Low-Fat Diet Designed for Weight Loss But Not Weight Maintenance Improves Nitric Oxide-Dependent Arteriolar Vasodilation in Obese Adults
Abstract
1. Introduction
2. Subjects and Methods
2.1. Human Participants
2.2. Study Design
2.3. Subcutaneous Adipose Tissue Biopsy
2.4. Microvascular Preparation
2.5. Flow-Induced Dilation Measurements
2.6. Nitric Oxide Measurements in Isolated Arterioles
2.7. Serum Nitric Oxide and C-Reactive Protein (CRP) Measurements
2.8. Cardio-Metabolic Risk Factor Assessment
2.9. Statistical Analysis
3. Results
3.1. Effect of LFWL and LFWM Diet on Body Composition and Cardiometabolic Risk Factors
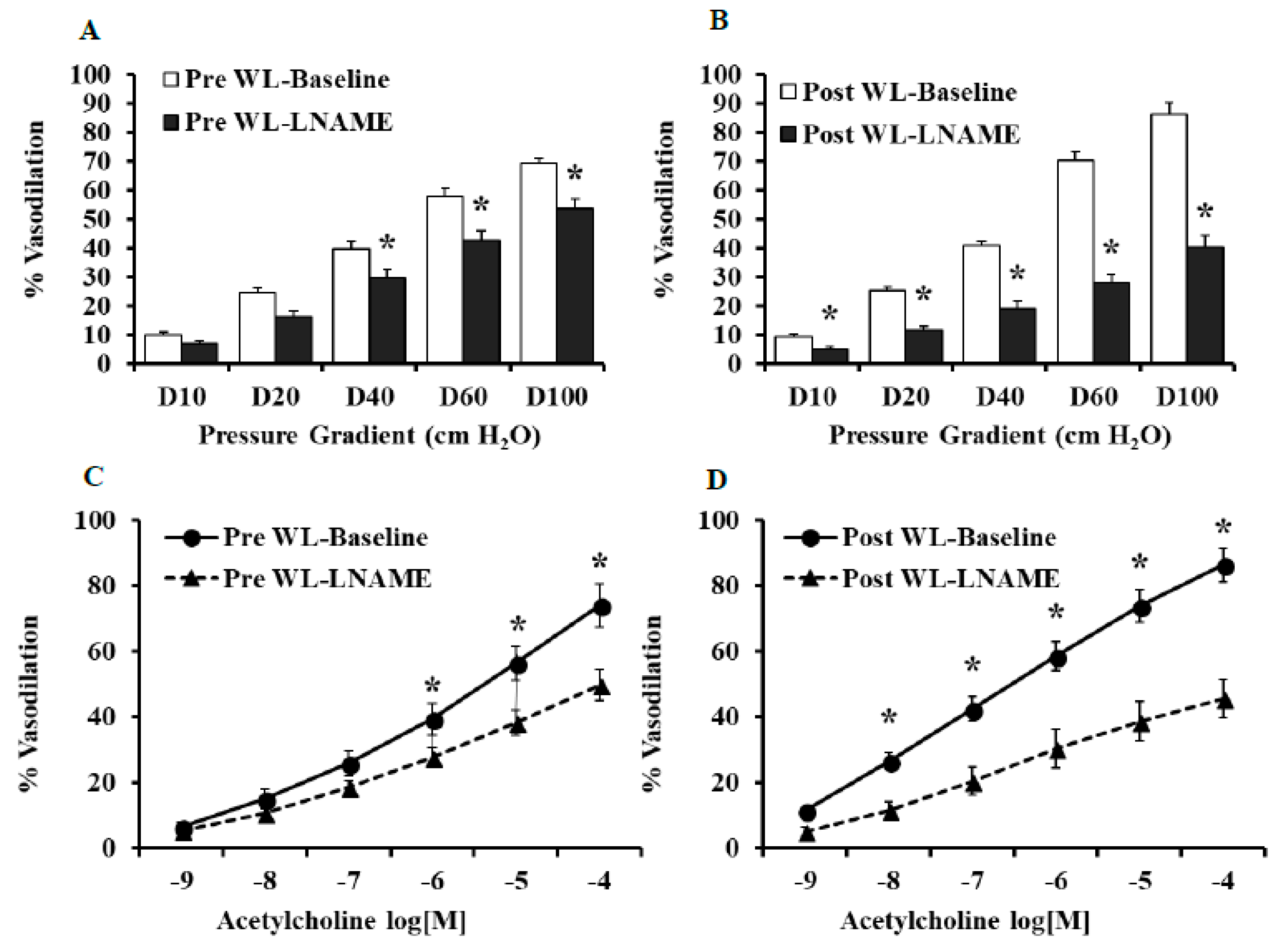
3.2. Effect of LFWL and LFWM Diet on Flow and Ach-Induced Dilation
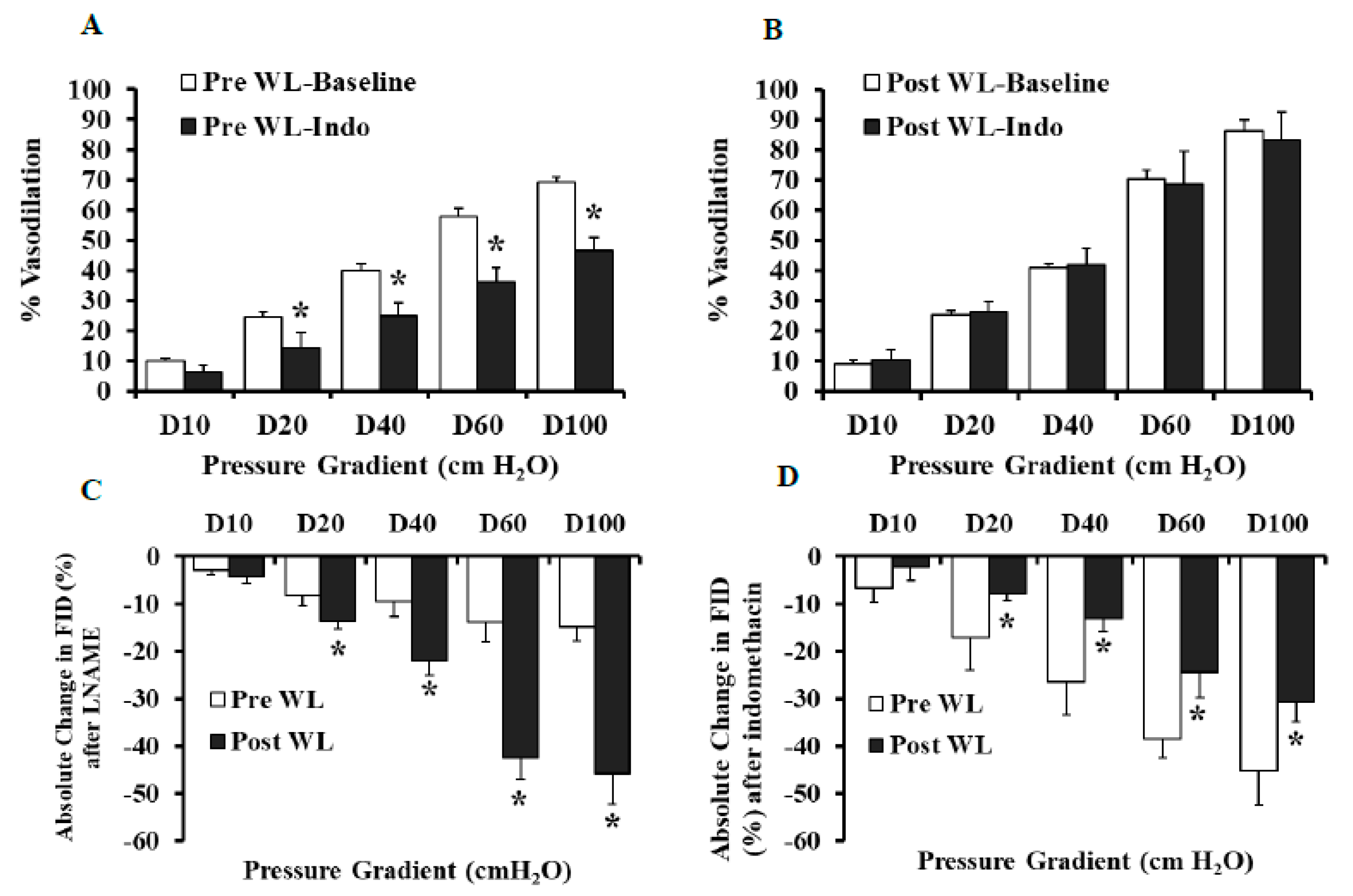
3.3. Effect of LNAME and Indomethacin on Flow and Ach-Induced Dilation in LFWL Group
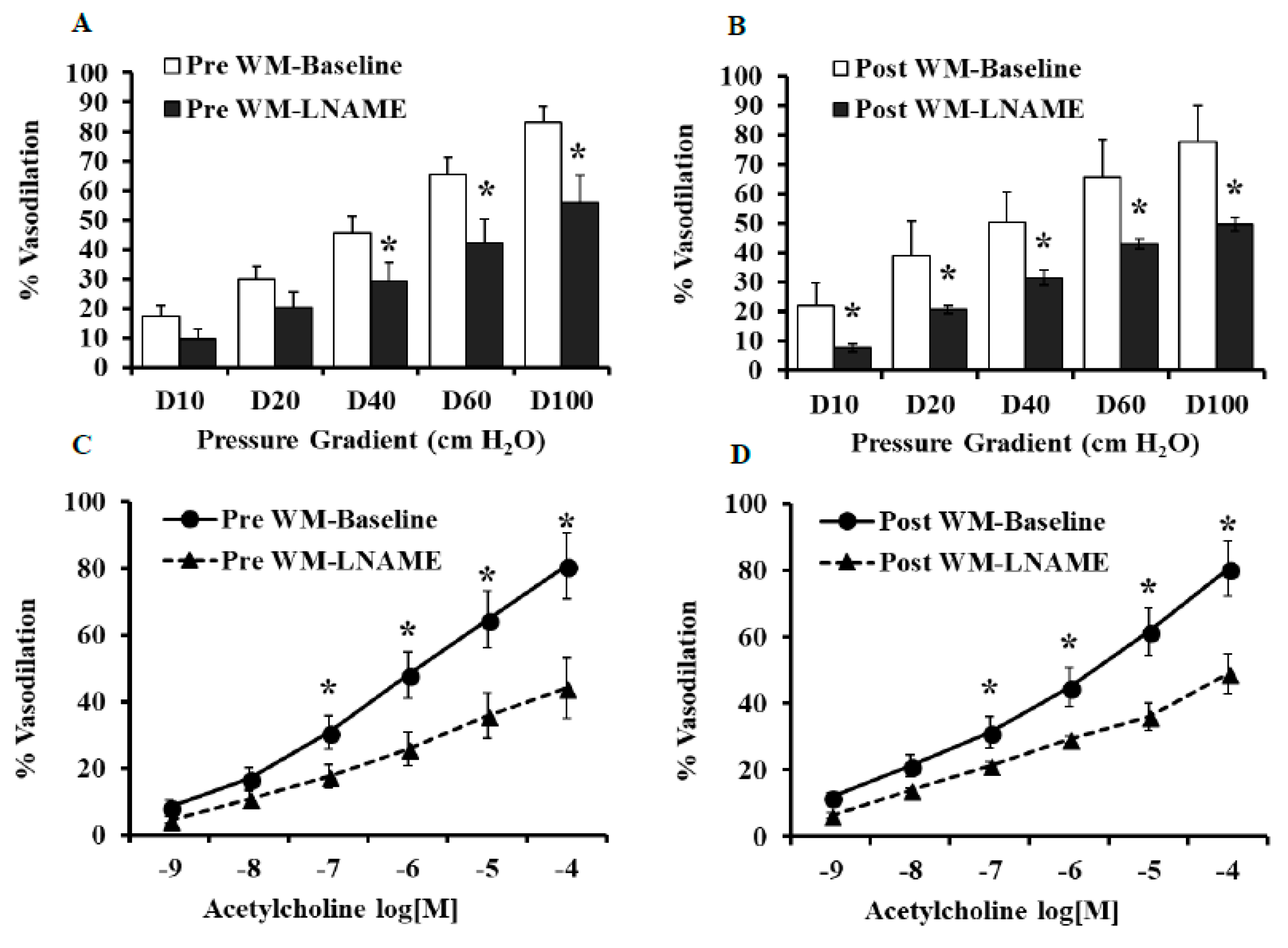
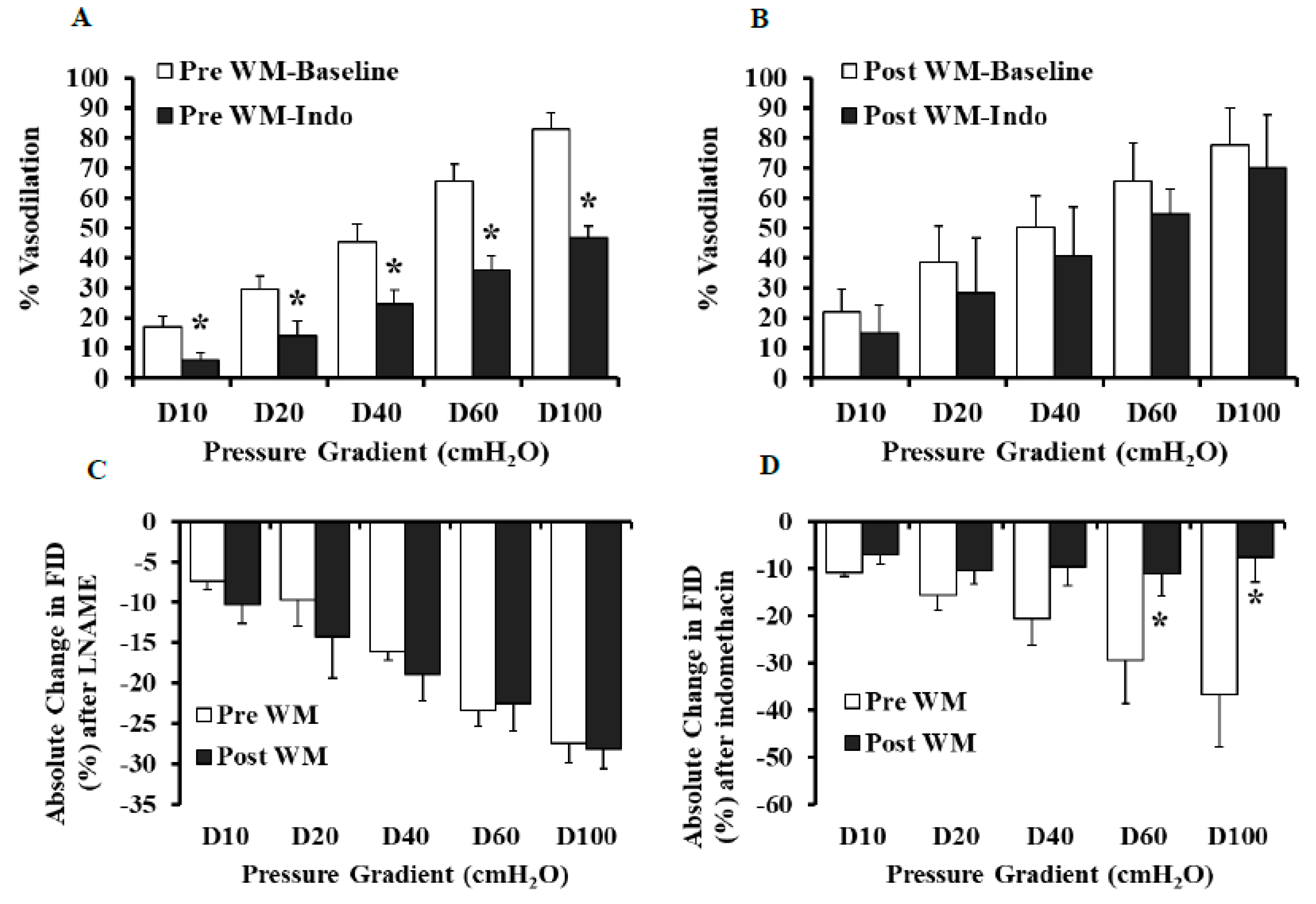
3.4. Effect of L-NAME and Indomethacin on Flow and Ach-Induced Dilation in LFWM Group
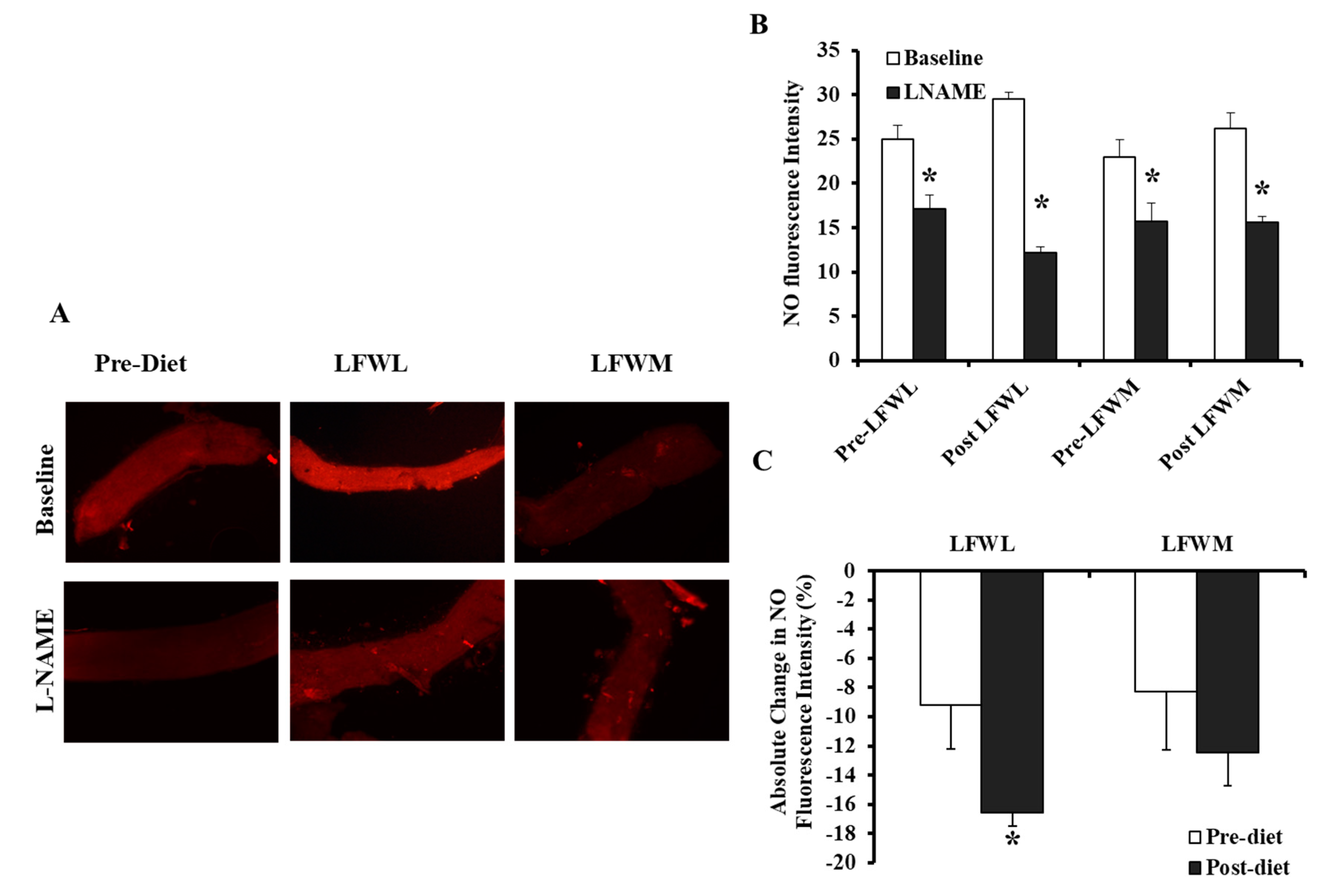
3.5. Flow-Induced NO Fluorescence in LFWL and LFWM Groups
3.6. Effect of LFWL and LFWM Diet on Serum NO and CRP
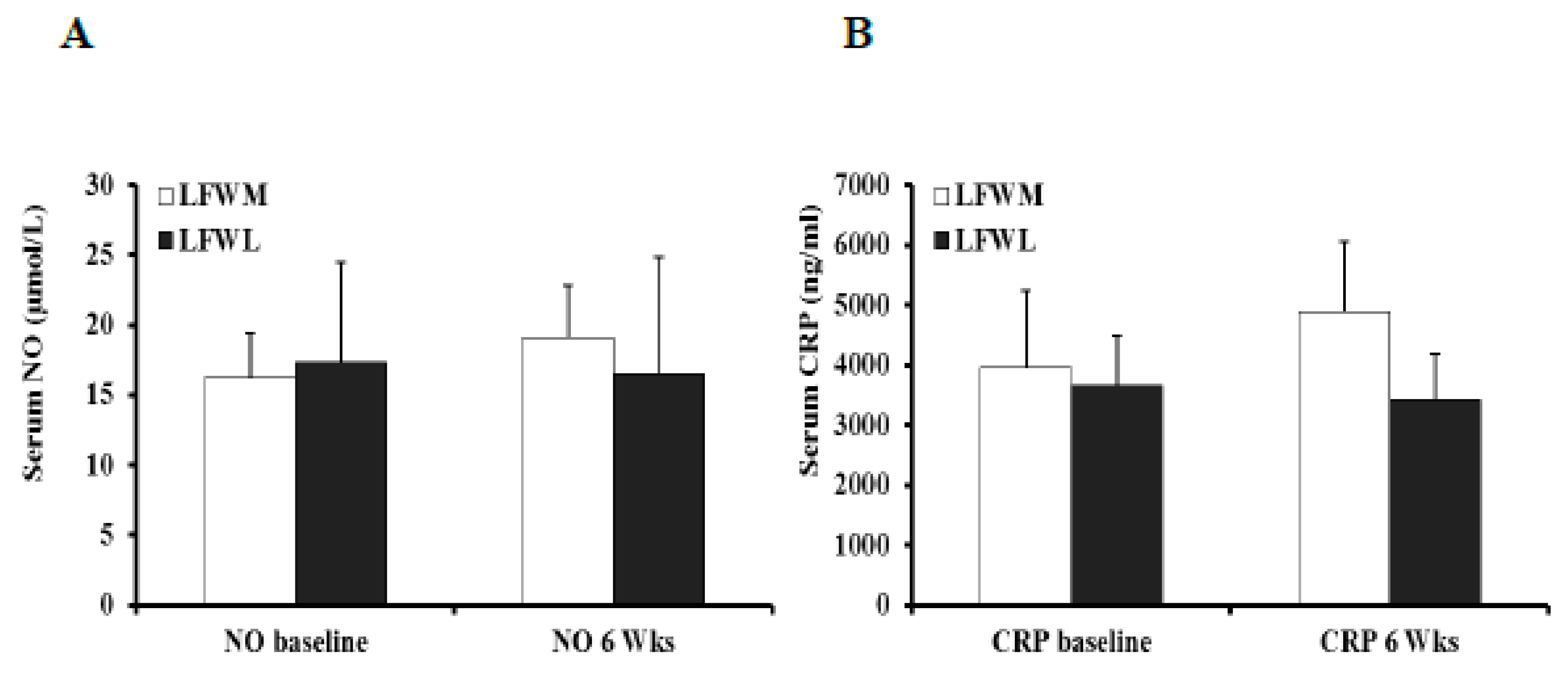
4. Discussion
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Hales, C.M.; Carroll, M.D.; Fryar, C.D.; Ogden, C.L. Prevalence of Obesity among Adults and Youth: United States, 2015–2016; NCHS Data Brief; National Center for Health Statistics: Hyattsville, MD, USA, 2017; pp. 1–8.
- Khaodhiar, L.; McCowen, K.C.; Blackburn, G.L. Obesity and its comorbid conditions. Clin Cornerstone 1999, 2, 17–31. [Google Scholar] [CrossRef]
- Fan, J.; Song, Y.; Chen, Y.; Hui, R.; Zhang, W. Combined effect of obesity and cardio-metabolic abnormality on the risk of cardiovascular disease: A meta-analysis of prospective cohort studies. Int. J. Cardiol. 2013, 168, 4761–4768. [Google Scholar] [CrossRef] [PubMed]
- Serdula, M.K.; Mokdad, A.H.; Williamson, D.F.; Galuska, D.A.; Mendlein, J.M.; Heath, G.W. Prevalence of attempting weight loss and strategies for controlling weight. JAMA 1999, 282, 1353–1358. [Google Scholar] [CrossRef] [PubMed]
- Krauss, R.M.; Eckel, R.H.; Howard, B.; Appel, L.J.; Daniels, S.R.; Deckelbaum, R.J.; Erdman, J.W., Jr.; Kris-Etherton, P.; Goldberg, I.J.; Kotchen, T.A.; et al. AHA Dietary Guidelines: Revision 2000: A statement for healthcare professionals from the Nutrition Committee of the American Heart Association. Circulation 2000, 102, 2284–2299. [Google Scholar] [CrossRef] [PubMed]
- Phillips, S.A.; Jurva, J.W.; Syed, A.Q.; Syed, A.Q.; Kulinski, J.P.; Pleuss, J.; Hoffmann, R.G.; Gutterman, D.D. Benefit of low-fat over low-carbohydrate diet on endothelial health in obesity. Hypertension 2008, 51, 376–382. [Google Scholar] [CrossRef] [PubMed]
- Volek, J.S.; Ballard, K.D.; Silvestre, R.; Judelson, D.A.; Quann, E.E.; Forsythe, C.E.; Fernandez, M.L.; Kraemer, W.J. Effects of dietary carbohydrate restriction versus low-fat diet on flow-mediated dilation. Metabolism 2009, 58, 1769–1777. [Google Scholar] [CrossRef] [PubMed]
- Keogh, J.B.; Brinkworth, G.D.; Clifton, P.M. Effects of weight loss on a low-carbohydrate diet on flow-mediated dilatation, adhesion molecules and adiponectin. Br. J. Nutr. 2007, 98, 852–859. [Google Scholar] [CrossRef]
- Karaca, U.; Schram, M.T.; Houben, A.J.; Muris, D.M.; Stehouwer, C.D. Microvascular dysfunction as a link between obesity, insulin resistance and hypertension. Diabetes Res. Clin. Pr. 2014, 103, 382–387. [Google Scholar] [CrossRef]
- De Boer, M.P.; Meijer, R.I.; Wijnstok, N.J.; Jonk, A.M.; Houben, A.J.; Stehouwer, C.D.; Smulders, Y.M.; Eringa, E.C.; Serne, E.H. Microvascular dysfunction: A potential mechanism in the pathogenesis of obesity-associated insulin resistance and hypertension. Microcirculation 2012, 19, 5–18. [Google Scholar] [CrossRef]
- Granger, D.N.; Rodrigues, S.F.; Yildirim, A.; Senchenkova, E.Y. Microvascular responses to cardiovascular risk factors. Microcirculation 2010, 17, 192–205. [Google Scholar] [CrossRef]
- Cooper, L.L.; Palmisano, J.N.; Benjamin, E.J.; Larson, M.G.; Vasan, R.S.; Mitchell, G.F.; Hamburg, N.M. Microvascular Function Contributes to the Relation Between Aortic Stiffness and Cardiovascular Events: The Framingham Heart Study. Circ. Cardiovasc. Imaging 2016, 9. [Google Scholar] [CrossRef] [PubMed]
- Mahmoud, A.M.; Szczurek, M.R.; Blackburn, B.K.; Mey, J.T.; Chen, Z.; Robinson, A.T.; Bian, J.T.; Unterman, T.G.; Minshall, R.D.; Brown, M.D.; et al. Hyperinsulinemia augments endothelin-1 protein expression and impairs vasodilation of human skeletal muscle arterioles. Physiol. Rep. 2016, 4. [Google Scholar] [CrossRef] [PubMed]
- Robinson, A.T.; Franklin, N.C.; Norkeviciute, E.; Bian, J.T.; Babana, J.C.; Szczurek, M.R.; Phillips, S.A. Improved arterial flow-mediated dilation after exertion involves hydrogen peroxide in overweight and obese adults following aerobic exercise training. J. Hypertens. 2016, 34, 1309–1316. [Google Scholar] [CrossRef] [PubMed]
- Joris, P.J.; Plat, J.; Kusters, Y.H.; Houben, A.J.; Stehouwer, C.D.; Schalkwijk, C.G.; Mensink, R.P. Diet-induced weight loss improves not only cardiometabolic risk markers but also markers of vascular function: A randomized controlled trial in abdominally obese men. Am. J. Clin. Nutr. 2017, 105, 23–31. [Google Scholar] [CrossRef] [PubMed]
- Choo, J.; Lee, J.; Cho, J.H.; Burke, L.E.; Sekikawa, A.; Jae, S.Y. Effects of weight management by exercise modes on markers of subclinical atherosclerosis and cardiometabolic profile among women with abdominal obesity: A randomized controlled trial. BMC Cardiovasc. Disord. 2014, 14, 82. [Google Scholar] [CrossRef] [PubMed]
- Ryan, A.S.; Ge, S.; Blumenthal, J.B.; Serra, M.C.; Prior, S.J.; Goldberg, A.P. Aerobic exercise and weight loss reduce vascular markers of inflammation and improve insulin sensitivity in obese women. J. Am. Geriatr. Soc. 2014, 62, 607–614. [Google Scholar] [CrossRef]
- Weiss, E.P.; Albert, S.G.; Reeds, D.N.; Kress, K.S.; McDaniel, J.L.; Klein, S.; Villareal, D.T. Effects of matched weight loss from calorie restriction, exercise, or both on cardiovascular disease risk factors: A randomized intervention trial. Am. J. Clin. Nutr. 2016, 104, 576–586. [Google Scholar] [CrossRef]
- Clifton, P.M.; Keogh, J.B. Effects of Different Weight Loss Approaches on CVD Risk. Curr. Atheroscler. Rep. 2018, 20, 27. [Google Scholar] [CrossRef]
- Tobias, D.K.; Chen, M.; Manson, J.E.; Ludwig, D.S.; Willett, W.; Hu, F.B. Effect of low-fat diet interventions versus other diet interventions on long-term weight change in adults: A systematic review and meta-analysis. Lancet Diabetes Endocrinol. 2015, 3, 968–979. [Google Scholar] [CrossRef]
- Mansoor, N.; Vinknes, K.J.; Veierod, M.B.; Retterstol, K. Effects of low-carbohydrate diets v. low-fat diets on body weight and cardiovascular risk factors: A meta-analysis of randomised controlled trials. Br. J. Nutr. 2016, 115, 466–479. [Google Scholar] [CrossRef]
- Lu, M.; Wan, Y.; Yang, B.; Huggins, C.E.; Li, D. Effects of low-fat compared with high-fat diet on cardiometabolic indicators in people with overweight and obesity without overt metabolic disturbance: A systematic review and meta-analysis of randomised controlled trials. Br. J. Nutr. 2018, 119, 96–108. [Google Scholar] [CrossRef] [PubMed]
- Kahleova, H.; Dort, S.; Holubkov, R.; Barnard, N.D. A Plant-Based High-Carbohydrate, Low-Fat Diet in Overweight Individuals in a 16-Week Randomized Clinical Trial: The Role of Carbohydrates. Nutrients 2018, 10. [Google Scholar] [CrossRef] [PubMed]
- Mahmoud, A.M.; Brown, M.D.; Phillips, S.A.; Haus, J.M. Skeletal Muscle Vascular Function: A Counterbalance of Insulin Action. Microcirculation 2015, 22, 327–347. [Google Scholar] [CrossRef] [PubMed]
- Catapano, A.L.; Pirillo, A.; Norata, G.D. Vascular inflammation and low-density lipoproteins: Is cholesterol the link? A lesson from the clinical trials. Br. J. Pharm. 2017, 174, 3973–3985. [Google Scholar] [CrossRef] [PubMed]
- Mifflin, M.D.; St Jeor, S.T.; Hill, L.A.; Scott, B.J.; Daugherty, S.A.; Koh, Y.O. A new predictive equation for resting energy expenditure in healthy individuals. Am. J. Clin. Nutr. 1990, 51, 241–247. [Google Scholar] [CrossRef] [PubMed]
- Durand, M.J.; Dharmashankar, K.; Bian, J.T.; Das, E.; Vidovich, M.; Gutterman, D.D.; Phillips, S.A. Acute exertion elicits a H2O2-dependent vasodilator mechanism in the microvasculature of exercise-trained but not sedentary adults. Hypertension 2015, 65, 140–145. [Google Scholar] [CrossRef]
- Phillips, S.A.; Hatoum, O.A.; Gutterman, D.D. The mechanism of flow-induced dilation in human adipose arterioles involves hydrogen peroxide during CAD. Am. J. Physiol. Heart Circ. Physiol. 2007, 292, H93–H100. [Google Scholar] [CrossRef]
- Mahmoud, A.M.; Ali, M.M.; Miranda, E.R.; Mey, J.T.; Blackburn, B.K.; Haus, J.M.; Phillips, S.A. Nox2 contributes to hyperinsulinemia-induced redox imbalance and impaired vascular function. Redox Biol. 2017, 13, 288–300. [Google Scholar] [CrossRef]
- Miura, H.; Wachtel, R.E.; Liu, Y.; Loberiza, F.R., Jr.; Saito, T.; Miura, M.; Gutterman, D.D. Flow-induced dilation of human coronary arterioles: Important role of Ca(2+)-activated K(+) channels. Circulation 2001, 103, 1992–1998. [Google Scholar] [CrossRef]
- Solomon, T.P.; Haus, J.M.; Li, Y.; Kirwan, J.P. Progressive hyperglycemia across the glucose tolerance continuum in older obese adults is related to skeletal muscle capillarization and nitric oxide bioavailability. J. Clin. Endocrinol. Metab. 2011, 96, 1377–1384. [Google Scholar] [CrossRef]
- Whelton, P.K.; Carey, R.M.; Aronow, W.S.; Casey, D.E., Jr.; Collins, K.J.; Dennison Himmelfarb, C.; DePalma, S.M.; Gidding, S.; Jamerson, K.A.; Jones, D.W.; et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension 2018, 71, 1269–1324. [Google Scholar] [CrossRef] [PubMed]
- Lavie, C.J.; De Schutter, A.; Parto, P.; Jahangir, E.; Kokkinos, P.; Ortega, F.B.; Arena, R.; Milani, R.V. Obesity and Prevalence of Cardiovascular Diseases and Prognosis-The Obesity Paradox Updated. Prog. Cardiovasc. Dis. 2016, 58, 537–547. [Google Scholar] [CrossRef] [PubMed]
- Joris, P.J.; Zeegers, M.P.; Mensink, R.P. Weight loss improves fasting flow-mediated vasodilation in adults: A meta-analysis of intervention studies. Atherosclerosis 2015, 239, 21–30. [Google Scholar] [CrossRef] [PubMed]
- Keogh, J.B.; Grieger, J.A.; Noakes, M.; Clifton, P.M. Flow-mediated dilatation is impaired by a high-saturated fat diet but not by a high-carbohydrate diet. Arter. Thromb. Vasc. Biol. 2005, 25, 1274–1279. [Google Scholar] [CrossRef] [PubMed]
- Varady, K.A.; Bhutani, S.; Klempel, M.C.; Phillips, S.A. Improvements in vascular health by a low-fat diet, but not a high-fat diet, are mediated by changes in adipocyte biology. Nutr. J. 2011, 10, 8. [Google Scholar] [CrossRef] [PubMed]
- Gokce, N.; Vita, J.A.; McDonnell, M.; Forse, A.R.; Istfan, N.; Stoeckl, M.; Lipinska, I.; Keaney, J.F., Jr.; Apovian, C.M. Effect of medical and surgical weight loss on endothelial vasomotor function in obese patients. Am. J. Cardiol. 2005, 95, 266–268. [Google Scholar] [CrossRef] [PubMed]
- Charakida, M.; Masi, S.; Luscher, T.F.; Kastelein, J.J.; Deanfield, J.E. Assessment of atherosclerosis: The role of flow-mediated dilatation. Eur. Heart J. 2010, 31, 2854–2861. [Google Scholar] [CrossRef]
- Pasterkamp, G.; de Kleijn, D.P.; Borst, C. Arterial remodeling in atherosclerosis, restenosis and after alteration of blood flow: Potential mechanisms and clinical implications. Cardiovasc. Res. 2000, 45, 843–852. [Google Scholar] [CrossRef]
- Dharmashankar, K.; Welsh, A.; Wang, J.; Kizhakekuttu, T.J.; Ying, R.; Gutterman, D.D.; Widlansky, M.E. Nitric oxide synthase-dependent vasodilation of human subcutaneous arterioles correlates with noninvasive measurements of endothelial function. Am. J. Hypertens. 2012, 25, 528–534. [Google Scholar] [CrossRef]
- Mitchell, J.A.; Ali, F.; Bailey, L.; Moreno, L.; Harrington, L.S. Role of nitric oxide and prostacyclin as vasoactive hormones released by the endothelium. Exp. Physiol. 2008, 93, 141–147. [Google Scholar] [CrossRef]
- Rallidis, L.S.; Lekakis, J.; Kolomvotsou, A.; Zampelas, A.; Vamvakou, G.; Efstathiou, S.; Dimitriadis, G.; Raptis, S.A.; Kremastinos, D.T. Close adherence to a Mediterranean diet improves endothelial function in subjects with abdominal obesity. Am. J. Clin. Nutr. 2009, 90, 263–268. [Google Scholar] [CrossRef] [PubMed]
- Brook, R.D.; Bard, R.L.; Rubenfire, M.; Ridker, P.M.; Rajagopalan, S. Usefulness of visceral obesity (waist/hip ratio) in predicting vascular endothelial function in healthy overweight adults. Am. J. Cardiol. 2001, 88, 1264–1269. [Google Scholar] [CrossRef]
- Sturm, W.; Sandhofer, A.; Engl, J.; Laimer, M.; Molnar, C.; Kaser, S.; Weiss, H.; Tilg, H.; Ebenbichler, C.F.; Patsch, J.R. Influence of visceral obesity and liver fat on vascular structure and function in obese subjects. Obesity 2009, 17, 1783–1788. [Google Scholar] [CrossRef] [PubMed]
- Lu, Q.; Cheng, L.T.; Wang, T.; Wan, J.; Liao, L.L.; Zeng, J.; Qin, C.; Li, K.J. Visceral fat, arterial stiffness, and endothelial function in peritoneal dialysis patients. J. Ren. Nutr. 2008, 18, 495–502. [Google Scholar] [CrossRef] [PubMed]
- Romero-Corral, A.; Sert-Kuniyoshi, F.H.; Sierra-Johnson, J.; Orban, M.; Gami, A.; Davison, D.; Singh, P.; Pusalavidyasagar, S.; Huyber, C.; Votruba, S.; et al. Modest visceral fat gain causes endothelial dysfunction in healthy humans. J. Am. Coll. Cardiol. 2010, 56, 662–666. [Google Scholar] [CrossRef] [PubMed]
- Hashimoto, M.; Akishita, M.; Eto, M.; Kozaki, K.; Ako, J.; Sugimoto, N.; Yoshizumi, M.; Toba, K.; Ouchi, Y. The impairment of flow-mediated vasodilatation in obese men with visceral fat accumulation. Int. J. Obes. Relat. Metab. Disord. 1998, 22, 477–484. [Google Scholar] [CrossRef] [PubMed]
- Muniyappa, R.; Montagnani, M.; Koh, K.K.; Quon, M.J. Cardiovascular actions of insulin. Endocr. Rev. 2007, 28, 463–491. [Google Scholar] [CrossRef] [PubMed]
- Levin, E.R. Endothelins. N. Engl. J. Med. 1995, 333, 356–363. [Google Scholar] [CrossRef]
- Vane, J.R.; Anggard, E.E.; Botting, R.M. Regulatory functions of the vascular endothelium. N. Engl. J. Med. 1990, 323, 27–36. [Google Scholar] [CrossRef]
- Bradley, U.; Spence, M.; Courtney, C.H.; McKinley, M.C.; Ennis, C.N.; McCance, D.R.; McEneny, J.; Bell, P.M.; Young, I.S.; Hunter, S.J. Low-fat versus low-carbohydrate weight reduction diets: Effects on weight loss, insulin resistance, and cardiovascular risk: A randomized control trial. Diabetes 2009, 58, 2741–2748. [Google Scholar] [CrossRef]
- Magkos, F.; Fraterrigo, G.; Yoshino, J.; Luecking, C.; Kirbach, K.; Kelly, S.C.; de Las Fuentes, L.; He, S.; Okunade, A.L.; Patterson, B.W.; et al. Effects of Moderate and Subsequent Progressive Weight Loss on Metabolic Function and Adipose Tissue Biology in Humans with Obesity. Cell Metab. 2016, 23, 591–601. [Google Scholar] [CrossRef] [PubMed]
- Sharifi, A.M.; Mohseni, S.; Nekoparvar, S.; Larijani, B.; Fakhrzadeh, H.; Oryan, S. Effect of caloric restriction on nitric oxide production, ACE activity, and blood pressure regulation in rats. Acta Physiol. Hung. 2008, 95, 55–63. [Google Scholar] [CrossRef] [PubMed]
- Zanetti, M.; Gortan Cappellari, G.; Burekovic, I.; Barazzoni, R.; Stebel, M.; Guarnieri, G. Caloric restriction improves endothelial dysfunction during vascular aging: Effects on nitric oxide synthase isoforms and oxidative stress in rat aorta. Exp. Gerontol. 2010, 45, 848–855. [Google Scholar] [CrossRef] [PubMed]
- Garcia-Prieto, C.F.; Fernandez-Alfonso, M.S. Caloric Restriction as a Strategy to Improve Vascular Dysfunction in Metabolic Disorders. Nutrients 2016, 8. [Google Scholar] [CrossRef] [PubMed]
- Kerr, S.M.; Livingstone, M.B.; McCrorie, T.A.; Wallace, J.M. Endothelial dysfunction associated with obesity and the effect of weight loss interventions. Proc. Nutr. Soc. 2011, 70, 418–425. [Google Scholar] [CrossRef] [PubMed]
- Korybalska, K.; Luczak, J.; Swora-Cwynar, E.; Kanikowska, A.; Czepulis, N.; Kanikowska, D.; Skalisz, H.; Breborowicz, A.; Grzymislawski, M.; Witowski, J. Weight loss-dependent and -independent effects of moderate calorie restriction on endothelial cell markers in obesity. J. Physiol. Pharm. 2017, 68, 597–608. [Google Scholar]
- Trujillo, M.E.; Scherer, P.E. Adipose tissue-derived factors: Impact on health and disease. Endocr. Rev. 2006, 27, 762–778. [Google Scholar] [CrossRef]
- Gomez-Delgado, F.; Garcia-Rios, A.; Alcala-Diaz, J.F.; Rangel-Zuniga, O.; Delgado-Lista, J.; Yubero-Serrano, E.M.; Lopez-Moreno, J.; Tinahones, F.J.; Ordovas, J.M.; Garaulet, M.; et al. Chronic consumption of a low-fat diet improves cardiometabolic risk factors according to the CLOCK gene in patients with coronary heart disease. Mol. Nutr. Food Res. 2015, 59, 2556–2564. [Google Scholar] [CrossRef]
- Hernandez, T.L.; Van Pelt, R.E.; Anderson, M.A.; Reece, M.S.; Reynolds, R.M.; de la Houssaye, B.A.; Heerwagen, M.; Donahoo, W.T.; Daniels, L.J.; Chartier-Logan, C.; et al. Women With Gestational Diabetes Mellitus Randomized to a Higher-Complex Carbohydrate/Low-Fat Diet Manifest Lower Adipose Tissue Insulin Resistance, Inflammation, Glucose, and Free Fatty Acids: A Pilot Study. Diabetes Care 2016, 39, 39–42. [Google Scholar] [CrossRef]
- Davis, N.J.; Crandall, J.P.; Gajavelli, S.; Berman, J.W.; Tomuta, N.; Wylie-Rosett, J.; Katz, S.D. Differential effects of low-carbohydrate and low-fat diets on inflammation and endothelial function in diabetes. J. Diabetes Complicat. 2011, 25, 371–376. [Google Scholar] [CrossRef]
- Davidge, S.T. Prostaglandin H synthase and vascular function. Circ. Res. 2001, 89, 650–660. [Google Scholar] [CrossRef] [PubMed]
- Cavka, A.; Cosic, A.; Jukic, I.; Jelakovic, B.; Lombard, J.H.; Phillips, S.A.; Seric, V.; Mihaljevic, I.; Drenjancevic, I. The role of cyclo-oxygenase-1 in high-salt diet-induced microvascular dysfunction in humans. J. Physiol. 2015, 593, 5313–5324. [Google Scholar] [CrossRef] [PubMed]
- Widlansky, M.E.; Price, D.T.; Gokce, N.; Eberhardt, R.T.; Duffy, S.J.; Holbrook, M.; Maxwell, C.; Palmisano, J.; Keaney, J.F., Jr.; Morrow, J.D.; et al. Short- and long-term COX-2 inhibition reverses endothelial dysfunction in patients with hypertension. Hypertension 2003, 42, 310–315. [Google Scholar] [CrossRef] [PubMed]
- Asztalos, B.; Lefevre, M.; Wong, L.; Foster, T.A.; Tulley, R.; Windhauser, M.; Zhang, W.; Roheim, P.S. Differential response to low-fat diet between low and normal HDL-cholesterol subjects. J. Lipid. Res. 2000, 41, 321–328. [Google Scholar] [PubMed]
- Brinton, E.A.; Eisenberg, S.; Breslow, J.L. A low-fat diet decreases high density lipoprotein (HDL) cholesterol levels by decreasing HDL apolipoprotein transport rates. J. Clin. Investig. 1990, 85, 144–151. [Google Scholar] [CrossRef] [PubMed]
- Hayek, T.; Ito, Y.; Azrolan, N.; Verdery, R.B.; Aalto-Setala, K.; Walsh, A.; Breslow, J.L. Dietary fat increases high density lipoprotein (HDL) levels both by increasing the transport rates and decreasing the fractional catabolic rates of HDL cholesterol ester and apolipoprotein (Apo) A-I. Presentation of a new animal model and mechanistic studies in human Apo A-I transgenic and control mice. J. Clin. Investig. 1993, 91, 1665–1671. [Google Scholar] [CrossRef]
- Richard, C.; Couture, P.; Desroches, S.; Nehme, B.; Bourassa, S.; Droit, A.; Lamarche, B. Effect of an isoenergetic traditional Mediterranean diet on the high-density lipoprotein proteome in men with the metabolic syndrome. J. Nutr. Nutr. 2014, 7, 48–60. [Google Scholar] [CrossRef]
- Richard, C.; Couture, P.; Desroches, S.; Lichtenstein, A.H.; Lamarche, B. Effect of an isoenergetic traditional Mediterranean diet on apolipoprotein A-I kinetic in men with metabolic syndrome. Nutr. J. 2013, 12, 76. [Google Scholar] [CrossRef]
- Panel on Macronutrients; Panel on the Definition of Dietary Fiber; Subcommittee on Upper References Levels of Nutrients; Subcommittee on Interpretation and Uses of Dietary Reference Intakes; Standing Committee on the Scientific Evaluation of Dietary Reference Intakes, Food and Nutrition Board, Institute of Medicine. Dietary Reference Intakes for Energy, Carbohydrate, Fiber, Fat, Fatty Acids, Cholesterol, Protein, and Amino Acids; National Academies Press: Washington, DC, USA, 2005.
- Cao, Y.; Mauger, D.T.; Pelkman, C.L.; Zhao, G.; Townsend, S.M.; Kris-Etherton, P.M. Effects of moderate (MF) versus lower fat (LF) diets on lipids and lipoproteins: A meta-analysis of clinical trials in subjects with and without diabetes. J. Clin. Lipidol. 2009, 3, 19–32. [Google Scholar] [CrossRef]
- Sacks, F.M.; Bray, G.A.; Carey, V.J.; Smith, S.R.; Ryan, D.H.; Anton, S.D.; McManus, K.; Champagne, C.M.; Bishop, L.M.; Laranjo, N.; et al. Comparison of weight-loss diets with different compositions of fat, protein, and carbohydrates. N. Engl. J. Med. 2009, 360, 859–873. [Google Scholar] [CrossRef]
- Nordmann, A.J.; Nordmann, A.; Briel, M.; Keller, U.; Yancy, W.S., Jr.; Brehm, B.J.; Bucher, H.C. Effects of low-carbohydrate vs low-fat diets on weight loss and cardiovascular risk factors: A meta-analysis of randomized controlled trials. Arch. Intern. Med. 2006, 166, 285–293. [Google Scholar] [CrossRef] [PubMed]
- Bonow, R.O.; Eckel, R.H. Diet, obesity, and cardiovascular risk. N. Engl. J. Med. 2003, 348, 2057–2058. [Google Scholar] [CrossRef] [PubMed]


| LFWL-pre (n = 11) | LFWL-post (n = 11) | LFWL (Pre-post) p a | LFWM-pre (n = 10) | LFWM-post (n = 10) | LFWM (Pre-post) p a | Group Effect (LFWL vs. LFWM) p b | |
|---|---|---|---|---|---|---|---|
| Age (year) | 36 ± 8 | 31 ± 6 | |||||
| Body Weight (kg) | 90.7 ± 5.2 | 87.5 ± 5.1 * | (3.0 ± 0.6) 0.000 | 101 ± 3.9 | 101 ± 3.8 | (1.1 ± 0.9) 0.270 | 0.006 |
| BMI (kg/m2) | 32.6 ± 2.5 | 29.3 ± 2.9 * | (1.1 ± 0.3) 0.002 | 35.0 ± 3.9 | 35.2 ± 3.3 | (−0.1 ± 0.6) 0.974 | 0.039 |
| Body fat % | 40.6 ± 1.4 | 39.5 ± 1.0 | (1.9 ± 1.1) 0.105 | 41.9 ± 1.6 | 42.4 ± 1.1 | (0.2 ± 0.4) 0.653 | 0.168 |
| Waist Circum. (cm) | 93.7 ± 2.7 | 90 ± 3.1 * | (3.3 ± 0.6) 0.000 | 107.4 ± 2.4 | 102.6 ± 3.7 | (3.4 ± 2.4) 0.192 | 0.627 |
| Systolic BP (mm Hg) | 112.5 ± 6.8 | 111.7 ± 9.1 | (0.8 ± 3.2) 0.503 | 120 ± 11.7 | 118.1 ± 10.3 | (2.2 ± 4.4) 0.624 | 0.292 |
| Diastolic BP (mm Hg) | 70.3 ± 9.4 | 62.2 ± 8.2 * | (8.1 ± 3.1) 0.027 | 71.4 ± 9.6 | 70.0 ± 8.1 | (1.8 ± 2.6) 0.494 | 0.055 |
| Heart Rate (beats/min) | 68.7 ± 11.3 | 62.9 ± 7.3 | (5.8 ± 3.0) 0.083 | 63.2 ± 9.8 | 63.0 ± 10.0 | (0.3 ± 2.2) 0.890 | 0.436 |
| Total Chol (mg/dL) | 179.0 ± 12.5 | 168 ± 11.1 * | (9.5 ± 5.0) 0.041 | 183 ± 9.5 | 158 ± 8.9 * | (24.6 ± 6.0) 0.003 | 0.080 |
| LDL Chol (mg/dL) | 104 ± 9.7 | 100 ± 9.3 * | (4.1 ± 0.7) 0.048 | 100 ± 7.6 | 89 ± 7.6 * | (13.2 ± 3.5) 0.004 | 0.044 |
| HDL Chol (mg/dL) | 56 ± 5.7 | 48 ± 3.9 * | (8.2 ± 2.7) 0.013 | 59 ± 7.1 | 49 ± 5.1 * | (10.3 ± 2.4) 0.002 | 0.479 |
| Triglycerides (mg/dL) | 95.2 ± 14.8 | 96.7 ± 12.1 | (6.7 ± 8.5) 0.449 | 92.0 ± 8.1 | 92.0 ± 15.2 | (7.6 ± 16.5) 0.659 | 0.870 |
| Glucose (mg/dL) | 93.7 ± 14.0 | 92.5 ± 8.4 | (1.3 ± 2.9) 0.663 | 91.0 ± 12.1 | 87.8 ± 12.1 | (2.4 ± 3.7) 0.534 | 0.442 |
| Insulin (μIU/mL) | 11.6 ± 7.2 | 6.1 ± 6.5 * | (4.8 ± 1.7) 0.017 | 13.8 ± 6.7 | 10.3 ± 7.7 | (2.7 ± 1.3) 0.065 | 0.046 |
| HOMA-IR (AU) | 2.6 ± 0.7 | 1.5 ± 0.4 * | (1.2 ± 0.4) 0.013 | 3.2 ± 1.1 | 2.3 ± 0.5 * | (0.7 ± 0.3) 0.036 | 0.043 |
| LFWL-pre (n = 11) | LFWL-post (n = 11) | LFWL (Pre vs. post) p a | LFWM-pre (n = 10) | LFWM-post (n = 10) | LFWM (Pre vs. post) p a | Group Effect (LFWL vs. LFWM) p b | |
|---|---|---|---|---|---|---|---|
| Baseline FID Δ10 | 9.9 ± 1.0 | 9.1 ± 1.1 | 0.128 | 17.1 ± 3.6 | 22.1 ± 7.6 | 0.272 | 0.163 |
| Baseline FID Δ20 | 24.5 ± 1.7 | 25.4 ± 1.3 | 0.469 | 29.7 ± 4.5 | 38.9 ± 11.9 | 0.226 | 0.088 |
| Baseline FID Δ40 | 39.7 ± 2.4 | 41.0 ± 1.3 | 0.174 | 45.4 ± 5.9 | 50.5 ± 10.3 | 0.332 | 0.151 |
| Baseline FID Δ60 | 57.8 ± 2.8 | 70.2 ± 3.0 * | 0.015 | 65.6 ± 5.7 | 65.7 ± 12.7 | 0.497 | 0.025 |
| Baseline FID Δ100 | 69.3 ± 1.5 | 86.2 ± 3.9 * | 0.002 | 83.2 ± 5.2 | 77.8 ± 12.1 | 0.334 | 0.011 |
| Baseline AchID 10−9 | 6.6 ± 1.4 | 11.4 ± 1.0 * | 0.016 | 8.5 ± 2.1 | 12.0 ± 2.9 | 0.167 | 0.452 |
| Baseline AchID 10−8 | 15.1 ± 2.8 | 26.6 ± 2.6 * | 0.005 | 16.9 ± 3.3 | 21.3 ± 4.6 | 0.221 | 0.092 |
| Baseline AchID 10−7 | 26.0 ± 3.8 | 42.5 ± 3.8 * | 0.004 | 30.7 ± 4.9 | 31.3 ± 6.9 | 0.473 | 0.012 |
| Baseline AchID 10−6 | 39.4 ± 4.9 | 58.6 ± 4.4 * | 0.005 | 48.1 ± 6.9 | 44.9 ± 10.2 | 0.397 | 0.006 |
| Baseline AchID 10−5 | 56.4 ± 5.1 | 73.8 ± 4.9 * | 0.015 | 64.5 ± 8.5 | 61.5 ± 13.4 | 0.422 | 0.027 |
| Baseline AchID 10−4 | 74.1 ± 6.5 | 86.4 ± 5.2 | 0.070 | 80.7 ± 9.9 | 80.3 ± 9.4 | 0.491 | 0.119 |
| LFWL-pre (n = 11) | LFWL-post (n = 11) | LFWL (Pre vs. post) p a | LFWM-pre (n = 10) | LFWM-post (n = 10) | LFWM (Pre vs. post) p a | Group Effect (LFWL vs. LFWM) p b | |
|---|---|---|---|---|---|---|---|
| LNAME FIDΔ10 | −2.9 ± 1.0 | −4.3 ± 1.4 | 0.107 | −7.4 ± 1.0 | −10.3 ± 2.4 | 0.261 | 0.463 |
| LNAME FIDΔ20 | −8.4 ± 2.2 | −13.7 ± 1.6 * | 0.042 | −9.6 ± 3.3 | −14.3 ± 5.1 | 0.149 | 0.301 |
| LNAME FIDΔ40 | −9.6 ± 3.2 | −22.2 ± 2.9 * | 0.021 | −16.1 ± 1.1 | −19 ± 3.2 | 0.105 | 0.051 |
| LNAME FIDΔ60 | −14 ± 4.1 | −42.5 ± 4.6 * | 0.005 | −23.3 ± 2.1 | −22.6 ± 3.3 | 0.099 | 0.002 |
| LNAME FIDΔ100 | −14.8 ± 3.0 | −46 ± 6.3 * | 0.003 | −27.4 ± 2.5 | −28.1 ± 2.4 | 0.087 | 0.000 |
| Indo FIDΔ10 | −6.7 ± 3.1 | −2.4 ±2.8 | 0.052 | −11 ± 0.7 | −7.1 ± 2.0 | 0.055 | 0.232 |
| Indo FIDΔ20 | −17 ± 7.0 | −7.9 ± 1.4 * | 0.046 | −15.6 ± 3.3 | −10.5 ± 2.8 | 0.084 | 0.103 |
| Indo FIDΔ40 | −26.5 ± 6.9 | −13.1 ± 2.9 * | 0.040 | −20.7 ± 5.6 | −9.6 ± 4.1 | 0.050 | 0.221 |
| Indo FIDΔ60 | −38.6 ± 3.9 | −24.5 ± 5.5 * | 0.017 | −29.5 ± 9.2 | −11 ± 4.8 * | 0.030 | 0.069 |
| Indo FIDΔ100 | −45.2 ± 7.3 | −30.7 ± 4.1 * | 0.025 | −36.6 ± 11.2 | −7.8 ± 5.1 * | 0.007 | 0.012 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mahmoud, A.M.; Hwang, C.-L.; Szczurek, M.R.; Bian, J.-T.; Ranieri, C.; Gutterman, D.D.; Phillips, S.A. Low-Fat Diet Designed for Weight Loss But Not Weight Maintenance Improves Nitric Oxide-Dependent Arteriolar Vasodilation in Obese Adults. Nutrients 2019, 11, 1339. https://doi.org/10.3390/nu11061339
Mahmoud AM, Hwang C-L, Szczurek MR, Bian J-T, Ranieri C, Gutterman DD, Phillips SA. Low-Fat Diet Designed for Weight Loss But Not Weight Maintenance Improves Nitric Oxide-Dependent Arteriolar Vasodilation in Obese Adults. Nutrients. 2019; 11(6):1339. https://doi.org/10.3390/nu11061339
Chicago/Turabian StyleMahmoud, Abeer M., Chueh-Lung Hwang, Mary R. Szczurek, Jing-Tan Bian, Christine Ranieri, David D. Gutterman, and Shane A. Phillips. 2019. "Low-Fat Diet Designed for Weight Loss But Not Weight Maintenance Improves Nitric Oxide-Dependent Arteriolar Vasodilation in Obese Adults" Nutrients 11, no. 6: 1339. https://doi.org/10.3390/nu11061339
APA StyleMahmoud, A. M., Hwang, C.-L., Szczurek, M. R., Bian, J.-T., Ranieri, C., Gutterman, D. D., & Phillips, S. A. (2019). Low-Fat Diet Designed for Weight Loss But Not Weight Maintenance Improves Nitric Oxide-Dependent Arteriolar Vasodilation in Obese Adults. Nutrients, 11(6), 1339. https://doi.org/10.3390/nu11061339






