Ready to Change: Attitudes of an Elderly CKD Stage 3–5 Population towards Testing Protein-Free Food
Abstract
1. Introduction
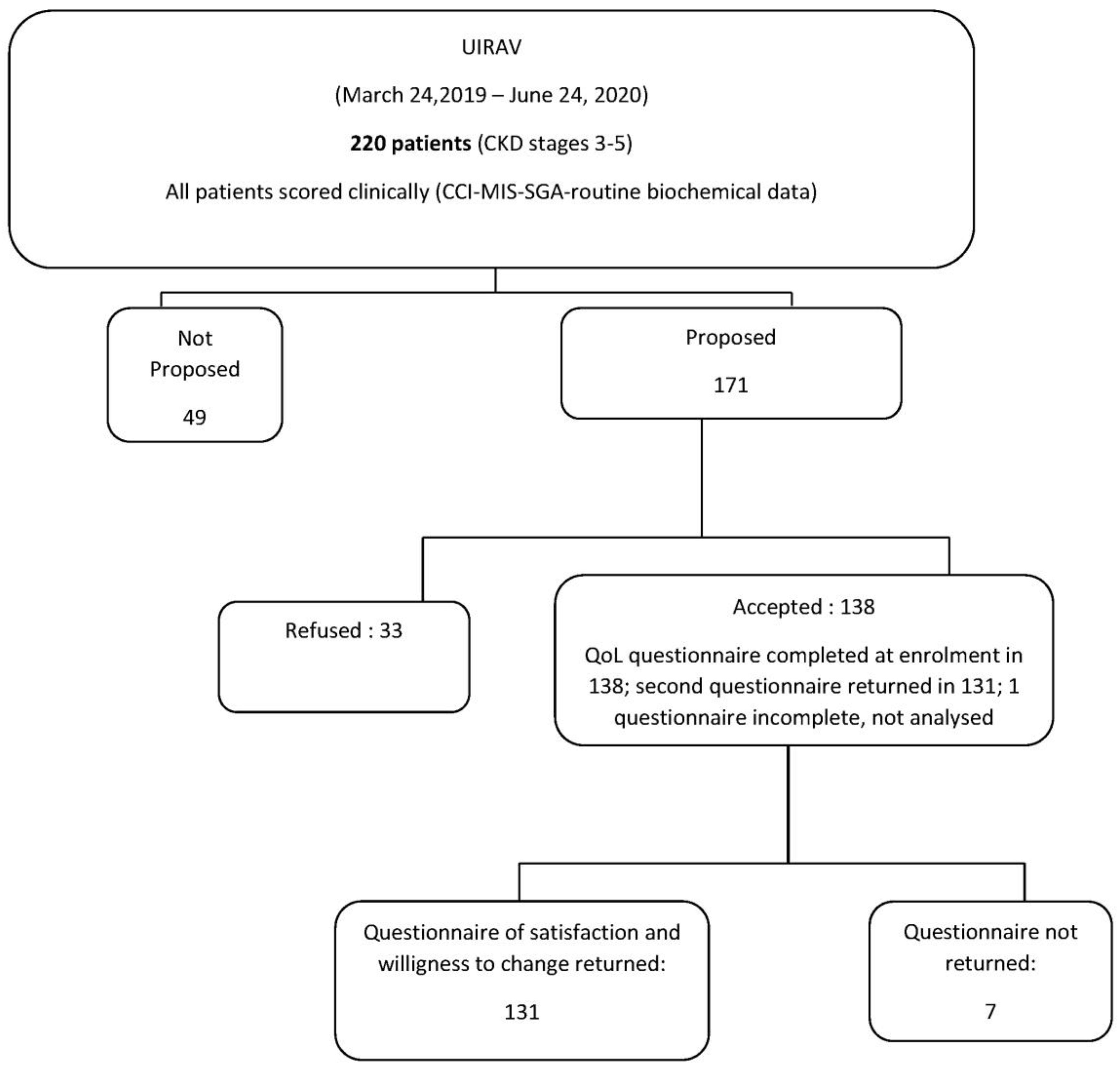
2. Materials and Methods
2.1. Study Setting
2.2. Study Population
2.3. Design of the Study and Choice of the Products
2.4. Satisfaction Questionnaire
- -
- Assessment of satisfaction with the products tested, based on a 1–10 visual analogue scale;
- -
- Identification of the frequency with which new products could replace products they normally ate;
- -
- Semi-structured questions on possible barriers (price, variety of products, therapeutic efficacy, ease of supply, reimbursement, taste) to their use.
2.5. Statistical Analysis
2.6. Ethical Issues
3. Results
3.1. Baseline Data
3.2. Willingness to Change and Satisfaction with the Test
3.3. Logistic Regression Analysis: Refusal to Participate in the Test and Low Willingness to Change
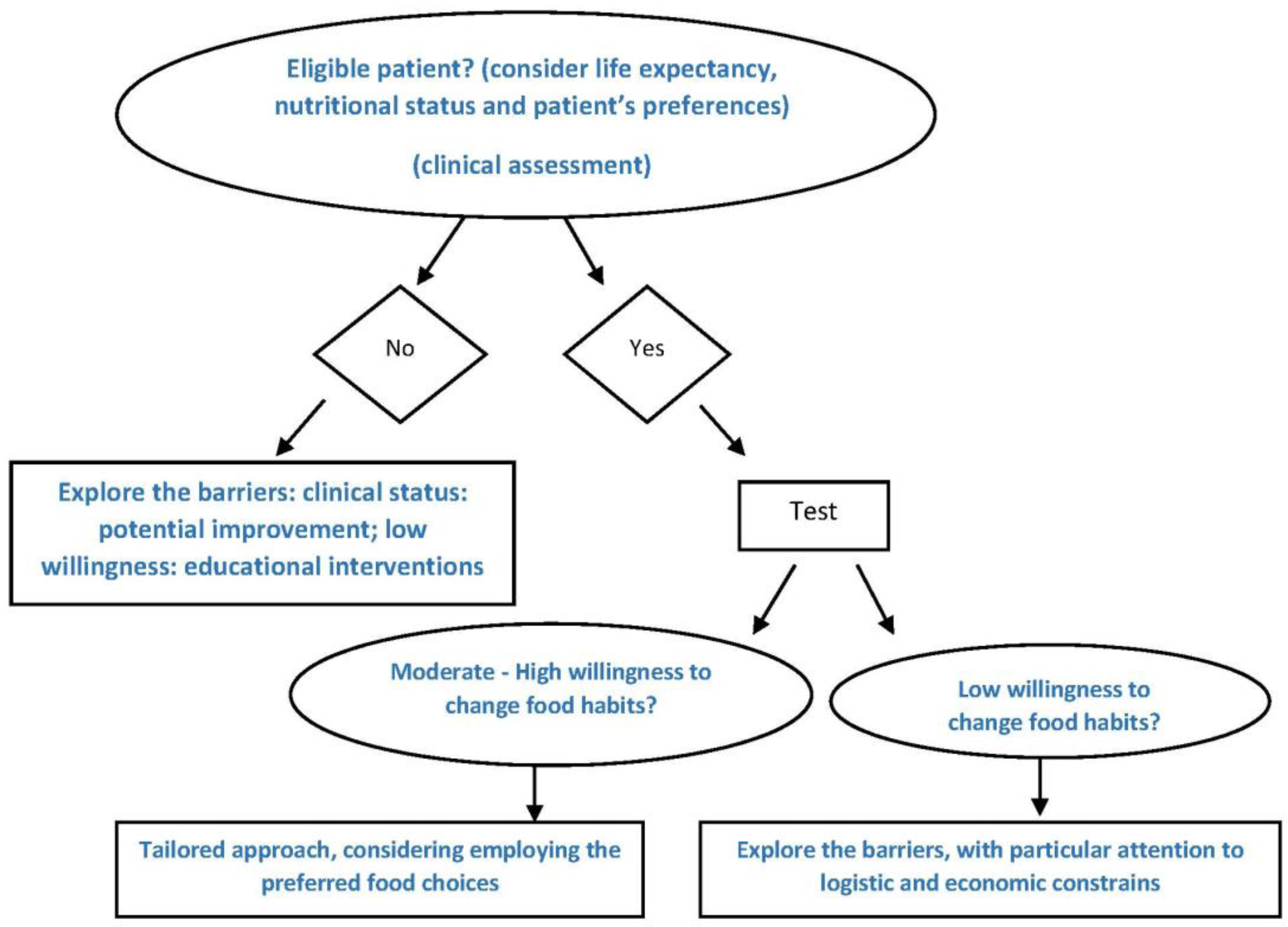
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Brenner, B.M.; Lawler, E.V.; MacKenzie, H.S. The hyperfiltration theory: A paradigm shift in nephrology. Kidney Int. 1996, 49, 1774–1777. [Google Scholar] [CrossRef] [PubMed]
- Mitch, W.E.; Remuzzi, G. Diets for patients with chronic kidney disease, should we reconsider? BMC Nephrol. 2016, 17, 80. [Google Scholar] [CrossRef] [PubMed]
- Mitch, W.E. Diets For Patients with Chronic Kidney Disease, Still Worth Prescribing. J. Am. Soc. Nephrol. 2004, 15, 234–237. [Google Scholar] [CrossRef] [PubMed]
- Hanafusa, N.; Lodebo, B.T.; Kopple, J.D. Current Uses of Dietary Therapy for Patients with Far-Advanced CKD. Clin. J. Am. Soc. Nephrol. 2017, 12, 1190–1195. [Google Scholar] [CrossRef]
- Cupisti, A.; Brunori, G.; Di Iorio, B.R.; D’Alessandro, C.; Pasticci, F.; Cosola, C.; Bellizzi, V.; Bolasco, P.; Capitanini, A.; Fantuzzi, A.L.; et al. Nutritional treatment of advanced CKD: Twenty consensus statements. J. Nephrol. 2018, 31, 457–473. [Google Scholar] [CrossRef]
- Hahn, D.; Hodson, E.M.; Fouque, D. Low protein diets for non-diabetic adults with chronic kidney disease. Cochrane Database Syst. Rev. 2018, 10, CD001892. [Google Scholar] [CrossRef]
- Brunori, G.; Viola, B.F.; Parrinello, G.; De Biase, V.; Como, G.; Franco, V.; Garibotto, G.; Zubani, R.; Cancarini, G.C. Efficacy and Safety of a Very-Low-Protein Diet When Postponing Dialysis in the Elderly: A Prospective Randomized Multicenter Controlled Study. Am. J. Kidney Dis. 2007, 49, 569–580. [Google Scholar] [CrossRef]
- Piccoli, G.B.; Di Iorio, B.R.; Chatrenet, A.; D’Alessandro, C.; Nazha, M.; Capizzi, I.; Vigotti, F.N.; Fois, A.; Maxia, S.; Saulnier, P.; et al. Dietary satisfaction and quality of life in chronic kidney disease patients on low-protein diets: A multicentre study with long-term outcome data (TOrino-Pisa study). Nephrol. Dial. Transpl. 2019, 35, 790–802. [Google Scholar] [CrossRef]
- Fouque, D.; Laville, M.; Boissel, J.P.; Chifflet, R.; Labeeuw, M.; Zech, P.Y. Controlled low protein diets in chronic renal insufficiency: Meta-analysis. BMJ 1992, 304, 216–220. [Google Scholar] [CrossRef]
- Kasiske, B.L.; Lakatua, J.D.; Ma, J.Z.; Louis, T.A. A meta-analysis of the effects of dietary protein restriction on the rate of decline in renal function. Am. J. Kidney Dis. 1998, 31, 954–961. [Google Scholar] [CrossRef]
- Locatelli, F.; Alberti, D.; Graziani, G.; Buccianti, G.; Redaelli, B.; Giangrande, A. Prospective, randomised, multicentre trial of effect of protein restriction on progression of chronic renal insufficiency. Lancet 1991, 337, 1299–1304. [Google Scholar] [CrossRef]
- Wang, M.; Chou, J.; Chang, Y.; Lau, W.L.; Reddy, U.; Rhee, C.M.; Chen, J.; Hao, C.; Kalantar-Zadeh, K. The role of low protein diet in ameliorating proteinuria and deferring dialysis initiation: What is old and what is new. Panminerva Med. 2016, 59, 157–165. [Google Scholar] [PubMed]
- Ko, G.J.; Obi, Y.; Tortoricci, A.R.; Kalantar-Zadeh, K. Dietary protein intake and chronic kidney disease. Curr. Opin. Clin. Nutr. Metab. Care 2017, 20, 77–85. [Google Scholar] [CrossRef] [PubMed]
- Fouque, D.P.; Aparicio, M. Eleven reasons to control the protein intake of patients with chronic kidney disease. Nat. Clin. Pract. Nephrol. 2007, 3, 383–392. [Google Scholar] [CrossRef] [PubMed]
- Kalantar-Zadeh, K.; Fouque, D. Nutritional Management of Chronic Kidney Disease. N. Engl. J. Med. 2017, 377, 1765–1776. [Google Scholar] [CrossRef]
- Sabatino, A.; Regolisti, G.; Gandolfini, I.; Delsante, M.; Fani, F.; Gregorini, M.C.; Fiaccadori, E. Diet and enteral nutrition in patients with chronic kidney disease not on dialysis: A review focusing on fat, fiber and protein intake. J. Nephrol. 2017, 30, 743–754. [Google Scholar] [CrossRef]
- Ikizler, T.A.; Burrowes, J.D.; Byham-Gray, L.D.; Campbell, K.L.; Carrero, J.-J.; Chan, W.; Fouque, D.; Friedman, A.N.; Ghaddar, S.; Goldstein-Fuchs, D.J.; et al. KDOQI Clinical Practice Guideline for Nutrition in CKD: 2020 Update. Am. J. Kidney Dis. 2020, 76, S1–S107. [Google Scholar] [CrossRef]
- Bellizzi, V.; Cupisti, A.; Locatelli, F.; Bolasco, P.; Brunori, G.; Cancarini, G.; Caria, S.; De Nicola, L.; Di Iorio, B.R.; Di Micco, L.; et al. Low-protein diets for chronic kidney disease patients: The Italian experience. BMC Nephrol. 2016, 17, 77. [Google Scholar] [CrossRef]
- Giovannetti, S.; Maggiore, Q. A Low-Nitrogen Diet with Proteins of High Biological Value for Severe Chronic Uræmia. Lancet 1964, 283, 1000–1003. [Google Scholar] [CrossRef]
- Giordano, C. The Role of Diet in Renal Disease. Hosp. Pract. 1977, 12, 113–119. [Google Scholar] [CrossRef]
- Giordano, M.; Ciarambino, T.; Castellino, P.; Paolisso, G. Light and shadows of dietary protein restriction in elderly with Chronic Kidney Disease. Nutrition 2013, 29, 1090–1093. [Google Scholar] [CrossRef] [PubMed]
- D’Alessandro, C.; Rossi, A.; Innocenti, M.; Ricchiuti, G.; Bozzoli, L.; Sbragia, G.; Meola, M.; Cupisti, A. Dietary Protein Restriction for Renal Patients: Don’t Forget Protein-Free Foods. J. Ren. Nutr. 2013, 23, 367–371. [Google Scholar] [CrossRef] [PubMed]
- D’Alessandro, C.; Piccoli, G.B.; Calella, P.; Brunori, G.; Pasticci, F.; Egidi, M.F.; Capizzi, I.; Bellizzi, V.; Cupisti, A. “Dietaly”: Practical issues for the nutritional management of CKD patients in Italy. BMC Nephrol. 2016, 17, 102. [Google Scholar] [CrossRef] [PubMed]
- Chauveau, P.; Couzi, L.; Vendrely, B.; De Précigout, V.; Combe, C.; Fouque, D.; Aparicio, M. Long-term outcome on renal replacement therapy in patients who previously received a keto acid–supplemented very-low-protein diet. Am. J. Clin. Nutr. 2009, 90, 969–974. [Google Scholar] [CrossRef]
- Adaptive Response to a Low-Protein Diet in Predialysis Chronic Renal Failure Patients. Available online: https://pubmed.ncbi.nlm.nih.gov/11373349/ (accessed on 28 August 2020).
- Nutritional Diet Therapy in the Management of the Patient with Chronic Kidney Disease in Advanced Phase to Delay the Beginning and Reduce the Frequency of Dialysis. An Option also in the Pre-Emptive Transplant Program. Available online: https://pubmed.ncbi.nlm.nih.gov/30234228/ (accessed on 28 August 2020).
- Kopple, J.D.; Modification of Diet in Renal Disease Study Group; Levey, A.S.; Greene, T.; Chumlea, W.C.; Gassman, J.J.; Hollinger, D.L.; Maroni, B.J.; Merrill, D.; Scherch, L.K.; et al. Effect of dietary protein restriction on nutritional status in the Modification of Diet in Renal Disease Study. Kidney Int. 1997, 52, 778–791. [Google Scholar] [CrossRef]
- Obi, Y.; Qader, H.; Kovesdy, C.P.; Kalantar-Zadeh, K. Latest consensus and update on protein-energy wasting in chronic kidney disease. Curr. Opin. Clin. Nutr. Metab. Care 2015, 18, 254–262. [Google Scholar] [CrossRef]
- Shah, B.V.; Patel, Z.M. Role of low protein diet in management of different stages of chronic kidney disease—Practical aspects. BMC Nephrol. 2016, 17, 1–9. [Google Scholar] [CrossRef]
- Rhee, C.M.; Ahmadi, S.-F.; Kovesdy, C.P.; Kalantar-Zadeh, K. Low-protein diet for conservative management of chronic kidney disease: A systematic review and meta-analysis of controlled trials. J. Cachex Sarcopenia Muscle 2017, 9, 235–245. [Google Scholar] [CrossRef]
- Fois, A.; Chatrenet, A.; Cataldo, E.; Lippi, F.; Kaniassi, A.; Vigreux, J.; Froger, L.; Mongilardi, E.; Capizzi, I.; Biolcati, M.; et al. Moderate Protein Restriction in Advanced CKD: A Feasible Option in An Elderly, High-Comorbidity Population. A Stepwise Multiple-Choice System Approach. Nutrients 2018, 11, 36. [Google Scholar] [CrossRef]
- Levey, A.S.; Stevens, L.A.; Schmid, C.H.; Zhang, Y.L.; Castro, A.F., 3rd; Feldman, H.I.; Kusek, J.W.; Eggers, P.; Van Lente, F.; Greene, T.; et al. A New Equation to Estimate Glomerular Filtration Rate. Ann. Intern. Med. 2009, 150, 604–612. [Google Scholar] [CrossRef]
- Charlson, M.E.; Pompei, P.; Ales, K.L.; MacKenzie, C. A new method of classifying prognostic comorbidity in longitudinal studies: Development and validation. J. Chronic Dis. 1987, 40, 373–383. [Google Scholar] [CrossRef]
- Kalantar-Zadeh, K.; Kopple, J.D.; Block, G.; Humphreys, M.H. A Malnutrition-Inflammation Score is correlated with morbidity and mortality in maintenance hemodialysis patients. Am. J. Kidney Dis. 2001, 38, 1251–1263. [Google Scholar] [CrossRef] [PubMed]
- Skevington, S.; Lotfy, M.; O’Connell, K. The World Health Organization’s WHOQOL-BREF quality of life assessment: Psychometric properties and results of the international field trial. A Report from the WHOQOL Group. Qual. Life Res. 2004, 13, 299–310. [Google Scholar] [CrossRef] [PubMed]
- Piccoli, G.B.; Ferraresi, M.; Deagostini, M.C.; Vigotti, F.N.; Consiglio, V.; Scognamiglio, S.; Moro, I.; Clari, R.; Fassio, F.; Biolcati, M.; et al. Vegetarian low-protein diets supplemented with keto analogues: A niche for the few or an option for many? Nephrol. Dial. Transpl. 2013, 28, 2295–2305. [Google Scholar] [CrossRef] [PubMed]
- Cupisti, A.; Avesani, C.M.; D’Alessandro, C.; Garibotto, G. Nutritional management of kidney diseases: An unmet need in patient care. J. Nephrol. 2020, 1, 3. [Google Scholar] [CrossRef]
- Thilly, N. Low-protein diet in chronic kidney disease: From questions of effectiveness to those of feasibility. Nephrol. Dial. Transpl. 2013, 28, 2203–2205. [Google Scholar] [CrossRef]
- Hetherington, M.M. The physiological-psychological dichotomy in the study of food intake. Proc. Nutr. Soc. 2002, 61, 497–507. [Google Scholar] [CrossRef]
- Kamphuis, C.B.M.; Jansen, T.; MacKenbach, J.P.; Van Lenthe, F.J. Bourdieu’s Cultural Capital in Relation to Food Choices: A Systematic Review of Cultural Capital Indicators and an Empirical Proof of Concept. PLoS ONE 2015, 10, e0130695. [Google Scholar] [CrossRef]
- Piccoli, G.B.; Nazha, M.; Capizzi, I.; Vigotti, F.N.; Scognamiglio, S.; Consiglio, V.; Mongilardi, E.; Biolcati, M.; Avagnina, P.; Versino, E. Diet as a system: An observational study investigating a multi-choice system of moderately restricted low-protein diets. BMC Nephrol. 2016, 17, 197. [Google Scholar] [CrossRef]

| Proposed | Not Proposed | p | Accepted | Refused | p | |
|---|---|---|---|---|---|---|
| n | 171 | 49 | 138 | 33 | ||
| Gender, n (%) | 0.006 | 0.861 | ||||
| males, n (%) | 117 (68.42%) | 23 (46.94%) | 94 (68.12%) | 23 (69.70%) | ||
| females, n (%) | 54 (31.58%) | 26 (53.06%) | 44 (31.88%) | 10 (30.30%) | ||
| Age, median (min–max) | 77 (25–103) | 79 (27–95) | 0.156 | 73 (25–97) | 83 (55–103) | <0.001 |
| BMI (kg/m2), median (min–max) | 28.25(17.43–51.20) | 28.67(19.81–38.38) | 0.978 | 28.73 (18.56–51.20) | 26.56 (17.43–44.29) | 0.051 |
| Caucasian, n (%) | 165 (96.49%) | 47 (95.92%) | 0.850 | 132 (95.65%) | 33 (100%) | 0.223 |
| Charlson Comorbidity Index, median (min–max) | 7 (2–17) | 8 (2–14) | 0.299 | 7 (2–17) | 8 (3–13) | 0.008 |
| SGA score, n (%) | <0.001 | 0.016 | ||||
| SGA A | 154 (90.06%) | 31 (63.27%) | 128 (92.75%) | 26 (78.79%) | ||
| SGA B | 17 (9.94%) | 17 (34.69%) | 10 (7.25%) | 7 (21.21%) | ||
| SGA C | 0 | 1 (2.04%) | 0 | 0 | ||
| MIS score, median (min–max) | 4 (0–12) | 6 (1–13) | <0.001 | 4 (0–12) | 5 (1–12) | 0.010 |
| sCreatinine (mg/dL), median (min–max) | 2.14 (0.9–9.14) | 2.30 (1.25–14.69) | 0.204 | 2.18 (0.90–9.14) | 1.91 (1.05–5.44) | 0.055 |
| eGFR-EPI (mL/min), median (min–max) | 27 (6–68) | 21 (3–59) | 0.021 | 26.00 (6.00–60.00) | 30.00 (7.00–68.00) | 0.145 |
| eGFR stage, n (%) | <0.001 | 0.026 | ||||
| Stage 3a * | 14 (8.19%) | 4 (8.16%) | 7 (5.07%) | 7 (21.21%) | ||
| Stage 3b | 59 (34.50%) | 15 (30.61%) | 49 (35.51%) | 10 (30.30%) | ||
| Stage 4 | 79 (46.20%) | 13 (26.53%) | 66 (47.83%) | 13 (39.39%) | ||
| Stage 5 | 19 (11.11%) | 17 (34.69%) | 16 (11.59%) | 3 (9.09%) | ||
| Proteinuria (g/day), median (min–max) | 0.4 (<0.01–8.10) | 0.3 (<0.01–6.02) | 0.563 | 0.50 (<0.01–8.10) | 0.20 (<0.01–3.10) | 0.285 |
| Diabetes, n (%) | 73 (42.69%) | 18 (36.73%) | 0.455 | 60 (43.48%) | 13 (39.39%) | 0.670 |
| Protein intake, n (%) | <0.001 | 0.200 | ||||
| Unrestricted, n (%) | 0 | 12 (24.49%) | 0 | 0 | ||
| 0.8 g/kg/day, n (%) | 102 (59.65%) | 21 (42.86%) | 78 (56.52%) | 24 (72.73%) | ||
| 0.6 g/kg/day, n (%) | 45 (26.32%) | 9 (18.37%) | 40 (28.99%) | 5 (15.15%) | ||
| 0.6 g/kg/day supplemented, n (%) | 24 (14.03%) | 7 (14.29%) | 20 (14.49%) | 4 (12.12%) |
| Low Willingness to Change | Moderate Willingness to Change | High Willingness to Change | p | |
|---|---|---|---|---|
| N 130 | 33 (25.38%) | 49 (37.69%) | 48 (36.92%) | |
| Gender, n (%) | 0.987 | |||
| males | 22 (66.67%) | 32 (65.31%) | 32 (66.67%) | |
| females | 11 (33.33%) | 17 (34.69%) | 16 (33.33%) | |
| Age, median (min–max) | 77 (25–97) | 72 (35–96) | 74 (37–97) | 0.897 |
| BMI (kg/m2), median (min–max) | 28.25 (20.31–51.20) | 28.04 (18.56–51.17) | 29.02 (19.33–44.20) | 0.951 |
| Caucasian, n (%) | 32 (96.97%) | 47 (95.92%) | 45 (93.75%) | 0.774 |
| Charlson score, median (min–max) | 7 (2–13) | 7 (2–14) | 7 (2–13) | 0.746 |
| SGA score, n (%) | 0.999 | |||
| SGA A | 31 (93.94%) | 46 (93.88%) | 45 (93.75%) | |
| SGA B | 2 (6.06%) | 3 (6.12%) | 3 (6.25%) | |
| MIS score, median (min–max) | 4 (1–8) | 4 (0–10) | 3.5 (1–9) | 0.129 |
| sCreatinine (mg/dL), median (min–max) | 2.13 (1.15–5.77) | 2.40 (1.31–5.40) | 2.13 (0.90–9.14) | 0.824 |
| eGFR-EPI (mL/min), median (min–max) | 25 (7–58) | 24 (10–55) | 28 (6–60) | 0.648 |
| eGFR stages, n (%) | 0.656 | |||
| Stage 3a * | 1 (3.03%) | 4 (8.16%) | 2 (4.17%) | |
| Stage 3b | 14 (42.42%) | 12 (24.49%) | 18 (37.50%) | |
| Stage 4 | 15 (45.45%) | 26 (53.06%) | 23 (47.92%) | |
| Stage 5 | 3 (9.09%) | 7 (14.29%) | 5 (10.41%) | |
| Proteinuria (g/day), median (min–max) | 0.20 (0–6.50) | 0.80 (0.10–7.70) | 0.35 (0–8.10) | 0.111 |
| Diabetes, n (%) | 16 (48.48%) | 22 (44.90%) | 18 (37.50%) | 0.586 |
| Protein intake, n (%) | 0.199 | |||
| Unrestricted, n (%) | 0 | 0 | 0 | |
| 0.8 g/kg/d, n (%) | 24 (72.73%) | 23 (46.94%) | 27 (56.25%) | |
| 0.6 g/kg/d, n (%) | 7 (21.21%) | 16 (32.65%) | 14 (29.17%) | |
| 0.6 g/kg/d, Ketosteril, n (%) | 2 (6.06%) | 10 (20.41%) | 7 (14.58%) | |
| WHOQOL-BREF domains, median (min–max) | ||||
| Domain 1: physical health, median (min–max) | 3.33 (2.17–4.00) | 3.33 (2–4.33) | 3.42 (2.14–4.71) | 0.882 |
| Domain 2: psychological, median (min–max) | 3.67 (2.33–4.5) | 4 (2–5) | 4 (2.17–5) | 0.557 |
| Domain 3: social relationships, median (min–max) | 3.67 (2.67–4.50) | 4 (2–5) | 4 (1.67–5) | 0.619 |
| Domain 4: environment, median (min–max) | 3.63 (2.88–4.75) | 3.63 (2.75–4.63) | 3.82 (2.25–4.75) | 0.790 |
| 95% Confidence Intervals | |||||
|---|---|---|---|---|---|
| Odds-Ratio | Lower | Higher | p-Value | ||
| Step 1 | Gender (females/males) | 0.643 | 0.257 | 1.608 | 0.345 |
| Age (≥80 years) | 5.408 | 1.894 | 15.447 | 0.002 | |
| Charlson (≥7) | 1.039 | 0.300 | 3.600 | 0.952 | |
| SGA (B vs. A) | 1.856 | 0.580 | 5.938 | 0.297 | |
| Step 2 | Gender (females/males) | 0.643 | 0.257 | 1.607 | 0.345 |
| Age (≥80 years) | 5.503 | 2.263 | 13.384 | <0.001 | |
| SGA (B vs. A) | 1.856 | 0.580 | 5.935 | 0.297 | |
| Step 3 | Age (≥80 years) | 5.308 | 2.197 | 12.826 | <0.001 |
| SGA (B vs. A) | 1.639 | 0.532 | 5.051 | 0.390 | |
| Step 4 | Age (≥80 years) | 5.891 | 2.527 | 13.737 | <0.001 |
| 95% Confidence Intervals | |||||
|---|---|---|---|---|---|
| Odds Ratio | Lower | Higher | p-Value | ||
| Step 1 | Gender (females/males) | 0.996 | 0.419 | 2.367 | 0.992 |
| Age (≥80 years) | 0.814 | 0.296 | 2.239 | 0.690 | |
| SGA (B vs. A) | 1.043 | 0.177 | 6.135 | 0.963 | |
| Charlson (≥7) | 1.292 | 0.506 | 3.298 | 0.593 | |
| Step 2 | Age (≥80 years) | 0.814 | 0.298 | 2.223 | 0.687 |
| SGA (B vs. A) | 1.041 | 0.183 | 5.935 | 0.964 | |
| Charlson (≥7) | 1.292 | 0.508 | 3.289 | 0.591 | |
| Step 3 | Age (≥80 years) | 0.819 | 0.313 | 2.140 | 0.684 |
| Charlson (≥7) | 1.291 | 0.507 | 3.285 | 0.592 | |
| Step 4 | Charlson (≥7) | 1.180 | 0.513 | 2.714 | 0.696 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Longhitano, E.; Trabace, T.; Fois, A.; Chatrenet, A.; Moio, M.R.; Lippi, F.; Vigreux, J.; Beaumont, C.; Santoro, D.; Torreggiani, M.; et al. Ready to Change: Attitudes of an Elderly CKD Stage 3–5 Population towards Testing Protein-Free Food. Nutrients 2020, 12, 3519. https://doi.org/10.3390/nu12113519
Longhitano E, Trabace T, Fois A, Chatrenet A, Moio MR, Lippi F, Vigreux J, Beaumont C, Santoro D, Torreggiani M, et al. Ready to Change: Attitudes of an Elderly CKD Stage 3–5 Population towards Testing Protein-Free Food. Nutrients. 2020; 12(11):3519. https://doi.org/10.3390/nu12113519
Chicago/Turabian StyleLonghitano, Elisa, Tiziana Trabace, Antioco Fois, Antoine Chatrenet, Maria Rita Moio, Francoise Lippi, Jerome Vigreux, Coralie Beaumont, Domenico Santoro, Massimo Torreggiani, and et al. 2020. "Ready to Change: Attitudes of an Elderly CKD Stage 3–5 Population towards Testing Protein-Free Food" Nutrients 12, no. 11: 3519. https://doi.org/10.3390/nu12113519
APA StyleLonghitano, E., Trabace, T., Fois, A., Chatrenet, A., Moio, M. R., Lippi, F., Vigreux, J., Beaumont, C., Santoro, D., Torreggiani, M., & Piccoli, G. B. (2020). Ready to Change: Attitudes of an Elderly CKD Stage 3–5 Population towards Testing Protein-Free Food. Nutrients, 12(11), 3519. https://doi.org/10.3390/nu12113519








