Factors Related to Diet Quality: A Cross-Sectional Study of 1055 University Students
Abstract
1. Introduction
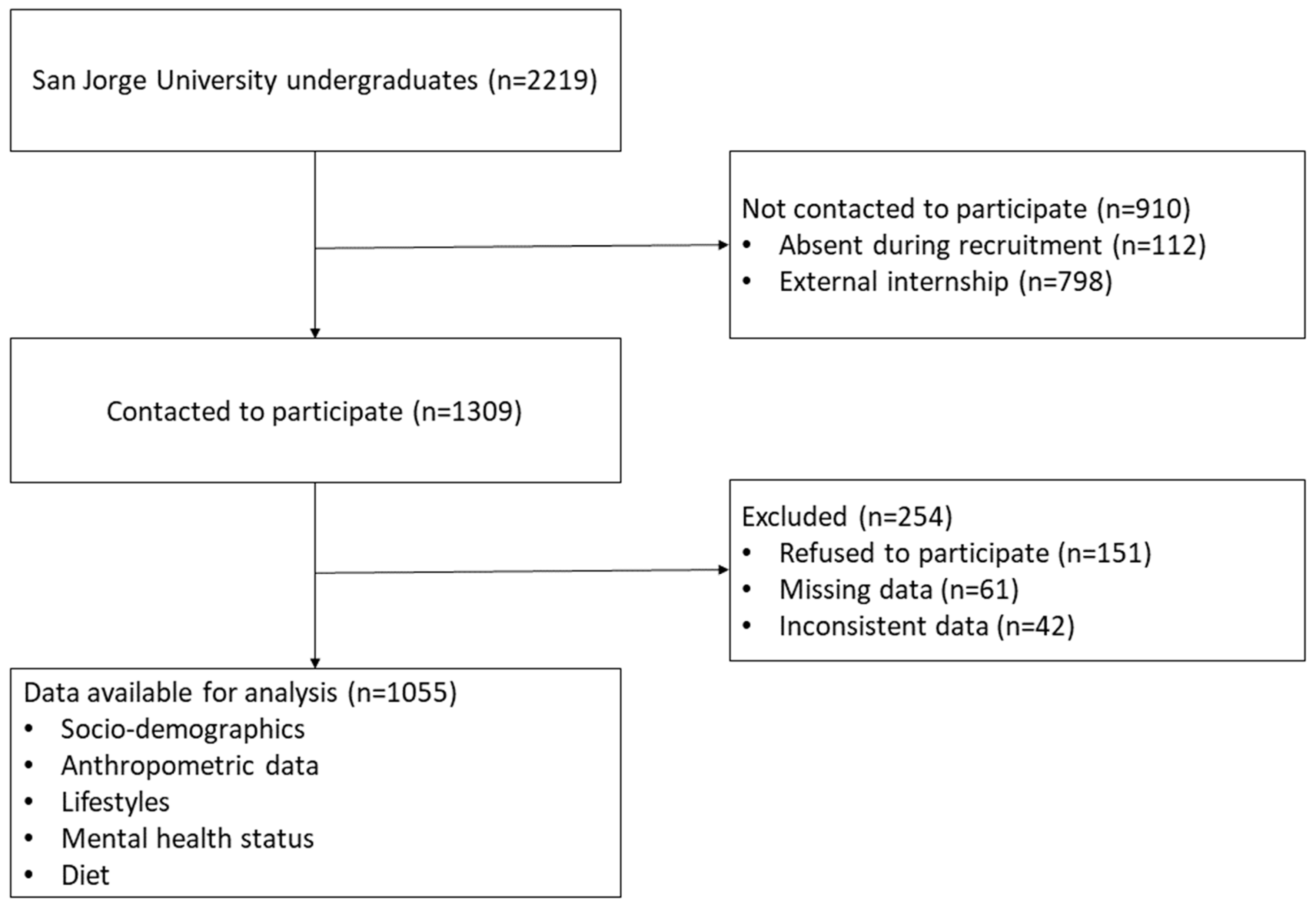
2. Materials and Methods
2.1. Design and Study Population
2.2. Data Collection
- Anxiety: Normal (0–7 points), mild (8–9), moderate (10–14), severe (15–19), and extremely severe (>19);
- Depression: Normal (0–9 points), mild (10–13), moderate (14–20), severe (21–27), and extremely severe (>27);
- Stress: Normal (0–14 points), mild (15–18), moderate (19–25), severe (26–33), and extremely severe (>33).
2.3. Data Analysis
3. Results
4. Discussion
5. Conclusions and Recommendations
- (1)
- the early detection of trends of poor DQ among students entering university as part of existing systems that offer students support;
- (2)
- activities that aim to interrupt and prevent unhealthy dietary habits such as providing gender-specific information about immediate health concerns or organising community-wide public health campaigns that ensure that students have access to needed resources and affordable healthy foods;
- (3)
- the empowerment of students by encouraging, for example, the acquisition of skills for making dietary choices and increasing resilience so that they can develop their own adaptive strategies to confront dietary problems and avoid unhealthy dietary habits;
- (4)
- the consideration and handling of any underlying mental health conditions that could be present among university students with poor DQ.
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Jankovic, N.; Geelen, A.; Streppel, M.T.; de Groot, L.C.; Kiefte-de Jong, J.C.; Orfanos, P.; Bamia, C.; Trichopoulou, A.; Boffetta, P.; Es Bobak, M.; et al. WHO Guidelines for a Healthy Diet and Mortality from Cardiovascular Disease in European and American Elderly: The CHANCES Project. Am. J. Clin. Nutr. 2015, 102, 745–756. [Google Scholar] [CrossRef]
- Jankovic, N.; Geelen, A.; Streppel, M.T.; de Groot, L.C.P.G.M.; Orfanos, P.; van den Hooven, E.H.; Pikhart, H.; Boffetta, P.; Trichopoulou, A.; Bobak, M.; et al. Adherence to a Healthy Diet According to the World Health Organization Guidelines and All-Cause Mortality in Elderly Adults from Europe and the United States. Am. J. Epidemiol. 2014, 180, 978–988. [Google Scholar] [CrossRef] [PubMed]
- Liese, A.D.; Krebs-Smith, S.M.; Subar, A.F.; George, S.M.; Harmon, B.E.; Neuhouser, M.L.; Boushey, C.J.; Schap, T.E.; Reedy, J. The Dietary Patterns Methods Project: Synthesis of Findings across Cohorts and Relevance to Dietary Guidance. J. Nutr. 2015, 145, 393–402. [Google Scholar] [CrossRef] [PubMed]
- Neelakantan, N.; Koh, W.-P.; Yuan, J.-M.; van Dam, R.M. Diet-Quality Indexes Are Associated with a Lower Risk of Cardiovascular, Respiratory, and All-Cause Mortality among Chinese Adults. J. Nutr. 2018, 148, 1323–1332. [Google Scholar] [CrossRef] [PubMed]
- Micha, R.; Peñalvo, J.L.; Cudhea, F.; Imamura, F.; Rehm, C.D.; Mozaffarian, D. Association Between Dietary Factors and Mortality from Heart Disease, Stroke, and Type 2 Diabetes in the United States. JAMA 2017, 317, 912–924. [Google Scholar] [CrossRef]
- Harrison, S.; Couture, P.; Lamarche, B. Diet Quality, Saturated Fat and Metabolic Syndrome. Nutrients 2020, 12, 3232. [Google Scholar] [CrossRef]
- Martínez Valero, A.P.; Amo-Saus, E.; Pardo-García, I.; Escribano-Sotos, F. Calidad de la dieta en mayores de 65 años y factores socioeconómicos relacionados. Atención Primaria 2021, 53, 27–35. [Google Scholar] [CrossRef]
- Gil, Á. Indicadores de Evaluación de La Calidad de La Dieta. Nutr. Hosp. 2015, 128–144. [Google Scholar] [CrossRef]
- Asadi, Z.; Ghaffarian Zirak, R.; Yaghooti Khorasani, M.; Saedi, M.; Parizadeh, S.M.; Jafarzadeh-Esfehani, R.; Khorramruz, F.; Jandari, S.; Mohammadi-Bajgiran, M.; Zare-Feyzabadi, R.; et al. Dietary Inflammatory Index Is Associated with Healthy Eating Index, Alternative Healthy Eating Index, and Dietary Patterns among Iranian Adults. J. Clin. Lab. Anal. 2020, 34, e23523. [Google Scholar] [CrossRef]
- Murakami, K.; Livingstone, M.B.E.; Fujiwara, A.; Sasaki, S. Application of the Healthy Eating Index-2015 and the Nutrient-Rich Food Index 9.3 for Assessing Overall Diet Quality in the Japanese Context: Different Nutritional Concerns from the US. PLoS ONE 2020, 15, e0228318. [Google Scholar] [CrossRef]
- Sedaghat, F.; Heidari, Z.; Jalali, S.; Doustmohammadian, A.; Ehteshami, M.; Rashidkhani, B. Healthy Eating Index 2010 and Breast Cancer Risk. Nutr. Cancer 2018, 70, 860–866. [Google Scholar] [CrossRef] [PubMed]
- Al-Ibrahim, A.A.; Jackson, R.T. Healthy Eating Index versus Alternate Healthy Index in Relation to Diabetes Status and Health Markers in U.S. Adults: NHANES 2007–2010. Nutr. J. 2019, 18, 26. [Google Scholar] [CrossRef]
- Tay, M.E.; Foster, E.; Stevenson, L.; Brownlee, I. The Adherence of Singaporean Students in Different Educational Institutions to National Food-Based Dietary Guidelines. Nutrients 2020, 12, 2995. [Google Scholar] [CrossRef]
- Merhout, F.; Doyle, J. Socioeconomic Status and Diet Quality in College Students. J. Nutr. Educ. Behav. 2019, 51, 1107–1112. [Google Scholar] [CrossRef]
- El Ansari, W.; Stock, C. Is the Health and Wellbeing of University Students Associated with Their Academic Performance? Cross Sectional Findings from the United Kingdom. Int. J. Environ. Res. Public Health 2010, 7, 509–527. [Google Scholar] [CrossRef]
- Deliens, T.; Clarys, P.; De Bourdeaudhuij, I.; Deforche, B. Determinants of Eating Behaviour in University Students: A Qualitative Study Using Focus Group Discussions. BMC Public Health 2014, 14, 53. [Google Scholar] [CrossRef] [PubMed]
- Sogari, G.; Velez-Argumedo, C.; Gómez, M.I.; Mora, C. College Students and Eating Habits: A Study Using an Ecological Model for Healthy Behavior. Nutrients 2018, 10, 1823. [Google Scholar] [CrossRef] [PubMed]
- Suliga, E.; Cieśla, E.; Michel, S.; Kaducakova, H.; Martin, T.; Śliwiński, G.; Braun, A.; Izova, M.; Lehotska, M.; Kozieł, D.; et al. Diet Quality Compared to the Nutritional Knowledge of Polish, German, and Slovakian University Students—Preliminary Research. Int. J. Environ. Res. Public Health 2020, 17, 9062. [Google Scholar] [CrossRef]
- Kabir, A.; Miah, S.; Islam, A. Factors Influencing Eating Behavior and Dietary Intake among Resident Students in a Public University in Bangladesh: A Qualitative Study. PLoS ONE 2018, 13, e0198801. [Google Scholar] [CrossRef]
- Vélez-Toral, M.; Rodríguez-Reinado, C.; Ramallo-Espinosa, A.; Andrés-Villas, M. “It’s Important but, on What Level?”: Healthy Cooking Meanings and Barriers to Healthy Eating among University Students. Nutrients 2020, 12, 2309. [Google Scholar] [CrossRef] [PubMed]
- Bárbara, R.; Ferreira-Pêgo, C. Changes in Eating Habits among Displaced and Non-Displaced University Students. Int. J. Environ. Res. Public Health 2020, 17, 5369. [Google Scholar] [CrossRef]
- Ramón-Arbués, E.; Martínez Abadía, B.; Granada López, J.M.; Echániz Serrano, E.; Pellicer García, B.; Juárez Vela, R.; Guerrero Portillo, S.; Saéz Guinoa, M. Eating behavior and relationships with stress, anxiety, depression and insomnia in university students. Nutr. Hosp. 2019, 36, 1339–1345. [Google Scholar] [CrossRef] [PubMed]
- Whatnall, M.C.; Patterson, A.J.; Siew, Y.Y.; Kay-Lambkin, F.; Hutchesson, M.J. Are Psychological Distress and Resilience Associated with Dietary Intake Among Australian University Students? Int. J. Environ. Res. Public Health 2019, 16, 4099. [Google Scholar] [CrossRef] [PubMed]
- El Hajj, J.S.; Julien, S.G. Factors Associated with Adherence to the Mediterranean Diet and Dietary Habits among University Students in Lebanon. J. Nutr. Metab. 2021, 2021, 6688462. [Google Scholar] [CrossRef] [PubMed]
- Wattick, R.A.; Hagedorn, R.L.; Olfert, M.D. Relationship between Diet and Mental Health in a Young Adult Appalachian College Population. Nutrients 2018, 10, 957. [Google Scholar] [CrossRef] [PubMed]
- Norte Navarro, A.I.; Ortiz Moncada, R. Spanish diet quality according to the healthy eating index. Nutr. Hosp. 2011, 26, 330–336. [Google Scholar] [CrossRef] [PubMed]
- Hernández Galiot, A.; Goñi Cambrodón, I. Calidad de La Dieta de La Población Española Mayor de 80 Años No Institucionalizada. Nutr. Hosp. 2015, 31, 2571–2577. [Google Scholar] [CrossRef]
- Valdés, J.; Grau, M.; Subirana, I.; Marrugat, J.; Covas, M.-I.; Schröder, H. Secular Trends in Energy Intake and Diet Quality in a Mediterranean Population. Ann. Nutr. Metab. 2009, 54, 177–183. [Google Scholar] [CrossRef] [PubMed]
- Cebrino, J.; Portero de la Cruz, S. Diet Quality According to Mental Status and Associated Factors during Adulthood in Spain. Nutrients 2021, 13, 1727. [Google Scholar] [CrossRef]
- Varoucha-Azcarate, A.C. Analysis of the Diet in a Spanish Prison and the Level of Perception in a Sample of Prisoners. Rev. Esp. Sanid. Penit. 2019, 21, 18–27. [Google Scholar] [CrossRef]
- Bartrina, J.A.; Grupo Colaborativo de la Sociedad Española de Nutrición Comunitaria (SENC); Arija Val, A.; Maíz Aldalur, E.; de la Victoria Muñoz, E.; Ortega Anta, R.M.; Pérez-Rodrigo, C.; Quiles Izquierdo, J.; Rodríguez Martín, A.; Román Viñas, B.; et al. Dietary guidelines for the Spanish population (SENC, December 2016): The new graphic icon of healthy nutrition. Nutr. Hosp. 2016, 33, 1–48. [Google Scholar] [CrossRef]
- World Health Organization. Body Mass Index-BMI. Available online: https://www.euro.who.int/en/health-topics/disease-prevention/nutrition/a-healthy-lifestyle/body-mass-index-bmi (accessed on 11 June 2021).
- Lovibond, P.F.; Lovibond, S.H. The Structure of Negative Emotional States: Comparison of the Depression Anxiety Stress Scales (DASS) with the Beck Depression and Anxiety Inventories. Behav. Res. Ther. 1995, 33, 335–343. [Google Scholar] [CrossRef]
- Pedrero, E.F.; Piñeiro, M.; de las, M.P.; Giráldez, S.L.; Fernández, J.M. Propiedades psicométricas de la Depresión Anxiety and Stress Scales-21 (DASS-21) en universitarios españoles. Ansiedad Estrés 2010, 16, 215–226. [Google Scholar]
- Rodríguez Martos, A.; Navarro, R.; Vecino, C.; Pérez, R. Validación de Los Cuestionarios KFA (CBA) y CAGE Para El Diagnóstico Del Alcoholismo. Droga-Alcohol 1986, 11, 132–139. [Google Scholar]
- Sierra-Guerra, K.L.; Viveros-Contreras, C.; Martínez-Carrillo, G.; Hernández-León, O.; Caballero-Ambriz, G. Calidad de Vida En Pacientes Con Cáncer de Próstata, Operados de Prostatectomía Radical Laparoscópica. Rev. Mex. Urol. 2014, 74, 133–140. [Google Scholar] [CrossRef][Green Version]
- Dietch, J.R.; Taylor, D.J.; Sethi, K.; Kelly, K.; Bramoweth, A.D.; Roane, B.M. Psychometric Evaluation of the PSQI in U.S. College Students. J. Clin. Sleep Med. 2016, 12, 1121–1129. [Google Scholar] [CrossRef]
- Veqar, Z.; Hussain, M.E. Validity and Reliability of Insomnia Severity Index and Its Correlation with Pittsburgh Sleep Quality Index in Poor Sleepers among Indian University Students. Int. J. Adolesc. Med. Health 2017, 32, 20160090. [Google Scholar] [CrossRef]
- Rodríguez-Muñoz, S.; Corella, C.; Abarca-Sos, A.; Zaragoza, J. Validation of Three Short Physical Activity Questionnaires with Accelerometers among University Students in Spain. J. Sports Med. Phys. Fit. 2017, 57, 1660–1668. [Google Scholar] [CrossRef]
- IPAQ. Scoring, Protocol-International Physical Activity Questionnaire. Available online: https://sites.google.com/site/theipaq/scoring-protocol (accessed on 24 July 2021).
- Ramón-Arbués, E.; Gea-Caballero, V.; Granada-López, J.M.; Juárez-Vela, R.; Pellicer-García, B.; Antón-Solanas, I. The Prevalence of Depression, Anxiety and Stress and Their Associated Factors in College Students. Int. J. Environ. Res. Public Health 2020, 17, 7001. [Google Scholar] [CrossRef]
- Amaral Alves, D.; Hernández Regidor, N.; Basabe Baraño, N.; Rocandio Pablo, A.M.; Arroyo Izaga, M. Body satisfaction and diet quality in female university students from the Basque Country. Endocrinol. Nutr. 2012, 59, 239–245. [Google Scholar] [CrossRef]
- Telleria-Aramburu, N.; Bermúdez-Marín, N.; Rocandio, A.M.; Telletxea, S.; Basabe, N.; Rebato, E.; Arroyo-Izaga, M. Nutritional Quality and Carbon Footprint of University Students’ Diets: Results from the EHU12/24 Study. Public Health Nutr. 2021, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Vadeboncoeur, C.; Foster, C.; Townsend, N. Freshman 15 in England: A Longitudinal Evaluation of First Year University Student’s Weight Change. BMC Obes. 2016, 3, 45. [Google Scholar] [CrossRef]
- Haidar, S.A.; de Vries, N.K.; Papandreou, D.; Rizk, R.; Karavetian, M. The Freshman Weight Gain Phenomenon: Does It Apply To. Open Access Maced. J. Med. Sci. 2018, 6, 2214–2220. [Google Scholar] [CrossRef]
- Mihalopoulos, N.L.; Auinger, P.; Klein, J.D. The Freshman 15: Is It Real? J. Am. Coll. Health 2008, 56, 531–533. [Google Scholar] [CrossRef] [PubMed]
- Bach-Faig, A.; Fuentes-Bol, C.; Ramos, D.; Carrasco, J.L.; Roman, B.; Bertomeu, I.F.; Cristià, E.; Geleva, D.; Serra-Majem, L. The Mediterranean Diet in Spain: Adherence Trends during the Past Two Decades Using the Mediterranean Adequacy Index. Public Health Nutr. 2011, 14, 622–628. [Google Scholar] [CrossRef] [PubMed]
- García Cabrera, S.; Herrera Fernández, N.; Rodríguez Hernández, C.; Nissensohn, M.; Román-Viñas, B.; Serra-Majem, L. KIDMED Test; Prevalence of Low Adherence to the Mediterranean Diet in Children and Young: A Systematic Review. Nutr. Hosp. 2015, 32, 2390–2399. [Google Scholar] [CrossRef]
- Riccardi, G.; Vitale, M.; Vaccaro, O. Are Europeans Moving towards Dietary Habits More Suitable for Reducing Cardiovascular Disease Risk? Nutr. Metab. Cardiovasc. Dis. 2020, 30, 1857–1860. [Google Scholar] [CrossRef] [PubMed]
- Calderon, R.; Pupanead, S.; Prachakul, W.; Kim, G. Happiness, Perceived Stress, Psychological Well-Being, and Health Behaviors of Thai University Students: Preliminary Results from a Multinational Study on Well-Being. J. Am. Coll. Health 2021, 69, 176–184. [Google Scholar] [CrossRef] [PubMed]
- Quehl, R.; Haines, J.; Lewis, S.P.; Buchholz, A.C. Food and Mood: Diet Quality Is Inversely Associated with Depressive Symptoms in Female University Students. Can. J. Diet. Pract. Res. 2017, 78, 124–128. [Google Scholar] [CrossRef]
- Delicado-Soria, A.; Serrano-Urrea, R.; Cervera-Burriel, F.; Daouas, T.; García-Meseguer, M.-J. Food Consumption in Tunisian University Students and Its Association with Sociodemographic Characteristics and Lifestyle Behaviours. Public Health Nutr. 2020, 24, 4949–4964. [Google Scholar] [CrossRef]
- Cervera Burriel, F.; Serrano Urrea, R.; Daouas, T.; Delicado Soria, A.; García Meseguer, M.J. Food habits and nutritional assessment in a tunisian university population. Nutr. Hosp. 2014, 30, 1350–1358. [Google Scholar] [CrossRef] [PubMed]
- García-Meseguer, M.J.; Burriel, F.C.; García, C.V.; Serrano-Urrea, R. Adherence to Mediterranean Diet in a Spanish University Population. Appetite 2014, 78, 156–164. [Google Scholar] [CrossRef]
- Ejeda-Manzanera, J.M.; Rodrigo-Vega, M. Hábitos de alimentación y calidad de dieta en estudiantes universitarias de magisterio en relación a su adherencia a la dieta mediterránea. Rev. Española Salud Pública 2021, 95, e1–e14. [Google Scholar]
- Salas, R.; del Mar Bibiloni, M.; Zapata, M.E.; Coll, J.L.; Pons, A.; Tur, J.A. Balearic Adults Have Low Intakes of Fruits and Vegetables Compared with the Dietary Guidelines for Adults in Spain. Nutr. Res. 2013, 33, 204–210. [Google Scholar] [CrossRef]
- Beaudry, K.M.; Ludwa, I.A.; Thomas, A.M.; Ward, W.E.; Falk, B.; Josse, A.R. First-Year University Is Associated with Greater Body Weight, Body Composition and Adverse Dietary Changes in Males than Females. PLoS ONE 2019, 14, e0218554. [Google Scholar] [CrossRef] [PubMed]
- Leblanc, V.; Bégin, C.; Corneau, L.; Dodin, S.; Lemieux, S. Gender Differences in Dietary Intakes: What Is the Contribution of Motivational Variables? J. Hum. Nutr. Diet. 2015, 28, 37–46. [Google Scholar] [CrossRef] [PubMed]
- Menozzi, D.; Sogari, G.; Mora, C. Explaining Vegetable Consumption among Young Adults: An Application of the Theory of Planned Behaviour. Nutrients 2015, 7, 7633–7650. [Google Scholar] [CrossRef] [PubMed]
- Grzymisławska, M.; Puch, E.A.; Zawada, A.; Grzymisławski, M. Do Nutritional Behaviors Depend on Biological Sex and Cultural Gender? Adv. Clin. Exp. Med. 2020, 29, 165–172. [Google Scholar] [CrossRef]
- Aljadani, H.M.; Patterson, A.J.; Sibbritt, D.; Collins, C.E. Diet Quality and Six-Year Risk of Overweight and Obesity among Mid-Age Australian Women Who Were Initially in the Healthy Weight Range. Health Promot. J. Austr. 2016, 27, 29–35. [Google Scholar] [CrossRef] [PubMed]
- Aljadani, H.M.A.; Sibbritt, D.; Patterson, A.; Collins, C. The Australian Recommended Food Score Did Not Predict Weight Gain in Middle-Aged Australian Women during Six Years of Follow-Up. Aust. N. Z. J. Public Health 2013, 37, 322–328. [Google Scholar] [CrossRef]
- El Ansari, W.; Stock, C.; Mikolajczyk, R.T. Relationships between Food Consumption and Living Arrangements among University Students in Four European Countries—A Cross-Sectional Study. Nutr. J. 2012, 11, 28. [Google Scholar] [CrossRef] [PubMed]
- Lupi, S.; Bagordo, F.; Stefanati, A.; Grassi, T.; Piccinni, L.; Bergamini, M.; Donno, A.D. Assessment of Lifestyle and Eating Habits among Undergraduate Students in Northern Italy. Ann. Ist. Super. Sanità 2015, 51, 154–161. [Google Scholar] [CrossRef]
- Côté, M.; Bégin, C. Review of the Experience of Weight-Based Stigmatization in Romantic Relationships. Curr. Obes. Rep. 2020, 9, 280–287. [Google Scholar] [CrossRef]
- van Woerden, I.; Brewis, A.; Hruschka, D.; Dunton, G.; Adams, M.A.; Bruening, M. Young Adults’ BMI and Changes in Romantic Relationship Status during the First Semester of College. PLoS ONE 2020, 15, e0230806. [Google Scholar] [CrossRef]
- Moreno-Gómez, C.; Romaguera-Bosch, D.; Tauler-Riera, P.; Bennasar-Veny, M.; Pericas-Beltran, J.; Martinez-Andreu, S.; Aguilo-Pons, A. Clustering of Lifestyle Factors in Spanish University Students: The Relationship between Smoking, Alcohol Consumption, Physical Activity and Diet Quality. Public Health Nutr. 2012, 15, 2131–2139. [Google Scholar] [CrossRef]
- Romaguera, D.; Tauler, P.; Bennasar, M.; Pericas, J.; Moreno, C.; Martinez, S.; Aguilo, A. Determinants and Patterns of Physical Activity Practice among Spanish University Students. J. Sports Sci. 2011, 29, 989–997. [Google Scholar] [CrossRef] [PubMed]
- Sánchez-Ojeda, M.A.; De Luna-Bertos, E. Healthy lifestyles of the university population. Nutr. Hosp. 2015, 31, 1910–1919. [Google Scholar] [CrossRef] [PubMed]
- Bennasar-Veny, M.; Yañez, A.M.; Pericas, J.; Ballester, L.; Fernandez-Dominguez, J.C.; Tauler, P.; Aguilo, A. Cluster Analysis of Health-Related Lifestyles in University Students. Int. J. Environ. Res. Public Health 2020, 17, 1776. [Google Scholar] [CrossRef]
- Adan, R.A.H.; van der Beek, E.M.; Buitelaar, J.K.; Cryan, J.F.; Hebebrand, J.; Higgs, S.; Schellekens, H.; Dickson, S.L. Nutritional Psychiatry: Towards Improving Mental Health by What You Eat. Eur. Neuropsychopharmacol. 2019, 29, 1321–1332. [Google Scholar] [CrossRef]
- Moreno-Agostino, D.; Caballero, F.F.; Martín-María, N.; Tyrovolas, S.; López-García, P.; Rodríguez-Artalejo, F.; Haro, J.M.; Ayuso-Mateos, J.L.; Miret, M. Mediterranean Diet and Wellbeing: Evidence from a Nationwide Survey. Psychol. Health 2019, 34, 321–335. [Google Scholar] [CrossRef]
- Emerson, S.D.; Carbert, N.S. An Apple a Day: Protective Associations between Nutrition and the Mental Health of Immigrants in Canada. Soc. Psychiatry Psychiatr. Epidemiol. 2019, 54, 567–578. [Google Scholar] [CrossRef]
- Fresán, U.; Bes-Rastrollo, M.; Segovia-Siapco, G.; Sanchez-Villegas, A.; Lahortiga, F.; de la Rosa, P.-A.; Martínez-Gonzalez, M.-A. Does the MIND Diet Decrease Depression Risk? A Comparison with Mediterranean Diet in the SUN Cohort. Eur. J. Nutr. 2019, 58, 1271–1282. [Google Scholar] [CrossRef]
- Smith, A.D.; Warren, M.J.; Refsum, H. Chapter Six-Vitamin B12. In Advances in Food and Nutrition Research; New Research and Developments of Water-Soluble Vitamins; Eskin, N.A.M., Ed.; Academic Press: Cambridge, MA, USA, 2018; Volume 83, pp. 215–279. [Google Scholar]
- Spaeth, A.M.; Dinges, D.F.; Goel, N. Sex and Race Differences in Caloric Intake during Sleep Restriction in Healthy Adults. Am. J. Clin. Nutr 2014, 100, 559–566. [Google Scholar] [CrossRef]
- Fang, Z.; Spaeth, A.M.; Ma, N.; Zhu, S.; Hu, S.; Goel, N.; Detre, J.A.; Dinges, D.F.; Rao, H. Altered Salience Network Connectivity Predicts Macronutrient Intake after Sleep Deprivation. Sci. Rep. 2015, 5, 8215. [Google Scholar] [CrossRef] [PubMed]
- Heath, G.; Roach, G.D.; Dorrian, J.; Ferguson, S.A.; Darwent, D.; Sargent, C. The Effect of Sleep Restriction on Snacking Behaviour during a Week of Simulated Shiftwork. Accid. Anal. Prev. 2012, 45, 62–67. [Google Scholar] [CrossRef]
- Mozaffarian, N.; Heshmat, R.; Ataie-Jafari, A.; Motlagh, M.E.; Ziaodini, H.; Shafiee, G.; Taheri, M.; Mansourian, M.; Qorbani, M.; Kelishadi, R. Association of Sleep Duration and Snack Consumption in Children and Adolescents: The CASPIAN-V Study. Food Sci. Nutr. 2020, 8, 1888–1897. [Google Scholar] [CrossRef] [PubMed]
- Martinez, S.M.; Tschann, J.M.; Butte, N.F.; Gregorich, S.E.; Penilla, C.; Flores, E.; Greenspan, L.C.; Pasch, L.A.; Deardorff, J. Short Sleep Duration Is Associated with Eating More Carbohydrates and Less Dietary Fat in Mexican American Children. Sleep 2017, 40, zsw057. [Google Scholar] [CrossRef] [PubMed]
- Nedeltcheva, A.V.; Kilkus, J.M.; Imperial, J.; Kasza, K.; Schoeller, D.A.; Penev, P.D. Sleep Curtailment Is Accompanied by Increased Intake of Calories from Snacks. Am. J. Clin. Nutr. 2009, 89, 126–133. [Google Scholar] [CrossRef]
- Stern, J.H.; Grant, A.S.; Thomson, C.A.; Tinker, L.; Hale, L.; Brennan, K.M.; Woods, N.F.; Chen, Z. Short Sleep Duration Is Associated with Decreased Serum Leptin, Increased Energy Intake and Decreased Diet Quality in Postmenopausal Women. Obesity 2014, 22, E55–E61. [Google Scholar] [CrossRef]
- Haghighatdoost, F.; Karimi, G.; Esmaillzadeh, A.; Azadbakht, L. Sleep Deprivation Is Associated with Lower Diet Quality Indices and Higher Rate of General and Central Obesity among Young Female Students in Iran. Nutrition 2012, 28, 1146–1150. [Google Scholar] [CrossRef]
- Dashti, H.S.; Scheer, F.A.; Jacques, P.F.; Lamon-Fava, S.; Ordovás, J.M. Short Sleep Duration and Dietary Intake: Epidemiologic Evidence, Mechanisms, and Health Implications. Adv. Nutr. 2015, 6, 648–659. [Google Scholar] [CrossRef]
- Binks, H.E.; Vincent, G.; Gupta, C.; Irwin, C.; Khalesi, S. Effects of Diet on Sleep: A Narrative Review. Nutrients 2020, 12, 936. [Google Scholar] [CrossRef]
- King, B.M.; Cespedes, V.M.; Burden, G.K.; Brady, S.K.; Clement, L.R.; Abbott, E.M.; Baughman, K.S.; Joyner, S.E.; Clark, M.M.; Pury, C.L.S. Extreme Under-Reporting of Body Weight by Young Adults with Obesity: Relation to Social Desirability. Obes. Sci. Pract. 2018, 4, 129–133. [Google Scholar] [CrossRef]
- Burke, M.A.; Carman, K.G. You Can Be Too Thin (but Not Too Tall): Social Desirability Bias in Self-Reports of Weight and Height. Econ. Hum. Biol. 2017, 27, 198–222. [Google Scholar] [CrossRef]
- Mattioli, A.V.; Sciomer, S.; Cocchi, C.; Maffei, S.; Gallina, S. Quarantine during COVID-19 Outbreak: Changes in Diet and Physical Activity Increase the Risk of Cardiovascular Disease. Nutr. Metab. Cardiovasc. Dis. 2020, 30, 1409–1417. [Google Scholar] [CrossRef]
- Izzo, L.; Santonastaso, A.; Cotticelli, G.; Federico, A.; Pacifico, S.; Castaldo, L.; Colao, A.; Ritieni, A. An Italian Survey on Dietary Habits and Changes during the COVID-19 Lockdown. Nutrients 2021, 13, 1197. [Google Scholar] [CrossRef] [PubMed]
- Ferrante, G.; Camussi, E.; Piccinelli, C.; Senore, C.; Armaroli, P.; Ortale, A.; Garena, F.; Giordano, L. Did Social Isolation during the SARS-CoV-2 Epidemic Have an Impact on the Lifestyles of Citizens? Epidemiol. Prev. 2020, 44, 353–362. [Google Scholar] [CrossRef]
- Sidor, A.; Rzymski, P. Dietary Choices and Habits during COVID-19 Lockdown: Experience from Poland. Nutrients 2020, 12, 1657. [Google Scholar] [CrossRef] [PubMed]
- Alegria-Lertxundi, I.; Rocandio, A.M.; Telletxea, S.; Rincón, E.; Arroyo-Izaga, M. Relación Entre El Índice de Consumo de Pescado y Carne y La Adecuación y Calidad de La Dieta En Mujeres Jóvenes Universitarias. Nutr. Hosp. 2014, 30, 1135–1143. [Google Scholar] [CrossRef] [PubMed]
- Rodríguez-Rodríguez, E.; López-Sobaler, A.M.; Ortega, R.M.; Delgado-Losada, M.L.; López-Parra, A.M.; Aparicio, A. Association between Neutrophil-to-Lymphocyte Ratio with Abdominal Obesity and Healthy Eating Index in a Representative Older Spanish Population. Nutrients 2020, 12, 855. [Google Scholar] [CrossRef] [PubMed]
- Weinstein, S.J.; Vogt, T.M.; Gerrior, S.A. Healthy Eating Index Scores Are Associated with Blood Nutrient Concentrations in the Third National Health and Nutrition Examination Survey. J. Am. Diet. Assoc. 2004, 104, 576–584. [Google Scholar] [CrossRef] [PubMed]
- Fallaize, R.; Livingstone, K.M.; Celis-Morales, C.; Macready, A.L.; San-Cristobal, R.; Navas-Carretero, S.; Marsaux, C.F.M.; O’Donovan, C.B.; Kolossa, S.; Moschonis, G.; et al. Association between Diet-Quality Scores, Adiposity, Total Cholesterol and Markers of Nutritional Status in European Adults: Findings from the Food4Me Study. Nutrients 2018, 10, 49. [Google Scholar] [CrossRef] [PubMed]

| Variable | Mean ± SD/n (%) | |
|---|---|---|
| Age | 21.74 ± 5.15 | |
| Gender | Female | 744 (70.5%) |
| Male | 311 (29.5%) | |
| BMI (kg/m2) | 22.15 ± 3.48 | |
| BMI Categories | Underweight (<18.5 kg/m2) | 160 (15.2%) |
| Normal weight (18.5–24.9 kg/m2) | 736 (69.8%) | |
| Overweight/obese (≥25 kg/m2) | 159 (15.1%) | |
| Living arrangement | Living alone | 64 (6.1%) |
| Living with a partner | 291 (27.6%) | |
| Living with family | 700 (66.4%) | |
| Relationship status | Currently in a relationship | 494 (46.8%) |
| Currently not in a relationship | 561 (53.2%) | |
| Smoking status (current) | No | 535 (76.6%) |
| Yes | 163 (23.4%) | |
| CAGE score | 0.48 ± 0.78 | |
| CAGE categories | Problematic alcohol consumption | 343 (32.5%) |
| Non-problematic alcohol consumption | 712 (67.5%) | |
| SHEI score | 68.57 ± 12.17 | |
| Diet quality | Inadequate (<51 points) | 73 (6.9%) |
| Need changes (51–80 points) | 798 (75.6%) | |
| Healthy (>80 points) | 184 (17.4%) | |
| Physical activity (METs/week) | 1877.03 ± 1966.54 | |
| Physical activity categories | High | 236 (22.4%) |
| Medium | 351 (33.3%) | |
| Low | 468 (44.4%) | |
| Sedentary time (hours/day) | 6.76 ± 2.45 | |
| Sedentary time categories | <3 h/day | 133 (12.6%) |
| 3–6 h/day | 342 (32.4%) | |
| ≥6 h/day | 580 (54.9%) | |
| DASS-E score | 12.39 ± 8.08 | |
| DASS-E categories | No stress | 697 (66.1%) |
| Mild stress | 121 (11.5%) | |
| Moderate stress | 174 (16.5%) | |
| Severe stress | 46 (4.4%) | |
| Extremely severe stress | 17 (1.6%) | |
| DASS-D score | 5.45 ± 7.12 | |
| DASS-D categories | No depression | 859 (81.4%) |
| Mild depression | 80 (7.6%) | |
| Moderate depression | 48 (4.5%) | |
| Severe depression | 38 (3.6%) | |
| Extremely severe depression | 30 (2.8%) | |
| DASS-A score | 4.84 ± 5.75 | |
| DASS-A categories | No anxiety | 807 (76.5%) |
| Mild anxiety | 83 (7.9%) | |
| Moderate anxiety | 95 (9.0%) | |
| Severe anxiety | 9 (0.9%) | |
| Extremely severe anxiety | 61 (5.8%) | |
| ISI score | 7.91 ± 4.88 | |
| Sleep quality | No insomnia | 600 (56.9%) |
| Sub-threshold insomnia | 333 (31.6%) | |
| Moderate insomnia | 114 (10.8%) | |
| Severe insomnia | 8 (0.8%) |
| Food Group | Mean ± SD | Min. | Max. | Mode |
|---|---|---|---|---|
| Bread and grains | 7.27 ± 3.25 | 0 | 10 | 10 (Consumed daily) |
| Vegetables | 8.38 ± 2.91 | 0 | 10 | 10 (Consumed daily) |
| Fruits | 8.23 ± 3.54 | 0 | 10 | 10 (Consumed daily) |
| Dairy products | 9.27 ± 2.82 | 0 | 10 | 10 (Consumed daily) |
| Meat | 6.90 ± 2.83 | 0 | 10 | 7.5 (3 or more times a week but not daily) |
| Legumes | 9.17 ± 1.97 | 0 | 10 | 7.5 (3 or more times a week but not daily) |
| Cold meats and cuts | 6.29 ± 3.75 | 0 | 10 | 5 (Once or twice a week) |
| Sweets | 4.45 ± 3.28 | 0 | 10 | 5 (Once or twice a week) |
| Soft drinks with sugar | 8.62 ± 3.36 | 0 | 10 | 7.5 (Less than once a week) |
| SHEI score | 68.57 ± 12.17 | 25 | 96.5 | 70.5 (Need changes) |
| Independent Variable | B (CI 95%) | Std. Error | β | p |
|---|---|---|---|---|
| Age. <20 years (Ref.) | ||||
| 20–24.9 | 3.54 (2.05, 5.04) | 0.76 | 0.14 | 0.00 |
| ≥25 | 4.76 (2.68, 6.85) | 1.06 | 0.14 | 0.00 |
| Gender. Male (Ref.) | ||||
| Female | 2.47 (0.94, 4.00) | 0.781 | 0.09 | 0.00 |
| BMI categories. Normal weight (Ref.) | ||||
| Underweight (<18.5 kg/m2) | 3.55 (1.63, 5.48) | 0.98 | 0.10 | 0.00 |
| Overweight/obese (≥25 kg/m2) | 6.42 (4.53, 8.31) | 0.96 | 0.19 | 0.00 |
| Living arrangement. Living with family (Ref.) | ||||
| Living alone | −11.49 (−14.27, −8.71) | 1.42 | −0.22 | 0.00 |
| Living with a partner | −0.50 (−2.06, 1.07) | 0.80 | −0.02 | 0.53 |
| Relationship status. Currently in a relationship (Ref.) | ||||
| Currently not in a relationship | 3.63 (2.01, 5.25) | 0.83 | 0.15 | 0.00 |
| Smoking status. Not a smoker (Ref.) | ||||
| Smoker | −2.82 (−4.41, −1.24) | 0.81 | −0.10 | 0.00 |
| CAGE Categories. Non-problematic alcohol consumption (Ref.) | ||||
| Problematic alcohol consumption | −1.82 (−3.20, −0.45) | 0.702 | −0.070 | 0.01 |
| Physical activity. Medium (Ref.) | ||||
| High PA | 1.74 (−0.05, 3.53) | 0.91 | 0.06 | 0.06 |
| Low PA | −2.77 (−4.45, −1.09) | 0.86 | −0.11 | 0.00 |
| Sedentary time. 3–6 h per day | ||||
| <3 h/day | −0.29 (−2.48, 1.90) | 1.11 | −0.01 | 0.80 |
| ≥6 h/day | −2.40 (−3.86, −0.93) | 0.75 | −0.10 | 0.00 |
| DASS-E categories. No stress (Ref.) | ||||
| Mild stress | 12.10 (9.63, 14.57) | 1.26 | 0.32 | 0.00 |
| Moderate stress | −1.08 (−3.08, 0.92) | 1.02 | −0.03 | 0.29 |
| Severe stress | −0.29 (−3.93, 3.35) | 1.85 | −0.00 | 0.88 |
| Extremely severe stress | −5.56 (−11.37, 0.24) | 2.96 | −0.06 | 0.06 |
| DASS-D categories. No depression (Ref.) | ||||
| Mild depression | 2.13 (−1.00, 5.27) | 1.60 | 0.05 | 0.18 |
| Moderate depression | −3.23 (−6.71, 0.25) | 1.77 | −0.05 | 0.07 |
| Severe depression | −18.04 (−22.12, −3.97) | 2.07 | −0.28 | 0.00 |
| Extremely severe depression | −7.77 (−12.22, −3.33) | 2.26 | −0.11 | 0.00 |
| DASS-A categories. No anxiety (Ref.) | ||||
| Mild anxiety | −3.25 (−5.91, −0.60) | 1.35 | −0.07 | 0.01 |
| Moderate anxiety | −3.32 (−5.93, −0.70) | 1.33 | −0.08 | 0.01 |
| Severe anxiety | −10.96 (−18.25, −3.66) | 3.72 | −0.08 | 0.00 |
| Extremely severe anxiety | −1.29 (−5.18, 2.61) | 1.98 | −0.02 | 0.52 |
| ISI categories. No insomnia (Ref.) | ||||
| Sub-threshold insomnia | −4.93 (−6.50, −3.37) | 0.79 | −0.19 | 0.00 |
| Moderate insomnia | −6.62 (−9.11, −4.14) | 1.27 | −0.17 | 0.00 |
| Severe insomnia | −13.51 (−21.46, −5.56) | 4.05 | −0.10 | 0.00 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ramón-Arbués, E.; Granada-López, J.-M.; Martínez-Abadía, B.; Echániz-Serrano, E.; Antón-Solanas, I.; Jerue, B.A. Factors Related to Diet Quality: A Cross-Sectional Study of 1055 University Students. Nutrients 2021, 13, 3512. https://doi.org/10.3390/nu13103512
Ramón-Arbués E, Granada-López J-M, Martínez-Abadía B, Echániz-Serrano E, Antón-Solanas I, Jerue BA. Factors Related to Diet Quality: A Cross-Sectional Study of 1055 University Students. Nutrients. 2021; 13(10):3512. https://doi.org/10.3390/nu13103512
Chicago/Turabian StyleRamón-Arbués, Enrique, José-Manuel Granada-López, Blanca Martínez-Abadía, Emmanuel Echániz-Serrano, Isabel Antón-Solanas, and Benjamin Adam Jerue. 2021. "Factors Related to Diet Quality: A Cross-Sectional Study of 1055 University Students" Nutrients 13, no. 10: 3512. https://doi.org/10.3390/nu13103512
APA StyleRamón-Arbués, E., Granada-López, J.-M., Martínez-Abadía, B., Echániz-Serrano, E., Antón-Solanas, I., & Jerue, B. A. (2021). Factors Related to Diet Quality: A Cross-Sectional Study of 1055 University Students. Nutrients, 13(10), 3512. https://doi.org/10.3390/nu13103512







