Effect of Family-Based REDUCE Intervention Program on Children Eating Behavior and Dietary Intake: Randomized Controlled Field Trial
Abstract
1. Introduction
2. Materials and Methods
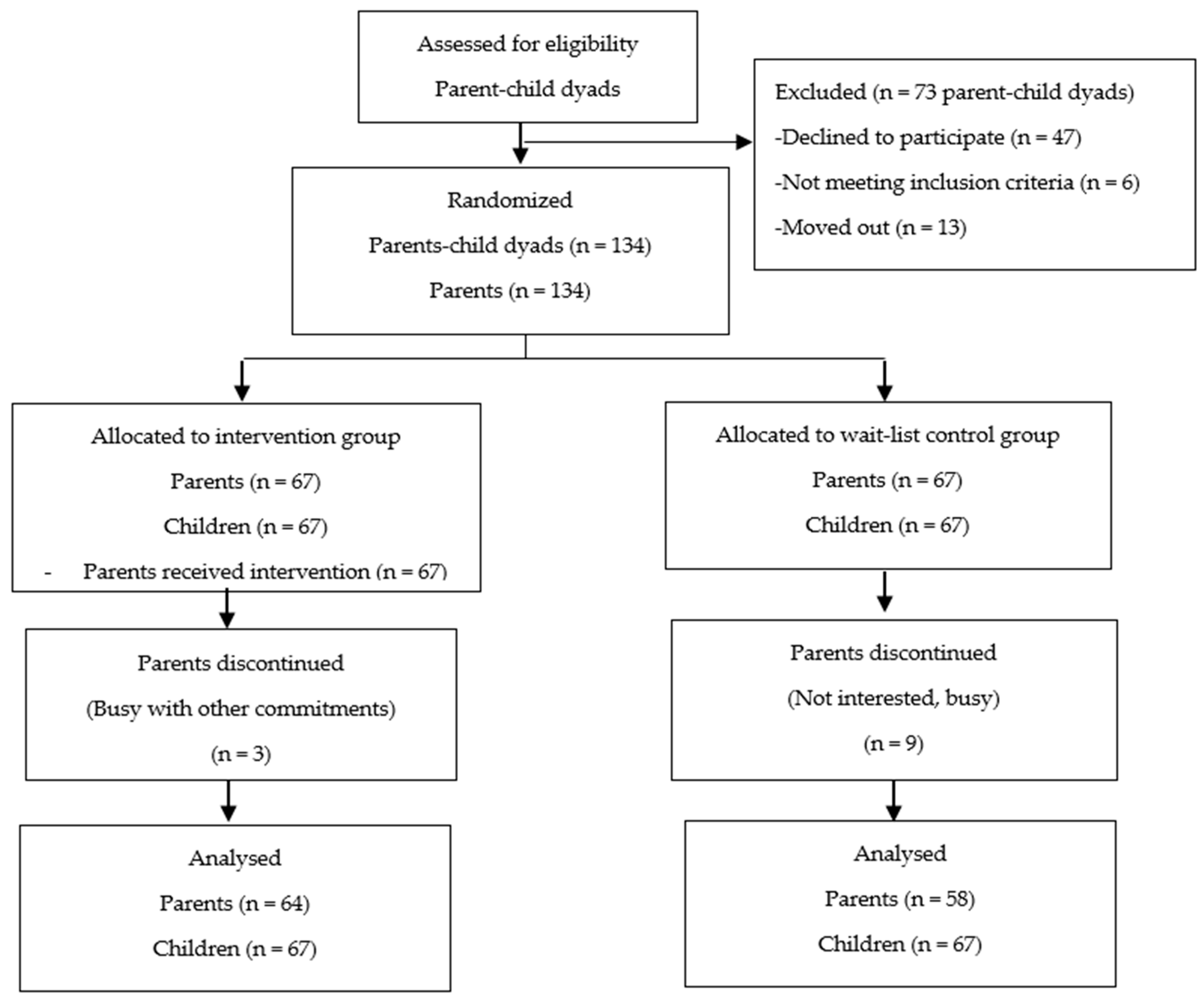
2.1. Participants and Design
2.2. Intervention
2.3. Measures
2.4. Data Collection
2.5. Ethical Considerations
2.6. Statistical Analysis
3. Results
Effectiveness of the Intervention on Children’s Eating Behaviors
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- World Health Organization. New Global Estimates of Child and Adolescent Obesity Released on World Obesity Day. Available online: https://www.who.int/end-childhood-obesity/news/new-estimate-child-adolescent-obesity/en/ (accessed on 6 September 2020).
- Institute of Public Health Malaysia. National Health and Morbidity Survey 2011. Non Communicable Diseases. Volume II. [Internet]. Institute of Public Health Malaysia. 2011, p. 192. Available online: http://www.iku.gov.my/images/IKU/Document/REPORT/NHMS2011-VolumeII.pdf (accessed on 6 June 2017).
- Institute of Public Health Malaysia. National Health & Morbidity Survey 2015. Non-Communicable Diseases, Risk Factors & Other Health Problems. 2015. Available online: http://www.iku.gov.my/images/IKU/Document/REPORT/nhmsreport2015vol2.pdf (accessed on 6 June 2017).
- Andexer, C. Fattest Kids in Asia: Malaysia’s Childhood Obesity a Fast-Growing Concern. Available online: https://today.mims.com/fattest-kids-in-asia—Malaysia-s-childhood-obesity-a-fast-growing-concern (accessed on 6 September 2020).
- World Health Organization. Global Strategy on Diet, Physical Activity and Health. The Role of Parents. Available online: https://www.who.int/dietphysicalactivity/childhood_parents/en/#:~:text=The%20promotion%20of%20 healthy%20diets,can%20influence%20their%20children’s%20behavior (accessed on 6 September 2020).
- Yee, A.Z.H.; Lwin, M.O.; Ho, S.S. The influence of parental practices on child promotive and preventive food consumption behaviors: A systematic review and meta- analysis. Int. J. Behav. Nutr. Phys. Act. 2017, 14, 47. [Google Scholar] [CrossRef] [PubMed]
- Niemeier, B.S.; Hektner, J.M.; Enger, K.B. Parent participation in weight-related health interventions for children and adolescents: A systematic review and meta-analysis. Prev. Med. 2012, 55, 3–13. [Google Scholar] [CrossRef] [PubMed]
- Freitas, A.; Silva, C. Appetite-Related Eating Behaviours: An Overview of Assessment Methods, Determinants and Effects on Children’s Weight. Ann. Nutr. Metab. 2018, 73, 19–29. [Google Scholar] [CrossRef] [PubMed]
- Santos, J.L.; Ho-Urriola, J.; González, A.; Smalley, S.V.; Domínguez-Vásquez, P.; Cataldo, R. Association between eating behavior scores and obesity in Chilean children. Nutr. J. BioMed Cent. Ltd. 2011, 10, 108. [Google Scholar] [CrossRef]
- Viana, V.; Sinde, S.; Saxton, J.C. Children’s Eating Behaviour Questionnaire: Associations with BMI in Portuguese children. Br. J. Nutr. 2018, 100, 445–450. [Google Scholar] [CrossRef]
- Webber, L.; Hill, C.; Saxton, J.; Van Jaarsveld, C.H.M.; Wardle, J. Eating behaviour and weight in children. Int. J. Obes. 2009, 33, 21–28. [Google Scholar] [CrossRef]
- Wardle, J.; Guthrie, C.A.; Sanderson, S.; Rapoport, L. Development of the Children’s Eating Behaviour Questionnaire. J. Child Psychol. Psychiatry 2001, 42, 963–970. [Google Scholar] [CrossRef]
- Magarey, A.; Mauch, C.; Mallan, K.; Perry, R.; Elovaris, R.; Meedeniya, J. Child dietary and eating behavior outcomes up to 3.5 years after an early feeding intervention: The Nourish RCT. Obesity 2016, 24, 1537–1545. [Google Scholar] [CrossRef]
- Pérez-Escamilla, R.; Obbagy, J.E.; Altman, J.M.; Essery, E.V.; McGrane, M.M.; Wong, Y.P. Dietary Energy Density and Body Weight in Adults and Children: A Systematic Review. J. Acad. Nutr. Diet. Elsevier 2012, 112, 671–684. [Google Scholar] [CrossRef]
- Moreno, L.A.; Rodríguez, G. Dietary risk factors for development of childhood obesity. Curr. Opin. Clin. Nutr. Metab. Care 2007, 10, 336–341. [Google Scholar] [CrossRef]
- Epstein, L.H.; Gordy, C.C.; Raynor, H.A.; Beddome, M.; Kilanowski, C.K.; Paluch, R. Increasing Fruit and Vegetable Intake and Decreasing Fat and Sugar Intake in Families at Risk for Childhood Obesity. Obes. Res. 2001, 9, 171–178. [Google Scholar] [CrossRef]
- Ello-martin, J.A.; Roe, L.S.; Ledikwe, J.H.; Beach, A.M.; Rolls, B.J. Dietary energy density in the treatment of obesity: A year-long trial comparing 2 weight-loss diets. Am. J. Clin. Nutr. 2007, 85, 1465–1477. [Google Scholar] [CrossRef] [PubMed]
- National Center for Chronic Disease Prevention and Health Promotion. Can eating fruits and vegetables help people to manage their weight ? Res. Pract. 2012, 1, 1–6. Available online: http://www.cdc.gov/nccdphp/dnpa/nutrition/pdf/rtp_practitioner_10_07.pdf (accessed on 4 April 2014).
- Malik, V.S.; Pan, A.; Willett, W.C.; Hu, F.B. Sugar-sweetened beverages and weight gain in children and adults: A systematic review and meta-analysis. Am. J. Clin. Nutr. 2013, 98, 1084–1102. [Google Scholar] [CrossRef] [PubMed]
- Torre, S.B.D.; Keller, A.; Depeyre, J.; Kruseman, M. Sugar-Sweetened Beverages and Obesity Risk in Children and Adolescents: A Systematic Analysis on How Methodological Quality May Influence Conclusions. J. Acad. Nutr. Diet. 2016, 116, 638–659. [Google Scholar] [CrossRef] [PubMed]
- Saidatul Norbaya, B. School Health Service. Available online: http://www.myhealth.gov.my/en/school-health-service/ (accessed on 14 April 2017).
- Norliza, A.; Zalilah, M.S.; Firdaus, M.; Lye, M.S. Family-based intervention using face-to- face sessions and social media to improve Malay primary school children’s adiposity: A randomized controlled field trial of the Malaysian REDUCE programme. Nutr. J. 2018, 17, 74. [Google Scholar]
- Bandura, A. On the Functional Properties of Perceived Self-Efficacy Revisited. J. Manag. 2012, 38, 9–44. [Google Scholar] [CrossRef]
- Bandura, A. Social Foundations of Thought and Action: A Social-Cognitive Theory; Prentice-Hall: Englewood Cliffs, NJ, USA, 1986; pp. 23–28. [Google Scholar]
- Sacher, P.M.; Kolotourou, M.; Chadwick, P.M.; Cole, T.J.; Lawson, M.S.; Lucas, A. Randomized Controlled Trial of the MEND Program: A Family-based Community Intervention for Childhood Obesity. Obesity 2010, 18 (Suppl. S1), S62–S68. [Google Scholar] [CrossRef]
- Catenacci, V.; Barrett, C.; Odgen, L.; Browning, R.; Schaefer, C.A.; Hill, J.; Wyatt, H. Changes in physical activity and sedentary behavior in a randomized trial of an internet-based versus workbook-based family intervention study. J. Phys. Act. 2014, 11, 348–358. [Google Scholar] [CrossRef][Green Version]
- Chen, J.L.; Weiss, S.; Heyman, M.B.; Cooper, B.; Lustig, R.H. The efficacy of the web-based childhood obesity prevention program in Chinese American adolescents (Web ABC study). J. Adolesc. Health 2011, 49, 148–154. [Google Scholar] [CrossRef]
- Cooperberg, J. Food for Thought: A Parental Internet-based Intervention to Treat Childhood Obesity in Preschool-Aged Children. Ph.D. Thesis, Washington University, St Louis, MO, USA, 2013. [Google Scholar]
- Williamson, D.A.; Walden, H.M.; White, M.A.; York-Crowe, E.; Newton, R.L.; Alfonso, A. Two-year internet-based randomized controlled trial for weight loss in African-American girls. Obesity (Silver Spring) 2006, 14, 1231–1243. [Google Scholar] [CrossRef]
- Knowlden, A.P. Feasibility and Efficacy of the Enabling Mothers to Prevent Pediatric Obesity through Web-Based Education and REciprocal Determinism (EMPOWER) Randomized Control Trial. Ph.D. Thesis, University of Cincinnati, Cincinnati, OH, USA, 2013. [Google Scholar]
- Lochrie, A.; Wysocki, T.; Hossain, J.; Milkes, A.; Antal, H.; Buckloh, L. The Effects of a Family-Based Intervention (FBI) for Overweight/Obese Children on Health and Psychological Functioning. Clin. Pract. Pediatr. Psychol. 2013, 1, 159–170. [Google Scholar] [CrossRef]
- Esfarjani, F.; Khalafi, M.; Mohammadi, F.; Mansour, A.; Roustaee, R.; Zamani-Nour, N. Family-based intervention for controlling childhood obesity: An experience among iranian children. Int. J. Prev. Med. 2013, 4, 358–365. [Google Scholar] [PubMed]
- Schwartz, R.P.; Vitolins, M.Z.; Case, L.D.; Armstrong, S.C.; Perrin, E.M.; Cialone, J.; Bell, R.A. The YMCA Healthy, Fit, and Strong Program: A community-based, family-centered, low-cost obesity prevention/treatment pilot study. Child. Obes. 2012, 8, 577–582. [Google Scholar] [CrossRef] [PubMed]
- Croker, H.; Viner, R.; Nicholls, D.; Haroun, D.; Chadwick, P.; Edwards, C. Family-based behavioural treatment of childhood obesity in a UK National Health Service setting: Randomized controlled trial. Int. J. Obes. 2012, 36, 16–26. [Google Scholar] [CrossRef] [PubMed]
- West, F.; Sanders, M.R.; Cleghorn, G.J.; Davies, P.S.W. Randomised clinical trial of a family-based lifestyle intervention for childhood obesity involving parents as the exclusive agents of change. Behav. Res. Ther. 2010, 48, 1170–1179. [Google Scholar] [CrossRef] [PubMed]
- Golley, R.K.; Magarey, A.M.; Baur, L.A.; Steinbeck, K.S.; Daniels, L.A. Twelve-Month Effectiveness of a Parent-led, Family-Focused Weight-Management Program for Prepubertal Children: A Randomized, Controlled Trial. Pediatrics 2007, 119, 517–525. [Google Scholar] [CrossRef] [PubMed]
- Golan, M.; Crow, S. Targeting parents exclusively in the treatment of childhood obesity: Long-term results. Obes. Res. 2004, 12, 357–361. [Google Scholar] [CrossRef]
- Epstein, L.H. Family-based behavioural intervention for obese children. Int. J. Obes. Relat. Metab Disord 1996, 20 (Suppl. S1), S14–S21. [Google Scholar]
- Epstein, L.H.; McCurley, J.; Wing, R.R.; Valoski, A. Five-year follow-up of family-based behavioral treatments for childhood obesity. J. Consult. Clin. Psychol. 1990, 58, 661. [Google Scholar] [CrossRef]
- Horton, L.A.; Parada, H.; Slymen, D.J.; Arredondo, E.; Ibarra, L.; Ayala, G.X. Targeting children’s dietary behaviors in a family intervention: Entre familia: Reflejos de salud. Salud Publica Mex. 2013, 55 (Suppl. S3), 397–405. [Google Scholar] [PubMed]
- Anand, S.S.; Davis, A.D.; Ahmed, R.; Jacobs, R.; Xie, C.; Hill, A. A family-based intervention to promote healthy lifestyles in an aboriginal community in Canada. Can. J. Public Health 2007, 98, 447–452. [Google Scholar] [CrossRef] [PubMed]
- Nyberg, G.; Sundblom, E.; Norman, Å.; Bohman, B.; Hagberg, J.; Elinder, L.S. Effectiveness of a universal parental support programme to promote healthy dietary habits and physical activity and to prevent overweight and obesity in 6-year-old children: The healthy school start study, a cluster-randomised controlled trial. Int. J. Behav. Nutr. Phys. Act. 2015, 10, 1–14. [Google Scholar] [CrossRef] [PubMed]
- Ministry of Health Malaysia. Malaysian Dietary Guidelines for Children and Adolescents. 2013. Available online: http://nutrition.moh.gov.my/wp-content/uploads/penerbitan/buku/MDG_Children_adolescent_2014.pdf (accessed on 4 April 2017).
- Krølner, R.; Rasmussen, M.; Brug, J.; Klepp, K.-I.; Wind, M.; Due, P. Determinants of fruit and vegetable consumption among children and adolescents: A review of the literature. Part II: Qualitative studies. Int. J. Behav. Nutr. Phys. Act. 2011, 8, 112. [Google Scholar] [CrossRef] [PubMed]
- Zimmerman, F.J.; Bell, J.F. Associations of television content type and obesity in children. Am. J. Public Health 2010, 100, 334–340. [Google Scholar] [CrossRef]
- Edward, R. Children Exposed to Junk Food at Schools. The Star Online [Internet]. 2016. Available online: http://www.thestar.com.my/metro/community/2016/05/25/children-exposed-to-junk-food-at-schools-street-vendors-serve-up-unhealthy-fare-right-at-the-gates/ (accessed on 4 April 2017).
- Hayati Adilin, M.A.M.; Holdsworth, M.; McCullough, F.; Swift, J.A.; Norimah, A.K. Whole school mapping to investigate the school environment’s potential to promote a healthy diet and physical activity in Malaysia. Malays J. Nutr. 2015, 21, 1–14. [Google Scholar]
| Unit | Topic and Contents in REDUCE Program | Unit | Topic and Contents in REDUCE Program |
|---|---|---|---|
| 1 | Introduction and parenting skills * • Introduction of program • Obesity and healthy lifestyles • Parenting skills and parental role • How to fill in food record • Information on REDUCE program | 2 | Sugar-sweetened beverages (SSB) * • Target for SSB • What is SSB? • Why are SSBs bad for health? • Tips to reduce SSB intake • Parenting skills and roles • Problematic scenarios and suggested solutions • SSB Diary • Feedback and discussion during face-to-face training |
| 3 | Fruit and vegetable (FV) ** • Target for FV • Why FV are good for health? • Example of servings for fruit and vegetables • How to cook vegetables • Tips to increase FV intake • Parenting skills and roles • Problematic scenarios and suggested solutions • SSB and FV Diary • Feedback and discussion on social media | 4 | Unhealthy snacks/junk food ** • Target for snacks • What are snacks? • Why are snacks bad for health? • Types of fat • Reading food labels • Tips to reduce snack intake • Parenting skills and roles • Problematic scenarios and suggested solutions • Food record • Feedback and discussion on social media |
| 5 | Physical activity ** • Target for physical activity • What is physical activity? • Why is physical activity good for health? • Examples of moderate and vigorous activities • Examples of activity to strengthen muscles and bones • Tips to increase physical activity • Parenting skills and roles • Problematic scenarios and suggested solutions • Physical activity record • Feedback and discussion on social media | 6 | Screen time ** • Target for screen time • What is screen time? • Why prolong screen time bad for health? • Tips to reduce screen time • Parenting skills and roles • Scenario of problem and suggested solutions • Physical activity record including screen time • Feedback and discussion on social media |
| 7 | Risky situations and review of performance * • What are “risky situations” • Examples of risky situation • Why are these risky situations bad for health? • How to deal with “risky situations” • Parenting skills and roles • Problematic scenarios and suggested solutions • Feedback and discussion during face-to-face training | 8 | Further role and action * • Obesity issues • Exercise Tips *** • Calories needed and examples of serving according to age and sex • Examples of success stories • Summary of REDUCE program • Parental role |
| SCT’s Behavioral Change Techniques | REDUCE Program |
|---|---|
| Goal setting | Units 2, 3, 4, 5 and 6: These units explain about the five targets * and parents are expected to set goals that are suitable after discussion with their children. Parents are encouraged to choose one goal and make small changes, one at a time. |
| Self-monitoring | Units 2, 3, 4, 5 and 6: Parents are encouraged to monitor the achievement of the goals * that they set using the booklet which was provided to them. |
| Problem solving | Units 2, 3, 4, 5, 6 and 7: Parents are informed about problems that may arise in achieving the goals * and examples of how to manage them. Parents are encouraged to write down any problems they have encountered and how they have managed them in the booklet. They are also encouraged to communicate with the researcher about the problems through Facebook or WhatsApp if they are unable to solve them. |
| Behavioral capability | Unit 1 to Unit 8: Parents are expected to gain the knowledge and skills needed to achieve the goals *. Parents are also equipped with authoritative parenting skills to handle their reluctant children. Helping parents to handle the problems they face may improve their self-efficacy. Parents are also provided with feedback on their children’s anthropometric progress. |
| Stimulus control | Units 2, 4 and 7: Parents are taught to avoid or control the environment, either outside or inside the house that might induce intake of unhealthy foods. |
| Relapse prevention | Unit 8: Parents are taught about high-risk situations where it is difficult for them to achieve the goals * and how to handle them. |
| Characteristics | Mean (SD) or N (%) | ||
|---|---|---|---|
| Intervention | Wait-List Control | p-Value | |
| Parent | |||
| Age (years) | 39.8 (3.6) | 41.3 (5.7) | 0.079 |
| Gender—female a | 39 (58.2) | 37 (55.2) | 0.862 |
| BMI (kg/m2) b | 27.4 (4.41) | 27.8 (4.27) | 0.622 |
| Mother’s education a | 0.665 | ||
| Secondary and below | 24 (35.8) | 27 (40.3) | |
| Tertiary | 43 (64.2) | 40 (59.7) | |
| Father’s education a | 0.419 | ||
| Secondary and below | 20 (29.9) | 28 (41.8) | |
| Tertiary | 47 (70.1) | 39 (58.2) | |
| Monthly family income a | 0.921 | ||
| Less than RM5000 | 21 (31.3) | 22 (32.8) | |
| RM5000 to RM10000 | 29 (43.3) | 30 (44.8) | |
| More than RM10000 | 17 (25.4) | 15 (22.4) | |
| Child | |||
| Age (years) | 9.6 (1.2) | 9.6 (1.2) | 0.826 |
| Gender—female a | 40 (59.7) | 38 (56.7) | 0.861 |
| BMI z-score | 2.0 (0.4) | 2.1 (0.4) | 0.381 |
| BMI z-score category a,b | 0.861 | ||
| Overweight (%) | 28 (41.8) | 27 (40.3) | |
| Obese (%) | 39 (58.2) | 40 (59.7) | |
| Children’s Eating Behaviors | Parameter | F statistics | Df1 | Df2 | p-Value a |
|---|---|---|---|---|---|
| Enjoyment of food | Group | 1.167 | 1 | 481 | 0.280 |
| (n = 119) | Group × Time | 4.653 | 6 | 481 | <0.001 * |
| Satiety responsiveness | Group | 7.142 | 1 | 481 | 0.008 * |
| (n = 120) | Group × Time | 1.430 | 6 | 481 | 0.201 |
| Food responsiveness | Group | 0.525 | 1 | 475 | 0.469 |
| (n = 118) | Group × Time | 2.054 | 6 | 475 | 0.057 |
| Dietary Intake | Parameter | F | Df1 | Df2 | p-Value a |
|---|---|---|---|---|---|
| SSB intake (n = 122) | Group | 9.647 | 1 | 480 | 0.002 * |
| Group × Time | 1.373 | 6 | 480 | 0.224 | |
| Fruit and vegetable intake (n = 122) | Group | 1.493 | 1 | 480 | 0.222 |
| Group × Time | 4.165 | 6 | 480 | <0.001 * | |
| Unhealthy snack intake (n = 122) | Group | 0.166 | 1 | 480 | 0.684 |
| Group × Time | 5.062 | 6 | 480 | <0.001 * |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ahmad, N.; Shariff, Z.M.; Mukhtar, F.; Lye, M.-S. Effect of Family-Based REDUCE Intervention Program on Children Eating Behavior and Dietary Intake: Randomized Controlled Field Trial. Nutrients 2020, 12, 3065. https://doi.org/10.3390/nu12103065
Ahmad N, Shariff ZM, Mukhtar F, Lye M-S. Effect of Family-Based REDUCE Intervention Program on Children Eating Behavior and Dietary Intake: Randomized Controlled Field Trial. Nutrients. 2020; 12(10):3065. https://doi.org/10.3390/nu12103065
Chicago/Turabian StyleAhmad, Norliza, Zalilah Mohd Shariff, Firdaus Mukhtar, and Munn-Sann Lye. 2020. "Effect of Family-Based REDUCE Intervention Program on Children Eating Behavior and Dietary Intake: Randomized Controlled Field Trial" Nutrients 12, no. 10: 3065. https://doi.org/10.3390/nu12103065
APA StyleAhmad, N., Shariff, Z. M., Mukhtar, F., & Lye, M.-S. (2020). Effect of Family-Based REDUCE Intervention Program on Children Eating Behavior and Dietary Intake: Randomized Controlled Field Trial. Nutrients, 12(10), 3065. https://doi.org/10.3390/nu12103065





