Nutritional Status and Quality of Life in Hospitalised Cancer Patients Who Develop Intestinal Failure and Require Parenteral Nutrition: An Observational Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Setting
2.2. Study Population
2.3. Data Collection
2.3.1. Demographics and Serum Biochemistry
2.3.2. Anthropometrics, NS, QoLand PS
2.4. Ethical Considerations
2.5. Statistical Analysis
3. Results
3.1. Descriptives
3.2. Nutritional Status
3.2.1. Prevalence of Malnutrition
3.2.2. Agreement between Malnutrition Risk Assessment Tools
3.2.3. Nutritional Status Indicators
3.3. Quality of Life
3.3.1. Exploratory Factor Analysis and Internal Consistency
3.3.2. Quality of Life Correlations
3.4. Performance Status
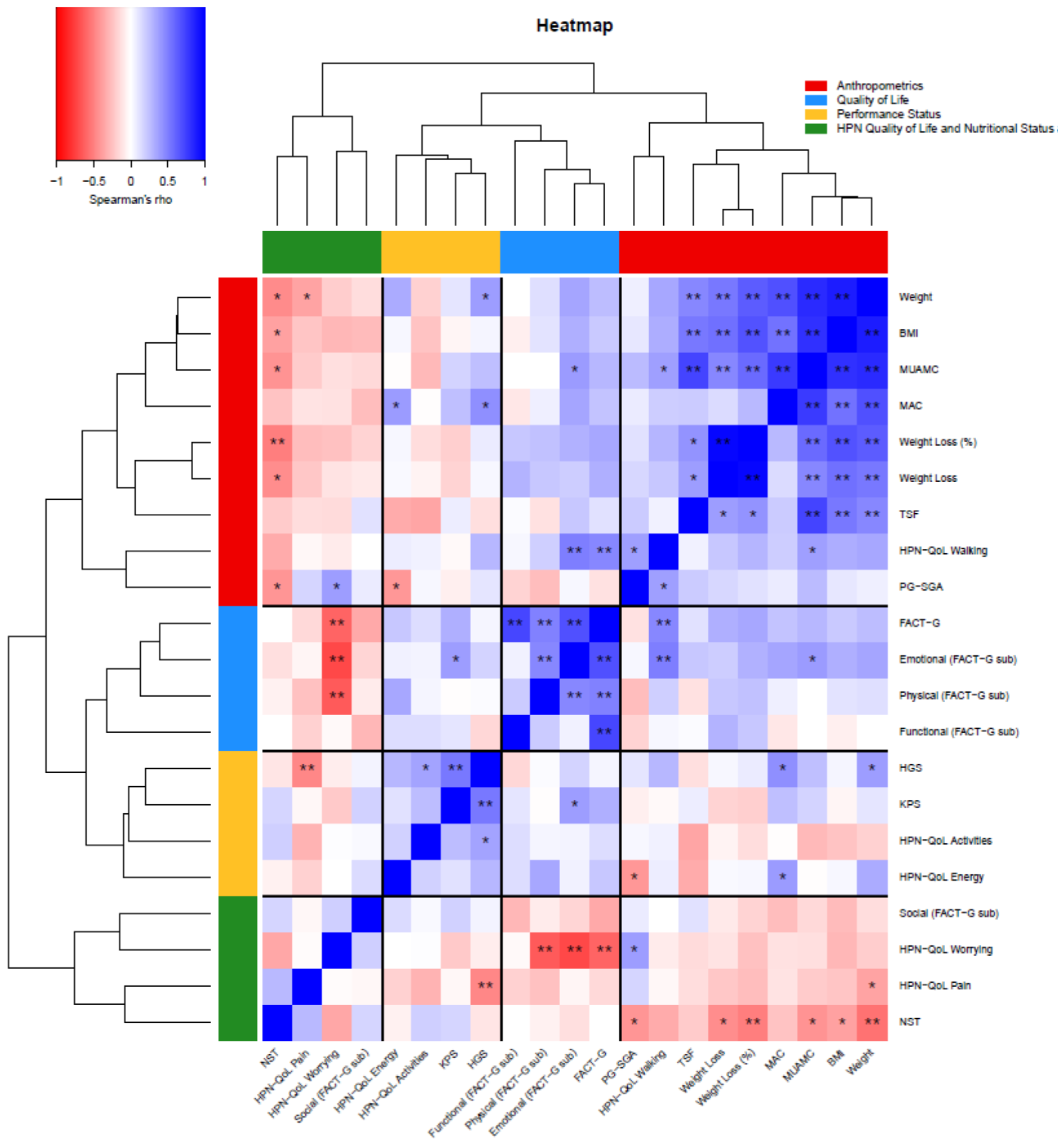
3.5. Cluster Heatmap
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
References
- Arends, J.; Bachmann, P.; Baracos, V.; Barthelemy, N.; Bertz, H.; Bozzetti, F.; Fearon, K.; Hütterer, E.; Isenring, E.; Kaasa, S.; et al. ESPEN guidelines on nutrition in cancer patients. Clin. Nutr. 2017, 36, 11–48. [Google Scholar] [CrossRef]
- Fearon, K.; Strasser, F.; Anker, S.D.; Bosaeus, I.; Bruera, E.; Fainsinger, R.L.; Jatoi, A.; Loprinzi, C.; MacDonald, N.; Mantovani, G.; et al. Definition and classification of cancer cachexia: An international consensus. Lancet Oncol. 2011, 12, 489–495. [Google Scholar] [CrossRef]
- Vashi, P.G.; Dahlk, S.; Popiel, B.; Lammersfeld, C.A.; Ireton-Jones, C.; Gupta, D. A longitudinal study investigating quality of life and nutritional outcomes in advanced cancer patients receiving home parenteral nutrition. BMC Cancer 2014, 14, 593. [Google Scholar] [CrossRef]
- Baracos, V.E.; Martin, L.; Korc, M.; Guttridge, D.C.; Fearon, K.C.H. Cancer-associated cachexia. Nat. Rev. Dis. Primers 2018, 4, 17105. [Google Scholar] [CrossRef] [PubMed]
- Aversa, Z.; Costelli, P.; Muscaritoli, M. Cancer-induced muscle wasting: Latest findings in prevention and treatment. Ther. Adv. Med. Oncol. 2017, 9, 369–382. [Google Scholar] [CrossRef] [PubMed]
- Bozzetti, F.; Arends, J.; Lundholm, K.; Micklewright, A.; Zurcher, G.; Muscaritoli, M. ESPEN Guidelines on Parenteral Nutrition: Non-surgical oncology. Clin. Nutr. 2009, 28, 445–454. [Google Scholar] [CrossRef] [PubMed]
- Arends, J.; Baracos, V.; Bertz, H.; Bozzetti, F.; Calder, P.C.; Deutz, N.E.; Erickson, N.; Laviano, A.; Lisanti, M.P.; Lobo, D.N.; et al. ESPEN expert group recommendations for action against cancer-related malnutrition. Clin. Nutr. 2017, 36, 1187–1196. [Google Scholar] [CrossRef] [PubMed]
- Cotogni, P.; Monge, T.; Fadda, M.; De Francesco, A. Bioelectrical impedance analysis for monitoring cancer patients receiving chemotherapy and home parenteral nutrition. BMC Cancer 2018, 18, 990. [Google Scholar] [CrossRef]
- Drissi, M.; Cwieluch, O.; Lechner, P.; Radziwill, R.; Vehling-Kaiser, U.; Hengst, K.; Masin, M. Nutrition care in patients with cancer: A retrospective multicenter analysis of current practice-Indications for further studies? Clin. Nutr. 2015, 34, 207–211. [Google Scholar] [CrossRef]
- Douglas, E.; McMillan, D.C. Towards a simple objective framework for the investigation and treatment of cancer cachexia: The Glasgow Prognostic Score. Cancer Treat. Rev. 2014, 40, 685–691. [Google Scholar] [CrossRef]
- Virizuela, J.A.; Camblor-Álvarez, M.; Luengo-Pérez, L.M.; Grande, E.; Álvarez-Hernández, J.; Sendrós-Madroño, M.J.; Jiménez-Fonseca, P.; Cervera-Peris, M.; Ocón-Bretón, M.J. Nutritional support and parenteral nutrition in cancer patients: An expert consensus report. Clin. Transl. Oncol. 2018, 20, 619–629. [Google Scholar] [CrossRef] [PubMed]
- Pironi, L.; Arends, J.; Baxter, J.; Bozzetti, F.; Peláez, R.B.; Cuerda, C.; Forbes, A.; Gabe, S.; Gillanders, L.; Holst, M.; et al. ESPEN endorsed recommendations: Definition and classification of intestinal failure in adults. Clin. Nutr. 2015, 34, 171–180. [Google Scholar] [CrossRef] [PubMed]
- O’Hanlon, F.J.; Fragkos, K.C.; Fini, L.; Patel, P.S.; Mehta, S.J.; Rahman, F.; Di Caro, S. Home Parenteral Nutrition in Patients with Advanced Cancer: A Systematic Review and Meta-Analysis. Nutr. Cancer 2020. [Google Scholar] [CrossRef]
- Keane, N.; Fragkos, K.C.; Patel, P.S.; Bertsch, F.; Mehta, S.J.; Di Caro, S.; Rahman, F. Performance status, prognostic scoring, and parenteral nutrition requirements predict survival in patients with advanced cancer receiving home parenteral nutrition. Nutr. Cancer 2018, 70, 73–82. [Google Scholar] [CrossRef]
- Berlana, D.; Almendral, M.A.; Abad, M.R.; Fernández, A.; Torralba, A.; Cervera-Peris, M.; Piñeiro, G.; Romero-Jiménez, R.; Vázquez, A.; Ramírez, E.; et al. Cost, Time, and Error Assessment During Preparation of Parenteral Nutrition: Multichamber Bags Versus Hospital-Compounded Bags. J. Parenter. Enter. Nutr. 2019, 43, 557–565. [Google Scholar] [CrossRef] [PubMed]
- Druml, C.; Ballmer, P.E.; Druml, W.; Oehmichen, F.; Shenkin, A.; Singer, P.; Soeters, P.; Weimann, A.; Bischoff, S.C. ESPEN guideline on ethical aspects of artificial nutrition and hydration. Clin. Nutr. 2016, 35, 545–556. [Google Scholar] [CrossRef]
- Laird, B.J.A.; Fallon, M.; Hjermstad, M.J.; Tuck, S.; Kaasa, S.; Klepstad, P.; McMillan, D.C. Quality of life in patients with advanced cancer: Differential association with performance status and systemic inflammatory response. J. Clin. Oncol. 2016, 34, 2769–2775. [Google Scholar] [CrossRef]
- Aaronson, N.K.; Ahmedzai, S.; Bergman, B.; Bullinger, M.; Cull, A.; Duez, N.J.; Filiberti, A.; Flechtner, H.; Fleishman, S.B.; de Haes, J.C.; et al. The European Organization for Research and Treatment of Cancer QLQ-C30: A quality-of-life instrument for use in international clinical trials in oncology. J. Natl. Cancer Inst. 1993, 85, 365–376. [Google Scholar] [CrossRef]
- Cella, D.F.; Tulsky, D.S.; Gray, G.; Sarafian, B.; Linn, E.; Bonomi, A.; Silberman, M.; Yellen, S.B.; Winicour, P.; Brannon, J.; et al. The Functional Assessment of Cancer Therapy scale: Development and Validation of the General Measure. J. Clin. Oncol. 1993, 11, 570–579. [Google Scholar] [CrossRef]
- Cotogni, P.; De Carli, L.; Passera, R.; Amerio, M.L.; Agnello, E.; Fadda, M.; Ossola, M.; Monge, T.; De Francesco, A.; Bozzetti, F. Longitudinal study of quality of life in advanced cancer patients on home parenteral nutrition. Cancer Med. 2017, 6, 1799–1806. [Google Scholar] [CrossRef]
- Patel, P.S.; Fragkos, K.C.; Keane, N.; Cauldwell, K.; O’Hanlon, F.; Rogers, J.; Obbard, S.; Barragry, J.; Sebepos-Rogers, G.; Neerkin, J.; et al. Clinical and Nutritional Care Pathways of Patients with Malignant Bowel Obstruction: A Retrospective Analysis in a Tertiary UK Center. Nutr. Cancer 2020. [Google Scholar] [CrossRef] [PubMed]
- Frisancho, A.R. Anthropometric Standards. In An Interactive Nutritional Reference of Body Size and Body Composition for Children and Adults; The University of Michigan Press: Ann Arbor, MI, USA, 2008. [Google Scholar]
- Schlüssel, M.M.; dos Anjos, L.A.; de Vasconcellos, M.T.; Kag, G. Reference values of handgrip dynamometry of healthy adults: A population-based study. Clin. Nutr. 2008, 27, 601–607. [Google Scholar] [CrossRef] [PubMed]
- Gurney, J.; Jelliffe, D.B. Arm anthropometry in nutritional assessment: Nomogram for rapid calculation of muscle circumference and cross-sectional muscle and fat areas. Am. J. Clin. Nutr. 1973, 26, 912–915. [Google Scholar] [CrossRef] [PubMed]
- Slee, A.; Ahmed, T.; Storey, L.; Wilkinson, L.; Wilson, G.; Garden, G. The relationship between markers of malnutrition and muscle wasting with frailty and physical function in older care home residents. J. Aging Res. Clin. Pract. 2017, 6, 176–181. [Google Scholar]
- Ottery, F. Definition of standardized nutritional assessment and interventional pathways in oncology. Nutrition 1996, 12 (Suppl. 1), S15–S19. [Google Scholar] [CrossRef]
- Questionnaires-FACIT.org. Available online: https://www.facit.org/FACITOrg/Questionnaires (accessed on 16 July 2019).
- Baxter, J.P.; Fayers, P.M.; Bozzetti, F.; Kelly, D.; Joly, F.; Wanten, G.; Jonkers, C.; Cuerda, C.; Van Gossum, A.; Klek, S.; et al. An international study of the quality of life of adult patients treated with home parenteral nutrition. Clin. Nutr. 2019, 38, 1788–1796. [Google Scholar] [CrossRef]
- Karnofsky, D.A.; Abelmann, W.H.; Craver, L.F.; Burchenal, J.H. The use of the nitrogen mustards in the palliative treatment of carcinoma.With particular reference to broncho-genic carcinoma. Cancer 1948, 1, 634–656. [Google Scholar] [CrossRef]
- Schag, C.C.; Heinrich, R.L.; Ganz, P.A. Karnofsky performance status revisited: Reliability, validity, and guidelines. J. Clin. Oncol. 1984, 2, 187–193. [Google Scholar] [CrossRef]
- Oken, M.M.; Creech, R.H.; Tormey, D.C.; Horton, J.; Davis, T.E.; McFadden, E.T.; Carbone, P.P. Toxicity and response criteria of the eastern cooperative oncology group. Am. J. Clin. Oncol. 1982, 5, 649–655. [Google Scholar] [CrossRef]
- Cohen, J. A coefficient of agreement for nominal scales. Educ. Psychol. Meas. 1960, 20, 37–46. [Google Scholar] [CrossRef]
- Cattell, R.B. The Scientific Use of Factor Analysis in Behavioral and Life Sciences; Plenum: New York, NY, USA, 1978. [Google Scholar]
- Cronbach, L. Coefficient alpha and the internal structure of tests. Psychometrika 1951, 16, 297–334. [Google Scholar] [CrossRef]
- Kaiser, H.F. The application of electronic computers to factor analysis. Educ. Psychol. Meas. 1960, 20, 141–151. [Google Scholar] [CrossRef]
- Cattell, R. The scree test for the number of factors. Multivar. Behav. Res. 1966, 1, 245–276. [Google Scholar] [CrossRef] [PubMed]
- Bailey, K.D. Methods of Social Research, 3rd ed.; Free Press: New York, NY, USA, 1987; p. 533. [Google Scholar]
- Guo, Z.Q.; Yu, J.M.; Li, W.; Fu, Z.M.; Lin, Y.; Shi, Y.Y.; Hu, W.; Ba, Y.; Li, S.Y.; Li, Z.N.; et al. Survey and analysis of the nutritional status in hospitalized patients with malignant gastric tumors and its influence on the quality of life. Support Care Cancer 2020, 28, 373–380. [Google Scholar] [CrossRef] [PubMed]
- Chen, W.; Zhang, Z.; Xiong, M.; Meng, X.; Dai, F.; Fang, J.; Wan, H.; Wang, M. Early enteral nutrition after total gastrectomy for gastric cancer. Asia Pac. J. Clin. Nutr. 2014, 23, 607–611. [Google Scholar]
- El-Ghammaz, A.M.S.; Ben Matoug, R.; Elzimaity, M.; Mostafa, N. Nutritional status of allogeneic hematopoietic stem cell transplantation recipients: Influencing risk factors and impact on survival. Support Care Cancer 2017, 25, 3085–3093. [Google Scholar] [CrossRef]
- Rieger, C.; Wischumerski, I.; Rust, C.; Fiegl, M. Weight Loss and Decrease of Body Mass Index during Allogeneic Stem Cell Transplantation Are Common Events with Limited Clinical Impact. PLoS ONE 2015, 10, e0145445. [Google Scholar] [CrossRef]
- Jager-Wittenaar, H.; Ottery, F.; de Bats, H.; Welink-Lamberts, B.J.; van der Laan, B.; Roodenburg, J.L.N. Diagnostic accuracy of PG-SGA SF, MUST and SNAQ in patients with head and neck cancer. Clin. Nutr. 2016, 35, S103–S104. [Google Scholar] [CrossRef]
- Abbott, J.; Teleni, L.; McKavanagh, D.; Watson, J.; McCarthy, A.L.; Isenring, E. Patient-Generated Subjective Global Assessment Short Form (PG-SGA SF) is a valid screening tool in chemotherapy outpatients. Support Care Cancer 2016, 24, 3883–3887. [Google Scholar] [CrossRef]
- Dewansingh, P.; Euwes, M.; Strijbos, J.; Ottery, F.D.; van der Schans, C.; Jager-Wittenaar, H. Agreement between Patient-Generated Subjective Global Assessment (PG-SGA) and Mini Nutritional Assessment (MNA) in long-stay nursing home residents. Clin. Nutr. 2016, 35, S1–S108. [Google Scholar]
- Wiegert, E.V.M.; De Carvalho Padilha, P.; Peres, W.A.F. Performance of Patient-Generated Subjective Global Assessment (PG-SGA) in Patients With Advanced Cancer in Palliative Care. Nutr. Clin. Pract. 2017, 32, 675–681. [Google Scholar] [CrossRef] [PubMed]
- Ozorio, G.; Barão, K.; Manoukian Forones, N. Cachexia Stage, Patient-Generated Subjective Global Assessment, Phase Angle, and Handgrip Strength in Patients with Gastrointestinal Cancer. Nutr. Cancer 2017, 69, 772–779. [Google Scholar] [CrossRef] [PubMed]
- Lundholm, K.; Daneryd, P.; Bosaeus, I.; Körner, U.; Lindholm, E. Palliative Nutritional Intervention in Addition to Cyclooxygenase and Erythropoietin Treatment for Patients with Malignant Disease: Effects on Survival, Metabolism, and Function: A Randomized Prospective Study. Cancer 2004, 100, 1967–1977. [Google Scholar] [CrossRef]
- Shen, S.; Araujo, J.L.; Altorki, N.K.; Sonett, J.R.; Rodriguez, A.; Sungur-Stasik, K.; Spinelli, C.F.; Neugut, A.I.; Abrams, J.A. Variation by stage in the effects of prediagnosis weight loss on mortality in a prospective cohort of esophageal cancer patients. Dis. Esophagus 2017, 30, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Bozzetti, F.; Migliavacca, S.; Scotti, A.; Bonalumi, M.G.; Scarpa, D.; Baticci, F.; Ammatuna, M.; Pupa, A.; Terno, G.; Sequeira, C.; et al. Impact of cancer, type, site, stage and treatment on the nutritional status of patients. Ann. Surg. 1982, 196, 170–179. [Google Scholar] [CrossRef]
- Senesse, P.; Tadmouri, A.; Culine, S.; Dufour, P.R.; Seys, P.; Radji, A.; Rotarski, M.; Balian, A.; Chambrier, C. A prospective observational study assessing home parenteral nutrition in patients with gastrointestinal cancer: Benefits for quality of life. J. Pain Symptom Manag. 2015, 49, 183–191. [Google Scholar] [CrossRef]
- Mantzorou, M.; Koutelidakis, A.; Theocharis, S.; Giaginis, C. Clinical Value of Nutritional Status in Cancer: What is its Impact and how it Affects Disease Progression and Prognosis? Nutr. Cancer 2017, 69, 1151–1176. [Google Scholar] [CrossRef]
- Alkan, S.; Artaç, M.; Rakıcıoğlu, N. The relationship between nutritional status and handgrip strength in adult cancer patients: A cross-sectional study. Support Care Cancer 2017, 26, 2441–2451. [Google Scholar] [CrossRef]
- Blauwhoff-Buskermolen, S.; Langius, J.A.; Becker, A.; Verheul, H.M.; de van der Schueren, M.A. The influence of different muscle mass measurements on the diagnosis of cancer cachexia. J. Cachexia Sarcopenia Muscle Publ. Online Wiley Online Libr. 2017, 8, 615–622. [Google Scholar] [CrossRef]
- Inácio Pinto, N.; Carnier, J.; Oyama, L.M.; Otoch, J.P.; Alcântara, P.S.; Tokeshi, F.; Nascimento, C.M. Cancer as a Proinflammatory Environment: Metastasis and Cachexia. Mediat. Inflamm. 2015, 2015, 791060. [Google Scholar] [CrossRef]
- Norman, K.; Stobäus, N.; Smoliner, C.; Zocher, D.; Scheufele, R.; Valentini, L.; Lochs, H.; Pirlich, M. Determinants of hand grip strength, knee extension strength and functional status in cancer patients. Clin. Nutr. 2010, 29, 586–591. [Google Scholar] [CrossRef] [PubMed]
- Hu, C.L.; Yu, M.; Yuan, K.T.; Yu, H.L.; Shi, Y.Y.; Yang, J.J.; Li, W.; Jiang, H.P.; Li, Z.N.; Xu, H.X.; et al. Determinants and nutritional assessment value of hand grip strength in patients hospitalized with cancer. Asia Pac. J. Clin. Nutr. 2018, 27, 777–784. [Google Scholar] [PubMed]
- Guerra, R.; Fonseca, I.; Pichel, F.; Restivo, M.; Amaral, T. Handgrip strength and associated factors in hospitalized patients. J. Parenter. Enter. Nutr. 2013, 39, 322–330. [Google Scholar] [CrossRef]
- Ordan, M.A.; Mazza, C.; Barbe, C.; Perrier, M.; Botsen, D.; Renard, Y.; Moreau, J.; Brasseur, M.; Taillière, B.; Bertin, É.; et al. Feasibility of Systematic Handgrip Strength Testing in Digestive Cancer Patients Treated With Chemotherapy: The FIGHTDIGO Study. Cancer 2018, 124, 1501–1506. [Google Scholar] [CrossRef] [PubMed]
- White, J.; Guenter, P.; Jensen, G.; Malone, A.; Schofield, M. Consensus statement: Academy of Nutrition and Dietetics and American Society for Parenteral and Enteral Nutrition: Characteristics recommended for the identification and documentation of adult malnutrition (undernutrition). J. Parenter. Enter. Nutr. 2012, 36, 275–283. [Google Scholar] [CrossRef] [PubMed]
- Aredes, M.A.; Garcez, M.R.; Chaves, G.V. Influence of chemoradiotherapy on nutritional status, functional capacity, quality of life and toxicity of treatment for patients with cervical cancer. Nutr. Diet. 2018, 75, 263–270. [Google Scholar] [CrossRef]
- Humphreys, J.; de la Maza, P.; Hirsch, S.; Barrera, G.; Gattas, V.; Bunout, D. Muscle Strength as a Predictor of Loss of Functional Status in Hospitalized Patients. Nutrition 2002, 18, 616–620. [Google Scholar] [CrossRef]
- Kilgour, R.D.; Vigano, A.; Trutschnigg, B.; Lucar, E.; Borod, M.; Morais, J.A. Handgrip strength predicts survival and is associated with markers of clinical and functional outcomes in advanced cancer patients. Support Care Cancer 2013, 21, 3261–3270. [Google Scholar] [CrossRef]
- Cheng, K.K.; Lee, D.T. Effects of pain, fatigue, insomnia, and mood disturbance on functional status and quality of life of elderly patients with cancer. Crit. Rev. Oncol. Hematol. 2010, 78, 127–137. [Google Scholar] [CrossRef]
- Kenis, C.; Decoster, L.; Bastin, J.; Bode, H.; Van Puyvelde, K.; De Grève, J.; Conings, G.; Fagard, K.; Flamaing, J.; Milisen, K.; et al. Functional decline in older patients with cancer receiving chemotherapy: Amulticenter prospective study. J. Geriatr. Oncol. 2017, 8, 196–205. [Google Scholar] [CrossRef]
- Neo, J.; Fettes, L.; Gao, W.; Higginson, I.J.; Maddocks, M. Disability in activities of daily living among adults with cancer: A systematic review and meta-analysis. Cancer Treat. Rev. 2017, 61, 94–106. [Google Scholar] [CrossRef] [PubMed]
- Arends, J. Struggling with nutrition in patients with advanced cancer: Nutrition and nourishment—focusing on metabolism and supportive care. Ann. Oncol. 2018, 29 (Suppl. 2), ii27–ii34. [Google Scholar] [CrossRef]
- Reis, A.D.; Pereira, P.T.V.T.; Diniz, R.R.; de Castro Filha, J.G.L.; Dos Santos, A.M.; Ramallo, B.T.; Filho, F.A.A.; Navarro, F.; Garcia, J.B.S. Effect of exercise on pain and functional capacity in breast cancer patients. Health Qual. Life Outcomes 2018, 16, 58. [Google Scholar] [CrossRef] [PubMed]
- Ganesh, V.; Agarwal, A.; Popovic, M.; Cella, D.; McDonald, R.; Vuong, S.; Lam, H.; Rowbottom, L.; Chan, S.; Barakat, T.; et al. Comparison of the FACT-C, EORTC QLQ-CR38, and QLQ-CR29 quality of life questionnaires for patients with colorectal cancer: A literature review. Support Care Cancer 2016, 24, 3661–3668. [Google Scholar] [CrossRef] [PubMed]
- Chang, V.T.; Scott, C.B.; Gonzalez, M.L.; Einhorn, J.; Yan, H.; Kasimis, B.S. Patient-Reported Outcomes for Determining Prognostic Groups in Veterans With Advanced Cancer. J. Pain Symptom Manag. 2015, 50, 313–320. [Google Scholar] [CrossRef]
| N (%) | |
|---|---|
| Age (years) | |
| ≤49 | 8 (26.7) |
| 50–64 | 12 (40.0) |
| ≥65 | 10 (33.3) |
| Gender | |
| Female | 13 (43.3) |
| Male | 17 (56.7) |
| Admission present complaint | |
| Chemotherapy related | 3 (10.0) |
| Disease progression | 17 (56.7) |
| Elective admission | 10 (33.3) |
| Type of malignancy * | |
| Gynaecological | 2 (6.7) |
| Upper gastrointestinal | 11 (36.7) |
| Lower gastrointestinal | 4 (13.3) |
| Haematological | 11 (36.7) |
| Other | 2 (6.7) |
| Metastatic disease | |
| No | 16 (53.3) |
| Yes | 14 (46.7) |
| Location of metastases | |
| No Metastases | 16 (53.3) |
| Lower diaphragm | 8 (26.7) |
| Upper diaphragm | 4 (13.3) |
| Both | 2 (6.2) |
| Surgery for malignancy | |
| No | 10 (55.6) |
| Yes | 8 (44.4) |
| Chemotherapy before/during PN | |
| No | 3 (13.6) |
| Yes | 19 (86.44) |
| Radiotherapy before/during PN | |
| No | 8 (66.7) |
| Yes | 4 (33.3) |
| Indication for PN | |
| Extensive small bowel mucosal disease | 12 (40.0%) |
| Intestinal dysmotility | 4 (13.3) |
| Mechanical obstruction | 13 (43.3) |
| Short bowel syndrome or intestinal fistula | 1 (3.3) |
| % weight loss upon starting PN | |
| ≤5% | 8 (30.8) |
| 5–10% | 7 (26.9) |
| 10–15% | 4 (15.4) |
| ≥15% | 7 (26.9) |
| BMI upon starting PN (kg/m2) | |
| BMI ≤ 20.0 | 10 (34.5) |
| BMI > 20.0 | 19 (65.5) |
| Cancer cachexia | |
| No | 9 (30.0) |
| Yes | 21 (70.0) |
| NST score | |
| Low risk | 5 (20.0) |
| Medium risk | 4 (16.0) |
| High risk | 16 (64.0) |
| PG-SGA score | |
| Moderately malnourished | 7 (29.2) |
| Severely malnourished | 17 (70.8) |
| KPS score | |
| <50 | 9 (30.0) |
| 50–100 | 21 (70.0) |
| WHO PS | |
| 1 | 3 (10.0) |
| 2 | 13 (43.3) |
| 3 | 13 (43.3) |
| 4 | 1 (3.3) |
| Referral to palliative care | |
| No | 11 (57.9) |
| Yes | 8 (42.1) |
| Line for PN | |
| PICC | 30 (100.0) |
| N | Mean (SD) | |
|---|---|---|
| Anthropometrics | ||
| Age (years) | 30 | 56.2 (16.4) |
| Usual weight (kg) | 26 | 71.4 (15.8) |
| Height (m) | 29 | 1.7 (0.1) |
| Usual BMI (kg/m2) | 25 | 24.1 (4.6) |
| Weight upon starting PN (kg) | 30 | 60.3 (16.6) |
| Weight loss upon starting PN (%) | 26 | –20.0 (21.9) |
| BMI upon starting PN (kg/m2) | 29 | 21.0 (5.1) |
| HGS on non-dominant Hand (kg) | 27 | 38.2 (21.4) |
| Loss of HGS on non-dominant hand (%) | 27 | −2.7 (43.7) |
| MAC (cm) | 27 | 20.3 (4.1) |
| TSF (mm) | 27 | 12.3 (9.0) |
| MUAMC (cm) | 27 | 24.2 (5.1) |
| Serum Biochemistry | ||
| CRP (mg/L) | 14 | 44.2 (79.2) |
| WCC (×109/L) | 19 | 9.4 (5.0) |
| Albumin (g/L) | 19 | 36.8 (8.0) |
| Haemoglobin (g/L) | 19 | 113.4 (23.7) |
| Sodium (mmol/L) | 19 | 136.5 (5.0) |
| Potassium (mmol/L) | 19 | 4.0 (0.7) |
| Magnesium (mmol/L) | 13 | 0.8 (0.1) |
| Phosphate (mmol/L) | 17 | 0.9 (0.3) |
| Adjusted calcium (mmol/L) | 17 | 2.4 (0.1) |
| Urea | 19 | 5.3 (1.9) |
| Creatinine | 19 | 62.9 (17.0) |
| Nutritional Status | ||
| NST | 25 | 7.0 (4.1) |
| PS-SGA | 25 | 12.4 (5.1) |
| Performance Status | ||
| KPS | 30 | 60.7 (10.5) |
| Quality of Life | ||
| FACT-G | 24 | 26.6 (9.8) |
| Physical well-being | 24 | 11.0 (5.8) |
| Social/family well-being | 24 | 22.8 (5.6) |
| Emotional well-being | 24 | 14.7 (6.2) |
| Functional well-being | 24 | 10.8 (6.6) |
| Length of stay | 29 | 44.0 (24.3) |
| Age (years) | Weight upon Starting PN (kg) | Weight Loss upon Starting PN (%) | BMI upon Starting PN (kg/m2) | HGS | MAC | TSF | MUAMC | NST Score | PG-SGA | KPS | Length of Stay | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Type of Malignancy | ||||||||||||
| Gynaecological | 61.9 (12.6) | 61.4 (7.8) | −11.6 (3.7) | 23.8 (4.3) | 20.7 (7.8) | 21.1 (1.1) | 21.6 (9.3) | 27.8 (1.8) | 8.0 (2.8) | 23.0 (.) | 65.0 (7.1) | 41.0 (18.4) |
| Upper gastrointestinal | 63.3 (12.1) | 48.1 (10.0) | −11.9 (10.3) | 17.22 (4.5) | 32.6 (14.6) | 18.4 (4.4) | 6.8 (5.9) | 20.5 (5.7) | 8.75 (4.6) | 11.1 (3.9) | 58.2 (9.8) | 51.0 (28.8) |
| Lower gastrointestinal | 55.8 (25.2) | 60.7 (12.3) | −9.7 (5.0) | 20.8 (3.1) | 49.2 (23.3) | 20.9 (3.4) | 13.3 (10.2) | 25.0 (2.3) | 8.33 (1.5) | 12.7 (3.2) | 70.0 (8.2) | 35.7 (9.7) |
| Haematological | 48.1 (16.1) | 66.5 (15.6) | −10.4 (13.1) | 23.4 (3.1) | 40.9 (26.4) | 21.5 (4.1) | 15.9 (9.3) | 26.5 (3.9) | 5.6 (4.0) | 12.7 (6.3) | 57.3 (11.0) | 37.6 (19.0) |
| Other | 56.4 (18.9) | 86.2 (22.6) | −1.8 (2.8) | 28.0 (7.6) | 61.8 (.) | 24.3 (.) | 9.5 (.) | 27.3 (.) | 4.0 (5.6) | 11.0 (7.0) | 70.0 (0.0) | 57.0 (52.3) |
| p-value | 0.301 | 0.004 | 0.815 | 0.005 | 0.365 | 0.401 | 0.093 | 0.054 | 0.418 | 0.334 | 0.135 | 0.644 |
| Indication for PN | ||||||||||||
| Extensive small bowel mucosal disease | 56.7 (20.2) | 58.8 (17.6) | −25.0 (27.8) | 20.5 (4.9) | 39.4 (26.9) | 20.8 (4.8) | 13.1 (10.6) | 25.0 (5.2) | 5.3 (4.4) | 11.9 (4.5) | 56.7 (11.5) | 42.6 (21.9) |
| Intestinal dysmotility | 59.5 (12.9) | 64.9 (11.7) | −18.7 (22.0) | 24.0 (3.3) | 38.3 (16.0) | 20.8 (3.8) | 11.7 (8.2) | 24.5 (6.3) | 9.0 (1.4) | 10.7 (2.7) | 60.0 (8.2) | 46.5 (32.4) |
| Mechanical obstruction | 54.9 (15.2) | 60.0 (18.5) | −16.6 (18.1) | 20.7 (5.8) | 34.0 (15.8) | 19.8 (3.0) | 12.6 (8.6) | 23.4 (5.2) | 8.0 (4.1) | 13.9 (6.4) | 63.8 (9.6) | 47.1 (28.1) |
| Small bowel syndrome or intestinal fistula | 54. 4 (.) | 64.0 (.) | 14.1 (.) | 20.7 (.) | 78.8 (.) | 24.4 (.) | 4.1 (.) | 25.7 (.) | 8.0 (.) | 8.0 (.) | 70.0 (.) | 50.0 (.) |
| p-value | 0.970 | 0.936 | 0.841 | 0.695 | 0.260 | 0.732 | 0.836 | 0.906 | 0.423 | 0585 | 0.299 | 0.971 |
| Metastatic Disease | ||||||||||||
| No | 54.3 (17.3) | 64.6 (19.3) | −9.7 (11.7) | 22.8 (5.2) | 37.3 (24.5) | 21.1 (4.4) | 13.8 (9.9) | 25.5 (5.3) | 5.6 (3.7) | 11.9 (5.6) | 57.5 (11.2) | 45.2 (25.6) |
| Yes | 58.3 (15.7) | 55.4 (11.7) | −10.8 (8.3) | 19.2 (4.3) | 39.3 (19.0) | 19.6 (3.7) | 11.0 (8.2) | 23.1 (4.9) | 8.5 (4.2) | 13.9 (5.1) | 64.3 (8.5) | 42.7 (23.7) |
| p-value | 0.517 | 0.130 | 0.774 | 0.055 | 0.814 | 0.341 | 0.428 | 0.228 | 0.080 | 0.599 | 0.076 | 0.789 |
| Cancer Cachexia | ||||||||||||
| No | 47.6 (16.2) | 72.6 (17.3) | 0.3 (3.9) | 24.8 (5.2) | 38.5 (22.8) | 21.2 (5.7) | 18.1 (10.5) | 26.9 (6.7) | 3.9 (3.5) | 14.4 (6.6) | 58.8 (8.3) | 38.6 (26.6) |
| Yes | 59.9 (16.7) | 56.1 (15.2) | −14.9 (8.1) | 19.3 (4.4) | 39.4 (22.4) | 20.2 (3.6) | 10.3 (7.9) | 23.4 (4.2) | 8.2 (4.0) | 12.0 (4.7) | 63.3 (10.8) | 41.4 (21.8) |
| p-value | 0.094 | 0.023 | 0.000 | 0.012 | 0.930 | 0.584 | 0.055 | 0.130 | 0.022 | 0.337 | 0.300 | 0.787 |
| NST | ||||||||||||
| Low risk | 49.7 (23.3) | 69.0 (22.1) | −5.0 (4.3) | 23.0 (5.6) | 57.1 (31.6) | 23.4 (5.5) | 13.1 (9.4) | 27.5 (6.3) | 0.8 (1.1) | 14.8 (3.6) | 64.0 (11.4) | 30.4 (96.6) |
| Medium risk | 44.5 (12.1) | 66.0 (15.5) | −6.1 (8.3) | 22.3 (5.4) | 31.3 (18.1) | 19.1 (3.4) | 20.5 (12.3) | 25.5 (5.1) | 4.7 (1.5) | 17.3 (8.6) | 57.5 (5.0) | 41.3 (25.5) |
| High risk | 58.7 (15.3) | 59.0 (15.5) | −13.1 (8.0) | 20.4 (5.2) | 36.8 (16.7) | 20.5 (3.0) | 11.2 (8.1) | 24.0 (3.8) | 9.5 (2.4) | 10.6 (4.7) | 63.7 (10.2) | 47.6 (26.4) |
| p-value | 0.258 | 0.462 | 0.082 | 0.595 | 0.134 | 0.208 | 0.220 | 0.354 | 0.000 | 0.082 | 0.517 | 0.385 |
| PG-SGA | ||||||||||||
| At risk | 55.4 (15.6) | 61.7 (19.3) | −10.8 (9.6) | 21.0 (5.9) | 38.5 (24.0) | 20.0 (3.0) | 13.3 (10.9) | 24.2 (1.7) | 8.9 (3.6) | 7.3 (0.9) | 62.9 (9.5) | 50.9 (33.6) |
| Severely malnourished | 53.1 (17.6) | 61.2 (17.2) | −10.5 (9.7) | 21.6 (5.0) | 40.9 (22.2) | 21.1 (4.2) | 12.5 (8.1) | 25.0 (5.4) | 5.6 (4.4) | 14.6 (4.8) | 62.0 (9.8) | 35.0 (18.6) |
| p-value | 0.767 | 0.952 | 0.936 | 0.807 | 0.819 | 0.572 | 0.854 | 0.715 | 0.102 | 0.001 | 0.985 | 0.158 |
| KPS | ||||||||||||
| <50 | 58.7 (14.4) | 58.4 (17.2) | −9.3 (14.6) | 21.0 (4.9) | 24.6 (9.2) | 18.9 (3.8) | 11.9 (9.9) | 22.7 (5.8) | 6.4 (3.8) | 13.5 (7.7) | 47.8 (4.4) | 55.5 (26.8) |
| ≥50 | 55.1 (17.4) | 61.1 (16.7) | −10.6 (8.2) | 21.1 (5.3) | 44.1 (22.6) | 20.9 (4.1) | 12.5 (8.8) | 24.9 (4.8) | 7.1 (4.3) | 12.1 (4.4) | 66.2 (6.6) | 39.6 (22.4) |
| p-value | 0.586 | 0.684 | 0.786 | 0.988 | 0.028 | 0.249 | 0.877 | 0.316 | 0.724 | 0.587 | 0.000 | 0.117 |
| WHO-PS | ||||||||||||
| 1 | 52.5 (27.3) | 48.5 (6.9) | −11.2 (5.5) | 17.8 (2.5) | 35.2 (12.0) | 19.3 (2.4) | 15.3 (10.8) | 24.1 (2.3) | 10.7 (4.0) | 12.3 (3.8) | 73.3 (5.7) | 28.0 (7.2) |
| 2 | 58.7 (16.0) | 58.3 (16.7) | −14.5 (10.8) | 20.4 (5.0) | 42.1 (25.0) | 20.7 (4.5) | 11.0 (8.6) | 24.1 (5.2) | 7.5 (4.3) | 11.9 (4.4) | 64.6 (7.8) | 36.3 (22.0) |
| 3 | 52.9 (14.5) | 63.9 (17.6) | −5.0 (8.5) | 22.3 (5.6) | 35.4 (21.1) | 20.1 (4.4) | 13.8 (9.6) | 24.5 (6.1) | 5.2 (3.5) | 13.1 (6.7) | 55.4 (8.7) | 55.9 (25.8) |
| 4 | 77.8 (.) | 75.1 (.) | −7.9 (.) | 21.5 (.) | 33.9 (.) | 21.8 (.) | 4.0 (.) | 23.1 (.) | 8.0 (.) | ∙ | 40.0 (.) | 49.0 (.) |
| p-value | 0.457 | 0.394 | 0.169 | 0.548 | 0.889 | 0.944 | 0.655 | 0.995 | 0.213 | 0.883 | 0.001 | 0.132 |
| FACT-G Subscales | Alpha | Mean (SD) |
| Physical well-being | 0.605 | 11.0 (5.8) |
| Social/Family well-being | 0.818 | 22.8 (5.60 |
| Emotional well-being | 0.567 | 14.7 (6.2) |
| Functional well-being | 0.840 | 10.8 (6.6) |
| HPN-QoL factors | Median (IQR25-IQR75) | |
| Pain | 0.88 | −0.06 (−1.13–0.82) |
| Worrying | 0.80 | 0.17 (−0.91–0.71) |
| Walking/socialising | 0.81 | −0.34 (−0.66–0.60) |
| Energy/independence | 0.84 | −0.10 (−0.63–0.73) |
| Activities | 0.81 | −0.27 (−0.83–0.75) |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Plyta, M.; Patel, P.S.; Fragkos, K.C.; Kumagai, T.; Mehta, S.; Rahman, F.; Di Caro, S. Nutritional Status and Quality of Life in Hospitalised Cancer Patients Who Develop Intestinal Failure and Require Parenteral Nutrition: An Observational Study. Nutrients 2020, 12, 2357. https://doi.org/10.3390/nu12082357
Plyta M, Patel PS, Fragkos KC, Kumagai T, Mehta S, Rahman F, Di Caro S. Nutritional Status and Quality of Life in Hospitalised Cancer Patients Who Develop Intestinal Failure and Require Parenteral Nutrition: An Observational Study. Nutrients. 2020; 12(8):2357. https://doi.org/10.3390/nu12082357
Chicago/Turabian StylePlyta, Marina, Pinal S. Patel, Konstantinos C. Fragkos, Tomoko Kumagai, Shameer Mehta, Farooq Rahman, and Simona Di Caro. 2020. "Nutritional Status and Quality of Life in Hospitalised Cancer Patients Who Develop Intestinal Failure and Require Parenteral Nutrition: An Observational Study" Nutrients 12, no. 8: 2357. https://doi.org/10.3390/nu12082357
APA StylePlyta, M., Patel, P. S., Fragkos, K. C., Kumagai, T., Mehta, S., Rahman, F., & Di Caro, S. (2020). Nutritional Status and Quality of Life in Hospitalised Cancer Patients Who Develop Intestinal Failure and Require Parenteral Nutrition: An Observational Study. Nutrients, 12(8), 2357. https://doi.org/10.3390/nu12082357






