; Pham, Q.T.; Ta, N.K.T.; et al. Evaluating the Psychological Impacts Related to COVID-19 of Vietnamese People Under the First Nationwide Partial Lockdown in Vietnam. Front. Psychiatry 2020, 11, 824. [Google Scholar] [CrossRef]
- Kushlev, K.; Heintzelman, S.J.; Lutes, L.D.; Wirtz, D.; Kanippayoor, J.M.; Leitner, D.; Diener, E. Does Happiness Improve Health? Evidence From a Randomized Controlled Trial. Psychol. Sci. 2020, 31, 807–821. [Google Scholar] [CrossRef]
- Elran-Barak, R.; Mozeikov, M. One Month into the Reinforcement of Social Distancing due to the COVID-19 Outbreak: Subjective Health, Health Behaviors, and Loneliness among People with Chronic Medical Conditions. Int. J. Environ. Res. Public Health 2020, 17, 5403. [Google Scholar] [CrossRef]
- Piko, B. Health-related predictors of self-perceived health in a student population: The importance of physical activity. J. Community Health 2000, 25, 125–137. [Google Scholar] [CrossRef]
- Qiu, J.; Shen, B.; Zhao, M.; Wang, Z.; Xie, B.; Xu, Y. A nationwide survey of psychological distress among Chinese people in the COVID-19 epidemic: Implications and policy recommendations. Gen. Psychiatry 2020, 33, e100213. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Serafini, G.; Parmigiani, B.; Amerio, A.; Aguglia, A.; Sher, L.; Amore, M. The psychological impact of COVID-19 on the mental health in the general population. QJM Mon. J. Assoc. Physicians 2020, 113, 531–537. [Google Scholar] [CrossRef] [PubMed]
- Ohlbrecht, H.; Jellen, J. Unequal tensions: The effects of the coronavirus pandemic in light of subjective health and social inequality dimensions in Germany. Eur. Soc. 2021, 23, S905–S922. [Google Scholar] [CrossRef]
- Gallagher, J.E.; Wilkie, A.A.; Cordner, A.; Hudgens, E.E.; Ghio, A.J.; Birch, R.J.; Wade, T.J. Factors associated with self-reported health: Implications for screening level community-based health and environmental studies. BMC Public Health 2016, 16, 640. [Google Scholar] [CrossRef] [Green Version]
- Eder, S.J.; Steyrl, D.; Stefanczyk, M.M.; Pieniak, M.; Martínez Molina, J.; Pešout, O.; Binter, J.; Smela, P.; Scharnowski, F.; Nicholson, A.A. Predicting fear and perceived health during the COVID-19 pandemic using machine learning: A cross-national longitudinal study. PLoS ONE 2021, 16, e0247997. [Google Scholar] [CrossRef] [PubMed]
- Dowd, J.B.; Andriano, L.; Brazel, D.M.; Rotondi, V.; Block, P.; Ding, X.; Liu, Y.; Mills, M.C. Demographic science aids in understanding the spread and fatality rates of COVID-19. Proc. Natl. Acad. Sci. USA 2020, 117, 9696–9698. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Benyamini, Y.; Burns, E. Views on aging: Older adults’ self-perceptions of age and of health. Eur. J. Ageing 2020, 17, 477–487. [Google Scholar] [CrossRef] [PubMed]
- Tull, M.T.; Edmonds, K.A.; Scamaldo, K.M.; Richmond, J.R.; Rose, J.P.; Gratz, K.L. Psychological Outcomes Associated with Stay-at-Home Orders and the Perceived Impact of COVID-19 on Daily Life. Psychiatry Res. 2020, 289, 113098. [Google Scholar] [CrossRef]
- Johns Hopkins Coronavirus Resource Center (CRC). Mortality Analysis. Available online: https://coronavirus.jhu.edu/data/mortality (accessed on 28 June 2021).
- Chew, H.S.J.; Lopez, V. Global Impact of COVID-19 on Weight and Weight-Related Behaviors in the Adult Population: A Scoping Review. Int. J. Environ. Res. Public Health 2021, 18, 1876. [Google Scholar] [CrossRef]
- Urzeala, C.; Duclos, M.; Chris Ugbolue, U.; Bota, A.; Berthon, M.; Kulik, K.; Thivel, D.; Bagheri, R.; Gu, Y.; Baker, J.S.; et al. COVID-19 lockdown consequences on body mass index and perceived fragility related to physical activity: A worldwide cohort study. Health Expect. Int. J. Public Particip. Health Care Health Policy 2021. [Google Scholar] [CrossRef]
- Bhutani, S.; van Dellen, M.R.; Haskins, L.B.; Cooper, J.A. Energy Balance-Related Behavior Risk Pattern and Its Correlates During COVID-19 Related Home Confinement. Front. Nutr. 2021, 8, 680105. [Google Scholar] [CrossRef] [PubMed]
- Flanagan, E.W.; Beyl, R.A.; Fearnbach, S.N.; Altazan, A.D.; Martin, C.K.; Redman, L.M. The Impact of COVID-19 Stay-At-Home Orders on Health Behaviors in Adults. Obesity 2021, 29, 438–445. [Google Scholar] [CrossRef] [PubMed]
- Sánchez-Sánchez, E.; Ramírez-Vargas, G.; Avellaneda-López, Y.; Orellana-Pecino, J.I.; García-Marín, E.; Díaz-Jimenez, J. Eating Habits and Physical Activity of the Spanish Population during the COVID-19 Pandemic Period. Nutrients 2020, 12, 2826. [Google Scholar] [CrossRef] [PubMed]
- Reyes-Olavarría, D.; Latorre-Román, P.; Guzmán-Guzmán, I.P.; Jerez-Mayorga, D.; Caamaño-Navarrete, F.; Delgado-Floody, P. Positive and Negative Changes in Food Habits, Physical Activity Patterns, and Weight Status during COVID-19 Confinement: Associated Factors in the Chilean Population. Int. J. Environ. Res. Public Health 2020, 17, 5431. [Google Scholar] [CrossRef]
- Cooper, J.A.; Tokar, T. A prospective study on vacation weight gain in adults. Physiol. Behav. 2016, 156, 43–47. [Google Scholar] [CrossRef]
- Zhang, X.; Oluyomi, A.; Woodard, L.; Raza, S.A.; Adel Fahmideh, M.; El-Mubasher, O.; Byun, J.; Han, Y.; Amos, C.I.; Badr, H. Individual-Level Determinants of Lifestyle Behavioral Changes during COVID-19 Lockdown in the United States: Results of an Online Survey. Int. J. Environ. Res. Public Health 2021, 18, 4364. [Google Scholar] [CrossRef]
- Sidor, A.; Rzymski, P. Dietary Choices and Habits during COVID-19 Lockdown: Experience from Poland. Nutrients 2020, 12, 1657. [Google Scholar] [CrossRef] [PubMed]
- Maffoni, S.; Brazzo, S.; De Giuseppe, R.; Biino, G.; Vietti, I.; Pallavicini, C.; Cena, H. Lifestyle Changes and Body Mass Index during COVID-19 Pandemic Lockdown: An Italian Online-Survey. Nutrients 2021, 13, 1117. [Google Scholar] [CrossRef]
- Neira, C.; Godinho, R.; Rincón, F.; Mardones, R.; Pedroso, J. Consequences of the COVID-19 Syndemic for Nutritional Health: A Systematic Review. Nutrients 2021, 13, 1168. [Google Scholar] [CrossRef]
- Ammar, A.; Brach, M.; Trabelsi, K.; Chtourou, H.; Boukhris, O.; Masmoudi, L.; Bouaziz, B.; Bentlage, E.; How, D.; Ahmed, M.; et al. Effects of COVID-19 Home Confinement on Eating Behaviour and Physical Activity: Results of the ECLB-COVID19 International Online Survey. Nutrients 2020, 12, 1583. [Google Scholar] [CrossRef] [PubMed]
- Enriquez-Martinez, O.G.; Martins, M.C.T.; Pereira, T.S.S.; Pacheco, S.O.S.; Pacheco, F.J.; Lopez, K.V.; Huancahuire-Vega, S.; Silva, D.A.; Mora-Urda, A.I.; Rodriguez-Vásquez, M.; et al. Diet and Lifestyle Changes During the COVID-19 Pandemic in Ibero-American Countries: Argentina, Brazil, Mexico, Peru, and Spain. Front. Nutr. 2021, 8, 671004. [Google Scholar] [CrossRef]
- Mehta, V. The Impact of COVID-19 on the Dietary Habits of Middle-Class Population in Mulund, Mumbai, India. AIJR Preprints. 2020. [Google Scholar] [CrossRef]
- Paoli, A.; Tinsley, G.; Bianco, A.; Moro, T. The Influence of Meal Frequency and Timing on Health in Humans: The Role of Fasting. Nutrients 2019, 11, 719. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ha, K.; Song, Y. Associations of Meal Timing and Frequency with Obesity and Metabolic Syndrome among Korean Adults. Nutrients 2019, 11, 2437. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kahleova, H.; Lloren, J.I.; Mashchak, A.; Hill, M.; Fraser, G.E. Meal Frequency and Timing Are Associated with Changes in Body Mass Index in Adventist Health Study 2. J. Nutr. 2017, 147, 1722–1728. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Celorio-Sardà, R.; Comas-Basté, O.; Latorre-Moratalla, M.L.; Zerón-Rugerio, M.F.; Urpi-Sarda, M.; Illán-Villanueva, M.; Farran-Codina, A.; Izquierdo-Pulido, M.; Vidal-Carou, M.D.C. Effect of COVID-19 Lockdown on Dietary Habits and Lifestyle of Food Science Students and Professionals from Spain. Nutrients 2021, 13, 1494. [Google Scholar] [CrossRef] [PubMed]
- Nyberg, S.T.; Singh-Manoux, A.; Pentti, J.; Madsen, I.E.H.; Sabia, S.; Alfredsson, L.; Bjorner, J.B.; Borritz, M.; Burr, H.; Goldberg, M.; et al. Association of Healthy Lifestyle with Years Lived without Major Chronic Diseases. JAMA Intern. Med. 2020, 180, 760–768. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Li, Y.; Schoufour, J.; Wang, D.D.; Dhana, K.; Pan, A.; Liu, X.; Song, M.; Liu, G.; Shin, H.J.; Sun, Q.; et al. Healthy lifestyle and life expectancy free of cancer, cardiovascular disease, and type 2 diabetes: Prospective cohort study. BMJ (Clin. Res. Ed.) 2020, 368, l6669. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hossain, M.M.; Sultana, A.; Purohit, N. Mental health outcomes of quarantine and isolation for infection prevention: A systematic umbrella review of the global evidence. Epidemiol. Health 2020, 42, e2020038. [Google Scholar] [CrossRef] [PubMed]
- WHO-Europe. Stay Physically Active during Self-Quarantine. Available online: https://www.euro.who.int/en/health-topics/health-emergencies/coronavirus-covid-19/publications-and-technical-guidance/noncommunicable-diseases/stay-physically-active-during-self-quarantine#:~:text=Physical%20activity%20and%20relaxation%20techniques,or%20a%20combination%20of%20both. (accessed on 28 June 2021).
- Bhutani, S.; Cooper, J.A.; Vandellen, M.R. Self-reported changes in energy balance behaviors during COVID-19 related home confinement: A Cross-Sectional Study. medRxiv 2020. [Google Scholar] [CrossRef]
- Matsungo, T.M.; Chopera, P. Effect of the COVID-19-induced lockdown on nutrition, health and lifestyle patterns among adults in Zimbabwe. BMJ Nutr. Prev. Health 2020, 3, 205–212. [Google Scholar] [CrossRef]
- van Gelder, M.M.; Bretveld, R.W.; Roeleveld, N. Web-based questionnaires: The future in epidemiology? Am. J. Epidemiol. 2010, 172, 1292–1298. [Google Scholar] [CrossRef] [PubMed]


| n | % | ||
|---|---|---|---|
| Gender | Female | 500 | 50.0 |
| Male | 500 | 50.0 | |
| Generation | Gen X (41–50 y/o) | 100 | 10.0 |
| Millennial (26–40 y/o) | 450 | 45.0 | |
| Gen Z (18–25 y/o) | 450 | 45.0 | |
| City | Bangalore | 250 | 25.0 |
| Delhi/NCR | 250 | 25.0 | |
| Kolkata | 250 | 25.0 | |
| Mumbai | 250 | 25.0 | |
| Education level of chief wage earner | Graduate/Postgraduate: Professional | 308 | 30.8 |
| Graduate/Postgraduate: General | 469 | 46.9 | |
| Some College (including Diploma) but not Grad | 122 | 12.2 | |
| SSC/HSC | 59 | 5.9 | |
| School—5–9 years | 18 | 1.8 | |
| Literate but no formal schooling/school—up to 4 years | 8 | 0.8 | |
| Illiterate | 16 | 1.6 |
| Food Group | Pre-COVID-19 Frequency | during-COVID-19 Frequency | Test of Symmetry | |||
|---|---|---|---|---|---|---|
| <3 Times a Week | 4–5 Times a Week to Twice a Day | ≥3 Times a Day | Unadjusted p-Value | Adjusted q-Value | ||
| Cooked brown/red/black rice | <3 times a week | 225 (22.5) | 67 (6.7) | 31 (3.1) | 0.24 | 0.37 |
| From 4–5 times a week to twice a day | 57 (5.7) | 394 (39.4) | 67 (6.7) | |||
| ≥3 times a day | 22 (2.2) | 52 (5.2) | 85 (8.5) | |||
| Cooked leafy green and other vegetables | <3 times a week | 38 (3.8) | 39 (3.9) | 12 (1.2) | 0.32 | 0.40 |
| From 4–5 times a week to twice a day | 36 (3.6) | 567 (56.7) | 82 (8.2) | |||
| ≥3 times a day | 16 (1.6) | 105 (10.5) | 105 (10.5) | |||
| Cooked millets | <3 times a week | 236 (23.6) | 77 (7.7) | 20 (2.0) | 0.046 | 0.13 |
| From 4–5 times a week to twice a day | 48 (4.8) | 390 (39.0) | 69 (6.9) | |||
| ≥3 times a day | 26 (2.6) | 61 (6.1) | 73 (7.3) | |||
| Cooked oats | <3 times a week | 206 (20.6) | 58 (5.8) | 24 (2.4) | 0.94 | 0.94 |
| From 4–5 times a week to twice a day | 59 (5.9) | 405 (40.5) | 67 (6.7) | |||
| ≥3 times a day | 20 (2.0) | 65 (6.5) | 96 (9.6) | |||
| Eggs | <3 times a week | 175 (17.5) | 46 (4.6) | 21 (2.1) | 0.28 | 0.39 |
| From 4–5 times a week to twice a day | 50 (5.0) | 493 (49.3) | 77 (7.7) | |||
| ≥3 times a day | 11 (1.1) | 68 (6.8) | 59 (5.9) | |||
| Fruits | <3 times a week | 54 (5.4) | 41 (4.1) | 13 (1.3) | 0.024 | 0.11 |
| From 4–5 times a week to twice a day | 37 (3.7) | 584 (58.4) | 102 (10.2) | |||
| ≥3 times a day | 20 (2.0) | 66 (6.6) | 83 (8.3) | |||
| Meat and seafood | <3 times a week | 324 (32.4) | 70 (7.0) | 26 (2.6) | 0.042 | 0.13 |
| From 4–5 times a week to twice a day | 44 (4.4) | 367 (36.7) | 46 (4.6) | |||
| ≥3 times a day | 17 (1.7) | 52 (5.2) | 54 (5.4) | |||
| Milk/curd/paneer (dairy) | <3 times a week | 73 (7.3) | 38 (3.8) | 15 (1.5) | 0.65 | 0.73 |
| From 4–5 times a week to twice a day | 48 (4.8) | 577 (57.7) | 71 (7.1) | |||
| ≥3 times a day | 19 (1.9) | 70 (7.0) | 89 (8.9) | |||
| Other milk products (cheese, khoa) | <3 times a week | 212 (21.2) | 55 (5.5) | 16 (1.6) | 0.15 | 0.26 |
| From 4–5 times a week to twice a day | 62 (6.2) | 414 (41.4) | 88 (8.8) | |||
| ≥3 times a day | 16 (1.6) | 61 (6.1) | 76 (7.6) | |||
| Plain dal/sambhar | <3 times a week | 87 (8.7) | 53 (5.3) | 20 (2.0) | 0.002 | 0.023 |
| From 4–5 times a week to twice a day | 31 (3.1) | 610 (61.0) | 68 (6.8) | |||
| ≥3 times a day | 10 (1.0) | 42 (4.2) | 79 (7.9) | |||
| Vegetables—salads | <3 times a week | 78 (7.8) | 47 (4.7) | 25 (2.5) | 0.67 | 0.73 |
| From 4–5 times a week to twice a day | 36 (3.6) | 491 (49.1) | 94 (9.4) | |||
| ≥3 times a day | 27 (2.7) | 94 (9.4) | 108 (10.8) | |||
| White flour | <3 times a week | 263 (26.3) | 70 (7.0) | 24 (2.4) | 0.10 | 0.24 |
| From 4–5 times a week to twice a day | 46 (4.6) | 370 (37.0) | 66 (6.6) | |||
| ≥3 times a day | 25 (2.5) | 54 (5.4) | 82 (8.2) | |||
| White rice | <3 times a week | 80 (8.0) | 44 (4.4) | 19 (1.9) | 0.007 | 0.048 |
| From 4–5 times a week to twice a day | 30 (3.0) | 623 (62.3) | 77 (7.7) | |||
| ≥3 times a day | 10 (1.0) | 48 (4.8) | 69 (6.9) | |||
| Whole wheat | <3 times a week | 69 (6.9) | 29 (2.9) | 13 (1.3) | 0.13 | 0.26 |
| From 4–5 times a week to twice a day | 26 (2.6) | 606 (60.6) | 67 (6.7) | |||
| ≥3 times a day | 26 (2.6) | 80 (8.0) | 84 (8.4) | |||
| Lifestyle Parameter | Pre-COVID-19 Time | during-COVID-19 Time | Test of Symmetry | |||
|---|---|---|---|---|---|---|
| <30 min | from 30 min to 3 h | >3 h | Unadjusted p-Value | Adjusted q-Value | ||
| Physically active | <30 min | 132 (13.2) | 122 (12.2) | 12 (1.2) | <0.001 | <0.001 |
| From 30 min to 3 h | 79 (7.9) | 449 (44.9) | 78 (7.8) | |||
| >3 h | 5 (0.5) | 48 (4.8) | 75 (7.5) | |||
| <5 h | 6–8 h | >8 h | ||||
| Sleeping | <5 h | 274 (27.4) | 74 (7.4) | 26 (2.6) | <0.001 | <0.001 |
| 6–8 h | 68 (6.8) | 316 (31.6) | 133 (13.3) | |||
| >8 h | 7 (0.7) | 24 (2.4) | 78 (7.8) | |||
| <1 h | 1–5 h | ≥6 h | ||||
| Cleaning | <1 h | 388 (38.8) | 185 (18.5) | 13 (1.3) | <0.001 | <0.001 |
| 1–5 h | 88 (8.8) | 230 (23.0) | 29 (2.9) | |||
| ≥6 h | 14 (1.4) | 25 (2.5) | 28 (2.8) | |||
| Connecting virtually | <1 h | 314 (31.4) | 201 (20.1) | 13 (1.3) | <0.001 | <0.001 |
| 1–5 h | 98 (9.8) | 254 (25.4) | 45 (4.5) | |||
| ≥6 h | 6 (0.6) | 27 (2.7) | 42 (4.2) | |||
| Cooking | <1 h | 348 (34.8) | 194 (19.4) | 12 (1.2) | <0.001 | <0.001 |
| 1–5 h | 90 (9.0) | 263 (26.3) | 38 (3.8) | |||
| ≥6 h | 8 (0.8) | 20 (2.0) | 27 (2.7) | |||
| Doing professional work | <1 h | 132 (13.2) | 75 (7.5) | 9 (0.9) | <0.001 | <0.001 |
| 1–5 h | 81 (8.1) | 300 (30.0) | 60 (6.0) | |||
| ≥6 h | 31 (3.1) | 122 (12.2) | 190 (19.0) | |||
| Leisure entertainment activities | <1 h | 217 (21.7) | 188 (18.8) | 15 (1.5) | <0.001 | <0.001 |
| 1–5 h | 92 (9.2) | 344 (34.4) | 54 (5.4) | |||
| ≥6 h | 9 (0.9) | 36 (3.6) | 45 (4.5) | |||
| On social media | <1 h | 236 (23.6) | 185 (18.5) | 10 (1.0) | <0.001 | <0.001 |
| 1–5 h | 89 (8.9) | 346 (34.6) | 43 (4.3) | |||
| ≥6 h | 10 (1.0) | 32 (3.2) | 49 (4.9) | |||
| Socializing with family or roommates | <1 h | 281 (28.1) | 134 (13.4) | 11 (1.1) | 0.93 | 0.93 |
| 1–5 h | 134 (13.4) | 286 (28.6) | 45 (4.5) | |||
| ≥6 h | 11 (1.1) | 39 (3.9) | 59 (5.9) | |||
| Travelling in the city | <1 h | 350 (35.0) | 91 (9.1) | 7 (0.7) | <0.001 | <0.001 |
| 1–5 h | 269 (26.9) | 176 (17.6) | 24 (2.4) | |||
| ≥6 h | 31 (3.1) | 24 (2.4) | 28 (2.8) | |||
| Watching recipe related videos | <1 h | 358 (35.8) | 190 (19.0) | 20 (2.0) | <0.001 | <0.001 |
| 1–5 h | 89 (8.9) | 238 (23.8) | 42 (4.2) | |||
| ≥6 h | 5 (0.5) | 18 (1.8) | 40 (4.0) | |||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Madan, J.; Blonquist, T.; Rao, E.; Marwaha, A.; Mehra, J.; Bharti, R.; Sharma, N.; Samaddar, R.; Pandey, S.; Mah, E.; et al. Effect of COVID-19 Pandemic-Induced Dietary and Lifestyle Changes and Their Associations with Perceived Health Status and Self-Reported Body Weight Changes in India: A Cross-Sectional Survey. Nutrients 2021, 13, 3682. https://doi.org/10.3390/nu13113682
Madan J, Blonquist T, Rao E, Marwaha A, Mehra J, Bharti R, Sharma N, Samaddar R, Pandey S, Mah E, et al. Effect of COVID-19 Pandemic-Induced Dietary and Lifestyle Changes and Their Associations with Perceived Health Status and Self-Reported Body Weight Changes in India: A Cross-Sectional Survey. Nutrients. 2021; 13(11):3682. https://doi.org/10.3390/nu13113682
Chicago/Turabian StyleMadan, Jagmeet, Traci Blonquist, Eram Rao, Ankita Marwaha, Joshya Mehra, Richa Bharti, Nishi Sharma, Ritika Samaddar, Sandhya Pandey, Eunice Mah, and et al. 2021. "Effect of COVID-19 Pandemic-Induced Dietary and Lifestyle Changes and Their Associations with Perceived Health Status and Self-Reported Body Weight Changes in India: A Cross-Sectional Survey" Nutrients 13, no. 11: 3682. https://doi.org/10.3390/nu13113682
APA StyleMadan, J., Blonquist, T., Rao, E., Marwaha, A., Mehra, J., Bharti, R., Sharma, N., Samaddar, R., Pandey, S., Mah, E., Shete, V., Chu, Y., & Chen, O. (2021). Effect of COVID-19 Pandemic-Induced Dietary and Lifestyle Changes and Their Associations with Perceived Health Status and Self-Reported Body Weight Changes in India: A Cross-Sectional Survey. Nutrients, 13(11), 3682. https://doi.org/10.3390/nu13113682








