Frailty Intervention through Nutrition Education and Exercise (FINE). A Health Promotion Intervention to Prevent Frailty and Improve Frailty Status among Pre-Frail Elderly—A Study Protocol of a Cluster Randomized Controlled Trial
Abstract
1. Introduction
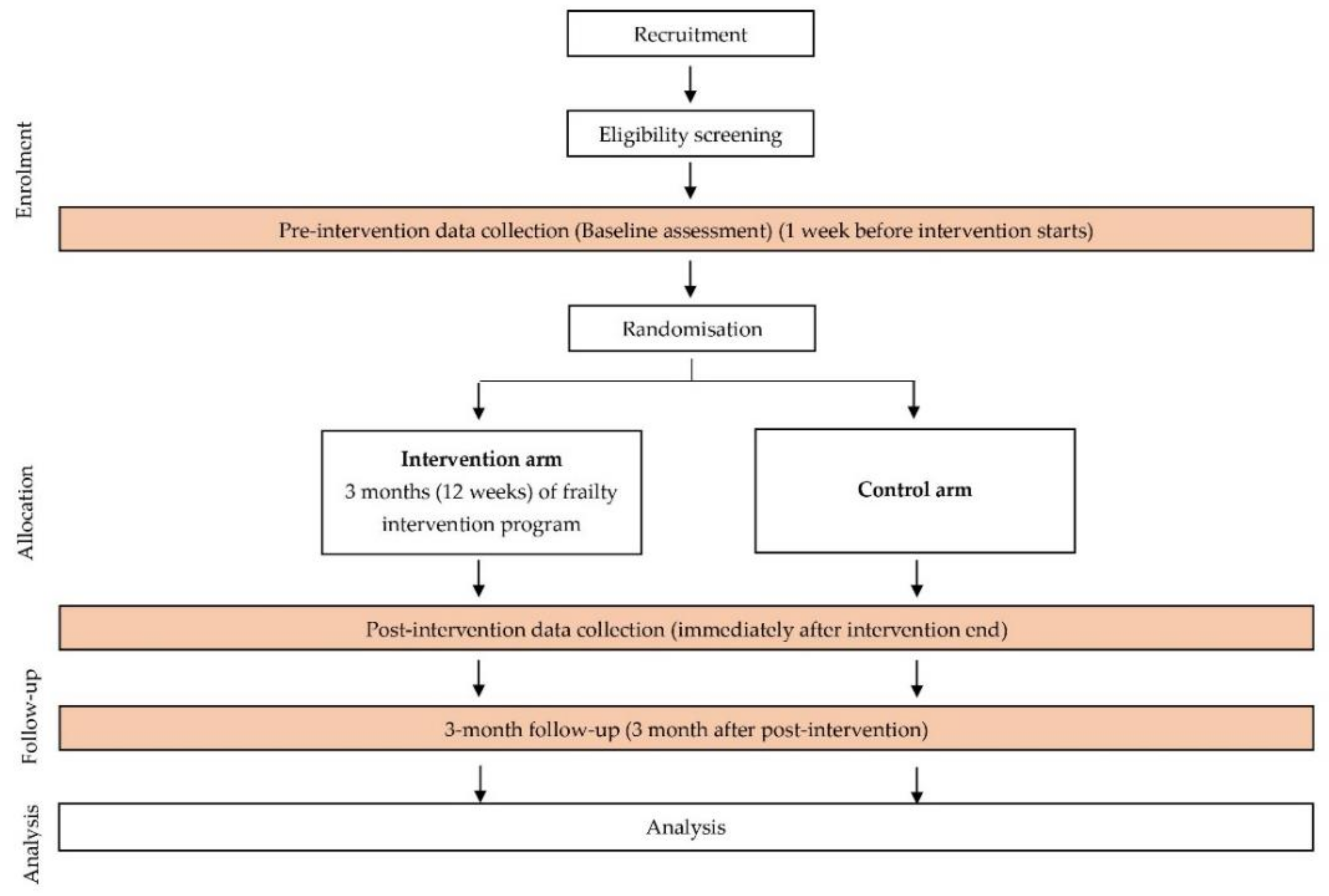
2. Materials and Methods
2.1. Trial Design
2.2. Participants
2.2.1. Ethics Approval
2.2.2. Screening of Frailty Status
2.2.3. Eligibility and Recruitment
2.2.4. Sample Size Calculation
2.2.5. Randomization and Allocation
2.3. Intervention
2.4. Outcome Measures
2.4.1. Primary Outcome
Frailty Score/Status
2.4.2. Secondary Outcomes
Knowledge, Attitude, and Practice (KAP) towards Frailty, Nutrition, and Exercise
Dietary Intake
Anthropometric Measurements
- Body weight will be measured using an electronic flat scale (SECA 803, Hamburg, Germany).
- Height of the participant will be measured using stadiometer (SECA 213, Hamburg, Germany).
- When no valid measurement can be obtained due to particularities (e.g., kyphosis, scoliosis), an alternative method will be used to measure the height using a demi-span measurement. The height will be measured using equations developed for the Malaysian elderly [52].
- Body Mass Index (BMI) will be derived using the calculation: weight in kilograms divided by the height in meters squared [weight (kg)/height2 (m2)] [53]
- Body part circumference including mid-upper arm circumference (MUAC) and calf circumference (CC) will be measured using a flexible non-stretchable measuring tape (SECA 201, Hamburg, Germany) [52].
- Body composition including body fat percentage and muscle percentage will be assessed using a portable body composition analyzer (OMRON HBF-375, Japan).
Cognitive Status
Functional Ability
Mobility Status
Risk of Falls
2.5. Statistical Analysis
3. Discussion
4. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Loh, D.A.; Hairi, N.N.; Choo, W.Y.; Mohd Hairi, F.; Peramalah, D.; Kandiben, S.; Lee, P.L.; Gani, N.; Madzlan, M.F.; Abd Hamid, M.A.I.; et al. MultiCfomponent Exercise and theRApeutic lifeStyle (CERgAS) intervention to improve physical performance and maintain independent living among urban poor older people—A cluster randomised controlled trial. BMC Geriatr. 2015, 15, 8. [Google Scholar] [CrossRef] [PubMed]
- Sathasivam, J.; Bahyah Kamaruzzaman, S.; Hairi, F.; Wan Ng, C.; Chinna, K. Frail elders in an urban district setting in Malaysia: Multidimensional frailty and its correlates. Asia Pacific J. Public Health 2015, 27, 52–61. [Google Scholar] [CrossRef] [PubMed]
- Gallucci, M.; Ongaro, F.; Amici, G.P.; Regini, C. Frailty, disability and survival in the elderly over the age of seventy: Evidence from “The Treviso Longeva (TRELONG) Study”. Arch. Gerontol. Geriatr. 2009, 48, 281–283. [Google Scholar] [CrossRef] [PubMed]
- Fairhall, N.; Aggar, C.; Kurrle, S.E.; Sherrington, C.; Lord, S.; Lockwood, K.; Monaghan, N.; Cameron, I.D. Frailty intervention trial (FIT). BMC Geriatr. 2008, 8, 27. [Google Scholar] [CrossRef] [PubMed]
- Fried, L.P.; Tangen, C.M.; Walston, J.; Newman, A.B.; Hirsch, C.; Gottdiener, J.; Seeman, T.; Tracy, R.; Kop, W.J.; Burke, G.; et al. Frailty in older adults: Evidence for a phenotype. J. Gerontol. Ser. A Biol. Sci. Med. Sci. 2001, 56, 146–157. [Google Scholar] [CrossRef]
- Van Kan, G.A.; Rolland, Y.; Bergman, H.; Morley, J.E.; Kritchevsky, S.B.; Vellas, B. The I.A.N.A. task force on frailty assessment of older people in clinical practice. J. Nutr. Health Aging 2008, 12, 29–37. [Google Scholar] [CrossRef]
- Sánchez-García, S.; Sánchez-Arenas, R.; García-Peña, C.; Rosas-Carrasco, O.; Ávila-Funes, J.A.; Ruiz-Arregui, L.; Juárez-Cedillo, T. Frailty among community-dwelling elderly Mexican people: Prevalence and association with sociodemographic characteristics, health state and the use of health services. Geriatr. Gerontol. Int. 2014, 14, 395–402. [Google Scholar] [CrossRef]
- Robertson, D.A.; Savva, G.M.; Kenny, R.A. Frailty and cognitive impairment—A review of the evidence and causal mechanisms. Ageing Res. Rev. 2013, 12, 840–851. [Google Scholar] [CrossRef]
- Etman, A.; Burdorf, A.; Van der Cammen, T.J.M.; Mackenbach, J.P.; Van Lenthe, F.J. Socio-demographic determinants of worsening in frailty among community-dwelling older people in 11 European countries. J. Epidemiol. Community Health 2012, 66, 1116–1121. [Google Scholar] [CrossRef]
- Soysal, P.; Veronese, N.; Thompson, T.; Kahl, K.G.; Fernandes, B.S.; Prina, A.M.; Solmi, M.; Schofield, P.; Koyanagi, A.; Tseng, P.T.; et al. Relationship between depression and frailty in older adults: A systematic review and meta-analysis. Ageing Res. Rev. 2017, 36, 78–87. [Google Scholar] [CrossRef]
- Ensrud, K.E.; Ewing, S.K.; Taylor, B.C.; Fink, H.A.; Stone, K.L.; Cauley, J.A.; Tracy, J.K.; Hochberg, M.C.; Rodondi, N.; Cawthon, P.M.; et al. Frailty and risk of falls, fracture, and mortality in older women: The study of osteoporotic fractures. J. Gerontol. A Biol. Sci. Med. Sci. 2007, 62, 744–751. [Google Scholar] [CrossRef] [PubMed]
- Choi, J.; Ahn, A.; Kim, S. Global prevalence of physical frailty by fried’s criteria in community-dwelling elderly with national population-based surveys. J. Am. Med. Dir. Assoc. 2015, 16, 548–550. [Google Scholar] [CrossRef] [PubMed]
- Liu, L.K.; Lee, W.J.; Chen, L.Y.; Hwang, A.C.; Lin, M.H.; Peng, L.N.; Chen, L.K. Association between frailty, osteoporosis, falls and hip fractures among community-dwelling people aged 50 years and older in Taiwan: Results from I-Lan longitudinal aging study. PLoS ONE 2015, 10, e0136968. [Google Scholar] [CrossRef] [PubMed]
- Ng, T.P.; Feng, L.; Nyunt, M.S.Z.; Feng, L.; Niti, M.; Tan, B.Y.; Chan, G.; Khoo, S.A.; Chan, S.M.; Yap, P.; et al. Nutritional, physical, cognitive, and combination interventions and frailty reversal among older adults: A randomized controlled trial. Am. J. Med. 2015, 128, 1225–1236. [Google Scholar] [CrossRef]
- Badrasawi, M.; Shahar, S.; Singh, D.K.A. Risk factors of frailty among multi-ethnic malaysian older adults. Int. J. Gerontol. 2017, 11, 154–160. [Google Scholar] [CrossRef]
- Mohd Hamidin, F.A.; Adznam, S.N.; Ibrahim, Z.; Chan, Y.M.; Abdul Aziz, N.H. Prevalence of frailty syndrome and its associated factors among community-dwelling elderly in East Coast of Peninsular Malaysia. SAGE Open Med. 2018, 6. [Google Scholar] [CrossRef]
- Nur Farhana, M.; Suzana, S.; Manal, S.; Devinder, K.A. Frailty and nutritional status among older adults in Perak and Kelantan. In Proceedings of the NSM Conference, Renaissance Hotel, Kuala Lumpur, Malaysia, 3–4 June 2014. [Google Scholar]
- Kwon, J.; Yoshida, Y.; Yoshida, H.; Kim, H.; Suzuki, T.; Lee, Y. Effects of a combined physical training and nutrition intervention on physical performance and health-related quality of life in prefrail older women living in the community: A randomized controlled trial. J. Am. Med. Dir. Assoc. 2015, 16, 2631–2638. [Google Scholar]
- Drey, M.; Zech, A.; Freiberger, E.; Bertsch, T.; Uter, W.; Sieber, C.C.; Pfeifer, K.; Bauer, J.M. Effects of strength training versus power training on physical performance in prefrail community-dwelling older adults. Gerontology 2012, 58, 197–204. [Google Scholar] [CrossRef]
- Badrasawi, M.; Shahar, S.; Zahara, A.M.; Nor Fadilah, R.; Singh, D.K.A. Efficacy of L-carnitine supplementation on frailty status and its biomarkers, nutritional status, and physical and cognitive function among prefrail older adults: A double-blind, randomized, placebo-controlled clinical trial. Clin. Interv. Aging 2016, 11, 1675–1686. [Google Scholar] [CrossRef]
- Faber, M.J.; Bosscher, R.J.; Chin, A.; Paw, M.J.; Van Wieringen, P.C. Effects of exercise programs on falls and mobility in frail and pre-frail older adults: A multicenter randomized controlled trial. Arch. Phys. Med. Rehabil. 2006, 87, 885–896. [Google Scholar] [CrossRef]
- Hutchins-Wiese, H.L.; Kleppinger, A.; Annis, K.; Liva, E.; Lammi-Keefe, C.J.; Durham, H.A.; Kenny, A.M. The impact of supplemental n-3 long chain polyunsaturated fatty acids and dietary antioxidants on physical performance in postmenopausal women. J. Nutr. Health Aging. 2013, 17, 76–80. [Google Scholar] [CrossRef] [PubMed]
- Kim, C.O.; Lee, K.R. Preventive effect of protein-energy supplementation on the functional decline of frail older adults with low socioeconomic status: A community-based randomized controlled study. J. Gerontol. A Biol. Sci. Med. Sci. 2013, 68, 309–316. [Google Scholar] [CrossRef] [PubMed]
- Tieland, M.; Van de Rest, O.; Dirks, M.L.; Van der Zwaluw, N.; Mensink, M.; Van Loon, L.J.C.; De Groot, L.C.P.G.M. Protein supplementation improves physical performance in frail elderly people: A randomized, double-blind, placebo-controlled trial. J. Am. Med. Dir. Assoc. 2012, 13, 720–726. [Google Scholar] [CrossRef]
- Smoliner, C.; Norman, K.; Scheufele, R.; Hartig, W.; Pirlich, M.; Lochs, H. Effects of food fortification on nutritional and functional status in frail elderly nursing home residents at risk of malnutrition. Nutrition 2008, 24, 1139–1144. [Google Scholar] [CrossRef] [PubMed]
- Chan, D.C.; Tsou, H.H.; Yang, R.S.; Tsauo, J.Y.; Chen, C.Y.; Hsiung, C.A.; Kuo, K.N. A pilot randomized controlled trial to improve geriatric frailty. BMC Geriatr. 2012, 12, 5. [Google Scholar] [CrossRef]
- Nykänen, I.; Rissanen, T.H.; Sulkava, R.; Hartikainen, S. Effects of individual dietary counseling as part of a comprehensive geriatric assessment (CGA) on frailty status: A population-based intervention study. J. Clin. Gerontol. Geriatr. 2012, 3, 89–93. [Google Scholar] [CrossRef][Green Version]
- Manal, B.; Shahar, S.; Singh, D.K.A. Nutrition and frailty: A review of clinical intervention studies. J. Frailty Aging 2015, 4, 100–106. [Google Scholar]
- Tarazona-Santabalbina, F.J.; Gómez-Cabrera, M.C.; Pérez-Ros, P.; Martínez-Arnau, F.M.; Cabo, H.; Tsaparas, K.; Salvador-Pascual, A.; Rodriguez-Mañas, L.; Viña, J. A multicomponent exercise intervention that reverses frailty and improves cognition, emotion, and social networking in the community-dwelling frail elderly: A randomized clinical trial. J. Am. Med. Dir. Assoc. 2016, 17, 426–433. [Google Scholar] [CrossRef]
- Langlois, F.; Vu, T.T.M.; Chassé, K.; Dupuis, G.; Kergoat, M.-J.; Bherer, L. Benefits of physical exercise training on cognition and quality of life in frail older adults. J. Gerontol. B Psychol. Sci. Soc. Sci. 2012, 68, 400–404. [Google Scholar] [CrossRef]
- Giné-Garriga, M.; Guerra, M.; Unnithan, V.B. The effect of functional circuit training on self-reported fear of falling and health status in a group of physically frail older individuals: A randomized controlled trial. Aging Clin. Exp. Res. 2013, 25, 329–336. [Google Scholar] [CrossRef]
- Brown, M.; Sinacore, D.R.; Ehsani, A.A.; Binder, E.F.; Holloszy, J.O.; Kohrt, W.M. Low-intensity exercise as a modifier of physical frailty in older adults. Arch. Phys. Med. Rehabil. 2000, 81, 960–965. [Google Scholar] [CrossRef] [PubMed]
- Dedeyne, L.; Deschodt, M.; Verschueren, S.; Tournoy, J.; Gielen, E. Effects of multi-domain interventions in (pre) frail elderly on frailty, functional, and cognitive status: A systematic review. Clin. Interv. Aging 2017, 12, 873–896. [Google Scholar] [CrossRef] [PubMed]
- Lee, P.H.; Lee, Y.S.; Chan, D.C. Interventions targeting geriatric frailty: A systemic review. J. Clin. Gerontol. Geriatr. 2012, 3, 47–52. [Google Scholar] [CrossRef][Green Version]
- Theou, O.; Stathokostas, L.; Roland, K.P.; Jakobi, J.M.; Patterson, C.; Vandervoort, A.A.; Jones, G.R. The effectiveness of exercise interventions for the management of frailty: A systematic review. J. Aging Res. 2011. [Google Scholar] [CrossRef]
- Nash, K.C.M. The effects of exercise on strength and physical performance in frail older people: A systematic review. Rev. Clin. Gerontol. 2012, 22, 274–285. [Google Scholar] [CrossRef]
- Çakmur, H. Frailty among elderly adults in a rural area of Turkey. Med. Sci. Monit. 2015, 21, 1232–1242. [Google Scholar] [CrossRef]
- Timpini, A.; Facchi, E.; Cossi, S.; Ghisla, M.K.; Romanelli, G.; Marengoni, A. Self-reported socio-economic status, social, physical and leisure activities and risk for malnutrition in late life: A cross-sectional population-based study. J. Nutr. Health Aging 2011, 15, 233–238. [Google Scholar] [CrossRef]
- Lilamand, M.; Kelaiditi, E.; Cesari, M.; Raynaud-Simon, A.; Ghisolfi, A.; Guyonnet, S.; Vellas, B.; Abellan van Kan, G.; The Toulouse Frailty Platform Team. Validation of the mini nutritional assessment-short form in a population of frail elders without disability. Analysis of the toulouse frailty platform population in 2013. J. Nutr. Health Aging 2015, 19, 570–574. [Google Scholar] [CrossRef]
- Tee, G.A.; Ahmad, Y. Public low-cost housing in malaysia: Case studies on PPR low-cosr flats in Kuala Lumpur. J. Des. Built Environ. 2012, 8, 1–18. [Google Scholar]
- Campbell, M.K.; Piaggio, G.; Elbourne, D.R.; Altman, D.G. Consort 2010 statement: Extension to cluster randomised trials. BMJ 2012, 345, e5661. [Google Scholar] [CrossRef]
- Daniel, W. Biostatistics: A Foundation for Analysis in the Health Sciences, 7th ed.; John Wiley & Sons: New York, NY, USA, 1999. [Google Scholar]
- Gledhill, N. Physical Activity Readiness Questionnaire (PAR-Q) and You; Canadian Society for Exercise Physiology: Ottawa, ON, Canada, 2002. [Google Scholar]
- Kua, E.H.; Ko, S.M. A questionnaire to screen for cognitive impairment among elderly people in developing countries. Acta Psychiatr. Scand. 1992, 85, 119–122. [Google Scholar] [CrossRef]
- Tokolahi, E.; Hocking, C.; Kersten, P.; Vandal, A.C. Quality and reporting of cluster randomized controlled trials evaluating occupational therapy interventions: A systematic review. OTJR Occup. Particip. Health 2016, 36, 14–24. [Google Scholar] [CrossRef]
- Apóstolo, J.; Cooke, R.; Bobrowicz-Campos, E.; Santana, S.; Marcucci, M.; Cano, A.; Vollenbroek-Hutten, M.; Germini, F.; D′Avanzo, B.; Gwyther, H.; et al. Effectiveness of interventions to prevent pre-frailty and frailty progression in older adults. JBI Database Syst. Rev. Implement. Rep. 2018, 16, 140–232. [Google Scholar] [CrossRef] [PubMed]
- Dent, E.; Lien, C.; Lim, W.S.; Wong, W.C.; Wong, C.H.; Ng, T.P.; Woo, J.; Dong, B.; De la Vega, S.; Hua Poi, P.J.; et al. The asia-pacific clinical practice guidelines for the management of frailty. J. Am. Med. Dir. Assoc. 2017, 18, 564–575. [Google Scholar] [CrossRef] [PubMed]
- Alibhai, S.M.H.; Greenwood, C.; Payette, H. An approach to the management of unintentional weight loss in elderly people. Can. Med. Assoc. J. 2005, 172, 773–780. [Google Scholar] [CrossRef] [PubMed]
- National Coordinating Committee on Food and Nutrition. Malaysian Dietary Guidelines, 1st ed.; Technical Working Group on Nutritional Guidelines: Putrajaya, Malaysia, 2010; p. 27. [Google Scholar]
- Dorner, T.E.; Lackinger, C.; Haider, S.; Luger, E.; Kapan, A.; Luger, M.; Schindler, K.E. Nutritional intervention and physical training in malnourished frail community-dwelling elderly persons carried out by trained lay “buddies”: Study protocol of a randomized controlled trial. BMC Public Health 2013, 13, 1232. [Google Scholar] [CrossRef] [PubMed]
- Ministry of Health (MOH). Recommended Nutrient Intakes for Malaysia (RNI). In A Report of the Technical Working Group on Nutritional Guidelines; National Coordinating Committee on Food and Nutrition (NCCFN): Putrajaya, Malaysia, 2017; pp. 519–523. [Google Scholar]
- Ngoh, H.J.; Sakinah, H.; Harsa Amylia, M.S. Development of demi-span equations for predicting height among the Malaysian elderly. Malays. J. Nutr. 2012, 18, 149–159. [Google Scholar] [PubMed]
- Muhamad, A.R.; Hamirudin, A.H.; Zainudin, N.; Sidek, S.; Rahman, N.A.A. Nutritional risk according to mini nutritional assessment-short form amonng community dwelling elderly in Kuantan, Pahang: A pilot study. Int. J. Allied Health Sci. 2019, 3, 247–667. [Google Scholar]
- Ibrahim, N.M.; Shohaimi, S.; Chong, H.T.; Rahman, A.H.A.; Razali, R.; Esther, E.; Basri, H.B. Validation study of the mini-mental state examination in a Malay-speaking elderly population in Malaysia. Dement. Geriatr. Cogn. Disord. 2009, 27, 247–253. [Google Scholar] [CrossRef]
- Singh, D.K.A.; Pillai, S.G.K.; Tan, S.T.; Tai, C.C.; Shahar, S. Association between physiological falls risk and physical performance tests among community-dwelling older adults. Clin. Interv. Aging 2015, 10, 1319–1326. [Google Scholar] [CrossRef]
- Berg, K.; Wood-Dauphinee, S.; Ivan Williams, J.; Maki, B. Measuring balance in the elderly: Development and validation of an instrument. Can. J. Public Health 1992, 83, 1–130. [Google Scholar]
- Maneesriwongul, W.; Dixon, J.K. Instrument translation process: A methods review. J. Adv. Nurs. 2004, 48, 175–186. [Google Scholar] [CrossRef] [PubMed]
- Hayes, R.J.; Moulton, L.H. Cluster Randomised Trials, 2nd ed.; CRC Press Taylor & Francis Group: Boca Raton, FL, USA, 2017; pp. 197–199. [Google Scholar]
- Haider, S.; Dorner, T.E.; Luger, E.; Kapan, A.; Titze, S.; Lackinger, C.; Schindler, K.E. Impact of a home-based physical and nutritional intervention program conducted by lay-volunteers on handgrip strength in prefrail and frail older adults: A randomized control trial. PLoS ONE 2017, 12, e0169613. [Google Scholar] [CrossRef] [PubMed]
- Shahar, S.; Kamaruddin, N.S.; Badrasawi, M.; Mohamed Sakian, N.I.; Manaf, Z.A.; Yassin, Z.; Joseph, L. Effectiveness of exercise and protein supplementation intervention on body composition, functional fitness, and oxidative stress among elderly Malays with sarcopenia. Clin. Interv. Aging 2013, 8, 1365–1375. [Google Scholar] [CrossRef] [PubMed]
- Fougère, B.; Morley, J.E. Weight loss is a major cause of frailty. J. Nutr. Health Aging 2017, 21, 933–935. [Google Scholar] [CrossRef]
| Inclusion Criteria | Exclusion Criteria |
|---|---|
|
|
|
|
|
|
|
|
|
|
| |
| |
| |
|
| Intervention Group | Control Group | ||||
|---|---|---|---|---|---|
| 12 weeks intervention program | Week | Day 1 | Day 2 | Day 3 | * No intervention |
| 1 | Talk on frailty | Talk on exercise | Talk on healthy eating | ||
| 2 | Multicomponent exercise * | ||||
| 3 | Multicomponent exercise * | Nutrition education class | |||
| 4 | Multicomponent exercise * | ||||
| 5 | Multicomponent exercise * | Nutrition education class | |||
| 6 | Multicomponent exercise * | ||||
| 7 | Multicomponent exercise * | Nutrition education class | |||
| 8 | Multicomponent exercise * | ||||
| 9 | Multicomponent exercise * | Nutrition education class | |||
| 10 | Multicomponent exercise * | ||||
| 11 | Multicomponent exercise * | Nutrition education class | |||
| 12 | INTERVENTION END | ||||
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mohd Suffian, N.I.; Adznam, S.N.‘A.; Abu Saad, H.; Chan, Y.M.; Ibrahim, Z.; Omar, N.; Murat, M.F. Frailty Intervention through Nutrition Education and Exercise (FINE). A Health Promotion Intervention to Prevent Frailty and Improve Frailty Status among Pre-Frail Elderly—A Study Protocol of a Cluster Randomized Controlled Trial. Nutrients 2020, 12, 2758. https://doi.org/10.3390/nu12092758
Mohd Suffian NI, Adznam SN‘A, Abu Saad H, Chan YM, Ibrahim Z, Omar N, Murat MF. Frailty Intervention through Nutrition Education and Exercise (FINE). A Health Promotion Intervention to Prevent Frailty and Improve Frailty Status among Pre-Frail Elderly—A Study Protocol of a Cluster Randomized Controlled Trial. Nutrients. 2020; 12(9):2758. https://doi.org/10.3390/nu12092758
Chicago/Turabian StyleMohd Suffian, Nurul Izzati, Siti Nur ‘Asyura Adznam, Hazizi Abu Saad, Yoke Mun Chan, Zuriati Ibrahim, Noraida Omar, and Muhammad Faizal Murat. 2020. "Frailty Intervention through Nutrition Education and Exercise (FINE). A Health Promotion Intervention to Prevent Frailty and Improve Frailty Status among Pre-Frail Elderly—A Study Protocol of a Cluster Randomized Controlled Trial" Nutrients 12, no. 9: 2758. https://doi.org/10.3390/nu12092758
APA StyleMohd Suffian, N. I., Adznam, S. N. ‘A., Abu Saad, H., Chan, Y. M., Ibrahim, Z., Omar, N., & Murat, M. F. (2020). Frailty Intervention through Nutrition Education and Exercise (FINE). A Health Promotion Intervention to Prevent Frailty and Improve Frailty Status among Pre-Frail Elderly—A Study Protocol of a Cluster Randomized Controlled Trial. Nutrients, 12(9), 2758. https://doi.org/10.3390/nu12092758





