Development and Validation of a Questionnaire to Measure Adherence to the Mediterranean Diet in Korean Adults
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Population
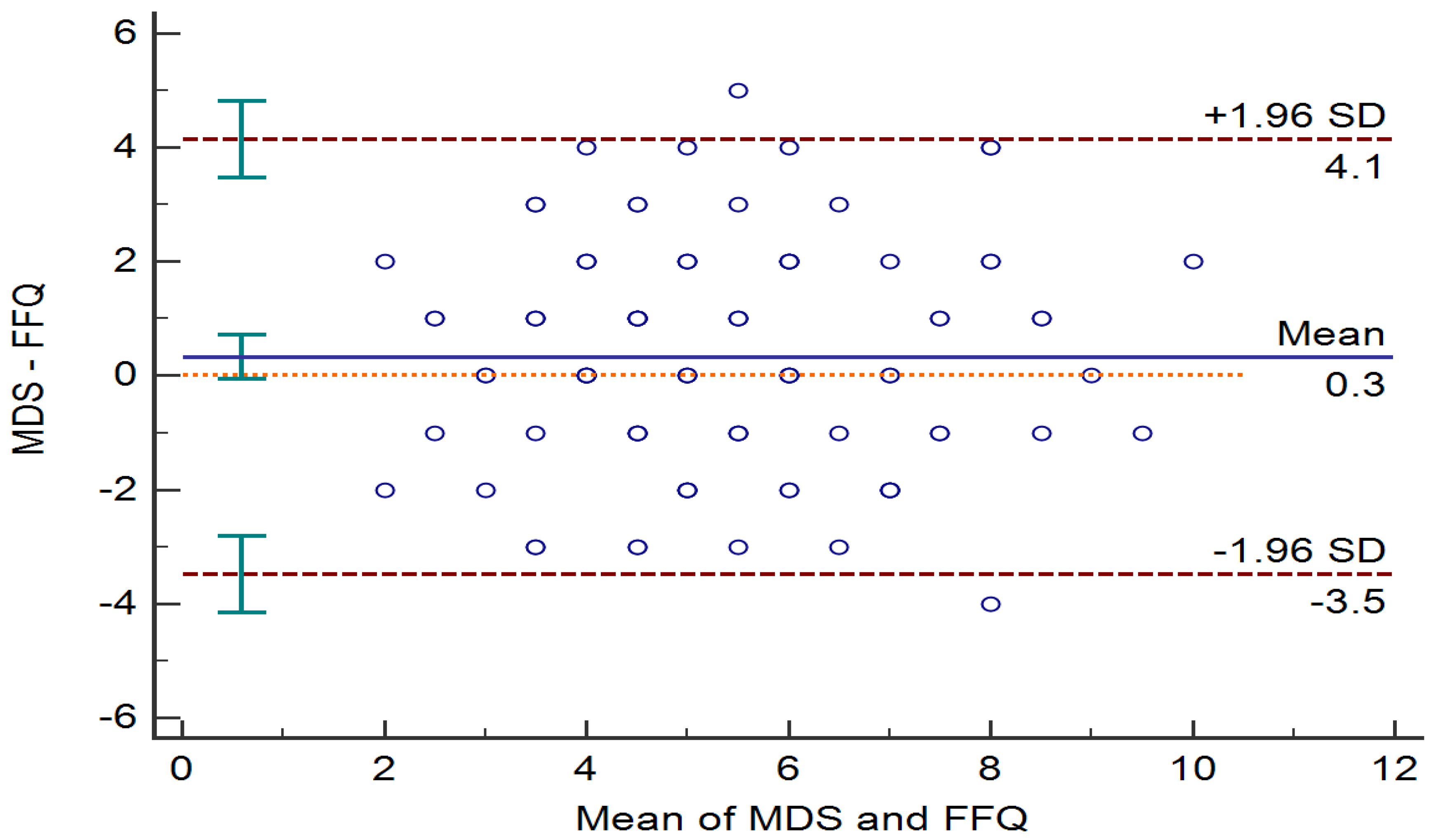
2.2. Development of the Korean Version of the Mediterranean Diet Adherence Screener
2.3. Lifestyles and Dietary Assessment
2.4. Anthropometric and Laboratory Measurements
2.5. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
Appendix A
| MD Scores | Total | Tertile 1 (≤4) | Tertile 2(5–6) | Tertile 3 (≥7) |
|---|---|---|---|---|
| n | 116 | 37 | 45 | 34 |
| Age | 53.0 ± 10.4 | 49.9 ± 10.8 | 54.1 ± 8.1 | 54.6 ± 12.8 |
| Sex, female, n (%) | 108 (89.1) | 32 (86.4) | 41 (91.1) | 31 (91.2) |
| Body mass index, kg/m2 | 26.2 ± 4.4 | 27.1 ± 5.3 | 26.0 ± 4.3 | 25.5 ± 3.7 |
| Waist circumference, cm | 87.5 ± 11.0 | 88.6 ± 11.7 | 87.4 ± 11.7 | 86.1 ± 9.6 |
| Systolic blood pressure, mmHg | 117.0 ± 14.6 | 113.9 ± 12.6 | 119.8 ± 16.9 | 115.6 ± 13.3 |
| Diastolic blood pressure, mmHg | 73.9 ± 10.0 | 73.9 ± 9.1 | 74.3 ± 11.0 | 73.2 ± 10.5 |
| Smoking, n (%) | 8(6.9) | 5 (13.5) | 2 (4.9) | 0 (-) |
| Alcohol intake, n (%) | 48 (41.4) | 18 (48.6) | 32 (71.1) | 20(58.8) |
| Physical activity, n (%) | 34 (29.3) | 7 (18.9) | 11 (24.4) | 17 (44.1) |
| Glucose, mg/dl | 105.6 ± 18.0 | 107.8 ± 23.0 | 105.4 ± 18.6 | 103.5 ± 10.7 |
| Total cholesterol, mg/dl | 212.5 ± 39.5 | 214.1 ± 37.5 | 212.8 ± 44.7 | 207.3 ± 35.1 |
| Triglyceride, mg/dl | 132.3 ± 62.1 | 137.6 ± 57.3 | 132.0 ± 64.4 | 118.5 ± 62.6 |
| Low-density lipoprotein cholesterol, mg/dl | 129.5 ± 34.6 | 131.7 ± 33.3 | 129.6 ± 39.4 | 124.9 ± 29.5 |
| High-density lipoprotein cholesterol, mg/dl | 57.2 ± 13.2 | 56.5 ± 13.2 | 56.5 ± 13.0 | 59.2 ± 13.9 |
| Non-high-density lipoprotein cholesterol, mg/dl | 155.4 ± 38.2 | 157.6 ± 37.8 | 156.2 ± 42.9 | 148.1 ± 32.5 |
| Total energy (kcal) | 1545.2 ± 584.6 | 1596.7 ± 702.3 | 1544.0 ± 616.0 | 1458.8 ± 420.7 |
| Carbohydrate, % | 57.6 ± 13.0 | 52.8 ± 14.8 | 60.5 ± 11.3 | 60.4 ± 11.8 |
| Fiber, g | 20.1 ± 9.6 | 18.7 ± 10.6 | 20.1 ± 8.0 | 21.1 ± 10.2 |
| Protein, % | 16.3 ± 4.7 | 16.9 ± 5.7 | 15.9 ± 4.0 | 15.9 ± 4.9 |
| Fat, % | 25.0 ± 9.7 | 27.7 ± 11.3 | 23.2 ± 8.3 | 23.4 ± 8.5 |
| Saturated fat, % | 5.7 ± 10.8 | 5.2 ± 4.9 | 5.5 ± 6.9 | 3.8 ± 3.0 |
| Monounsaturated fatty acid, % | 6.9 ± 7.4 | 6.9 ± 5.9 | 7.7 ± 9.5 | 5.3 ± 3.3 |
| Polyunsaturated fatty acid, % | 4.7 ± 3.9 | 5.6 ± 4.4 | 4.6 ± 3.8 | 3.7 ± 2.7 |
| Omega-6, % | 2.0 ± 4.0 | 1.9 ± 2.5 | 1.6 ± 1.7 | 1.6 ± 1.7 |
| Omega-3, % | 0.9 ± 1.8 | 0.6 ± 1.1 | 0.4 ± 0.8 | 0.6 ± 0.9 |
| Omega-6/Omega-3 | 10.0 ± 7.2 | 9.0 ± 6.6 | 9.8 ± 6.9 | 11.1 ± 8.1 |
| Vitamin C, mg † | 100.6 ± 116.2 | 0.06 ± 0.08 | 0.07 ± 0.05 | 0.08 ± 0.07 |
| Vitamin E, mg † | 11.8 ± 9.2 | 0.008 ± 0.005 | 0.007 ± 0.003 | 0.006 ± 0.003 |
| Folic acid, µg † | 454.3 ± 230.0 | 0.28 ± 0.15 | 0.32 ± 0.13 | 0.32 ± 0.14 |
| β-carotene, µg † | 3390.1 ± 3085.2 | 1.7 ± 1.2 | 2.5 ± 2.4 | 2.6 ± 2.7 |
References
- Magkos, F.; Tetens, I.; Bugel, S.G.; Felby, C.; Schacht, S.R.; Hill, J.O.; Ravussin, E.; Astrup, A. A Perspective on the Transition to Plant-Based Diets: A Diet Change May Attenuate Climate Change, but Can It Also Attenuate Obesity and Chronic Disease Risk? Adv. Nutr. 2020, 11, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Sofi, F.; Abbate, R.; Gensini, G.F.; Casini, A. Accruing evidence on benefits of adherence to the Mediterranean diet on health: An updated systematic review and meta-analysis. Am. J. Clin. Nutr. 2010, 92, 1189–1196. [Google Scholar] [CrossRef] [PubMed]
- Bellavia, A.; Tektonidis, T.G.; Orsini, N.; Wolk, A.; Larsson, S.C. Quantifying the benefits of Mediterranean diet in terms of survival. Eur. J. Epidemiol. 2016, 31, 527–530. [Google Scholar] [CrossRef] [PubMed]
- Trichopoulou, A.; Costacou, T.; Bamia, C.; Trichopoulos, D. Adherence to a Mediterranean diet and survival in a Greek population. N. Engl. J. Med. 2003, 348, 2599–2608. [Google Scholar] [CrossRef] [PubMed]
- Schwingshackl, L.; Schwedhelm, C.; Galbete, C.; Hoffmann, G. Adherence to Mediterranean Diet and Risk of Cancer: An Updated Systematic Review and Meta-Analysis. Nutrients 2017, 9, 1063. [Google Scholar] [CrossRef]
- Tosti, V.; Bertozzi, B.; Fontana, L. Health Benefits of the Mediterranean Diet: Metabolic and Molecular Mechanisms. J. Gerontol. A Biol. Sci. Med. Sci. 2018, 73, 318–326. [Google Scholar] [CrossRef]
- Trichopoulou, A.; Kouris-Blazos, A.; Wahlqvist, M.L.; Gnardellis, C.; Lagiou, P.; Polychronopoulos, E.; Vassilakou, T.; Lipworth, L.; Trichopoulos, D. Diet and overall survival in elderly people. BMJ 1995, 311, 1457–1460. [Google Scholar] [CrossRef]
- Buckland, G.; Gonzalez, C.A.; Agudo, A.; Vilardell, M.; Berenguer, A.; Amiano, P.; Ardanaz, E.; Arriola, L.; Barricarte, A.; Basterretxea, M.; et al. Adherence to the Mediterranean diet and risk of coronary heart disease in the Spanish EPIC Cohort Study. Am. J. Epidemiol. 2009, 170, 1518–1529. [Google Scholar] [CrossRef]
- Schroder, H.; Fito, M.; Estruch, R.; Martinez-Gonzalez, M.A.; Corella, D.; Salas-Salvado, J.; Lamuela-Raventos, R.; Ros, E.; Salaverria, I.; Fiol, M.; et al. A short screener is valid for assessing Mediterranean diet adherence among older Spanish men and women. J. Nutr. 2011, 141, 1140–1145. [Google Scholar] [CrossRef]
- Hebestreit, K.; Yahiaoui-Doktor, M.; Engel, C.; Vetter, W.; Siniatchkin, M.; Erickson, N.; Halle, M.; Kiechle, M.; Bischoff, S.C. Validation of the German version of the Mediterranean Diet Adherence Screener (MEDAS) questionnaire. BMC Cancer 2017, 17, 341. [Google Scholar] [CrossRef]
- Papadaki, A.; Johnson, L.; Toumpakari, Z.; England, C.; Rai, M.; Toms, S.; Penfold, C.; Zazpe, I.; Martinez-Gonzalez, M.A.; Feder, G. Validation of the English Version of the 14-Item Mediterranean Diet Adherence Screener of the PREDIMED Study, in People at High Cardiovascular Risk in the UK. Nutrients 2018, 10, 138. [Google Scholar] [CrossRef] [PubMed]
- Kanauchi, M.; Kanauchi, K. Development of a Mediterranean diet score adapted to Japan and its relation to obesity risk. Food Nutr. Res. 2016, 60, 32172. [Google Scholar] [CrossRef] [PubMed]
- Kim, Y.; Je, Y. A modified Mediterranean diet score is inversely associated with metabolic syndrome in Korean adults. Eur. J. Clin. Nutr. 2018, 72, 1682–1689. [Google Scholar] [CrossRef] [PubMed]
- Song, Y.; Joung, H. A traditional Korean dietary pattern and metabolic syndrome abnormalities. Nutr. Metab. Cardiovasc. Dis. 2012, 22, 456–462. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.; Moon, S.; Popkin, B.M. The nutrition transition in South Korea. Am. J. Clin. Nutr. 2000, 71, 44–53. [Google Scholar] [CrossRef] [PubMed]
- Rhee, E.J.; Kim, H.C.; Kim, J.H.; Lee, E.Y.; Kim, B.J.; Kim, E.M.; Song, Y.; Lim, J.H.; Kim, H.J.; Choi, S.; et al. 2018 Guidelines for the management of dyslipidemia. Korean J. Intern. Med. 2019, 34, 723–771. [Google Scholar] [CrossRef] [PubMed]
- Jensen, M.D.; Ryan, D.H.; Apovian, C.M.; Ard, J.D.; Comuzzie, A.G.; Donato, K.A.; Hu, F.B.; Hubbard, V.S.; Jakicic, J.M.; Kushner, R.F.; et al. 2013 AHA/ACC/TOS guideline for the management of overweight and obesity in adults: A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and The Obesity Society. Circulation 2014, 129, S102–S138. [Google Scholar] [CrossRef]
- Martinez-Gonzalez, M.A.; Corella, D.; Salas-Salvado, J.; Ros, E.; Covas, M.I.; Fiol, M.; Warnberg, J.; Aros, F.; Ruiz-Gutierrez, V.; Lamuela-Raventos, R.M.; et al. Cohort profile: Design and methods of the PREDIMED study. Int. J. Epidemiol. 2012, 41, 377–385. [Google Scholar] [CrossRef]
- Lee, P.H.; Macfarlane, D.J.; Lam, T.H.; Stewart, S.M. Validity of the International Physical Activity Questionnaire Short Form (IPAQ-SF): A systematic review. Int. J. Behav. Nutr. Phys. Act. 2011, 8, 115. [Google Scholar] [CrossRef]
- Oh, J.Y.; Yang, Y.J.; Kim, B.S.; Kang, J.H. Validity and Reliability of Korean Version of International Physical Activity Questionnaire (IPAQ) Short Form. J. Korean Acad. Fam. Med. 2007, 28, 532–541. [Google Scholar]
- Kim, Y.; Han, B.G. Cohort Profile: The Korean Genome and Epidemiology Study (KoGES) Consortium. Int. J. Epidemiol. 2017, 46, e20. [Google Scholar] [CrossRef] [PubMed]
- Sim, J.; Wright, C.C. The kappa statistic in reliability studies: Use, interpretation, and sample size requirements. Phys. Ther. 2005, 85, 257–268. [Google Scholar] [CrossRef] [PubMed]
- Cena, H.; Calder, P.C. Defining a Healthy Diet: Evidence for The Role of Contemporary Dietary Patterns in Health and Disease. Nutrients 2020, 12, 334. [Google Scholar] [CrossRef] [PubMed]
- Gaforio, J.J.; Visioli, F.; Alarcon-de-la-Lastra, C.; Castaner, O.; Delgado-Rodriguez, M.; Fito, M.; Hernandez, A.F.; Huertas, J.R.; Martinez-Gonzalez, M.A.; Menendez, J.A.; et al. Virgin Olive Oil and Health: Summary of the III International Conference on Virgin Olive Oil and Health Consensus Report, JAEN (Spain) 2018. Nutrients 2019, 11, 2039. [Google Scholar] [CrossRef]
- Pettid, M.J. Korean Cuisine: An Illustrated History; Reaktion Books: London, UK, 2008. [Google Scholar]
- Asif, M. Health effects of omega-3,6,9 fatty acids: Perilla frutescens is a good example of plant oils. Orient. Pharm. Exp. Med. 2011, 11, 51–59. [Google Scholar] [CrossRef]
- Kim, H.N.; Song, S.W. Association between carbohydrate intake and body composition: The Korean National Health and Nutrition Examination Survey. Nutrition 2019, 61, 187–193. [Google Scholar] [CrossRef]
- Park, S.H.; Lee, K.S.; Park, H.Y. Dietary carbohydrate intake is associated with cardiovascular disease risk in Korean: Analysis of the third Korea National Health and Nutrition Examination Survey (KNHANES III). Int. J. Cardiol. 2010, 139, 234–240. [Google Scholar] [CrossRef]
- Song, S.; Lee, J.E.; Song, W.O.; Paik, H.Y.; Song, Y. Carbohydrate intake and refined-grain consumption are associated with metabolic syndrome in the Korean adult population. J. Acad. Nutr. Diet. 2014, 114, 54–62. [Google Scholar] [CrossRef]
- McKeown, N.M.; Meigs, J.B.; Liu, S.; Wilson, P.W.; Jacques, P.F. Whole-grain intake is favorably associated with metabolic risk factors for type 2 diabetes and cardiovascular disease in the Framingham Offspring Study. Am. J. Clin. Nutr. 2002, 76, 390–398. [Google Scholar] [CrossRef]
- Shannon, O.M.; Mendes, I.; Kochl, C.; Mazidi, M.; Ashor, A.W.; Rubele, S.; Minihane, A.M.; Mathers, J.C.; Siervo, M. Mediterranean Diet Increases Endothelial Function in Adults: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. J. Nutr. 2020. [Google Scholar] [CrossRef]
- Guasch-Ferre, M.; Liu, G.; Li, Y.; Sampson, L.; Manson, J.E.; Salas-Salvado, J.; Martinez-Gonzalez, M.A.; Stampfer, M.J.; Willett, W.C.; Sun, Q.; et al. Olive Oil Consumption and Cardiovascular Risk in U.S. Adults. J. Am. Coll. Cardiol. 2020. [Google Scholar] [CrossRef] [PubMed]
- Martinez-Gonzalez, M.A.; Gea, A.; Ruiz-Canela, M. The Mediterranean Diet and Cardiovascular Health. Circ. Res. 2019, 124, 779–798. [Google Scholar] [CrossRef] [PubMed]
- Kris-Etherton, P.M.; Pearson, T.A.; Wan, Y.; Hargrove, R.L.; Moriarty, K.; Fishell, V.; Etherton, T.D. High-monounsaturated fatty acid diets lower both plasma cholesterol and triacylglycerol concentrations. Am. J. Clin. Nutr. 1999, 70, 1009–1015. [Google Scholar] [CrossRef] [PubMed]
- Gill, J.M.; Brown, J.C.; Caslake, M.J.; Wright, D.M.; Cooney, J.; Bedford, D.; Hughes, D.A.; Stanley, J.C.; Packard, C.J. Effects of dietary monounsaturated fatty acids on lipoprotein concentrations, compositions, and subfraction distributions and on VLDL apolipoprotein B kinetics: Dose-dependent effects on LDL. Am. J. Clin. Nutr. 2003, 78, 47–56. [Google Scholar] [CrossRef] [PubMed]
- Wang, D.D.; Li, Y.; Chiuve, S.E.; Stampfer, M.J.; Manson, J.E.; Rimm, E.B.; Willett, W.C.; Hu, F.B. Association of Specific Dietary Fats With Total and Cause-Specific Mortality. JAMA Intern. Med. 2016, 176, 1134–1145. [Google Scholar] [CrossRef] [PubMed]
- Salas-Salvado, J.; Farres, X.; Luque, X.; Narejos, S.; Borrell, M.; Basora, J.; Anguera, A.; Torres, F.; Bullo, M.; Balanza, R. Effect of two doses of a mixture of soluble fibres on body weight and metabolic variables in overweight or obese patients: A randomised trial. Br. J. Nutr. 2008, 99, 1380–1387. [Google Scholar] [CrossRef]
- Naumann, S.; Schweiggert-Weisz, U.; Bader-Mittermaier, S.; Haller, D.; Eisner, P. Differentiation of Adsorptive and Viscous Effects of Dietary Fibres on Bile Acid Release by Means of In Vitro Digestion and Dialysis. Int. J. Mol. Sci. 2018, 19, 2193. [Google Scholar] [CrossRef]
| MD Scores | Total | Tertile1 (≤5) | Tertile2 (6–7) | Tertile3 (≥8) |
|---|---|---|---|---|
| n | 211 | 85 | 63 | 63 |
| Age | 47.4 ± 10.0 | 43.6 ± 9.1 a | 47.6 ± 10.0 b | 53.3 ± 8.3 c |
| Sex, female, n (%) | 116 (55.0) | 41 (48.2) | 32 (27.6) | 43 (68.3) |
| Body mass index, kg/m2 | 23.6 ± 3.7 | 23.4 ± 3.6 | 24.0 ± 3.9 | 23.5 ± 3.7 |
| Waist circumference, cm | 80.2 ± 10.5 | 80.1 ± 10.9 | 82.1 ± 10.3 | 78.6 ± 10.0 |
| Systolic blood pressure, mmHg | 117.9 ± 12.3 | 116.9 ± 12.7 | 118.0 ± 12.2 | 119.2 ± 12.1 |
| Diastolic blood pressure, mmHg | 73.5 ± 10.0 | 72.7 ± 10.4 | 72.9 ± 9.9 | 75.2 ± 9.3 |
| Smoking, n (%) | 66 (31.3) | 15 (32.9) | 21 (33.3) | 17 (27.0) |
| Alcohol intake, n (%) | 114 (54.0) | 47 (56.0) | 40 (63.5) | 27 (42.9) |
| Physical activity, MET | 1699.1 ± 1604.3 | 1435.8 ± 1672.6 a | 1624.1 ± 1137.2 | 2129.2 ± 1829.1 c |
| Glucose, mg/dl | 97.5 ± 17.3 | 97.4 ± 18.0 | 97.6 ± 14.7 | 97.4 ± 19.0 |
| Total cholesterol, mg/dl | 200.2 ± 37.6 | 207.9 ± 32.2 | 195.2 ± 38.6 | 194.8 ± 38.6 |
| Triglyceride, mg/dl | 109.2 ± 63.0 | 110.1 ± 58.9 | 115.1 ± 70.6 | 101.9 ± 60.4 |
| Low-density lipoprotein cholesterol, mg/dl | 119.3 ± 34.8 | 126.4 ± 37.4 | 112.6 ± 35.0 | 108.4 ± 36.5 |
| High-density lipoprotein cholesterol, mg/dl | 58.7 ± 13.9 | 60.0 ± 14.9 | 56.6 ± 12.3 | 59.2 ± 14.0 |
| Non-high-density lipoprotein cholesterol, mg/dl | 141.5 ± 37.4 | 147.9 ± 36.4 | 138.7 ± 38.6 | 135.7 ± 36.6 |
| Total energy (kcal) | 1315.5 ± 488.5 | 1352.2 ± 506.9 | 1226.6 ± 488.3 | 1354.7 ± 458.4 |
| Carbohydrate, % | 57.3 ± 9.5 | 56.3 ± 7.2 | 57.4 ± 13.7 | 58.6 ± 6.7 |
| Fiber, g | 10.4 ± 6.1 | 8.9 ± 4.4 a | 9.2 ± 5.4 b | 13.6 ± 7.5 c |
| Protein, % | 17.7 ± 3.3 | 17.5 ± 3.4 | 17.5 ± 3.0 | 17.7 ± 3.4 |
| Fat, % | 25.4 ± 6.8 | 25.8 ± 6.6 | 25.7 ± 7.5 | 24.4 ± 6.2 |
| Saturated fat, % | 5.9 ± 2.3 | 6.3 ± 2.4 | 5.9 ± 2.1 | 5.5 ± 2.2 |
| Monounsaturated fatty acid, % | 6.6 ± 4.6 | 6.4 ± 2.1 | 6.5 ± 2.2 | 6.6 ± 4.6 |
| Polyunsaturated fatty acid, % | 5.4 ± 1.9 | 5.0 ± 1.8 a | 5.3 ± 2.1 a,b | 6.1 ± 1.7 b |
| Omega-6, % | 4.6 ± 3.1 | 4.8 ± 1.6 | 5.0 ± 5.2 | 4.8 ± 1.3 |
| Omega-3, % | 0.9 ± 0.6 | 0.7 ± 0.4 a | 0.8 ± 0.6 b | 1.2 ± 0.8 c |
| Omega-6/Omega-3 | 6.9 ± 3.8 | 7.4 ± 3.2 a | 7.6 ± 4.8 b | 5.5 ± 2.9 c |
| Vitamin C, mg | 53.1 ± 42.2 | 48.5 ± 46.3 a | 44.5 ± 30.0 b | 67.7 ± 43.5 c |
| Vitamin E, mg | 9.2 ± 4.7 | 8.7 ± 4.3 a | 8.4 ± 4.3 b | 10.8 ± 5.0 c |
| Folic acid, µg | 164.7 ± 114.4 | 135.6 ± 77.7 a | 147.3 ± 118.6 b | 221.3 ± 131.7 c |
| β-carotene, µg | 2499.8 ± 2035.0 | 1883.0 ± 1252.3 a | 2104.0 ± 1437.1 b | 3727.7 ± 2761.1 c |
| K-MEDAS Questions | FFQ * | Kappa | ICC |
|---|---|---|---|
| Q1. Do you usually use perilla oil or olive oil when cooking? | 1 point given based on use of perilla oil or olive oil when cooking † | 0.676 (0.517, 0.783) | N/A |
| Q2. How much perilla oil or olive oil do you consume per day? | n/a | - | - |
| Q3. How many vegetables do you eat per day? | 1 point given based on FFQ calculation, if ≥3 portions of vegetables per day | 0.426 (0.143, 0.615) | N/A |
| Q4. How many fruits do you eat per day? | 1 point given based on FFQ calculation, if ≥2 portions of fruits per day | 0.528 (0.296, 0.684) | N/A |
| Q5. How much of red meat (i.e., beef, pork, etc.) and processed meat (ham, sausage, etc.) do you consume per day? | 1 point given based on FFQ calculation, if <2 portions of red meat and processed meats per day | 0.194 (−0.203, 0.460) | N/A |
| Q6. How much butter, margarine, and cream did you consume per day? | 1 point given based on FFQ calculation, if <1 portion of butter and margarine per day | 0.664 (0.498, 0.775) | N/A |
| Q7. How many drinks that contain sugar do you drink per day (carbonated drinks, juices, processed drinks, etc.)? | 1 point given based on FFQ calculation, if <1 portion of soft drinks per day | 0.595 (0.395, 0.728) | N/A |
| Q8. How much wine do you consume per week? | 1 point given based on FFQ calculation, if ≥7 cups of wine per week | N/A | N/A |
| Q9. How much did you consume beans or tofu per week? | 1 point given based on FFQ calculation, if ≥3 portions of beans and tofu per week | 0.613 (0.422, 0.740) | N/A |
| Q10. How much fish or seafood did you consume per week? | 1 point given based on FFQ calculation, if ≥3 portions of fish and seafood per week | 0.273 (−0.085, 0.513) | N/A |
| Q11. How many times do you consume sweets (chocolate, candy, ice cream, snacks), breads (except whole wheat bread), cakes, and cookies per week? | 1 point given based on FFQ calculation, if <2 times of sweets, cakes, cookies, and breads per week | 0.707 (0.563, 0.804) | N/A |
| Q12. How many times do you consume nut products per week? | 1 point given based on FFQ calculation, if ≥3 times of nuts per week | 0.876 (0.815, 0.917) | N/A |
| Q13. Do you have a higher preference to consume white meat (chicken breasts, etc.) rather than red meat (beef, pork, etc.) and processed meat (ham, sausage, etc.)? | 1 point given based on FFQ calculation, if consumption frequency of poultry and chicken > those of red meat and processed meat. | 0.386 (0.084, 0.589) | N/A |
| Q14. How many times do you consume whole grains (multi-grain rice, rye bread, etc.) per week? | 1 point given based on FFQ calculation, if ≥3 times of whole grains per week | 0.851 (0.777, 0.900) | N/A |
| Total scores | NA | 0.678(0.520,0.785) |
| General Population | High Risk Group | |||||||
|---|---|---|---|---|---|---|---|---|
| Dependent Variables | Beta | 95% CI | p-Value | Beta | 95% CI | p-Value | ||
| Total cholesterol | −4.838 | −0.7482 | −2.194 | <0.001 | −5.640 | −10.224 | −1.055 | 0.017 |
| LDL cholesterol | −2.558 | −5.584 | −0.723 | 0.011 | −5.373 | −9.507 | −1.239 | 0.012 |
| Non-HDL-C | −3.993 | −6.588 | −1.398 | 0.003 | −6.470 | −10.915 | −2.026 | 0.005 |
| Triglyceride | −3.417 | −7.591 | 0.757 | 0.108 | −6.641 | −14.434 | 1.152 | 0.094 |
| HDL-cholesterol | −0.845 | −1.701 | 0.012 | 0.053 | 0.830 | −0.987 | 2.648 | 0.365 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kwon, Y.-J.; Lee, H.; Yoon, Y.; Kim, H.M.; Chu, S.H.; Lee, J.-W. Development and Validation of a Questionnaire to Measure Adherence to the Mediterranean Diet in Korean Adults. Nutrients 2020, 12, 1102. https://doi.org/10.3390/nu12041102
Kwon Y-J, Lee H, Yoon Y, Kim HM, Chu SH, Lee J-W. Development and Validation of a Questionnaire to Measure Adherence to the Mediterranean Diet in Korean Adults. Nutrients. 2020; 12(4):1102. https://doi.org/10.3390/nu12041102
Chicago/Turabian StyleKwon, Yu-Jin, Hyangkyu Lee, Yooeun Yoon, Hyung Mi Kim, Sang Hui Chu, and Ji-Won Lee. 2020. "Development and Validation of a Questionnaire to Measure Adherence to the Mediterranean Diet in Korean Adults" Nutrients 12, no. 4: 1102. https://doi.org/10.3390/nu12041102
APA StyleKwon, Y.-J., Lee, H., Yoon, Y., Kim, H. M., Chu, S. H., & Lee, J.-W. (2020). Development and Validation of a Questionnaire to Measure Adherence to the Mediterranean Diet in Korean Adults. Nutrients, 12(4), 1102. https://doi.org/10.3390/nu12041102





