Milk Therapy: Unexpected Uses for Human Breast Milk
Abstract
1. Introduction
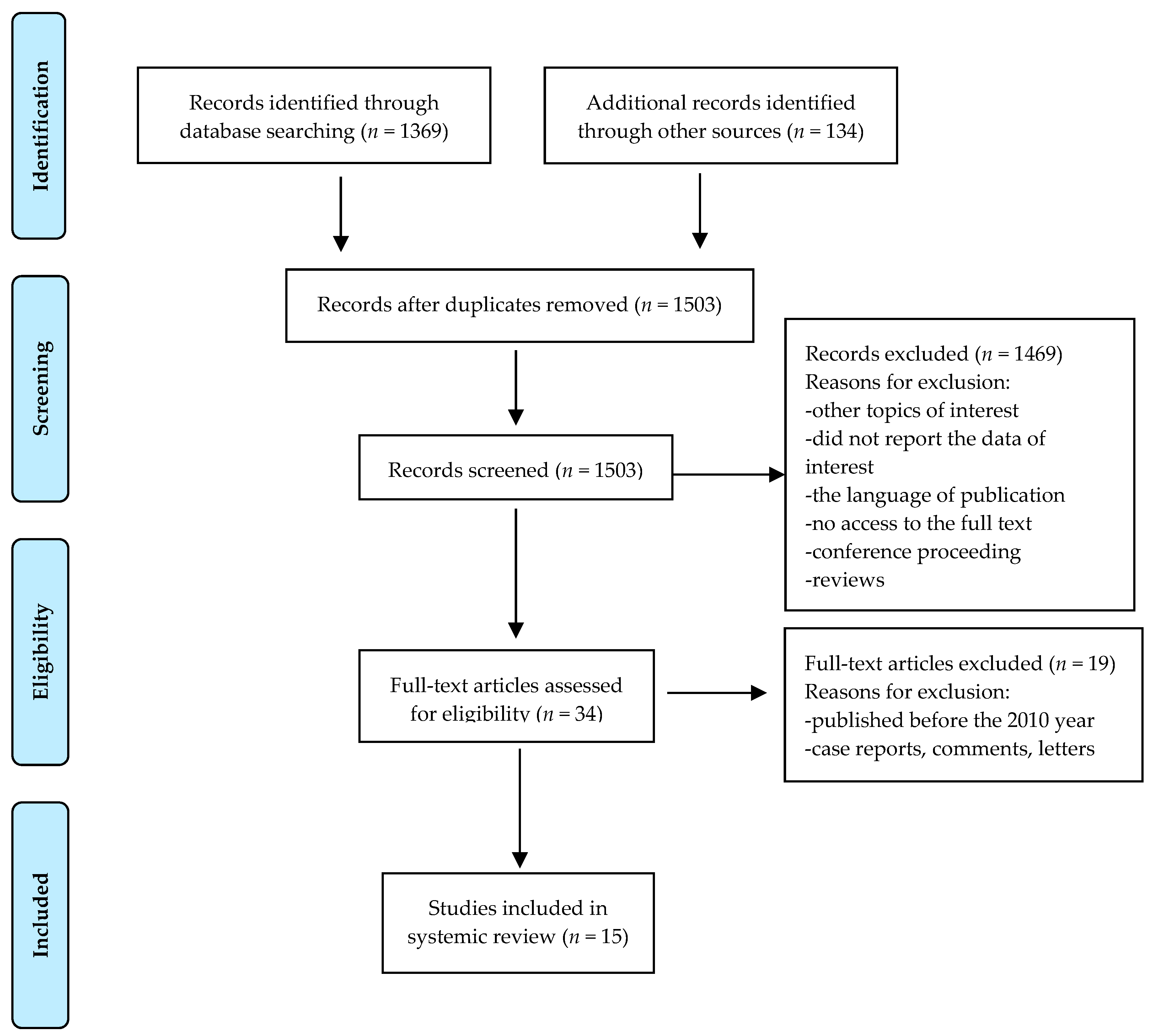
2. Methods
3. Results
3.1. Skin Problems: Atopic Eczema and Diaper Dermatitis
3.2. Nipple Problems
3.3. Eye Problems
3.4. Umbilical Cord Care
3.5. The Antitumoricidal Effect of HAMLET
4. Discussion
4.1. Implications for Future Research
4.2. Limitations
4.3. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Kramer, M.S. “Breast is best”: The evidence. Early Hum. Dev. 2010, 86, 729–732. [Google Scholar] [CrossRef] [PubMed]
- Allam, N.; Megrin, W.; Talat, A. The effect of topical application of mother milk on separation of umbilical cord for newborn babies. Am. J. Nurs. Sci. 2015, 4, 288–296. [Google Scholar] [CrossRef]
- Mahrous, E.S.; Darwish, M.M.; Dabash, S.A.; Marie, I.; Abdelwahab, S.F. Topical application of human milk reduces umbilical cord separation time and bacterial colonization compared to ethanol in newborns. Transl. Biomed. 2012, 3, 4. [Google Scholar]
- Arroyo, R.; Martín, V.; Maldonado, A.; Jiménez, E.; Fernández, L.; Rodríguez, J.M. Treatment of infectious mastitis during lactation: Antibiotics versus oral administration of Lactobacilli isolated from breast milk. Clin. Infect. Dis. 2010, 50, 1551–1558. [Google Scholar] [CrossRef]
- Berents, T.L.; Rønnevig, J.; Søyland, E.; Gaustad, P.; Nylander, G.; Løland, B.F. Topical treatment with fresh human milk versus emollient on atopic eczema spots in young children: A small, randomized, split body, controlled, blinded pilot study. BMC Dermatol. 2015, 15, 7. [Google Scholar] [CrossRef] [PubMed]
- Kasrae, H.; AmiriFarahani, L.; Yousefi, P. Efficacy of topical application of human breast milk on atopic eczema healing among infants: A randomized clinical trial. Int. J. Dermatol. 2015, 54, 966–971. [Google Scholar] [CrossRef]
- Farahani, L.A.; Ghobadzadeh, M.; Yousefi, P. Comparison of the effect of human milk and topical hydrocortisone 1% on diaper dermatitis. Pediatr. Dermatol. 2013, 30, 725–729. [Google Scholar] [CrossRef]
- Gozen, D.; Caglar, S.; Bayraktar, S.; Atici, F. Diaper dermatitis care of newborns human breast milk or barrier cream. J. Clin. Nurs. 2014, 23, 515–523. [Google Scholar] [CrossRef]
- Seifi, B.; Jalali, S.; Heidari, M. Assessment Effect of Breast Milk on Diaper Dermatitis. Dermatol. Rep. 2017, 9, 7044. [Google Scholar] [CrossRef]
- Abou-Dakn, M.; Fluhr, J.W.; Gensch, M.; Wöckel, A. Positive effect of HPA lanolin versus expressed breastmilk on painful and damaged nipples during lactation. Skin Pharmacol. Physiol. 2011, 24, 27–35. [Google Scholar] [CrossRef]
- Golshan, M.; Hossein, N. Impact of ethanol, dry care and human milk on the time for umbilical cord separation. J. Pak. Med. Assoc. 2013, 63, 1117–1119. [Google Scholar] [PubMed]
- Aghamohammadi, A.; Zafari, M.; Moslemi, L. Comparing the effect of topical application of human milk and dry cord care on umbilical cord separation time in healthy newborn infants. Iran J. Pediatr. 2012, 22, 158–162. [Google Scholar] [PubMed]
- Abbaszadeh, F.; Hajizadeh, Z.; Jahangiri, M. Comparing the Impact of Topical Application of Human Milk and Chlorhexidine on Cord Separation Time in Newborns. Pak. J. Med. Sci. 2016, 32, 239–243. [Google Scholar] [CrossRef] [PubMed]
- Ghaemi, S.; Navaei, P.; Rahimirad, S.; Behjati, M.; Kelishadi, R. Evaluation of preventive effects of colostrum against neonatal conjunctivitis: A randomized clinical trial. J. Educ. Health Promot. 2014, 3, 63. [Google Scholar] [CrossRef]
- Asena, L.; Suveren, E.H.; Karabay, G.; Dursun-Altinors, D. Human Breast Milk Drops Promote Corneal Epithelial Wound Healing. Curr. Eye Res. 2017, 42, 506–512. [Google Scholar] [CrossRef] [PubMed]
- Baynham, J.T.; Moorman, M.A.; Donnellan, C.; Cevallos, V.; Keenan, J.D. Antibacterial effect of human milk for common causes of paediatric conjunctivitis. Br. J. Ophthalmol. 2013, 97, 377–379. [Google Scholar] [CrossRef] [PubMed]
- Diego, J.L.; Bidikov, L.; Pedler, M.G.; Kennedy, J.B.; Quiroz-Mercado, H.; Gregory, D.G.; Petrash, J.M.; McCourt, E.A. Effect of human milk as a treatment for dry eye syndrome in a mouse model. Mol. Vis. 2016, 22, 1095–1102. [Google Scholar] [PubMed]
- Mossberg, A.K.; Hou, Y.; Svensson, M.; Holmqvist, B.; Svanborg, C. HAMLET treatment delays bladder cancer development. J. Urol. 2010, 183, 1590–1597. [Google Scholar] [CrossRef] [PubMed]
- Puthia, M.; Storm, P.; Nadeem, A.; Hsiung, S.; Svanborg, C. Prevention and treatment of colon cancer by peroral administration of HAMLET (human α-lactalbumin made lethal to tumour cells). Gut 2014, 63, 131–142. [Google Scholar] [CrossRef] [PubMed]
- Chaumeil, C.; Liotet, S.; Kogbe, O. Treatment of severe eye dryness and problematic eye lesions with enriched bovine colostrum lactoserum. Adv. Exp. Med. Biol. 1994, 350, 595–599. [Google Scholar]
- Mohammadzadeh, A.; Farhat, A.; Esmaeily, H. The effect of breast milk and lanolin on sore nipples. Saudi Med. J. 2005, 26, 1231–1234. [Google Scholar] [PubMed]
- Pugh, L.C.; Buchko, B.L.; Bishop, B.A.; Cochran, J.F.; Smith, L.R.; Lerew, D.J. A comparison of topical agents to relieve nipple pain and enhance breastfeeding. Birth 1996, 23, 88–93. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Care of the Umbilical Cord: A Review of the Evidence; WHO: Geneva, Switzerland, 1998; p. 19. [Google Scholar]
- Karumbi, J.; Mulaku, M.; Aluvaala, J.; English, M.; Opiyo, N. Topical umbilical cord care for prevention of infection and neonatal mortality. Pediatr. Infect. Dis. J. 2013, 32, 78–83. [Google Scholar] [CrossRef]
- Håkansson, A.; Zhivotovsky, B.; Orrenius, S.; Sabharwal, H.; Svanborg, C. Apoptosisinduced by a human milkprotein. Proc. Natl. Acad. Sci. USA. 1995, 92, 8064–8068. [Google Scholar] [CrossRef] [PubMed]
- Trulsson, M.; Yu, H.; Gisselsson, L.; Chao, Y.; Urbano, A.; Aits, S.; Mossberg, A.K.; Svanborg, C. HAMLET Binding to α-Actinin Facilitates Tumor Cell Detachment. PLoS ONE 2011, 6, e17179. [Google Scholar] [CrossRef] [PubMed]
- Ho, J.C.S.; Nadeem, A.; Svanborg, C. HAMLET—A protein-lipid complex with broad tumoricidal activity. Biochem. Biophys. Res. Commun. 2017, 482, 454–458. [Google Scholar] [CrossRef]
- Rath, A.E.; Duff, A.P.; Håkansson, A.P.; Vacher, C.S.; Li, G.J.; Knott, R.B.; Church, W.B. Structure and potential cellular targets of HAMLET-like anti-cancer compounds made from milk components. J. Pharm. Pharm. Sci. 2015, 18, 773–824. [Google Scholar] [CrossRef]
- Hakansson, A.P.; Roche-Hakansson, H.; Mossberg, A.K.; Svanborg, C. Apoptosis-like death in bacteria induced by HAMLET, a human milk lipid-protein complex. PLoS ONE 2011, 6, e17717. [Google Scholar] [CrossRef]
- Hassiotou, F.; Geddes, D.T. Immune cell-mediated protection of the mammary gland and the infant during breastfeeding. Adv. Nutr. 2015, 6, 267–275. [Google Scholar] [CrossRef]
- McGuire, M.K.; McGuire, M.A. Human milk: Mother nature’s prototypical probiotic food. Adv. Nutr. 2015, 6, 112–123. [Google Scholar] [CrossRef]
- Witkowska-Zimny, M.; Kaminska-El-Hassan, E. Cells of human breast milk. Cell Mol. Biol. Lett. 2017, 22, 11. [Google Scholar] [CrossRef] [PubMed]
- Gustafsson, L.; Leijonhufvud, I.; Aronsson, A.; Mossberg, A.K.; Svanborg, C. Treatment of skin papillomas with topical alpha-lactalbumin-oleic acid. N. Engl. J. Med. 2004, 350, 2663–2672. [Google Scholar] [CrossRef] [PubMed]
- Heikkila, M.P.; Saris, P.E. Inhibition of Staphylococcus aureus by the commensal bacteria of human milk. J. Appl. Microbiol. 2003, 95, 471–478. [Google Scholar] [CrossRef]
- Simpson, M.R.; Brede, G.; Johansen, J.; Johnsen, R.; Storrø, O.; Sætrom, P.; Øien, T. Human Breast MilkmiRNA, Maternal Probiotic Supplementation and Atopic Dermatitis in Offspring. PLoS ONE 2015, 10, e0143496. [Google Scholar] [CrossRef] [PubMed]
| References | Intervention/Study Type | Sample Size | The Dropout Rate | Study Design | Outcomes | Main Findings |
|---|---|---|---|---|---|---|
| Berents et al. (2015) [5] | Atopic eczema/Randomized clinical trial | 18 participants | 33% | HBM or emollient was applied on the spot, three times a day for four weeks. The severity and area of the eczema spots was calculated weekly by SCORAD. | Both control and intervention areas of the eczema spots were increased during the intervention. At inclusion mean SCORAD (SCORing Atopic Dermatitis) was 35 and at the end of study 34. | No effect with topical application of HBM was found. |
| Kasrae et al. (2015) [6] | Atopic eczema/Randomized clinical trial | 116 participants | 10% | HBM or hydrocortisone 1% was applied twice a day for 21 days on the affected area. Efficiency of the treatment was defined by SCORAD index. | The frequency of healed infants was 81.5% and 76% in HBM and 1% hydrocortisone groups on day 21, respectively (p < 0.24). | HBM was as effective as 1% hydrocortisone. |
| Farahani et al. (2013) [7] | Diaper dermatitis/Randomized clinical trial | 152 participants | 4.6% | HBM or hydrocortisone 1% was applied for 7 days on the affected area. The efficiency of the treatment was evaluated at 3 and 7 days by a 6-point scale. | The severity score was not different between the topical HBM and hydrocortisone 1% groups at 3 and 7 days (p < 0.95). | HBM was as effective as 1% hydrocortisone. |
| Gozen et al. (2014) [8] | Diaper dermatitis/Randomized clinical trial | 70 participants | 10% | HBM and barrier cream containing 40% zinc oxide and cod liver oil was applied on diaper dermatitis change for 5 days and the postlesion score was establish by a 4-point scale. | The condition of dermatitis was improved in 60% of infant from HBM group and 93.6% treated with barrier cream. The postlesion score of barrier cream group was lower than HBM group (p = 0.002). | Barrier cream was more effective than HBM. |
| Seifi et al. (2017) [9] | Diaper dermatitis/Randomized clinical trial | 30 participants | 0 | Infants suffering from diaper dermatitis assigned to HBM group and the control group were followed up for 5 days and the efficiency of the treatment was evaluated by a 5-point scale rash severity. | In the control group 26.1% infants showed improvement, in HBM group—80%. HBM has decreased the incidence of anal dermatitis rash (p = 0.009). | A positive effect with topical application of HBM was found. |
| Abou-Dakn et al. (2011) [10] | Painful and damaged nipples/No full randomized clinical trial | 84 participants | 14% | The efficacy of HBM and lanolin on pain and damage nipples was assessed on the 10-range Visual Analog Scale (VAS) and the Nipple Trauma Score (NTS) over 14 days after delivery. | Lanolin was more effective than HBM, including faster healing of nipple trauma and reducing nipple pain (p = 0.043). | No positive effect with topical application of HBM was found. |
| Golshan and Hossein (2013) [11] | Umbilical cord care/Randomized clinical trial | 316 participants | 5% | The neonates were divided into three groups: Topical ethanol or HBM application twice a day, the control group kept the stump dry. Umbilical separation time and local infection frequency were considered. | Umbilical separation time in human milk group was significantly shorter (6.5 days) than in ethanol (8.94 days) (p < 0.0001) and drying groups (7.54 days) (p < 0.003). | A positive effect with topical application of HBM was found. |
| Aghamohammadi et al. (2012) [12] | Umbilical cord care/Randomized clinical trial | 152 participants | 14.5% | The umbilical separation time was compared in the group of topical HBM application (three times a day) and dry cord care for 10 days. | Median time of cord separation in human milk application group (150.95 ± 28.68 h) was significantly shorter than dry cord care group (180.93 ± 37.42 h) (p < 0.001). | A positive effect with topical application of HBM was found. |
| Abbaszadeh et al. (2016) [13] | Umbilical cord care/Randomized clinical trial | 174 participants | 6.9% | The infant from HBM group received topical application of milk and group 2 chlorhexidine solution 4% to the umbilical stump 2 times a day. Follow-up and visit at home were done. | The mean cordseparation time in the human milk group (7.14 ± 2.15 days) was shorter than the chlorhexidine group (13.28 ± 6.79 days) (p < 0.001). | A positive effect with topical application of HBM was found. |
| Ghaemi et al. (2014) [14] | Neonatal conjunctivitis/Randomized clinical trial | 300 preterm neonates | 10.6% | The intervention group with culture-negative eye swab received two drops of HBM in each eye or erythromycin ointment (0.5%), control group—no treatment. All neonates were followed for the occurrence of clinical conjunctivitis for 28 days. | The beneficial preventive effects of colostrum against neonatal conjunctivitis (p = 0.036). | A positive effect with application of HBM was found. |
| Asena et al. (2017) [15] | Corneal epithelial wound/Randomized trial on mice model | 24 female experimental corneal epithelial defect mice model | 0 | A central corneal epithelial defect was created in mice and HBM, autologous serum, artificial tears four times a day was applied for 3 days. Histopathological and electron microscopy examination was performed. | Topical human breast milk drops causedfaster and better healing of central corneal epithelial defect than serum drops, artificial tears and in the control group (p < 0.001). | A positive effect with application of HBM was found. |
| Beynham et al. (2013) [16] | Antimicrobial effect on pediatric conjunctivitis/in vitro study | milk from 23 women/9 bacterial species tested | not applicable | The inhibitory effects of HBM against three common ocular pathogens were assessed. Zones of inhibition by milk samples, sterile saline, and trimethoprim ophthalmic solution were measured | Growth of N gonorrhoeae, M catarrhalis, M viridans was significantly inhibited (p ≤ 0.01) by human milk samples. | A positive effect with application of HBM was found. |
| Diego et al. (2016) [17] | Dry eye syndrome/Animal in vivo study | 91 BALB/c mice | 0 | The animals with dry eye syndrome were treated with HBM, nopal, nopal extract derivatives, or cyclosporine four times daily for 7 days. Punctate staining and preservation of corneal epithelial thickness were used as indices of therapeutic efficacy. | Reduction in corneal epithelial thickness was largely prevented by administration of HBM (33.2 ± 2.5 μm). | HBM decreased epithelial damage. |
| Mossberg et al. (2010) [18] | Bladder cancer treatment/animal model and in vitro studies | 6 C57BL mice bladder cancer model | 0 | Bladder tumors cells and bladder mice cancel models were instilled by HAMLET. Effects of HAMLET on tumor size and apoptosis were analyzed. | HAMLET caused a dose dependent decrease in MB49 cell viability in vitro. Five intravesical HAMLET instillations significantly decreased tumor size anddelayed development in vivo compared to controls. | HAMLET from HBM delays bladder cancer development. |
| Puthia et al. (2014) [19] | Colon cancer prevention and treatment/animal model and in vitro studies | ApcMin/+ mice colorectal tumors model | 0 | HAMLET was given in therapeutic and prophylactic regimens. Tumor burden and animal survival were compared, and biochemistry and molecular methods were used to determine effects on colon cancer cells. | Peroral HAMLET administration reduced tumor progression and mortality in ApcMin/+ mice. | HAMLET from HBM delays colon cancer development. |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Witkowska-Zimny, M.; Kamińska-El-Hassan, E.; Wróbel, E. Milk Therapy: Unexpected Uses for Human Breast Milk. Nutrients 2019, 11, 944. https://doi.org/10.3390/nu11050944
Witkowska-Zimny M, Kamińska-El-Hassan E, Wróbel E. Milk Therapy: Unexpected Uses for Human Breast Milk. Nutrients. 2019; 11(5):944. https://doi.org/10.3390/nu11050944
Chicago/Turabian StyleWitkowska-Zimny, Malgorzata, Ewa Kamińska-El-Hassan, and Edyta Wróbel. 2019. "Milk Therapy: Unexpected Uses for Human Breast Milk" Nutrients 11, no. 5: 944. https://doi.org/10.3390/nu11050944
APA StyleWitkowska-Zimny, M., Kamińska-El-Hassan, E., & Wróbel, E. (2019). Milk Therapy: Unexpected Uses for Human Breast Milk. Nutrients, 11(5), 944. https://doi.org/10.3390/nu11050944






