Food Consumption Patterns and Nutrient Intakes of Children and Adolescents in the Eastern Mediterranean Region: A Call for Policy Action
Abstract
1. Introduction
2. Approach
3. Results
3.1. Food Consumption Patterns Amongst Children and Adolescents in the EMR
3.1.1. School-Aged Children
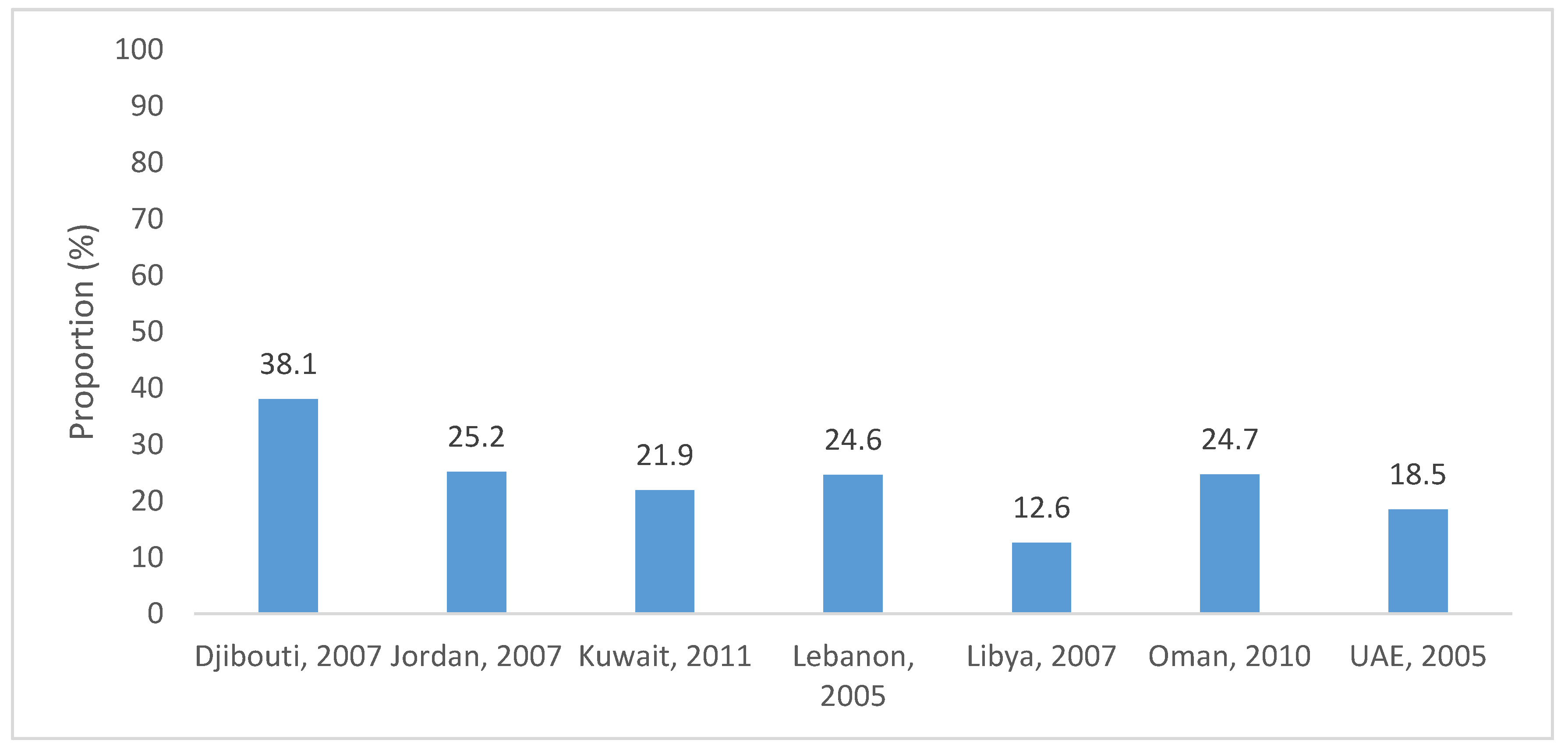
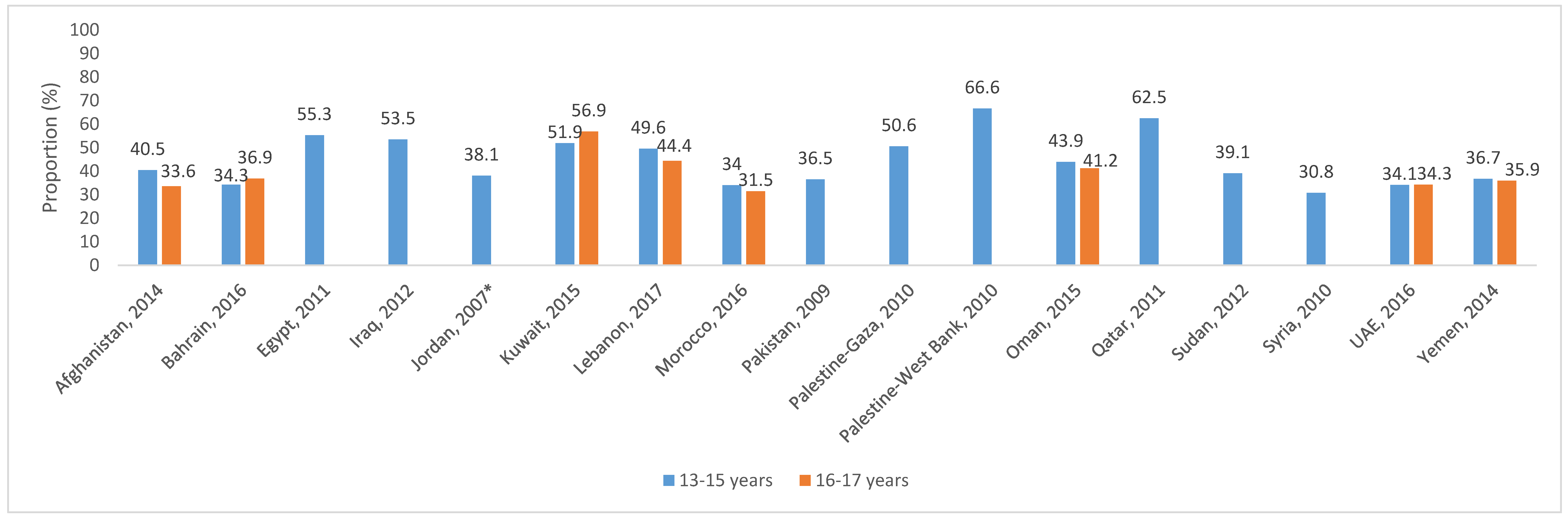
3.1.2. Adolescents
3.2. Macronutrient Intakes Amongst School-Aged Children and Adolescents in the EMR
3.2.1. School-Aged Children
3.2.2. Adolescents
3.3. Micronutrient Intakes Amongst School-Aged Children and Adolescents in the EMR
3.3.1. School-Aged Children
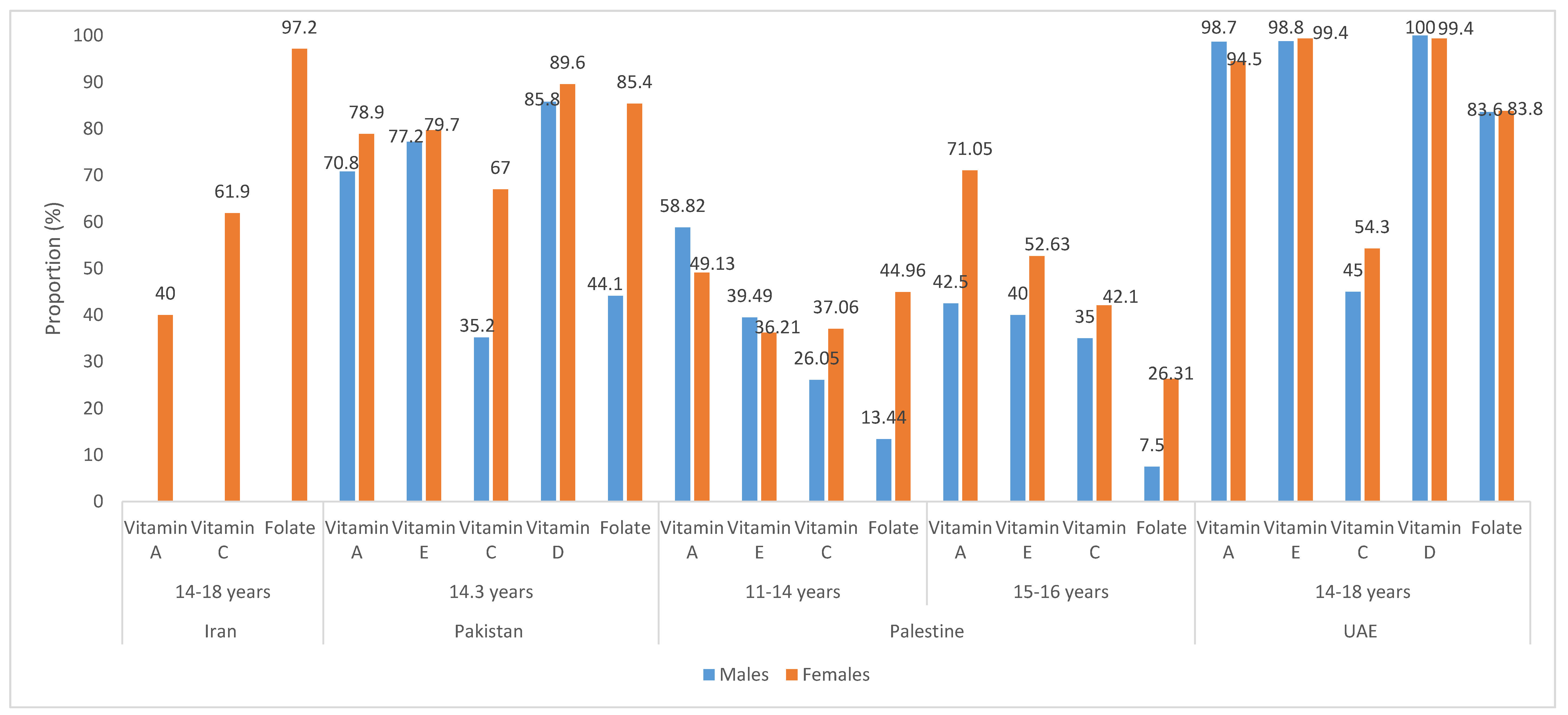
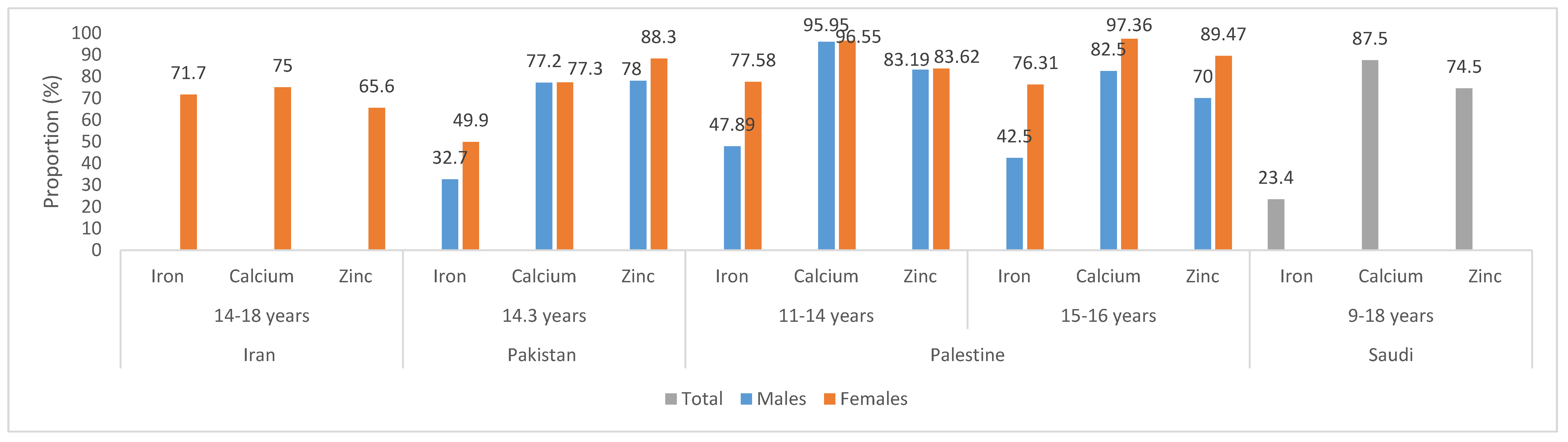
3.3.2. Adolescents
4. Discussion
5. Missing Knowledge and Future Research
6. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- World Health Organization Regional Office for Europe. Fact Sheets on Sustainable Development Goals: Health Targets: Child and Adolescent Health; WHO: Copenhagen, Denmark, 2017. [Google Scholar]
- World Health Organization Regional Office for Africa. Child and Adolescent Health and Nutrition (CAN) Program. Available online: https://www.afro.who.int/about-us/programmes-clusters/CAN (accessed on 8 October 2020).
- Institute of Medicine. Nutrition-Related Health Concerns, Dietary Intakes, and Eating Behaviors of Children and Adolescents. In Nutrition Standards for Foods in Schools: Leading the Way Toward Healthier Youth; The National Academies Press: Washington, DC, USA, 2007. [Google Scholar] [CrossRef]
- Story, M.; Holt, K.; Sofka, D. Bright Futures in Practice, 2nd ed.; National Center for Education in Maternal and Child Health: Arlington, VA, USA, 2002. [Google Scholar]
- Daniels, S.R. The consequences of childhood overweight and obesity. Future Child 2006, 16, 47–67. [Google Scholar] [CrossRef]
- Institute of Medicine. Preventing Childhood Obesity: Health in the Balance; The National Academies Press: Washington, DC, USA, 2005. [Google Scholar]
- Nasreddine, L.; Naja, F.; Tabet, M.; Habbal, M.-Z.; El-Aily, A.; Haikal, C.; Sidani, S.; Adra, N.; Hwalla, N. Obesity is associated with insulin resistance and components of the metabolic syndrome in Lebanese adolescents. Ann. Hum. Biol. 2012, 39, 122–128. [Google Scholar] [CrossRef]
- Nasreddine, L.; Ouaijan, K.; Mansour, M.; Adra, N.; Sinno, D.; Hwalla, N. Metabolic syndrome and insulin resistance in obese prepubertal children in Lebanon: A primary health concern. Ann. Nutr. Metab. 2010, 57, 135–142. [Google Scholar] [CrossRef]
- Gidding, S.S.; Dennison, B.A.; Birch, L.L.; Daniels, S.R.; Gilman, M.W.; Lichtenstein, A.H.; Rattay, K.T.; Steinberger, J.; Stettler, N.; Van Horn, L. Dietary recommendations for children and adolescents: A guide for practitioners: Consensus statement from the American Heart Association. Circulation 2005, 112, 2061–2075. [Google Scholar] [CrossRef]
- World Health Organization. Technical paper. Regional strategy on nutrition 2010–2019. Regional Committee for the Eastern Mediterranean. Fifty-Seventh Session. Agenda Item 4 (b); WHO: Geneva, Switzerland, 2010. [Google Scholar]
- Nasreddine, L.; Naja, F.; Sibai, A.-M.; Helou, K.; Adra, N.; Hwalla, N. Trends in nutritional intakes and nutrition-related cardiovascular disease risk factors in Lebanon: The need for immediate action. Leb. Med. J. 2014, 103, 1–9. [Google Scholar] [CrossRef]
- Popkin, B.M.; Adair, L.S.; Ng, S.W. Global nutrition transition and the pandemic of obesity in developing countries. Nutr. Rev. 2012, 70, 3–21. [Google Scholar] [CrossRef]
- World Health Organization Regional Office for the Eastern Mediterranean. Nutrition. Available online: http://www.emro.who.int/health-topics/nutrition/index.html (accessed on 26 August 2020).
- Rahim, H.F.A.; Sibai, A.; Khader, Y.; Hwalla, N.; Fadhil, I.; Alsiyabi, H.; Mataria, A.; Mendis, S.; Mokdad, A.H.; Husseini, A. Non-communicable diseases in the Arab world. Lancet 2014, 383, 356–367. [Google Scholar] [CrossRef]
- Moghames, P.; Hammami, N.; Hwalla, N.; Yazbeck, N.; Shoaib, H.; Nasreddine, L.; Naja, F. Validity and reliability of a food frequency questionnaire to estimate dietary intake among Lebanese children. Nutr. J. 2015, 15, 4. [Google Scholar] [CrossRef]
- Bagchi, K. Nutrition in the eastern Mediterranean region of the World Health Organization. East. Mediterr. Health J. 2008, 14, S107–S113. [Google Scholar]
- World Health Organization Regional Office for the Eastern Mediterranean. Countries in the Eastern Mediterranean Region. Available online: http://www.emro.who.int/countries.html (accessed on 15 July 2020).
- World Health Organization. Global School-Based Student Health Survey (GSHS). Available online: https://www.who.int/ncds/surveillance/gshs/factsheets/en/ (accessed on 11 August 2020).
- Keats, E.C.; Rappaport, A.I.; Shah, S.; Oh, C.; Jain, R.; Bhutta, Z.A. The dietary intake and practices of adolescent girls in low-and middle-income countries: A systematic review. Nutrients 2018, 10, 1978. [Google Scholar] [CrossRef]
- World Health Organization. Healthy Diet FACT SHEET N°394; WHO: Geneva, Switzerland, 2015. [Google Scholar]
- Abbass, M.M.; Mahmoud, S.A.; El Moshy, S.; Rady, D.; AbuBakr, N.; Radwan, I.A.; Ahmed, A.; Abdou, A.; Al Jawaldeh, A. The prevalence of dental caries among Egyptian children and adolescences and its association with age, socioeconomic status, dietary habits and other risk factors. A cross-sectional study. F1000Research 2019, 8, 1–19. [Google Scholar] [CrossRef] [PubMed]
- Hashim, R.; Williams, S.M.; Murray Thomson, W. Diet and caries experience among preschool children in Ajman, United Arab Emirates. Eur. J. Oral. Sci. 2009, 117, 734–740. [Google Scholar] [CrossRef] [PubMed]
- Jaghasi, I.; Hatahet, W.; Dashash, M. Dietary patterns and oral health in schoolchildren from Damascus, Syrian Arab Republic. East. Mediterr. Health J. 2012, 18, 358–364. [Google Scholar] [CrossRef]
- Nasreddine, L.; Naja, F.; Akl, C.; Chamieh, M.C.; Karam, S.; Sibai, A.-M.; Hwalla, N. Dietary, lifestyle, and socio-economic correlates of overweight, obesity and central obesity in Lebanese children and adolescents. Nutrients 2014, 6, 1038–1062. [Google Scholar] [CrossRef]
- Hasanein, M.A.; Jawad, S.H.A. Prevalence of obesity and risk factors among female school-aged children in primary school in Madinah Munawarah. Life Sci. J. 2014, 11. [Google Scholar]
- Kelishadi, R.; Gheisari, A.; Zare, N.; Farajian, S.; Shariatinejad, K. Salt intake and the association with blood pressure in young Iranian children: First report from the middle East and north Africa. Int. J. Prev. Med. 2013, 4, 475. [Google Scholar]
- Khatib, I.; Elmadfa, I. High prevalence rates of anemia, vitamin A deficiency and stunting imperil the health status of Bedouin schoolchildren in North Badia, Jordan. Ann. Nutr. Metab. 2009, 55, 358–367. [Google Scholar] [CrossRef]
- Gharib, N.; Rasheed, P. Energy and macronutrient intake and dietary pattern among school children in Bahrain: A cross-sectional study. Nutr. J. 2011, 10, 62. [Google Scholar] [CrossRef]
- Ali, H.I.; Ng, S.W.; Zaghloul, S.; Harrison, G.G.; Qazaq, H.S.; El Sadig, M.; Yeatts, K. High proportion of 6 to 18-year-old children and adolescents in the United Arab Emirates are not meeting dietary recommendations. Nutr. Res. 2013, 33, 447–456. [Google Scholar] [CrossRef]
- Alsubaie, A.S.R. Intake of fruit, vegetables and milk products and correlates among school boys in Saudi Arabia. Int. J. Adolesc. Med. Health 2018, 1. [Google Scholar] [CrossRef]
- Hassan, A.S.; Al-Dosari, S.N. Breakfast habits and snacks consumed at school among Qatari schoolchildren aged 9–10 years. Nutr. Food Sci. 2008, 38, 264–270. [Google Scholar] [CrossRef]
- Amini, M.; Dadkhah-Piraghaj, M.; Abtahi, M.; Abdollahi, M.; Houshiarrad, A.; Kimiagar, M. Nutritional assessment for primary school children in Tehran: An evaluation of dietary pattern with emphasis on snacks and meals consumption. Int. J. Prev. Med. 2014, 5, 611. [Google Scholar] [PubMed]
- Mirmiran, P.; Ziadlou, M.; Karimi, S.; Hosseini-Esfahani, F.; Azizi, F. The association of dietary patterns and adherence to WHO healthy diet with metabolic syndrome in children and adolescents: Tehran lipid and glucose study. BMC Public Health 2019, 19, 1457. [Google Scholar] [CrossRef]
- Naeeni, M.M.; Jafari, S.; Fouladgar, M.; Heidari, K.; Farajzadegan, Z.; Fakhri, M.; Karami, P.; Omidi, R. Nutritional knowledge, practice, and dietary habits among school children and adolescents. Int. J. Prev. Med. 2014, 5, S171. [Google Scholar] [CrossRef]
- Kelishadi, R.; Ardalan, G.; Gheiratmand, R.; Gouya, M.M.; Razaghi, E.M.; Delavari, A.; Majdzadeh, R.; Heshmat, R.; Motaghian, M.; Barekati, H. Association of physical activity and dietary behaviours in relation to the body mass index in a national sample of Iranian children and adolescents: CASPIAN Study. Bull. World Health Organ. 2007, 85, 19–26. [Google Scholar] [CrossRef]
- Musaiger, A.O.; Al-Mufty, B.A.; Al-Hazzaa, H.M. Eating habits, inactivity, and sedentary behavior among adolescents in Iraq: Sex differences in the hidden risks of noncommunicable diseases. Food Nutr. Bull. 2014, 35, 12–19. [Google Scholar] [CrossRef] [PubMed]
- Mikki, N.; Abdul-Rahim, H.F.; Shi, Z.; Holmboe-Ottesen, G. Dietary habits of Palestinian adolescents and associated sociodemographic characteristics in Ramallah, Nablus and Hebron governorates. Public Health Nutr. 2010, 13, 1419–1429. [Google Scholar] [CrossRef]
- Nabhani-Zeidan, M.; Naja, F.; Nasreddine, L. Dietary intake and nutrition-related knowledge in a sample of Lebanese adolescents of contrasting socioeconomic status. Food Nutr. Bull. 2011, 32, 75–83. [Google Scholar] [CrossRef]
- Waly, I.; Zayed, K.; Al Haddabi, B. Obesity, eating habits and sedentary behaviour of Omani young adolescents: A cross-sectional study. EC Nutr. 2017, 7, 3–10. [Google Scholar]
- Makansi, N.; Allison, P.; Awad, M.; Bedos, C. Fruit and vegetable intake among Emirati adolescents: A mixed methods study. East. Mediterr. Health J. 2018, 24. [Google Scholar] [CrossRef]
- Hejazi, N.; Mazloom, Z. Socioeconomic status, youth’s eating patterns and meals consumed away from home. Pak. J. Biol. Sci. 2009, 12, 730. [Google Scholar] [PubMed]
- Abdel-Hady, D.; El-Gilany, A.-H.; Sarraf, B. Dietary habits of adolescent students in Mansoura, Egypt. Int. J. Collab. Res. Intern. Med. Public Health 2014, 6, 132. [Google Scholar]
- El Achhab, Y.; Marfa, A.; Echarbaoui, I.; Chater, R.; El-Haidani, A.; Filali-Zegzouti, Y. Physical inactivity, sedentary behaviors and dietary habits among Moroccan adolescents in secondary school. Sci. Sport 2018, 33, 58–62. [Google Scholar] [CrossRef]
- Hamrani, A.; Mehdad, S.; El Kari, K.; El Hamdouchi, A.; El Menchawy, I.; Belghiti, H.; El Mzibri, M.; Musaiger, A.O.; Al-Hazzaa, H.M.; Hills, A.P. Physical activity and dietary habits among Moroccan adolescents. Public Health Nutr. 2015, 18, 1793–1800. [Google Scholar] [CrossRef] [PubMed]
- Shokrvash, B.; Salehi, L.; Akbari, M.H.; Mamagani, M.E.; Nedjat, S.; Asghari, M.; Majlessi, F.; Montazeri, A. Social support and dairy products intake among adolescents: A study from Iran. BMC Public Health 2015, 15, 1078. [Google Scholar] [CrossRef][Green Version]
- Nasreddine, L.; Mehio-Sibai, A.; Mrayati, M.; Adra, N.; Hwalla, N. Adolescent obesity in Syria: Prevalence and associated factors. Child Care Health Dev. 2010, 36, 404–413. [Google Scholar] [CrossRef]
- Mahfouz, A.A.; Shatoor, A.S.; Hassanein, M.A.; Mohamed, A.; Farheen, A. Gender differences in cardiovascular risk factors among adolescents in Aseer Region, southwestern Saudi Arabia. J. Saudi Heart Assoc. 2012, 24, 61–67. [Google Scholar] [CrossRef]
- Montazerifar, F.; Karajibani, M.; Dashipour, A.R. Evaluation of dietary intake and food patterns of adolescent girls in Sistan and Baluchistan Province, Iran. Funct. Foods Health Dis. 2012, 2, 62–71. [Google Scholar] [CrossRef]
- Sachithananthan, V.; Gad, N. A Study on the Frequency of Food Consumption and Its Relationship to BMI in School Children and Adolescents in Abha City, KSA. Cur. Res. Nutr. Food Sci. 2016, 4, 203. [Google Scholar] [CrossRef]
- Moukhyer, M.E.; van Eijk, J.T.; De Vries, N.K.; Bosma, H. Health-related behaviors of Sudanese adolescents. Educ. Health 2008, 21, 184. [Google Scholar]
- Musaiger, A.O.; Nabag, F.O.; Al-Mannai, M. Obesity, dietary habits, and sedentary behaviors among adolescents in Sudan: Alarming risk factors for chronic diseases in a poor country. Food Nutr. Bull. 2016, 37, 65–72. [Google Scholar] [CrossRef] [PubMed]
- Musaiger, A.; Bader, Z.; Al-Roomi, K.; D’Souza, R. Dietary and lifestyle habits amongst adolescents in Bahrain. Food Nutr. Res. 2011, 55, 7122. [Google Scholar] [CrossRef]
- Abudayya, A.H.; Stigum, H.; Shi, Z.; Abed, Y.; Holmboe-Ottesen, G. Sociodemographic correlates of food habits among school adolescents (12–15 year) in North Gaza Strip. BMC Public Health 2009, 9, 185. [Google Scholar] [CrossRef]
- Dalky, H.F.; Al Momani, M.H.; Al-Drabaah, T.K.; Jarrah, S. Eating habits and associated factors among adolescent students in Jordan. Clin. Nurs. Res. 2017, 26, 538–552. [Google Scholar] [CrossRef]
- Mahfouz, A.A.; Abdelmoneim, I.; Khan, M.Y.; Daffalla, A.A.; Diab, M.M.; Al-Gelban, K.S.; Moussa, H. Obesity and related behaviors among adolescent school boys in Abha City, Southwestern Saudi Arabia. J. Trop. Pediatr. 2008, 54, 120–124. [Google Scholar] [CrossRef] [PubMed]
- Musaiger, A.O.; Kalam, F. Dietary habits and lifestyle among adolescents in Damascus, Syria. Ann. Agric. Environ. Med. 2014, 21. [Google Scholar] [CrossRef] [PubMed]
- Allafi, A.; Al-Haifi, A.R.; Al-Fayez, M.A.; Al-Athari, B.I.; Al-Ajmi, F.A.; Al-Hazzaa, H.M.; Musaiger, A.O.; Ahmed, F. Physical activity, sedentary behaviours and dietary habits among Kuwaiti adolescents: Gender differences. Public Health Nutr. 2014, 17, 2045–2052. [Google Scholar] [CrossRef]
- Honkala, S.; Honkala, E.; Al-Sahli, N. Consumption of sugar products and associated life-and school-satisfaction and self-esteem factors among schoolchildren in Kuwait. Acta Odontol. Scand. 2006, 64, 79–88. [Google Scholar] [CrossRef]
- Al Muammar, M.; El Shafie, M. Association between dietary habits and body mass index of adolescent females in intermediate schools in Riyadh, Saudi Arabia. East. Mediterr. Health J. 2014, 20, 39–45. [Google Scholar] [CrossRef]
- Bello, L.; Al-Hammad, N. Pattern of fluid consumption in a sample of Saudi Arabian adolescents aged 12–13 years. Int. J. Paediatr. Dent. 2006, 16, 168–173. [Google Scholar] [CrossRef]
- Subih, H.S.; Abu-Shquier, Y.; Bawadi, H.; Al-Bayyari, N. Assessment of body weight, maternal dietary knowledge and lifestyle practices among children and adolescents in north Jordan. Public Health Nutr. 2018, 21, 2803–2810. [Google Scholar] [CrossRef]
- Institute of Medicine; Food and Nutrition Board. Dietary Reference Intakes for Water, Potassium, Sodium, Chloride, and Sulfate. Available online: https://www.nal.usda.gov/sites/default/files/fnic_uploads/water_full_report.pdf (accessed on 10 September 2020).
- Jomaa, L.; Hwalla, N.; Constant, F.; Naja, F.; Nasreddine, L. Water and beverage consumption among children aged 4–13 years in Lebanon: Findings from a National Cross-Sectional Study. Nutrients 2016, 8, 554. [Google Scholar] [CrossRef]
- Ali, H.I.; Al Dhaheri, A.S.; Elmi, F.; Ng, S.W.; Zaghloul, S.; Ohuma, E.O.; Qazaq, H.S. Water and Beverage Consumption among a Nationally Representative Sample of Children and Adolescents in the United Arab Emirates. Nutrients 2019, 11, 2110. [Google Scholar] [CrossRef] [PubMed]
- Al Sabbah, H.; Vereecken, C.; Kolsteren, P.; Abdeen, Z.; Maes, L. Food habits and physical activity patterns among Palestinian adolescents: Findings from the national study of Palestinian schoolchildren (HBSC-WBG2004). Public Health Nutr. 2007, 10, 739–746. [Google Scholar] [CrossRef]
- Kerkadi, A.; Sadig, A.H.; Bawadi, H.; Al Thani, A.A.M.; Al Chetachi, W.; Akram, H.; Al-Hazzaa, H.M.; Musaiger, A.O. The relationship between lifestyle factors and obesity indices among adolescents in Qatar. Int. J. Environ. Res. Public Health 2019, 16, 4428. [Google Scholar] [CrossRef]
- Al-Hazzaa, H.M.; Abahussain, N.A.; Al-Sobayel, H.I.; Qahwaji, D.M.; Musaiger, A.O. Physical activity, sedentary behaviors and dietary habits among Saudi adolescents relative to age, gender and region. Int. J. Behav. Nutr. Phys. Act. 2011, 8, 140. [Google Scholar] [CrossRef]
- Nazik, M.; Malde, M.; Ahmed, M.; Trovik, T. Correlation between caries experience in Sudanese school children and dietary habits, according to a food frequency questionnaire and a modified 24-hr recall method. Afr. J. Food Agric. Nutr. Dev. 2013, 13. [Google Scholar]
- FAO and FHI 360. Minimum Dietary Diversity for Women: A Guide for Measurement; Food and Agriculture Organization of the United Nations: Rome, Italy, 2016. [Google Scholar]
- Friel, S.; Hattersley, L.; Snowdon, W.; Thow, A.M.; Lobstein, T.; Sanders, D.; Barquera, S.; Mohan, S.; Hawkes, C.; Kelly, B. Monitoring the impacts of trade agreements on food environments. Obes. Rev. 2013, 14, 120–134. [Google Scholar] [CrossRef] [PubMed]
- El-Gazzar, H.H.; Saleh, S.M.; Khairy, S.A.; Marei, A.S.; ElKelany, K.; Al Soda, M.F. Relationship between dietary intake and obesity among a group of primary school-aged children in Cairo Governorate. J. Med. Sci. Res. 2019, 2, 42. [Google Scholar]
- Khatib, I.; Hijazi, S.S. Micronutrient deficiencies among children may be endemic in underprivileged areas in Jordan. Jordan Med. J. 2009, 43, 324–332. [Google Scholar]
- Al-Rewashdeh, A. Assessment of the nutritional status for preschool children in Jordan. Bull. Fac. Agric. Cairo Univ. 2009, 60, 423–432. [Google Scholar]
- Institute of Medicine; Food and Nutrition Board. Dietary Reference Intakes for Energy, Carbohydrate, Fiber, Fat, Fatty Acids, Cholesterol, Protein and Amino Acids. Available online: https://www.nap.edu/catalog/10490/dietary-reference-intakes-for-energy-carbohydrate-fiber-fat-fatty-acids-cholesterol-protein-and-amino-acids-macronutrients (accessed on 30 April 2017).
- Jabre, P.; Sikias, P.; Khater-Menassa, B.; Baddoura, R.; Awada, H. Overweight children in Beirut: Prevalence estimates and characteristics. Child Care Health Dev. 2005, 31, 159–165. [Google Scholar] [CrossRef]
- Akl, C. Prevalence and Determinants of Overweight and Obesity in a Nationally Representative Sample of Lebanese Children 5 to 12 Years Old; American University of Beirut: Beirut, Lebanon, 2012. [Google Scholar]
- Alredaisy, M.; Ibrahim, S. Assessment of nutritional status of children less than 10 years old in rural western Kordafan. IIOABJ 2011, 2, 40–49. [Google Scholar]
- Ng, S.W.; Zaghloul, S.; Ali, H.; Harrison, G.; Yeatts, K.; El Sadig, M.; Popkin, B.M. Nutrition transition in the United Arab Emirates. Eur. J. Clin. Nutr. 2011, 65, 1328–1337. [Google Scholar] [CrossRef] [PubMed]
- Kilani, H.; Al-Hazzaa, H.; Waly, M.I.; Musaiger, A. Lifestyle Habits: Diet, physical activity and sleep duration among Omani adolescents. Sultan Qaboos Univ. Med. J. 2013, 13, 510. [Google Scholar] [CrossRef] [PubMed]
- Bazhan, M.; Kalantari, N.; Houhiar-Rad, A.; Alavi-Majd, H.; Kalantari, S. Dietary habits and nutrient intake in adolescent girls living in Northern Iran. Arch. Adv. Biosci. 2013, 4. [Google Scholar]
- ALFaris, N.A.; Al-Tamimi, J.Z.; Al-Jobair, M.O.; Al-Shwaiyat, N.M. Trends of fast food consumption among adolescent and young adult Saudi girls living in Riyadh. Food Nutr. Res. 2015, 59, 26488. [Google Scholar] [CrossRef] [PubMed]
- Washi, S.A.; Ageib, M.B. Poor diet quality and food habits are related to impaired nutritional status in 13-to 18-year-old adolescents in Jeddah. Nutr. Res. 2010, 30, 527–534. [Google Scholar] [CrossRef]
- Department of Health. Dietary Reference Values for Food Energy, Nutrients for the United Kingdom. In Report of the Panel on Dietary Values of the Committee on Medical Aspects of Food Policy, 8th ed.; HMSO: London, UK, 1996. [Google Scholar]
- Zaghloul, S.; Al-Hooti, S.N.; Al-Hamad, N.; Al-Zenki, S.; Alomirah, H.; Alayan, I.; Al-Attar, H.; Al-Othman, A.; Al-Shami, E.; Al-Somaie, M. Evidence for nutrition transition in Kuwait: Over-consumption of macronutrients and obesity. Public Health Nutr. 2013, 16, 596–607. [Google Scholar] [CrossRef]
- Jildeh, C.; Papandreou, C.; Mourad, T.A.; Hatzis, C.; Kafatos, A.; Qasrawi, R.; Philalithis, A.; Abdeen, Z. Assessing the nutritional status of Palestinian adolescents from East Jerusalem: A school-based study 2002–03. J. Trop. Pediatr. 2011, 57, 51–58. [Google Scholar] [CrossRef][Green Version]
- Ahmed, N.M.K.; Onsa, Z.O. Nutritional Assessment of the Adolescents in the Northern State of Sudan. Pak. J. Nutr. 2014, 13, 79. [Google Scholar] [CrossRef]
- Mohseni-Takalloo, S.; Mirmiran, P.; Hosseini-Esfahani, F.; Azizi, F. Dietary fat intake and its relationship with serum lipid profiles in tehranian adolescents. J. Food Nutr. Res. 2014, 2, 330–334. [Google Scholar] [CrossRef][Green Version]
- World Health Organization. Interim summary of conclusions and dietary recommendations on total fat & fatty acids. In From the Joint FAO/WHO Expert Consultation on Fats and Fatty Acids in Human Nutrition; World Health Organization: Geneva, Switzerland, 2008. [Google Scholar]
- Nasreddine, L.; Chamieh, M.C.; Ayoub, J.; Hwalla, N.; Sibai, A.-M.; Naja, F. Sex disparities in dietary intake across the lifespan: The case of Lebanon. Nutr. J. 2020, 19, 1–18. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Diet, Nutrition and the Prevention of Chronic Diseases. Joint WHO/FAO Expert Consultation. WHO Technical Report Series no. 916. Available online: https://apps.who.int/iris/bitstream/handle/10665/42665/WHO_TRS_916.pdf?sequence=1 (accessed on 1 September 2020).
- Aounallah-Skhiri, H.; Traissac, P.; El Ati, J.; Eymard-Duvernay, S.; Landais, E.; Achour, N.; Delpeuch, F.; Romdhane, H.B.; Maire, B. Nutrition transition among adolescents of a south-Mediterranean country: Dietary patterns, association with socio-economic factors, overweight and blood pressure. A cross-sectional study in Tunisia. Nutr. J. 2011, 10, 38. [Google Scholar] [CrossRef]
- Huew, R.; Maguire, A.; Waterhouse, P.; Moynihan, P. Nutrient intake and dietary patterns of relevance to dental health of 12-year-old Libyan children. Public Health Nutr. 2014, 17, 1107–1113. [Google Scholar] [CrossRef]
- Montero, P.; Mora Urda, A.; Cherkaoui, M.; Anzid, K. Transition nutritionnelle au Maroc: Étude comparative de l’état nutritionnel des adolescents entre 1991 et 2007. Bull Séances. 2009, 60, 433–450. [Google Scholar]
- Montero, M.D.P.; Mora-Urda, A.I.; Anzid, K.; Cherkaoui, M.; Marrodan, M.D. Diet quality of Moroccan adolescents living in Morocco and in Spain. J. Biosoc. Sci. 2017, 49, 173. [Google Scholar] [CrossRef] [PubMed]
- Anderson, J.W.; Baird, P.; Davis, R.H.; Ferreri, S.; Knudtson, M.; Koraym, A.; Waters, V.; Williams, C.L. Health benefits of dietary fiber. Nutr. Rev. 2009, 67, 188–205. [Google Scholar] [CrossRef]
- Collison, K.S.; Zaidi, M.Z.; Subhani, S.N.; Al-Rubeaan, K.; Shoukri, M.; Al-Mohanna, F.A. Sugar-sweetened carbonated beverage consumption correlates with BMI, waist circumference, and poor dietary choices in school children. BMC Public Health 2010, 10, 234. [Google Scholar] [CrossRef]
- Tayel, D.I.; El-Sayed, N.A.; El-Sayed, N.A. Dietary pattern and blood pressure levels of adolescents in Sohag, Egypt. J. Egypt Public Health Assoc. 2013, 88, 97–103. [Google Scholar] [CrossRef]
- Al-Ansari, J.M.; Al-Jairan, L.Y.; Gillespie, G.M. Dietary habits of the primary to secondary school population and implications for oral health. J. Allied Health 2006, 35, 75–80. [Google Scholar] [PubMed]
- Rifat-uz-Zaman, Z.I.; Ali, U. Dietary Intakes of Urban Adolescents of Sialkot, Pakistan Do Not Meet the Standards of Adequacy. Pak. J. Nutr. 2013, 12, 460–467. [Google Scholar] [CrossRef]
- Aziz, S.; Hosain, K. Carbohydrate (CHO), protein and fat intake of healthy Pakistani school children in a 24 hour period. J. Pak. Med. Assoc. 2014, 64, 1255–1259. [Google Scholar]
- Abuzaid, O.I. Eating Patterns and Physical Activity Characteristics among Urban and Rural Students in Saudi Arabia; Nutrition and Health Sciences Department, University of Nebraska-Lincoln: Lincoln, NE, USA, 2012. [Google Scholar]
- Institute of Medicine; Food and Nutrition Board. Dietary Reference Intakes: RDA and AI for Vitamins and Elements. Available online: http://www.nationalacademies.org/hmd/~/media/Files/Activity%20Files/Nutrition/DRI-Tables/2_%20RDA%20and%20AI%20Values_Vitamin%20and%20Elements.pdf?la=en (accessed on 30 April 2017).
- Khatib, I. High prevalence of subclinical vitamin A deficiency in Jordan: A forgotten risk. Food Nutr. Bull. 2002, 23, 228–236. [Google Scholar] [CrossRef] [PubMed]
- Salamoun, M.; Kizirian, A.; Tannous, R.; Nabulsi, M.; Choucair, M.; Deeb, M.; Fuleihan, G.E.-H. Low calcium and vitamin D intake in healthy children and adolescents and their correlates. Eur. J. Clin. Nutr. 2005, 59, 177–184. [Google Scholar] [CrossRef] [PubMed]
- Al-Musharaf, S.; Al-Othman, A.; Al-Daghri, N.M.; Krishnaswamy, S.; Yusuf, D.S.; Alkharfy, K.M.; Al-Saleh, Y.; Al-Attas, O.S.; Alokail, M.S.; Moharram, O. Vitamin D deficiency and calcium intake in reference to increased body mass index in children and adolescents. Eur. J. Pediatr. 2012, 171, 1081–1086. [Google Scholar] [CrossRef]
- Saeid, N.; Elmzibri, M.; Hamrani, A.; Latifa, Q.; Belghiti, H.; El Berri, H.; Benjeddou, K.; Bouziani, A.; Benkirane, H.; Taboz, Y. Assessment of sodium and potassium intakes in children aged 6 to 18 years by 24 h urinary excretion in city of rabat, Morocco. J. Nutr. Metab. 2018, 2018. [Google Scholar] [CrossRef]
- Al-Daghri, N.M.; Al-Othman, A.; Alkharfy, K.M.; Alokail, M.S.; Khan, N.; Alfawaz, H.A.; Aiswaidan, I.A.; Chrousos, G.P. Assessment of selected nutrients intake and adipocytokines profile among Saudi children and adults. Endocrine J. 2012, EJ12-0167. [Google Scholar] [CrossRef]
- Nasreddine, L.M.; Kassis, A.N.; Ayoub, J.J.; Naja, F.A.; Hwalla, N.C. Nutritional status and dietary intakes of children amid the nutrition transition: The case of the Eastern Mediterranean Region. Nutr. Res. 2018, 57, 12–27. [Google Scholar] [CrossRef]
- Nasreddine, L.; Ayoub, J.J.; Al Jawaldeh, A. Review of the nutrition situation in the Eastern Mediterranean Region. East. Mediterr. Health J. 2018, 24, 77–91. [Google Scholar] [CrossRef]
- Kelishadi, R.; Ardalan, G.; Gheiratmand, R.; Majdzadeh, R.; Hosseini, M.; Gouya, M.; Razaghi, E.; Delavari, A.; Motaghian, M.; Barekati, H. Thinness, overweight and obesity in a national sample of Iranian children and adolescents: CASPIAN Study. Child Care Health Dev. 2008, 34, 44–54. [Google Scholar] [CrossRef] [PubMed]
- Mirmohammadi, S.-J.; Hafezi, R.; Mehrparvar, A.H.; Rezaeian, B.; Akbari, H. Prevalence of overweight and obesity among Iranian school children in different ethnicities. Iran J. Pediatr. 2011, 21, 514. [Google Scholar] [PubMed]
- Nasreddine, L.; Naja, F.; Chamieh, M.C.; Adra, N.; Sibai, A.-M.; Hwalla, N. Trends in overweight and obesity in Lebanon: Evidence from two national cross-sectional surveys (1997 and 2009). BMC Public Health 2012, 12, 798. [Google Scholar] [CrossRef] [PubMed]
- Bener, A.; Kamal, A.A. Growth patterns of Qatari school children and adolescents aged 6–18 years. J. Health Popul. Nutr. 2005, 23, 250–258. [Google Scholar]
- Rootwelt, C.; Fosse, K.B.; Tuffaha, A.; Said, H.; Sandridge, A.; Janahi, I.; Greer, W.; Hedin, L. Qatar s Youth Is Putting on Weight: The Increase in Obesity Between 2003 and 2009. In Proceedings of the Qatar Foundation Annual Research Conference Proceedings, Doha, Qatar, November 2014; Volume 2014, p. HBSP1130. [Google Scholar]
- El-Hazmi, M.A.; Warsy, A.S. A comparative study of prevalence of overweight and obesity in children in different provinces of Saudi Arabia. J. Trop. Pediatr. 2002, 48, 172–177. [Google Scholar] [CrossRef]
- Al-Almaie, S.M. Prevalence of obesity and overweight among Saudi adolescents in Eastern Saudi Arabia. Saudi Med. J. 2005, 26, 607. [Google Scholar]
- Al-Nuaim, A.A.; Al-Nakeeb, Y.; Lyons, M.; Al-Hazzaa, H.M.; Nevill, A.; Collins, P.; Duncan, M.J. The prevalence of physical activity and sedentary behaviours relative to obesity among adolescents from Al-Ahsa, Saudi Arabia: Rural versus urban variations. J. Nutr. Metab. 2012, 2012. [Google Scholar] [CrossRef]
- Aounallah-Skhiri, H.; El Ati, J.; Traissac, P.; Romdhane, H.B.; Eymard-Duvernay, S.; Delpeuch, F.; Achour, N.; Maire, B. Blood pressure and associated factors in a North African adolescent population. a national cross-sectional study in Tunisia. BMC Public Health 2012, 12, 98. [Google Scholar] [CrossRef]
- Musaiger, A.O. The state of nutrition in Bahrain. Nutr. Health 2000, 14, 63–74. [Google Scholar] [CrossRef]
- Musaiger, A.O. Overweight and obesity in eastern mediterranean region: Prevalence and possible causes. J. Obes. 2011, 2011. [Google Scholar] [CrossRef]
- Black, R.E.; Victora, C.G.; Walker, S.P.; Bhutta, Z.A.; Christian, P.; De Onis, M.; Ezzati, M.; Grantham-McGregor, S.; Katz, J.; Martorell, R. Maternal and child undernutrition and overweight in low-income and middle-income countries. Lancet 2013, 382, 427–451. [Google Scholar] [CrossRef]
- Itoh, H.; Kanayama, N. Nutritional conditions in early life and risk of non-communicable diseases (NCDs) from the perspective of preemptive medicine in perinatal care. Hypertens. Res. Pregnancy 2015, 3, 1–12. [Google Scholar] [CrossRef][Green Version]
- Weiss, R.; Dziura, J.; Burgert, T.S.; Tamborlane, W.V.; Taksali, S.E.; Yeckel, C.W.; Allen, K.; Lopes, M.; Savoye, M.; Morrison, J. Obesity and the metabolic syndrome in children and adolescents. N. Engl. J. Med. 2004, 350, 2362–2374. [Google Scholar] [CrossRef] [PubMed]
- Khader, Y.; Batieha, A.; Jaddou, H.; El-Khateeb, M.; Ajlouni, K. Metabolic syndrome and its individual components among Jordanian children and adolescents. Int. J. Pediatr. Endocrinol. 2010, 2010, 316170. [Google Scholar] [CrossRef] [PubMed]
- Taha, D.; Ahmed, O.; Sadiq, B.B. The prevalence of metabolic syndrome and cardiovascular risk factors in a group of obese Saudi children and adolescents: A hospital-based study. Ann. Saudi Med. 2009, 29, 357–360. [Google Scholar] [CrossRef] [PubMed]
- Eapen, V.; Mabrouk, A.; Yousef, S. Metabolic syndrome among the young obese in the United Arab Emirates. J. Trop. Pediatr. 2010, 56, 325–328. [Google Scholar] [CrossRef]
- Ho, K.K.; Ferruzzi, M.G.; Wightman, J.D. Potential health benefits of (poly) phenols derived from fruit and 100% fruit juice. Nutr. Rev. 2020, 78, 145–174. [Google Scholar] [CrossRef]
- Tetens, I.; Alinia, S. The role of fruit consumption in the prevention of obesity. J. Hortic. Sci. Biotech. 2009, 84, 47–51. [Google Scholar] [CrossRef]
- Ello-Martin, J.A.; Roe, L.S.; Ledikwe, J.H.; Beach, A.M.; Rolls, B.J. Dietary energy density in the treatment of obesity: A year-long trial comparing 2 weight-loss diets. Am. J. Clin. Nutr. 2007, 85, 1465–1477. [Google Scholar] [CrossRef]
- Malik, V.S.; Schulze, M.B.; Hu, F.B. Intake of sugar-sweetened beverages and weight gain: A systematic review–. Am. J. Clin. Nutr. 2006, 84, 274–288. [Google Scholar] [CrossRef]
- Malik, V.S.; Pan, A.; Willett, W.C.; Hu, F.B. Sugar-sweetened beverages and weight gain in children and adults: A systematic review and meta-analysis. Am. J. Clin. Nutr. 2013, 98, 1084–1102. [Google Scholar] [CrossRef] [PubMed]
- Teff, K.L.; Grudziak, J.; Townsend, R.R.; Dunn, T.N.; Grant, R.W.; Adams, S.H.; Keim, N.L.; Cummings, B.P.; Stanhope, K.L.; Havel, P.J. Endocrine and metabolic effects of consuming fructose-and glucose-sweetened beverages with meals in obese men and women: Influence of insulin resistance on plasma triglyceride responses. J. Clin. Endocrinol. Metab. 2009, 94, 1562–1569. [Google Scholar] [CrossRef]
- Stanhope, K.L.; Schwarz, J.M.; Keim, N.L.; Griffen, S.C.; Bremer, A.A.; Graham, J.L.; Hatcher, B.; Cox, C.L.; Dyachenko, A.; Zhang, W. Consuming fructose-sweetened, not glucose-sweetened, beverages increases visceral adiposity and lipids and decreases insulin sensitivity in overweight/obese humans. J. Clin. Investig. 2009, 119, 1322–1334. [Google Scholar] [CrossRef]
- Stanhope, K.L.; Griffen, S.C.; Bair, B.R.; Swarbrick, M.M.; Keim, N.L.; Havel, P.J. Twenty-four-hour endocrine and metabolic profiles following consumption of high-fructose corn syrup-, sucrose-, fructose-, and glucose-sweetened beverages with meals. Am. J. Clin. Nutr. 2008, 87, 1194–1203. [Google Scholar] [CrossRef] [PubMed]
- Stanhope, K.L.; Havel, P.J. Endocrine and metabolic effects of consuming beverages sweetened with fructose, glucose, sucrose, or high-fructose corn syrup. Am. J. Clin. Nutr. 2008, 88, 1733S–1737S. [Google Scholar] [CrossRef]
- Muth, N.D.; Dietz, W.H.; Magge, S.N.; Johnson, R.K.; Pediatrics, A.A.O.; Association, A.H. Public policies to reduce sugary drink consumption in children and adolescents. Pediatrics 2019, 143. [Google Scholar] [CrossRef]
- Engin, A. Fat cell and fatty acid turnover in obesity. In Obes Lipotoxicity; Springer: Berlin/Heidelberg, Germany, 2017; pp. 135–160. [Google Scholar]
- Liberali, R.; Kupek, E.; Assis, M.A.A.d. Dietary Patterns and Childhood Obesity Risk: A Systematic Review. Child Obes. 2020, 16, 70–85. [Google Scholar] [CrossRef] [PubMed]
- Eyles, H.; Bhana, N.; Lee, S.E.; Grimes, C.; McLean, R.; Nowson, C.; Wall, C. Measuring Children’s Sodium and Potassium Intakes in NZ: A Pilot Study. Nutrients 2018, 10, 1198. [Google Scholar] [CrossRef]
- UNICEF-GAIN. Food Systems for Children and Adolescents. In Working Together to Secure Nutritious Diets; UNICEF Office of Research: Rome, Italy, 2018. [Google Scholar]
- Al-Isa, A. Nutritional Knowledge among High School Male Students in Kuwait. J. Community Med. Health Educ. 2018, 8. [Google Scholar] [CrossRef]
- Al-Yateem, N.; Rossiter, R. Nutritional knowledge and habits of adolescents aged 9 to 13 years in Sharjah, United Arab Emirates: A crosssectional study. East. Mediterr. Health J. 2017, 23, 551–558. [Google Scholar] [CrossRef]
- McClain, A.D.; Chappuis, C.; Nguyen-Rodriguez, S.T.; Yaroch, A.L.; Spruijt-Metz, D. Psychosocial correlates of eating behavior in children and adolescents: A review. Int. J. Behav. Nutr. Phys. Act. 2009, 6, 54. [Google Scholar] [CrossRef] [PubMed]
- Banna, J.C.; Buchthal, O.V.; Delormier, T.; Creed-Kanashiro, H.M.; Penny, M.E. Influences on eating: A qualitative study of adolescents in a periurban area in Lima, Peru. BMC Public Health 2015, 16, 40. [Google Scholar] [CrossRef] [PubMed]
- Becker, A.E.; Burwell, R.A.; Herzog, D.B.; Hamburg, P.; Gilman, S.E. Eating behaviours and attitudes following prolonged exposure to television among ethnic Fijian adolescent girls. Br. J. Psychiatry 2002, 180, 509–514. [Google Scholar] [CrossRef]
- Karimi-Shahanjarini, A.; Omidvar, N.; Bazargan, M.; Rashidian, A.; Majdzadeh, R.; Shojaeizadeh, D. Iranian female adolescent’s views on unhealthy snacks consumption: A qualitative study. Iran J. Public Health 2010, 39, 92. [Google Scholar] [PubMed]
- Anthrologica-World Food Programme (WFP). Bridging the Gap: Engaging Adolescents for Nutrition, Health and Sustainable Development; World Food Programme: Rome, Italy, 2018. [Google Scholar]
- Pachón, H.; Simondon, K.B.; Fall, S.T.; Menon, P.; Ruel, M.T.; Hotz, C.; Creed-Kanashiro, H.; Arce, B.; Domínguez, M.R.L.; Frongillo, E.A. Constraints on the delivery of animal-source foods to infants and young children: Case studies from five countries. Food Nutr. Bull. 2007, 28, 215–229. [Google Scholar] [CrossRef]
- Armar-Klemesu, M.; Osei-Menya, S.; Zakariah-Akoto, S.; Tumilowicz, A.; Lee, J.; Hotz, C. Using ethnography to identify barriers and facilitators to optimal Infant and Young Child Feeding in rural Ghana: Implications for programs. Food Nutr. Bull. 2018, 39, 231–245. [Google Scholar] [CrossRef]
- Burns, J.; Emerson, J.A.; Amundson, K.; Doocy, S.; Caulfield, L.E.; Klemm, R.D. A qualitative analysis of barriers and facilitators to optimal breastfeeding and complementary feeding practices in South Kivu, Democratic Republic of Congo. Food Nutr. Bull. 2016, 37, 119–131. [Google Scholar] [CrossRef]
- Darmon, N.; Drewnowski, A. Contribution of food prices and diet cost to socioeconomic disparities in diet quality and health: A systematic review and analysis. Nutr. Rev. 2015, 73, 643–660. [Google Scholar] [CrossRef]
- Kelly, B.; Halford, J.C.; Boyland, E.J.; Chapman, K.; Bautista-Castaño, I.; Berg, C.; Caroli, M.; Cook, B.; Coutinho, J.G.; Effertz, T. Television food advertising to children: A global perspective. Am. J. Public Health 2010, 100, 1730–1736. [Google Scholar] [CrossRef]
- Nasreddine, L.; Taktouk, M.; Dabbous, M.; Melki, J. The extent, nature, and nutritional quality of foods advertised to children in Lebanon: The first study to use the WHO nutrient profile model for the Eastern Mediterranean Region. Food Nutr. Res. 2019, 63. [Google Scholar] [CrossRef]
- Amini, M.; Omidvar, N.; Yeatman, H.; Shariat-Jafari, S.; Eslami-Amirabadi, M.; Zahedirad, M. Content analysis of food advertising in Iranian children’s television programs. Int. J. Prev. Med. 2014, 5, 1337. [Google Scholar] [PubMed]
- World Health Organization. Nutrition-Friendly Schools Initiative (NFSI). Available online: https://www.who.int/nutrition/topics/nutrition_friendly_schools_initiative/en/ (accessed on 8 October 2020).
- World Health Organization. Global Accelerated Action for the Health of Adolescents (AA-HA!): Guidance to Support Country Implementation; World Health Organization: Geneva, Switzerland, 2017. [Google Scholar]
- World Health Organization Regional Office for the Eastern Mediterranean. Implementing the WHO Recommendations on the Marketing of Food and Nonalcoholic Beverages to Children in the Eastern Mediterranean Region; 9290222247; World Health Organization: Cairo, Egypt, 2018. [Google Scholar]
- World Health Organization Regional Office for the Eastern Mediterranean. Strategy on Nutrition for the Eastern Mediterranean Region 2020–2030; World Health Organization: Cairo, Egypt, 2019. [Google Scholar]
- World Health Organization Regional Office for the Eastern Mediterranean. Regional Framework for Action on Obesity Prevention 2019–2023; World Health Organization: Cairo, Egypt, 2019. [Google Scholar]
- World Health Organization. Policy Statement and Recommended Actions for Lowering Sugar Intake and Reducing Prevalence of Type 2 Diabetes and Obesity in the Eastern Mediterranean Region; World Health Organization: Cairo, Egypt, 2016. [Google Scholar]
- World Health Organization. Policy Statement and Recommended Actions for Reducing Fat Intake and Lowering Heart Attack Rates in the Eastern Mediterranean Region; World Health Organization: Cairo, Egypt, 2014. [Google Scholar]
- World Health Organization. Policy Statement and Recommended Actions to Lower National Salt Intakes and Lower Death Rates from High Blood Pressure and Strokes in the Eastern Mediterranean Region; World Health Organization: Cairo, Egypt, 2014. [Google Scholar]
- HLPE. Nutrition and food systems. In A Report by the High Level Panel of Experts on Food Security and Nutrition of the Committee on World Food Security; High Level Panel of Experts: Rome, Italy, 2017. [Google Scholar]
- UNICEF. The Faces of Malnutrition. Available online: https://www.unicef.org/nutrition/index_faces-of-malnutrition.html (accessed on 30 September 2020).
| Country | Fruits | Vegetables | Dairy | Meat, Poultry, and Fish | Fast Foods | SSBs | Sweet Snacks (Including Confectionary) | Salty and Fried Snacks | |
|---|---|---|---|---|---|---|---|---|---|
| Cakes/Pastries | Sweets/Chocolates | ||||||||
| Bahrain [52] (National) | 25.3% | 26.3% | 37.1% | Meat: 20% Fish: 6.9% Poultry: 18.2% | 14.4% | 42.2% | -- | Sweets: 31.4% Chocolates: 32% | -- |
| Egypt [42] | 29% | 78.2% | 58.9% | -- | 64.6% | 19.7% | -- | -- | -- |
| Iran [48] | 16.2% | 16.3% | Meat: 31.9% | -- | 75.4% | 45.5% | 84.7% | ||
| Iraq [36] | M: 24.3% F: 46.3% | M: 46.1% F: 62.3% | Milk: M: 37.2% F: 35.2% | -- | >3 days/w: M: 37.1% F: 24.9% | >3 days/w: M: 66.9% F: 60.4% | >3 days/w: M: 46.1% F: 55% | >3 days/w: M: 43.5% F: 52.2% | >3 days/w: M: 51% F: 64.6% |
| Jordan [54] | 20% | 43% | -- | 1–3 times/w: Meat: 47% Fish: 54% 4–6 times/w: Poultry: 40% | 1–3 times/w: 57% | -- | -- | Chocolates: 40% | -- |
| Kuwait [57] | M: 17.5% F: 11.8% | M: 26% F: 22.1% | M: 36.3% F: 25.3% | -- | M: 9.4% F: 10.4% | M: 42.2% F: 37.5% | M: 7% F: 14.7% | M: 21.1% F: 35.6% | Potato fries/chips: M: 9.4%; F: 12.4% |
| Kuwait [58] (National) | -- | -- | -- | -- | -- | >1 time/d: 43% | >1 time/d: 42.5% | >1 time/d: 42% | -- |
| Morocco [43,44] | M: 18.7% F: 20.4% | M: 33.1% F: 42.5% | M: 78.1% F: 76.9% | -- | >3 times/w: M: 15% F: 12.9% | >3 times/w: M: 37.5% F: 41.9% | >3 times/w: M: 66.9% F: 79% | 3 times/w: M: 66.9% F: 72% | >3 times/w: Potato fries/chips: M: 18.8%; F: 29% |
| Palestine [53] | M: 11.6% F: 16.2% | M: 27.6% F: 34.1% | Milk: M: 33.7% F: 29.9% Yogurt: M: 19.8% F: 20.8% | >3 times/w: Meat: M: 7.3% F: 7.9% Poultry: M: 3.4% F: 3.8% | -- | M: 6.2% F: 9.3% | Cookies: M: 14.6% F: 19.6% | Chocolates: M: 10.7% F: 17% | -- |
| Palestine [65] (National) | 31% | 45% | Milk: 22% | Meat and poultry: 16% | -- | 24% | 35% | -- | |
| Palestine [37] | M: 58.9% F: 55.2% | M: 72.8% F:73.8% | Milk: M: 32.9% F: 18.3% Yogurt: M: 31.8% F: 28.3% | Meat: M: 11.4% F: 10.7% Poultry: M: 11.9% F: 12.2% | -- | M: 39.6% F: 28.4% | M: 42.3% F: 49.2% | Salty snacks: M: 50.3% F: 61.5% Fried potatoes: M: 20.5% F: 23.8% | |
| Qatar [66] | 13.9% | 20.3% | 24.1% | -- | ≥4 days/w: 27.3% | ≥4 days/w: 48.8% | ≥4 days/w: 24.5% | ≥4 days/w: 49.4% | ≥4 days/w: 28.7% |
| Saudi [67] | M: 16% F: 9.6% | M: 23.3% F: 22.3% | Milk: M: 33.2% F: 25.1% | -- | >3 days/w: M: 30.2% F: 24.9% | >3 days/w: M: 67.3% F: 57.4% | >3 days/w: M: 24.8% F: 28.8% | >3 days/w: M: 37.3% F: 52.6% | >3 days/w: M: 25% F: 30.7% |
| Sudan [50] | M: 33.5% F: 31.9% | M: 70.1% F: 69.7% | -- | Meat: M: 55.7% F: 60.7% | -- | M: 43.9% F: 44.8% | Sweets: M: 55.4% F: 60.6% | -- | Crisps: M: 38.7% F: 39.2% Other salty snacks: M: 42.9% F: 32% |
| Sudan [51] | >4 times/w: 30.1% | >4 times/w: 63.9% | >4 times/w: 58.1% | >4 times/w: Meat: 59.1% Fish: 11.4% Poultry: 27.8% | >4 times/w: 26.6% | >4 times/w: 43.4% | >4 times/w: 37.1% | >4 times/w: Chocolates: 30.1% | -- |
| Sudan [68] | -- | -- | -- | -- | -- | 80.6% | Dessert: 69.3% Sweet biscuits: 65.3% | Chocolates: 80% Popsicles: 61.4% Sweets: 48.7% | -- |
| UAE [40] | -- | -- | -- | -- | ≥1 time/w: M: 77.3% F: 81.4% | ≥1 time/d: M: 41.1% F: 34% | -- | -- | -- |
| Country | Study Area | Study Population | Dietary Assessment | CHO (%EI) | Protein (%EI) | Fat (%EI) |
|---|---|---|---|---|---|---|
| Bahrain [28] | 11 regions of Bahrain | 11–18 year old children and adolescents; n = 496 | 24-HR | M: 45–52.5; F: 52–53 | M: 15.5–15.9; F: 15–15.4 | M: 31.1–32.5; F: 32.7–33.9 |
| Egypt [97] | Sohag | 12–18 year old adolescents; n = 300 | 24-HR | 59.1–61.3 | 15.7–15.9 | 26.9–28.5 |
| Iran [80] | Lahijan, Northern Iran | 14–17 year old girls; n = 400 | 24-HR | 59.3 | 11.9 | 28.8 |
| Iran [87] | Tehan | 10–19 year old girls; n = 717 | FFQ | -- | -- | 30.6 |
| Iran [48] | Sistan and Baluchistan | 14–18 year old girls; n = 753 | 2-day 24-HR | 54 | 14 | 31.9 |
| Iran [33] | Tehan | 6–18 year old; n = 424 | FFQ | M: 57.2; F: 56.8 | M: 12.9; F: 13.2 | M: 32.1; F: 32.4 |
| Iran [34] | Isfahan | Primary school and junior high school pupils; n = 4700 | FFQ | 64.1 | 12 | 23.8 |
| Kuwait [98] | Different regions in Kuwait | 8, 13 and 17 year old students; n = 588 | Questionnaire | 60.6 | 13 | 32.2 |
| Kuwait [84] | National | 9–18 year old children and adolescents; n = 614 | 24-HR | M: 53–54; F: 53 | M: 15; F: 14–15 | M: 31–32; F: 32–33 |
| Lebanon [24] | National | 12–19 year old adolescents; n = 498 | 24-HR | 51.1 | 13.5 | 36.2 |
| Lebanon [89] | National | 12–19 year old children and adolescents; n = 3394 | 24-HR | 51.4 | 13.4 | 36 |
| Libya [92] | Benghazi | 12 year old adolescents; n = 180 | 3-day food record | 54 | 15.7 | 30.2 |
| Morocco [93,94] | Ouarzazate | 15–18 year old adolescents; n = 327 | 3-day food record | M: 58.8; F: 56.6 | M: 12.9; F: 12.1 | M: 28.3; F: 31.3 |
| Oman [79] | Muscat | 15–18 year old adolescents; n = 802 | FFQ | M: 55.5; F: 51.1 | M: 22.5; F: 18.7 | M: 30.4; F: 22.6 |
| Pakistan [99] | Sialkot | Mean age: 14.3 years; n = 328 | 3-day food record | 51.5 | 12.5 | 36.3 |
| Pakistan [100] | National | 6–16 year old children and adolescents; n = 237 | 24-HR | 60–74 | 10–12 | 18–32 |
| Palestine [85] | East Jerusalem | 11–16 year old adolescents; n = 313 | 24-HR | 54 | 12.7 | 34.7 |
| Saudi-Arabia [101] | Riyadh and Dawadami | 17–19 year old adolescents; n = 600 | 24-HR | R: 54.4; U: 54.3 | R: 16.9; U: 15.1 | R: 29.5; U: 32.8 |
| Saudi-Arabia [82] | Jeddah | 13–18 year old adolescents; n = 239 | 3-day 24-HR | 56.6 | 13 | 30.5 |
| Sudan [86] | Northern State | 10–19 year old adolescents; n = 401 | 24-HR | 77.4 | 12.6 | 9.9 |
| Tunisia [91] | 3 regions in Tunisia | 15–19 year old adolescents; n = 1019 | FFQ | 52 | 12 | 36 |
| UAE [78] | National | 11–18 year old adolescents; n = 276 | 24-HR | M: 59.1; F: 58.2 | M: 16; F: 14.9 | M: 25.8; F: 27.8 |
| UAE [29] | National | 11–18 year old adolescents; n = 276 | 24-HR | -- | M: 15–16; F: 14.7–15.3 | M: 25.2–26.7; F: 27.6–27.9 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Al-Jawaldeh, A.; Taktouk, M.; Nasreddine, L. Food Consumption Patterns and Nutrient Intakes of Children and Adolescents in the Eastern Mediterranean Region: A Call for Policy Action. Nutrients 2020, 12, 3345. https://doi.org/10.3390/nu12113345
Al-Jawaldeh A, Taktouk M, Nasreddine L. Food Consumption Patterns and Nutrient Intakes of Children and Adolescents in the Eastern Mediterranean Region: A Call for Policy Action. Nutrients. 2020; 12(11):3345. https://doi.org/10.3390/nu12113345
Chicago/Turabian StyleAl-Jawaldeh, Ayoub, Mandy Taktouk, and Lara Nasreddine. 2020. "Food Consumption Patterns and Nutrient Intakes of Children and Adolescents in the Eastern Mediterranean Region: A Call for Policy Action" Nutrients 12, no. 11: 3345. https://doi.org/10.3390/nu12113345
APA StyleAl-Jawaldeh, A., Taktouk, M., & Nasreddine, L. (2020). Food Consumption Patterns and Nutrient Intakes of Children and Adolescents in the Eastern Mediterranean Region: A Call for Policy Action. Nutrients, 12(11), 3345. https://doi.org/10.3390/nu12113345






