Plasma Trans Fatty Acid Levels, Cardiovascular Risk Factors and Lifestyle: Results from the Akershus Cardiac Examination 1950 Study
Abstract
1. Introduction
2. Materials and Methods
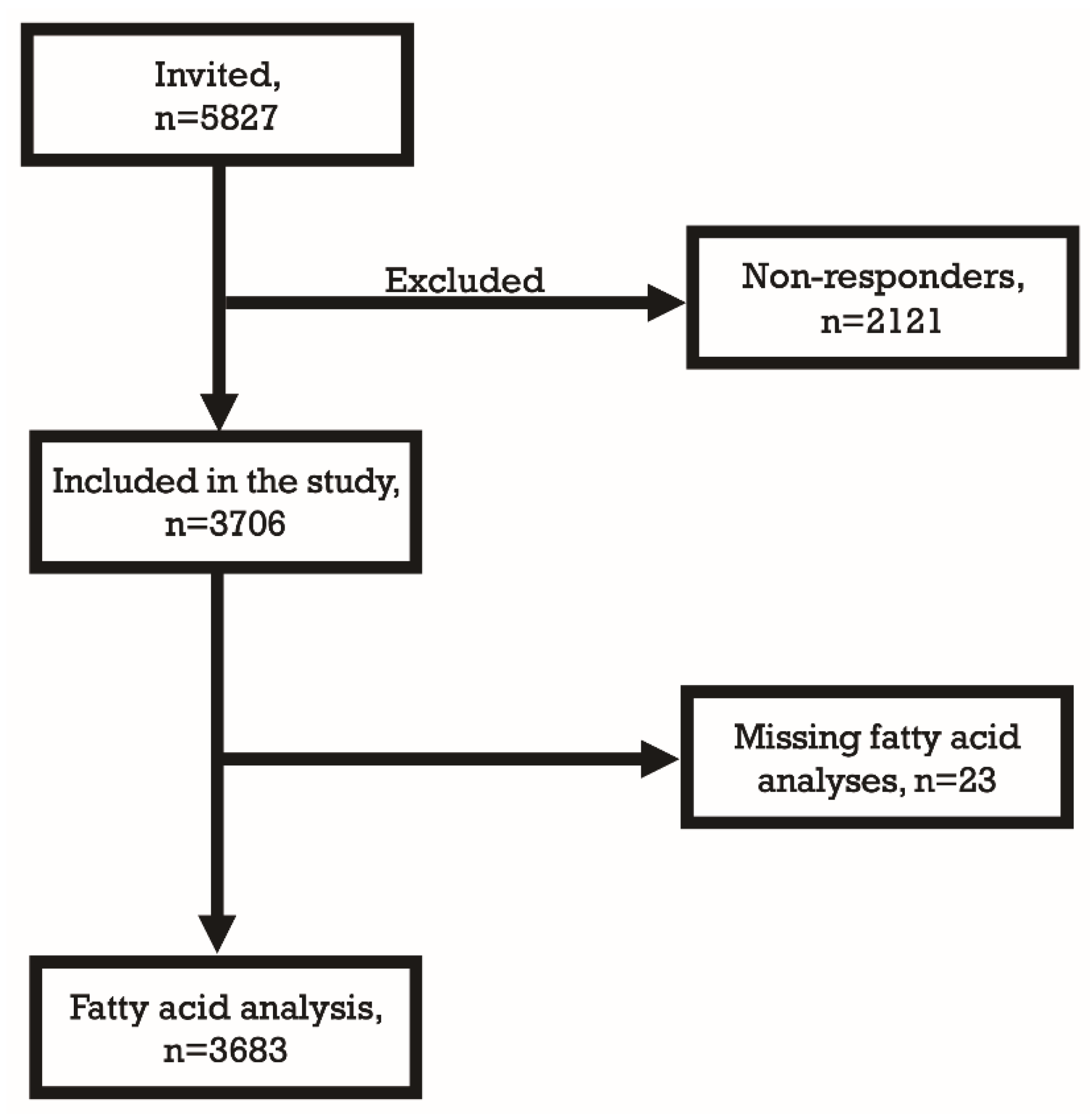
2.1. Study Cohort
2.2. Study Variables
2.3. Statistical Analysis
2.4. Ethics
3. Results
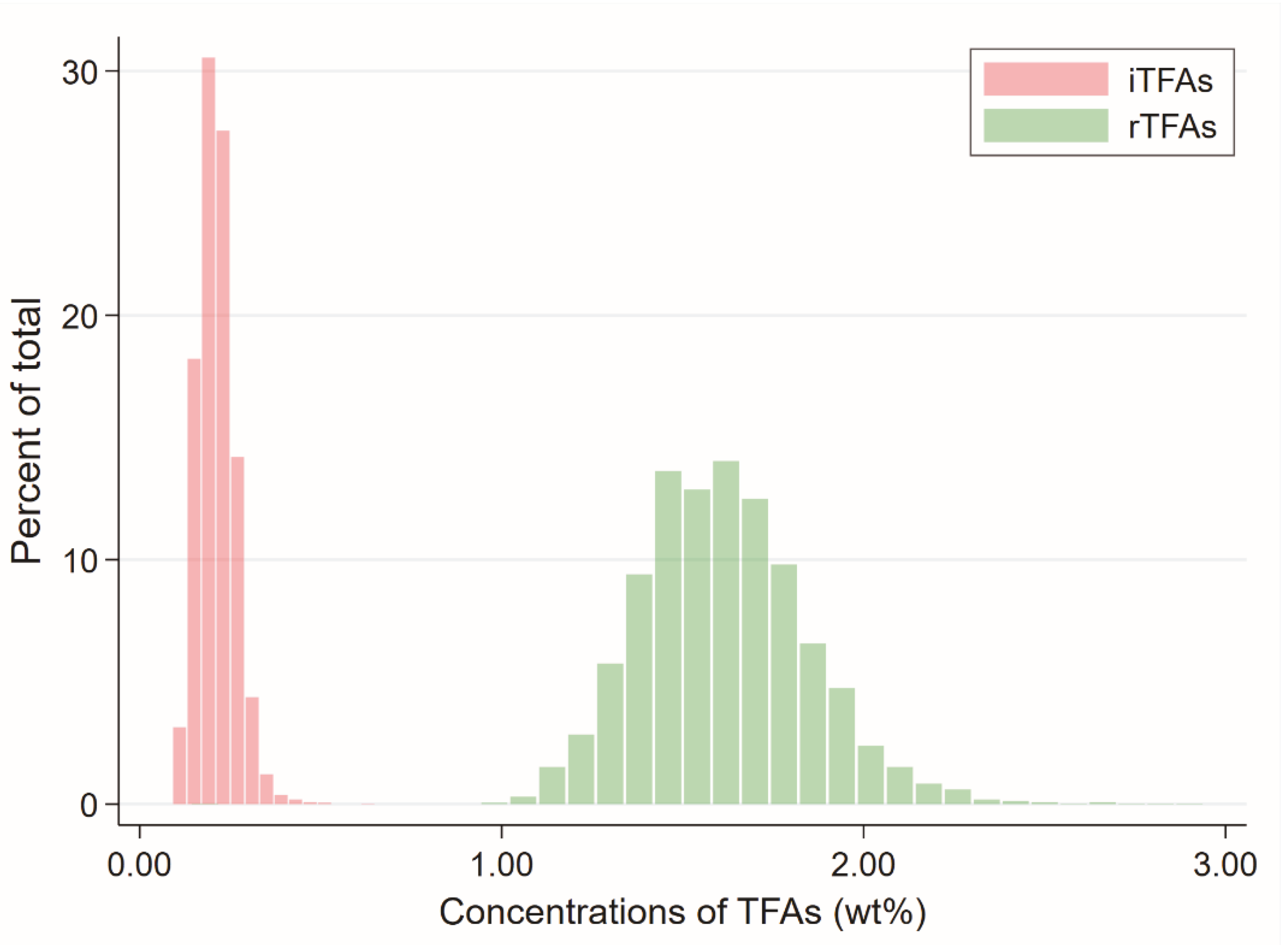
3.1. Demographics
3.2. Plasma iTFA Levels and CV Risk Factors
3.3. Plasma rTFA Levels and CV Risk Factors
4. Discussion
4.1. Plasma iTFA Levels and CV Risk Factors
4.2. Plasma rTFA Levels and CV Risk Factors
4.3. iTFA Legislation and Global Aspects
4.4. Strengths and Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Micha, R.; Mozaffarian, D. Trans fatty acids: Effects on cardiometabolic health and implications for policy. Prostaglandins Leukot. Essent. Fat. Acids 2008, 79, 147–152. [Google Scholar] [CrossRef]
- Mozaffarian, D.; Katan, M.B.; Ascherio, A.; Stampfer, M.J.; Willett, W.C. Trans fatty acids and cardiovascular disease. N. Engl. J. Med. 2006, 354, 1601–1613. [Google Scholar] [CrossRef]
- Willett, W.C.; Stampfer, M.J.; Manson, J.E.; Colditz, G.A.; Speizer, F.E.; Rosner, B.A.; Sampson, L.A.; Hennekens, C.H. Intake of trans fatty acids and risk of coronary heart disease among women. Lancet 1993, 341, 581–585. [Google Scholar] [CrossRef]
- Ascherio, A.; Rimm, E.B.; Giovannucci, E.L.; Spiegelman, D.; Stampfer, M.; Willett, W.C. Dietary fat and risk of coronary heart disease in men: Cohort follow up study in the United States. BMJ 1996, 313, 84–90. [Google Scholar] [CrossRef] [PubMed]
- Pietinen, P.; Ascherio, A.; Korhonen, P.; Hartman, A.M.; Willett, W.C.; Albanes, D.; Virtamo, J. Intake of fatty acids and risk of coronary heart disease in a cohort of Finnish men. The Alpha-Tocopherol, Beta-Carotene Cancer Prevention Study. Am. J. Epidemiol. 1997, 145, 876–887. [Google Scholar] [CrossRef] [PubMed]
- Oomen, C.M.; Ocke, M.C.; Feskens, E.J.; van Erp-Baart, M.A.; Kok, F.J.; Kromhout, D. Association between trans fatty acid intake and 10-year risk of coronary heart disease in the Zutphen Elderly Study: A prospective population-based study. Lancet 2001, 357, 746–751. [Google Scholar] [CrossRef]
- Oh, K.; Hu, F.B.; Manson, J.E.; Stampfer, M.J.; Willett, W.C. Dietary fat intake and risk of coronary heart disease in women: 20 years of follow-up of the nurses′ health study. Am. J. Epidemiol. 2005, 161, 672–679. [Google Scholar] [CrossRef]
- Astrup, A. The trans fatty acid story in Denmark. Athe. Suppl. 2006, 7, 43–46. [Google Scholar] [CrossRef]
- Stender, S. In equal amounts, the major ruminant trans fatty acid is as bad for LDL cholesterol as industrially produced trans fatty acids, but the latter are easier to remove from foods. Am. J. Clin. Nutr. 2015, 102, 1301–1302. [Google Scholar] [CrossRef]
- Diet, Nutrition and the Prevention of Chronic Diseases; World Health Organ Technical Report Series: Geneva, Switzerland, 2003; Volume 916, pp. 1–149.
- Johansson, L.; Borgejordet, A.; Pedersen, J.I. Trans fatty acids in the Norwegian diet. Tidsskr. Nor. Laegeforen. 2006, 126, 760–763. [Google Scholar]
- Laake, I.; Pedersen, J.I.; Selmer, R.; Kirkhus, B.; Lindman, A.S.; Tverdal, A.; Veierod, M.B. A prospective study of intake of trans-fatty acids from ruminant fat, partially hydrogenated vegetable oils, and marine oils and mortality from CVD. Br. J. Nutr. 2012, 108, 743–754. [Google Scholar] [CrossRef]
- Gebauer, S.K.; Destaillats, F.; Dionisi, F.; Krauss, R.M.; Baer, D.J. Vaccenic acid and trans fatty acid isomers from partially hydrogenated oil both adversely affect LDL cholesterol: A double-blind, randomized controlled trial. Am. J. Clin. Nutr. 2015, 102, 1339–1346. [Google Scholar] [CrossRef] [PubMed]
- Baylin, A.; Kim, M.K.; Donovan-Palmer, A.; Siles, X.; Dougherty, L.; Tocco, P.; Campos, H. Fasting whole blood as a biomarker of essential fatty acid intake in epidemiologic studies: Comparison with adipose tissue and plasma. Am. J. Epidemiol. 2005, 162, 373–381. [Google Scholar] [CrossRef] [PubMed]
- Berge, T.; Vigen, T.; Pervez, M.O.; Ihle-Hansen, H.; Lyngbakken, M.N.; Omland, T.; Smith, P.; Steine, K.; Rosjo, H.; Tveit, A.; et al. Heart and Brain Interactions—The Akershus Cardiac Examination (ACE) 1950 Study Design. Scand. Cardiovasc. J. 2015, 49, 308–315. [Google Scholar] [CrossRef] [PubMed]
- Svilaas, A.; Strom, E.C.; Svilaas, T.; Borgejordet, A.; Thoresen, M.; Ose, L. Reproducibility and validity of a short food questionnaire for the assessment of dietary habits. Nutr. Metab. Cardiovasc. Dis. 2002, 12, 60–70. [Google Scholar] [PubMed]
- Morseth, B.; Hopstock, L.A. Time trends in physical activity in the Tromso study: An update. PLoS ONE 2020, 15, e0231581. [Google Scholar] [CrossRef]
- Lamprea-Montealegre, J.A.; Zelnick, L.R.; Hall, Y.N.; Bansal, N.; de Boer, I.H. Prevalence of Hypertension and Cardiovascular Risk According to Blood Pressure Thresholds Used for Diagnosis. Hypertension 2018, 72, 602–609. [Google Scholar] [CrossRef]
- Obesity: Preventing and Managing the Global Epidemic: Report of a WHO Consultation; World Health Organization: Geneva, Switzerland, 2000; Volume 894, pp. 1–253.
- Expert Panel on Detection E. Treatment of High Blood Cholesterol in A: Executive Summary of The Third Report of The National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, And Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). JAMA 2001, 285, 2486–2497. [Google Scholar]
- American Diabetes Association. Diagnosis and Classification of Diabetes Mellitus. Diabetes Care 2014, 37, S81–S90. [Google Scholar] [CrossRef]
- Levey, A.S.; Stevens, L.A.; Schmid, C.H.; Zhang, Y.L.; Castro, A.F., III; Feldman, H.I.; Kusek, J.W.; Eggers, P.; Van Lente, F.; Greene, T.; et al. A new equation to estimate glomerular filtration rate. Ann. Intern. Med. 2009, 150, 604–612. [Google Scholar] [CrossRef]
- Ihle-Hansen, H.; Vigen, T.; Ihle-Hansen, H.; Ronning, O.M.; Berge, T.; Thommessen, B.; Lyngbakken, M.N.; Orstad, E.B.; Enger, S.; Nygard, S.; et al. Prevalence of Carotid Plaque in a 63- to 65-Year-Old Norwegian Cohort From the General Population: The ACE (Akershus Cardiac Examination) 1950 Study. J. Am. Heart Assoc. 2018, 7, e008562. [Google Scholar] [CrossRef] [PubMed]
- Eide, I.A.; Jenssen, T.; Hartmann, A.; Diep, L.M.; Dahle, D.O.; Reisaeter, A.V.; Bjerve, K.S.; Christensen, J.H.; Schmidt, E.B.; Svensson, M. The association between marine n-3 polyunsaturated fatty acid levels and survival after renal transplantation. Clin. J. Am. Soc. Nephrol. 2015, 10, 1246–1256. [Google Scholar] [CrossRef] [PubMed]
- Gebauer, S.K.; Chardigny, J.M.; Jakobsen, M.U.; Lamarche, B.; Lock, A.L.; Proctor, S.D.; Baer, D.J. Effects of ruminant trans fatty acids on cardiovascular disease and cancer: A comprehensive review of epidemiological, clinical, and mechanistic studies. Adv. Nutr. 2011, 2, 332–354. [Google Scholar] [CrossRef] [PubMed]
- Mensink, R.P.; Zock, P.L.; Kester, A.D.; Katan, M.B. Effects of dietary fatty acids and carbohydrates on the ratio of serum total to HDL cholesterol and on serum lipids and apolipoproteins: A meta-analysis of 60 controlled trials. Am. J. Clin. Nutr. 2003, 77, 1146–1155. [Google Scholar] [CrossRef]
- Mozaffarian, D. Trans fatty acids—Effects on systemic inflammation and endothelial function. Atheroscler. Suppl. 2006, 7, 29–32. [Google Scholar] [CrossRef]
- Tardy, A.L.; Morio, B.; Chardigny, J.M.; Malpuech-Brugere, C. Ruminant and industrial sources of trans-fat and cardiovascular and diabetic diseases. Nutr. Res. Rev. 2011, 24, 111–117. [Google Scholar] [CrossRef]
- Wilczek, M.M.; Olszewski, R.; Krupienicz, A. Trans-Fatty Acids and Cardiovascular Disease: Urgent Need for Legislation. Cardiology 2017, 138, 254–258. [Google Scholar] [CrossRef]
- Ascherio, A.; Hennekens, C.H.; Buring, J.E.; Master, C.; Stampfer, M.J.; Willett, W.C. Trans-fatty acids intake and risk of myocardial infarction. Circulation 1994, 89, 94–101. [Google Scholar] [CrossRef]
- Stender, S.; Astrup, A.; Dyerberg, J. Artificial trans fat in popular foods in 2012 and in 2014: A market basket investigation in six European countries. BMJ Open 2016, 6, e010673. [Google Scholar] [CrossRef]
- Ministers, N.C. Nordic Nutrition Recommendations 2012. 2014. Available online: https://www.nordic-ilibrary.org/content/publication/nord2014-002 (accessed on 20 February 2020).
- Chandra, A.; Svensson, M.; Asberg, A.; Schmidt, E.B.; Bjerve, K.S.; Jenssen, T.; Hartmann, A.; Ueland, T.; Eide, I.A. Trans-fatty Acids and Survival in Renal Transplantation. J. Ren. Nutr. 2019, 29, 169–180. [Google Scholar] [CrossRef]
- Lefevre, M.; Lovejoy, J.C.; Smith, S.R.; Delany, J.P.; Champagne, C.; Most, M.M.; Denkins, Y.; de Jonge, L.; Rood, J.; Bray, G.A. Comparison of the acute response to meals enriched with cis- or trans-fatty acids on glucose and lipids in overweight individuals with differing FABP2 genotypes. Metabolism 2005, 54, 1652–1658. [Google Scholar] [CrossRef] [PubMed]
- Field, A.E.; Willett, W.C.; Lissner, L.; Colditz, G.A. Dietary fat and weight gain among women in the Nurses’ Health Study. Obesity (Silver Spring) 2007, 15, 967–976. [Google Scholar] [CrossRef]
- Wang, L.; Manson, J.E.; Forman, J.P.; Gaziano, J.M.; Buring, J.E.; Sesso, H.D. Dietary fatty acids and the risk of hypertension in middle-aged and older women. Hypertension 2010, 56, 598–604. [Google Scholar] [CrossRef] [PubMed]
- Mozaffarian, D.; Pischon, T.; Hankinson, S.E.; Rifai, N.; Joshipura, K.; Willett, W.C.; Rimm, E.B. Dietary intake of trans fatty acids and systemic inflammation in women. Am. J. Clin. Nutr. 2004, 79, 606–612. [Google Scholar] [CrossRef] [PubMed]
- Transfettsyrer. Available online: https://www.matportalen.no/kosthold_og_helse/transfettsyrer (accessed on 20 February 2020).
- Stender, S.; Astrup, A.; Dyerberg, J. Ruminant and industrially produced trans fatty acids: Health aspects. Food Nutr Res. 2008, 52, 1651. [Google Scholar] [CrossRef]
- Jakobsen, M.U.; Bysted, A.; Andersen, N.L.; Heitmann, B.L.; Hartkopp, H.B.; Leth, T.; Overvad, K.; Dyerberg, J. Intake of ruminant trans fatty acids in the Danish population aged 1–80 years. Eur. J. Clin. Nutr. 2006, 60, 312–318. [Google Scholar] [CrossRef]
- Motard-Belanger, A.; Charest, A.; Grenier, G.; Paquin, P.; Chouinard, Y.; Lemieux, S.; Couture, P.; Lamarche, B. Study of the effect of trans fatty acids from ruminants on blood lipids and other risk factors for cardiovascular disease. Am. J. Clin. Nutr. 2008, 87, 593–599. [Google Scholar] [CrossRef]
- Mozaffarian, D.; Cao, H.; King, I.B.; Lemaitre, R.N.; Song, X.; Siscovick, D.S.; Hotamisligil, G.S. Trans-palmitoleic acid, metabolic risk factors, and new-onset diabetes in U.S. adults: A cohort study. Ann. Intern. Med. 2010, 153, 790–799. [Google Scholar] [CrossRef]
- Mozaffarian, D.; de Oliveira Otto, M.C.; Lemaitre, R.N.; Fretts, A.M.; Hotamisligil, G.; Tsai, M.Y.; Siscovick, D.S.; Nettleton, J.A. Trans-Palmitoleic acid, other dairy fat biomarkers, and incident diabetes: The Multi-Ethnic Study of Atherosclerosis (MESA). Am. J. Clin. Nutr. 2013, 97, 854–861. [Google Scholar] [CrossRef]
- Tholstrup, T.; Raff, M.; Basu, S.; Nonboe, P.; Sejrsen, K.; Straarup, E.M. Effects of butter high in ruminant trans and monounsaturated fatty acids on lipoproteins, incorporation of fatty acids into lipid classes, plasma C-reactive protein, oxidative stress, hemostatic variables, and insulin in healthy young men. Am. J. Clin. Nutr. 2006, 83, 237–243. [Google Scholar] [CrossRef]
- Hansen, C.P.; Berentzen, T.L.; Halkjær, J.; Tjønneland, A.; Sørensen, T.I.; Overvad, K.; Jakobsen, M.U. Intake of ruminant trans fatty acids and changes in body weight and waist circumference. Eur. J. Clin. Nutr. 2012, 66, 1104–1109. [Google Scholar] [CrossRef] [PubMed]
- Hansen, C.P.; Heitmann, B.L.; Sørensen TIa Overvad, K.; Jakobsen, M.U. Intake of ruminant trans-fatty acids, assessed by diet history interview, and changes in measured body size, shape and composition. Public Health Nutr. 2016, 19, 494–502. [Google Scholar] [CrossRef] [PubMed]
- Mensink, R.P.; de Louw, M.H.; Katan, M.B. Effects of dietary trans fatty acids on blood pressure in normotensive subjects. Eur. J. Clin. Nutr. 1991, 45, 375–382. [Google Scholar] [PubMed]
- Brouwer, I.A.; Wanders, A.J.; Katan, M.B. Trans fatty acids and cardiovascular health: Research completed? Eur. J. Clin. Nutr. 2013, 67, 541–547. [Google Scholar] [CrossRef] [PubMed]
- Micha, R.; Khatibzadeh, S.; Shi, P.; Fahimi, S.; Lim, S.; Andrews, K.G.; Engell, R.E.; Powles, J.; Ezzati, M.; Mozaffarian, D.; et al. Global, regional, and national consumption levels of dietary fats and oils in 1990 and 2010: A systematic analysis including 266 country-specific nutrition surveys. BMJ 2014, 348, g2272. [Google Scholar] [CrossRef]
- Wanders, A.J.; Zock, P.L.; Brouwer, I.A. Trans Fat Intake and Its Dietary Sources in General Populations Worldwide: A Systematic Review. Nutrients 2017, 9, 840. [Google Scholar] [CrossRef]
- Restrepo, B.J.; Rieger, M. Denmark′s Policy on Artificial Trans Fat and Cardiovascular Disease. Am. J. Prev. Med. 2016, 50, 69–76. [Google Scholar] [CrossRef]
| All Participants | Quartile 1 | Quartile 2 | Quartile 3 | Quartile 4 | p for Trend | p for Q1 vs. Q4 | |
|---|---|---|---|---|---|---|---|
| Industrial trans fatty acid level, wt% | 0.09–0.62 | ≤0.17 | 0.18–0.20 | 0.21–0.24 | ≥0.25 | ||
| Number of participants | 3683 | 1025 | 886 | 893 | 879 | ||
| Age, years | 63.9 (0.6) | 63.8 (0.6) | 63.9 (0.7) | 63.9 (0.7) | 64.0 (0.7) | <0.001 | <0.001 |
| Sex (Male), % | 51.3 (n = 1890) | 59.1 (n = 606) | 54.1 (n = 479) | 48.7 (n = 435) | 42.1 (n = 370) | <0.001 | <0.001 |
| Weekly intake of milk, 1 glass or more, % | 56.5 (n = 2042) | 55.4 (n = 560) | 55.2 (n = 476) | 58.0 (n = 508) | 57.6 (n = 498) | 0.52 | 0.34 |
| Use butter or margarine in cooking, % | 50.4 (n = 1782) | 50.1 (n = 496) | 51.8 (n = 441) | 50.6 (n = 431) | 48.9 (n = 414) | 0.68 | 0.61 |
| Use oil in cooking, % | 48.2 (n = 1706) | 48.6 (n = 481) | 46.1 (n = 392) | 48.3 (n = 411) | 49.8 (n = 422) | 0.47 | 0.60 |
| Weekly intake of fast food, once or more, % | 18.1 (n = 651) | 20.7 (n = 208) | 18.2 (n = 157) | 18.9 (n = 165) | 14.0 (n = 121) | 0.002 | <0.001 |
| Current smoker, % | 14.5 (n = 530) | 16.7 (n = 171) | 14.9 (n = 131) | 13.1 (n = 115) | 13.0 (n = 113) | 0.06 | 0.02 |
| Alcohol consumption, (≥2 times weekly), % | 47.4 (n = 1739) | 55.4 (n = 568) | 50.0 (n = 440) | 43.6 (n = 388) | 39.2 (n = 343) | <0.001 | <0.001 |
| Alcohol consumption, >5 units at same occasion, % | 46.6 (n = 1701) | 56.4 (n = 576) | 49.1 (431) | 43.5 (n = 383) | 35.9 (n = 311) | <0.001 | <0.001 |
| Physical activity (≥2 times weekly), % | 61.7 (n = 2240) | 59.1 (n = 600) | 61.5 (n = 536) | 63.4 (n = 554) | 63.4 (n = 550) | 0.17 | 0.06 |
| Higher education, % | 46.5 (n = 1708) | 39.0 (n = 399) | 48.6 (n = 429) | 48.8 (n = 435) | 50.7 (n = 445) | <0.001 | <0.001 |
| Hypertension, % | 62.0 (n = 2282) | 70.5 (n = 723) | 60.2 (n = 549) | 59.6 (n = 532) | 54.4 (n = 478) | <0.001 | <0.001 |
| Hypercholesterolemia, % | 52.6 (n = 1931) | 57.3 (n = 584) | 50.5 (n = 446) | 54.4 (n = 485) | 47.4 (n = 416) | <0.001 | <0.001 |
| Cerebrovascular disease, % | 3.7 (n = 138) | 3.2 (n = 33) | 3.3 (n = 29) | 4.7 (n = 42) | 3.9 (n = 34) | 0.30 | 0.44 |
| Coronary artery disease, % | 7.0 (n = 259) | 9.7 (n = 99) | 6.9 (n = 61) | 6.2 (n = 55) | 5.0 (n = 44) | 0.001 | <0.001 |
| Diabetes mellitus, % | 8.5 (n = 313) | 12.9 (n = 132) | 7.8 (n = 69) | 6.7 (n = 60) | 5.9 (n = 52) | <0.001 | <0.001 |
| Obesity (BMI ≥ 30), % | 22.6 (n = 831) | 27.7 (n = 284) | 21.3 (n = 189) | 23.2 (n = 207) | 17.2 (n = 151) | <0.001 | <0.001 |
| CKD stages 3–5 (eGFR <60 mL/min × 1.73 m2), % | 3.9 (n = 142) | 3.9 (n = 40) | 2.6 (n = 23) | 3.7 (n = 33) | 5.3 (n = 46) | 0.04 | 0.16 |
| Medication, % | |||||||
| Diuretics | 3.1 | 5.0 | 2.3 | 2.5 | 2.3 | 0.001 | <0.001 |
| Beta blockers | 13.4 | 18.6 | 13.7 | 10.8 | 9.6 | <0.001 | <0.001 |
| Calcium-channel blockers | 8.1 | 10.7 | 9.0 | 6.7 | 5.7 | <0.001 | <0.001 |
| ACEi or ARB | 26.9 | 34.2 | 26.5 | 24.3 | 21.5 | <0.001 | <0.001 |
| Lipid-lowering drugs | 26.1 | 31.4 | 27.3 | 24.3 | 20.7 | <0.001 | <0.001 |
| Glucose-lowering drugs | 5.4 | 7.6 | 5.4 | 4.6 | 3.6 | <0.001 | <0.001 |
| Systolic blood pressure, mmHg | 138 (19) | 140 (19) | 138 (19) | 137 (19) | 136 (18) | <0.001 | <0.001 |
| Diastolic blood pressure, mmHg | 77 (10) | 78 (10) | 77 (10) | 77 (10) | 76 (10) | <0.001 | <0.001 |
| HDL cholesterol, mmol/L | 1.5 (0.5) | 1.5 (0.5) | 1.5 (0.5) | 1.6 (0.5) | 1.6 (0.5) | <0.001 | <0.001 |
| LDL cholesterol, mmol/L | 3.3 (1.0) | 3.3 (1.0) | 3.2 (1.0) | 3.4 (1.0) | 3.3 (1.0) | 0.01 | 0.22 |
| Triglycerides, mmol/L | 1.2 (0.4–2–0) | 1.4 (0.5–2.3) | 1.2 (0.3–2.1) | 1.1 (0.4–1.8) | 1.0 (0.3–1.7) | <0.001 | <0.001 |
| FPG, mmol/L | 5.3 (4.5–6.1) | 5.4 (4.5–6.3) | 5.3 (4.5–6.1) | 5.2 (4.4–6.0) | 5.2 (4.4–6.0) | <0.001 | <0.001 |
| HbA1c, % | 5.7 (5.3–6.1) | 5.7 (5.2–6.2) | 5.7 (5.3–6.1) | 5.7 (5.3–6.1) | 5.7 (5.3–6.1) | 0.004 | 0.002 |
| Body mass index (BMI), kg/m2 | 27.1 (4.4) | 28.0 (4.4) | 27.2 (4.3) | 27.0 (4.5) | 26.2 (4.3) | <0.001 | <0.001 |
| eGFR, ml/min × 1.73m2 | 83 (11.9) | 83 (12.2) | 84 (11.4) | 83 (11.7) | 83 (12.4) | 0.18 | 0.14 |
| cIMT, mm | 0.73 (0.1) | 0.73 (0.1) | 0.73 (0.1) | 0.73 (0.1) | 0.72 (0.1) | 0.52 | 0.17 |
| CRP, mg/L | 1.5 (1.4–1.6) | 1.5 (1.4–1.6) | 1.5 (1.4–1.6) | 1.5 (1.4–1.6) | 1.5 (1.4–1.6) | - | - |
| Marine n-3 PUFAs, wt% | 8.1 (2.6) | 8.2 (2.8) | 8.2 (2.7) | 8.0 (2.5) | 7.9 (2.5) | 0.08 | 0.03 |
| LA, wt% | 20.8 (3.0) | 20.1 (3.0) | 20.6 (2.9) | 21.1 (2.8) | 21.4 (2.9) | <0.001 | <0.001 |
| AA, wt% | 9.2 (2.0) | 9.5 (2.1) | 9.3 (2.1) | 9.2 (2.0) | 8.9 (2.0) | <0.001 | <0.001 |
| SFA, wt% | 42.4 (0.9) | 42.8 (0.8) | 42.5 (0.8) | 42.3 (0.7) | 42.0 (0.9) | <0.001 | <0.001 |
| MUFA, wt% | 10.3 (1.4) | 10.3 (1.5) | 10.3 (1.4) | 10.2 (1.4) | 10.3 (1.3) | 0.17 | 0.84 |
| Univariable Linear Regression Analysis | |||||
| Cardiovascular Risk Factors | n | Unstd. β-coeff. (95% CI) | Std. β-coeff. | p | R2 |
| HDL cholesterol, mmol/L | 3680 | 1.02 (0.72, 1.32) | 0.11 | <0.001 | 0.01 |
| LDL cholesterol, mmol/L | 3657 | 0.55 (−0.05, 1.15) | 0.03 | 0.07 | 0.001 |
| Triglycerides, mmol/L | 3680 | −7.89 (−10.57, −5.89) | −0.22 | <0.001 | 0.05 |
| FPG, mmol/L | 3675 | −1.62 (−1.81, −1.47) | −0.15 | <0.001 | 0.02 |
| HbA1c, % | 3669 | −1.13 (−1.21, −1.06) | −0.07 | <0.001 | 0.004 |
| BMI, kg/m2 | 3683 | −13.50 (−16.23, −10.78) | −0.16 | <0.001 | 0.03 |
| SBP | 3679 | −30.09 (−41.77, −18.42) | −0.08 | <0.001 | 0.01 |
| DBP | 3679 | −16.45 (−22.70, −10.20) | −0.09 | <0.001 | 0.01 |
| eGFR, mL/min × 1.73m2 | 3664 | −5.43 (−12.90, 2.04) | −0.02 | 0.15 | 0.00 |
| cIMT, mm | 3661 | −0.07 (−0.14, 0.004) | −0.03 | 0.07 | 0.001 |
| CRP, mg/L | 3669 | −3.26 (−4.90, −2.14) | −0.09 | <0.001 | 0.01 |
| Multivariable Linear Regression Analysis | |||||
| Cardiovascular Risk Factors | n | Unstd. β-coeff. (95% CI) | Std. β-coeff. | p | R2 |
| HDL cholesterol, mmol/L a | 3640 | 0.20 (−0.06, 0.46) | 0.02 | 0.14 | 0.30 |
| LDL cholesterol, mmol/L b | 3617 | −0.44 (−0.97, 0.10) | −0.02 | 0.11 | 0.27 |
| Triglycerides, mmol/L c | 3640 | −4.19 (−5.52, −3.17) | −0.15 | <0.001 | 0.21 |
| FPG, mmol/L d | 3636 | −1.19 (−1.29, −1.09) | −0.05 | <0.001 | 0.39 |
| HbA1c, % e | 3630 | −1.01 (−1.06, 1.04) | −0.004 | 0.77 | 0.38 |
| BMI, kg/m2 f | 3612 | −11.22 (−13.90, −8.53) | −0.13 | <0.001 | 0.12 |
| SBP g | 3640 | −20.62 (−32.53, −8.72) | −0.06 | 0.001 | 0.03 |
| DBP h | 3640 | −6.68 (−12.80, −0.57) | −0.03 | 0.03 | 0.12 |
| eGFR, mL/min × 1.73m2 i | 3624 | −3.08 (−10.80, 4.61) | −0.01 | 0.43 | 0.03 |
| cIMT, mm j | 3625 | 0.04 (−0.03, 0.11) | 0.02 | 0.27 | 0.05 |
| CRP, mg/L k | 3629 | −2.07 (−3.14, −1.37) | −0.06 | 0.001 | 0.07 |
| Univariable Linear Regression Analysis | |||||
| Cardiovascular Risk Factors | n | Unstd. β-coeff. (95% CI) | Std. β-coeff. | p | R2 |
| HDL cholesterol, mmol/L a | 3680 | 0.25 (0.18, 0.32) | 0.12 | <0.001 | 0.01 |
| LDL cholesterol, mmol/L b | 3657 | −0.62 (−0.76, −0.49) | −0.15 | <0.001 | 0.02 |
| Triglycerides, mmol/L c | 3680 | −1.51 (−1.61, −1.41) | −0.20 | <0.001 | 0.04 |
| FPG, mmol/L d | 3675 | −1.11 (−1.14, −1.08) | −0.14 | <0.001 | 0.02 |
| HbA1c, % e | 3669 | −1.08 (−1.10, −1.07) | −0.19 | <0.001 | 0.04 |
| BMI, kg/m2 f | 3683 | −2.60 (−3.21, −1.99) | −0.14 | <0.001 | 0.02 |
| SBP g | 3679 | −5.14 (−7.75, −2.53) | −0.06 | <0.001 | 0.004 |
| DBP h | 3679 | −3.40 (−4.80, −2.01) | −0.08 | <0.001 | 0.01 |
| eGFR, mL/min × 1.73m2 i | 3664 | −0.01 (−1.68, 1.66) | 0.00 | 0.99 | 0.00 |
| cIMT, mm j | 3661 | −0.002 (−0.02, 0.01) | −0.004 | 0.83 | 0.00 |
| CRP, mg/L k | 3669 | −1.12 (−1.23, −1.02) | −0.04 | 0.01 | 0.001 |
| Multivariable Linear Regression Analysis | |||||
| Cardiovascular Risk Factors | n | Unstd. β-coeff. (95% CI) | Std. β-coeff. | p | R2 |
| HDL cholesterol, mmol/L a | 3640 | 0.16 (0.10, 0.22) | 0.08 | <0.001 | 0.27 |
| LDL cholesterol, mmol/L b | 3617 | −0.42 (−0.54, −0.30) | −0.10 | <0.001 | 0.28 |
| Triglycerides, mmol/L c | 3640 | −1.37 (−1.46, −1.29) | −0.15 | <0.001 | 0.21 |
| FPG, mmol/L d | 3636 | −1.06 (−1.08, −1.04) | −0.08 | <0.001 | 0.39 |
| HbA1c, % e | 3630 | −1.06 (−1.07, −1.04) | −0.13 | <0.001 | 0.39 |
| BMI, kg/m2 f | 3612 | −1.96 (−2.55, −1.37) | −0.10 | <0.001 | 0.10 |
| SBP g | 3640 | −3.31 (−5.92, −0.69) | −0.04 | 0.01 | 0.03 |
| DBP g | 3640 | −2.98 (−4.32, −1.64) | −0.07 | <0.001 | 0.12 |
| eGFR, mL/min × 1.73m2 i | 3624 | −0.83 (−2.52, 0.85) | −0.02 | 0.33 | 0.03 |
| cIMT, mm j | 3625 | 0.01 (−0.01, 0.02) | 0.01 | 0.56 | 0.05 |
| CRP, mg/L k | 3629 | −1.03 (−1.12, 1.04) | −0.01 | 0.49 | 0.07 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chandra, A.; Lyngbakken, M.N.; Eide, I.A.; Røsjø, H.; Vigen, T.; Ihle-Hansen, H.; Orstad, E.B.; Rønning, O.M.; Berge, T.; Schmidt, E.B.; et al. Plasma Trans Fatty Acid Levels, Cardiovascular Risk Factors and Lifestyle: Results from the Akershus Cardiac Examination 1950 Study. Nutrients 2020, 12, 1419. https://doi.org/10.3390/nu12051419
Chandra A, Lyngbakken MN, Eide IA, Røsjø H, Vigen T, Ihle-Hansen H, Orstad EB, Rønning OM, Berge T, Schmidt EB, et al. Plasma Trans Fatty Acid Levels, Cardiovascular Risk Factors and Lifestyle: Results from the Akershus Cardiac Examination 1950 Study. Nutrients. 2020; 12(5):1419. https://doi.org/10.3390/nu12051419
Chicago/Turabian StyleChandra, Anupam, Magnus Nakrem Lyngbakken, Ivar Anders Eide, Helge Røsjø, Thea Vigen, Håkon Ihle-Hansen, Eivind Bjørkan Orstad, Ole Morten Rønning, Trygve Berge, Erik Berg Schmidt, and et al. 2020. "Plasma Trans Fatty Acid Levels, Cardiovascular Risk Factors and Lifestyle: Results from the Akershus Cardiac Examination 1950 Study" Nutrients 12, no. 5: 1419. https://doi.org/10.3390/nu12051419
APA StyleChandra, A., Lyngbakken, M. N., Eide, I. A., Røsjø, H., Vigen, T., Ihle-Hansen, H., Orstad, E. B., Rønning, O. M., Berge, T., Schmidt, E. B., Tveit, A., Omland, T., & Svensson, M. (2020). Plasma Trans Fatty Acid Levels, Cardiovascular Risk Factors and Lifestyle: Results from the Akershus Cardiac Examination 1950 Study. Nutrients, 12(5), 1419. https://doi.org/10.3390/nu12051419





