Reduced Rank Regression-Derived Dietary Patterns Related to the Fatty Liver Index and Associations with Type 2 Diabetes Mellitus among Ghanaian Populations under Transition: The RODAM Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Population
2.2. Assessment of NAFLD Proxy Markers
2.3. Dietary Assessment
2.4. Assessment of Covariates
3. Statistical Analysis
3.1. Descriptive Statistics
3.2. Reduced Rank Regression
3.3. Association Analyses
3.4. Sensitivity Analysis
4. Results
4.1. Study Population
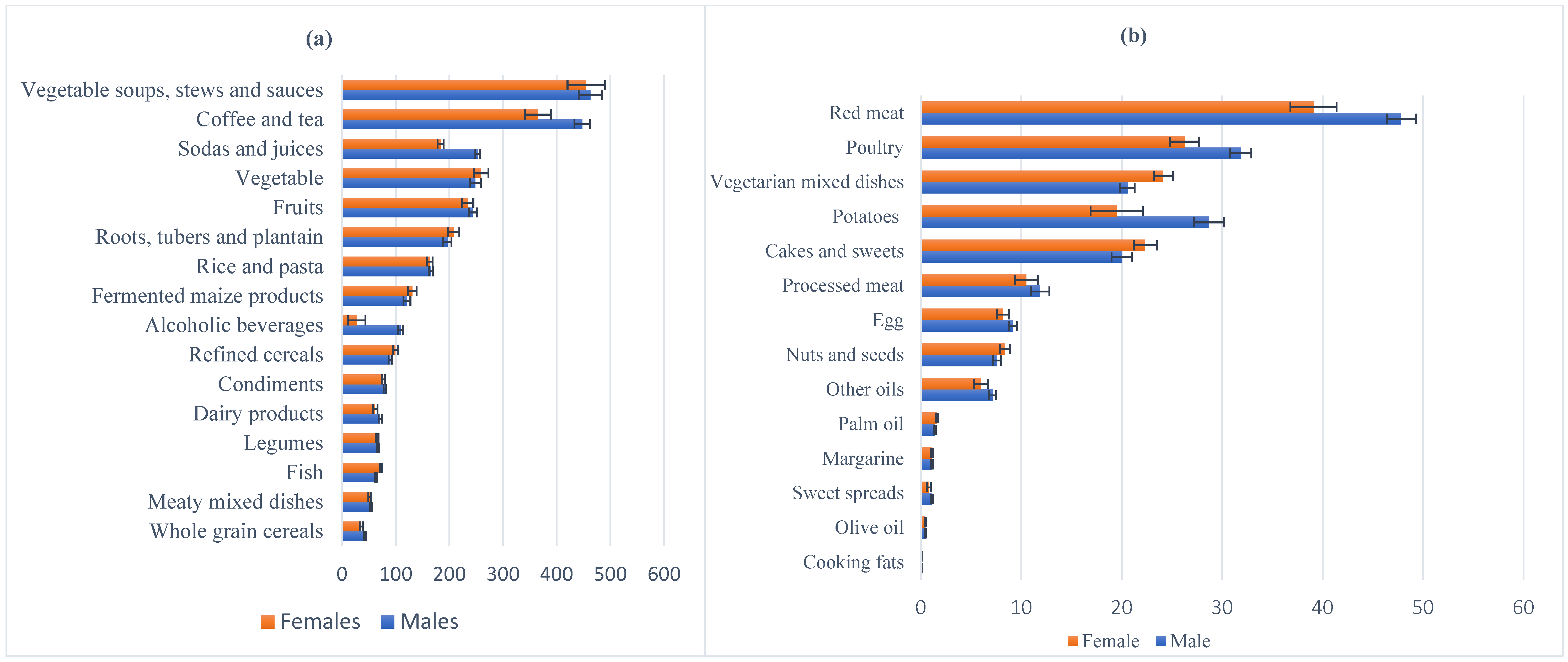
4.2. Intakes of Energy, Nutrients and Food Groups
4.3. RRR-Derived Dietary Patterns Related to the Fatty Liver Index
4.4. Associations of FLI-Related Pattern Scores with T2DM
4.5. RRR-Derived Dietary Patterns Related to the NAFLD Biomarkers
4.6. Associations of NAFLD Biomarker-Related Pattern Scores with T2DM
5. Discussion
5.1. Dietary Patterns and Proxy Markers of NALFD and T2DM
5.2. Strengths and Limitations
6. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Agyemang, C.; Meeks, K.; Beune, E.; Owusu-Dabo, E.; Mockenhaupt, F.P.; Addo, J.; de Graft Aikins, A.; Bahendeka, S.; Danquah, I.; Schulze, M.B.; et al. Obesity and type 2 diabetes in sub-Saharan Africans–Is the burden in today’s Africa similar to African mi-grants in Europe? The RODAM study. BMC Med. 2016, 14, 166. [Google Scholar] [CrossRef] [Green Version]
- Onyekwere, C.A.; Ogbera, A.O.; Balogun, B.O. Non-alcoholic fatty liver disease and the metabolic syndrome in an urban hos-pital serving an African community. Ann. Hepatol. 2016, 10, 119–124. [Google Scholar] [CrossRef]
- Ahmed, M.H.; Noor, S.K.; Bushara, S.O.; Husain, N.E.; Elmadhoun, W.M.; Ginawi, I.A.; Osman, M.M.; Mahmoud, A.O.; Almobarak, A.O. Non-alcoholic fatty liver disease in Africa and Middle East: An attempt to predict the present and future impli-cations on the healthcare system. Gastroenterol. Res. 2017, 10, 271. [Google Scholar] [CrossRef] [Green Version]
- Campos-Murguía, A.; Ruiz-Margáin, A.; González-Regueiro, J.; Macías-Rodríguez, R.U. Clinical assessment and management of liver fibrosis in non-alcoholic fatty liver disease. World J. Gastroenterol. 2020, 26, 5919–5943. [Google Scholar] [CrossRef]
- Lallukka, S.; Yki-Järvinen, H. Non-alcoholic fatty liver disease and risk of type 2 diabetes. Best Pract. Res. Clin. Endocrinol. Metab. 2016, 30, 385–395. [Google Scholar] [CrossRef] [Green Version]
- Machado, M.V.; Cortez-Pinto, H. Non-alcoholic fatty liver disease: What the clinician needs to know. World J. Gas-Troenterol. 2014, 20, 12956. [Google Scholar] [CrossRef]
- Idalsoaga, F.; Kulkarni, A.V.; Mousa, O.Y.; Arrese, M.; Arab, J.P. Non-alcoholic Fatty Liver Disease and Alcohol-Related Liver Disease: Two Intertwined Entities. Front. Med. 2020, 7, 7. [Google Scholar] [CrossRef]
- Lee, B.-W.; Lee, Y.H.; Park, C.Y.; Rhee, E.J.; Lee, W.Y.; Kim, N.H.; Choi, M.K.; Park, K.-G.; Choi, Y.-K.; Cha, B.S.; et al. Non-alcoholic fatty liver disease in patients with type 2 diabetes mellitus: A position statement of the fatty liver re-search group of the korean diabetes association. Diabetes Metab. J. 2020, 44, 382–401. [Google Scholar] [CrossRef]
- Ciardullo, S.; Monti, T.; Perseghin, G. High Prevalence of Advanced Liver Fibrosis Assessed by Transient Elastography among U.S. Adults with Type 2 Diabetes. Diabetes Care 2021, 44, 519–525. [Google Scholar] [CrossRef]
- Galbete, C.; Nicolaou, M.; Meeks, K.; Aikins, A.D.-G.; Addo, J.; Amoah, S.K.; Smeeth, L.; Owusu-Dabo, E.; Klipstein-Grobusch, K.; Bahendeka, S.; et al. Food consumption, nutrient intake, and dietary patterns in Ghanaian migrants in Europe and their compatriots in Ghana. Food Nutr. Res. 2017, 61, 1341809. [Google Scholar] [CrossRef] [Green Version]
- Erridge, C. Diet, commensals and the intestine as sources of pathogen-associated molecular patterns in atherosclerosis, type 2 diabetes and non-alcoholic fatty liver disease. Atherosclerosis 2011, 216, 1–6. [Google Scholar] [CrossRef]
- Jegatheesan, P.; De Bandt, J. Fructose and NAFLD: The Multifaceted Aspects of Fructose Metabolism. Nutrients 2017, 9, 230. [Google Scholar] [CrossRef] [Green Version]
- Yki-Järvinen, H.; Luukkonen, P.K.; Hodson, L.; Moore, J.B. Dietary carbohydrates and fats in nonalcoholic fatty liver disease. Nat. Rev. Gastroenterol. Hepatol. 2021, 1–17. [Google Scholar] [CrossRef]
- Della Pepa, G.; Vetrani, C.; Lombardi, G.; Bozzetto, L.; Annuzzi, G.; Rivellese, A.A. Isocaloric Dietary Changes and Non-Alcoholic Fatty Liver Disease in High Cardiometabolic Risk Individuals. Nutrients 2017, 9, 1065. [Google Scholar] [CrossRef] [Green Version]
- Tana, C.; Ballestri, S.; Ricci, F.; Di Vincenzo, A.; Ticinesi, A.; Gallina, S.; Giamberardino, M.A.; Cipollone, F.; Sutton, R.; Vettor, R.; et al. Cardiovascular Risk in Non-Alcoholic Fatty Liver Disease: Mechanisms and Therapeutic Implications. Int. J. Environ. Res. Public Health 2019, 16, 3104. [Google Scholar] [CrossRef] [Green Version]
- Frank, L.K.; Jannasch, F.; Kröger, J.; Bedu-Addo, G.; Mockenhaupt, F.P.; Schulze, M.B.; Danquah, I. A Dietary Pattern Derived by Reduced Rank Regression is Associated with Type 2 Diabetes in An Urban Ghanaian Population. Nutrients 2015, 7, 5497–5514. [Google Scholar] [CrossRef] [Green Version]
- Livingstone, K.M.; McNaughton, S.A. Association between diet quality, dietary patterns and cardiometabolic health in Aus-tralian adults: A cross-sectional study. Nutr. J. 2018, 17, 19. [Google Scholar] [CrossRef] [Green Version]
- Vermeulen, E.; Stronks, K.; Visser, M.; Brouwer, I.A.; Schene, A.H.; Mocking, R.J.T.; Colpo, M.; Bandinelli, S.; Ferrucci, L.; Nicolaou, M. The association between dietary patterns derived by reduced rank regression and depressive symptoms over time: The Invecchiare in Chianti (InCHIANTI) study. Br. J. Nutr. 2016, 115, 2145–2153. [Google Scholar] [CrossRef] [Green Version]
- Byrne, C.D.; Targher, G. NAFLD: A multisystem disease. J. Hepatol. 2015, 62, S47–S64. [Google Scholar] [CrossRef] [Green Version]
- Drescher, H.K.; Weiskirchen, S.; Weiskirchen, R. Current Status in Testing for Nonalcoholic Fatty Liver Disease (NAFLD) and Nonalcoholic Steatohepatitis (NASH). Cells 2019, 8, 845. [Google Scholar] [CrossRef] [Green Version]
- Younossi, Z.M.; Loomba, R.; Anstee, Q.M.; Rinella, M.E.; Bugianesi, E.; Marchesini, G.; Neuschwander-Tetri, B.A.; Serfaty, L.; Negro, F.; Caldwell, S.H.; et al. Diagnostic modalities for nonalcoholic fatty liver disease, nonalcoholic steatohepatitis, and associated fibrosis. Hepatology 2018, 68, 349–360. [Google Scholar] [CrossRef] [Green Version]
- Agyemang, C.; Beune, E.; Meeks, K.; Owusu-Dabo, E.; Agyei-Baffour, P.; Aikins, A.D.-G.; Dodoo, F.; Smeeth, L.; Addo, J.; Mockenhaupt, F.; et al. Rationale and cross-sectional study design of the Research on Obesity and type 2 Diabetes among African Migrants: The RODAM study. BMJ Open 2014, 4, e004877. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bedogni, G.; Bellentani, S.; Miglioli, L.; Masutti, F.; Passalacqua, M.; Castiglione, A.; Tiribelli, C. The Fatty Liver Index: A simple and accurate predictor of hepatic steatosis in the general population. BMC Gastroenterol. 2006, 6, 33. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Haskell, W.L.; Lee, I.M.; Pate, R.R.; Powell, K.E.; Blair, S.N.; Franklin, B.A.; Macera, C.A.; Heath, G.W.; Thompson, P.T.; Bauman, A. Physical activity and public health: Updated recommendation for adults from the American College of Sports Medicine and the American Heart Association. Circulation 2007, 116, 1081. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hoffmann, K.; Schulze, M.B.; Schienkiewitz, A.; Nöthlings, U.; Boeing, H. Application of a New Statistical Method to Derive Dietary Patterns in Nutritional Epidemiology. Am. J. Epidemiol. 2004, 159, 935–944. [Google Scholar] [CrossRef]
- Addo, J.; Agyemang, C.; de-Graft Aikins, A.; Beune, E.; Schulze, M.B.; Danquah, I.; Galbete, C.; Nicolaou, M.; Meeks, K.; Klipstein-Grobusch, K.; et al. Association between socioeconomic position and the prevalence of type 2 diabetes in Ghanaians in different geo-graphic locations: The RODAM study. J. Epidemiol. Community Health 2017, 71, 633–639. [Google Scholar] [CrossRef] [Green Version]
- He, K.; Li, Y.; Guo, X.; Zhong, L.; Tang, S. Food groups and the likelihood of non-alcoholic fatty liver disease: A systematic review and meta-analysis. Br. J. Nutr. 2020, 124, 1–13. [Google Scholar] [CrossRef]
- Birerdinc, A.; Stepanova, M.; Pawloski, L.; Younossi, Z.M. Caffeine is protective in patients with non-alcoholic fatty liver disease. Aliment. Pharmacol. Ther. 2012, 35, 76–82. [Google Scholar] [CrossRef]
- Molloy, J.W.; Calcagno, C.J.; Williams, C.D.; Jones, F.J.; Torres, D.M.; Harrison, S.A. Association of coffee and caffeine consumption with fatty liver disease, nonalcoholic steatohepatitis, and degree of hepatic fibrosis. Hepatology 2012, 55, 429–436. [Google Scholar] [CrossRef]
- Xia, Y.; Zhang, Q.; Liu, L.; Meng, G.; Wu, H.; Bao, X.; Gu, Y.; Sun, S.; Wang, X.; Zhou, M.; et al. Intermediary effect of inflammation on the association between dietary patterns and non-alcoholic fatty liver disease. Nutrients 2020, 71, 110562. [Google Scholar] [CrossRef]
- Franco, I.; Bianco, A.; Mirizzi, A.; Campanella, A.; Bonfiglio, C.; Sorino, P.; Notarnicola, M.; Tutino, V.; Cozzolongo, R.; Giannuzzi, V.; et al. Physical Activity and Low Glycemic Index Mediterranean Diet: Main and Modification Effects on NAFLD Score. Results from a Randomized Clinical Trial. Nutrients 2020, 13, 66. [Google Scholar] [CrossRef] [PubMed]
- Abenavoli, L.; Boccuto, L.; Federico, A.; Dallio, M.; Loguercio, C.; Di Renzo, L.; De Lorenzo, A. Diet and Non-Alcoholic Fatty Liver Disease: The Mediterranean Way. Int. J. Environ. Res. Public Health 2019, 16, 3011. [Google Scholar] [CrossRef] [Green Version]
- Giraldi, L.; Miele, L.; Aleksovska, K.; Manca, F.; Leoncini, E.; Biolato, M.; Pirro, M.A.; Marrone, G.; Cefalo, C.; Racco, S.; et al. Mediterranean diet and the prevention of non-alcoholic fatty liver disease: Results from a case-control study. Eur. Rev. Med. Pharmacol. Sci. 2020, 24, 7391–7398. [Google Scholar] [PubMed]
- Noureddin, M.; Jones, C.; Alkhouri, N.; Gomez, E.V.; Dieterich, D.T.; Rinella, M.E.; Therapondos, G.; Girgrah, N.; Mantry, P.S.; Sussman, N.L.; et al. Screening for Nonalcoholic Fatty Liver Disease in Persons with Type 2 Diabetes in the United States Is Cost-effective: A Comprehensive Cost-Utility Analysis. Gastroenterology 2020, 159, 1985–1987.e4. [Google Scholar] [CrossRef] [PubMed]
- Treviño, L.S.; Katz, T.A. Endocrine Disruptors and Developmental Origins of Nonalcoholic Fatty Liver Disease. Endocrinology 2017, 159, 20–31. [Google Scholar] [CrossRef] [PubMed]
- Van Dijk, A.-M.; Dingerink, S.; Chilunga, F.P.; Meeks, K.A.C.; Bahendeka, S.; Schulze, M.B.; Danquah, I.; Osei, T.B.; Serné, E.; Agyemang, C.; et al. Metabolic-associated Fatty Liver Disease as Assessed by the Fatty Liver Index Among Migrant and Non-migrant Ghanaian Populations. J. Clin. Transl. Hepatol. 2021, 9, 494–502. [Google Scholar] [PubMed]
- Christensen, D.L.; Faurholt-Jepsen, D.; Birkegaard, L.; Mwaniki, D.L.; Boit, M.K.; Kilonzo, B.; Brage, S.; Friis, H.; Tetens, I.; Borch-Johnsen, K.; et al. Cardiovascular risk factors in rural Kenyans are associated with differential age gradients, but not modified by sex or ethnicity. Ann. Hum. Biol. 2015, 43, 42–49. [Google Scholar] [CrossRef] [Green Version]
- Paquette, M.; Gauthier, D.; Chamberland, A.; Prat, A.; Rolfe, E.D.L.; Rasmussen, J.J.; Kaduka, L.; Seidah, N.G.; Bernard, S.; Christensen, D.L.; et al. Circulating PCSK9 is associated with liver biomarkers and hepatic steatosis. Clin. Biochem. 2020, 77, 20–25. [Google Scholar] [CrossRef]
- Danquah, I.; Othmer, T.; Frank, L.K.; Bedu-Addo, G.; Schulze, M.B.; Mockenhaupt, F.P. The TCF7L2 rs7903146 (T) allele is associated with type 2 diabetes in urban Ghana: A hospital-based case–control study. BMC Med. Genet. 2013, 14, 96. [Google Scholar] [CrossRef] [Green Version]
- Darko, S.N.; Meeks, K.A.; Owiredu, W.K.; Laing, E.F.; Boateng, D.; Beune, E.; Addo, J.; Aikins, A.D.-G.; Bahendeka, S.; Mockenhaupt, F.; et al. Anthropometric indices and their cut-off points in relation to type 2 diabetes among Ghanaian migrants and non-migrants: The RODAM study. Diabetes Res. Clin. Pr. 2021, 173, 108687. [Google Scholar] [CrossRef] [PubMed]
- Goedecke, J.H.; Olsson, T. Pathogenesis of type 2 diabetes risk in black Africans: A South African perspective. J. Intern. Med. 2020, 288, 284–294. [Google Scholar] [CrossRef] [Green Version]
- Aljefree, N.; Ahmed, F. Association between dietary pattern and risk of cardiovascular disease among adults in the Middle East and North Africa region: A systematic review. Food Nutr. Res. 2015, 59, 27486. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cempaka, A.R.; Tseng, S.-H.; Yuan, K.-C.; Bai, C.-H.; Tinkov, A.A.; Skalny, A.V.; Chang, J.-S. Dysregulated Iron Metabolism-Associated Dietary Pattern Predicts an Altered Body Composition and Metabolic Syndrome. Nutrients 2019, 11, 2733. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fung, T.T.; Schulze, M.B.; Manson, J.E.; Willett, W.C.; Hu, F.B. Dietary Patterns, Meat Intake, and the Risk of Type 2 Diabetes in Women. Arch. Intern. Med. 2004, 164, 2235–2240. [Google Scholar] [CrossRef]
- Jannasch, F.; Kröger, J.; Schulze, M.B. Dietary Patterns and Type 2 Diabetes: A Systematic Literature Review and Me-ta-Analysis of Prospective Studies. J. Nutr. 2017, 147, 1174–1182. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Galbete, C.; Nicolaou, M.; Meeks, K.; Klipstein-Grobusch, K.; Aikins, A.D.-G.; Addo, J.; Amoah, S.K.; Smeeth, L.; Owusu-Dabo, E.; Spranger, J.; et al. Dietary patterns and type 2 diabetes among Ghanaian migrants in Europe and their compatriots in Ghana: The RODAM study. Nutr. Diabetes 2018, 8, 25. [Google Scholar] [CrossRef] [PubMed]
- Feinglos, M.N.; Bethel, M.A. Type 2 Diabetes Mellitus: An Evidence-Based Approach to Practical Management; Springer Science & Business Media: Berlin/Heidelberg, Germany, 2008. [Google Scholar]
- Von Eckardstein, A. Laboratory diagnostics of non-alcoholic fatty liver disease. Laboratoriums Medizin 2015, 38, s1. [Google Scholar] [CrossRef] [Green Version]
- Olubamwo, O.O.; Virtanen, J.K.; Pihlajamaki, J.; Mantyselka, P.; Tuomainen, T.P. Fatty liver index as a predictor of increased risk of cardiometabolic disease: Finding from the Kuopio Is-chaemic Heart Disease Risk Factor Study Cohort. BMJ Open 2019, 9, e031420. [Google Scholar] [CrossRef] [Green Version]
- Weikert, C.; Schulze, M.B. Evaluating dietary patterns: The role of reduced rank regression. Curr. Opin. Clin. Nutr. Metab. Care 2016, 19, 341–346. [Google Scholar] [CrossRef] [PubMed]
- Danquah, I.; Bedu-Addo, G.; Terpe, K.-J.; Micah, F.; Amoako, Y.A.; Awuku, Y.A.; Dietz, E.; Van Der Giet, M.; Spranger, J.; Mockenhaupt, F.P. Diabetes mellitus type 2 in urban Ghana: Characteristics and associated factors. BMC Public Health 2012, 12, 210. [Google Scholar] [CrossRef] [Green Version]
| Characteristics | Total (n = 3687) | Men (n = 1366) | Women (n = 2321) | Rural Ghana (n = 820) | Urban Ghana (n = 1358) | Amsterdam (n = 707) | Berlin (n = 451) | London (n = 351) |
|---|---|---|---|---|---|---|---|---|
| Sex (female%) | 63.0 | - | - | 61.6 | 72.2 | 60.1 | 45.0 | 59.0 |
| Age (years) | 46.1 ± 11.1 | 46.9 ± 11.3 | 45.6 ± 10.9 | 46.7 ± 12.6 | 45.3 ± 11.4 | 46.6 ± 8.5 | 45.2 ± 10.4 | 47.9 ± 10.9 |
| Education | ||||||||
| Never or elementary% | 37.6 | 21.9 | 46.9 | 56.8 | 43.9 | 35.5 | 9.3 | 9.1 |
| Low | 37.7 | 41.6 | 35.5 | 31.6 | 38.9 | 37.8 | 50.1 | 31.6 |
| Intermediate | 16.2 | 22.5 | 12.5 | 7.9 | 12.5 | 21.8 | 26.6 | 24.8 |
| Higher vocational | 8.5 | 14.1 | 5.2 | 3.7 | 4.71 | 5.0 | 14.0 | 34.5 |
| Length of stay (years) | - | - | - | - | - | 16.4 ± 8.1 | 17.0 ± 10.9 | 17.2 ± 11.0 |
| Body mass index (kg/m2) | 26.7 ± 5.5 | 24.8 ± 4.4 | 27.8 ± 5.7 | 22.7 ± 4.3 | 26.9 ± 5.4 | 28.9 ± 5 | 27.6 ± 4.8 | 29.4 ± 4.8 |
| Waist circumference (cm) | 89.5 ± 12.5 | 87 ± 12.1 | 91 ± 12.5 | 81.2 ± 10.9 | 89.4 ± 11.8 | 94.6 ± 11.6 | 92.2 ± 11.5 | 95.4 ± 11.3 |
| Smoking (current or former%) | 9.3 | 19.6 | 3.2 | 7.9 | 6.9 | 11.6 | 18.4 | 5.4 |
| Physical activities (MET-min/day) | 72 (14–168) | 96 (28–196) | 56 (10–156) | 90 (36–161) | 60 (6–156) | 88.7 (26–258) | 72 (12–198) | 28 (5–112) |
| Total energy intake (kcal/day) | 2533 ± 837 | 2628 ± 827 | 2477 ± 817 | 2594 ± 828 | 2298 ± 661 | 2478 ± 854 | 2929 ± 944 | 2898 ± 953 |
| Carbohydrate intake (energy%) | 53.0 ± 9.1 | 52.2 ± 9.5 | 53.5 ± 8.9 | 56.4.5 ± 8.3 | 54.5 ± 8.1 | 50.5 ± 8.3 | 48.5 ± 10.9 | 50.2 ± 9.6 |
| Fat intake (energy%) | 32.2 ± 8.2 | 32 ± 8.6 | 32.3 ± 8 | 31.4 ± 7.3 | 31.6 ± 7.2 | 32.1 ± 8.3 | 33.7 ± 10.6 | 34.1 ± 9.6 |
| Protein intake (energy%) | 13.8 ± 2.9 | 13.9 ± 3.1 | 13.8 ± 2.9 | 11.5 ± 2.2 | 13.6 ± 2.4 | 15.8 ± 2.7 | 14.8 ± 3.1 | 15.1 ± 2.9 |
| Alcohol intake (g/day) | 0 (0–0.1) | 0 (0–0.3) | 0 (0–0.1) | 0 (0–0.1) | 0 (0–0.1) | 0.1 (0–0.4) | 0.1 (0–0.6) | 0 (0–0.1) |
| AST U/L | 32.3 (26.6–39.8) | 35.1 (29.1–43.1) | 30.6 (25.3–37.7) | 36.1 (30.4–43.1) | 34.4 (28.7–41.5) | 26.1 (22.4–30.8) | 28.9 (24.7–34.9) | 34.1 (28.0–43.1) |
| ALT U/L | 19.2 (14.9–25.7) | 23.0 (17.4–31.2) | 17.6 (13.9–22.7) | 19.2 (15–24.9) | 19.3 (15–25.8) | 17.4 (13.7–23.0) | 19.9 (14.8–26.9) | 22.5 (18.3–30.3) |
| GGT U/L | 30.8 (23.2–43.1) | 37.4 (27.3–52.6) | 27.9 (21.7–37.3) | 29.5 (22.3–42.2) | 31.4 (23.9–42.9) | 30.2 (22.8–42.0) | 32.9 (24.7–46.1) | 30.6 (22.7–43.9) |
| CRP mg/L | 0.7 (0.2–2.5) | 0.5 (0.1–1.5) | 0.9 (0.2- 3.2) | 0.7 (0.2–2.6) | 0.9 (0.2–3.1) | 0.8 (0.2–2.3) | 0.5 (0.2–1.9) | 0.8 (0.2–2.3) |
| Total cholesterol (mmol/L) | 5.0 ± 1.1 | 4.9 ± 1.1 | 5.1 ± 1.1 | 4.6 ± 1.1 | 5.2 ± 1.2 | 5.0 ± 1.1 | 5.1 ± 1.1 | 5.0 ± 1.0 |
| LDL-cholesterol (mmol/L) | 3.2 ± 1.0 | 3.1 ± 1.0 | 3.2 ± 1.0 | 2.8 ± 1.0 | 3.4 ± 1.0 | 3.2 ± 0.9 | 3.2 ± 1.0 | 3.3 ± 0.9 |
| HDL-cholesterol (mmol/L) | 1.3 ± 0.4 | 1.3 ± 0.4 | 1.3 ± 0.4 | 1.2 ± 0.4 | 1.3 ± 0.3 | 1.4 ± 0.3 | 1.5 ± 0.4 | 1.3 ± 0.3 |
| Triglycerides (mmol/L) | 0.9 (0.7–1.2) | 1.0 (0.7–1.3) | 0.9 (0.7–1.2) | 1.0 (0.8- 1.3) | 1.0 (0.8–1.3) | 0.8 (0.6–1.0) | 0.9 (0.6–1.1) | 0.8 (0.6–1.1) |
| Fatty Liver Index | 2.6 ± 6.3 | 2.0 ± 5.4 | 2.9 ± 6.8 | 1.0 ± 3.2 | 2.8 ± 6.7 | 3.3 ± 7.2 | 3.1 ± 7.3 | 3.1 ± 6.0 |
| Food Group | Men (n = 1366) | Women (n = 2321) | ||
|---|---|---|---|---|
| Explained Variation (%) | Factor Loading | Explained Variation (%) | Factor Loading | |
| Poultry | 30.8 | 0.32 | 16.6 | 0.29 |
| Whole-grain cereals | 21.5 | 0.27 | 15.8 | 0.29 |
| Coffee and tea | 19.9 | 0.26 | 21.0 | 0.33 |
| Condiments | 18.3 | 0.25 | 15.7 | 0.28 |
| Potatoes | 17.8 | 0.25 | 2.1 | 0.10 |
| Alcoholic beverages | 10.3 | 0.19 | 7.5 | 0.20 |
| Margarine | 10.2 | 0.19 | 10.6 | 0.23 |
| Olive oil | 7.7 | 0.16 | 0.4 | 0.04 |
| Processed meat | 7.2 | 0.16 | 0.3 | 0.04 |
| Other oils | 5.5 | 0.14 | 2.4 | 0.11 |
| Dairy products | 4.9 | 0.13 | 0.4 | 0.04 |
| Sodas and juices | 3.8 | 0.11 | 1.8 | 0.10 |
| Cakes and sweets | 3.4 | 0.11 | 0.6 | −0.05 |
| Red meat | 2.6 | 0.09 | 0.0 | 0.01 |
| Vegetables | 2.5 | 0.09 | 5.2 | 0.16 |
| Sweet spreads | 1.7 | 0.08 | 0.0 | −0.01 |
| Cooking fats | 1.5 | 0.07 | 0.2 | −0.03 |
| Eggs | 1.3 | 0.07 | 2.1 | −0.10 |
| Rice and pasta | 1.1 | 0.06 | 1.7 | 0.09 |
| Vegetable soups, stews and sauces | 0.9 | 0.06 | 0.0 | −0.01 |
| Nuts and seeds | 0.5 | 0.04 | 1.5 | 0.09 |
| Fish | 0.1 | 0.02 | 9.5 | 0.22 |
| Meat mixed dishes | 2.1 | −0.08 | 1.3 | −0.08 |
| Fruits | 4.1 | −0.12 | 1.6 | −0.09 |
| Legumes | 4.8 | −0.13 | 2.4 | −0.11 |
| Vegetarian mixed dishes | 7.2 | −0.16 | 0.9 | −0.07 |
| Fermented maize products | 18.4 | −0.25 | 19.8 | −0.32 |
| Refined cereal | 22.4 | −0.27 | 13.3 | −0.26 |
| Roots, tubers and plantains | 28.7 | −0.31 | 22.0 | −0.34 |
| Palm oil | 35.1 | −0.34 | 17.3 | −0.30 |
| Total | 9.9 | 6.5 | ||
| Model | Odds Ratio (95% Confidence Interval) | ||||||
|---|---|---|---|---|---|---|---|
| Q1 | Q2 | Q3 | Q4 | Q5 | p for Trend | Per 1 Score-SD | |
| Men | |||||||
| Diabetes/Control | 17/256 | 22/251 | 31/243 | 46/227 | 43/230 | ||
| Crude | 1 (reference) | 1.32 (0.69, 2.54) | 1.92 (1.06, 3.56) | 3.05 (1.70, 5.47) | 2.82 (1.56, 5.07) | <0.0001 | 1.55 (1.30, 1.86) |
| Model 1 | 1 (reference) | 1.41 (0.71, 2.79) | 1.79 (0.90, 3.56) | 2.30 (1.07, 4.97) | 1.97 (0.89, 4.35) | 0.11 | 1.34 (1.04, 1.73) |
| Model 2 | 1(reference) | 1.25 (0.62, 2.49) | 1.58 (0.79, 3.16) | 2.14 (0.98, 4.68) | 2.03 (0.90, 4.60) | 0.07 | 1.45 (1.10, 1.93) |
| Women | |||||||
| Diabetes/Control | 25/439 | 38/426 | 32/433 | 47/417 | 47/417 | ||
| Crude | 1(reference) | 1.57 (0.93, 2.64) | 1.30 (0.76, 2.23) | 1.98 (1.20, 3.27) | 1.98 (1.20, 3.27) | <0.005 | 1.24 (1.07, 1.44) |
| Model 1 | 1(reference) | 1.59 (0.93, 2.71) | 1.31 (0.75, 2.30) | 2.05 (1.19, 3.54) | 1.98 (1.09, 3.59) | <0.02 | 1.23 (1.03, 1.48) |
| Model 2 | 1(reference) | 1.28 (0.74, 2.21) | 1.03 (0.58, 1.83) | 1.64 (0.94, 2.84) | 1.65 (0.90, 3.02) | 0.07 | 1.16 (0.95, 1.42) |
| Food Group | Men (n = 1366) | Women (n = 2321) | ||
|---|---|---|---|---|
| Explained Variation (%) | Factor Loading | Explained Variation (%) | Factor Loading | |
| Whole-grain cereals | 36.5 | 0.33 | 25.3 | −0.26 |
| Poultry | 26.6 | 0.28 | 35.1 | −0.31 |
| Dairy products | 25.8 | 0.28 | 13.4 | −0.19 |
| Coffee and tea | 23.8 | 0.27 | 44.9 | −0.35 |
| Condiments | 21.4 | 0.25 | 33.0 | −0.30 |
| Potatoes | 19.0 | 0.24 | 28.7 | −0.28 |
| Margarine | 12.8 | 0.20 | 14.6 | −0.20 |
| Olive oil | 13.6 | 0.20 | 18.3 | −0.22 |
| Sodas and juices | 7.9 | 0.15 | 6.1 | −0.13 |
| Sweet spreads | 7.8 | 0.15 | 6.6 | −0.13 |
| Rice and pasta | 7.5 | 0.15 | 0.7 | −0.05 |
| Processed meat | 5.5 | 0.13 | 5.7 | −0.13 |
| Palm oil | 32.7 | −0.31 | 27.1 | 0.27 |
| Roots, tubers and plantains | 30.6 | −0.30 | 12.4 | 0.18 |
| Fermented maize products | 23.5 | −0.26 | 6.1 | 0.13 |
| Vegetarian mixed dishes | 10.5 | −0.18 | 27.3 | 0.27 |
| Refined cereals | 5.6 | −0.13 | 7.4 | 0.14 |
| Cakes and sweets | 4.0 | 0.11 | 7.5 | −0.14 |
| Vegetables | 3.9 | 0.11 | 9.2 | −0.16 |
| Meaty mixed dishes | 4.1 | −0.11 | 0.9 | 0.05 |
| Legumes | 3.9 | −0.11 | 0.5 | −0.04 |
| Other oils | 2.8 | 0.09 | 4.2 | −0.11 |
| Cooking fats | 1.5 | 0.07 | 0.1 | −0.01 |
| Fish | 1.6 | −0.07 | 13.1 | 0.19 |
| Fruits | 1.4 | −0.06 | 1.7 | −0.07 |
| Eggs | 0.9 | 0.05 | 5.9 | −0.13 |
| Vegetable soups, stews and sauces | 0.3 | 0.03 | 0.1 | 0.01 |
| Red meat | 0.3 | −0.03 | 1.1 | −0.05 |
| Nuts and seeds | 0.4 | −0.03 | 0.0 | −0.01 |
| Alcoholic beverages | 0.1 | −0.02 | 6.3 | −0.13 |
| Total | 11.2 | 12.1 | ||
| Biomarker | Men (n = 1366) | Women (n = 2321) | ||
|---|---|---|---|---|
| Explained Variation (%) | Response Weight | Explained Variation (%) | Response Weight | |
| Cholesterol | 4.5 | 0.45 | 0.3 | 0.09 |
| LDL-cholesterol | 4.2 | 0.44 | 1.0 | 0.16 |
| HDL-cholesterol | 2.9 | 0.36 | 8.6 | −0.49 |
| AST | 7.4 | −0.58 | 12.3 | 0.58 |
| GGT | 1.5 | −0.26 | 0.3 | 0.09 |
| Triglycerides | 1.3 | −0.24 | 11.1 | 0.55 |
| C-reactive protein | 0.3 | −0.12 | 0.4 | 0.11 |
| ALT | 0.2 | 0.08 | 2.2 | 0.25 |
| Total | 2.80 | 4.50 | ||
| Odds Ratio (95% Confidence Interval) | |||||||
|---|---|---|---|---|---|---|---|
| Q1 | Q2 | Q3 | Q4 | Q5 | p for Trend | Per 1 Score-SD | |
| Men | |||||||
| Diabetes/Control | 15/258 | 27/246 | 33/241 | 47/226 | 37/236 | ||
| Crude | 1 (reference) | 1.89 (0.98, 3.63) | 2.36 (1.25, 4.44) | 3.58 (1.95, 6.57) | 2.7 0(1.44, 5.04) | <0.0002 | 1.42 (1.20, 1.68) |
| Model 1 | 1 (reference) | 1.91 (0.97, 3.76) | 2.06 (1.00, 4.22) | 2.42 (1.07, 5.50) | 1.64 (0.72, 3.75) | 0.578 | 1.15 (0.89, 1.48) |
| Model 2 | 1 (reference) | 1.76 (0.89, 3.50) | 1.8 (0.86, 3.75) | 2.07 (0.90, 4.78) | 1.44 (0.61, 3.40) | 0.743 | 1.13 (0.86, 1.49) |
| Model 3 | 1 (reference) | 1.62 (0.81–3.22) | 1.46 (0.69–3.10) | 1.70 (0.72–4.01) | 1.21 (0.50, 2.89) | 0.962 | 1.07 (0.81, 1.42) |
| Women | |||||||
| Diabetes/Control | 37/427 | 38/426 | 36/429 | 36/430 | 44/420 | ||
| Crude | 1 (reference) | 1.03 (0.64, 1.65) | 0.97 (0.60, 1.56) | 0.91 (0.56, 1.48) | 1.21 (0.77, 1.91) | 0.592 | 1.08 (0.93, 1.25) |
| Model 1 | 1 (reference) | 1.24 (0.76, 2.05) | 1.63 (0.84, 3.14) | 1.46 (0.73, 2.92) | 1.69 (0.84, 3.39) | 0.229 | 1.35 (1.05, 1.73) |
| Model 2 | 1 (reference) | 1.16 (0.70, 1.94) | 1.39 (0.69, 2.79) | 1.20 (0.57, 2.52) | 1.40 (0.67, 2.93) | 0.522 | 1.29 (0.99, 1.68) |
| Model 3 | 1 (reference) | 1.11 (0.66, 1.86) | 1.32 (0.65, 2.67) | 1.20 (0.57, 2.57) | 1.42 (0.67, 3.02) | 0.422 | 1.30 (0.99, 1.71) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Osei, T.B.; van Dijk, A.-M.; Dingerink, S.; Chilunga, F.P.; Beune, E.; Meeks, K.A.C.; Bahendeka, S.; Schulze, M.B.; Agyemang, C.; Nicolaou, M.; et al. Reduced Rank Regression-Derived Dietary Patterns Related to the Fatty Liver Index and Associations with Type 2 Diabetes Mellitus among Ghanaian Populations under Transition: The RODAM Study. Nutrients 2021, 13, 3679. https://doi.org/10.3390/nu13113679
Osei TB, van Dijk A-M, Dingerink S, Chilunga FP, Beune E, Meeks KAC, Bahendeka S, Schulze MB, Agyemang C, Nicolaou M, et al. Reduced Rank Regression-Derived Dietary Patterns Related to the Fatty Liver Index and Associations with Type 2 Diabetes Mellitus among Ghanaian Populations under Transition: The RODAM Study. Nutrients. 2021; 13(11):3679. https://doi.org/10.3390/nu13113679
Chicago/Turabian StyleOsei, Tracy Bonsu, Anne-Marieke van Dijk, Sjoerd Dingerink, Felix Patience Chilunga, Erik Beune, Karlijn Anna Catharina Meeks, Silver Bahendeka, Matthias Bernd Schulze, Charles Agyemang, Mary Nicolaou, and et al. 2021. "Reduced Rank Regression-Derived Dietary Patterns Related to the Fatty Liver Index and Associations with Type 2 Diabetes Mellitus among Ghanaian Populations under Transition: The RODAM Study" Nutrients 13, no. 11: 3679. https://doi.org/10.3390/nu13113679
APA StyleOsei, T. B., van Dijk, A.-M., Dingerink, S., Chilunga, F. P., Beune, E., Meeks, K. A. C., Bahendeka, S., Schulze, M. B., Agyemang, C., Nicolaou, M., Holleboom, A. G., & Danquah, I. (2021). Reduced Rank Regression-Derived Dietary Patterns Related to the Fatty Liver Index and Associations with Type 2 Diabetes Mellitus among Ghanaian Populations under Transition: The RODAM Study. Nutrients, 13(11), 3679. https://doi.org/10.3390/nu13113679








