Food Habits and Screen Time Play a Major Role in the Low Health Related to Quality of Life of Ethnic Ascendant Schoolchildren
Abstract
1. Introduction
2. Materials and Methods
2.1. Ethnicity Classification
2.2. Anthropometry Measurement
2.3. Cardiovascular Outcomes
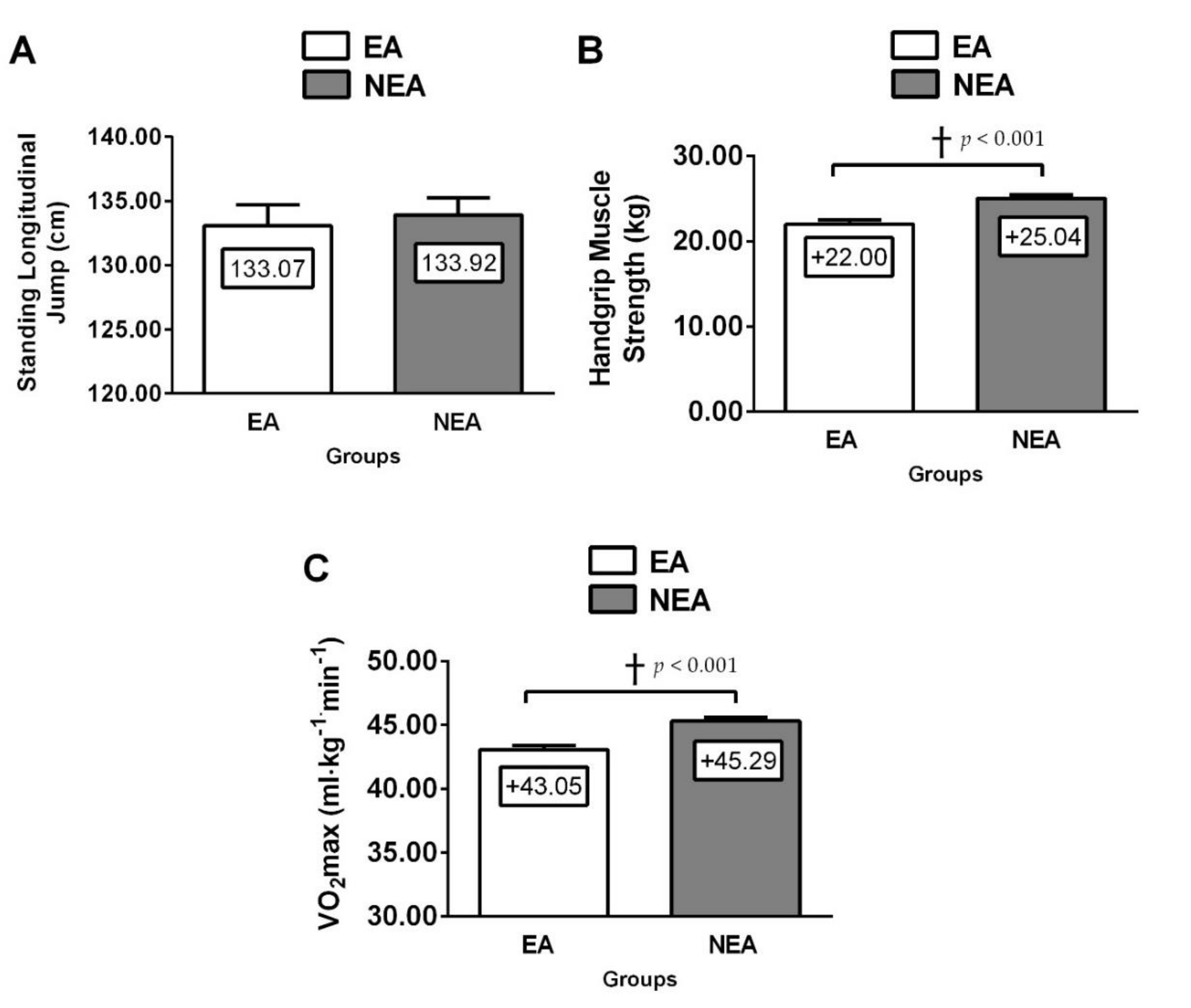
2.4. Physical Fitness
2.5. Children’s Food Habits
2.6. Physical Activity Level
2.7. ScreenTime
2.8. Health-Related Quality of Life (HRQoL) Markers
2.9. Statistical Analysis
3. Results
3.1. Differences between EA vs. NEA
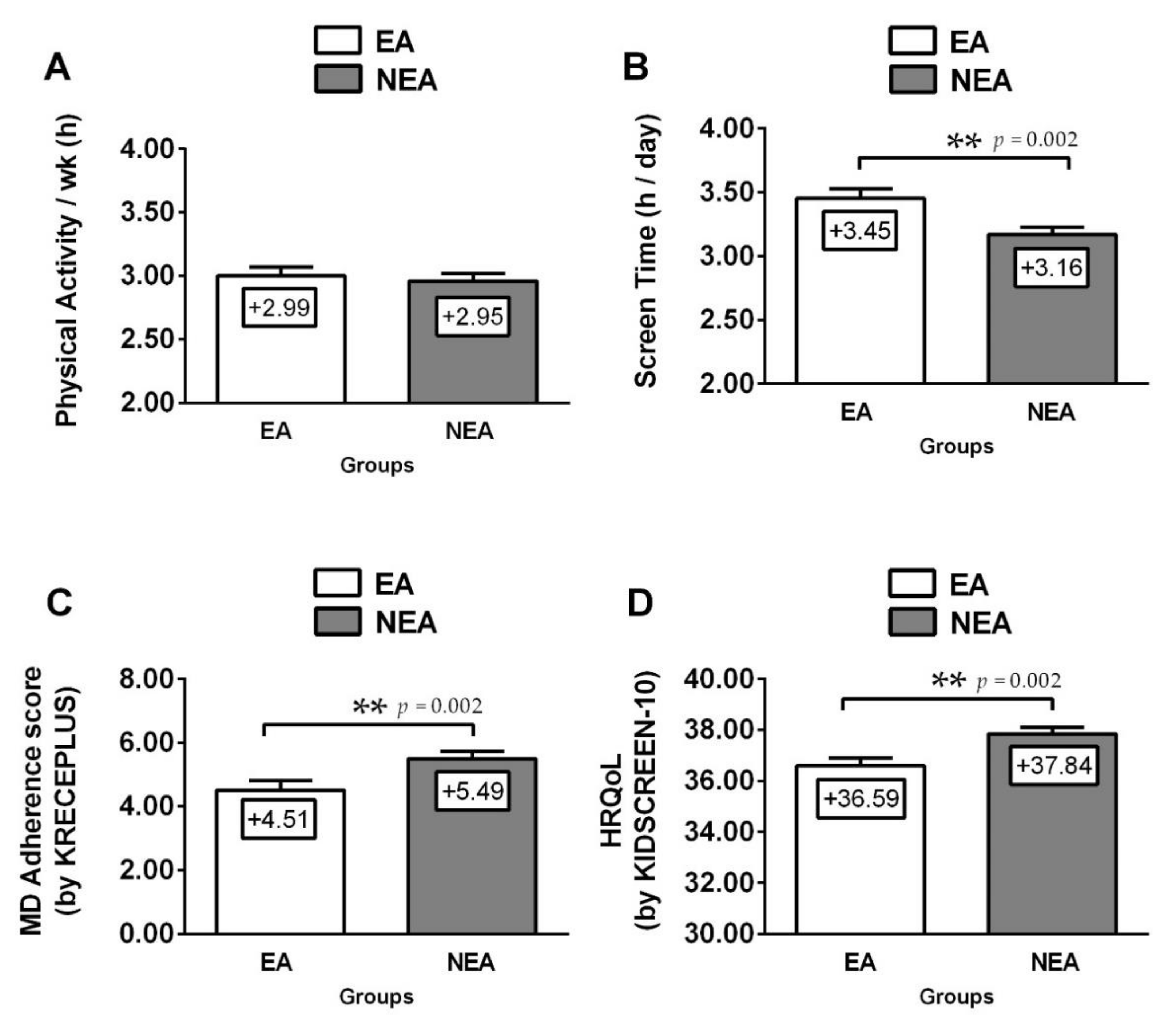
3.2. Lifestyle Differences between EA vs. NEA
3.3. Foods Habits Differences between EA vs. NEA
3.4. Association of Variables with HRQoL
3.5. Association of Variables with Ethnic Ascendant
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Garrido-Miguel, M.; Cavero-Redondo, I.; Álvarez-Bueno, C.; Rodríguez-Artalejo, F.; Moreno, L.A.; Ruiz, J.R.; Ahrens, W.; Martínez-Vizcaíno, V. Prevalence and Trends of Overweight and Obesity in European Children From 1999 to 2016. JAMA Pediatr. 2019, 173, e192430. [Google Scholar] [CrossRef]
- Ntuk, U.E.; Gill, J.M.; Mackay, D.F.; Sattar, N.; Pell, J.P. Ethnic-Specific Obesity Cutoffs for Diabetes Risk: Cross-sectional Study of 490,288 UK Biobank Participants. Diabetes Care 2014, 37, 2500–2507. [Google Scholar] [CrossRef]
- Alvarez, C.; Flores-Opazo, M.; Mancilla, R.; Martínez-Salazar, C.; Mangiamarchi, P.; Sade-Calles, F.; Ramirez-Campillo, R. Gender differences in blood pressure and body composition in schoolchildren ascendants from Amerindian and European. Ethn. Heal. 2019, 1–12. [Google Scholar] [CrossRef]
- Farhud, D.D. Impact of Lifestyle on Health. Iran. J. Public Heal. 2015, 44, 1442–1444. [Google Scholar]
- Wake, M.; Hughes, E.K.; Collins, C.; Poulakis, Z. Parent-Reported Health-Related Quality of Life in Children With Congenital Hearing Loss: A Population Study. Ambul. Pediatr. 2004, 4, 411–417. [Google Scholar] [CrossRef] [PubMed]
- Michel, G.; The KIDSCREEN Group; Bisegger, C.; Fuhr, D.C.; Abel, T. Age and gender differences in health-related quality of life of children and adolescents in Europe: A multilevel analysis. Qual. Life Res. 2009, 18, 1147–1157. [Google Scholar] [CrossRef] [PubMed]
- Degoy, E.; Berra, S. Differences in health-related quality of life by academic performance in children of the city of Cordoba-Argentina. Qual. Life Res. 2018, 27, 1463–1471. [Google Scholar] [CrossRef] [PubMed]
- WHO. World Recommendations for Physical Activity and Health. Ginebra, Suiza. 2010. Available online: http://apps.who.int/iris/bitstream/10665/44441/1/9789243599977_spa.pdf (accessed on 3 January 2020).
- Stiglic, N.; Viner, R. Effects of screentime on the health and well-being of children and adolescents: A systematic review of reviews. BMJ Open 2019, 9, e023191. [Google Scholar] [CrossRef] [PubMed]
- Roberge, J.-B.; Van Hulst, A.; Barnett, T.; Drapeau, V.; Benedetti, A.; Tremblay, A.; Henderson, M. Lifestyle Habits, Dietary Factors and the Metabolically Unhealthy Obese Phenotype in Youth. J. Pediatr. 2019, 204, 46–52.e1. [Google Scholar] [CrossRef]
- Muros, J.J.; Cofre-Bolados, C.; Arriscado, D.; Zurita, F.; Knox, E. Mediterranean diet adherence is associated with lifestyle, physical fitness and mental wellness among 10-y-olds in Chile. Nutrients 2017, 35, 87–92. [Google Scholar] [CrossRef]
- Ferrer-Cascales, R.; Albaladejo-Blázquez, N.; Ruiz-Robledillo, N.; Clement-Carbonell, V.; Sánchez-SanSegundo, M.; Zaragoza-Martí, A. Higher Adherence to the Mediterranean Diet is Related to More Subjective Happiness in Adolescents: The Role of Health-Related Quality of Life. Nutrients 2019, 11, 698. [Google Scholar] [CrossRef] [PubMed]
- Dinu, M.; Pagliai, G.; Casini, A.; Sofi, F. Mediterranean diet and multiple health outcomes: An umbrella review of meta-analyses of observational studies and randomised trials. Eur. J. Clin. Nutr. 2018, 72, 30–43. [Google Scholar] [CrossRef] [PubMed]
- Aguilar-Farias, N.; Miranda-Marquez, S.; Sadarangani, K.P.; Martino-Fuentealba, P.; Cristi-Montero, C.; Carcamo-Oyarzun, J.; Delgado-Floody, P.; Chandia-Poblete, D.; Mella-Garcia, C.; Rodríguez-Rodríguez, F.; et al. Results from Chile’s 2018 Report Card on Physical Activity for Children and Youth. J. Phys. Act. Heal. 2018, 15, S331–S332. [Google Scholar] [CrossRef] [PubMed]
- Garber, M.D.; Sajuria, M.; Lobelo, F. Geographical Variation in Health-Related Physical Fitness and Body Composition among Chilean 8th Graders: A Nationally Representative Cross-Sectional Study. PLOS ONE 2014, 9, e108053. [Google Scholar] [CrossRef]
- Schnettler, B.; Miranda, H.; Sepúlveda, J.; Denegri, M.; Mora, M.; Lobos, G.A. Satisfaction with Life and Food-Related Life in Persons of the Mapuche Ethnic Group in Southern Chile: A Comparative Analysis Using Logit and Probit Models. J. Happiness Stud. 2011, 13, 225–246. [Google Scholar] [CrossRef]
- Satterthwaite, D.; McGranahan, G.; Tacoli, C. Urbanization and its implications for food and farming. Philos. Trans. R. Soc. B Biol. Sci. 2010, 365, 2809–2820. [Google Scholar] [CrossRef]
- Álvarez, C.; Ramírez-Campillo, R.; Sáez-Lafourcade, R.; Delgado-Floody, P.; Martínez-Salazar, C.; Celis-Morales, C.; Ramírez-Vélez, R.; Alonso-Martínez, A.; Izquierdo, M. Association of physical inactivity with blood pressure and cardiovascular risk factors in Amerindian schoolchildren. Am. J. Hum. Biol. 2019, 31, e23273. [Google Scholar] [CrossRef]
- Álvarez, C.; Lucia, A.; Ramírez-Campillo, R.; Martínez-Salazar, C.; Delgado-Floody, P.; Cadore, E.L.; Alonso-Martínez, A.M.; Izquierdo, M. Low sleep time is associated with higher levels of blood pressure and fat mass in Amerindian schoolchildren. Am. J. Hum. Biol. 2019, 31, e23303. [Google Scholar] [CrossRef]
- Elacqua, G. The impact of school choice and public policy on segregation: Evidence from Chile. Int. J. Educ. Dev. 2012, 32, 444–453. [Google Scholar] [CrossRef]
- Morgan, R.O.; Wei, I.I.; Virnig, B.A. Improving Identification of Hispanic Males in Medicare. Med. Care 2004, 42, 810–816. [Google Scholar] [CrossRef]
- Centers for Disease Control and Prevention. Overweight and Obesity; Defining Overweight and Obesity. 2010. Available online: https://www.cdc.gov/obesity/childhood/defining.html (accessed on 10 June 2018).
- Schröder, H.; Ribas, L.; Koebnick, C.; Funtikova, A.; Gomez, S.F.; Fíto, M.; Perez-Rodrigo, C.; Serra-Majem, L. Prevalence of Abdominal Obesity in Spanish Children and Adolescents. Do We Need Waist Circumference Measurements in Pediatric Practice? PLoS ONE 2014, 9, e87549. [Google Scholar] [CrossRef] [PubMed]
- Chung, I.H.; Park, S.; Park, M.J.; Yoo, E.-G. Waist-to-Height Ratio as an Index for Cardiometabolic Risk in Adolescents: Results from the 1998-2008 KNHANES. Yonsei. Med. J. 2016, 57, 658–663. [Google Scholar] [CrossRef] [PubMed]
- Falkner, B.; Daniels, S.R. Summary of the Fourth Report on the Diagnosis, Evaluation and Treatment of High Blood Pressure in Children and Adolescents. Hypertension 2004, 44, 387–388. [Google Scholar] [CrossRef] [PubMed]
- Ruiz, J.R.; Espana Romero, V.; Castro Pinero, J.; Artero, E.G.; Ortega, F.B.; Cuenca, M.; Jimenez, D.; Chillon, P.; Girela, M.J.; Mora, J.; et al. Bateria ALPHA-Fitness: Test de campo para la evaluacion de la condicion fisica relacionada con la salud en ninos y adolescentes. Nutr. Hosp. 2011, 26, 1210–1214. [Google Scholar] [CrossRef] [PubMed]
- Léger, L.A.; Mercier, D.; Gadoury, C.; Lambert, J. The multistage 20 metre shuttle run test for aerobic fitness. J. Sports Sci. 1988, 6, 93–101. [Google Scholar] [CrossRef]
- Majem, L.S.; Barba, L.R.; Aranceta-Bartrina, J.; Aranceta, J.; Santana, P.S.; Quintana, L.P. Obesidad infantil y juvenil en España. Resultados del Estudio enKid (1998-2000). Medicina Clínica 2003, 121, 725–732. [Google Scholar] [CrossRef]
- Manchola-González, J.; Bagur-Calafat, C.; Girabent-Farrés, M. Fiabilidad de la versión española del Cuestionario de actividad física PAQ-C / Reliability of the Spanish Version of Questionnaire of Physical Activity PAQ-C. Revista Internacional de Medicina y Ciencias de la Actividad Física y del Deporte 2017, 65. [Google Scholar] [CrossRef]
- Ravens-Sieberer, U.; Erhart, M.; Rajmil, L.; Herdman, M.; Auquier, P.; Bruil, J.; Power, M.; Duer, W.; Abel, T.; Czemy, L. Reliability, construct and criterion validity of the KIDSCREEN-10 score: A short measure for children and adolescents’ well-being and health-related quality of life. Qual. Life Res. 2010, 19, 1487–1500. [Google Scholar] [CrossRef]
- Wallander, J.L.; Fradkin, C.; Elliott, M.N.; Cuccaro, P.M.; Emery, S.T.; Schuster, M.A. Racial/ethnic disparities in health-related quality of life and health status across pre-, early- and mid-adolescence: A prospective cohort study. Qual. Life Res. 2019, 28, 1761–1771. [Google Scholar] [CrossRef]
- Gu, X.; Zhang, T.; Chu, T.L.; Wang, J.; Zhang, X.; Nelson, L.; Brown, K. Exploring Racial Disparities in Physical Activity and Quality of Life Through an Expectancy-Value Perspective. J. Racial Ethn. Heal. Disparities 2019, 6, 973–980. [Google Scholar] [CrossRef]
- Wallander, J.L.; Taylor, W.C.; Grunbaum, J.A.; Franklin, F.A.; Harrison, G.G.; Kelder, S.H.; Schuster, M.A. Weight Status, Quality of Life and Self-concept in African American, Hispanic and White Fifth-grade Children. Obesity 2009, 17, 1363–1368. [Google Scholar] [CrossRef] [PubMed]
- Evaristo, O.S.; Moreira, C.M.M.; Lopes, L.; Abreu, S.; Agostinis-Sobrinho, C.; Oliveira-Santos, J.; Póvoas, S.; Oliveira, A.; Santos, R.; Mota, J. Associations between physical fitness and adherence to the Mediterranean diet with health-related quality of life in adolescents: Results from the LabMed Physical Activity Study. Eur. J. Public Heal. 2018, 28, 631–635. [Google Scholar] [CrossRef] [PubMed]
- Suchert, V.; Hanewinkel, R.; Isensee, B. Sedentary behavior and indicators of mental health in school-aged children and adolescents: A systematic review. Prev. Med. 2015, 76, 48–57. [Google Scholar] [CrossRef] [PubMed]
- Spengler, S.; Woll, A. The More Physically Active, the Healthier? The Relationship Between Physical Activity and Health-Related Quality of Life in Adolescents: The MoMo Study. J. Phys. Act. Heal. 2013, 10, 708–715. [Google Scholar] [CrossRef]
- Iannotti, R.J.; Kogan, M.D.; Janssen, I.; Boyce, W.F. Patterns of Adolescent Physical Activity, Screen-Based Media Use and Positive and Negative Health Indicators in the U.S. and Canada. J. Adolesc. Heal. 2009, 44, 493–499. [Google Scholar] [CrossRef]
- Donin, A.S.; Nightingale, C.M.; Owen, C.G.; Rudnicka, A.R.; McNamara, M.C.; Prynne, C.J.; Stephen, A.M.; Cook, D.G.; Whincup, P.H. Nutritional composition of the diets of South Asian, black African-Caribbean and white European children in the United Kingdom: The Child Heart and Health Study in England (CHASE). Br. J. Nutr. 2010, 104, 276–285. [Google Scholar] [CrossRef]
- Kant, A.K.; I Graubard, B. Race-ethnic, family income and education differentials in nutritional and lipid biomarkers in US children and adolescents: NHANES 2003–2006. Am. J. Clin. Nutr. 2012, 96, 601–612. [Google Scholar] [CrossRef]
- Nightingale, C.M.; Donin, A.S.; Kerry, S.R.; Owen, C.G.; Rudnicka, A.R.; Brage, S.; Westgate, K.L.; Ekelund, U.; Cook, D.G.; Whincup, P.H. Cross-sectional study of ethnic differences in physical fitness among children of South Asian, black African–Caribbean and white European origin: The Child Heart and Health Study in England (CHASE). BMJ Open 2016, 6, e011131. [Google Scholar] [CrossRef]
- Redondo-Tébar, A.; Ruíz-Hermosa, A.; Martínez-Vizcaíno, V.; Cobo-Cuenca, A.I.; Bermejo-Cantarero, A.; Cavero-Redondo, I.; Sánchez-López, M. Associations between health-related quality of life and physical fitness in 4–7-year-old Spanish children: The MOVIKIDS study. Qual. Life Res. 2019, 28, 1751–1759. [Google Scholar] [CrossRef]
| Parameters/Outcomes | Total | EA | NEA | EA vs. NEA p-Value |
|---|---|---|---|---|
| Total, (n) | 619 | 236 | 383 | |
| Girls, (n/%) | 273 (100%) | 104 (38.1%) | 169 (61.9%) | p = 0.528 |
| Boys, (n/%) | 346 (100%) | 132 (38.2%) | 214 (61.8%) | |
| Age (years) | 11.72 ± 1.07 | 11.64 ± 1.00 | 11.77 ± 1.12 | p = 0.174 |
| Anthropometric | ||||
| Weight (kg) | 52.3 ± 14.1 | 52.5 ± 13.5 | 52.2 ± 14.7 | p = 0.826 |
| Height (cm) | 155.0 ± 0.10 | 154.0 ± 0.09 | 156.0 ± 0.11 | p =0.028 |
| Body mass index (kg/m2) | 21.57 ± 4.68 | 22.04 ± 4.75 | 21.28 ± 4.62 | p = 0.052 |
| Obesity prevalence ¶ | ||||
| Normal weight (n/%) | 312 (50.4) | 114 (48.3) | 198 (51.7) | p = 0.459 |
| Overweight (n/%) | 156 (25.2) | 66 (28.0) | 90 (23.5) | |
| Obesity (n/%) | 151 (24.4) | 56 (23.7) | 95 (24.8) | |
| Waist circumference (cm) | 73.40 ± 11.57 | 73.25 ± 11.46 | 73.49 ± 11.66 | p = 0.800 |
| WtHR (height /WC) (cm) | 0.47 ± 0.07 | 0.48 ± 0.07 | 0.47 ± 0.07 | p = 0.447 |
| Cardiovascular | ||||
| Systolic blood pressure (mmHg) | 119.22 ± 12.30 | 119.06 ± 12.72 | 119.32 ± 12.05 | p = 0.786 |
| Diastolic blood pressure (mmHg) | 79.85 ± 11.94 | 79.16 ± 12.14 | 80.28 ± 11.81 | p = 0.269 |
| Response | EA | NEA | p-Value |
|---|---|---|---|
| Skips breakfast | |||
| Yes | 16 (6.78%) | 4 (1.04%) | p < 0.001 |
| Consumes a dairy product for breakfast (yogurt, milk, etc.) | |||
| Yes | 187 (79.24%) | 335 (87.47%) | p = 0.005 |
| Consumes cereals or grains (bread, etc.) for breakfast | |||
| Yes | 73 (30.93%) | 167 (43.60%) | p < 0.001 |
| Has commercially baked goods or pastries for breakfast | |||
| Yes | 84 (35.59%) | 110 (28.72%) | p = 0.045 |
| Takes a fruit or fruit juice every day | |||
| Yes | 92 (38.98%) | 195 (50.91%) | p = 0.002 |
| Consumes a second fruit every day | |||
| Yes | 63 (26.69%) | 133 (34.73%) | p = 0.022 |
| Consumes a dairy product ˃1 time/day | |||
| Yes | 69 (29.24%) | 166 (43.34) | p < 0.001 |
| Consumes fresh or cooked vegetables regularly 1 time/day | |||
| Yes | 146 (61.86%) | 257 (67.10%) | p = 0.107 |
| Consumes fresh or cooked vegetables ˃1 time/day | |||
| Yes | 61 (25.85%) | 141 (36.81%) | p = 0.003 |
| Consumes fish regularly (2–3 times/week) | |||
| Yes | 98 (41.53%) | 177 (46.21%) | p = 0.145 |
| Eats at a fast food restaurant ≥1 time/week | |||
| Yes | 103 (43.64%) | 129 (33.68%) | p = 0.008 |
| Eats pulses (lentils, beans, more than once a week) | |||
| Yes | 146 (61.86%) | 257 (67.10%) | p = 0.107 |
| Consumes sweets and candy several times every day | |||
| Yes | 84 (35.59%) | 110 (28.72%) | p = 0.045 |
| Consumes pasta or rice almost every day (≥5/week) | |||
| Yes | 181 (76.69%) | 301 (78.59%) | p = 0.324 |
| Uses olive oil at home | |||
| Yes | 146 (61.86%) | 257 (67.10%) | p = 0.107 |
| Variables | Models | EA | p-Value | NEA | p-Value |
|---|---|---|---|---|---|
| Coefficient β (95% CI) | Coefficient β (95% CI) | ||||
| Anthropometrics parameters | |||||
| BMI (kg/m2) | Model 0 | 0.10 (−0.07, 0.27) | p = 0.253 | −0.02 (−0.14, 0.11) | p = 0.806 |
| Model 1 | 0.01 (−0.15, 0.18) | p = 0.862 | 0.04 (−0.08, 0.16) | p = 0.494 | |
| WC (cm) | Model 0 | −0.05 (−0.15, 0.05) | p = 0.340 | 0.04 (−0.03, 0.11) | p = 0.289 |
| Model 1 | 0.00 (−0.10, 0.10) | p = 0.942 | 0.06 (−0.03, 0.14) | p = 0.175 | |
| WtHR (WC/size) | Model 0 | 6.13 (−0.67, 22.93) | p = 0.473 | −11.32 (−22.37, −0.28) | p = 0.045 |
| Model 1 | 2.91(−13.29, 19.10) | p = 0.724 | −14.03 (−30.25, −3.21) | p = 0.032 | |
| Cardiovascular parameters | |||||
| SBP (mmHg) | Model 0 | 0.04 (0.00, 0.08) | p = 0.073 | −0.01 (−0.04, 0.03) | p = 0.666 |
| Model 1 | 0.02 (−0.02, 0.06) | p = 0.402 | 0.01 (−0.02, 0.04) | p = 0.537 | |
| DBP (mmHg) | Model 0 | 0.00 (−0.05, 0.04) | p = 0.914 | 0.00 (−0.03, 0.04) | p = 0.936 |
| Model 1 | 0.00 (−0.04, 0.05) | p = 0.907 | −0.01 (−0.04, 0.03) | p = 0.754 | |
| Physical fitness | |||||
| VO2max (mL/kg(min)) | Model 0 | 0.11 (0.02, 0.21) | p = 0.017 | 0.12 (0.05, 0.19) | p < 0.001 |
| Model 1 | 0.12 (0.03, 0.19) | p =0.018 | 0.13 (0.05, 0.21) | p =0.001 | |
| SJT (cm) | Model 0 | 0.00 (−0.01, 0.02) | p = 0.621 | 0.01 (0.00, 0.03) | p = 0.126 |
| Model 1 | 0.01 (−0.01, 0.03) | p = 0.263 | 0.01(−0.01, 0.02) | p = 0.434 | |
| Handgrip strength (kg) | Model 0 | 0.03 (−0.03, 0.09) | p = 0.274 | −0.04 (−0.08, 0.01) | p = 0.105 |
| Model 1 | 0.01 (−0.05, 0.07) | p = 0.645 | |||
| Lifestyle parameters | |||||
| Foods habits (score) | Model 0 | 0.11 (0.01, 0.21) | p = 0.034 | 0.01 (−0.07, 0.09) | p = 0.823 |
| Model 1 | 0.12 (0.04, 0.25) | p = 0.063 | 0.01 (−0.07, 0.09) | p = 0.763 | |
| Screen time (h/day) | Model 0 | −2.72 (−3.11, −2.32) | p <0.001 | −2.59 (−2.95, −2.24) | p < 0.001 |
| Model 1 | −2.60 (−3.01, −2.19) | p <0.001 | −2.57 (−2.90, −2.23) | p < 0.001 | |
| Physical activity (PAQ-C) | Model 0 | 0.35 (−0.18, 0.88) | p = 0.193 | −0.01 (−0.35, 0.34) | p = 0.966 |
| Model 1 | −0.08 (−0.54, 0.38) | p = 0.734 | 0.14 (−0.22, 0.49) | p = 0.454 | |
| Variable | Coefficient β (95% CI) | p-Value |
|---|---|---|
| Anthropometrics parameters | ||
| Body mass index (kg/m2) | ||
| Model 0 | 0.75 (−0.005 to 1.51) | p = 0.052 |
| Model 1 | 0.92 (−0.25 to 2.09) | p = 0.120 |
| Waist circumference (cm) | ||
| Model 0 | −0.24 (−2.12 to 1.63) | p = 0.800 |
| Model 1 | 2.08 (−0.80 to −4.97) | p = 0.150 |
| WtHR (WC/size) | ||
| Model 0 | 0.00 (−0.007 to 0.15) | p = 0.440 |
| Model 1 | 0.01 (−0.006 to 0.2) | p = 0.230 |
| Physical fitness | ||
| VO2max (ml/kg/min) | ||
| Model 0 | −2.24 (−3.14 to −1.33) | p < 0.001 |
| Model 1 | 0.71 (−0.64 to −2.07) | p = 0.300 |
| SLJ (cm) | ||
| Model 0 | −0.84 (−4.96 to 3.26) | p = 0.680 |
| Model 1 | −2.77 (−9.12 to 3.57) | p = 0.390 |
| Handgrip muscle strength (kg) | ||
| Model 0 | −3.03 (−4.36 to −1.70) | p < 0.001 |
| Model 1 | −2.74 (−4.80 to −0.68) | p = 0.009 |
| Physical activity level | ||
| Total Physical activity | ||
| Model 0 | −0.04 (−0.14 to 0.22) | p = 0.660 |
| Model 1 | −0.20 (−0.48 to 0.08) | p = 0.170 |
| Screen time | ||
| Model 0 | 0.28 (0.10 to −0.46) | p = 0.002 |
| Model 1 | 0.54 (0.26 to 0.82) | p < 0.001 |
| Children’s foods habits (Adherence to Mediterranean diet) | ||
| Krece Plus (score) | ||
| Model 0 | −0.18 (−1.93 to −0.43) | p = 0.002 |
| Model 1 | −2.07 (−3.22 to −0.92) | p < 0.001 |
| Health related to quality of life | ||
| HRQoL (raw score) | ||
| Model 0 | −1.24 (−2.02 to −0.47) | p = 0.002 |
| Model 1 | −2.54 (−3.73 to −1.34) | p < 0.001 |
| Variable | OR (95% CI) | p-Value |
|---|---|---|
| Anthropometric/health parameters | ||
| Obesity ¶ | 1.83 (0.97–3.46) | p = 0.061 |
| Cardiometabolic risk £ (WtHR ≥0.5) | 1.13 (0.65–1.97) | p = 0.640 |
| Hypertension ¥ ( ≥95th Percentile) | 1.50 (0.90–2.52) | p = 0.110 |
| Low nutritional level (≤5) | 3.28 (1.55–6.93) | p =0.002 |
| Screen time | ||
| 1 h | 1.0 | |
| 2 h | 1.03 (0.37–2.92) | p = 0.940 |
| 3 h | 2.18 (0.81–5.81) | p = 0.113 |
| 4 h | 2.44 (0.91–6.51) | p = 0.072 |
| 5 h | 5.34 (1.74–16.4) | p =0.003 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Delgado-Floody, P.; Caamaño-Navarrete, F.; Guzmán-Guzmán, I.P.; Jerez-Mayorga, D.; Martínez-Salazar, C.; Álvarez, C. Food Habits and Screen Time Play a Major Role in the Low Health Related to Quality of Life of Ethnic Ascendant Schoolchildren. Nutrients 2020, 12, 3489. https://doi.org/10.3390/nu12113489
Delgado-Floody P, Caamaño-Navarrete F, Guzmán-Guzmán IP, Jerez-Mayorga D, Martínez-Salazar C, Álvarez C. Food Habits and Screen Time Play a Major Role in the Low Health Related to Quality of Life of Ethnic Ascendant Schoolchildren. Nutrients. 2020; 12(11):3489. https://doi.org/10.3390/nu12113489
Chicago/Turabian StyleDelgado-Floody, Pedro, Felipe Caamaño-Navarrete, Iris Paola Guzmán-Guzmán, Daniel Jerez-Mayorga, Cristian Martínez-Salazar, and Cristian Álvarez. 2020. "Food Habits and Screen Time Play a Major Role in the Low Health Related to Quality of Life of Ethnic Ascendant Schoolchildren" Nutrients 12, no. 11: 3489. https://doi.org/10.3390/nu12113489
APA StyleDelgado-Floody, P., Caamaño-Navarrete, F., Guzmán-Guzmán, I. P., Jerez-Mayorga, D., Martínez-Salazar, C., & Álvarez, C. (2020). Food Habits and Screen Time Play a Major Role in the Low Health Related to Quality of Life of Ethnic Ascendant Schoolchildren. Nutrients, 12(11), 3489. https://doi.org/10.3390/nu12113489








