How Minority Parents Could Help Children Develop Healthy Eating Behaviors: Parent and Child Perspectives
Abstract
:1. Introduction
2. Materials and Methods
2.1. Design
2.2. Study Participants
2.3. Recruitment
2.4. Data Collection
2.5. Data Analysis
2.5.1. Surveys
2.5.2. Interviews
3. Results
3.1. Family Characteristics
3.2. Interview Findings
3.2.1. Parents
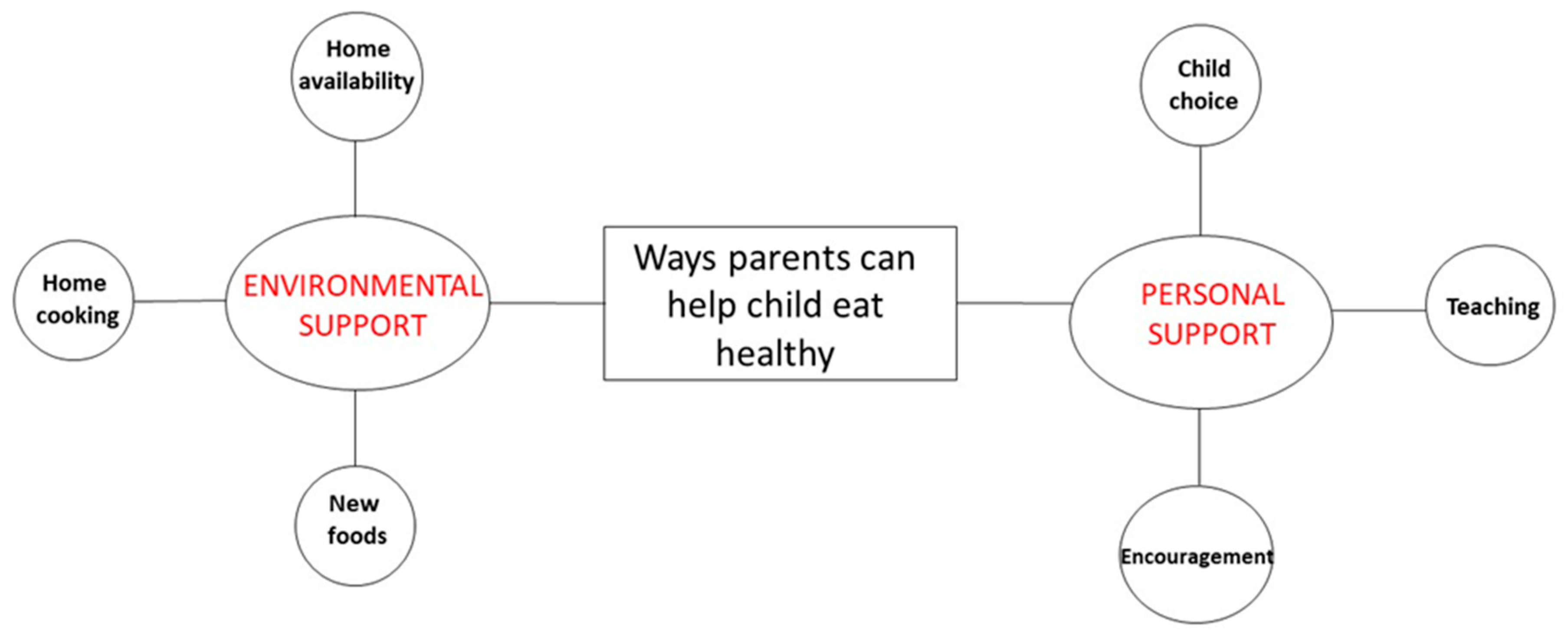
3.2.2. Children
3.2.3. Children’s Perspectives on Making Healthy Dietary Choices
Ease and Difficulty of Healthy Eating
Personal Eating Habits Assessment
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Fryar, C.D.; Carroll, M.D.; Ogden, C.L. Prevalence of Overweight, Obesity, and Severe Obesity among Children and Adolescents Aged 2–19 Years: United States, 1963–1965 through 2015. Available online: https://www.cdc.gov/nchs/data/hestat/obesity_child_15_16/obesity_child_15_16.htm (accessed on 29 June 2020).
- Mejia de Grubb, M.C.; Levine, R.S.; Zoorob, R.J. Diet and obesity issues in the underserved. Prim. Care 2017, 44, 127–140. [Google Scholar] [CrossRef] [PubMed]
- Hales, C.M.; Carroll, M.D.; Fryar, C.D.; Ogden, C.L. Prevalence of obesity among adults and youth: United States 2011–2014. NCHS Data Brief. 2017, 2017, 1–8. [Google Scholar]
- Ogden, C.L.; Carroll, M.D.; Fakhouri, T.H.; Hales, C.M.; Fryar, C.D.; Li, X.; Freedman, D.S. Prevalence of obesity among youths by household income and education level of head of household—United States 2011–2014. MMWR Morb. Mortal. Wkly. Rep. 2018, 67, 186–189. [Google Scholar] [CrossRef] [PubMed]
- U.S. Department of Health and Human Services. Healthy People. Available online: https://www.healthypeople.gov/ (accessed on 29 June 2020).
- Wilfley, D.E.; Saelens, B. Epidemiology and causes of obesity in children. In Eating Disorders and Obesity: A Comprehensive Handbook, 2nd ed.; Fairburn, C.G., Brownell, K.D., Eds.; The Guildford Press: New York, NY, USA, 2002; pp. 429–432. [Google Scholar]
- Kumar, S.; Kaufman, T. Childhood obesity. Panminerva Med. 2018, 60, 200–212. [Google Scholar] [CrossRef] [PubMed]
- Santiago-Torres, M.; Adams, A.K.; Carrel, A.L.; LaRowe, T.L.; Schoeller, D.A. Home food availability, parental dietary intake, and familial eating habits influence the diet quality of urban Hispanic children. Child. Obes. 2014, 10, 408–415. [Google Scholar] [CrossRef] [PubMed]
- Scaglioni, S.; De Cosmi, V.; Ciappolino, V.; Parazzini, F.; Brambilla, P.; Agostoni, C. Factors influencing children’s eating behaviours. Nutrients 2018, 10, 706. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Beckerman, J.P.; Alike, Q.; Lovin, E.; Tamez, M.; Mattei, J. The development and public health implications of food preferences in children. Front. Nutr. 2017, 4, 66. [Google Scholar] [CrossRef] [Green Version]
- French, S.A.; Tangney, C.C.; Crane, M.M.; Wang, Y.; Appelhans, B.M. Nutrition quality of food purchases varies by household income: The SHoPPER study. BMC Public Health 2019, 19, 231. [Google Scholar] [CrossRef] [Green Version]
- Banfield, E.C.; Liu, Y.; Davis, J.S.; Chang, S.; Frazier-Wood, A.C. Poor adherence to US dietary guidelines for children and adolescents in the National Health and Nutrition Examination Survey population. J. Acad Nutr. Diet. 2016, 116, 21–27. [Google Scholar] [CrossRef] [Green Version]
- Satia, J.A. Diet-related disparities: Understanding the problem and accelerating solutions. J. Am. Diet. Assoc. 2009, 109, 610–615. [Google Scholar] [CrossRef] [Green Version]
- Block, J.P.; Subramanian, S.V. Moving beyond “food deserts”: Reorienting United States policies to reduce disparities in diet quality. PLoS Med. 2015, 12, e1001914. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lucan, S.C.; Maroko, A.R.; Sanon, O.C.; Schechter, C.B. Unhealthful food-and-beverage advertising in subway stations: Targeted marketing, vulnerable groups, dietary intake, and poor health. J. Urban. Health 2017, 94, 220–232. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fleischhacker, S.E.; Evenson, K.R.; Rodriguez, D.A.; Ammerman, A.S. A systematic review of fast food access studies. Obes. Rev. 2011, 12, e460–e471. [Google Scholar] [CrossRef] [PubMed]
- Hager, E.R.; Cockerham, A.; O’Reilly, N.; Harrington, D.; Harding, J.; Hurley, K.M.; Black, M.M. Food swamps and food deserts in Baltimore City, MD, USA: Associations with dietary behaviours among urban adolescent girls. Public Health Nutr. 2017, 20, 2598–2607. [Google Scholar] [CrossRef] [Green Version]
- Gruber, K.J.; Haldeman, L.A. Using the family to combat childhood and adult obesity. Prev. Chronic Dis. 2009, 6, A106. [Google Scholar]
- Laraia, B.A.; Leak, T.M.; Tester, J.M.; Leung, C.W. Biobehavioral factors that shape nutrition in low-income populations: A narrative review. Am. J. Prev. Med. 2017, 52, S118–S126. [Google Scholar] [CrossRef] [Green Version]
- Evans, A.; Chow, S.; Jennings, R.; Dave, J.; Scoblick, K.; Sterba, K.R.; Loyo, J. Traditional foods and practices of Spanish-speaking Latina mothers influence the home food environment: Implications for future interventions. J. Am. Diet. Assoc. 2011, 111, 1031–1038. [Google Scholar] [CrossRef]
- Nepper, M.J.; Chai, W. Parents’ barriers and strategies to promote healthy eating among school-age children. Appetite 2016, 103, 15–64. [Google Scholar] [CrossRef] [Green Version]
- Parks, E.P.; Kazak, A.; Kumanyika, S.; Lewis, L.; Barg, F.K. Perspectives on stress, parenting, and children’s obesity-related behaviors in Black families. Health Educ. Behav. 2016, 43, 632–640. [Google Scholar] [CrossRef] [Green Version]
- Taverno Ross, S.E.; Macia, L.; Documét, P.I.; Escribano, C.; Kazemi Naderi, T.; Smith-Tapia, I. Latino parents’ perceptions of physical activity and healthy eating: At the intersection of culture, family, and health. J. Nutr. Educ. Behav. 2018, 50, 968–976. [Google Scholar] [CrossRef]
- Thompson, D.; Callender, C.; Velazquez, D.; Gonzalez, A.; Adera, M.; Li, P.; Mackey, G.; Dave, J.M.; Olvera, N.; Chen, T.A.; et al. Common Threads Grant—Final Report; Baylor College of Medicine: Houston, TX, USA, 2020; unpublished work. [Google Scholar]
- Jamshed, S. Qualitative research method-interviewing and observation. J. Basic Clin. Pharm. 2014, 5, 87–88. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fereday, J.; Muir-Cochrane, E. Demonstrating rigor using thematic analysis: A hybrid approach of inductive and deductive coding and theme development. Int. J. Qual. Methods 2006, 5, 80–92. [Google Scholar] [CrossRef]
- Lilo, E.A.; Muñoz, M.; Cruz, T.H. Perceptions of healthy eating among Hispanic parent-child dyads. Health Promot. Pract. 2019, 20, 231–238. [Google Scholar] [CrossRef] [PubMed]
- Danford, C.A.; Martyn, K.K. Exploring eating and activity behaviors with parent-child dyads using event history calendars. J. Fam. Nurs. 2013, 19, 375–398. [Google Scholar] [CrossRef] [PubMed]
- Yee, A.Z.; Lwin, M.O.; Ho, S.S. The influence of parental practices on child promotive and preventive food consumption behaviors: A systematic review and meta-analysis. Int. J. Behav. Nutr. Phys. Act. 2017, 14, 47. [Google Scholar] [CrossRef] [PubMed]
- van der Velde, L.A.; Schuilenburg, L.A.; Thrivikraman, J.K.; Numans, M.E.; Kiefte-de Jong, J.C. Needs and perceptions regarding healthy eating among people at risk of food insecurity: A qualitative analysis. Int. J. Equity Health 2019, 18, 184. [Google Scholar] [CrossRef]
- Couch, S.C.; Glanz, K.; Zhou, C.; Sallis, J.F.; Saelens, B.E. Home food environment in relation to children’s diet quality and weight status. J. Acad. Nutr. Diet. 2014, 114, 1569–1579.e1. [Google Scholar] [CrossRef] [Green Version]
- Dave, J.M.; Thompson, D.I.; Svendsen-Sanchez, A.; Cullen, K.W. Perspectives on barriers to eating healthy among food pantry clients. Health Equity 2017, 1, 28–34. [Google Scholar] [CrossRef]
- Oates, G.R.; Phillips, J.M.; Bateman, L.B.; Baskin, M.L.; Fouad, M.N.; Scarinci, I.C. Determinants of obesity in two urban communities: Perceptions and community-driven solutions. Ethn. Dis. 2018, 28, 33–42. [Google Scholar] [CrossRef] [Green Version]
- Callender, C.; Thompson, D. Text messaging based obesity prevention program for parents of pre-adolescent African American girls. Children 2017, 4, 105. [Google Scholar] [CrossRef] [Green Version]
- St. George, S.M.; Wilson, D.K. A qualitative study for understanding family and peer influences on obesity-related health behaviors in low-income African-American adolescents. Child. Obes. 2012, 8, 466–476. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Banna, J.C.; Buchthal, O.V.; Delormier, T.; Creed-Kanashiro, H.M.; Penny, M.E. Influences on eating: A qualitative study of adolescents in a periurban area in Lima, Peru. BMC Public Health 2016, 16, 40. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lopez-Dicastillo, O.; Grande, G.; Callery, P. School children’s own views, roles and contribution to choices regarding diet and activity in Spain. Child. Care Health Dev. 2013, 39, 109–117. [Google Scholar] [CrossRef] [PubMed]
- Dave, J.M.; Evans, A.E.; Condrasky, M.D.; Williams, J.E. Parent-reported social support for child’s fruit and vegetable intake: Validity of measures. J. Nutr. Educ. Behav. 2012, 44, 132–139. [Google Scholar] [CrossRef] [PubMed]
- Haines, J.; Haycraft, E.; Lytle, L.M.; Nicklaus, S.; Kok, F.; Merdji, M.; Fisberg, M.; Moreno, L.A.; Goulet, O.J.; Hughes, S.O. Nurturing children’s healthy eating: Position statement. Appetite 2019, 137, 124–133. [Google Scholar] [CrossRef] [PubMed]
- Holsten, J.E.; Deatrick, J.A.; Kumanyika, S.; Pinto-Martin, J.; Compher, C.W. Children’s food choice process in the home environment. A qualitative descriptive study. Appetite 2012, 58, 64–73. [Google Scholar] [CrossRef]
- Pearce, A.; Kirk, C.; Cummins, S.; Collins, M.; Elliman, D.; Connolly, A.; Law, C. Gaining children’s perspectives: A multiple method approach to explore environmental influences on healthy eating and physical activity. Health Place 2009, 15, 614–621. [Google Scholar] [CrossRef]
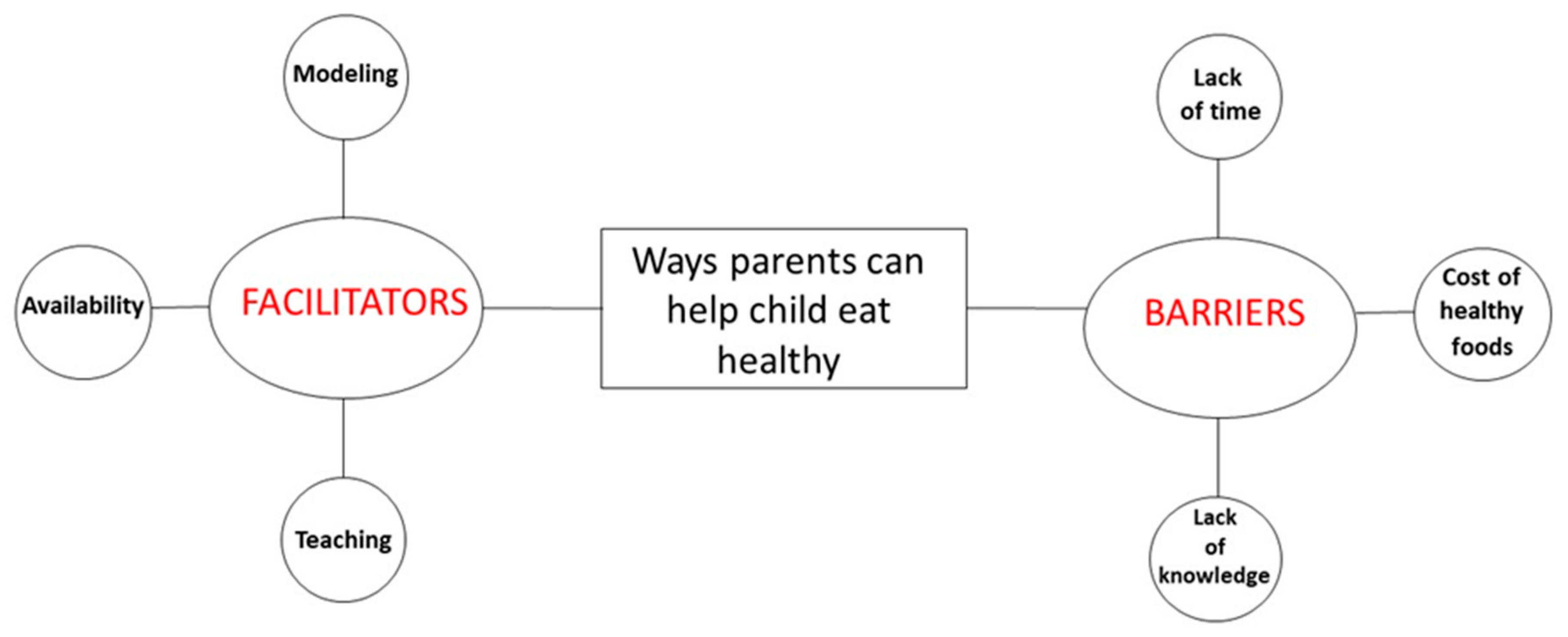
| Categories | Subcategories | Definitions |
|---|---|---|
| Facilitators |
|
|
| Barriers |
|
|
| Categories | Subcategories | Definitions |
|---|---|---|
| Environmental Support |
|
|
| Personal Support |
|
|
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Callender, C.; Velazquez, D.; Adera, M.; Dave, J.M.; Olvera, N.; Chen, T.-A.; Alford, S.; Thompson, D. How Minority Parents Could Help Children Develop Healthy Eating Behaviors: Parent and Child Perspectives. Nutrients 2020, 12, 3879. https://doi.org/10.3390/nu12123879
Callender C, Velazquez D, Adera M, Dave JM, Olvera N, Chen T-A, Alford S, Thompson D. How Minority Parents Could Help Children Develop Healthy Eating Behaviors: Parent and Child Perspectives. Nutrients. 2020; 12(12):3879. https://doi.org/10.3390/nu12123879
Chicago/Turabian StyleCallender, Chishinga, Denisse Velazquez, Meheret Adera, Jayna M. Dave, Norma Olvera, Tzu-An Chen, Shana Alford, and Debbe Thompson. 2020. "How Minority Parents Could Help Children Develop Healthy Eating Behaviors: Parent and Child Perspectives" Nutrients 12, no. 12: 3879. https://doi.org/10.3390/nu12123879
APA StyleCallender, C., Velazquez, D., Adera, M., Dave, J. M., Olvera, N., Chen, T.-A., Alford, S., & Thompson, D. (2020). How Minority Parents Could Help Children Develop Healthy Eating Behaviors: Parent and Child Perspectives. Nutrients, 12(12), 3879. https://doi.org/10.3390/nu12123879







