Compliance with the 2018 World Cancer Research Fund/American Institute for Cancer Research Cancer Prevention Recommendations and Prostate Cancer
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Setting
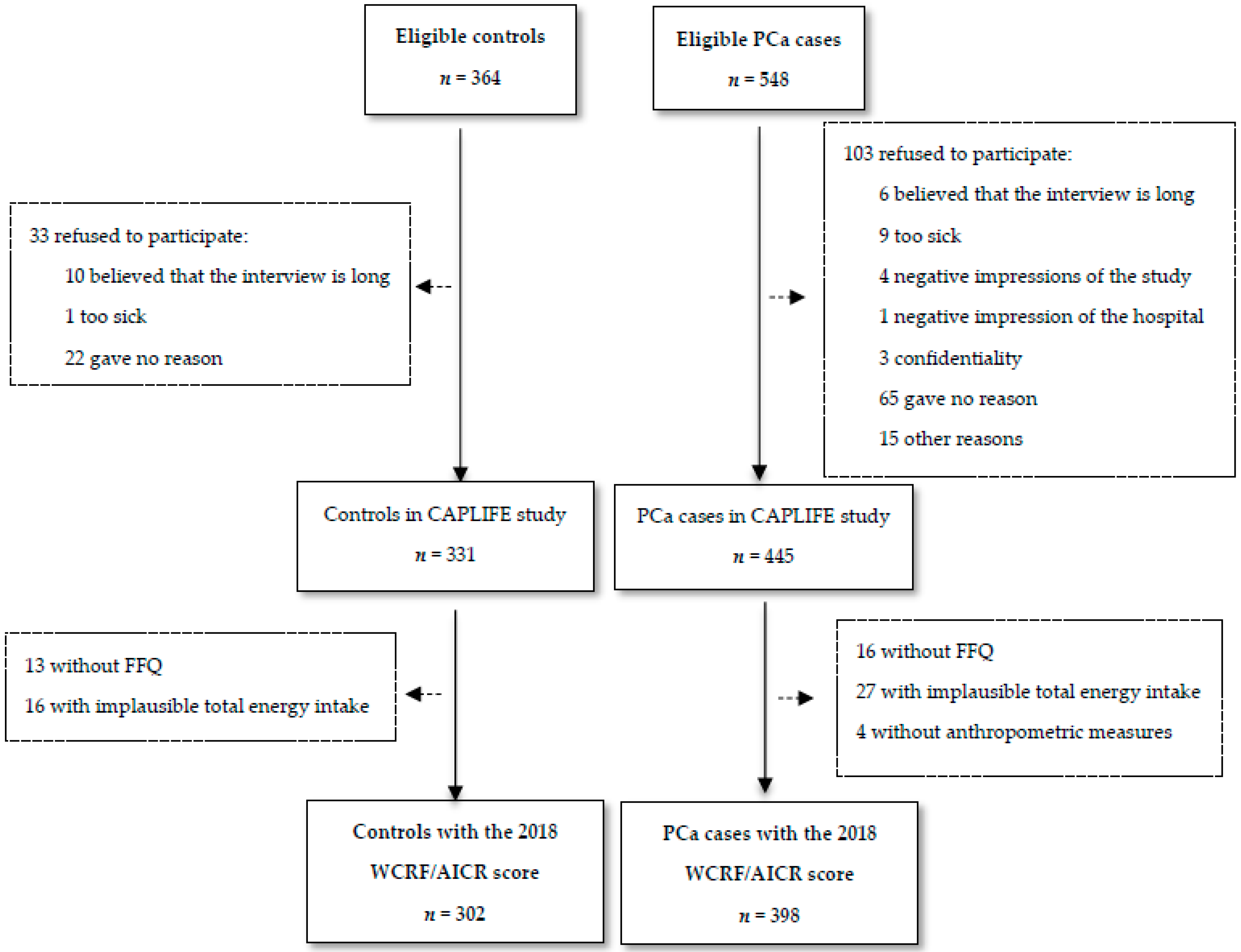
2.2. Participants
2.3. Data Sources and Variables
2.3.1. WCRF/AICR Score Construction
2.3.2. Measurement of Tumor Aggressiveness
2.4. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Bray, F.; Ferlay, J.; Soerjomataram, I.; Siegel, R.L.; Torre, L.A.; Jemal, A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 2018, 68, 394–424. [Google Scholar] [CrossRef] [PubMed]
- Rawla, P. Epidemiology of Prostate Cancer. World J. Oncol. 2019, 10, 63–89. [Google Scholar] [CrossRef] [PubMed]
- Ferlay, J.; Colombet, M.; Soerjomataram, I.; Dyba, T.; Randi, G.; Bettio, M.; Gavin, A.; Visser, O.; Bray, F. Cancer incidence and mortality patterns in Europe: Estimates for 40 countries and 25 major cancers in 2018. Eur. J. Cancer 2018, 103, 356–387. [Google Scholar] [CrossRef] [PubMed]
- Quinn, M.; Babb, P. Patterns and trends in prostate cancer incidence, survival, prevalence and mortality. Part I: International comparisons. BJU Int. 2002, 90, 162–173. [Google Scholar] [CrossRef] [PubMed]
- Eeles, R.A.; Al Olama, A.A.; Benlloch, S.; Saunders, E.J.; Leongamornlert, D.A.; Tymrakiewicz, M.; Ghoussaini, M.; Luccarini, C.; Dennis, J.; Jugurnauth-Little, S.; et al. Identification of 23 new prostate cancer susceptibility loci using the iCOGS custom genotyping array. Nat. Genet. 2013, 45, 385–391. [Google Scholar] [CrossRef] [PubMed]
- Tan, S.-H.; Petrovics, G.; Srivastava, S. Prostate Cancer Genomics: Recent Advances and the Prevailing Underrepresentation from Racial and Ethnic Minorities. Int. J. Mol. Sci. 2018, 19, 1255. [Google Scholar] [CrossRef]
- Chen, H.; Yu, H.; Wang, J.; Zhang, Z.; Gao, Z.; Chen, Z.; Lu, Y.; Liu, W.; Jiang, D.; Zheng, S.L.; et al. Systematic enrichment analysis of potentially functional regions for 103 prostate cancer risk-associated loci. Prostate 2015, 75, 1264–1276. [Google Scholar] [CrossRef]
- Ballon-Landa, E.; Parsons, J.K. Nutrition, physical activity, and lifestyle factors in prostate cancer prevention. Curr. Opin. Urol. 2018, 28, 55–61. [Google Scholar] [CrossRef]
- Papadimitriou, N.; Muller, D.; Van Den Brandt, P.A.; Geybels, M.; Patel, C.J.; Gunter, M.J. A nutrient—Wide association study for risk of prostate cancer in the European Prospective Investigation into Cancer and Nutrition and the Netherlands Cohort Study. Eur. J. Nutr. 2019. [Google Scholar] [CrossRef]
- Markozannes, G.; Tzoulaki, I.; Karli, D.; Evangelou, E.; Ntzani, E.; Gunter, M.J.; Norat, T.; Ioannidis, J.P.; Tsilidis, K.K. Diet, body size, physical activity and risk of prostate cancer: An umbrella review of the evidence. Eur. J. Cancer 2016, 69, 61–69. [Google Scholar] [CrossRef]
- Baena, R.; Salinas, P. Diet and colorectal cancer. Maturitas 2015, 80, 258–264. [Google Scholar] [CrossRef] [PubMed]
- Harvie, M.; Howell, A.; Evans, D.G. Can diet and lifestyle prevent breast cancer: What is the evidence? Am. Soc. Clin. Oncol. Educ. Book Am. Soc. Clin. Oncol. Annu. Meet. 2015, 35, e66–e73. [Google Scholar] [CrossRef] [PubMed]
- Glade, M.J. Food, nutrition, and the prevention of cancer: A global perspective. American Institute for Cancer Research/World Cancer Research Fund, American Institute for Cancer Research, 1997. Nutrition 1999, 15, 523–526. [Google Scholar] [PubMed]
- Wiseman, M. The second World Cancer Research Fund/American Institute for Cancer Research expert report. Food, nutrition, physical activity, and the prevention of cancer: A global perspective. Proc. Nutr. Soc. 2008, 67, 253–256. [Google Scholar] [CrossRef] [PubMed]
- World Cancer Research Fund/American Institute for Cancer Research. Diet, Nutrition, Physical Activity and Cancer: A Global Perspective. Continuous Update Project Expert Report 2018. Available online: http://dietandcancerreport.org (accessed on 11 October 2019).
- Shams-White, M.M.; Brockton, N.T.; Mitrou, P.; Romaguera, D.; Brown, S.; Bender, A.; Kahle, L.L.; Reedy, J. Operationalizing the 2018 World Cancer Research Fund/American Institute for Cancer Research (WCRF/AICR) Cancer Prevention Recommendations: A Standardized Scoring System. Nutrients 2019, 11, 1572. [Google Scholar] [CrossRef]
- Lohse, T.; Faeh, D.; Bopp, M.; Rohrmann, S. Adherence to the cancer prevention recommendations of the World Cancer Research Fund/American Institute for Cancer Research and mortality: A census-linked cohort. Am. J. Clin. Nutr. 2016, 104, 678–685. [Google Scholar] [CrossRef]
- Jankovic, N.; Geelen, A.; Winkels, R.M.; Mwungura, B.; Fedirko, V.; Jenab, M.; Illner, A.K.; Brenner, H.; Ordóñez-Mena, J.M.; Kiefte de Jong, J.C.; et al. Adherence to the WCRF/AICR Dietary Recommendations for Cancer Prevention and Risk of Cancer in Elderly from Europe and the United States: A Meta-Analysis within the CHANCES Project. Cancer Epidemiol. Biomark. Prev. 2017, 26, 136–144. [Google Scholar] [CrossRef]
- Hastert, T.A.; Beresford, S.A.A.; Patterson, R.E.; Kristal, A.R.; White, E. Adherence to WCRF/AICR Cancer Prevention Recommendations and Risk of Postmenopausal Breast Cancer. Cancer Epidemiol. Biomark. Prev. 2013, 22, 1498–1508. [Google Scholar] [CrossRef]
- Castelló, A.; Martín, M.; Ruiz, A.; Casas, A.M.; Baena-Cañada, J.M.; Lope, V.; Antolín, S.; Sánchez, P.; Ramos, M.; Antón, A.; et al. Lower Breast Cancer Risk among Women following the World Cancer Research Fund and American Institute for Cancer Research Lifestyle Recommendations: EpiGEICAM Case-Control Study. PLoS ONE 2015, 10, e0126096. [Google Scholar] [CrossRef]
- Makarem, N.; Lin, Y.; Bandera, E.V.; Jacques, P.F.; Parekh, N. Concordance with World Cancer Research Fund/American Institute for Cancer Research (WCRF/AICR) guidelines for cancer prevention and obesity-related cancer risk in the Framingham Offspring cohort (1991–2008). Cancer Causes Control 2015, 26, 277–286. [Google Scholar] [CrossRef]
- Romaguera, D.; Gracia-Lavedan, E.; Molinuevo, A.; de Batlle, J.; Mendez, M.; Moreno, V.; Vidal, C.; Castelló, A.; Pérez-Gómez, B.; Martín, V.; et al. Adherence to nutrition-based cancer prevention guidelines and breast, prostate and colorectal cancer risk in the MCC-Spain case-control study. Int. J. Cancer 2017, 141, 83–93. [Google Scholar] [CrossRef] [PubMed]
- Schulpen, M.; van den Brandt, P.A. Adherence to the Mediterranean Diet and Risks of Prostate and Bladder Cancer in the Netherlands Cohort Study. Cancer Epidemiol. Biomark. Prev. 2019, 28, 1480–1488. [Google Scholar] [CrossRef] [PubMed]
- Karavasiloglou, N.; Husing, A.; Masala, G.; van Gils, C.H.; Turzanski Fortner, R.; Chang-Claude, J.; Huybrechts, I.; Weiderpass, E.; Gunter, M.; Arveux, P.; et al. Adherence to the World Cancer Research Fund/American Institute for Cancer Research cancer prevention recommendations and risk of in situ breast cancer in the European Prospective Investigation into Cancer and Nutrition (EPIC) cohort. BMC Med. 2019, 17, 221. [Google Scholar] [CrossRef] [PubMed]
- Turati, F.; Bravi, F.; Di Maso, M.; Bosetti, C.; Polesel, J.; Serraino, D.; Dalmartello, M.; Giacosa, A.; Montella, M.; Tavani, A.; et al. Adherence to the World Cancer Research Fund/American Institute for Cancer Research recommendations and colorectal cancer risk. Eur. J. Cancer 2017, 85, 86–94. [Google Scholar] [CrossRef] [PubMed]
- Bravi, F.; Polesel, J.; Garavello, W.; Serraino, D.; Negri, E.; Franchin, G.; La Vecchia, C.; Bosetti, C. Adherence to the World Cancer Research Fund/American Institute for Cancer Research recommendations and head and neck cancers risk. Oral Oncol. 2017, 64, 59–64. [Google Scholar] [CrossRef] [PubMed]
- Lucas, A.L.; Bravi, F.; Boffetta, P.; Polesel, J.; Serraino, D.; La Vecchia, C.; Bosetti, C. Adherence to World Cancer Research Fund/American Institute for Cancer Research recommendations and pancreatic cancer risk. Cancer Epidemiol. 2016, 40, 15–21. [Google Scholar] [CrossRef]
- Solans, M.; Romaguera, D.; Gracia-Lavedan, E.; Molinuevo, A.; Benavente, Y.; Saez, M.; Marcos-Gragera, R.; Costas, L.; Robles, C.; Alonso, E.; et al. Adherence to the 2018 WCRF/AICR cancer prevention guidelines and chronic lymphocytic leukemia in the MCC-Spain study. Cancer Epidemiol. 2019, 64, 101629. [Google Scholar] [CrossRef]
- Romaguera, D.; Vergnaud, A.-C.; Peeters, P.H.; van Gils, C.H.; Chan, D.S.; Ferrari, P.; Romieu, I.; Jenab, M.; Slimani, N.; Clavel-Chapelon, F.; et al. Is concordance with World Cancer Research Fund/American Institute for Cancer Research guidelines for cancer prevention related to subsequent risk of cancer? Results from the EPIC study. Am. J. Clin. Nutr. 2012, 96, 150–163. [Google Scholar] [CrossRef]
- Arab, L.; Su, J.; Steck, S.E.; Ang, A.; Fontham, E.T.H.; Bensen, J.T.; Mohler, J.L. Adherence to World Cancer Research Fund/American Institute for Cancer Research lifestyle recommendations reduces prostate cancer aggressiveness among African and Caucasian Americans. Nutr. Cancer 2013, 65, 633–643. [Google Scholar] [CrossRef]
- Er, V.; Lane, J.A.; Martin, R.M.; Emmett, P.; Gilbert, R.; Avery, K.N.L.; Walsh, E.; Donovan, J.L.; Neal, D.E.; Hamdy, F.C.; et al. Adherence to dietary and lifestyle recommendations and prostate cancer risk in the prostate testing for cancer and treatment (ProtecT) trial. Cancer Epidemiol. Biomark. Prev. 2014, 23, 2066–2077. [Google Scholar] [CrossRef]
- Loeb, S.; Bjurlin, M.A.; Nicholson, J.; Tammela, T.L.; Penson, D.F.; Carter, H.B.; Carroll, P.; Etzioni, R. Overdiagnosis and overtreatment of prostate cancer. Eur. Urol. 2014, 65, 1046–1055. [Google Scholar] [CrossRef] [PubMed]
- ICD-10 Version: 2016. Available online: https://icd.who.int/browse10/2016/en (accessed on 20 January 2020).
- Román Viñas, B.; Ribas Barba, L.; Ngo, J.; Serra Majem, L. Validación en población catalana del cuestionario internacional de actividad física. Gac. Sanit. 2013, 27, 254–257. [Google Scholar] [CrossRef] [PubMed]
- Martin-Moreno, J.M.; Boyle, P.; Gorgojo, L.; Maisonneuve, P.; Fernandez-Rodriguez, J.C.; Salvini, S.; Willett, W.C. Development and validation of a food frequency questionnaire in Spain. Int. J. Epidemiol. 1993, 22, 512–519. [Google Scholar] [CrossRef] [PubMed]
- Tablas de composición de alimentos del CESNID. Available online: http://www.sennutricion.org/es/2013/05/13/tablas-de-composicin-de-alimentos-del-cesnid (accessed on 7 November 2019).
- Willett, W. Nutritional Epidemiology; Oxford University Press: Oxford, UK, 2013; ISBN 9780199979448. [Google Scholar]
- Monteiro, C.A.; Cannon, G.; Levy, R.; Moubarac, J.-C.; Jaime, P.; Paula Martins, A.; Canella, D.; Louzada, M.; Parra Also with Camila Ricardo, D.; Calixto, G.; et al. NOVA. The star shines bright. World Nutr. 2016, 7, 28–38. [Google Scholar]
- Epstein, J.I. An Update of the Gleason Grading System. J. Urol. 2010, 183, 433–440. [Google Scholar] [CrossRef] [PubMed]
- Epstein, J.I.; Egevad, L.; Amin, M.B.; Delahunt, B.; Srigley, J.R.; Humphrey, P.A. The 2014 International Society of Urological Pathology (ISUP) Consensus Conference on Gleason Grading of Prostatic Carcinoma: Definition of Grading Patterns and Proposal for a New Grading System. Am. J. Surg. Pathol. 2016, 40, 244–252. [Google Scholar] [CrossRef]
- Neuzillet, Y.; Raynaud, J.-P.; Dreyfus, J.-F.; Radulescu, C.; Rouanne, M.; Schneider, M.; Krish, S.; Roupret, M.; Drouin, S.J.; Comperat, E.; et al. Aggressiveness of Localized Prostate Cancer: The Key Value of Testosterone Deficiency Evaluated by Both Total and Bioavailable Testosterone: AndroCan Study Results. Horm. Cancer 2019, 10, 36–44. [Google Scholar] [CrossRef]
- Pérula de Torres, L.A.; Espina García, C. What is the European Code against Cancer, who knows it and why it serves? Aten. Primaria 2018, 50, 71–73. [Google Scholar] [CrossRef]
- Fiolet, T.; Srour, B.; Sellem, L.; Kesse-Guyot, E.; Alles, B.; Mejean, C.; Deschasaux, M.; Fassier, P.; Latino-Martel, P.; Beslay, M.; et al. Consumption of ultra-processed foods and cancer risk: Results from NutriNet-Sante prospective cohort. BMJ 2018, 360, k322. [Google Scholar] [CrossRef]
- Boyle, P.; Koechlin, A.; Autier, P. Sweetened carbonated beverage consumption and cancer risk: Meta-analysis and review. Eur. J. Cancer Prev. 2014, 23, 481–490. [Google Scholar] [CrossRef]
- Chazelas, E.; Srour, B.; Desmetz, E.; Kesse-Guyot, E.; Julia, C.; Deschamps, V.; Druesne-Pecollo, N.; Galan, P.; Hercberg, S.; Latino-Martel, P.; et al. Sugary drink consumption and risk of cancer: Results from NutriNet-Santé prospective cohort. BMJ 2019, 366, l2408. [Google Scholar] [CrossRef] [PubMed]
- Zhao, J.; Stockwell, T.; Roemer, A.; Chikritzhs, T. Is alcohol consumption a risk factor for prostate cancer? A systematic review and meta-analysis. BMC Cancer 2016, 16, 845. [Google Scholar] [CrossRef] [PubMed]
| Components | Personal Recommendations (Goals) | Operationalization | Scoring |
|---|---|---|---|
| 1. Have a healthy weight | Ensure that body weight during childhood and adolescence projects toward the lower end of the healthy adult BMI range | No information for operationalization | n.a |
| Keep your weight as low as you can within the healthy range throughout life | BMI ≥ 18.5–< 25 kg/m2 | 0.5 | |
| BMI ≥ 25–< 30 kg/m2 | 0.25 | ||
| BMI ≥ 30 kg/m2 or < 18.5–25 kg/m2 | 0 | ||
| Avoid weight gain (measured as body weight or waist circumference) throughout adulthood | WC < 94 cm | 0.5 | |
| WC ≥ 94–<102 cm | 0.25 | ||
| WC ≥ 102 cm | 0 | ||
| 2. Be physically active | Be at least moderately physically active, and follow or exceed national guidelines | Total moderate-vigorous PA ≥ 150 min/week | 1 |
| Total moderate-vigorous PA ≥ 75–< 150 min/week | 0.5 | ||
| Total moderate-vigorous PA < 75 min/week | 0 | ||
| Limit sedentary habits | No information for operationalization | n.a | |
| 3. Eat a diet rich in whole grains, vegetables, fruit, and beans | Consume a diet that provides at least 30 g/day of fiber from food sources | Dietary fiber intake ≥ 30 g/day | 0.5 |
| Dietary fiber intake ≥ 15–<30 g/day | 0.25 | ||
| Dietary fiber intake < 15 g/day | 0 | ||
| Include more foods containing wholegrains, non-starchy vegetables, fruit, and pulses (legumes) such as beans and lentils | No information for operationalization | n.a. | |
| Eat a diet high in all types of plant foods including at least five portions or servings (at least 400 g or 15 oz in total) of a variety of non-starchy vegetables and fruit every day | Fruits and vegetables intake a ≥ 400 g/day | 0.5 | |
| Fruits and vegetables intake a ≥ 200–< 400 g/day | 0.25 | ||
| Fruits and vegetables intake a < 200 g/day | 0 | ||
| If you eat starchy roots and tubers as staple foods, eat non-starchy vegetables, fruit, and pulses (legumes) regularly too if possible | No information for operationalization | n.a. | |
| 4. Limit consumption of ”fast foods” and other processed foods high in fat, starches, or sugars | Limit consumption of processed foods high in fat, starches or sugars including “fast foods”, many prepared dishes, snacks, bakery foods and desserts, and confectionery (candy) | Percent of total kcal from ultra-processed foods (aUPFs): Tercile 1 | 1 |
| Tercile 2 | 0.5 | ||
| Tercile 3 | 0 | ||
| 5. Limit consumption of red and processed meat | If you eat red meat, limit consumption to no more than about three portions per week. Three portions are equivalent to about 350 to 500 g (about 12 to 18 oz) cooked weight of red meat. Consume very little, if any, processed meat. | Red meat <500 g/wk and processed meat < 21 g/wk | 1 |
| Red meat <500 g/wk and processed meat ≥ 21–<100 g/wk | 0.5 | ||
| Red meat ≥500 g/wk or processed meat ≥ 100g/wk | 0 | ||
| 6. Limit consumption of sugar-sweetened drinks | Do not consume sugar-sweetened drinks | Sugary drinks intake b = 0 g/day | 1 |
| Sugary drinks intakeb >0–≤ 250 g/day | 0.5 | ||
| Sugary drinks intake b > 250 g/day | 0 | ||
| 7. Limit alcohol consumption | For cancer prevention, it is best not to drink alcohol | No ethanol intake = 0 g/day | 1 |
| Current ethanol intake > 0–< 28 g/day | 0.5 | ||
| Current ethanol intake ≥ 28 g/day | 0 | ||
| 8. Do not use supplements for cancer prevention | High-dose dietary supplements are not recommended for cancer prevention-aim to meet nutritional needs through diet alone | No information for operationalization | n.a |
| 9. For mothers: breastfeed your baby, if you can | This recommendation aligns with the advice of the World Health Organization, which recommends infants are exclusively breastfed to 6 months, and then up to 2 years of age or beyond alongside appropriate complementary foods. | Not applicable to this population | n.a. |
| 10. After a cancer diagnosis: follow our recommendations if you can | All cancer survivors should receive nutritional care and guidance on physical activity from trained professionals. | Not applicable to this study | n.a. |
| Unless otherwise advised, and if you can, all cancer survivors are advised to follow the Cancer Prevention Recommendations as far as possible after the acute stage of treatment | Not applicable to this study | n.a. |
| Controls | PCa Cases | p-Value | |
|---|---|---|---|
| (n = 302) | (n = 398) | ||
| Age (years), mean (SD) | 65.3 (8.2) | 67.7 (7.4) | <0.01 |
| Age (years), n (%) | <0.01 | ||
| 40–54 | 39 (12.9) | 21 (5.3) | |
| 55–69 | 162 (53.7) | 217 (54.5) | |
| 70–80 | 101 (33.4) | 160 (40.2) | |
| Education, n (%) | 0.38 | ||
| Primary | 92 (30.4) | 119 (29.9) | |
| Secondary | 147 (48.7) | 211 (53.0) | |
| University | 63 (20.9) | 68 (17.1) | |
| Energy intake (kcal/day), mean (SD) | 2438.1 (705.7) | 2511.8 (617.6) | 0.14 |
| Alcohol consumption 1, n (%) | 0.05 | ||
| No consumption | 56 (18.5) | 69 (17.4) | |
| Moderate | 215 (71.2) | 262 (65.8) | |
| High | 31 (10.3) | 67 (16.8) | |
| Smoking status, n (%) | 0.70 | ||
| Never | 88 (29.1) | 105 (26.4) | |
| Former | 157 (52.0) | 212 (53.3) | |
| Current | 57 (18.9) | 81 (20.3) | |
| First-degree family history of PCa 2, n (%) | 0.46 | ||
| No | 287 (95.0) | 373 (93.7) | |
| Yes | 15 (5.0) | 25 (6.3) | |
| Aggressiveness, n (%) | |||
| ISUP 1–2 | – | 307 (77.1) | |
| ISUP 3–5 | – | 91 (22.9) | |
| WCRF/AICR score, mean (SD) (Minimum–Maximum) | 3.42 (1.01) (1.00–6.25) | 3.27 (0.93) (0.75–6.25) | 0.05 |
| WCRF/AICR score, n (%) | 0.08 | ||
| ≤1 | 1 (0.3) | 3 (0.7) | |
| >1–≤2 | 27 (8.9) | 30 (7.6) | |
| >2–≤3 | 98 (32.4) | 160 (40.2) | |
| >3–≤4 | 105 (34.8) | 132 (33.2) | |
| >4–≤5 | 51 (16.9) | 63 (15.8) | |
| >5–≤6 | 18 (6.0) | 8 (2.0) | |
| >6–≤7 | 2 (0.7) | 1 (0.5) | |
| WCRF/AICR score 3, n (%) | 0.69 | ||
| Minimum compliance (T1) | 101 (33.4) | 140 (35.2) | |
| Intermediate compliance (T2) | 111 (36.8) | 151 (37.9) | |
| Maximum compliance (T3) | 90 (29.8) | 107 (26.9) |
| Tercile 1 n = 101 | Tercile 2 n = 111 | Tercile 3 n = 90 | p-Value | |
|---|---|---|---|---|
| min–max 0.75–2.75 | min–max 3.00–3.75 | min–max 4.00–6.50 | ||
| Age (years), mean (SD) | 62.7 (7.8) | 65.9 (7.3) | 67.3 (8.9) | 0.01 |
| Age (years), n (%) | 0.01 | |||
| 40–54 | 18 (17.8) | 9 (8.1) | 12 (13.3) | |
| 55–69 | 62 (61.4) | 64 (57.7) | 36 (40.0) | |
| 70–80 | 21 (20.8) | 38 (34.2) | 42 (46.7) | |
| Education, n (%) | 0.74 | |||
| Primary | 30 (39.7) | 35 (31.5) | 27 (30.0) | |
| Secondary | 54 (53.5) | 51 (46.0) | 42 (46.7) | |
| University | 17 (16.8) | 25 (22.5) | 21 (23.3) | |
| Energy intake (kcal/day), mean (SD) | 2510.5 (720.0) | 2557.0 (685.3) | 2210.3 (668.4) | <0.01 |
| Alcohol consumption 1, n (%) | <0.01 | |||
| No consumption | 10 (9.9) | 18 (16.2) | 28 (31.1) | |
| Moderate | 71 (70.3) | 85 (76.6) | 59 (65.6) | |
| High | 20 (19.8) | 8 (7.2) | 3 (3.3) | |
| Smoking status, n (%) | 0.26 | |||
| Never | 22 (21.8) | 37 (33.3) | 29 (32.2) | |
| Former | 57 (56.4) | 52 (46.9) | 48 (53.3) | |
| Current | 22 (21.8) | 22 (19.8) | 13 (14.4) | |
| First-degree history of PCa 2, n (%) | 0.12 | |||
| No | 98 (97.0) | 107 (96.4) | 82 (91.1) | |
| Yes | 3 (3.0) | 3 (3.6) | 8 (8.9) |
| WCRF/AICR Score Categories | |||||||
|---|---|---|---|---|---|---|---|
| N Control/Cases 1 | Tercile 1 | Tercile 2 | Tercile 3 | p-Trend | 1-Unit Increase | p-Value | |
| aOR 2 (95% CI) | aOR 2 (95% CI) | aOR 2 (95% CI) | aOR 2 (95% CI) | ||||
| Overall | |||||||
| 302/398 | 1.00 | 0.88 (0.61–1.27) | 0.79 (0.53–1.19) | 0.26 | 0.81 (0.69–0.96) | 0.02 | |
| Aggressiveness 2 | |||||||
| ISUP 1–2 | 302/307 | 1.00 | 0.87 (0.59–1.28) | 0.73 (0.48–1.13) | 0.16 | 0.79 (0.66–0.95) | 0.01 |
| ISUP 3–5 | 302/91 | 1.00 | 0.84 (0.47–1.53) | 0.87 (0.46–1.66) | 0.67 | 0.86 (0.69–1.06) | 0.16 |
| Components of the Score | N Controls/Cases | aOR (95% CI) 1 | p-Trend |
|---|---|---|---|
| 1. Be a healthy weight 2 | 0.81 | ||
| 0–0.25 | 129/181 | 1 | |
| 0.5 | 85/87 | 0.69 (0.46–1.02) | |
| 0.75–1 | 88/130 | 1.09 (0.75–1.60) | |
| 2. Be physical active | 0.63 | ||
| 0 | 227/315 | 1 | |
| 0.5 | 17/14 | 0.55 (0.26–1.19) | |
| 1 | 58/69 | 0.94 (0.62–1.44) | |
| 3. Eat a diet rich in whole grains, vegetables, fruit and beans 2 | 0.89 | ||
| 0–0.25 | 14/15 | 1 | |
| 0.5 | 16/26 | 1.35 (0.48–3.76) | |
| 0.75–1 | 272/357 | 1.08 (0.47–2.50) | |
| 4. Limit consumption of ‘fast foods’ and other processed foods high in fat, starches or sugars | 0.02 | ||
| 0 | 101/163 | 1 | |
| 0.5 | 100/125 | 0.75 (0.51–1.10) | |
| 1 | 101/110 | 0.63 (0.42–0.94) | |
| 5. Limit consumption of red and processed meat | 0.22 | ||
| 0 | 231/297 | 1 | |
| 0.5 | 65/82 | 0.96 (0.63–1.46) | |
| 1 | 6/19 | 2.82 (1.05–7.59) | |
| 6. Limit consumption of sugar-sweetened drinks | 0.02 | ||
| 0 | 7/25 | 1 | |
| 0.5 | 132/179 | 0.39 (0.16–0.97) | |
| 1 | 163/194 | 0.30 (0.12–0.77) | |
| 7. Limit alcohol consumption | 0.03 | ||
| 0 | 31/67 | 1 | |
| 0.5 | 215/262 | 0.57 (0.34–0.95) | |
| 1 | 56/69 | 0.49 (0.27–0.91) |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rocío, O.-R.; Macarena, L.-L.; Inmaculada, S.-B.; Antonio, J.-P.; Fernando, V.-A.; Marta, G.-C.; María-José, S.; José-Juan, J.-M. Compliance with the 2018 World Cancer Research Fund/American Institute for Cancer Research Cancer Prevention Recommendations and Prostate Cancer. Nutrients 2020, 12, 768. https://doi.org/10.3390/nu12030768
Rocío O-R, Macarena L-L, Inmaculada S-B, Antonio J-P, Fernando V-A, Marta G-C, María-José S, José-Juan J-M. Compliance with the 2018 World Cancer Research Fund/American Institute for Cancer Research Cancer Prevention Recommendations and Prostate Cancer. Nutrients. 2020; 12(3):768. https://doi.org/10.3390/nu12030768
Chicago/Turabian StyleRocío, Olmedo-Requena, Lozano-Lorca Macarena, Salcedo-Bellido Inmaculada, Jiménez-Pacheco Antonio, Vázquez-Alonso Fernando, García-Caballos Marta, Sánchez María-José, and Jiménez-Moleón José-Juan. 2020. "Compliance with the 2018 World Cancer Research Fund/American Institute for Cancer Research Cancer Prevention Recommendations and Prostate Cancer" Nutrients 12, no. 3: 768. https://doi.org/10.3390/nu12030768
APA StyleRocío, O.-R., Macarena, L.-L., Inmaculada, S.-B., Antonio, J.-P., Fernando, V.-A., Marta, G.-C., María-José, S., & José-Juan, J.-M. (2020). Compliance with the 2018 World Cancer Research Fund/American Institute for Cancer Research Cancer Prevention Recommendations and Prostate Cancer. Nutrients, 12(3), 768. https://doi.org/10.3390/nu12030768







