Create Our Own Kai: A Randomised Control Trial of a Cooking Intervention with Group Interview Insights into Adolescent Cooking Behaviours
Abstract
1. Introduction
2. Materials and Methods
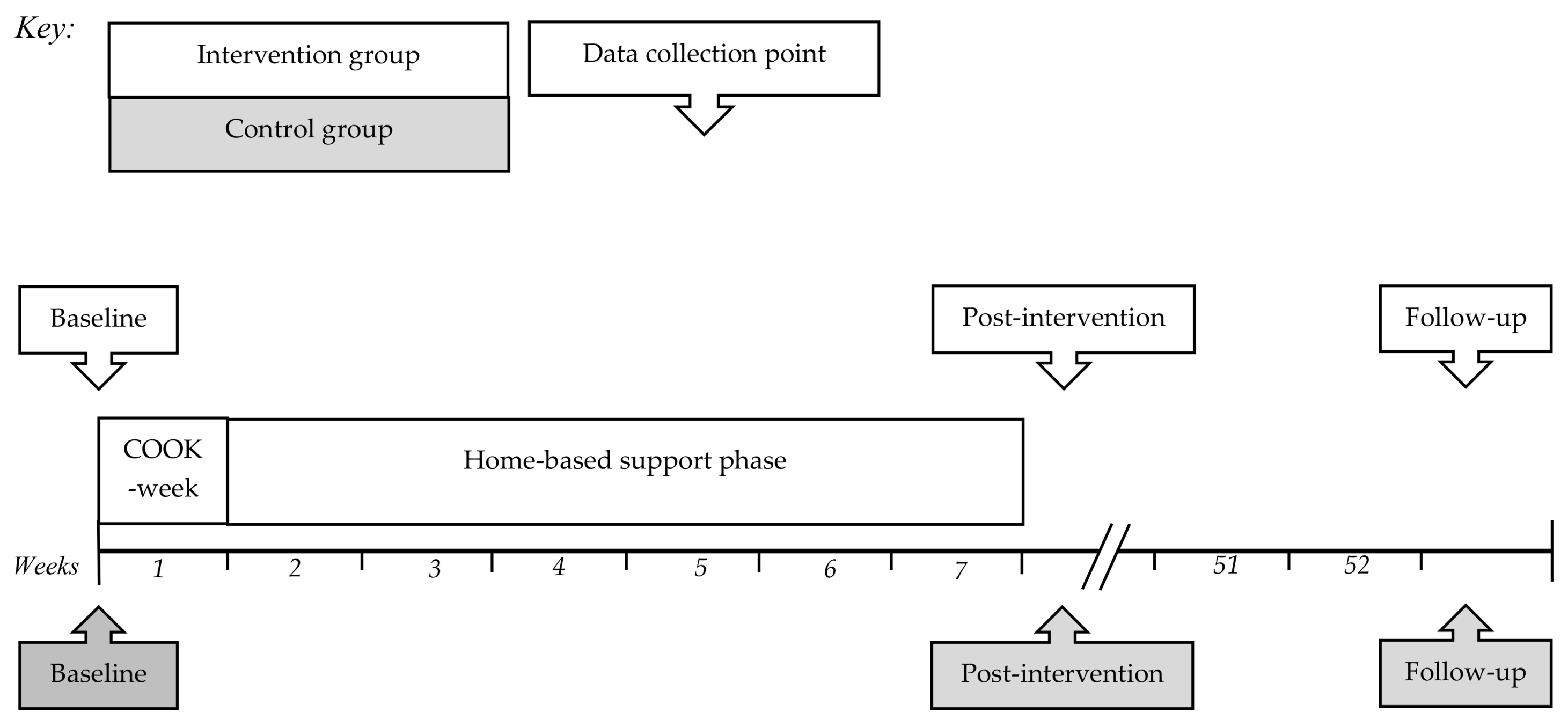
2.1. Study Design
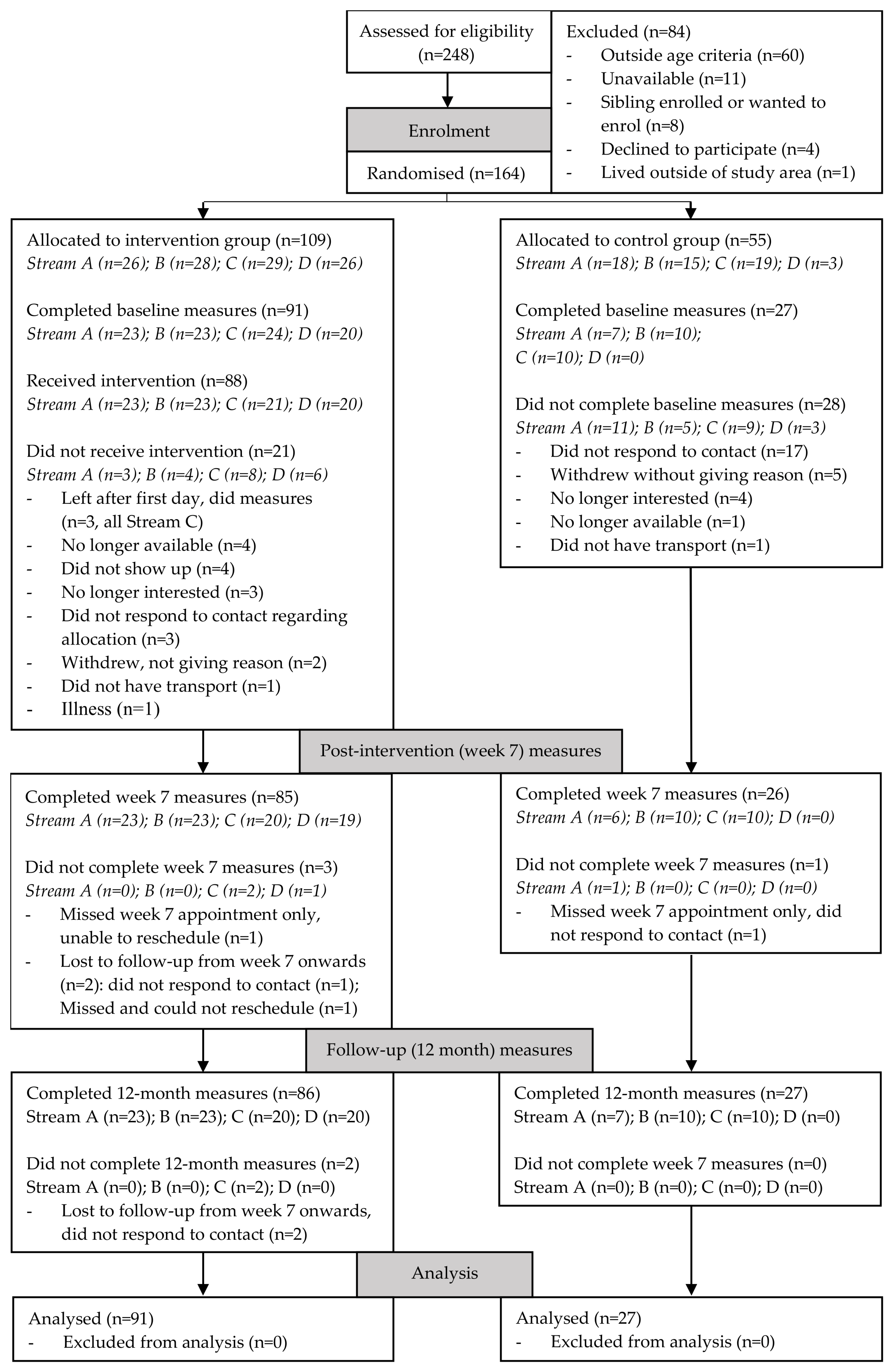
2.2. Recruitment and Allocation
2.3. Intervention Part 1: COOK Week
2.4. Intervention Part 2: Support Phase
2.5. Data Collection
2.6. Questionnaires
2.7. Anthropometry
2.8. Data Entry and Statistics
2.9. Group Interviews
3. Results
3.1. Participant Summary
3.2. Postintervention and Follow-up Results
3.3. Group Interviews
3.3.1. Intervention Experience and Perceived Changes
3.3.2. Adolescent Cooking Practices
3.3.3. Cooking from an Adolescent’s Perspective
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Condrasky, M.D.; Hegler, M. How culinary nutrition can save the health of a nation. J. Ext. 2010, 48, 1–6. [Google Scholar]
- Fertig, A.R.; Loth, K.A.; Trofholz, A.C.; Tate, A.D.; Miner, M.; Neumark-Sztainer, D.; Berge, J.M. Compared to Pre-prepared Meals, Fully and Partly Home-Cooked Meals in Diverse Families with Young Children Are More Likely to Include Nutritious Ingredients. J. Acad. Nutr. Diet. 2019, 119, 818–830. [Google Scholar] [CrossRef] [PubMed]
- Guthrie, J.F.; Lin, B.-H.; Frazao, E. Role of Food Prepared Away from Home in the American Diet, 1977–78 versus 1994–96: Changes and Consequences. J. Nutr. Educ. Behav. 2002, 34, 140–150. [Google Scholar] [CrossRef]
- Wolfson, J.A.; Bleich, S.N. Is cooking at home associated with better diet quality or weight-loss intention? Public Health Nutr. 2015, 18, 1397–1406. [Google Scholar] [CrossRef] [PubMed]
- Quelly, S.B. Helping with Meal Preparation and Children’s Dietary Intake: A Literature Review. J. Sch. Nurs. 2019, 35, 51–60. [Google Scholar] [CrossRef]
- Cherry, A.L.; Baltag, V.; Dillon, M.E. The epidemiology of adolescent health. In International Handbook on Adolescent Health and Development; Cherry, A.L., Baltag, V., Dillon, M.E., Eds.; Springer International Publishing: Cham, Switzerland, 2017; pp. 3–14. [Google Scholar]
- Bandura, A. Health promotion from the perspective of social cognitive theory. Psychol. Health 1998, 13, 623–649. [Google Scholar] [CrossRef]
- Lichtenstein, A.H.; Ludwig, D.S. Bring back home economics education. JAMA 2010, 303, 1857–1858. [Google Scholar] [CrossRef]
- Lang, T.; Caraher, M. Is there a culinary skills transition? Data and debate from the UK about changes in cooking culture. J. HEIA 2001, 8, 2–14. [Google Scholar]
- Caraher, M.; Lang, T. Can’t cook, won’t cook: A review of cooking skills and their relevance to health promotion. Int. J. Health Promot. Educ. 1999, 37, 89–100. [Google Scholar] [CrossRef]
- Utter, J.; Fay, A.P.; Denny, S. Child and Youth Cooking Programs: More Than Good Nutrition? J. Hunger Environ. Nutr. 2016. [Google Scholar] [CrossRef]
- Sawyer, S.M.; Afifi, R.A.; Bearinger, L.H.; Blakemore, S.-J.; Dick, B.; Ezeh, A.C.; Patton, G.C. Adolescence: A foundation for future health. Lancet 2012, 379, 1630–1640. [Google Scholar] [CrossRef]
- Beets, M.W.; Swanger, K.; Wilcox, D.R.; Cardinal, B.J. Using Hands-on Demonstrations to Promote Cooking Behaviors with Young Adolescents: The Culinary Camp Summer Cooking Program. J. Nutr. Educ. Behav. 2007, 39, 288–289. [Google Scholar] [CrossRef] [PubMed]
- Bierlich-Wesch, J.R. Pink and Dude Chefs: Impact of A Nutrition and Culinary Education Program with Middle School Students in an Afterschool Setting. Master’s Thesis, California Polytechnic State University, San Luis Obispo, CA, USA, 2016. [Google Scholar]
- Black, K.; Thomson, C.; Chryssidis, T.; Finigan, R.; Hann, C.; Jackson, R.; Robinson, C.; Toldi, O.; Skidmore, P. Pilot testing of an intensive cooking course for New Zealand adolescents: The create-our-own kai study. Nutrients 2018, 10, 556. [Google Scholar] [CrossRef] [PubMed]
- Chessen, J.A. The Development and Pilot of a Culinary Intervention Designed Using the Social Cognitive Theory to Teach Nutrition to Adolescent Girls. Master’s Thesis, California Polytechnic State University, San Luis Obispo, CA, USA, 2009. [Google Scholar]
- Condrasky, M.; Quinn, A.; Cason, K. Cooking camp provides hands-on nutrition education opportunity. J. Culin. Sci. Technol. 2007, 5, 37–52. [Google Scholar] [CrossRef]
- Meehan, M.; Yeh, M.-C.; Spark, A. Impact of exposure to local food sources and food preparation skills on nutritional attitudes and food choices among urban minority youth. J. Hunger Environ. Nutr. 2008, 3, 456–471. [Google Scholar] [CrossRef]
- Pierce, B.; Bowden, B.; McCullagh, M.; Diehl, A.; Chissell, Z.; Rodriguez, R.; Berman, B.M.; D’Adamo, C.R. A Summer Health Program for African-American High School Students in Baltimore, Maryland: Community Partnership for Integrative Health. Explor. J. Sci. Heal. 2017, 13, 186–197. [Google Scholar] [CrossRef]
- Sheehan, T.R. Pink and Dude Chefs: A Nutrition and Culinary Intervention for Middle School Students. Master’s Thesis, California Polytechnic State University, San Luis Obispo, CA, USA, 2013. [Google Scholar]
- Thomas, H.M.; Irwin, J.D. Cook It Up! Formative evaluation of a community-based cooking program for at-risk youth in London, Ontario. Int. J. Home Econ. 2012, 5, 64. [Google Scholar]
- Brown, B.J.; Hermann, J.R. Cooking Classes Increase Fruit and Vegetable Intake and Food Safety Behaviors in Youth and Adults. J. Nutr. Educ. Behav. 2005, 37, 104–105. [Google Scholar] [CrossRef]
- Condrasky, M.D.; Corr, A.Q.; Sharp, J.; Hegler, M.; Warmin, A. Culinary nutrition camp for adolescents assisted by dietetic student counselors. Top. Clin. Nutr. 2010, 25, 362–370. [Google Scholar] [CrossRef]
- Gatenby, L.; Donnelly, J.; Connell, R. Cooking Communities: Using multicultural after-school cooking clubs to enhance community cohesion. Nutr. Bull. 2011, 36, 108–112. [Google Scholar] [CrossRef]
- Santarossa, S.; Ciccone, J.; Woodruff, S.J. An evaluation of the Kinect-Ed presentation, a motivating nutrition and cooking intervention for young adolescents in grades 6–8. Appl. Physiol. Nutr. Metab. 2015, 40, 945–950. [Google Scholar] [CrossRef] [PubMed]
- Utter, J.; Denny, S.; Farrant, B.; Cribb, S. Feasibility of a Family Meal Intervention to Address Nutrition, Emotional Wellbeing, and Food Insecurity of Families with Adolescents. J. Nutr. Educ. Behav. 2019. [Google Scholar] [CrossRef] [PubMed]
- D’Adamo, C.R.; McArdle, P.F.; Balick, L.; Peisach, E.; Ferguson, T.; Diehl, A.; Bustad, K.; Bowden, B.; Pierce, B.A.; Berman, B.M. Spice MyPlate: Nutrition Education Focusing Upon Spices and Herbs Improved Diet Quality and Attitudes Among Urban High School Students. Am. J. Health Promot. 2016, 30, 346–356. [Google Scholar] [CrossRef] [PubMed]
- Jaenke, R.L.; Collins, C.E.; Morgan, P.J.; Lubans, D.R.; Saunders, K.L.; Warren, J.M. The Impact of a School Garden and Cooking Program on Boys’ and Girls’ Fruit and Vegetable Preferences, Taste Rating, and Intake. Health Educ. Behav. 2012, 39, 131–141. [Google Scholar] [CrossRef] [PubMed]
- McAleese, J.D.; Rankin, L.L. Garden-based nutrition education affects fruit and vegetable consumption in sixth-grade adolescents. J. Am. Diet. Assoc. 2007, 107, 662–665. [Google Scholar] [CrossRef]
- Harley, A.; Lemke, M.; Brazauskas, R.; Carnegie, N.B.; Bokowy, L.; Kingery, L. Youth Chef Academy: Pilot Results From a Plant-Based Culinary and Nutrition Literacy Program for Sixth and Seventh Graders. J. Sch. Health 2018, 88, 893–902. [Google Scholar] [CrossRef]
- Oakley, A.R.; Nelson, S.A.; Nickols-Richardson, S.M. Peer-Led Culinary Skills Intervention for Adolescents: Pilot Study of the Impact on Knowledge, Attitude, and Self-efficacy. J. Nutr. Educ. Behav. 2017, 49, 852–857. [Google Scholar] [CrossRef][Green Version]
- Revill, S.A. Evaluation of a School-Based Nutrition and Food Preparation Skills Intervention Delivered to Schoolchildren from Deprived Social Backgrounds. Ph.D. Thesis, Newcastle University, Newcastle, UK, 2004. [Google Scholar]
- Farmer, N.; Touchton-Leonard, K.; Ross, A. Psychosocial Benefits of Cooking Interventions: A Systematic Review. Health Educ. Behav. 2018, 45, 167–180. [Google Scholar] [CrossRef]
- Utter, J.; Denny, S.; Lucassen, M.; Dyson, B. Adolescent cooking abilities and behaviors: Associations with nutrition and emotional well-being. J. Nutr. Educ. Behav. 2016, 48, 35–41. [Google Scholar] [CrossRef]
- Patton, G.C.; Viner, R. Pubertal transitions in health. Lancet 2007, 369, 1130–1139. [Google Scholar] [CrossRef]
- Lai Yeung, W. A study of perceptions of food preparation skills in Hong Kong adolescents. HEIA J. 2007, 14, 16–24. [Google Scholar]
- Lai-Yeung, T.W.L. Hong Kong parents’ perceptions of the transference of food preparation skills. Int. J. Consum. Stud. 2015, 39, 117–124. [Google Scholar] [CrossRef]
- Hyland, R.; Stacy, R.; Adamson, A.; Moynihan, P. Nutrition-related health promotion through an after-school project: The responses of children and their families. Soc. Sci. Med. 2006, 62, 758–768. [Google Scholar] [CrossRef] [PubMed]
- Utter, J.; Denny, S. Supporting Families to Cook at Home and Eat Together: Findings From a Feasibility Study. J. Nutr. Educ. Behav. 2016, 48, 716–722. [Google Scholar] [CrossRef] [PubMed]
- Harmon, B.E.; Smith, N.; Pirkey, P.; Beets, M.W.; Blake, C.E. The impact of culinary skills training on the dietary attitudes and behaviors of children and parents. Am. J. Health Educ. 2015, 46, 283–292. [Google Scholar] [CrossRef]
- Fitzgerald, A.; Heary, C.; Nixon, E.; Kelly, C. Factors influencing the food choices of Irish children and adolescents: A qualitative investigation. Health Promot. Int. 2010, 25, 289–298. [Google Scholar] [CrossRef]
- Bassett, R.; Chapman, G.E.; Beagan, B.L. Autonomy and control: The co-construction of adolescent food choice. Appetite 2008, 50, 325–332. [Google Scholar] [CrossRef]
- Holsten, J.E.; Deatrick, J.A.; Kumanyika, S.; Pinto-Martin, J.; Compher, C.W. Children’s food choice process in the home environment. A qualitative descriptive study. Appetite 2012, 58, 64–73. [Google Scholar] [CrossRef]
- Tyrrell, R.L.; Townshend, T.G.; Adamson, A.J.; Lake, A.A. ‘I’m not trusted in the kitchen’: Food environments and food behaviours of young people attending school and college. J. Public Health 2016, 38, 289–299. [Google Scholar] [CrossRef]
- Stevenson, C.; Doherty, G.; Barnett, J.; Muldoon, O.T.; Trew, K. Adolescents’ views of food and eating: Identifying barriers to healthy eating. J. Adolesc. 2007, 30, 417–434. [Google Scholar] [CrossRef]
- Thomas, H.C.; Irwin, J.D. Using Photovoice with At-risk Youth: In a Community-based Cooking Program. Can. J. Diet. Pract. Res. 2013, 74, 14–20. [Google Scholar] [CrossRef] [PubMed]
- Manaakitanga Tikanga Related to Food Healthy Kai. Available online: https://bpac.org.nz/BPJ/2008/August/tikanga.aspx (accessed on 18 May 2019).
- Health, M.O. Ethnicity Data Protocols for the Health and Disability Sector; Ministry of Health: Wellington, New Zealand, 2004.
- Atkinson, J.; Salmond, C.; Crampton, P. NZDep2013 Index of Deprivation; Department of Public Health, University of Otago: Wellington, New Zealand, 2014. [Google Scholar]
- Topp, C.W.; Østergaard, S.D.; Søndergaard, S.; Bech, P. The WHO-5 Well-Being Index: A Systematic Review of the Literature. Psychother. Psychosom. 2015, 84, 167–176. [Google Scholar] [CrossRef] [PubMed]
- Wong, J.E.; Parnell, W.R.; Black, K.E.; Skidmore, P.M. Reliability and relative validity of a food frequency questionnaire to assess food group intakes in New Zealand adolescents. Nutr. J. 2012, 11, 65. [Google Scholar] [CrossRef] [PubMed]
- Wong, J.E.; Parnell, W.R.; Howe, A.S.; Black, K.E.; Skidmore, P.M. Development and validation of a food-based diet quality index for New Zealand adolescents. BMC Public Health 2013, 13, 562. [Google Scholar] [CrossRef]
- Larson, N.I.; Story, M.; Eisenberg, M.E.; Neumark-Sztainer, D. Food Preparation and Purchasing Roles among Adolescents: Associations with Sociodemographic Characteristics and Diet Quality. J. Am. Diet. Assoc. 2006, 106, 211–218. [Google Scholar] [CrossRef]
- Barton, K.L.; Wrieden, W.L.; Anderson, A.S. Validity and reliability of a short questionnaire for assessing the impact of cooking skills interventions. J. Hum. Nutr. Diet. 2011, 24, 588–595. [Google Scholar] [CrossRef]
- Condrasky, M.D.; Williams, J.E.; Catalano, P.M.; Griffin, S.F. Development of Psychosocial Scales for Evaluating the Impact of a Culinary Nutrition Education Program on Cooking and Healthful Eating. J. Nutr. Educ. Behav. 2011, 43, 511–516. [Google Scholar] [CrossRef]
- Survey, N.D.A.N. NDNS Year 1 Questionnaires, Showcards, Consent Booklets. Available online: http://doc.ukdataservice.ac.uk/doc/6533/mrdoc/pdf/6533_ndns_yrl_interviewing_documents.pdf (accessed on 7 December 2018).
- De Onis, M.; Onyango, A.W.; Borghi, E.; Siyam, A.; Nishida, C.; Siekmann, J. Development of a WHO growth reference for school-aged children and adolescents. Bull. World Health Organ. 2007, 85, 660–667. [Google Scholar] [CrossRef]
- World Health Organization. Wellbeing measures in primary health care/the DEPCARE project: Report on a WHO meeting, Stockholm, Sweden, 12–13 February 1998. In Proceedings of the Wellbeing Measures in Primary Health Care/the DEPCARE Project: Report on a WHO Meeting, Stockholm, Sweden, 12–13 February 1998. [Google Scholar]
- Currie, C.; Zanotti, C.; Morgan, A.; Currie, D.; Looze, M.d.; Roberts, C.; Samdal, O.; Smith, O.; Barnekow, V. Social determinants of health and well-being among young people. In Health Behaviour in School-Aged Children (HBSC) Study: International Report from the 2009/2010 Survey; World Health Organisation: Copenhagen, Denmark, 2012. [Google Scholar]
- Denissen, J.J.; Penke, L.; Schmitt, D.P.; Van Aken, M.A. Self-esteem reactions to social interactions: Evidence for sociometer mechanisms across days, people, and nations. J. Personal. Soc. Psychol. 2008, 95, 181. [Google Scholar] [CrossRef]
- Hasan, B.; Thompson, W.G.; Almasri, J.; Wang, Z.; Lakis, S.; Prokop, L.J.; Hensrud, D.D.; Frie, K.S.; Wirtz, M.J.; Murad, A.L.; et al. The effect of culinary interventions (cooking classes) on dietary intake and behavioral change: A systematic review and evidence map. BMC Nutr. 2019, 5, 29. [Google Scholar] [CrossRef]
- Neumark-Sztainer, D.; Wall, M.; Perry, C.; Story, M. Correlates of fruit and vegetable intake among adolescents: Findings from Project EAT. Prev. Med. 2003, 37, 198–208. [Google Scholar] [CrossRef]
- World Health Organisation. Growth Reference Data for 5–19 Years. 2007. Available online: https://www.who.int/growthref/en/ (accessed on 25 October 2019).
- Utter, J.; Denny, S.; Lucassen, M.; Dyson, B. Cooking and the health and wellbeing of adolescents. J. Nutr. Educ. Behav. 2016, 48, 35–41. [Google Scholar] [CrossRef] [PubMed]
- Wansink, B.; Kleef, E. Dinner rituals that correlate with child and adult BMI. Obesity 2013, 22, E91–E95. [Google Scholar] [CrossRef] [PubMed]
- Davis, J.N.; Ventura, E.E.; Cook, L.T.; Gyllenhammer, L.E.; Gatto, N.M. LA Sprouts: A Gardening, Nutrition, and Cooking Intervention for Latino Youth Improves Diet and Reduces Obesity. J. Am. Diet. Assoc. 2011, 111, 1224–1230. [Google Scholar] [CrossRef]
- White, A.A.; Colby, S.E.; Franzen-Castle, L.; Kattelmann, K.K.; Olfert, M.D.; Gould, T.A.; Hagedorn, R.L.; Mathews, D.R.; Moyer, J.; Wilson, K.; et al. The iCook 4-H Study: An Intervention and Dissemination Test of a Youth/Adult Out-of-School Program. J. Nutr. Educ. Behav. 2019, 51, S2–S20. [Google Scholar] [CrossRef]
- Herbert, J.; Flego, A.; Gibbs, L.; Waters, E.; Swinburn, B.; Reynolds, J.; Moodie, M. Wider impacts of a 10-week community cooking skills program—Jamie’s Ministry of Food, Australia. BMC Public Health 2014, 14, 1161. [Google Scholar] [CrossRef]
| Control Group (n = 27) | Intervention Group (n = 91) | |
|---|---|---|
| Age (years), mean (SD) | 14.3 (0.7) | 14.1 (0.8) |
| Sex (female), n (%) | 21 (78) | 55 (60) |
| Ethnicity, n (%) | ||
| Māori | 4 (15) | 13 (14) |
| Pacific | 0 (0) | 0 (0) |
| New Zealand European and Other | 23 (85) | 78 (86) |
| Socio-economic status a, n (%) | ||
| Low (NZDep 8–10) | 4 (15) | 12 (13) |
| Medium (NZDep 4–7) | 8 (30) | 39 (43) |
| High (NZDep 1–3) | 15 (56) | 40 (47) |
| Weight status c,d, n (%) | ||
| Healthy weight | 16 (59) | 55 (63) |
| Overweight | 7 (26) | 23 (26) |
| Obese | 4 (15) | 10 (11) |
| BMI z-score b, mean (SD) | 0.7 (1.2) | 0.4 (1.2) |
| Control Group | Intervention Group | Mean Difference | p-Value | |||
|---|---|---|---|---|---|---|
| n | Mean (SD) | n | Mean (SD) | (95% CI) a | ||
| Mental well-being b | ||||||
| Baseline | 27 | 65 (14) | 90 | 69 (19) | ||
| Change at 7 weeks | 26 | −1 (14) | 84 | 1 (19) | 3 (1, 5) | 0.005 |
| Change at 12 months | 27 | −2 (17) | 85 | −4 (21) | −1 (−10, 7) | 0.762 |
| Diet quality c | ||||||
| Baseline | 26 | 57 (14) | 88 | 60 (14) | ||
| Change at 7 weeks | 26 | −2 (12) | 82 | 2 (13) | 4 (0.2, 8) | 0.041 |
| Change at 12 months | 26 | −2 (9) | 81 | −2 (13) | 1 (−5, 7) | 0.751 |
| BMI z-score d | ||||||
| Change at 7 weeks | 26 | 0.00 (0.18) | 85 | 0.07 (0.17) | 0.08 (0.02, 0.14) | 0.006 |
| Change at 12 months | 27 | 0.05 (0.44) | 85 | 0.07 (0.40) | 0.02 (−0.002, 0.04) | 0.076 |
| Control Group | Intervention Group | Mean Difference | p-Value | |||
|---|---|---|---|---|---|---|
| n | Mean (SD) | n | Mean (SD) | (95% CI) a | ||
| Helps with dinner, times/week | ||||||
| Baseline, median (25th, 75th percentile) | 26 | 1 (0, 2) | 88 | 1 (0.5, 2) | ||
| Change at 7 weeks | 25 | 0.4 (1.5) | 82 | 0.7 (1.5) | 0.4 (0.1, 0.6) | 0.001 |
| Change at 12 months | 26 | 0.1 (1.0) | 82 | 0.2 (1.3) | 0.1 (−0.1, 0.3) | 0.455 |
| Cooks main meal, times/week | ||||||
| Baseline, median (25th, 75th percentile) | 27 | 0.5 (0.5, 1) | 91 | 0.5 (0, 1) | ||
| Change at 7 weeks | 26 | 0.5 (0.8) | 84 | 0.7 (1.7) | 0.2 (−0.6, 0.9) | 0.646 |
| Change at 12 months | 27 | 0.3 (1.0) | 86 | 0.2 (1.7) | 0.0 (−0.4, 0.4) | 0.931 |
| Self-efficacy for specific cooking tasks & techniques b | ||||||
| Baseline | 27 | 63 (21) | 91 | 53 (17) | ||
| Change at 7 weeks | 26 | −1 (12) | 85 | 26 (15) | 28 (17, 38) | <0.001 |
| Change at 12 months | 27 | 2 (16) | 86 | 22 (17) | 19 (12, 26) | <0.001 |
| General cooking self-efficacy b | ||||||
| Baseline | 27 | 66 (16) | 91 | 64 (17) | ||
| Change at 7 weeks | 26 | 2 (10) | 85 | 16 (13) | 15 (12, 18) | <0.001 |
| Change at 12 months | 27 | 4 (13) | 86 | 12 (16) | 9 (5, 7) | <0.001 |
| Positive cooking attitude b | ||||||
| Baseline | 27 | 67 (19) | 91 | 69 (17) | ||
| Change at 7 weeks | 26 | −3 (10) | 85 | 8 (14) | 11 (7, 15) | 0.001 |
| Change at 12 months | 27 | −2 (17) | 86 | −1 (17) | 2 (−1, 5) | 0.278 |
| Factor | Summary | Comments |
|---|---|---|
| Feeling like it | Participants mostly cooked when they were asked to, although they did volunteer to cook sometimes as well. Often participants were asked to cook when they did not feel like it. | A reason some did feel like cooking was that this meant they could choose what they felt like eating for the meal. However, this factor was seldom mentioned, possibly because most participants could not choose the meal (see below). Reasons participants may not feel like cooking included being tired, having other things they wanted or needed to do, or disliking being interrupted from something they were already doing. |
| Choosing what to cook | Although the decision for what to cook for the family might be influenced by what participants felt like, it was ultimately bound by:
Most participants felt they had more choice when cooking for themselves, as they need not accommodate others’ preferences. | Meals were often based on leftovers or fresh foods that needed using (“anything in the fridge”), although some participants had input into grocery purchase decisions (“if I’ve got an idea that I wanna cook and stuff, I’ll give them what I want them to buy and if they’ve got the money they’ll get it”). Virtually all participants said family dishes were constrained by what others would eat, particularly siblings. Parents ensured suitable choices by telling participants what to make or vetting their choice. Most participants agreed “getting told is a lot easier” than choosing what to cook for the family, as finding something they both had ingredients for and everyone would eat was difficult, and frustrating if they could not make what they wanted. Only a few participants preferred to choose what to cook, because “then I know I’ll get to eat it when I when I’m done and it’s nice”. Those who had tried commercial meal kit services appreciated the straightforwardness of having the choice made for them and ingredients and recipes provided. Although most participants felt they had more choice when cooking for themselves only, it was unclear how much freedom was actually exercised, given their convenience requirements and the limited range of foods they described making most often (e.g., noodles, toast). |
| Effort required | Participants generally wanted to cook something quick and easy. Cooking for the family often involved greater effort than cooking for themselves. | Some felt they put “about the same amount” of effort into cooking for themselves versus for others. One participant even used cooking for them self as an opportunity to experiment. Other participants had a stronger convenience orientation when cooking for themselves (“when I’m cooking for myself it’s generally a lot quicker because I got other things to do and, like, I’m hungry, I need to get something quick, done and then get back to doing whatever I want”). Cooking a family meal often meant more time and effort, particularly with presentation (“well if it looks good they’re gonna eat it, it makes sense!”), and for some constituted an “actual meal”. |
| Cooking the food | Some participants described enjoying alone time, autonomy and creativity while cooking. Less enjoyable aspects were the time it takes. Cooking was easier when there were clear instructions and family members cooperated. | Enjoyable aspects of cooking were having some alone time and exercising control over their environment, which included playing their choice of music or having some quiet. In some cases, being the cook endowed authority to tell others to go away (“[I’m] independent and bossy!”). One participant described a sense of achievement when cooking, while others enjoyed getting creative, especially with presentation. Dislikes included long repetitive tasks like chopping, which could be boring, using an unreliable oven, and being stuck looking after food (“yeah waiting for things to cook and cus’ you just want to go off and do something else but if you do that you might forget and you’ll burn, boil over or whatever”). Some participants had help from family, particularly when cooking for lots of people or when things were not going well, such as peeling and cutting, verbal direction and sometimes stirring. Cooking was easier with clear instructions on how long to cook something, rather than having to guess, and if family members were helpful or well-behaved if they came into the kitchen. |
| Family responses | Positive family responses showed support, appreciation, enjoyment, and helping. Family appreciation could also make participants feel self-conscious. Family members (particularly siblings) who disliked or refused to eat food was a barrier. | Positive family reactions included parents being appreciative and supportive, and siblings enjoying the food. Other positive behaviours were family members being cooperative during cooking, either by staying out of the way or assisting, and helping clean up. Some participants described feeling awkward when family members made a big deal of them cooking (Participant: “Um I think if its someone other than mum cooking they feel pressure to be extra nice about it.” Facilitator: “Does that perception that they are trying to be extra nice make you feel better or worse?” Participant: “No, I find it off-putting”). The most common complaint relating to families was siblings not liking or refusing to eat what participants had cooked. |
| Cleaning up | Cleaning up was the most common dislike about cooking. Cooking family meals did not usually mean being “off” dishes—in many cases it guaranteed another chore. | Some participants had to clean anything they dirtied (“everything in my house is kinda if you make a mess then you have to clean it up”). For others, whether they cooked was unrelated to whether they did dishes, as they always did dishes anyway or took turns with siblings. Arrangements where the person who cooks does not do dishes were a minority, and included participants doing dishes as they go but someone else doing the big pots at the end. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kuroko, S.; Black, K.; Chryssidis, T.; Finigan, R.; Hann, C.; Haszard, J.; Jackson, R.; Mahn, K.; Robinson, C.; Thomson, C.; et al. Create Our Own Kai: A Randomised Control Trial of a Cooking Intervention with Group Interview Insights into Adolescent Cooking Behaviours. Nutrients 2020, 12, 796. https://doi.org/10.3390/nu12030796
Kuroko S, Black K, Chryssidis T, Finigan R, Hann C, Haszard J, Jackson R, Mahn K, Robinson C, Thomson C, et al. Create Our Own Kai: A Randomised Control Trial of a Cooking Intervention with Group Interview Insights into Adolescent Cooking Behaviours. Nutrients. 2020; 12(3):796. https://doi.org/10.3390/nu12030796
Chicago/Turabian StyleKuroko, Sarahmarie, Katherine Black, Themis Chryssidis, Rosie Finigan, Callum Hann, Jillian Haszard, Rosalie Jackson, Katherine Mahn, Caleb Robinson, Carla Thomson, and et al. 2020. "Create Our Own Kai: A Randomised Control Trial of a Cooking Intervention with Group Interview Insights into Adolescent Cooking Behaviours" Nutrients 12, no. 3: 796. https://doi.org/10.3390/nu12030796
APA StyleKuroko, S., Black, K., Chryssidis, T., Finigan, R., Hann, C., Haszard, J., Jackson, R., Mahn, K., Robinson, C., Thomson, C., Toldi, O., Scullion, N., & Skidmore, P. (2020). Create Our Own Kai: A Randomised Control Trial of a Cooking Intervention with Group Interview Insights into Adolescent Cooking Behaviours. Nutrients, 12(3), 796. https://doi.org/10.3390/nu12030796






