Impact of a Ketogenic Diet on Metabolic Parameters in Patients with Obesity or Overweight and with or without Type 2 Diabetes: A Meta-Analysis of Randomized Controlled Trials
Abstract
1. Introduction
2. Materials and Methods
2.1. Data Sources
2.2. Study Selection and Data Collection
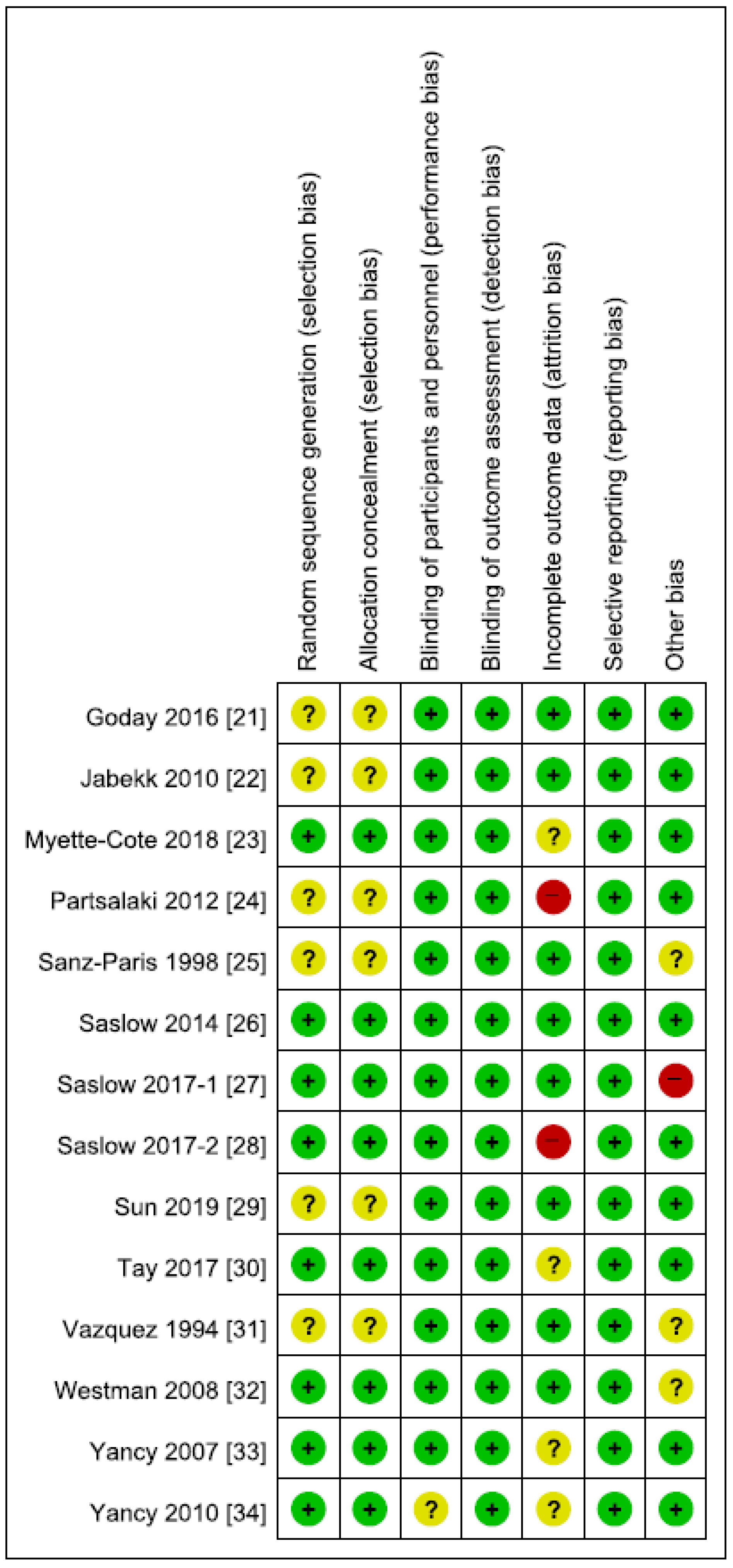
2.3. Risk of Bias and Quality Assessment of Evidence
2.4. Data Analysis and Statistical Methods
3. Results
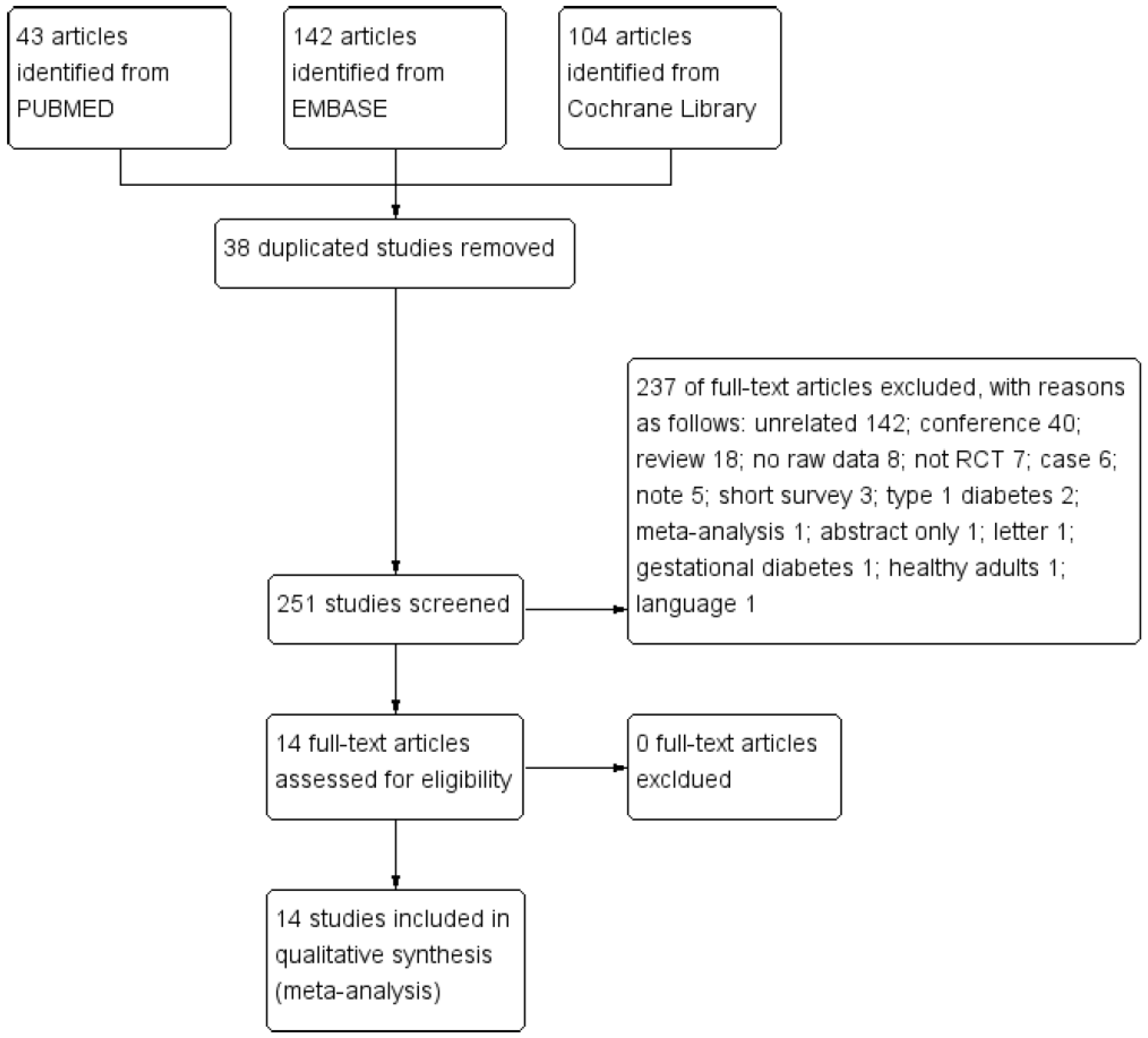
3.1. Selection of Relevant Studies
3.2. Study Characteristics
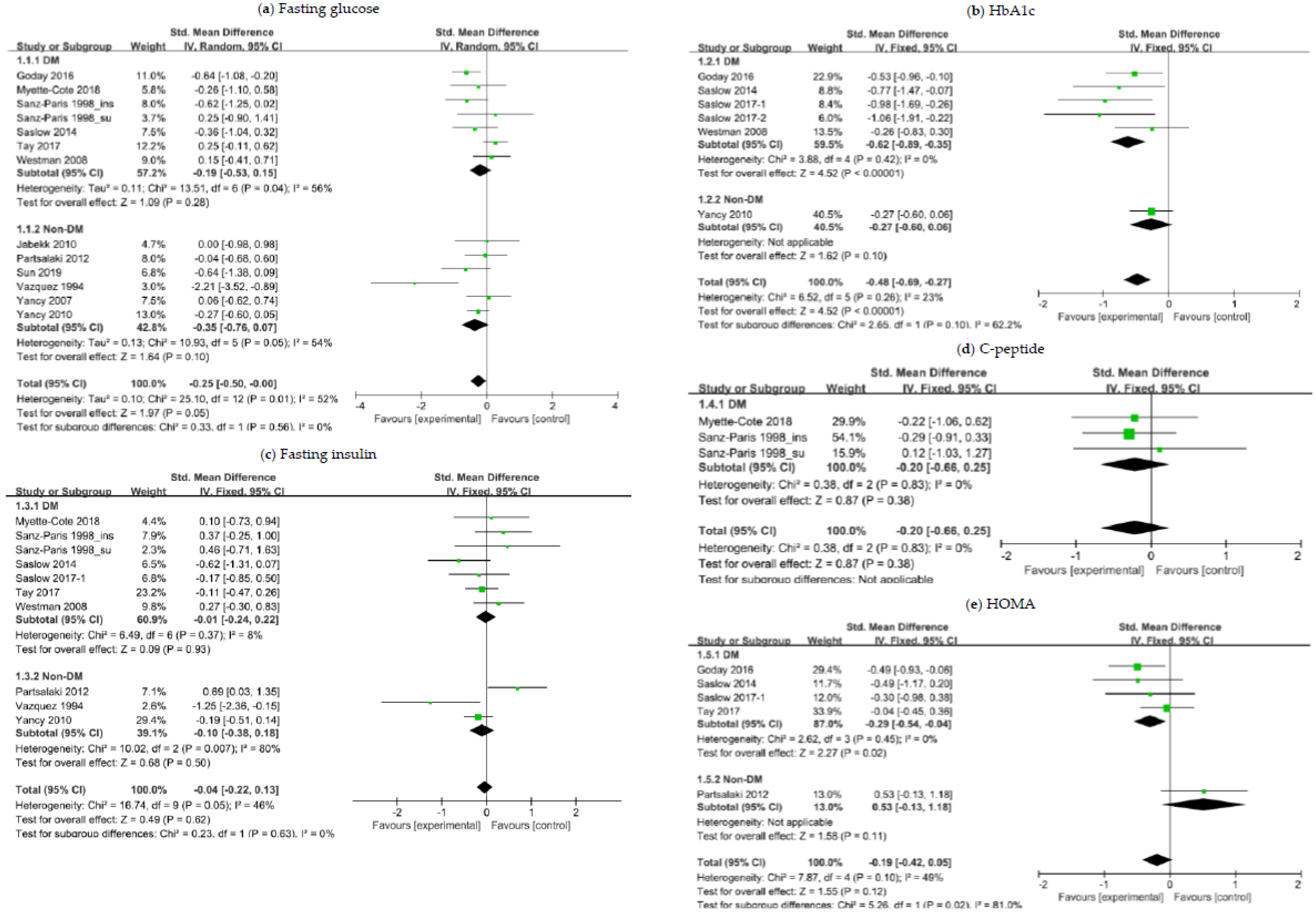
3.3. The Effects of a Ketogenic Diet on Glycemic Control
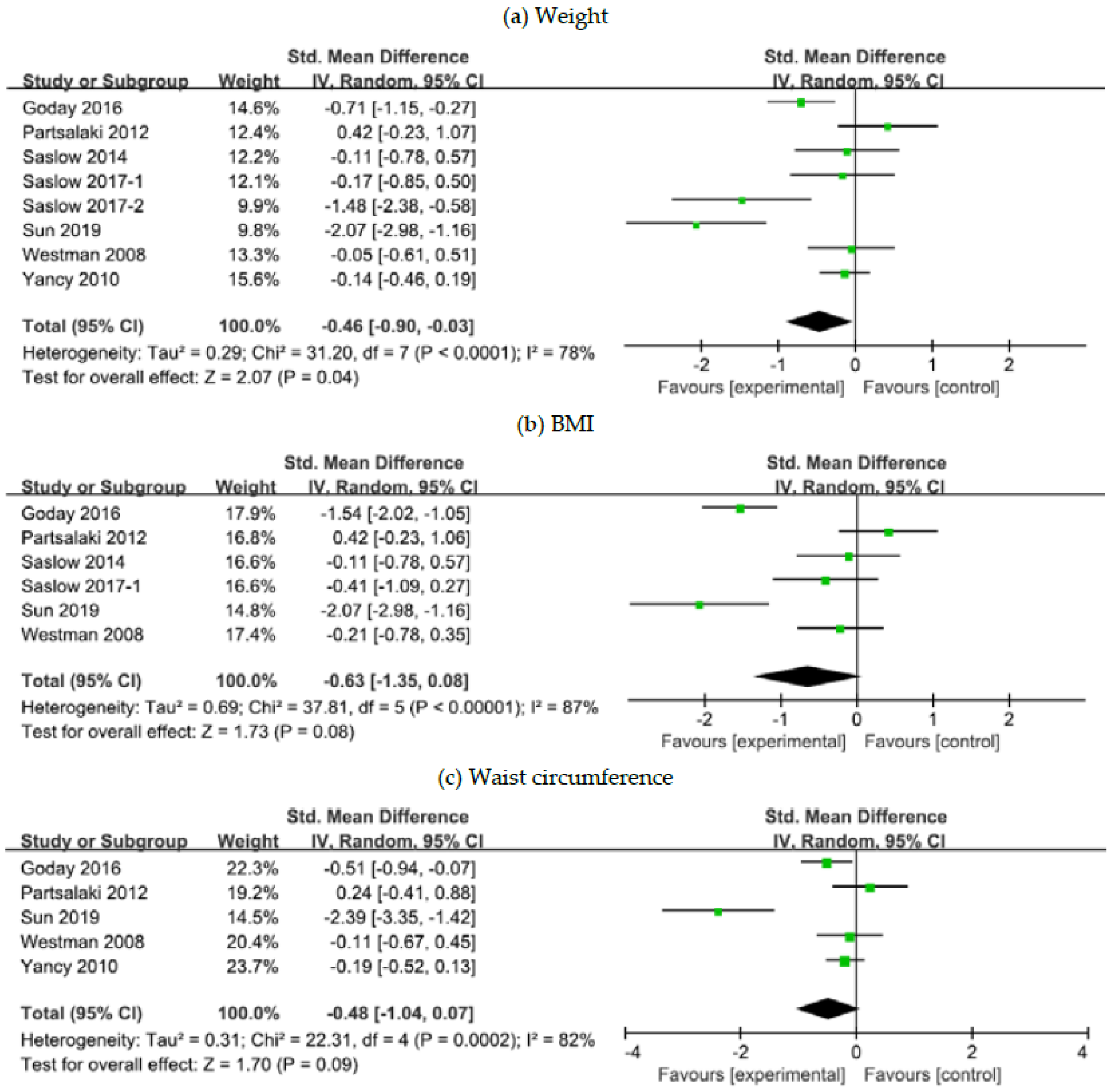
3.4. The Effects of a Ketogenic Diet on Weight Control
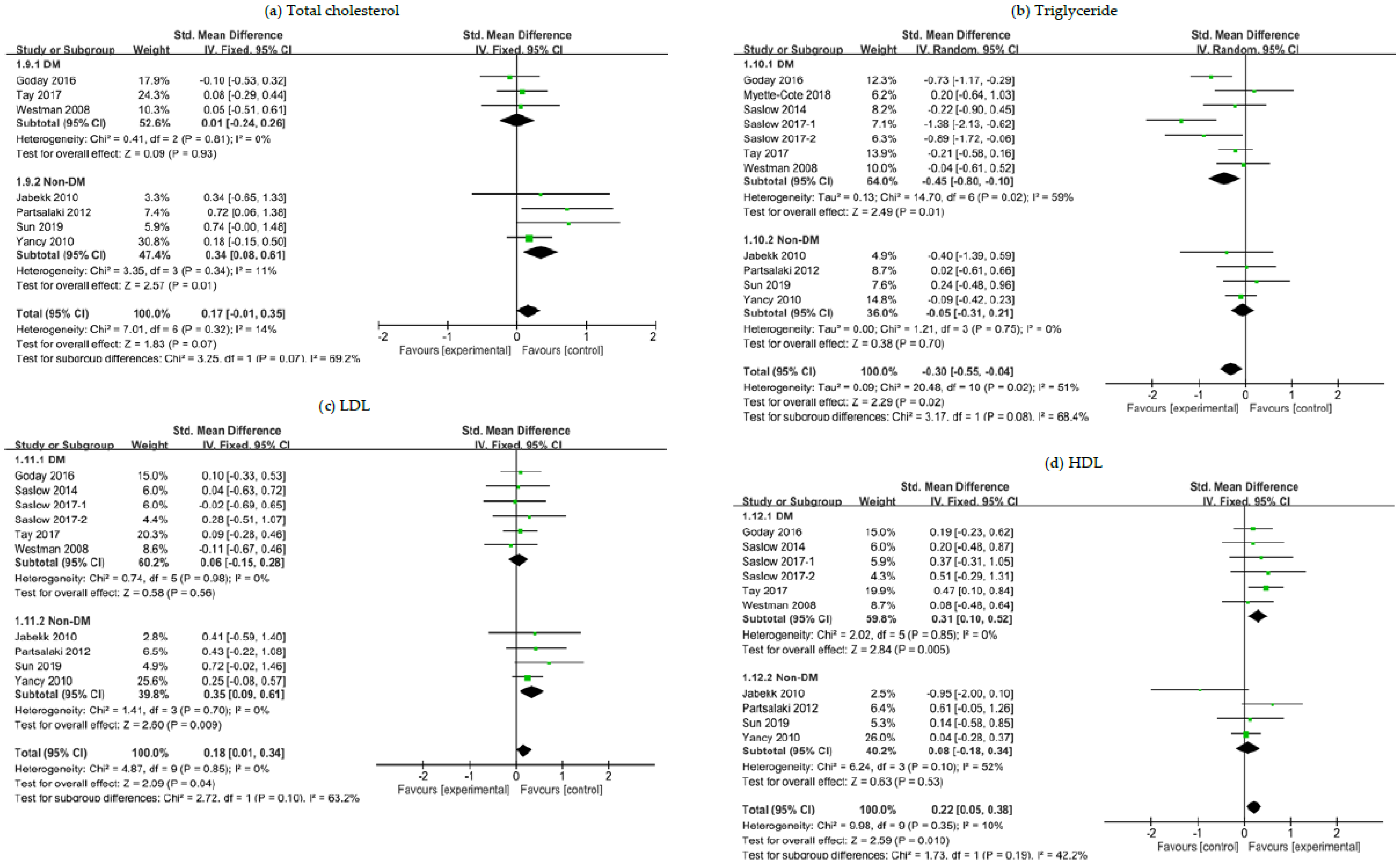
3.5. The Effects of a Ketogenic Diet on Lipid Panel
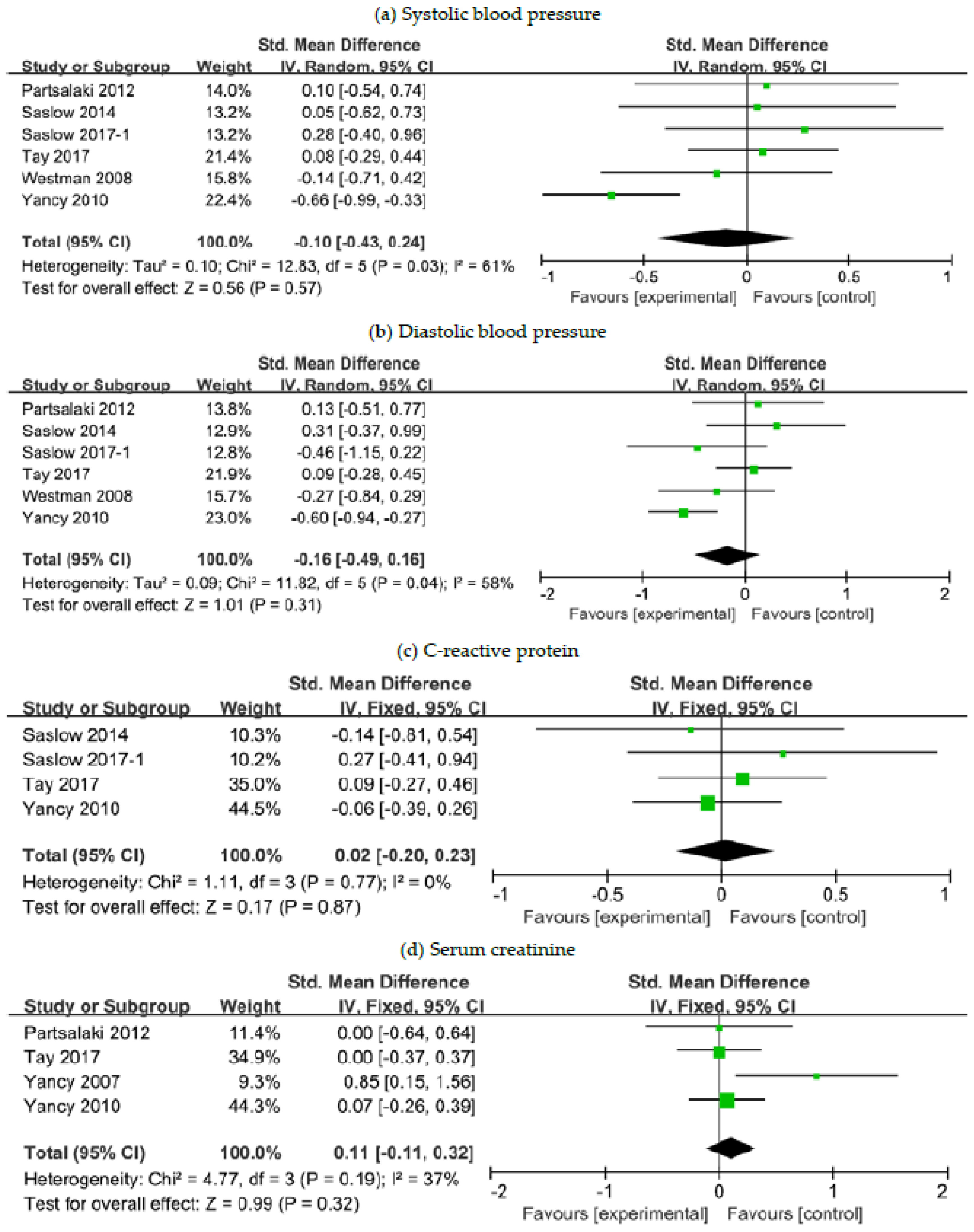
3.6. The Effects of a Ketogenic Diet on Other Risk Markers
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Pi-Sunyer, X. The medical risks of obesity. Postgrad Med. 2009, 121, 21–33. [Google Scholar] [CrossRef] [PubMed]
- Hruby, A.; Hu, F.B. The epidemiology of obesity: A big picture. Pharmacoeconomics 2015, 33, 673–689. [Google Scholar] [CrossRef] [PubMed]
- Sahoo, K.; Sahoo, B.; Choudhury, A.K.; Sofi, N.Y.; Kumar, R.; Bhadoria, A.S. Childhood obesity: Causes and consequences. J. Fam. Med. Prim. Care 2015, 4, 187–192. [Google Scholar] [CrossRef]
- Yumuk, V.; Tsigos, C.; Fried, M.; Schindler, K.; Busetto, L.; Micic, D.; Toplak, H. Obesity management task force of the european association for the study of obesity. European guidelines for obesity management in adults. Obes. Facts 2015, 8, 402–424. [Google Scholar] [CrossRef] [PubMed]
- Strychar, I. Diet in the management of weight loss. CMAJ 2006, 174, 56–63. [Google Scholar] [CrossRef] [PubMed]
- Hall, K.D.; Kahan, S. Maintenance of lost weight and long-term management of obesity. Med. Clin. N. Am. 2018, 102, 183–197. [Google Scholar] [CrossRef]
- Bough, K.J.; Rho, J.M. Anticonvulsant mechanisms of the ketogenic diet. Epilepsia 2007, 48, 43–58. [Google Scholar] [CrossRef]
- Lefevre, F.; Aronson, N. Ketogenic diet for the treatment of refractory epilepsy in children: A systematic review of efficacy. Pediatrics 2000, 105, e46. [Google Scholar] [CrossRef]
- Kossoff, E.H.; Zupec-Kania, B.A.; Auvin, S.; Ballaban-Gil, K.R.; Bergqvist, A.G.C.; Blackford, R.; Buchhalter, J.R.; Caraballo, R.H.; Cross, J.H.; Dahlin, M.G.; et al. Optimal clinical management of children receiving dietary therapies for epilepsy: Updated recommendations of the International Ketogenic Diet Study Group. Epilepsia Open 2018, 3, 175–192. [Google Scholar] [CrossRef]
- Yudkoff, M.; Daikhin, Y.; Melo, T.M.; Nissim, I.; Sonnewald, U.; Nissim, I. The ketogenic diet and brain metabolism of amino acids: Relationship to the anticonvulsant effect. Annu. Rev. Nutr. 2007, 27, 415–430. [Google Scholar] [CrossRef]
- Mazur, A. Why were "starvation diets" promoted for diabetes in the pre-insulin period? Nutr. J. 2011, 10, 23. [Google Scholar] [CrossRef] [PubMed]
- Bolla, A.M.; Caretto, A.; Laurenzi, A.; Scavini, M.; Piemonti, L. Low-carb and ketogenic diets in type 1 and type 2 diabetes. Nutrients 2019, 11, 962. [Google Scholar] [CrossRef] [PubMed]
- Osler, W.; McCrae, T. Diabetes mellitus. In The Principles and Practice of Medicine; Appleton and Co.: New York, NY, USA, 1923; Volume 1, pp. 421–433. [Google Scholar]
- Allen, F.M.; Stillman, E.; Fitz, R. Total Dietary Regulation in the Treatment of Diabetes: Monographs of the Rockefeller Institute for Medical Research; No. 11.; Rockefeller Institute: New York, NY, USA, 1919. [Google Scholar]
- Gershuni, V.; Yan, S.; Medici, V. Nutritional ketosis for weight management and reversal of metabolic syndrome. Curr. Nutr. Rep. 2018, 7, 97–106. [Google Scholar] [CrossRef] [PubMed]
- Dashti, H.; Mathhew, T.; Hussein, T.; Asfar, S.K.; Behbahani, A.; Khoursheed, M.A.; Al-Sayer, H.M.; Bo-Abbas, Y.Y.; Al-Zaid, N.S. Long-term effects of a ketogenic diet in obese patients. Exp. Clin. Cardiol. 2004, 9, 200–205. [Google Scholar]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef] [PubMed]
- Shamseer, L.; Moher, D.; Clarke, M.; Ghersi, D.; Liberati, A.; Petticrew, M.; Shekelle, P.; Stewart, L.A.; PRISMA-P Group. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015: Elaboration and explanation. BMJ 2015, 350, g7647. [Google Scholar] [CrossRef] [PubMed]
- Atkins, D.; Best, D.; Briss, P.A.; Eccles, M.; Falck-Ytter, Y.; Flottorp, S.; Guyatt, G.H.; Harbour, R.T.; Haugh, M.C.; Henry, D.; et al. Grading quality of evidence and strength of recommendations. BMJ 2004, 328, 1490. [Google Scholar] [CrossRef] [PubMed]
- Guyatt, G.H.; Oxman, A.D.; Vist, G.E.; Kunz, R.; Falck-Ytter, Y.; Alonso-Coello, P.; Schünemann, H.J.; GRADE Working Group. GRADE: An emerging consensus on rating quality of evidence and strength of recommendations. BMJ 2008, 336, 924–926. [Google Scholar] [CrossRef]
- Goday, A.; Bellido, D.; Sajoux, I.; Crujeiras, A.B.; Burguera, B.; García-Luna, P.P.; Oleaga, A.; Moreno, B.; Casanueva, F.F. Short-term safety, tolerability and efficacy of a very low-calorie-ketogenic diet interventional weight loss program versus hypocaloric diet in patients with type 2 diabetes mellitus. Nutr. Diabetes 2016, 6, e230. [Google Scholar] [CrossRef]
- Jabekk, P.; Moe, I.; Meen, H.; Tomten, S.; Hostmark, A. Resistance training in overweight women on a ketogenic diet conserved lean body mass while reducing body fat. Nutr. Metab. 2010, 7, 17. [Google Scholar] [CrossRef]
- Myette-Cote, E.; Durrer, C.; Neudorf, H.; Bammert, T.D.; Botezelli, J.D.; Johnson, J.D.; DeSouza, C.A.; Little, J.P. The effect of a short-term low-carbohydrate, high-fat diet with or without postmeal walks on glycemic control and inflammation in type 2 diabetes: A randomized trial. Am. J. Physiol. Regul. Integr. Comp. Physiol. 2018, 315, R1210–R1219. [Google Scholar] [CrossRef] [PubMed]
- Partsalaki, I.; Karvela, A.; Spiliotis, B. Metabolic impact of a ketogenic diet compared to a hypocaloric diet in obese children and adolescents. J. Pediatr. Endocrinol. Metab. 2012, 25, 697–704. [Google Scholar] [CrossRef] [PubMed]
- Sanz-Paris, A.; Calvo, L.; Guallard, A.; Salazar, I.; Albero, R. High-fat versus high-carbohydrate enteral formulae: Effect on blood glucose, C-peptide, and ketones in patients with type 2 diabetes treated with insulin or sulfonylurea. Nutrition 1998, 14, 840–845. [Google Scholar] [CrossRef]
- Saslow, L.R.; Kim, S.; Daubenmier, J.J.; Moskowitz, J.T.; Phinney, S.D.; Goldman, V.; Murphy, E.J.; Cox, R.M.; Moran, P.; Hecht, F.M. A randomized pilot trial of a moderate carbohydrate diet compared to a very low carbohydrate diet in overweight or obese individuals with type 2 diabetes mellitus or prediabetes. PLoS ONE 2014, 9, e91027. [Google Scholar] [CrossRef] [PubMed]
- Saslow, L.R.; Daubenmier, J.J.; Moskowitz, J.T.; Kim, S.; Murphy, E.J.; Phinney, S.D.; Ploutz-Snyder, R.; Goldman, V.; Cox, R.M.; Mason, A.E.; et al. Twelve-month outcomes of a randomized trial of a moderate-carbohydrate versus very low-carbohydrate diet in overweight adults with type 2 diabetes mellitus or prediabetes. Nutr. Diabetes 2017, 7, 304. [Google Scholar] [CrossRef]
- Saslow, L.R.; Mason, A.E.; Kim, S.; Goldman, V.; Ploutz-Snyder, R.; Bayandorian, H.; Daubenmier, J.; Hecht, F.M.; Moskowitz, J.T. An online intervention comparing a very low-carbohydrate ketogenic diet and lifestyle recommendations versus a plate method diet in overweight individuals with type 2 diabetes: A randomized controlled trial. J. Med. Internet Res. 2017, 19, e36. [Google Scholar] [CrossRef]
- Sun, S.; Kong, Z.; Shi, Q.; Hu, M.; Zhang, H.; Zhang, D.; Nie, J. Non-energy-restricted low-carbohydrate diet combined with exercise intervention improved cardiometabolic health in overweight Chinese females. Nutrients 2019, 11, 3051. [Google Scholar] [CrossRef]
- Tay, J.; Thompson, C.H.; Luscombe-Marsh, N.D.; Wycherley, T.P.; Noakes, M.; Buckley, J.D.; Wittert, G.A.; Yancy, W.S., Jr.; Brinkworth, G.D. Effects of an energy-restricted low-carbohydrate, high unsaturated fat/low saturated fat diet versus a high-carbohydrate, low-fat diet in type 2 diabetes: A 2-year randomized clinical trial. Diabetes Obes. Metab. 2018, 20, 858–871. [Google Scholar] [CrossRef]
- Vazquez, J.; Kazi, U. Lipolysis and gluconeogenesis from glycerol during weight reduction with very-low-calorie diets. Metabolism 1994, 43, 1293–1299. [Google Scholar] [CrossRef]
- Westman, E.C.; Yancy, W.S., Jr.; Mavropoulos, J.C.; Marquart, M.; McDuffie, J.R. The effect of a low-carbohydrate, ketogenic diet versus a low-glycemic index diet on glycemic control in type 2 diabetes mellitus. Nutr. Metab. 2008, 5, 36. [Google Scholar] [CrossRef]
- Yancy, W.S., Jr.; Olsen, M.K.; Dudley, T.; Westman, E.C. Acid-base analysis of individuals following two weight loss diets. Eur. J. Clin. Nutr. 2007, 61, 1416–1422. [Google Scholar] [CrossRef] [PubMed]
- Yancy, W.; Westman, E.; McDuffie, J.; Grambow, S.C.; Jeffreys, A.S.; Bolton, J.; Chalecki, A.; Oddone, E.Z. A randomized trial of a low-carbohydrate diet vs orlistat plus a low-fat diet for weight loss. Arch. Intern. Med. 2010, 170, 136–145. [Google Scholar] [CrossRef] [PubMed]
- Seagle, H.M.; Strain, G.W.; Makris, A.; Reeves, R.S.; American Dietetic Association. Position of the American Dietetic Association: Weight management. J. Am. Diet. Assoc. 2009, 109, 330–346. [Google Scholar] [CrossRef] [PubMed]
- Madeo, F.; Carmona-Gutierrez, D.; Hofer, S.J.; Kroemer, G. Caloric restriction mimetics against age-associated disease: Targets, mechanisms, and therapeutic potential. Cell Metab. 2019, 29, 592–610. [Google Scholar] [CrossRef]
- Most, J.; Tosti, V.; Redman, L.M.; Fontana, L. Calorie restriction in humans: An update. Ageing Res. Rev. 2017, 39, 36–45. [Google Scholar] [CrossRef]
- Stekovic, S.; Hofer, S.J.; Tripolt, N.; Aon, M.A.; Royer, P.; Pein, L.; Stadler, J.T.; Pendl, T.; Prietl, B.; Url, J.; et al. Alternate day fasting improves physiological and molecular markers of aging in healthy, non-obese humans. Cell Metab. 2019, 30, 462–476.e6. [Google Scholar] [CrossRef]
- Mattson, M.P.; Longo, V.D.; Harvie, M. Impact of intermittent fasting on health and disease processes. Ageing Res. Rev. 2017, 39, 46–58. [Google Scholar] [CrossRef]
- Carroll, J.; Koenigsberger, D. The ketogenic diet. J. Am. Diet. Assoc. 1998, 98, 316–321. [Google Scholar] [CrossRef]
- Chianese, R.; Coccurello, R.; Viggiano, A.; Scafuro, M.; Fiore, M.; Coppola, G.; Operto, F.F.; Fasano, S.; Laye, S.; Pierantoni, R.; et al. Impact of dietary fats on brain functions. Curr. Neuropharmacol. 2018, 16, 1059–1085. [Google Scholar] [CrossRef]
- Wlodarek, D. Role of ketogenic diets in neurodegenerative diseases (Alzheimer’s disease and Parkinson’s disease). Nutrients 2019, 11, 169. [Google Scholar] [CrossRef]
- Rusek, M.; Pluta, R.; Ulamek-Koziol, M.; Czuczwar, S.J. Ketogenic diet in Alzheimer’s disease. Int. J. Mol. Sci. 2019, 20, 3892. [Google Scholar] [CrossRef] [PubMed]
- Brouns, F. Overweight and diabetes prevention: Is a low-carbohydrate-high-fat diet recommendable? Eur. J. Nutr. 2018, 57, 1301–1312. [Google Scholar] [CrossRef] [PubMed]
- Johnstone, A.; Horgan, G.; Murison, S.; Bremner, D.; Lobley, G. Effects of a high-protein ketogenic diet on hunger, appetite, and weight loss in obese men feeding ad libitum. Am. J. Clin. Nutr. 2008, 87, 44–55. [Google Scholar] [CrossRef] [PubMed]
- Bueno, N.B.; de Melo, I.S.; de Oliveira, S.L.; da Rocha Ataide, T. Very-low-carbohydrate ketogenic diet v. low-fat diet for long-term weight loss: A meta-analysis of randomised controlled trials. Br. J. Nutr. 2013, 110, 1178–1187. [Google Scholar] [CrossRef]
- Kang, X.; Wang, C.; Lifang, L.; Chen, D.; Yang, Y.; Liu, G.; Wen, H.; Chen, L.; He, L.; Li, X.; et al. Effects of different proportion of carbohydrate in breakfast on postprandial glucose excursion in normal glucose tolerance and impaired glucose regulation subjects. Diabetes Technol. Ther. 2013, 15, 569–574. [Google Scholar] [CrossRef]
- Ye, J. Mechanisms of insulin resistance in obesity. Front. Med. 2013, 7, 14–24. [Google Scholar] [CrossRef]
- Vidal, J. Updated review on the benefits of weight loss. Int. J. Obes. Metab. Disord. 2002, 26, S25–S28. [Google Scholar] [CrossRef]
- Sainsbury, E.; Kizirian, N.V.; Partridge, S.R.; Gill, T.; Colagiuri, S.; Gibson, A.A. Effect of dietary carbohydrate restriction on glycemic control in adults with diabetes: A systematic review and meta-analysis. Diabetes Res. Clin. Pract. 2018, 139, 239–252. [Google Scholar] [CrossRef]
- American Diabetes Association. 5. Lifestyle management: Standards of medical care in diabetes-2019. Diabetes Care 2019, 42, S46–S60. [Google Scholar] [CrossRef]
- Hallberg, S.J.; McKenzie, A.L.; Williams, P.T.; Bhanpuri, N.H.; Peters, A.L.; Campbell, W.W.; Hazbun, T.L.; Volk, B.M.; McCarter, J.P.; Phinney, S.D.; et al. Effectiveness and safety of a novel care model for the management of type 2 diabetes at 1 year: An open-label, non-randomized, controlled study. Diabetes Ther. 2018, 9, 583–612. [Google Scholar] [CrossRef]
- Klop, B.; Elte, J.W.; Cabezas, M.C. Dyslipidemia in obesity: Mechanisms and potential targets. Nutrients 2013, 5, 1218–1240. [Google Scholar] [CrossRef] [PubMed]
- McLaughlin, T.; Abbasi, F.; Cheal, K.; Chu, J.; Lamendola, C.; Reaven, G. Use of metabolic markers to identify overweight individuals who are insulin resistant. Ann. Intern. Med. 2003, 139, 802–809. [Google Scholar] [CrossRef] [PubMed]
- Bitzur, R.; Cohen, H.; Kamari, Y.; Shaish, A.; Harats, D. Triglycerides and HDL cholesterol: Stars or second leads in diabetes? Diabetes Care 2009, 32, S373–S377. [Google Scholar] [CrossRef] [PubMed]
- Hession, M.; Rolland, C.; Kulkarni, U.; Wise, A.; Broom, J. Systematic review of randomized controlled trials of low-carbohydrate vs. low-fat/low-calorie diets in the management of obesity and its comorbidities. Obes. Rev. 2009, 10, 36–50. [Google Scholar] [CrossRef]
- Nordmann, A.; Nordmann, A.; Briel, M.; Keller, U.; Yancy, W.S., Jr.; Brehm, B.J.; Bucher, H.C. Effects of low-carbohydrate vs low-fat diets on weight loss and cardiovascular risk factors: A meta-analysis of randomized controlled trials. Arch. Intern. Med. 2006, 166, 285–293. [Google Scholar] [CrossRef]
- Accurso, A.; Bernstein, R.K.; Dahlqvist, A.; Draznin, B.; Feinman, R.D.; Fine, E.J.; Gleed, A.; Jacobs, D.B.; Larson, G.; Lustig, R.H.; et al. Dietary carbohydrate restriction in type 2 diabetes mellitus and metabolic syndrome: Time for a critical appraisal. Nutr. Metab. 2008, 5, 9. [Google Scholar] [CrossRef]
- Westman, E.C.; Yancy, W.S., Jr.; Olsen, M.K.; Dudley, T.; Guyton, J.R. Effect of a low-carbohydrate, ketogenic diet program compared to a low-fat diet on fasting lipoprotein subclasses. Int. J. Cardiol. 2006, 110, 212–216. [Google Scholar] [CrossRef]
- Wojciechowska, J.; Krajewski, W.; Bolanowski, M.; Krecicki, T.; Zatonski, T. Diabetes and cancer: A review of current knowledge. Exp. Clin. Endocrinol. Diabetes 2016, 124, 263–275. [Google Scholar] [CrossRef]
- Klement, R.J. Beneficial effects of ketogenic diets for cancer patients: A realist review with focus on evidence and confirmation. Med. Oncol. 2017, 34, 132. [Google Scholar] [CrossRef]
- Tan-Shalaby, J. Ketogenic diets and cancer: Emerging evidence. Fed. Pract. 2017, 34, 37S–42S. [Google Scholar]
| Study (Country) | Trial Design | Intervention Duration | Diet | N | Age, Mean ± SD (Years) | Female, N (%) | FG, Mean ± SD (mg/dL) | BMI, Mean ± SD (kg/m2) | Baseline T2DM | Inclusion Criteria |
|---|---|---|---|---|---|---|---|---|---|---|
| Goday 2016 [21] (Spain) | Prospective, open-label, multi-centric, parallel group randomized controlled trial | 4 months | I: very low-calorie-ketogenic diet | 45 | 54.89 ± 8.81 | 30 (66.6) | 136.87 ± 34.43 | 33.25 ± 1.52 | Yes | Age: 30–65 years; BMI: 30–35 kg/m2 |
| C: low-calorie diet | 44 | 54.17 ± 7.97 | 28 (63.6) | 142.81 ± 44.26 | 32.88 ± 1.60 | |||||
| Jabekk 2010 [22] (Norway) | Randomized controlled trial | 10 weeks | I: low carbohydrate, ketogenic diet | 8 | - | 8 (100) | 88.2 ± 5.4 | 32.9 ± 4.5 | No | Age: 20–40 years; BMI: ≥25 kg/m2 |
| C: regular diet | 8 | - | 8 (100) | 90.0 ± 5.4 | 31.7 ± 4.2 | |||||
| Myette-Cote 2018 [23] (Canada) | Randomized controlled crossover trial | 4 days | I: low-carbohydrate high-fat diet | 11 | 64 ± 8 | 7 (63.6) | 151.2 ± 34.2 | 34.0 ± 8.0 | Yes | HbA1c >6.5% or FG >7.0 mmol/L or 2-h OGTT >11.1 mmol/L |
| C: low-fat low-glycemic index guidelines diet | 149.4 ± 37.8 | |||||||||
| Partsalaki 2012 [24] (Greece) | Randomized controlled trial | 6 months | I: ketogenic diet | 21 | 12.8 ± 2.1 | 11 (52.4) | 84.3 ± 9.8 | 30.0 ± 4.3 | No | Age: 8–18 years; BMI: >95th percentile for gender and age |
| C: hypocaloric diet | 17 | 12.7 ± 2.8 | 10 (58.8) | 80.2 ± 17.6 | 28.1 ± 3.1 | |||||
| Sanz-Paris 1998 [25] (Spain) | Randomized controlled trial | 120 min | I: low-carbohydrate, high-fat formulation | 27 | 65 ± 7 | 33 (64) | 185 ± 56 | 29.2 ± 2.7 | Yes | Age: 45–72 years; good glycemic control (mean HbA1c: 6.5 ± 0.9%) |
| C: high-carbohydrate, low-fat formulation | 25 | 170 ± 48 | ||||||||
| Saslow 2014 [26] (US) | Single site, parallel group, balanced randomization (1:1) trial | 3 months | I: low-carbohydrate ketogenic diet | 16 | 64.8 ± 7.7 | 9 (56.3) | 124.4 ± 28.3 | 36.2 ± 8.2 | Yes(including prediabetes) | Age: ≥18 years;BMI: ≥25 kg/m2; HbA1c: ≥6.5% (T2DM) or >6% (prediabetes) |
| C: moderate-carbohydrate, calorie-restricted, low-fat diet | 18 | 55.1 ± 13.5 | 16 (88.9) | 140.6 ± 34.3 | 37.4 ± 6.4 | |||||
| Saslow 2017-1 [27] (US) | Single site, parallel group, balanced randomization (1:1) trial | 12 months | I: low-carbohydrate ketogenic diet | 16 | 64.8 ± 7.7 | 9 (56.3) | - | 36.2 ± 8.2 | Yes(including prediabetes) | Age: ≥18 years; BMI: ≥25 kg/m2; HbA1c: ≥6.5% (T2DM) or >6% (prediabetes) |
| C: moderate-carbohydrate, calorie-restricted, low-fat diet | 18 | 55.1 ± 13.5 | 16 (88.9) | - | 37.4 ± 6.4 | |||||
| Saslow 2017-2 [28] (US) | Parallel-group, balanced randomization (1:1) trial | 32 weeks | I: very low-carbohydrate ketogenic diet | 12 | 53.0 ± 10.2 | 6 (50) | - | - | Yes | Age: ≥18 years; BMI: ≥25 kg/m2; HbA1c: ≥6.5–9% |
| C: American Diabetes Associations’ “Create Your Plate” diet | 13 | 58.2 ± 6.7 | 9 (69) | - | - | |||||
| Sun 2019 [29] (China) | Randomized controlled trial | 4 weeks | I: low-carbohydrate, ketogenic diet | 18 | 20.9 ± 3.7 | 18 (100) | 84.6 ± 7.2 | 25.0 ± 2.9 | No | Age: 18–30 years; BMI: ≥23 kg/m2; past 6-month weight variation: <2kg; sedentary lifestyle |
| C: normal diet | 17 | 21.6 ± 3.9 | 17 (100) | 82.8 ± 9.0 | 24.8 ± 3.2 | |||||
| Tay 2017 [30] (Australia) | Single-center, parallel-groups, randomized controlled trial | 2 years | I: low-carbohydrate, high-unsaturated/low-saturated fat diet | 58 | 58 ± 7.6 | 21 (36) | 140.4 ± 37.8 | 34.2 ± 4.2 | Yes | Age: 35–68 years; BMI: 26–45 kg/m2; HbA1c: 7.0% or antidiabetic treatment |
| C: high-carbohydrate, low-fat diet | 57 | 58 ± 7.5 | 28 (49) | 151.2 ± 41.4 | 35.1 ± 4.1 | |||||
| Vazquez 1994 [31] (US) | Randomized controlled trial | 28 days | I: ketogenic diet | 8 | 48 ± 3 | 8 (100) | 86.4 ± 5.4 | 41 ± 5 | No | BMI: 35 kg/m2 |
| C: nonketogenic very-low-calorie diet | 8 | 44 ± 5 | 8 (100) | 88.2 ± 7.2 | 37 ± 6 | |||||
| Westman 2008 [32] (US) | Randomized controlled trial | 24 weeks | I: low-carbohydrate, ketogenic diet | 38 | 51.8 ± 7.3 | 29 (76.3) | 178.1 ± 72.9 | 37.7 ± 6.1 | Yes | Age: 18–65 years; BMI: 27–50 kg/m2; HbA1c: >6.0% |
| C: low-glycemic, reduced-calorie diet | 46 | 51.8 ± 7.8 | 37 (80.4) | 166.8 ± 63.7 | 38.5 ± 5.6 | |||||
| Yancy 2007 [33] (US) | Randomized controlled trial (prospective analysis of volunteers from two clinical trials) | 24 weeks | I: low carbohydrate ketogenic diet | 27 | 43.8 ± 10.2 | 19 (70) | 87.1 ± 2.2 | 36.0 ± 4.9 | No | Age 18–65 years; BMI: 30–60 kg/m2 |
| C: low fat diet | 12 | 42.8 ± 7.3 | 9 (75) | 95.8 ± 3.1 | 36.0 ± 5.7 | |||||
| Yancy 2010 [34] (US) | Randomized controlled trial | 48 weeks | I: low-carbohydrate, ketogenic diet | 72 | 52.9 ± 10.2 | 20 (28) | - | 39.9 ± 6.9 | No | Age: 18–70 years; BMI: 27–30 kg/m2 (plus obesity-related disease) or BMI: ≥30 kg/m2 |
| C: orlistat therapy plus low-fat diet | 74 | 52.0 ± 9.2 | 21 (28) | - | 38.8±7.0 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Choi, Y.J.; Jeon, S.-M.; Shin, S. Impact of a Ketogenic Diet on Metabolic Parameters in Patients with Obesity or Overweight and with or without Type 2 Diabetes: A Meta-Analysis of Randomized Controlled Trials. Nutrients 2020, 12, 2005. https://doi.org/10.3390/nu12072005
Choi YJ, Jeon S-M, Shin S. Impact of a Ketogenic Diet on Metabolic Parameters in Patients with Obesity or Overweight and with or without Type 2 Diabetes: A Meta-Analysis of Randomized Controlled Trials. Nutrients. 2020; 12(7):2005. https://doi.org/10.3390/nu12072005
Chicago/Turabian StyleChoi, Yeo Jin, Sang-Min Jeon, and Sooyoung Shin. 2020. "Impact of a Ketogenic Diet on Metabolic Parameters in Patients with Obesity or Overweight and with or without Type 2 Diabetes: A Meta-Analysis of Randomized Controlled Trials" Nutrients 12, no. 7: 2005. https://doi.org/10.3390/nu12072005
APA StyleChoi, Y. J., Jeon, S.-M., & Shin, S. (2020). Impact of a Ketogenic Diet on Metabolic Parameters in Patients with Obesity or Overweight and with or without Type 2 Diabetes: A Meta-Analysis of Randomized Controlled Trials. Nutrients, 12(7), 2005. https://doi.org/10.3390/nu12072005





