Investigating Risk of Suboptimal Macro and Micronutrient Intake and Their Determinants in Older Danish Adults with Specific Focus on Protein Intake—A Cross-Sectional Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Population
2.2. Ethical Approval and Consent to Participate
2.3. Dietary Assessment
2.4. Under-Reporters
2.5. Qualitative Questionnaire
2.6. Analyses and Statistical Methods
3. Results
3.1. Participant Characteristics
3.2. Intake of Macronutrients and Alcohol
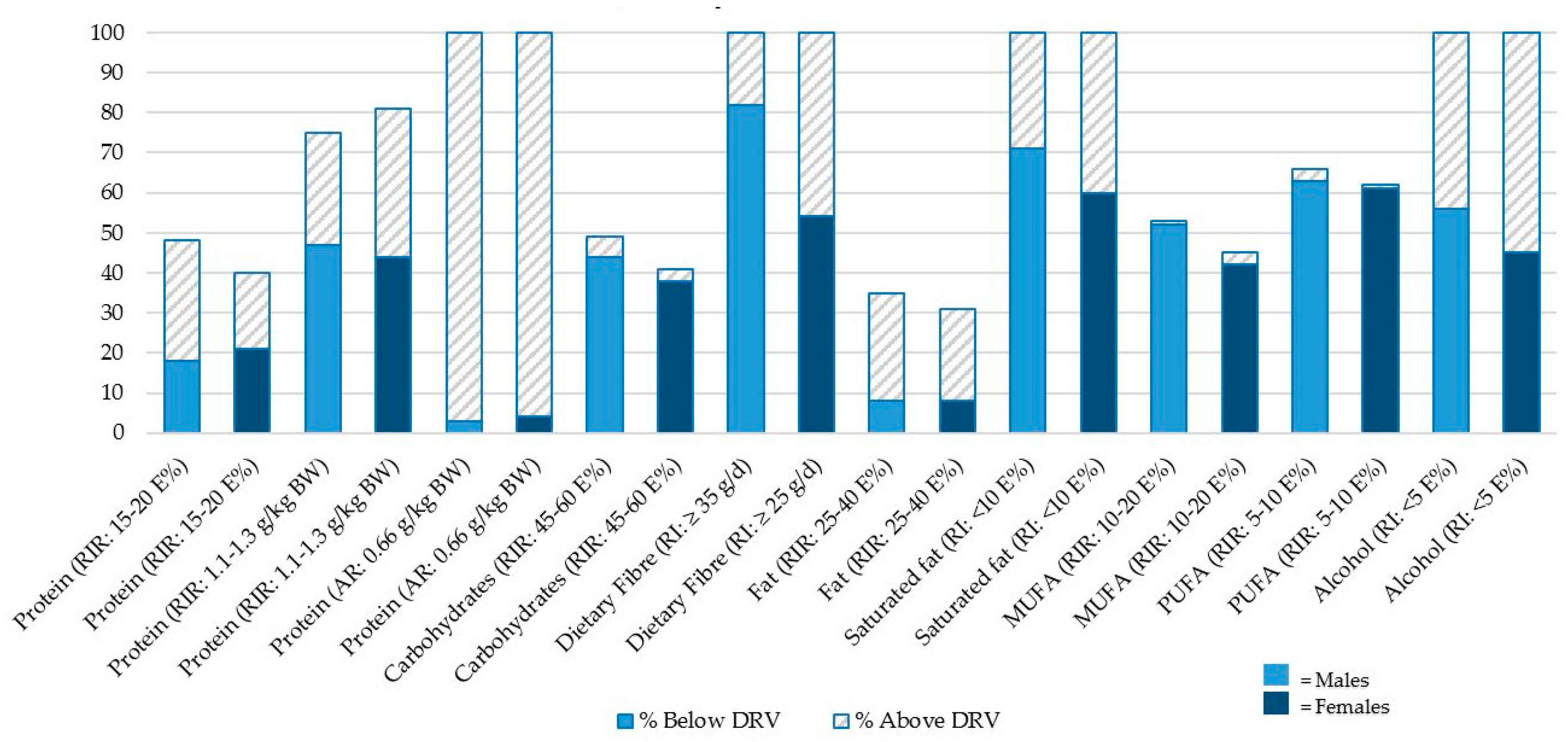
3.3. Comparing Macronutrient Intake to the Recommend Intake Values
3.3.1. Protein
3.3.2. Carbohydrate and Dietary Fiber
3.3.3. Fat
3.3.4. Alcohol
3.4. Comparing Micronutrient Intake to the Estimated Average Requirements
3.4.1. Vitamins
3.4.2. Minerals and Trace Elements
3.5. Potential Determinants of Low Nutrient Intake
4. Discussion
4.1. Protein Intake and Distribution
4.2. Carbohydrate, Fat, and Alcohol
4.3. Micronutrients
4.4. Determinants of Inadequate Nutrient Intake
4.5. Strengths and Limitations
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Abbreviations
| AMDR | Acceptable Macronutrient Distribution Range |
| AR | Average Requirement |
| EAR | Estimated Average Requirement |
| EFSA | European Food Safety Authority |
| g/kg BW | gram per kilo bodyweight |
| MUFA | Mono-Unsaturated Fatty Acids |
| NNR | Nordic Nutritional Recommendations |
| PUFA | Poly-Unsaturated Fatty Acids |
| SFA | Saturated Fatty Acids |
| RI | Reference Intake |
| RIR | Recommended Intake Range for macronutrients |
References
- He, W.; Goodkind, D.; Kowal, P. An Aging World: 2015 International Population Reports; United States Census Bureau: Albany, NY, USA, 2016.
- World Health Organization. World Report on Ageing and Health; World Health Organization: Geneva, Switzerland, 2015. [Google Scholar]
- Semba, R.D.; Bartali, B.; Zhou, J.; Blaum, C.; Ko, C.-W.; Fried, L.P. Low Serum Micronutrient Concentrations Predict Frailty Among Older Women Living in the Community. J. Gerontol. Ser. A 2006, 61, 594–599. [Google Scholar] [CrossRef]
- Ter Borg, S.; Verlaan, S.; Hemsworth, J.; Mijnarends, D.M.; Schols, J.M.G.A.; Luiking, Y.C.; De Groot, L.C. Micronutrient intakes and potential inadequacies of community-dwelling older adults: A systematic review. Br. J. Nutr. 2015, 113, 1195–1206. [Google Scholar] [CrossRef] [PubMed]
- Pirlich, M.; Lochs, H. Nutrition in the elderly. Best Pract. Res. Clin. Gastroenterol. 2001, 15, 869–884. [Google Scholar] [CrossRef] [PubMed]
- Rémond, D.; Shahar, D.R.; Gille, D.; Pinto, P.; Kachal, J.; Peyron, M.A.; Dos Santos, C.N.; Walther, B.; Bordoni, A.; Dupont, D.; et al. Understanding the gastrointestinal tract of the elderly to develop dietary solutions that prevent malnutrition. Oncotarget 2001, 6, 16. [Google Scholar] [CrossRef] [PubMed]
- Paddon-jones, D.; Rasmussen, B.B. Dietary protein recommendations and the prevention of sarcopenia: Protein, amino acid metabolism and therapy. Curr. Opin. Clin. Nutr. Metab. Care 2009, 12, 86–90. [Google Scholar] [CrossRef] [PubMed]
- Baum, J.I.; Kim, I.-Y.; Wolfe, R.R. Protein Consumption and the Elderly: What Is the Optimal Level of Intake? Nutrients 2016, 8, 359. [Google Scholar] [CrossRef] [PubMed]
- Woo, T.; Yu, S.; Visvanathan, R. Systematic Literature Review on the Relationship Between Biomarkers of Sarcopenia and Quality of Life in Older People. J. Frailty 2016, 5, 88–99. [Google Scholar] [CrossRef]
- Verlaan, S.; Mijnarends, D.M.; Luiking, Y.C.; Ter Borg, S.; Schols, J.M.; De Groot, L.C. Macronutrient Intake and Inadequacies of Community-Dwelling Older Adults, a Systematic Review. Ann. Nutr. Metab. 2015, 66, 242–255. [Google Scholar] [CrossRef]
- Otten, J.; Hellwig, J.; Meyers, L. Dietary Reference Intakes: The Essential Guide to Nutrient Requirements; Institute of Medicine: Washington, DC, USA, 2006. [Google Scholar]
- Nordic Council of Ministers. Nordic Nutrition Recommendations 2012. Nord. Nutr. Recomm. 2008, 5, 1–3. [Google Scholar] [CrossRef]
- Rand, W.M.; Pellett, P.L.; Young, V.R. Meta-analysis of nitrogen balance studies for estimating protein requirements in healthy adults. Am. J. Clin. Nutr. 2003, 77, 109–127. [Google Scholar] [CrossRef] [PubMed]
- Pedersen, A.N.; Cederholm, T. Health effects of protein intake in healthy elderly populations: A systematic literature review. Nutr. Res. 2014, 58, 23364. [Google Scholar] [CrossRef]
- Nowson, C.; O’Connell, S. Protein Requirements and Recommendations for Older People: A Review. Nutrients 2015, 7, 6874–6899. [Google Scholar] [CrossRef]
- Bechshøft, R.L.; Reitelseder, S.; Højfeldt, G.; Castro-Mejía, J.L.; Khakimov, B.; Bin Ahmad, H.F.; Kjær, M.; Engelsen, S.B.; Johansen, S.M.B.; Rasmussen, M.A.; et al. Counteracting Age-related Loss of Skeletal Muscle Mass: A clinical and ethnological trial on the role of protein supplementation and training load (CALM Intervention Study): Study protocol for a randomized controlled trial. Trials 2016, 17, 1–17. [Google Scholar] [CrossRef]
- Black, A. Critical evaluation of energy intake using the Goldberg cut-off for energy intake:basal metabolic rate. A practical guide to its calculation, use and limitations. Int. J. Obes. 2000, 24, 1119–1130. [Google Scholar] [CrossRef]
- Beaton, G.H. Approaches to analysis of dietary data: Relationship between planned analyses and choice of methodology. Am. J. Clin. Nutr. 1994, 59. [Google Scholar] [CrossRef] [PubMed]
- Houston, D.K.; Nicklas, B.J.; Ding, J.; Harris, T.B.; Tylavsky, F.A.; Newman, A.B.; Lee, J.S.; Sahyoun, N.R.; Visser, M.; Kritchevsky, S.B.; et al. Dietary protein intake is associated with lean mass change in older, community-dwelling adults: The Health, Aging, and Body Composition (Health ABC ) Study. Am. J. Clin. Nutr. 2008, 87, 150–155. [Google Scholar] [CrossRef]
- Bauer, J.; Biolo, G.; Cederholm, T.; Cesari, M.; Cruz-Jentoft, A.J.; Morley, J.E.; Phillips, S.; Sieber, C.; Stehle, P.; Teta, D.; et al. Evidence-Based Recommendations for Optimal Dietary Protein Intake in Older People: A Position Paper From the PROT-AGE Study Group. J. Am. Med. Dir. Assoc. 2013, 14, 542–559. [Google Scholar] [CrossRef]
- Mitchell, C.J.; Milan, A.M.; Mitchell, S.M.; Zeng, N.; Ramzan, F.; Sharma, P.; Knowles, S.O.; Roy, N.C.; Sjödin, A.; Wagner, K.-H.; et al. The effects of dietary protein intake on appendicular lean mass and muscle function in elderly men: A 10-wk randomized controlled trial. Am. J. Clin. Nutr. 2017, 106, 1375–1383. [Google Scholar] [CrossRef]
- Tieland, M.; Beelen, J.; Laan, A.C.; Poon, S.; De Groot, L.C.; Seeman, E.; Wang, X.; Iuliano, S. An Even Distribution of Protein Intake Daily Promotes Protein Adequacy but Does Not Influence Nutritional Status in Institutionalized Elderly. J. Am. Med. Dir. Assoc. 2018, 19, 33–39. [Google Scholar] [CrossRef] [PubMed]
- Pennings, B.; Groen, B.; De Lange, A.; Gijsen, A.P.; Zorenc, A.H.; Senden, J.M.G.; Van Loon, L.J.C. Amino acid absorption and subsequent muscle protein accretion following graded intakes of whey protein in elderly men. Am. J. Physiol. Metab. 2012, 302, E992–E999. [Google Scholar] [CrossRef] [PubMed]
- Cuthbertson, D.; Smith, K.; Babraj, J.; Leese, G.; Waddell, T.; Atherton, P.; Wackerhage, H.; Taylor, P.M.; Rennie, M.J. Anabolic signaling deficits underlie amino acid resistance of wasting, aging muscle. FASEB J. 2005, 19, 422–424. [Google Scholar] [CrossRef]
- Veronese, N.; Solmi, M.; Caruso, M.G.; Giannelli, G.; Osella, A.R.; Evangelou, E.; Maggi, S.; Fontana, L.; Stubbs, B.; Tzoulaki, I. Dietary fiber and health outcomes: An umbrella review of systematic reviews and meta-analyses. Am. J. Clin. Nutr. 2018, 107, 436–444. [Google Scholar] [CrossRef] [PubMed]
- Spinzi, G. Bowel Care in the Elderly. Dig. Dis. 2007, 25, 160–165. [Google Scholar] [CrossRef]
- Hamley, S. The effect of replacing saturated fat with mostly n-6 polyunsaturated fat on coronary heart disease: A meta-analysis of randomised controlled trials. Nutr. J. 2017, 16, 1–16. [Google Scholar] [CrossRef] [PubMed]
- Dufour, M.C.; Archer, L.; Gordis, E. Alcohol and the elderly. Clin. Geriatr. Med. 1992, 8, 127–141. [Google Scholar] [CrossRef]
- Seitz, H.K.; Stickel, F. Alcoholic Liver Disease in the Elderly. Clin. Geriatr. Med. 2007, 23, 905–921. [Google Scholar] [CrossRef]
- Rehm, J.; Gmel, G.; Imtiaz, S.; Popova, S.; Probst, C.; Roerecke, M.; Room, R.; Gmel, G.E.; Hasan, O.S.M.; Samokhvalov, A.V.; et al. The relationship between different dimensions of alcohol use and the burden of disease-an update. Addiction 2017, 112, 968–1001. [Google Scholar] [CrossRef]
- Lips, P.; Van Schoor, N.M. The effect of vitamin D on bone and osteoporosis. Best Pract. Res. Clin. Endocrinol. Metab. 2011, 25, 585–591. [Google Scholar] [CrossRef]
- Rejnmark, L. Effects of Vitamin D on Muscle Function and Performance: A Review of Evidence from Randomized Controlled Trials. Ther. Adv. Chronic Dis. 2011, 2, 25–37. [Google Scholar] [CrossRef]
- Balion, C.; Griffith, L.E.; Strifler, L.; Henderson, M.; Patterson, C.; Heckman, G.; Llewellyn, D.J.; Raina, P. Vitamin D, cognition, and dementia: A systematic review and meta-analysis. Neurology 2012, 79, 1397–1405. [Google Scholar] [CrossRef]
- Brouwer-Brolsma, E.M.; Bischoff-Ferrari, H.A.; Bouillon, R.; Feskens, E.J.M.; Gallagher, C.J.; Hyppönen, E.; Llewellyn, D.J.; Stoecklin, E.; Dierkes, J.; Kies, A.K.; et al. Vitamin D: Do we get enough? Osteoporos. Int. 2012, 24, 1567–1577. [Google Scholar] [CrossRef]
- Andersen, R.; Mølgaard, C.; Skovgaard, L.T.; Brot, C.; Cashman, K.D.; Chabros, E.; Charzewska, J.; Flynn, A.; Jakobsen, J.; Kärkkäinen, M.; et al. Teenage girls and elderly women living in northern Europe have low winter vitamin D status. Eur. J. Clin. Nutr. 2005, 59, 533–541. [Google Scholar] [CrossRef] [PubMed]
- Cashman, K.D.; Dowling, K.G.; Škrabáková, Z.; Gonzalez-Gross, M.; Valtueña, J.; De Henauw, S.; Moreno, L.; Damsgaard, C.T.; Michaelsen, K.F.; Mølgaard, C.; et al. Vitamin D deficiency in Europe: Pandemic? Am. J. Clin. Nutr. 2016, 103, 1033–1044. [Google Scholar] [CrossRef] [PubMed]
- O’Keeffe, S.T. Thiamine deficiency in elderly people. Age Ageing 2000, 29, 99–101. [Google Scholar] [CrossRef] [PubMed]
- Basiotis, P.P.; Welsh, S.O.; Cronin, F.J.; Kelsay, J.L.; Mertz, W. Number of Days of Food Intake Records Required to Estimate Individual and Group Nutrient Intakes with Defined Confidence. J. Nutr. 1987, 117, 1638–1641. [Google Scholar] [CrossRef] [PubMed]
- Tetens, I.; Biltoft-Jensen, A.P.; Spagner, C.; Christensen, T.; Gille, M.-B.; Bugel, S.; Rasmussen, L.B. Intake of micronutrients among Danish adult users and non-users of dietary supplements. Nutr. Res. 2011, 55, 7153. [Google Scholar] [CrossRef]
- Knudsen, V. The Use of Dietary Supplements by Danes [In Danish]; E-article-Tech; University Denmark: Copenhagen, Denmark, 2014. [Google Scholar]
- Danish National Food Institute. The Danish National Survey of Dietary Habits and Physical Activity (DANSDA) 2011–2013 [In Danish]; Danish National Food Institute: Copenhagen, Denmark, 2015. [Google Scholar]
| Men (n = 79) | Women (n = 78) | |
|---|---|---|
| Age, years | 69 (65–77) | 70 (65–78) |
| Weight, kg | 78.9 (64.6–100.4) | 66.7 (54.3–92.5) |
| Height, m | 1.76 (1.67–1.87) | 1.66 (1.57–1.79) |
| Body mass index (BMI), kg/m2 | 25.3 (21.5–32.7) | 23.9 (19.5–32.2) |
| Waist circumference, cm | 94 (82–115) | 85 (71–111) |
| Hip circumference, cm | 98 (91–109) | 101 (91–116) |
| Systolic blood pressure, mmHg | 142 (116–173) | 140 (113–167) |
| Diastolic blood pressure, mmHg | 84 (70–100) | 81 (68–96) |
| 400 m walking time, seconds | 223 (191–286) | 243 (213–303) |
| Married/cohabitating % | 83 | 46 |
| Men (n = 79) | Women (n = 78) | |
|---|---|---|
| Energy, MJ/day | 9.2 (6.9–12.4) | 7.9 (5.4–10.5) |
| Protein, E% | 17.9 (13.7–24.2) | 17.7 (13.1–24.8) |
| Protein, g/day | 92.3 (60.8–129.0) | 79.4 (48.8–114.5) |
| Protein, g/kg bodyweight | 1.1 (0.8–1.7) | 1.2 (0.7–1.8) |
| Carbohydrates, E% | 46.1 (35.7–59.9) | 46.3 (36.0–56.5) |
| Sugar, E% | 13.8 (8.2–23.0) | 16.9 (8.3–26.7) |
| Dietary fiber, g/day | 23.9 (13.0–40.4) | 23.9 (15.3–38.0) |
| Fat, E% | 35.6 (24.7–47.5) | 35.8 (24.0–44.5) |
| Saturated fat, E% | 12.0 (6.9–19.6) | 11.3 (6.9–16.4) |
| Mono-unsaturated fat, E% | 9.9 (5.5–16.6) | 10.6 (5.1–17.0) |
| Poly-unsaturated fat, E% | 4.3 (1.7–7.7) | 4.6 (2.5–7.5) |
| Alcohol, E% | 5.7 (0.0–23.2) | 4.5 (0.0–13.8) |
| Vitamin A, RE | 830 (209–3167) | 767 (239–2441) |
| Vitamin D, µg | 4.3 (1.0–21.6) | 3.3 (0.7–15.3) |
| Vitamin E, α-TE | 6.5 (2.2–12.1) | 6.8 (2.9–16.8) |
| Thiamine, mg | 1.2 (0.7–2.0) | 1.0 (0.6–1.7) |
| Riboflavin, mg | 1.4 (1.1–2.5) | 1.4 (0.8–2.7) |
| Niacin, NE | 25.8 (16.2–39.8) | 23.0 (12.0–34.2) |
| Vitamin B6, mg | 1.6 (1.0–2.7) | 1.5 (0.9–2.5) |
| Folate, µg | 307 (182–661) | 336 (161–765) |
| Vitamin B12, µg | 6.2 (2.7–16.1) | 4.8 (2.0–16.9) |
| Vitamin C, mg | 97 (31–243) | 125 (33–312) |
| Calcium, mg | 851 (497–1377) | 766 (431–1379) |
| Phosphorus, mg | 1302 (925–2151) | 1221 (752–1836) |
| Potassium, mg | 2884 (1990–4579) | 2807 (1781–4175) |
| Iron, mg | 9.9 (6.1–16.4) | 8.9 (5.1–14.0) |
| Zinc, mg | 9.7 (6.3–16.0) | 9.2 (5.1–12.9) |
| Copper, mg | 2.4 (0.7–6.3) | 2.4 (0.8–5.9) |
| Iodine, µg | 127 (64–274) | 104 (38–252) |
| Selenium, µg | 49.5 (25.4–90.6) | 37.8 (21.4–81.2) |
| NNR DRV | Men | Women | Total | |
|---|---|---|---|---|
| (n = 79) | (n = 78) | (n = 157) | ||
| Protein | RIR: 15–20 E% | 18 * (30) ** | 21 (19) | 19 (25) |
| RIR: 1.1–1.3 g/kg BW | 47 (28) | 44 (37) | 45 (32) | |
| AR $: 0.66 g/kg BW | 3 (97) | 4 (96) | 3 (97) | |
| Carbohydrates | RIR: 45–60 E% | 44 (5) | 38 (3) | 41 (4) |
| Dietary fiber | RI: ≥ 35 g/day (men), ≥ 25 g/day (women) | 82 | 54 | 68 |
| Fat | RIR: 25–40 E% | 8 (27) | 8 (23) | 8 (25) |
| Saturated fat | RI: <10 E% | 71 | 60 | 66 |
| Mono-unsaturated fat | RIR: 10–20 E% | 52 (1) | 42 (3) | 47 (2) |
| Poly-unsaturated fat | RIR: 5–10 E% | 63 (3) | 61 (1) | 62 (2) |
| Alcohol | RI: <5 E% | 56 | 45 | 50 |
| Reference Value | Men | Women | Total | |
|---|---|---|---|---|
| (n = 79) | (n = 78) | (n = 157) | ||
| Vitamin A | 600 RE (men) 500 RE (women) | 33 | 27 | 30 |
| Thiamine | 1.2 mg (men) 0.9 mg (women) | 57 | 33 | 45 |
| Riboflavin | 1.4 mg (men) 1.1 mg (women) | 38 | 26 | 32 |
| Niacin | 15 NE (men) 12 NE (women) | 5 | 4 | 4 |
| Vitamin B6 | 1.3 mg (men) 1.1 mg (women) | 23 | 12 | 17 |
| Folate | 200 µg | 10 | 13 | 11 |
| Vitamin B12 | 1.4 µg | 0 | 3 | 1 |
| Vitamin C | 60 mg (men) 50 mg (women) | 25 | 13 | 19 |
| Vitamin D | 7.5 µg | 76 | 83 | 80 |
| Vitamin E | 6 α-TE (men) 5 α-TE (women) | 46 | 18 | 32 |
| Calcium | 500 mg | 5 | 12 | 8 |
| Phosphorus | 450 mg | 0 | 0 | 0 |
| Iron | 7 mg (men) 6 mg (women) | 16 | 13 | 15 |
| Zinc | 6 mg (men) 5 mg (women) | 3 | 5 | 4 |
| Copper | 0.7 mg | 5 | 4 | 4 |
| Iodine | 100 µg | 28 | 46 | 37 |
| Selenium | 35 mg (men) 30 mg (women) | 25 | 33 | 27 |
| Youngest | Oldest | p-Value ** | Married/Cohabitating | Living Alone | p-Value | Healthy Attitude | Non-Healthy Attitude | p-Value | Highest Energy to Bodyweight Ratio | Lowest Energy to Bodyweight Ratio | p-Value | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Protein RIR: 1.1 g/kg | 39.6 * | 47.7 | 0.39 | 43.0 | 44.9 | 0.83 | 41.8 | 51.1 | 0.10 | 11.5 | 73.6 | <0.001 |
| Dietary fiber RI: $ 25 & 35 g/day | 56.3 | 73.4 | 0.05 | 67.4 | 61.2 | 0.57 | 57.0 | 78.7 | 0.28 | 49.2 | 77.8 | <0.001 |
| Vitamin D AR: 7.5 µg/day | 83.3 | 75.4 | 0.31 | 74.4 | 83.7 | 0.21 | 70.9 | 89.3 | 0.02 | 72.1 | 82.0 | 0.18 |
| Thiamine AR: $ 0.9 & 1.2 mg/day | 43.8 | 46.1 | 0.80 | 44.2 | 42.9 | 0.88 | 35.5 | 45.2 | 0.69 | 33.9 | 44.8 | 0.22 |
| Iodine AR: 100 µg/day | 35.4 | 36.9 | 0.87 | 37.2 | 36.7 | 0.95 | 38.4 | 34.0 | 0.66 | 29.5 | 43.1 | 0.11 |
| Selenium AR: $ 30 & 35 mg/day | 20.8 | 36.9 | 0.07 | 22.1 | 36.7 | 0.07 | 24.4 | 34.0 | 0.03 | 26.2 | 29.2 | 0.71 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rønnow Schacht, S.; Vendelbo Lind, M.; Bechshøft, R.L.; Højfeldt, G.; Reitelseder, S.; Jensen, T.; Pernille Jespersen, A.; Sandris Nielsen, D.; Holm, L.; Tetens, I. Investigating Risk of Suboptimal Macro and Micronutrient Intake and Their Determinants in Older Danish Adults with Specific Focus on Protein Intake—A Cross-Sectional Study. Nutrients 2019, 11, 795. https://doi.org/10.3390/nu11040795
Rønnow Schacht S, Vendelbo Lind M, Bechshøft RL, Højfeldt G, Reitelseder S, Jensen T, Pernille Jespersen A, Sandris Nielsen D, Holm L, Tetens I. Investigating Risk of Suboptimal Macro and Micronutrient Intake and Their Determinants in Older Danish Adults with Specific Focus on Protein Intake—A Cross-Sectional Study. Nutrients. 2019; 11(4):795. https://doi.org/10.3390/nu11040795
Chicago/Turabian StyleRønnow Schacht, Simon, Mads Vendelbo Lind, Rasmus Leidesdorff Bechshøft, Grith Højfeldt, Søren Reitelseder, Tenna Jensen, Astrid Pernille Jespersen, Dennis Sandris Nielsen, Lars Holm, and Inge Tetens. 2019. "Investigating Risk of Suboptimal Macro and Micronutrient Intake and Their Determinants in Older Danish Adults with Specific Focus on Protein Intake—A Cross-Sectional Study" Nutrients 11, no. 4: 795. https://doi.org/10.3390/nu11040795
APA StyleRønnow Schacht, S., Vendelbo Lind, M., Bechshøft, R. L., Højfeldt, G., Reitelseder, S., Jensen, T., Pernille Jespersen, A., Sandris Nielsen, D., Holm, L., & Tetens, I. (2019). Investigating Risk of Suboptimal Macro and Micronutrient Intake and Their Determinants in Older Danish Adults with Specific Focus on Protein Intake—A Cross-Sectional Study. Nutrients, 11(4), 795. https://doi.org/10.3390/nu11040795





