Breakfast Skipping, Weight, Cardiometabolic Risk, and Nutrition Quality in Children and Adolescents: A Systematic Review of Randomized Controlled and Intervention Longitudinal Trials
Abstract
:1. Introduction
2. Materials and Methods
2.1. Literature Search
2.2. Outcome Measures
2.3. Inclusion and Exclusion Criteria
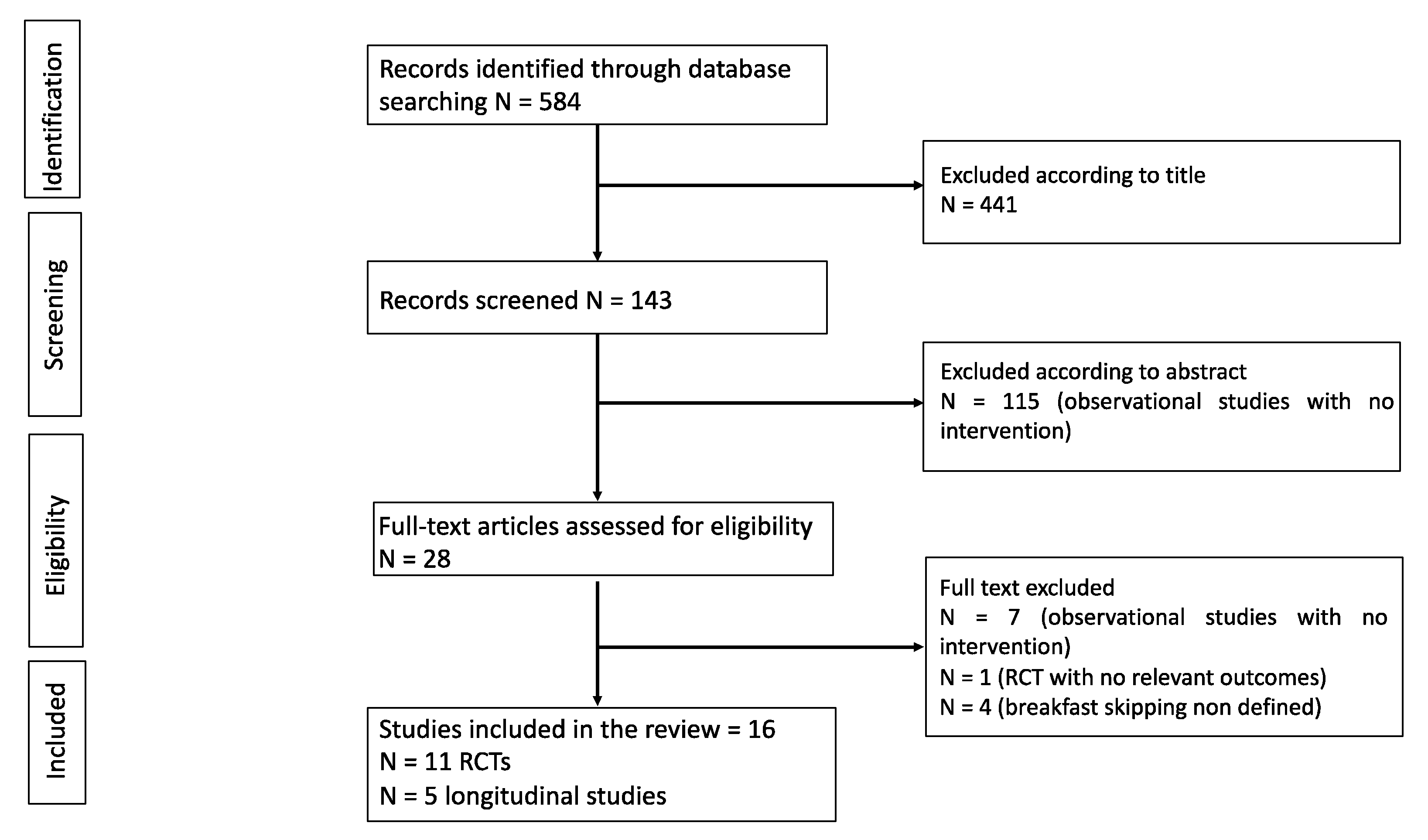
2.4. Identification of Relevant Studies
2.5. Data Extraction and Synthesis
2.6. Quality Assessment
3. Results
3.1. Study Characteristics
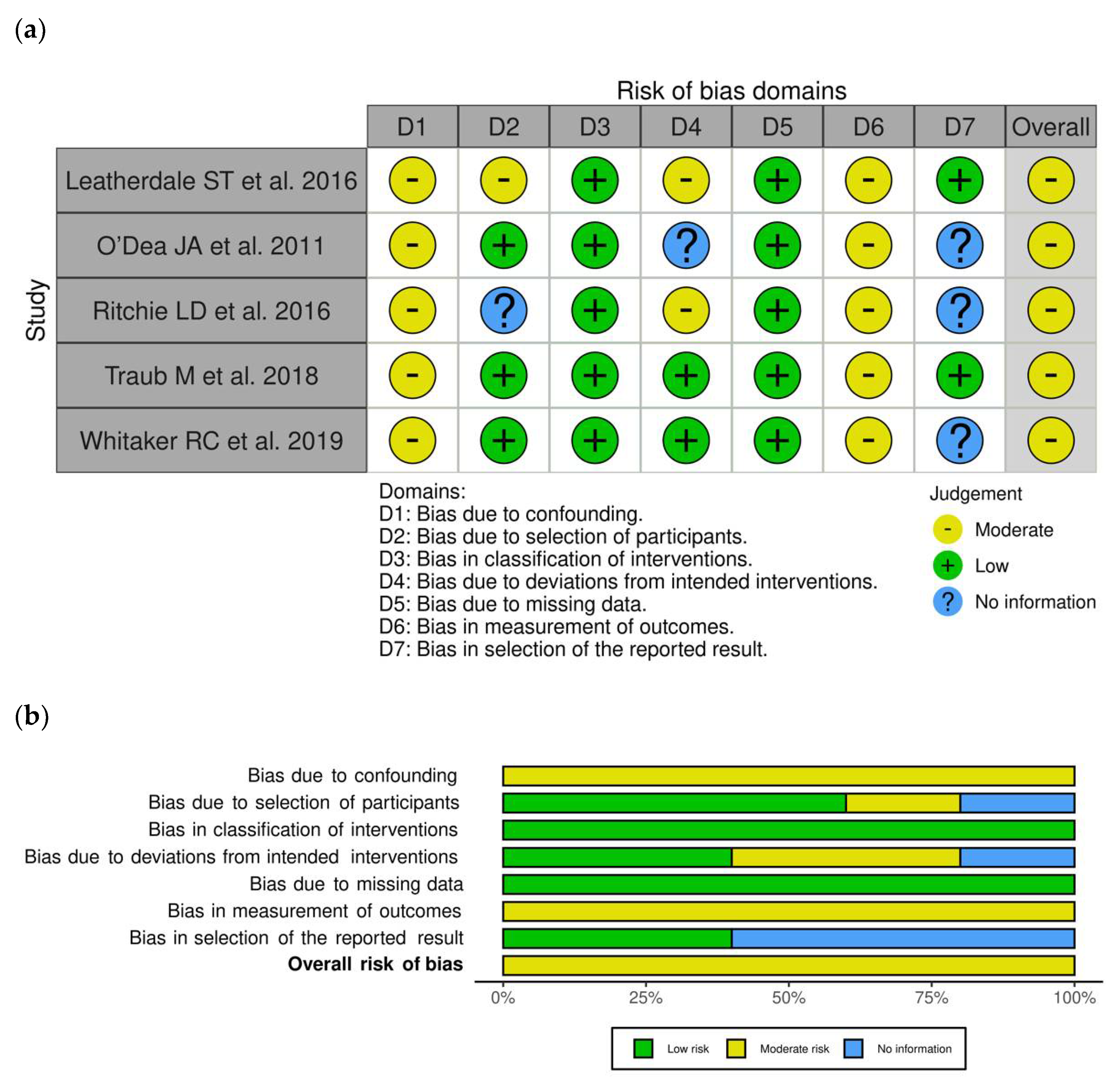
3.2. Risk of Bias within Longitudinal Studies
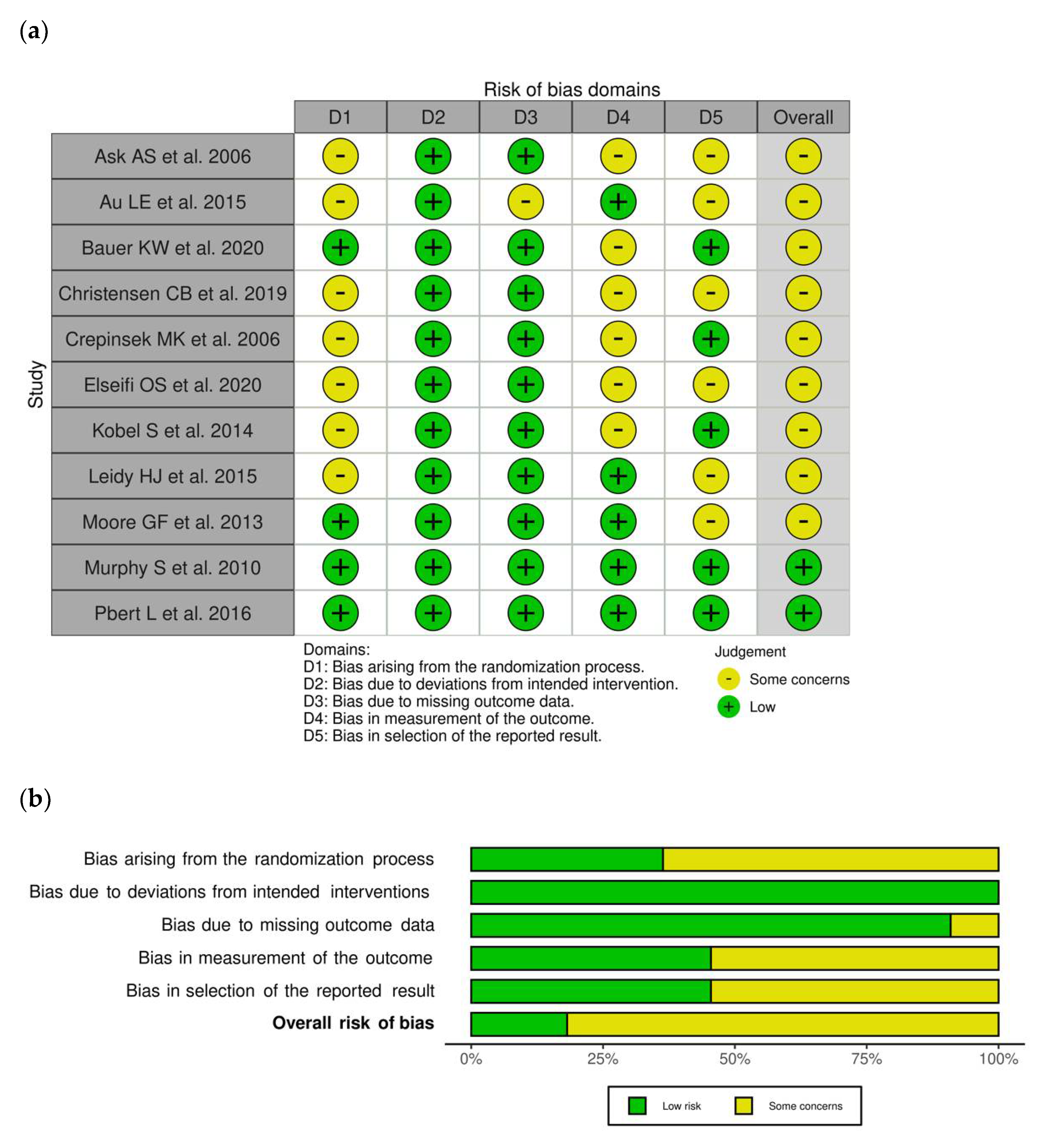
3.3. Risk of Bias within RCTs
3.4. Findings
4. Discussion
Author Contributions
Funding
Conflicts of Interest
References
- NCD Risk Factor Collaboration (NCD-RisC). Worldwide trends in body-mass index, underweight, overweight, and obesity from 1975 to 2016: A pooled analysis of 2416 population-based measurement studies in 128·9 million children, adolescents, and adults. Lancet 2017, 390, 2627–2642. [Google Scholar] [CrossRef] [Green Version]
- Moraeus, L.; Lissner, L.; Yngve, A.; Poortvliet, E.; Al-Ansari, U.; Sjöberg, A. Multi-level influences on childhood obesity in Sweden: Societal factors, parental determinants and child’s lifestyle. Int. J. Obes. 2012, 36, 969–976. [Google Scholar] [CrossRef] [Green Version]
- Wijnhoven, T.M.A.; van Raaij, J.M.A.; Yngve, A.; Sjöberg, A.; Kunešov, M.; Duleva, V.; Petrauskiene, A.; Rito, A.I.; Breda, J. WHO European Childhood Obesity Surveillance Initiative: Health-risk behaviours on nutrition and physical activity in 6–9-year-old schoolchildren. Public. Health Nutr. 2015, 18, 3108–3124. [Google Scholar] [CrossRef] [Green Version]
- Rampersaud, G.C.; Pereira, M.A.; Girard, B.L.; Adams, J.; Metzl, J.D. Breakfast habits, nutritional status, body weight, and academic performance in children and adolescents. J. Am. Diet. Assoc. 2005, 105, 743–760. [Google Scholar] [CrossRef] [PubMed]
- Al Abdi, T.; Andreou, E.; Papageorgiou, A.; Heraclides, A.; Philippou, E. Personality, chrono-nutrition and cardiometabolic health: A narrative review of the evidence. Adv. Nutr. 2020, 11, 1201–1210. [Google Scholar] [CrossRef] [PubMed]
- Laermans, J.; Depoortere, I. Chronobesity: Role of the circadian system in the obesity epidemic. Obes. Rev. 2016, 17, 108–125. [Google Scholar] [CrossRef]
- Allison, K.C.; Goel, N. Timing of eating in adults across the weight spectrum: Metabolic factors and potential circadian mechanisms. Physiol. Behav. 2018, 192, 158–166. [Google Scholar] [CrossRef] [PubMed]
- Paoli, A.; Tinsley, G.; Bianco, A.; Moro, T. The influence of meal frequency and timing on health in humans: The role of fasting. Nutrients 2019, 11, 719. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- St-Onge, M.P.; Ard, J.; Baskin, M.L.; Chiuve, S.E.; Johnson, H.M.; Kris-Etherton, P.; Varady, K. Meal timing and frequency: Implications for cardiovascular disease prevention: A scientific statement from the American Heart Association. Circulation 2017, 135, 96–121. [Google Scholar] [CrossRef] [PubMed]
- Monzani, A.; Ricotti, R.; Caputo, M.; Solito, A.; Archero, F.; Bellone, S.; Prodam, F. A systematic review of the association of skipping breakfast with weight and cardiometabolic risk factors in children and adolescents. What should we better investigate in the future? Nutrients 2019, 11, 387. [Google Scholar] [CrossRef] [Green Version]
- Sievert, K.; Hussain, S.M.; Page, M.J.; Wang, Y.; Hughes, H.J.; Malek, M.; Cicuttini, F.M. Effect of breakfast on weight and energy intake: Systematic review and meta-analysis of randomised controlled trials. BMJ 2019, 364, l42. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Blumberg, J.; Heaney, R.P.; Huncharek, M.; Scholl, T.; Stampfer, M.; Vieth, R.; Weaver, C.M.; Zeisel, S.H. Evidence-based criteria in the nutritional context. Nutr. Rev. 2010, 68, 478–484. [Google Scholar] [CrossRef] [PubMed]
- Shamseer, L.; Moher, D.; Clarke, M.; Ghersi, D.; Liberati, A.; Petticrew, M.; Shekelle, P.; Stewart, L.A. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015: Elaboration and explanation. BMJ 2015, 349, 7647. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Moher, D.; Shamseer, L.; Clarke, M.; Ghersi, D.; Liberati, A.; Petticrew, M.; Shekelle, P.; Stewart, L.A.; Estarli, M.; Barrera, E.S.A.; et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Rev. Esp. Nutr. Hum. Diet. 2016, 20, 148–160. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sterne, J.A.; Hernán, M.A.; Reeves, B.C.; Savović, J.; Berkman, N.D.; Viswanathan, M.; Henry, D.; Altman, D.G.; Ansari, M.T.; Boutron, I.; et al. ROBINS-I: A tool for assessing risk of bias in non-randomised studies of interventions. BMJ 2016, 355, 4919. [Google Scholar] [CrossRef] [Green Version]
- Sterne, J.A.C.; Savović, J.; Page, M.J.; Elbers, R.G.; Blencowe, N.S.; Boutron, I.; Cates, C.J.; Cheng, H.-Y.; Corbett, M.S.; Eldridge, S.M.; et al. RoB 2: A revised tool for assessing risk of bias in randomised trials. BMJ 2019, 366, l4898. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- McGuinness, L.A.; Higgins, J.P.T. Risk-of-bias VISualization (robvis): An R package and Shiny web app for visualizing risk-of-bias assessments. Res. Syn. Meth. 2021, 12, 55–61. [Google Scholar] [CrossRef]
- Leatherdale, S.T.; Stefanczyk, J.M.; Kirkpatrick, S.I. School Breakfast-Club Program changes and youth eating breakfast during the school week in the COMPASS Study. J. Sch. Health 2016, 86, 568–577. [Google Scholar] [CrossRef]
- O’Dea, J.A.; Wagstaff, S. Increased breakfast frequency and nutritional quality among schoolchildren after a national breakfast promotion campaign in Australia between 2000 and 2006. Health Educ. Res. 2011, 26, 1086–1096. [Google Scholar] [CrossRef]
- Ritchie, L.D.; Rosen, N.J.; Fenton, K.; Au, L.E.; Goldstein, L.H.; Shimada, T. School breakfast policy is associated with dietary intake of fourth- and fifth-grade students. J. Acad. Nutr. Diet. 2016, 116, 449–457. [Google Scholar] [CrossRef] [Green Version]
- Traub, M.; Lauer, R.; Kesztyüs, T.; Wartha, O.; Steinacker, J.M.; Kesztyüs, D.; the Research Group “Join the Healthy Boat”. Skipping breakfast, overconsumption of soft drinks and screen media: Longitudinal analysis of the combined influence on weight development in primary schoolchildren. BMC Public Health 2018, 18, 363. [Google Scholar] [CrossRef] [PubMed]
- Whitaker, R.C.; Dearth-Wesley, T.; Herman, A.N.; Oakes, J.M.; Owens, J.A. A quasi-experimental study of the impact of school start time changes on adolescents’ mood, self-regulation, safety, and health. Sleep Health 2019, 5, 466–469. [Google Scholar] [CrossRef] [PubMed]
- Ask, A.S.; Hernes, S.; Aarek, I.; Johannessen, G.; Haugen, M. Changes in dietary pattern in 15 year old adolescents following a 4 month dietary intervention with school breakfast--a pilot study. Nutr. J. 2006, 5, 33. [Google Scholar] [CrossRef] [Green Version]
- Au, L.E.; Whaley, S.; Rosen, N.J.; Meza, M.; Ritchie, L.D. Online and in-person nutrition education improves breakfast knowledge, attitudes, and behaviors: A randomized trial of participants in the special supplemental nutrition program for women, infants, and children. J. Acad. Nutr. Diet. 2016, 116, 490–500. [Google Scholar] [CrossRef] [PubMed]
- Bauer, K.W.; Foster, G.D.; Weeks, H.M.; Polonsky, H.M.; Davey, A.; Sherman, S.; Abel, M.L.; Ruth, K.J.; Dale, L.C.; Fisher, J.O. Breakfast in the classroom initiative and students’ breakfast consumption behaviors: A group randomized trial. Am. J. Public Health 2020, 11, 540–546. [Google Scholar] [CrossRef]
- Christensen, C.B.; Mikkelsen, B.E.; Toft, U. The effect of introducing a free breakfast club on eating habits among students at vocational schools. BMC Public Health 2019, 19, 369. [Google Scholar] [CrossRef] [Green Version]
- Crepinsek, M.K.; Singh, A.; Bernstein, L.S.; McLaughlin, J.E. Dietary effects of universal-free school breakfast: Findings from the evaluation of the school breakfast program pilot project. J. Am. Diet. Assoc. 2006, 106, 1796–1803. [Google Scholar] [CrossRef]
- Elseifi, O.S.; Abdelrahman, D.M.; Mortada, E.M. Effect of a nutritional education intervention on breakfast consumption among preparatory school students in Egypt. Int. J. Public Health 2020, 65, 893–903. [Google Scholar] [CrossRef]
- Kobel, S.; Wirt, T.; Schreiber, A.; Kesztyüs, D.; Kettner, S.; Erkelenz, N.; Wartha, O.; Steinacker, J.M. Intervention effects of a school-based health promotion programme on obesity related behavioural outcomes. J. Obes. 2014, 2014, 476230. [Google Scholar] [CrossRef]
- Leidy, H.J.; Hoertel, H.A.; Douglas, S.M.; Higgins, K.A.; Shafer, R.S. A high-protein breakfast prevents body fat gain, through reductions in daily intake and hunger, in “Breakfast skipping” adolescents. Obesity 2015, 3, 1761–1764. [Google Scholar] [CrossRef]
- Moore, G.F.; Murphy, S.; Chaplin, K.; Lyons, R.A.; Atkinson, M.; Moore, L. Impacts of the Primary School Free Breakfast Initiative on socio-economic inequalities in breakfast consumption among 9–11-year-old schoolchildren in Wales. Public Health Nutr. 2013, 17, 1280–1289. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Murphy, S.; Moore, G.F.; Tapper, K.; Lynch, R.; Clarke, R.; Raisanen, L.; Desousa, C.; Moore, L. Free healthy breakfasts in primary schools: A cluster randomised controlled trial of a policy intervention in Wales, UK. Public Health Nutr. 2010, 14, 219–226. [Google Scholar] [CrossRef] [PubMed]
- Pbert, L.; Druker, S.; Barton, B.; Schneider, K.L.; Olendzki, B.; Gapinski, M.A.; Kurtz, S.; Osganian, S. A school-based program for overweight and obese adolescents: A randomized controlled trial. J. Sch. Health 2016, 86, 699–708. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hania Szajewska, H.; Ruszczyński, M. Systematic review demonstrating that breakfast consumption influences body weight outcomes in children and adolescents in Europe. Crit. Rev. Food Sci. Nutr. 2010, 50, 113–119. [Google Scholar] [CrossRef]
- Ardeshirlarijani, E.; Namazi, N.; Jabbari, M.; Zeinali, M.; Gerami, H.; Jalili, R.B.; Larijani, B.; Azadbakht, L. The link between breakfast skipping and overweigh/obesity in children and adolescents: A meta-analysis of observational studies. J. Diabetes Metab. Disord. 2019, 18, 657–664. [Google Scholar] [CrossRef]
- Wicherski, J.; Schlesinger, S.; Fischer, F. Association between breakfast skipping and body weight—A systematic review and meta-analysis of observational longitudinal studies. Nutrients 2021, 13, 272. [Google Scholar] [CrossRef]
- Paixão, C.; Dias, C.M.; Jorge, R.; Carraça, E.V.; Yannakoulia, M.; de Zwaan, M.; Soini, S.; Hill, J.O.; Teixeira, P.J.; Santos, I. Successful weight loss maintenance: A systematic review of weight control registries. Obes Rev. 2020, 21, 13003. [Google Scholar] [CrossRef]
- Ma, X.; Chen, Q.; Pu, Y.; Guo, M.; Jiang, Z.; Huang, W.; Long, Y.; Xu, Y. Skipping breakfast is associated with overweight and obesity: A systematic review and meta-analysis. Obes. Res. Clin. Pract. 2020, 14, 1–8. [Google Scholar] [CrossRef]
- Bonnet, J.P.; Cardel, M.I.; Cellini, J.; Hu, F.B.; Guasch-Ferré, M. Breakfast skipping, body composition, and cardiometabolic risk: A systematic review and meta-analysis of randomized trials. Obesity 2020, 28, 1098–1109. [Google Scholar] [CrossRef] [PubMed]
- Di Francesco, A.; Di Germanio, C.; Bernier, M.; de Cabo, R. A time to fast. Science 2018, 362, 770–775. [Google Scholar] [CrossRef] [Green Version]
- Asher, G.; Sassone-Corsi, P. Time for food: The intimate interplay between nutrition, metabolism, and the circadian clock. Cell 2015, 161, 84–92. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lopez-Minguez, J.; Gómez-Abellán, P.; Garaulet, M. Timing of breakfast, lunch, and dinner. Effects on obesity and metabolic risk. Nutrients 2019, 11, 2624. [Google Scholar] [CrossRef] [Green Version]
- Hatori, M.; Vollmers, C.; Zarrinpar, A.; DiTacchio, L.; Bushong, E.A.; Gill, S.; Leblanc, M.; Chaix, A.; Joens, M.; Fitzpatrick, J.A.; et al. Time-restricted feeding without reducing caloric intake prevents metabolic diseases in mice fed a high-fat diet. Cell Metab. 2012, 15, 848–860. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sherman, H.; Frumin, I.; Gutman, R.; Chapnik, N.; Lorentz, A.; Meylan, J.; le Coutre, J.; Froy, O. Long-term restricted feeding alters circadian expression and reduces the level of inflammatory and disease markers. J. Cell Mol. Med. 2011, 15, 2745–2759. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Woodie, L.N.; Luo, Y.; Wayne, M.J.; Graff, E.C.; Ahmed, B.; O’Neill, A.M.; Greene, M.W. Restricted feeding for 9h in the active period partially abrogates the detrimental metabolic effects of a Western diet with liquid sugar consumption in mice. Metabolism 2018, 82, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Almoosawi, S.; Vingeliene, S.; Gachon, F.; Voortman, T.; Palla, L.; Johnston, J.D.; Van Dam, R.M.; Darimont, C.; Karagounis, L.G. Chronotype: Implications for Epidemiologic studies on chrono-nutrition and cardiometabolic health. Adv. Nutr. 2019, 10, 30–42. [Google Scholar] [CrossRef] [Green Version]
- Mekonnen, T.; Havdal, H.H.; Lien, N.; O’Halloran, S.A.; Arah, O.A.; Papadopoulou, E.; Gebremariam, M.K. Mediators of socioeconomic inequalities in dietary behaviours among youth: A systematic review. Obes. Rev. 2020, 21, 13016. [Google Scholar] [CrossRef] [Green Version]
- Xu, Y.Y.; Sawadogo-Lewis, T.; King, S.E.; Mitchell, A.; Roberton, T. Integrating nutrition into the education sector in low- and middle-income countries: A framework for a win-win collaboration. Matern. Child Nutr. 2021, 17, 13156. [Google Scholar] [CrossRef]
- Downer, S.; Berkowitz, S.A.; Harlan, T.S.; Olstad, D.L.; Mozaffarian, D. Food is medicine: Actions to integrate food and nutrition into healthcare. BMJ 2020, 369, 2482. [Google Scholar] [CrossRef]
- Hoertel, H.A.; Will, M.J.; Leidy, H.J. A randomized crossover, pilot study examining the effects of a normal protein vs. high protein breakfast on food cravings and reward signals in overweight/obese “breakfast skipping”, late-adolescent girls. Nutr. J. 2014, 13, 80. [Google Scholar] [CrossRef] [Green Version]
- Leidy, H.J.; Racki, E.M. The addition of a protein-rich breakfast and its effects on acute appetite control and food intake in ‘breakfast-skipping’ adolescents. Int. J. Obes. 2010, 34, 1125–1133. [Google Scholar] [CrossRef] [Green Version]
- Leidy, H.J.; Lepping, R.J.; Savage, C.R.; Harris, C.T. Neural responses to visual food stimuli after a normal vs. higher protein breakfast in breakfast-skipping teens: A pilot fMRI study. Obesity 2011, 19, 2019–2025. [Google Scholar] [CrossRef] [PubMed]
- Astrup, A.; Rössner, S. Lessons from obesity management programmes: Greater initial weight loss improves long-term maintenance. Obes. Rev. 2000, 1, 17–19. [Google Scholar] [CrossRef] [PubMed]
- Shai, I.; Schwarzfuchs, D.; Henkin, Y.; Shahar, D.R.; Witkow, S.; Greenberg, I.; Golan, R.; Fraser, D.; Bolotin, A.; Vardi, H.; et al. Dietary Intervention Randomized Controlled Trial (DIRECT) Group. Weight loss with a low-carbohydrate, Mediterranean, or low-fat diet. N. Engl. J. Med. 2008, 359, 229–241. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Takagi, H.; Hari, Y.; Nakashima, K.; Kuno, T.; Ando, T.; ALICE (All-Literature Investigation of Cardiovascular Evidence) Group. Meta-analysis of relation of skipping breakfast with heart disease. Am. J. Cardiol. 2019, 124, 978–986. [Google Scholar] [CrossRef] [PubMed]
- Coppola, A.; Sasso, L.; Bagnasco, A.; Giustina, A.; Gazzaruso, C. The role of patient education in the prevention and management of type 2 diabetes: An overview. Endocrine 2016, 53, 18–27. [Google Scholar] [CrossRef]

| Author, Year, Reference | Subjects | Design | Intervention | Follow-Up Time | BS Definition | OW/OB Definition | General Results | BS | OW/OB | BP | Lipid Profile | Glucose | MetS | Nutrition Quality |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Leatherdale ST, 2016 [18] | Secondary school students (grades 9–12th) T0: 23,921 T1: 23,117 M/F, Canada | COMPASS longitudinal Study | School breakfast program | 1 year | Breakfast < 5 days in a usual school week (Monday to Friday) | NA | T0 Free school breakfast program: 37 secondary schools Paid school breakfast program: 1 secondary school No school breakfast program: 5 secondary schools T1 ↔ in school breakfast program: 38 secondary schools (control schools) Changed free school breakfast program: 3 secondary schools (intervention schools) Starting free school breakfast program: 1 secondary school (intervention school) Stopping free school breakfast program: 1 secondary school (intervention school) | T1 vs. T0 ↑ BS prevalence (54.5 vs. 54.9%) ↑ Breakfast program participation (12.3 vs. 13.6%) | NA | NA | NA | NA | NA | NA |
| O’Dea JA, 2011 [19] | School-children 7–18 yrs 32 schools T0: 4237 T1: 5645 M/F, Australia | Longitudinal study | National breakfast promotion campaign | 2000 vs. 2006 | “No” response to the question: “On most days, do you usually eat or drink something for breakfast? (yes/no)” | IOTF | T1 vs. T0 ↑ Prevalence of OW/OB: 24.8% vs. 21.6%; χ2= 13.78 ↔ prevalence of NW | T1 vs. T0 ↓ BS: - all students: 12.7 vs. 17.0%; χ2 = 35.12, p < 0.0001 - M: 11.6 vs. 15.3%; χ2 = 42.24, p < 0.0001 - F: 13.8 vs. 18.9%; χ2 = 22.77, p < 0.0001 - primary school: F: 9.6 vs. 6.0%; M: 9.4 vs. 6.0% - secondary school: F: 27.7 vs. 18.7%; M: 19.9 vs. 12.1% | T1 vs. T0 ↑ Prevalence of OW/OB : 24.8% vs. 21.6% BS among OW/OB > NW participants, both at T0 (20.7 vs. 16.0%, χ2 = 11.1) and T1 (14.3 vs. 10.4%) | NA | NA | NA | NA | T1 vs. T0 ↑ nutritional quality of breakfast scores - M: all year groups - F: mainly older year groups ↑ in students from low socio-economic status schools |
| Ritchie LD, 2016 [20] | 3944 students (4–5th grade) in 43 low-resource elementary schools M/F, USA | Observational study; longitudinal baseline data of a cluster RCT | School-based intervention | NA | Zero calories recorded as breakfast | NA | / | Breakfast in the classroom: - ↓ BS students - ↑ eating breakfast at both home and school (p < 0.001) | NA | NA | NA | NA | NA | Breakfast in the classroom: ↑ overall dietary quality |
| Traub M, 2018 [21] | 1733 children aged 7.08 ± 0.6 yrs M/F, Germany | Prospective, cluster randomized and longitudinal study | School-based health promotion program | 1 year | Frequency of breakfast before school “often/always” vs. “never/rarely” → BS | OW: >90th BMI percentile OB: >97th percentile (German charts) | T1 BS among F > M | NA | BS ↑ odds of abdominal OB/OW at follow-up BS ↑ WHtR, weight, BMI percentiles, BMI (0.21 ± 0.01) and BMI z-scores (0.09 ± 0.03) | NA | NA | NA | NA | NA |
| Whitaker RC, 2019 [22] | 3197 students (≥12 and <19.0 yrs) 19 schools (8 middle, 8 high, 3 secondary schools) M/F, USA | Quasi-experimental study | School start time changes | 1 year | “No” response to the question: “On most school days, do you eat breakfast before your first class begins? (yes/no)” | NA | T1 vs. T0 ↓ BS in 50 min delay school | ↓ | NA | NA | NA | NA | NA | NA |
| Author, Year, Reference | Subjects | Design | Intervention | Follow-Up Time | BS Definition | OW/OB Definition | General Results | BS | OW/OB | BP | Lipid Profile | Glucose | MetS | Nutrition Quality |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Ask AS, 2006 [23] | 54 students; 15 yrs; 2 classes 10th grade secondary school M/F, Norway | Cn = 28 In = 26 | Breakfast at school | 4 months | Not having breakfast every day/week | IOTF | T1 vs. T0 In: ↑ breakfast every day; back to breakfast habits after 1 week | ↓ | T1 vs. T0 Cn: ↑ weight (p < 0.01) and BMI (p < 0.05) In: ↑weight in M (p < 0.05) ↔ OW/OB in both groups | NA | NA | NA | NA | T1 vs. T0 In: - ↑ healthy eating index in M (p < 0.01) - ↔ food supplements intake |
| Au LE, 2015 [24] | 590 caregivers of 1–5-year-old children F, USA | Cn (In-person education) = 359 In (Online education) = 231 | In-person vs. Online nutrition education | 2–4 months | Breakfast eating frequency questions from the Healthy Kids Survey | NA | ↓ barriers to eating breakfast in both groups ↑ frequency of eating breakfast in the online > in-person education group | ↓ | NA | NA | NA | NA | NA | NA |
| Bauer KW, 2020 [25] | 1362 students 10.8 ± 1.0 yrs, family incomes ≤130% or 130–185% of the federal poverty level M/F, USA | Cn = 723 In = 639 | Breakfast at school | 2.5 years | “Did you eat/drink anything today?” “No” → BS | CDC | T1 vs. T0 In vs. Cn: ↑ breakfast consumption at school (44.3% vs. 13.1%) | ↔ | NA | NA | NA | NA | NA | T1 vs. T0 In vs. Cn: - ↑ fruit juice (25.4% vs. 14.7%); - ↓ sugar-sweetened beverages (10.6% vs. 15.6%) - ↓ foods high in saturated fat and added sugar (20.9% vs. 26.9%) |
| Christensen CB, 2019 [26] | 318 students ≥ 16 yrs 4 vocational schools T0: 253 T1 (week 8): 168 T2 (week 14–16): 104 M/F, Denmark | Cluster-RCT 2: 2 schools Cn and In not correctly reported | Breakfast club intervention at school | 4 months | Breakfast consumption (<9:00 a.m.) self-reported frequency scale; “daily breakfast eaters” if breakfast at school all days (yes/no) | NA | ↑ daily breakfast eaters T1 vs. T0 - ↑ In vs. Cn (OR: 3.77) T2: NS | ↓ | NA | NA | NA | NA | NA | ↑ WG products in In vs. Cn at T1 (OR: 4.13) and T2 (OR: 3.27) |
| Crepinsek MK, 2006 [27] | 4278 primary school students 9.8 ± 1.3 yrs M/F, USA | Cn = 2066 In =2212 | Free breakfast at school | 1 year | Not having breakfast. “Any breakfast” = consumption of any food or beverage; or “a nutritional breakfast” = 2 of 5 food groups and energy > 10% 1989 REA | NA | T1 In vs. Cn - ↑ school breakfast - ↔ any breakfast eating - ↑ of a nutritional breakfast - ↔24h dietary intakes | ↔ any breakfast - ↑ nutritional breakfast | NA | NA | NA | NA | NA | NA |
| Elseifi OS, 2020 [28] | Students 12–14 yrs M/F, Egypt | Pre-post In study Cn = 112 In =112 | Nutritional education message | 5 weeks + 2 months | Frequency breakfast per week, from 0 to 7 days: BS = 0–2 semi-BS = 3–4 non-BS = 5–7 | WHO | ↑ Breakfast in students with normal BMI and BP | T1 vs. T0 In: BS↓ 36.6% vs. 19%, non BS↑ 28.6% vs. 44.7 | NA | NA | NA | NA | NA | T1 vs. T0 In: ↑ healthy breakfast BS: 57.1% vs. 68.8%, non-BS: ↑ 28.6% vs. 44.7 |
| Kobel S, 2014 [29] | Primary school children 154 classes 7.1 ± 0.6 yrs T0: 1943 T1: 1736 M/F, Germany | Prospective, cluster RCT and longitudinal study Cn= 74 In= 80 | School-based health promotion program | 1 year | Frequency of breakfast before school “often/always” vs. “never/rarely” → BS | OW: >90th BMI percentile OB: >97th percentile (German charts) | T0 BS F > M (15.4 vs. 10.6 %) T1 - ↑ BS in Cn (NS); ↔ in In - BS among second-graders in Cn > in In (OR = 0.52, 95% CI 0.30; 0.92) | ↔ | NA | NA | NA | NA | NA | T1 vs. T0 ↓ soft drink in both groups ↓ In > Cn (NS) |
| Leidy HJ, 2015 [30] | 54 BS adolescents 18±1 yrs M/F, USA | Cn (BS) = 9 Normal-protein (NP) breakfast = 21 High-protein (HP) breakfast=24 | NP and HP breakfasts | 12 weeks | No food or drinks before 10:00 a.m. | NA | T0 vs. T1 HP vs. Cn: ↓ fat mass and % body fat | NA | ↔ | NA | NA | NA | NA | T0 vs. T1 HP vs. Cn: - ↓ daily food intake (-1724 ± 954 vs. +1556 ± 745 kJ) - ↓ fat consumption (-24 ±12 vs. -16±14 g) - ↓ daily hunger |
| Moore GF, 2013 [31] | 111 primary schools (58 in socio-economically deprived areas) subjects aged 9–11 yrs T0: 4350 T1: 4472 M/F, Wales | Cluster-RCT Cn= 56 (T0: 2145; T1: 220) In= 55 (T0: 2205; T1: 2272) | School-based breakfast | 1 year | BS: ≤2 days | NA | / | ↓ BS in more deprived schools | NA | NA | NA | NA | NA | T1 ↑ healthy breakfast ↑ in more deprived Schools |
| Murphy S, 2010 [32] | 111 primary schools (58 in socio-economically deprived areas) subjects aged 9–11 yrs T0: 4350 T1: 4472 M/F, Wales | Cluster-RCT Cn = 56 (T0: 2145; T1: 220) In = 55 (T0: 2205; T1: 2272) | School-based breakfast | 1 year | BS: ≤2 days | NA | / | ↔ | NA | NA | NA | NA | NA | T1 ↑ healthy breakfast |
| Pbert L, 2016 [33] | 126 adolescents grades 9–12th 8 public schools M/F, USA | Pair-matched cluster-RCT Cn = 58 In = 68 | School nurse-delivered counseling | 8 months | Number of days eat breakfast in past 7 days | CDC | T1 vs. T0 ↑ days/week eating breakfast in In vs. Cn (4.65 vs. 3.84 days) | ↓ | ↔ | NA | NA | NA | NA | T1 vs. T0 - ↔ fruit and vegetable intake, drinking soda, eating fast foods - ↔ barriers to healthy eating |
| Author, Year, Ref | Study Design | Intervention | Outcome Measures |
|---|---|---|---|
| Leatherdale ST, 2016 [18] | Longitudinal | School breakfast program: eating breakfast as part of a school program one or more days in a usual school-week (Monday to Friday) | COMPASS School Programs and Policies Questionnaire (SPP): paper-based survey completed annually by school administrators most knowledgeable about the school program and policy environment within a school |
| O’Dea JA, 2011 [19] | Longitudinal | National breakfast promotion campaign including classroom lessons about nutrition and ideas for a breakfast menu at each school canteen | Questionnaire collected demographic details of the students (gender, age, school grade/year, usual breakfast consumption patterns, breakfast consumption on the day of the study, and contents of breakfast consumed) Height and weight were measured |
| Ritchie LD, 2016 [20] | Longitudinal | School-based intervention: 3 breakfast policies: (1) breakfast in the cafeteria before the start of school (17 schools); (2) breakfast in the classroom (20 schools); (3) second chance breakfast (6 schools) | Student demographic data (sex, race/ethnicity, language spoken at home) obtained by survey completed by students in the classroom Diet quality measured by the Healthy Eating Index 2010 |
| Traub M, 2018 [21] | Longitudinal | School-based health promotion program “Join the Healthy Boat”: training courses for teachers at primary school to promote healthy lifestyle choices in children, to increase physical, mental, and emotional abilities and, consequently, to attenuate the increase in body fat and thus to prevent overweight and obesity | Anthropometric data of the children (height, weight, waist circumference) were assessed in schools Parental questionnaires at baseline and follow-up (parent’s anthropometric data, child’s health behaviour, lifestyle, and socioeconomic background) |
| Whitaker RC, 2019 [22] | Longitudinal | 2 district-wide school start time (SST) changes implemented: (1) a 50 min delay, from 7:20 a.m. to 8:10 a.m., in high schools (grades 9–12) and secondary schools (grades 7–12) and (2) a 30 min advance, from 8 a.m. to 7:30 a.m., in middle schools (grades 7–8) | Repeated cross-sectional school surveys to evaluate the impacts of SST changes in a US school district Self-report surveys in the areas of mood, self-regulation, safety, and health |
| Ask AS, 2006 [23] | RCT | Intervention group: consisted of served breakfast at the beginning of each school day; students were also offered a food supplement (vitamins, minerals, and omega-3 fatty acids) Control group: was not served breakfast but got the same information about the importance of a healthy diet All parents were encouraged to provide a packed lunch for their children every day | Food frequency questionnaire (covered frequency intake of 27 food items commonly used in the Norwegian diet) Height and weight were measured with standard equipment by the school nurse before and after the study Diet quality measured by a healthy eating index |
| Au LE, 2015 [24] | RCT | Online vs. in-person nutrition education on the importance of having breakfast | Participants (in-person and online groups) completed a questionnaire to assess breakfast knowledge, attitudes, and behaviors |
| Bauer KW, 2020 [25] | RCT | Intervention group: Breakfast in the Classroom (BIC) + breakfast-specific nutrition education (18 lessons), social marketing to promote consumption of a healthy breakfast, marketing at 14 corner stores promoting healthier breakfast foods and drinks, parent outreach via family newsletters (24 newsletters) and information available at schools’ parent events Control group: offered breakfast in the cafeteria before school | Breakfast Patterns Survey (BPS) at baseline, midpoint, and endpoint to measure students’ food and drink consumption Data on students’ background were obtained from the school district Weight and height were measured, and BMI calculated |
| Christensen CB, 2019 [26] | RCT | Breakfast club intervention (BCI) based on wholegrain (WG) products Intervention group: schools served a free wholegrain breakfast every school day as part of the first lesson, either in the classroom or in the cafeteria; the breakfast consisted of a choice among four WG cereal products Control group: schools carried on as normal without the availability of free breakfast | Questionnaires measured dietary intake (breakfast intake, type of breakfast, frequency of snacking unhealthy food) and background (demographic information, behavioral involvement, and attitudinal questions) |
| Crepinsek MK, 2006 [27] | RCT | Intervention group: universal-free school breakfast for 3 consecutive school years Control group: traditional means-tested School Breakfast Program | 24-h dietary recall to evaluated food intake (taken with students only and with students and parents together) A subsample of students completed a second dietary recall 7–10 days after the first |
| Elseifi OS, 2020 [28] | RCT | Intervention group: nutritional education message based on Pender’s health promotion model: a specific 58-item questionnaire to assess behavioural factors related to breakfast consumption; 5 sessions (one session every week), 30 min each Control group: any education message | General self-administrated questionnaires (sociodemographic characters, quality and frequency of breakfast intake) Questionnaire for the Pender’s Health Promotion Model (HPM) regarding Breakfast Consumption Weight, height, BMI, and blood pressure were measured by researcher |
| Kobel S, 2014 [29] | RCT | School-based health promotion program “Join the Healthy Boat” Intervention group: training courses for teachers at primary school to promote healthy lifestyle choices in children, to increase physical, mental, and emotional abilities, and, consequently, to attenuate the increase in body fat and thus to prevent overweight and obesity Control group: followed the regular school curriculum | Parental questionnaire evaluated parameters: daily screen media time, physical activity behavior, soft drink consumption and breakfast patterns, parental education levels, height, and body weight Child’s anthropometric measurements (height and weight) were taken by trained technicians and BMI was calculated |
| Leidy HJ, 2015 [30] | RCT | Intervention group: Normal protein (NP; 13 g protein) and High protein (HP; 35 g protein) groups provided with specific breakfast meals to consume between 6:00 and 9:45 a.m. each day Control group: continued to skip breakfast (with nothing to eat/drink, besides water) before 10:00 a.m. | Body weight, body composition, 3-day free-living perceived appetite, and 3-day daily food intake (24-h dietary recalls) were assessed at baseline and 12 weeks |
| Murphy S, 2010 [31] | RCT | Intervention group: school-based breakfast before the commencement of classes, without any cost being borne by parents; aim of intervention was to encourage breakfast but also improve the nutritional quality of children’s breakfasts Control group: schools in control group were asked to refrain from setting up a breakfast scheme during the 12-month evaluation period | Data were collected by attitudes and dietary recall questionnaires (modified version of the Day in the Life Questionnaire, Strengths and Difficulties Questionnaire) |
| Moore GF, 2013 [32] | RCT | Intervention group: school-based breakfast before the commencement of classes, without any cost being borne by parents; aim of intervention was to encourage breakfast but also improve the nutritional quality of children’s breakfasts Control group: schools in control group were asked to refrain from setting up a breakfast scheme during the 12-month evaluation period | Data were collected by attitudes and dietary recall questionnaires (modified version of the Day in the Life Questionnaire, Strengths and Difficulties Questionnaire) |
| Pbert L, 2016 [33] | RCT | Intervention group: “Lookin’ Good Feelin’ Good”: a school nurse-delivered counseling intervention (6 weekly 30-min individual sessions + maintenance phase of 6 monthly sessions), an after-school exercise program (3 sessions/week for 8 months); program goals/focus of the counseling: eating healthy and being more physically active Control group: 12-session nurse contact with weight management information to reduce BMI and improve diet and activity among overweight and obese adolescents | Dietary intake was assessed with a 24-h dietary recall interview—Interactive Nutrition Data System Physical activity and nutrition behaviors were monitored with questionnaires Height, weight, and waist circumference were measured |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ricotti, R.; Caputo, M.; Monzani, A.; Pigni, S.; Antoniotti, V.; Bellone, S.; Prodam, F. Breakfast Skipping, Weight, Cardiometabolic Risk, and Nutrition Quality in Children and Adolescents: A Systematic Review of Randomized Controlled and Intervention Longitudinal Trials. Nutrients 2021, 13, 3331. https://doi.org/10.3390/nu13103331
Ricotti R, Caputo M, Monzani A, Pigni S, Antoniotti V, Bellone S, Prodam F. Breakfast Skipping, Weight, Cardiometabolic Risk, and Nutrition Quality in Children and Adolescents: A Systematic Review of Randomized Controlled and Intervention Longitudinal Trials. Nutrients. 2021; 13(10):3331. https://doi.org/10.3390/nu13103331
Chicago/Turabian StyleRicotti, Roberta, Marina Caputo, Alice Monzani, Stella Pigni, Valentina Antoniotti, Simonetta Bellone, and Flavia Prodam. 2021. "Breakfast Skipping, Weight, Cardiometabolic Risk, and Nutrition Quality in Children and Adolescents: A Systematic Review of Randomized Controlled and Intervention Longitudinal Trials" Nutrients 13, no. 10: 3331. https://doi.org/10.3390/nu13103331
APA StyleRicotti, R., Caputo, M., Monzani, A., Pigni, S., Antoniotti, V., Bellone, S., & Prodam, F. (2021). Breakfast Skipping, Weight, Cardiometabolic Risk, and Nutrition Quality in Children and Adolescents: A Systematic Review of Randomized Controlled and Intervention Longitudinal Trials. Nutrients, 13(10), 3331. https://doi.org/10.3390/nu13103331








