Effects of the Human Gut Microbiota on Cognitive Performance, Brain Structure and Function: A Narrative Review
Abstract
1. Introduction
2. Materials and Methods
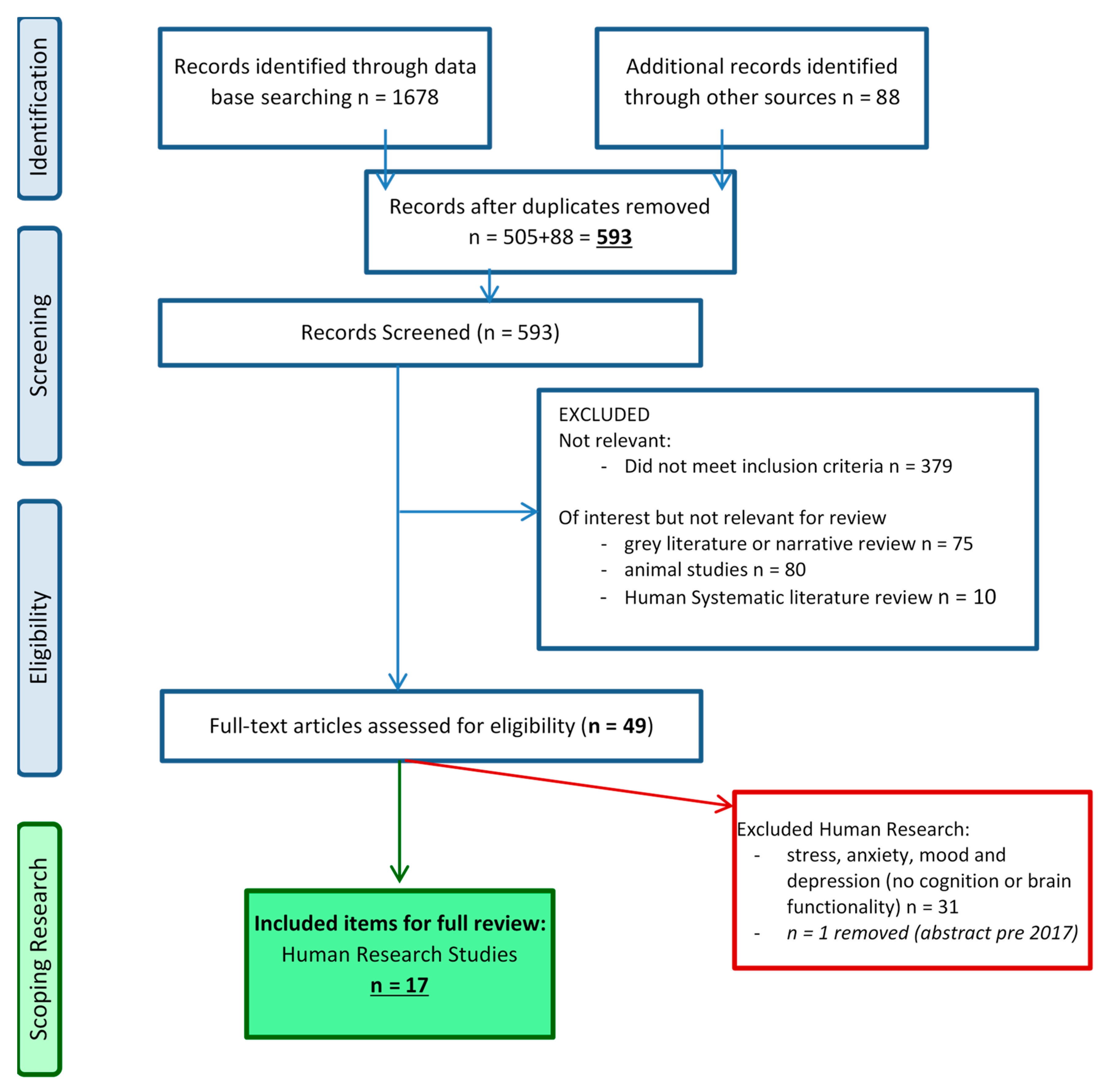
2.1. Identification and Screening of Relevant Studies
2.1.1. Search Criteria
2.1.2. Screening Process and Study Selection
2.1.3. Data Extraction for Analysis
3. Results
3.1. General Data Extraction and Matrices
3.2. Correlational Microbiota Design Studies
3.3. Intervention Design Studies Linking Microbiota Profile(s)/Signatures to Cognition and Brain Structures/Function
3.3.1. Probiotics
Single-Species Probiotic Intervention
Multi-Species Probiotic Intervention
3.3.2. Prebiotics
3.3.3. Paraprobiotics
3.3.4. Synbiotic
4. Discussion
4.1. Scope of Review
4.2. Overall Synthesis
4.3. Limitations
4.4. Recommendations
4.5. Future Directions
5. Conclusions
Supplementary Materials
Funding
Acknowledgments
Conflicts of Interest
References
- Scholz-Ahrens, K.E.; Ade, P.; Marten, B.; Weber, P.; Timm, W.; Acil, Y.; Gluer, C.C.; Schrezenmeir, J. Prebiotics, probiotics, and synbiotics affect mineral absorption, bone mineral content, and bone structure. J. Nutr. 2007, 137, 838s–846s. [Google Scholar] [CrossRef] [PubMed]
- Gonzalez-Ochoa, G.; Flores-Mendoza, L.K.; Icedo-Garcia, R.; Gomez-Flores, R.; Tamez-Guerra, P. Modulation of rotavirus severe gastroenteritis by the combination of probiotics and prebiotics. Arch. Microbiol. 2017, 199, 953–961. [Google Scholar] [CrossRef] [PubMed]
- Patterson, E.; Cryan, J.F.; Fitzgerald, G.F.; Ross, R.P.; Dinan, T.G.; Stanton, C. Gut microbiota, the pharmabiotics they produce and host health. Proc. Nutr. Soc. 2014, 73, 477–489. [Google Scholar] [CrossRef] [PubMed]
- Mayer, E.A.; Knight, R.; Mazmanian, S.K.; Cryan, J.F.; Tillisch, K. Gut microbes and the brain: Paradigm shift in neuroscience. J. Neurosci. 2014, 34, 15490–15496. [Google Scholar] [CrossRef] [PubMed]
- van Baarlen, P.; Troost, F.; van der Meer, C.; Hooiveld, G.; Boekschoten, M.; Brummer, R.J.; Kleerebezem, M. Human mucosal in vivo transcriptome responses to three lactobacilli indicate how probiotics may modulate human cellular pathways. Proc. Natl. Acad. Sci. USA 2011, 108 (Suppl. 1), 4562–4569. [Google Scholar] [CrossRef]
- Bagga, D.; Reichert, J.L.; Koschutnig, K.; Aigner, C.S.; Holzer, P.; Koskinen, K.; Moissl-Eichinger, C.; Schöpf, V. Probiotics drive gut microbiome triggering emotional brain signatures. Gut Microbes 2018, 9, 486–496. [Google Scholar] [CrossRef]
- Lew, L.C.; Hor, Y.Y.; Liong, M.T.; Yusoff, N.A.A.; Yusoff, M.S.B.; Roslan, N.S.; Ahmad, A.; Mohammad, J.A.M.; Zakaria, N.; Choi, S.B.; et al. Probiotic Lactobacillus plantarum P8 alleviated stress and anxiety while enhancing memory and cognition in stressed adults: A randomised, double-blind, placebo-controlled study. Clin. Nutr. 2018. [Google Scholar] [CrossRef] [PubMed]
- Tillisch, K.; Labus, J.; Kilpatrick, L.; Jiang, Z.; Stains, J.; Ebrat, B.; Guyonnet, D.; Legrain-Raspaud, S.; Trotin, B.; Naliboff, B.; et al. Consumption of fermented milk product with probiotic modulates brain activity. Gastroenterology 2013, 144, 1394–1401. [Google Scholar] [CrossRef]
- Sylvia, K.E.; Demas, G.E. A gut feeling: Microbiome-brain-immune interactions modulate social and affective behaviors. Horm. Behav. 2018, 99, 41–49. [Google Scholar] [CrossRef]
- Cawthon, C.R.; de La Serre, C.B. Gut bacteria interaction with vagal afferents. Brain Res. 2018, 1693, 134–139. [Google Scholar] [CrossRef]
- O’Mahony, S.M.; Clarke, G.; Borre, Y.E.; Dinan, T.G.; Cryan, J.F. Serotonin, tryptophan metabolism and the brain-gut-microbiome axis. Behav. Brain Res. 2015, 277, 32–48. [Google Scholar] [CrossRef]
- Osadchiy, V.; Labus, J.S.; Gupta, A.; Jacobs, J.; Ashe-McNalley, C.; Hsiao, E.Y.; Mayer, E.A. Correlation of tryptophan metabolites with connectivity of extended central reward network in healthy subjects. PLoS ONE 2018, 13, e0201772. [Google Scholar] [CrossRef]
- Mackos, A.R.; Maltz, R.; Bailey, M.T. The role of the commensal microbiota in adaptive and maladaptive stressor-induced immunomodulation. Horm. Behav. 2017, 88, 70–78. [Google Scholar] [CrossRef] [PubMed]
- Galley, J.D.; Bailey, M.T. Impact of stressor exposure on the interplay between commensal microbiota and host inflammation. Gut Microbes 2014, 5, 390–396. [Google Scholar] [CrossRef] [PubMed]
- Karl, J.P.; Margolis, L.M.; Madslien, E.H.; Murphy, N.E.; Castellani, J.W.; Gundersen, Y.; Hoke, A.V.; Levangie, M.W.; Kumar, R.; Chakraborty, N.; et al. Changes in intestinal microbiota composition and metabolism coincide with increased intestinal permeability in young adults under prolonged physiological stress. Am. J. Physiol. Gastrointest. Liver Physiol. 2017, 312, G559–G571. [Google Scholar] [CrossRef] [PubMed]
- Carding, S.; Verbeke, K.; Vipond, D.T.; Corfe, B.M.; Owen, L.J. Dysbiosis of the gut microbiota in disease. Microb. Ecol. Health Dis. 2015, 26, 26191. [Google Scholar] [CrossRef] [PubMed]
- Fröhlich, E.E.; Farzi, A.; Mayerhofer, R.; Reichmann, F.; Jačan, A.; Wagner, B.; Zinser, E.; Bordag, N.; Magnes, C.; Fröhlich, E.; et al. Cognitive impairment by antibiotic-induced gut dysbiosis: Analysis of gut microbiota-brain communication. Brain Behav. Immun. 2016, 56, 140–155. [Google Scholar] [CrossRef]
- Noble, E.E.; Hsu, T.M.; Kanoski, S.E. Gut to brain dysbiosis: Mechanisms linking western diet consumption, the microbiome, and cognitive impairment. Front. Behav. Neurosci. 2017, 11. [Google Scholar] [CrossRef]
- Jiang, H.; Zhang, X.; Yu, Z.; Zhang, Z.; Deng, M.; Zhao, J.; Ruan, B. Altered gut microbiota profile in patients with generalized anxiety disorder. J. Psychiatr. Res. 2018, 104, 130–136. [Google Scholar] [CrossRef]
- Chen, Z.; Hu, Z.; Chen, K.; Xie, P.; Li, J.; Gui, S.; Zhou, C.; Yang, C.; Wang, H.; Zhong, X.; et al. Comparative metaproteomics analysis shows altered fecal microbiota signatures in patients with major depressive disorder. NeuroReport 2018, 29, 417–425. [Google Scholar] [CrossRef]
- Sarkar, A.; Harty, S.; Dunbar, R.I.M.; Lehto, S.M.; Moeller, A.H.; Dinan, T.G.; Cryan, J.F.; Burnet, P.W.J. The Microbiome in Psychology and Cognitive Neuroscience. Trends Cogn. Sci. 2018, 22, 611–636. [Google Scholar] [CrossRef] [PubMed]
- Allen, A.P.; Hutch, W.; Borre, Y.E.; Kennedy, P.J.; Temko, A.; Boylan, G.; Murphy, E.; Cryan, J.F.; Dinan, T.G.; Clarke, G. Bifidobacterium longum 1714 as a translational psychobiotic: Modulation of stress, electrophysiology and neurocognition in healthy volunteers. Transl. Psychiatry 2016, 6, e939. [Google Scholar] [CrossRef] [PubMed]
- Schmidt, K.; Cowen, P.; Harmer, C.; Tzortzis, G.; Errington, S.; Burnet, P. Prebiotic intake reduces the waking cortisol response and alters emotional bias in healthy volunteers. Psychopharmacology 2015, 232, 1793–1801. [Google Scholar] [CrossRef]
- Li, X.; Kan, E.M.; Lu, J.; Cao, Y.; Wong, R.K.; Keshavarzian, A.; Wilder-Smith, C.H. Combat-training increases intestinal permeability, immune activation and gastrointestinal symptoms in soldiers. Aliment. Pharmacol. Ther. 2013, 37, 799–809. [Google Scholar] [CrossRef] [PubMed]
- Pomeroy, D.E.; Tooley, K.L.; Probert, B.; Wilson, A.; Kemps, E. A Systematic Review of the Effect of Dietary Supplements on Cognitive Performance in Healthy Young Adults and Military Personnel. Nutrients 2020, 12, 545. [Google Scholar] [CrossRef] [PubMed]
- Tricco, A.C.; Lillie, E.; Zarin, W.; O’Brien, K.K.; Colquhoun, H.; Levac, D.; Moher, D.; Peters, M.D.J.; Horsley, T.; Weeks, L.; et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. Ann. Intern. Med. 2018, 169, 467–473. [Google Scholar] [CrossRef] [PubMed]
- Arksey, H.; O’Malley, L. Scoping studies: Towards a methodological framework. Int. J. Soc. Res. Methodol. 2005, 8, 19–32. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef]
- Fernandez-Real, J.M.; Serino, M.; Blasco, G.; Puig, J.; Daunis-i-Estadella, J.; Ricart, W.; Burcelin, R.; Fernandez-Aranda, F.; Portero-Otin, M. Gut Microbiota Interacts with Brain Microstructure and Function. J. Clin. Endocrinol. Metab. 2015, 100, 4505–4513. [Google Scholar] [CrossRef]
- Anderson, J.R.; Carroll, I.; Azcarate-Peril, M.A.; Rochette, A.D.; Heinberg, L.J.; Peat, C.; Steffen, K.; Manderino, L.M.; Mitchell, J.; Gunstad, J. A preliminary examination of gut microbiota, sleep, and cognitive flexibility in healthy older adults. Sleep Med. 2017, 38, 104–107. [Google Scholar] [CrossRef]
- Taylor, A.M.; Edwards, C.G.; Khan, N.A.; Holscher, H.D. Gastrointestinal Microbiota and Cognitive Function in Adult Females. FASEB J. 2017, 31, 965. [Google Scholar]
- Labus, J.S.; Hollister, E.B.; Jacobs, J.; Kirbach, K.; Oezguen, N.; Gupta, A.; Acosta, J.; Luna, R.A.; Aagaard, K.; Versalovic, J.; et al. Differences in gut microbial composition correlate with regional brain volumes in irritable bowel syndrome. Microbiome 2017, 5, 49. [Google Scholar] [CrossRef] [PubMed]
- Kelly, J.R.; Allen, A.P.; Temko, A.; Hutch, W.; Kennedy, P.J.; Farid, N.; Murphy, E.; Boylan, G.; Bienenstock, J.; Cryan, J.F.; et al. Lost in translation? The potential psychobiotic Lactobacillus rhamnosus (JB-1) fails to modulate stress or cognitive performance in healthy male subjects. Brain Behav. Immun. 2017, 61, 50–59. [Google Scholar] [CrossRef]
- Bagga, D.; Aigner, C.S.; Reichert, J.L.; Cecchetto, C.; Fischmeister, F.P.S.; Holzer, P.; Moissl-Eichinger, C.; Schöpf, V. Influence of 4-week multi-strain probiotic administration on resting-state functional connectivity in healthy volunteers. Eur. J. Nutr. 2019, 58, 1821–1827. [Google Scholar] [CrossRef] [PubMed]
- Roman, P.; Sánchez-Labraca, N.; Cardona, D.; Estévez, A.F.; Cañadas, F.; Miras, A.; Vivas, A.B. A Pilot Randomized Controlled Trial to Explore Cognitive and Emotional Effects of Probiotics in Fibromyalgia. Sci. Rep. 2018, 8. [Google Scholar] [CrossRef] [PubMed]
- Smith, A.P.; Sutherland, D.; Hewlett, P. An Investigation of the Acute Effects of Oligofructose-Enriched Inulin on Subjective Wellbeing, Mood and Cognitive Performance. Nutrients 2015, 7, 8887–8896. [Google Scholar] [CrossRef]
- Chung, Y.-C.; Jin, H.-M.; Cui, Y.; Kim, D.S.; Jung, J.M.; Park, J.-I.; Jung, E.-S.; Choi, E.-K.; Chae, S.-W. Fermented milk of Lactobacillus helveticus IDCC3801 improves cognitive functioning during cognitive fatigue tests in healthy older adults. J. Funct. Foods 2014, 10, 465. [Google Scholar] [CrossRef]
- Ohsawa, K.; Nakamura, F.; Uchida, N.; Mizuno, S.; Yokogoshi, H. Lactobacillus helveticus-fermented milk containing lactononadecapeptide (NIPPLTQTPVVVPPFLQPE) improves cognitive function in healthy middle-aged adults: A randomised, double-blind, placebo-controlled trial. Int. J. Food Sci. Nutr. 2018, 69, 369–376. [Google Scholar] [CrossRef]
- Tooley, K.; Pomeroy, D.; Probert, B.; Govender, R.; Kemps, E. Beneficial cognitive effects of a synbiotic formulation in healthy young adults. In Proceedings of the Defence Human Sciences Symposium, Perth, Australia, 29–30 November 2018. [Google Scholar]
- Bravo, J.A.; Forsythe, P.; Chew, M.V.; Escaravage, E.; Savignac, H.M.; Dinan, T.G.; Bienenstock, J.; Cryan, J.F. Ingestion of Lactobacillus strain regulates emotional behavior and central GABA receptor expression in a mouse via the vagus nerve. Proc. Natl. Acad. Sci. USA 2011, 108, 16050–16055. [Google Scholar] [CrossRef]
- Janik, R.; Thomason, L.A.M.; Stanisz, A.M.; Forsythe, P.; Bienenstock, J.; Stanisz, G.J. Magnetic resonance spectroscopy reveals oral Lactobacillus promotion of increases in brain GABA, N-acetyl aspartate and glutamate. NeuroImage 2016, 125, 988–995. [Google Scholar] [CrossRef]
- Gibson, G.R.; Brummer, R.J.; Isolauri, E.; Lochs, H.; Morelli, L.; Ockhuizen, T.; Rowland, I.R.; Schrezenmeir, J.; Stanton, C.; Verbeke, K. The design of probiotic studies to substantiate health claims. Gut Microbes 2011, 2, 299–305. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Terpend, K.; Possemiers, S.; Daguet, D.; Marzorati, M. Arabinogalactan and fructo-oligosaccharides have a different fermentation profile in the Simulator of the Human Intestinal Microbial Ecosystem (SHIME®). Environ. Microbiol. Rep. 2013, 5, 595–603. [Google Scholar] [CrossRef] [PubMed]
- Hyland, N.; Stanton, C. The Gut-Brain Axis: Dietary, Probiotic, and Prebiotic Interventions on the Microbiota; Academic Press: London, UK, 2016. [Google Scholar]
- Kao, A.C.; Harty, S.; Burnet, P.W. The Influence of Prebiotics on Neurobiology and Behavior. Int. Rev. Neurobiol. 2016, 131, 21–48. [Google Scholar] [CrossRef] [PubMed]
- Pandey, K.R.; Naik, S.R.; Vakil, B.V. Probiotics, prebiotics and synbiotics—A review. J. Food Sci. Technol. 2015, 52, 7577–7587. [Google Scholar] [CrossRef]
- Taverniti, V.; Guglielmetti, S. The immunomodulatory properties of probiotic microorganisms beyond their viability (ghost probiotics: Proposal of paraprobiotic concept). Genes Nutr. 2011, 6, 261–274. [Google Scholar] [CrossRef]
- Ohsawa, K.; Uchida, N.; Ohki, K.; Nakamura, Y.; Yokogoshi, H. Lactobacillus helveticus-fermented milk improves learning and memory in mice. Nutr. Neurosci. 2015, 18, 232–240. [Google Scholar] [CrossRef]
- Ohsawa, K.; Uchida, N.; Ohki, K.; Yokogoshi, H. Identification of peptides present in sour milk whey that ameliorate scopolamine-induced memory impairment in mice. Int. J. Food Sci. Nutr. 2018, 69, 33–45. [Google Scholar] [CrossRef]
- Agans, R.T.; Giles, G.E.; Goodson, M.S.; Karl, J.P.; Leyh, S.; Mumy, K.L.; Racicot, K.; Soares, J.W. Evaluation of Probiotics for Warfighter Health and Performance. Front. Nutr. 2020, 7. [Google Scholar] [CrossRef]
| Search List 1 | Search List 2 | |
|---|---|---|
| “Lactobacillus” or “Bifidobacterium” or “probiotic” or “prebiotic” or “psycho-biotic” or “microbiota” or “gut-brain-axis” or “gut microbiota” or “commensal bacteria” or “vaccae” or “lactobacilli” or “mycobacteria” or “immunomodulation” or “proinflammatory cytokine” or “gut permeability” or “microbial” or “microbiome” or “neurome” | AND | “cognition” or “cognitive” or “memory” or “vigilance” or “decision making” or “attention” or “visuo-spatial” or “executive function” or “task-switching” or “emotional” or “emotion” or “behaviour” or “behavior” or “recognition” or “resting-state” or “salience” or “anxiety” or “anxious” or “mood” or “moody” or “depression” or “depressive” or “PTSD” or “stroop” or “go-nogo” or “n-back” or “functional state” or “neuroscience” or “psychobiology” |
| Author/Year | Participants/Sample (± SD) | Sex (M/F) | Study Design | Assessment | Main Findings Microbiome Link |
|---|---|---|---|---|---|
| Fernandez-Real et al. (2015) [29] | n = 19 obese; n = 20 non-obese patients; total age range 30–65 years (mean ± SD not specified) | Not known | Correlational (partial blind); microbiome markers of obese vs. non-obese patients | fMRI; Trail making test; 16S rRNA gene sequencing | Specific phyla linked to obesity, brain structures and trail map making |
| Anderson et al. (2017) [30] | n = 37 healthy (50–85 years; 64.6 ± 7.5 years) | 10/27 | Correlational; microbiome, sleep quality and cognition | Stroop Colour-Word (cog flexibility); PSQI (sleep) | Association with sleep quality and cognitive flexibility |
| Taylor et al. (2017) [31]—conf. abstract | n = 34 (25–45 years old); no average +SD given in conference abstract | 0/34 | Correlational: microbiota and cognition | Modified flanker test | Greater numbers of Bacteriodetes = cog. performance maintained with increasing task demand |
| Osadchiy et al. (2018) [12] | n = 63 healthy adults (29.4 ± 10.8 years) | 29/34 | Correlational; microbiome metabolites and links to brain networks, obesity and anxiety | HAD; YFAS; MRI (structural, functional, diffusion); faecal metabolomics | Faecal metabolites linked to brain connectivity, reward networks, and anxiety symptoms |
| Labus et al. (2017) [32] | n = 29 IBS patients (26.1 ± 5.7 years); n = 23 HC (26.0 ± 6.5 years) | 17/35 | Correlational: microbiome markers in IBS and correlates of brain structure | HADs + PHQ-15; ETI-SR; PSS; compact MRI 16S rRNA gene sequencing | Behavioural link to microbiome in IBS: sensory and salience network regions, early-life trauma |
| Author/Year | Participants/Sample (± SD) | Sex (M/F) | Study Design | Treatment | Dose/Frequency | Assessment | Main Findings—Microbiome Link |
|---|---|---|---|---|---|---|---|
| Probiotics | |||||||
| Allen et al. (2016) [22] | n = 22 healthy males (22.5 ± 1.2 SEM y) | 22/0 | Repeated measures, placebo-controlled within-subject (blinding not stated) | Bifidobacterium longum 1714 strain | PRO = 1 × 109 cfu/stick or PLA; 1 stick/day 4 weeks each. PLA→PRO | Cognitive tasks: CANTAB done with EEG | mild improvement vs. PLA in visuospatial memory; EEG profile consistent with improved memory |
| Kelly et al. (2017) [33] | Placebo-Probiotic group n = 15 (23.6 ± 1.0 year); Probiotic-Placebo group n = 14 (25.6 ± 1.1 year) | 29/0 | Randomised Placebo-controlled cross-over design (wash-out and randomisation not detailed) | Lactobacillus rhamnosus (JB-1) | Active treatment contained 1 × 109 cfu/capsule; f = 1 daily 4 wk then cross-over | CANTAB | No improvement in cognitive parameters |
| Lew et al. (2018) [7] | Moderately stressed adults: n = 51/66 PLA (32.1 ± 11.4 year); n = 52/66 probiotic (31.3 ± 10.8 year) | 12/39 12/40 (24/79) | RDBPC | Lactobacillus plantarum P8 (isolated from traditionally fermented sour milk—Mongolia) | 2 g sachet of probiotic P8 or PLA P8 dose: 2 × 1010 cfu/day Daily 12 weeks | CogState Brief Battery | Social emotional speed response and verbal & memory learning improved; Cognitive and memory traits correlated with stress and anxiety. Sex different responses. |
| Tillisch et al. (2013) [8] | Females aged females (22.8 ± 2.7 year); n = 12 in fermented probiotic group, n = 11 in non-fermented control; n = 13 nil intervention | 0/36 | RDBPC (treatment, PLA and nil intervention) | Fermented milk containing Bifidobacterium animalis subsp lactis (strain number I-2494, Streptococcus themophilus and Lactobacillus bulgaricus (Danone Research Facilities) | lactis = 1.25 × 1010, thermophilus + bulgaricus = 1.2 × 109; cfu/cup; f = daily 4 weeks | fMRI | affected activity of brain areas controlling central processing (emotion & sensation) |
| Bagga et al. (2018) [6] | Healthy volunteers: n = 15 no-intervention control (26.9 ± 5.0 year); n = 15 PLA (27.3 ± 5.8 year); n = 15 probiotic (28.3 ± 4.2 year) | 7/8 9/6 7/8 (22/23) | RDBPC (randomisation and blinding not specified) | 9 strains: Lactobacillus casei W56, L. acidophilus W22, L. paracasei W20, Bifidobacterium lactis W51, L. salivarius W24, Lactococcus lactis W19, B. lactis W52, L. plantarum W62 and B. bifidum W23 | 7.5 × 109/3 g dose (see extra table information) vs. PLA or CON; f = daily 4 weeks | PANAS; SCL-90; ADS; LEIDS; fMRI with emotional decision making and recognition tasks | Microbiome composition mirrored self-reported behavioural measures and memory performance; potential link between specific Bacteroides, brain memory and recognition |
| Bagga et al. (2019) [34] - Epub May 2018 | Healthy volunteers: n = 15 no-intervention control (26.9 ± 5.0 year); n = 15 PLA (27.3 ± 5.8 year); n = 15 probiotic (28.3 ± 4.2 year) | 7/8 9/6 7/8 (22/23) | RDBPC (randomisation and blinding not specified) | See Bagga 2018 study | 7.5 × 109/3 g dose vs. PLA or CON; f = daily 4 weeks | fMRI | Changes in functional connectivity (link to depression and stress disorders) vs. PLA and CON |
| Roman et al. (2018) [35] | n = 40 fibromyalgia patients; complete study: probiotic n = 16/20 (55.0 ± 2.1 year); PLA n = 15/20 (50.3 ± 2.0 year) | 1/15 2/13 (3/28) | Pilot RDBPC (blinding not specified) | ERGYPHILUS Plus (Laboratorios NUTERGIA, Spain): Lactobacillus Rhamnosus GG, Lactobacillus Casei, Lactobacillus Acidophilus, Bifidobacterium Bifidus. | 6 × 109/capsule (See Footnote) 2 capsules, twice daily; 8 weeks | Two-choice task and Iowa gambling task (impulsive choice and decision-making); mini mental state examination; urinary cortisol | probiotics improved impulsivity and decision-making in fibromyalgia patients |
| Prebiotics | |||||||
| Schmidt et al. (2015) [23] | n = 15 PLA (23.3 ± 3.9 year); n = 15 FOS (24.5 ± 3.9 year); n = 15 B-GOS (23.3 ± 4.0 year) | 7/8 8/7 7/8 (22/23) | RDBPC | Fructooligosaccharides (FOS) or Bimuno®-galacto-oligosaccharides (B-GOS) | 5.5 g of FOS, B-GOS or PLA; Daily; 3 weeks | Attentional dot-probe task | B-GOS increased attentional vigilance to positive to negative stimuli |
| Smith et al. (2015) [36] | n = 47 (ave 23.0 years, range 19–30 years) | 19/28 | Cross-over (randomisation or blinding not detailed) | Oligofructose-Enriched Inulin or PLA added to de-caffeinated tea or de-caffeinated coffee | Pre-fasted 5 g prebiotic f = once0–4 h (acute effects) | Memory tasks; psychomotor tasks (simple reaction and selective attention tasks); sustained attention | Episodic memory tasks improved Psychomotor performance and selective attention unchanged. |
| Paraprobiotics | |||||||
| Chung et al. (2014) [37] | Healthy adults n = 36/39: n = 10 PLA (64.5 ± 4.8 year); n = 10,500 mg (64.5 ± 2.2 year); n = 71,000 mg (64.43 ± 4.5 year); n = 92,000 mg (66.6 ± 5.0 year) | 4/6 9/1 2/5 5/4 (20/16) | RDBPC (blinding not specified) | Lactobacillus helveticus (IDCC3801) Fermented (heat-treated) milk (LHFM); supernatant extracted and placed in tablet form. | took 4 tablets daily to reach a conc. of 500, 1000, 2000 or 0 mg (PLA) 12 weeks | Digit-span; Story recall; verbal learning; RVIP (cognitive fatigue measure); stroop; serial 3 s and 7 s | minor improvement in RVIP accuracy only for low dose of heat-treated fermented milk tablet |
| Ohsawa et al. (2018) [38] | All with mild memory deficits: n = 31/31 in fermented probiotic milk (58.5 ± 6.5 year); n = 29/30 PLA (57.8 ± 5.9 year) | 13/18 13/16 (26/34) | RDBPC (blinding not specified) | Lactobacillus helveticus-fermented milk containing 2.4 mg lactononadeca-peptide (NIPPLTQTPV VVPPFLQPE). PLA contained no active ingredient | 190 g drink with/without fermented peptide (2.4 mg) One daily 8 weeks | RBANS | Improvement in total RBANs and delayed memory score. Attention and coding score also improved. All other measures NS |
| Synbiotics | |||||||
| Tooley et al. (2018) [39] - Conf abstract (manuscript in preparation) | Healthy young University Students: n = 34 Synbiotic; n = 33 PLA | 16/51 | RDBPC | Lactobacillus acidophilus L10 and Bifidobacterium lactis B94 plus arabinogalactan, inulin and trehalose | 1.5 × 1010 of both bacteria strains cfu/5 g dose f = daily 4 weeks | Cognitive Battery | Synbiotic improved memory: immediate & delayed recall. Vigilance, attention, simple reaction time, executive control NS. |
© 2020 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tooley, K.L. Effects of the Human Gut Microbiota on Cognitive Performance, Brain Structure and Function: A Narrative Review. Nutrients 2020, 12, 3009. https://doi.org/10.3390/nu12103009
Tooley KL. Effects of the Human Gut Microbiota on Cognitive Performance, Brain Structure and Function: A Narrative Review. Nutrients. 2020; 12(10):3009. https://doi.org/10.3390/nu12103009
Chicago/Turabian StyleTooley, Katie Louise. 2020. "Effects of the Human Gut Microbiota on Cognitive Performance, Brain Structure and Function: A Narrative Review" Nutrients 12, no. 10: 3009. https://doi.org/10.3390/nu12103009
APA StyleTooley, K. L. (2020). Effects of the Human Gut Microbiota on Cognitive Performance, Brain Structure and Function: A Narrative Review. Nutrients, 12(10), 3009. https://doi.org/10.3390/nu12103009




