Plant-Based Diet, Cholesterol, and Risk of Gallstone Disease: A Prospective Study
Abstract
:1. Introduction
2. Materials and Methods
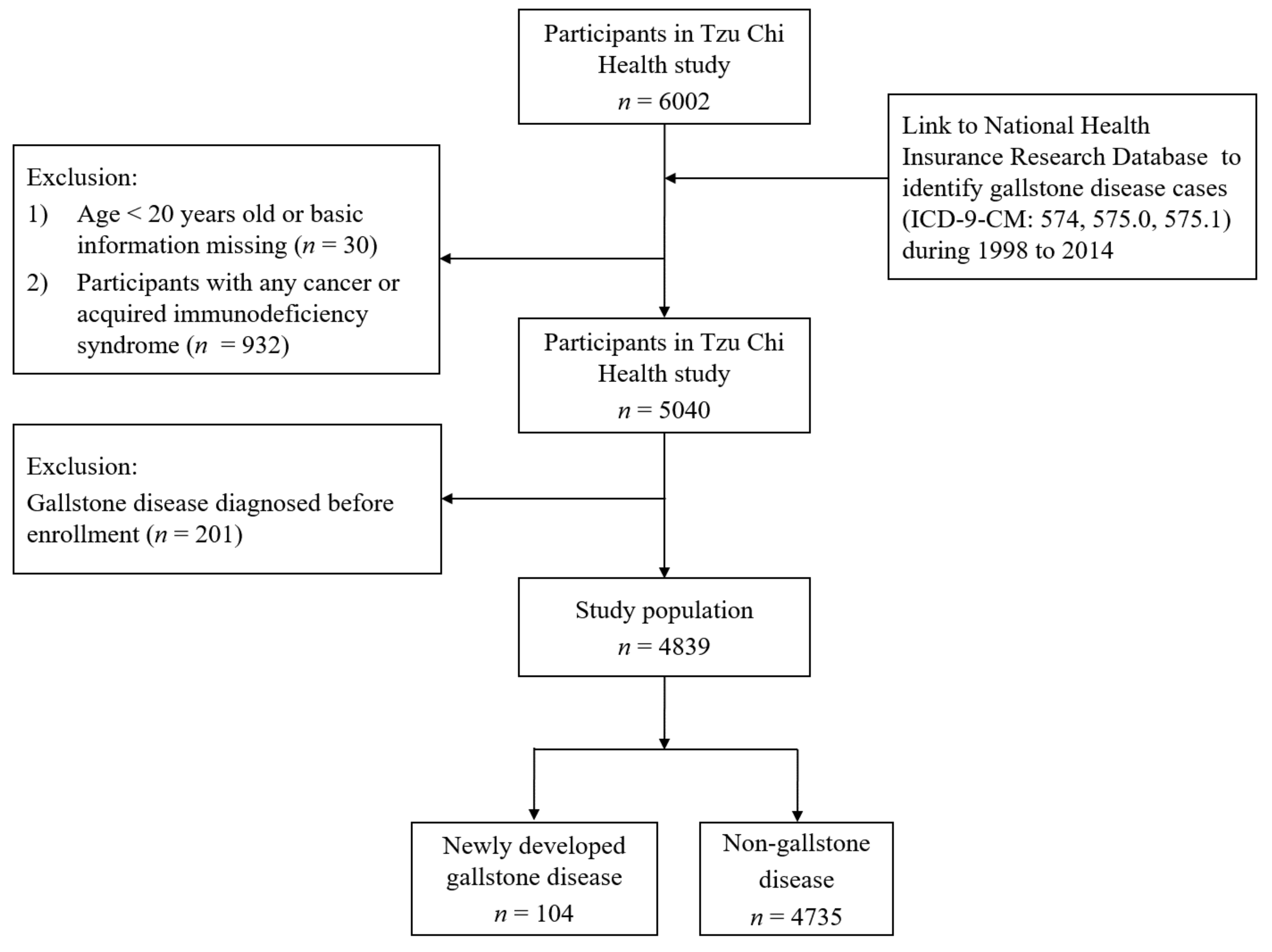
2.1. Study Design and Population
2.2. Assessment of Diet, Cholesterol, and Other Covariates
2.3. Cohort Follow-Up and Case Ascertainment
2.4. Ethics Statements
2.5. Statistical Analysis
3. Results
3.1. Baseline Characteristics
3.2. Dietary Intakes of Vegetarians and Nonvegetarians
3.3. Vegetarian Diet and Gallstone Disease
4. Discussion
4.1. Vegetarian Diet and Gallstone Disease as Related to Cholesterol and Metabolic Risk Factors
4.2. Vegetarian Diet and Gallstone Disease as Related to Female Sex
4.3. Strength and Limitation
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
References
- Chen, C.H.; Huang, M.H.; Yang, J.C.; Nien, C.K.; Etheredge, G.D.; Yang, C.C.; Yeh, Y.H.; Wu, H.S.; Chou, D.A.; Yueh, S.K. Prevalence and risk factors of gallstone disease in an adult population of Taiwan: An epidemiological survey. J. Gastroenterol. Hepatol. 2006, 21, 1737–1743. [Google Scholar] [CrossRef] [PubMed]
- Portincasa, P.; Moschetta, A.; Palasciano, G. Cholesterol gallstone disease. Lancet (Lond. Engl.) 2006, 368, 230–239. [Google Scholar] [CrossRef]
- Chen, Y.C.; Chiou, C.; Lin, M.N.; Lin, C.L. The prevalence and risk factors for gallstone disease in Taiwanese vegetarians. PLoS ONE 2014, 9, e115145. [Google Scholar] [CrossRef] [PubMed]
- Di Ciaula, A.; Wang, D.Q.; Portincasa, P. An update on the pathogenesis of cholesterol gallstone disease. Curr. Opin. Gastroenterol. 2018, 34, 71–80. [Google Scholar] [CrossRef] [PubMed]
- Tsai, C.J.; Leitzmann, M.F.; Willett, W.C.; Giovannucci, E.L. Long-term intake of dietary fiber and decreased risk of cholecystectomy in women. Am. J. Gastroenterol. 2004, 99, 1364–1370. [Google Scholar] [CrossRef]
- Barre, A.; Gusto, G.; Cadeau, C.; Carbonnel, F.; Boutron-Ruault, M.C. Diet and Risk of Cholecystectomy: A Prospective Study Based on the French E3N Cohort. Am. J. Gastroenterol. 2017, 112, 1448–1456. [Google Scholar] [CrossRef]
- Nordenvall, C.; Oskarsson, V.; Wolk, A. Fruit and vegetable consumption and risk of cholecystectomy: A prospective cohort study of women and men. Eur. J. Nutr. 2018, 57, 75–81. [Google Scholar] [CrossRef]
- Lander, E.M.; Wertheim, B.C.; Koch, S.M.; Chen, Z.; Hsu, C.H.; Thomson, C.A. Vegetable protein intake is associated with lower gallbladder disease risk: Findings from the Women’s Health Initiative prospective cohort. Prev. Med. 2016, 88, 20–26. [Google Scholar] [CrossRef]
- McConnell, T.J.; Appleby, P.N.; Key, T.J. Vegetarian diet as a risk factor for symptomatic gallstone disease. Eur. J. Clin. Nutr. 2017, 71, 731–735. [Google Scholar] [CrossRef]
- Wang, F.; Zheng, J.; Yang, B.; Jiang, J.; Fu, Y.; Li, D. Effects of Vegetarian Diets on Blood Lipids: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. J. Am. Heart Assoc. 2015, 4, e002408. [Google Scholar] [CrossRef]
- Chiu, Y.F.; Hsu, C.C.; Chiu, T.H.; Lee, C.Y.; Liu, T.T.; Tsao, C.K.; Chuang, S.C.; Hsiung, C.A. Cross-sectional and longitudinal comparisons of metabolic profiles between vegetarian and non-vegetarian subjects: A matched cohort study. Br. J. Nutr. 2015, 114, 1313–1320. [Google Scholar] [CrossRef] [PubMed]
- Yokoyama, Y.; Levin, S.M.; Barnard, N.D. Association between plant-based diets and plasma lipids: A systematic review and meta-analysis. Nutr. Rev. 2017, 75, 683–698. [Google Scholar] [CrossRef] [PubMed]
- Orlich, M.J.; Singh, P.N.; Sabate, J.; Jaceldo-Siegl, K.; Fan, J.; Knutsen, S.; Beeson, W.L.; Fraser, G.E. Vegetarian dietary patterns and mortality in Adventist Health Study 2. JAMA Intern. Med. 2013, 173, 1230–1238. [Google Scholar] [CrossRef] [PubMed]
- Crowe, F.L.; Appleby, P.N.; Allen, N.E.; Key, T.J. Diet and risk of diverticular disease in Oxford cohort of European Prospective Investigation into Cancer and Nutrition (EPIC): Prospective study of British vegetarians and non-vegetarians. BMJ (Clin. Res. Ed.) 2011, (343), d4131. [Google Scholar] [CrossRef] [PubMed]
- Orlich, M.J.; Singh, P.N.; Sabate, J.; Fan, J.; Sveen, L.; Bennett, H.; Knutsen, S.F.; Beeson, W.L.; Jaceldo-Siegl, K.; Butler, T.L.; et al. Vegetarian dietary patterns and the risk of colorectal cancers. JAMA Intern. Med. 2015, 175, 767–776. [Google Scholar] [CrossRef] [PubMed]
- Chiu, T.H.T.; Pan, W.H.; Lin, M.N.; Lin, C.L. Vegetarian diet, change in dietary patterns, and diabetes risk: A prospective study. Nutr. Diabetes 2018, 8, 12. [Google Scholar] [CrossRef] [PubMed]
- Yokoyama, Y.; Nishimura, K.; Barnard, N.D.; Takegami, M.; Watanabe, M.; Sekikawa, A.; Okamura, T.; Miyamoto, Y. Vegetarian diets and blood pressure: A meta-analysis. JAMA Intern. Med. 2014, 174, 577–587. [Google Scholar] [CrossRef] [PubMed]
- Chiu, T.H.; Huang, H.Y.; Chen, K.J.; Wu, Y.R.; Chiu, J.P.; Li, Y.H.; Chiu, B.C.; Lin, C.L.; Lin, M.N. Relative validity and reproducibility of a quantitative FFQ for assessing nutrient intakes of vegetarians in Taiwan. Public Health Nutr. 2014, 17, 1459–1466. [Google Scholar] [CrossRef]
- Chu, N.F. Prevalence of obesity in Taiwan. Obes. Rev. Off. J. Int. Assoc. Study Obes. 2005, 6, 271–274. [Google Scholar] [CrossRef]
- National Health Insurance Administration, Ministry of Health and Welfare, Taiwan. Available online: http://www.nhi.gov.tw/webdata/webdata.aspx?menu=17&menu_id=1023&WD_ID=1023&webdata_id=815 (accessed on 20 January 2015).
- Li, S.S.; Blanco Mejia, S.; Lytvyn, L.; Stewart, S.E.; Viguiliouk, E.; Ha, V.; de Souza, R.J.; Leiter, L.A.; Kendall, C.W.C.; Jenkins, D.J.A.; et al. Effect of Plant Protein on Blood Lipids: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. J. Am. Heart Assoc. 2017, 6. [Google Scholar] [CrossRef]
- Zak, A.; Zeman, M.; Hrubant, K.; Vecka, M.; Tvrzicka, E. Effect of hypolipidemic treatment on the composition of bile and the risk or cholesterol gallstone disease. Cas. Lek. Ceskych 2007, 146, 24–34. [Google Scholar]
- Holzbach, R.T.; Marsh, M.; Olszewski, M.; Holan, K. Cholesterol solubility in bile. Evidence that supersaturated bile is frequent in healthy man. J. Clin. Investig. 1973, 52, 1467–1479. [Google Scholar] [CrossRef] [PubMed]
- Carey, M.C. Pathogenesis of gallstones. Am. J. Surg. 1993, 165, 410–419. [Google Scholar] [CrossRef]
- Fu, X.; Gong, K.; Shao, X. The relationship between serum lipids, apolipoproteins level and bile lipids level, chemical type of stone. Zhonghua Yi Xue Za Zhi 1995, 75, 656–659. [Google Scholar] [PubMed]
- Atamanalp, S.S.; Keles, M.S.; Atamanalp, R.S.; Acemoglu, H.; Laloglu, E. The effects of serum cholesterol, LDL, and HDL levels on gallstone cholesterol concentration. Pak. J. Med Sci. 2013, 29, 187–190. [Google Scholar] [CrossRef] [PubMed]
- Weerakoon, H.T.; Ranasinghe, S.; Navaratne, A.; Sivakanesan, R.; Galketiya, K.B.; Rosairo, S. Serum lipid concentrations in patients with cholesterol and pigment gallstones. BMC Res. Notes 2014, 7, 548. [Google Scholar] [CrossRef] [PubMed]
- Aulakh, R.; Mohan, H.; Attri, A.K.; Kaur, J.; Punia, R.P. A comparative study of serum lipid profile and gallstone disease. Indian J. Pathol. Microbiol. 2007, 50, 308–312. [Google Scholar] [PubMed]
- Kahleova, H.; Matoulek, M.; Malinska, H.; Oliyarnik, O.; Kazdova, L.; Neskudla, T.; Skoch, A.; Hajek, M.; Hill, M.; Kahle, M.; et al. Vegetarian diet improves insulin resistance and oxidative stress markers more than conventional diet in subjects with Type 2 diabetes. Diabet. Med. A J. Br. Diabet. Assoc. 2011, 28, 549–559. [Google Scholar] [CrossRef] [PubMed]
- Huang, R.Y.; Huang, C.C.; Hu, F.B.; Chavarro, J.E. Vegetarian Diets and Weight Reduction: A Meta-Analysis of Randomized Controlled Trials. J. Gen. Intern. Med. 2016, 31, 109–116. [Google Scholar] [CrossRef] [PubMed]
- Tonstad, S.; Stewart, K.; Oda, K.; Batech, M.; Herring, R.P.; Fraser, G.E. Vegetarian diets and incidence of diabetes in the Adventist Health Study-2. Nutr. Metab. Cardiovasc. Dis. NMCD 2013, 23, 292–299. [Google Scholar] [CrossRef] [PubMed]
- Wang, H.H.; Liu, M.; Clegg, D.J.; Portincasa, P.; Wang, D.Q. New insights into the molecular mechanisms underlying effects of estrogen on cholesterol gallstone formation. Biochim. Biophys. Acta 2009, 1791, 1037–1047. [Google Scholar] [CrossRef] [PubMed]
- De Bari, O.; Wang, T.Y.; Liu, M.; Paik, C.N.; Portincasa, P.; Wang, D.Q. Cholesterol cholelithiasis in pregnant women: Pathogenesis, prevention and treatment. Ann. Hepatol. 2014, 13, 728–745. [Google Scholar] [PubMed]
- Nordenvall, C.; Oskarsson, V.; Sadr-Azodi, O.; Orsini, N.; Wolk, A. Postmenopausal hormone replacement therapy and risk of cholecystectomy: A prospective cohort study. Scand. J. Gastroenterol. 2014, 49, 109–113. [Google Scholar] [CrossRef]
- Racine, A.; Bijon, A.; Fournier, A.; Mesrine, S.; Clavel-Chapelon, F.; Carbonnel, F.; Boutron-Ruault, M.C. Menopausal hormone therapy and risk of cholecystectomy: A prospective study based on the French E3N cohort. CMAJ 2013, 185, 555–561. [Google Scholar] [CrossRef]
- Gann, P.H.; Chatterton, R.T.; Gapstur, S.M.; Liu, K.; Garside, D.; Giovanazzi, S.; Thedford, K.; Van Horn, L. The effects of a low-fat/high-fiber diet on sex hormone levels and menstrual cycling in premenopausal women: A 12-month randomized trial (the diet and hormone study). Cancer 2003, 98, 1870–1879. [Google Scholar] [CrossRef] [PubMed]
- Boyd, N.F.; Lockwood, G.A.; Greenberg, C.V.; Martin, L.J.; Tritchler, D.L. Effects of a low-fat high-carbohydrate diet on plasma sex hormones in premenopausal women: Results from a randomized controlled trial. Canadian Diet and Breast Cancer Prevention Study Group. Br. J. Cancer 1997, 76, 127–135. [Google Scholar] [CrossRef] [PubMed]
- Bagga, D.; Ashley, J.M.; Geffrey, S.P.; Wang, H.J.; Barnard, R.J.; Korenman, S.; Heber, D. Effects of a very low fat, high fiber diet on serum hormones and menstrual function. Implications for breast cancer prevention. Cancer 1995, 76, 2491–2496. [Google Scholar] [CrossRef]
- Harmon, B.E.; Morimoto, Y.; Beckford, F.; Franke, A.A.; Stanczyk, F.Z.; Maskarinec, G. Oestrogen levels in serum and urine of premenopausal women eating low and high amounts of meat. Public Health Nutr. 2014, 17, 2087–2093. [Google Scholar] [CrossRef]
- Fung, T.T.; Hu, F.B.; Barbieri, R.L.; Willett, W.C.; Hankinson, S.E. Dietary patterns, the Alternate Healthy Eating Index and plasma sex hormone concentrations in postmenopausal women. Int. J. Cancer 2007, 121, 803–809. [Google Scholar] [CrossRef]
- Karelis, A.D.; Fex, A.; Filion, M.E.; Adlercreutz, H.; Aubertin-Leheudre, M. Comparison of sex hormonal and metabolic profiles between omnivores and vegetarians in pre- and post-menopausal women. Br. J. Nutr. 2010, 104, 222–226. [Google Scholar] [CrossRef]
- Thomas, H.V.; Davey, G.K.; Key, T.J. Oestradiol and sex hormone-binding globulin in premenopausal and post-menopausal meat-eaters, vegetarians and vegans. Br. J. Cancer 1999, 80, 1470–1475. [Google Scholar] [CrossRef] [PubMed]
- Kaur, J.; Rana, S.V.; Gupta, R.; Gupta, V.; Sharma, S.K.; Dhawan, D.K. Prolonged orocecal transit time enhances serum bile acids through bacterial overgrowth, contributing factor to gallstone disease. J. Clin. Gastroenterol. 2014, 48, 365–369. [Google Scholar] [CrossRef] [PubMed]
- Heaton, K.W.; Emmett, P.M.; Symes, C.L.; Braddon, F.E. An explanation for gallstones in normal-weight women: Slow intestinal transit. Lancet (Lond. Engl.) 1993, 341, 8–10. [Google Scholar] [CrossRef]
- Meier, R.; Beglinger, C.; Dederding, J.P.; Meyer-Wyss, B.; Fumagalli, M.; Rowedder, A.; Turberg, Y.; Brignoli, R. Influence of age, gender, hormonal status and smoking habits on colonic transit time. Neurogastroenterol. Motil. 1995, 7, 235–238. [Google Scholar] [CrossRef]
- Xie, M.; Kotecha, V.R.; Andrade, J.D.; Fox, J.G.; Carey, M.C. Augmented cholesterol absorption and sarcolemmal sterol enrichment slow small intestinal transit in mice, contributing to cholesterol cholelithogenesis. J. Physiol. 2012, 590, 1811–1824. [Google Scholar] [CrossRef] [PubMed]
- Hillemeier, C. An overview of the effects of dietary fiber on gastrointestinal transit. Pediatrics 1995, 96, 997–999. [Google Scholar] [PubMed]
- Shabanzadeh, D.M.; Sorensen, L.T.; Jorgensen, T. A Prediction Rule for Risk Stratification of Incidentally Discovered Gallstones: Results From a Large Cohort Study. Gastroenterology 2016, 150, 156–167.e1. [Google Scholar] [CrossRef] [PubMed]
- Halldestam, I.; Enell, E.L.; Kullman, E.; Borch, K. Development of symptoms and complications in individuals with asymptomatic gallstones. Br. J. Surg. 2004, 91, 734–738. [Google Scholar] [CrossRef]
- Ibrahim, M.; Sarvepalli, S.; Morris-Stiff, G.; Rizk, M.; Bhatt, A.; Walsh, R.M.; Hayat, U.; Garber, A.; Vargo, J.; Burke, C.A. Gallstones: Watch and wait, or intervene? Clevel. Clin. J. Med. 2018, 85, 323–331. [Google Scholar] [CrossRef]
| All | Male | Female | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Nonvegetarians | Vegetarians | p-Value | Nonvegetarians | Vegetarians | p-Value | Nonvegetarians | Vegetarians | p-Value | |
| n (%)/mean ± SD | n (%)/mean ± SD | n (%)/mean ± SD | n (%)/mean ± SD | n (%)/mean ± SD | n (%)/mean ± SD | ||||
| Age, mean ± SD years | 51.8 ± 10.5 | 54.0 ± 9.3 | <0.001 | 51.8 ± 10.9 | 54.2 ± 8.8 | <0.001 | 51.7 ± 10.1 | 54.0 ± 9.4 | <0.001 |
| Sex | <0.001 | ||||||||
| Male | 1625 (47.3%) | 345 (24.6%) | |||||||
| Female | 1811 (52.7%) | 1058 (75.4%) | |||||||
| Education degree | <0.001 | <0.001 | <0.001 | ||||||
| Elementary school or less | 733 (21.3%) | 397 (28.3%) | 232 (14.3%) | 60 (17.4%) | 501 (27.7%) | 337 (31.9%) | |||
| High school | 1654 (48.2%) | 719 (51.2%) | 765 (47.1%) | 178 (51.6%) | 889 (49.1%) | 541 (51.1%) | |||
| College or higher | 1049 (30.5%) | 287 (20.5%) | 628 (38.6%) | 107 (31.0%) | 421 (23.2%) | 180 (17.0%) | |||
| Smoking status | <0.001 | <0.001 | 0.014 | ||||||
| Ever | 718 (20.9%) | 116 (8.3%) | 676 (41.6%) | 105 (30.4%) | 42 (2.3%) | 11 (1.0%) | |||
| Never | 2718 (79.1%) | 1287 (91.7%) | 949 (58.4%) | 240 (69.6%) | 1769 (97.7%) | 1047 (99.0%) | |||
| Alcohol drinking status | <0.001 | 0.076 | <0.001 | ||||||
| Ever | 614 (17.9%) | 115 (8.2%) | 539 (33.2%) | 97 (28.1%) | 75 (4.1%) | 18 (1.7%) | |||
| Never | 2822 (82.1%) | 1288 (91.8%) | 1086 (66.8%) | 248 (71.9%) | 1736 (95.9%) | 1040 (98.3%) | |||
| Sport habit | 0.003 | 0.428 | 0.098 | ||||||
| Yes | 2365 (68.8%) | 904 (64.4%) | 1176 (72.4%) | 242 (70.1%) | 1189 (65.7%) | 662 (62.6%) | |||
| No | 1071 (31.2%) | 499 (35.6%) | 449 (27.6%) | 103 (29.9%) | 622 (34.3%) | 396 (37.4%) | |||
| Hypertension * | 0.564 | 0.2641 | 0.471 | ||||||
| Yes | 752 (21.9%) | 296 (21.1%) | 391 (24.1%) | 73 (21.2%) | 361 (19.9%) | 223 (21.1%) | |||
| No | 2684 (78.1%) | 1107 (78.9%) | 1234 (75.9%) | 272 (78.8%) | 1450 (80.1%) | 835 (78.9%) | |||
| Diabetes mellitus * | 0.005 | 0.423 | 0.021 | ||||||
| Yes | 318 (9.3%) | 95 (6.8%) | 161 (9.9%) | 29 (8.4%) | 157 (8.7%) | 66 (6.2%) | |||
| No | 3118 (90.7%) | 1308 (93.2%) | 1464 (90.1%) | 316 (91.6%) | 1654 (91.3%) | 992 (93.8%) | |||
| Heart disease * | 0.461 | 0.186 | 0.642 | ||||||
| Yes | 338 (9.8%) | 148 (10.5%) | 172 (10.6%) | 45 (13.0%) | 166 (9.2%) | 103 (9.7%) | |||
| No | 3098 (90.2%) | 1255 (89.5%) | 1453 (89.4%) | 300 (87.0%) | 1645 (90.8%) | 955 (90.3%) | |||
| Liver disease * | 0.403 | 0.677 | 0.409 | ||||||
| Yes | 689 (20.1%) | 266 (19.0%) | 391 (24.1%) | 79 (22.9%) | 298 (16.5%) | 187 (17.7%) | |||
| No | 2747 (79.9%) | 1137 (81.0%) | 1234 (75.9%) | 266 (77.1%) | 1513 (83.5%) | 871 (82.3%) | |||
| Kidney disease * | 0.040 | 0.241 | 0.275 | ||||||
| Yes | 170 (4.9%) | 50 (3.6%) | 93 (5.7%) | 14 (4.1%) | 77 (4.3%) | 36 (3.4%) | |||
| No | 3266 (95.1%) | 1353 (96.4%) | 1532 (94.3%) | 331 (95.9%) | 1734 (95.7%) | 1022 (96.6%) | |||
| Body mass index | <0.001 | <0.001 | <0.001 | ||||||
| ≧24 | 1611 (46.9%) | 471 (33.6%) | 914 (56.2%) | 135 (39.1%) | 697 (38.5%) | 336 (31.8%) | |||
| <24 | 1825 (53.1%) | 932 (66.4%) | 711 (43.8%) | 210 (60.9%) | 1114 (61.5%) | 722 (68.2%) | |||
| Total cholesterol | <0.001 | <0.001 | <0.001 | ||||||
| ≧200 | 1526 (44.4%) | 369 (26.3%) | 696 (42.8%) | 69 (20.0%) | 830 (45.8%) | 300 (28.4%) | |||
| <200 | 1910 (55.6%) | 1034 (73.7%) | 929(57.2%) | 276 (80.0%) | 981 (54.2%) | 758 (71.6%) | |||
| Lipid-lowering medications | <0.001 | <0.001 | <0.001 | ||||||
| Yes | 872 (25.4%) | 224 (16.0%) | 424 (26.1%) | 56 (16.2%) | 448 (24.7%) | 168 (15.9%) | |||
| No | 2564 (74.6%) | 1179 (84.0%) | 1201 (73.9%) | 289 (83.8%) | 1363 (75.3%) | 890 (84.1%) | |||
| Menopause | <0.001 | ||||||||
| Yes | 1032 (57.0%) | 694 (65.6%) | |||||||
| No | 779 (43.0%) | 364 (34.4%) | |||||||
| Total cholesterol, mean ± SD | 196.7 ± 36.7 | 180.7 ± 33.1 | <0.001 | 194.0 ± 36.6 | 175.0 ± 34.4 | <0.001 | 199.0 ± 36.6 | 183.0 ± 32.4 | <0.001 |
| HDL cholesterol, mean ± SD | 54.2 ± 14.7 | 52.4 ± 13.7 | <0.001 | 48.7 ± 12.4 | 44.9 ± 10.4 | <0.001 | 59.1 ± 14.9 | 54.9 ± 13.7 | <0.001 |
| LDL cholesterol, mean ± SD | 129.0 ± 33.4 | 116.0 ± 29.3 | <0.001 | 130.0 ± 33.3 | 115.0 ± 28.1 | <0.001 | 129.0 ± 33.5 | 117.0 ± 29.7 | <0.001 |
| Triglyceride, mean ± SD | 117.0 ± 85.4 | 114.0 ± 77.8 | 0.230 | 133.0 ± 104.0 | 129.0 ± 93.6 | 0.481 | 102.0 ± 61.4 | 109.0 ± 71.3 | 0.014 |
| Food and Nutrients | All | Male | Female | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Nonvegetarians | Vegetarians | p-Value | Nonvegetarians | Vegetarians | p-Value | Nonvegetarians | Vegetarians | p-Value | |
| Median (P25, P75) | Median (P25, P75) | Median (P25, P75) | Median (P25, P75) | Median (P25, P75) | Median (P25, P75) | ||||
| Energy, kcal | 1739 (1312, 2290) | 1702 (1273, 2262) | 0.118 | 2066 (1616, 2669) | 2234 (1653, 2799) | 0.068 | 1486 (1119, 1931) | 1608 (1218, 2028) | <0.0001 |
| Meat, servings | 0.6 (0.2, 1.6) | - | - | 1.0 (0.3, 2.2) | - | - | 0.4 (0.1, 1.1) | - | - |
| Fish, servings | 0.5 (0.1, 1.1) | - | - | 0.6 (0.2, 1.3) | - | - | 0.3 (0.1, 0.9) | - | - |
| Soy, servings | 0.9 (0.5, 1.7) | 1.5 (0.8, 2.5) | <0.0001 | 1.0 (0.5, 1.7) | 1.6 (1.0, 2.9) | <0.0001 | 0.9 (0.5, 1.6) | 1.4 (0.8, 2.3) | <0.0001 |
| Dairy, servings | 0.2 (0, 0.7) | 0.2 (0, 0.6) | <0.0001 | 0.2 (0, 0.7) | 0.2 (0, 0.7) | 0.626 | 0.2 (0, 0.7) | 0.2 (0, 0.6) | <0.0001 |
| Eggs, servings | 0.3 (0.1, 0.6) | 0.3 (0.1, 0.4) | <0.0001 | 0.4 (0.2, 0.6) | 0.3 (0.1, 0.5) | <0.0001 | 0.3 (0.1, 0.5) | 0.3 (0.1, 0.4) | <0.0001 |
| Vegetables, servings | 3.8 (2.3, 5.7) | 4.5 (2.9, 6.8) | <0.0001 | 3.5 (2.2, 5.5) | 4.9 (3.0, 7.3) | <0.0001 | 3.9 (2.4, 5.9) | 4.4 (2.9, 6.8) | <0.0001 |
| Fruits, servings | 1.0 (0.5, 2.0) | 1.0 (0.6, 2.0) | 0.020 | 1.0 (0.5, 2.0) | 1.0 (0.6, 2.0) | 0.112 | 1.0 (0.5, 2.0) | 1.0 (0.5, 2.0) | 0.226 |
| Vitamin C, mg | 164 (112, 233) | 172 (118, 249) | 0.001 | 165 (112, 226) | 184 (130, 262) | <0.0001 | 163 (112, 237) | 168 (115, 243) | 0.191 |
| Dietary fiber, g | 19 (14, 26) | 23 (16, 31) | <0.0001 | 19 (15, 27) | 25 (19, 35) | <0.0001 | 19 (14, 26) | 21 (16, 29) | <0.0001 |
| Protein (% energy) | 13 (12, 15) | 12 (11, 13) | <0.001 | 13 (11, 15) | 12 (10, 13) | <0.001 | 13 (12, 15) | 12 (11, 14) | <0.001 |
| Fat (% energy) | 27 (21, 33) | 25 (20, 30) | <0.001 | 26 (20, 32) | 22 (18, 29) | <0.001 | 28 (22, 34) | 25 (20, 30) | <0.001 |
| Carbohydrate (% energy) | 60 (54, 67) | 64 (59, 70) | <0.001 | 61 (54, 68) | 66 (59, 71) | <0.001 | 59 (53, 66) | 64 (58, 69) | <0.001 |
| Cases/Person-Years | All | Male | Female |
|---|---|---|---|
| 104/29295 | 4311964 | 61/17332 | |
| HR (95% CI) | HR (95% CI) | HR (95% CI) | |
| Crude model | 0.66 (0.41, 1.05) | 1.08 (0.50, 2.33) | 0.51 (0.28, 0.92) |
| Adjusted model | |||
| Vegetarians vs. nonvegetarians | 0.70 (0.43, 1.14) | 1.26 (0.57, 2.77) | 0.52 (0.28, 0.96) |
| Age | 1.03 (1.01, 1.06) | 1.04 (1.01, 1.08) | 1.06 (1.02, 1.10) |
| Sex (male vs. female) | 0.86 (0.53, 1.40) | - | - |
| High school vs. elementary | 1.11 (0.68, 1.82) | 1.58 (0.62, 3.99) | 0.83 (0.44, 1.56) |
| College or higher vs. elementary | 1.07 (0.59, 1.96) | 1.67 (0.62, 4.52) | 0.71 (0.30, 1.68) |
| Alcohol drinker | 1.37 (0.76, 2.49) | 1.68 (0.87, 3.23) | 0.39 (0.05, 2.92) |
| Smoking | 0.90 (0.48, 1.70) | 0.78 (0.4, 1.54) | 2.94 (0.68, 12.6) |
| Sport habit | 1.01 (0.66, 1.56) | 1.44 (0.66, 3.16) | 0.89 (0.52, 1.52) |
| Diabetes mellitus | 1.75 (0.98, 3.12) | 2.25 (1.01, 5.03) | 1.38 (0.59, 3.23) |
| Kidney disease | 1.27 (0.58, 2.77) | 0.66 (0.16, 2.76) | 1.99 (0.78, 5.09) |
| BMI ≧ 24 kg/m2 | 1.36 (0.92, 2.03) | 1.49 (0.79, 2.81) | 1.35 (0.80, 2.27) |
| Lipid-lowering medications | 0.82 (0.51, 1.32) | 0.90 (0.44, 1.85) | 0.72 (0.37, 1.39) |
| TCH ≧ 200 mg/dL | 1.69 (1.12, 2.55) | 1.89 (1.00, 3.59) | 1.74 (1.00, 3.03) |
| Menopause | - | - | 0.34 (0.16, 0.73) |
| All | Male | Female | ||
|---|---|---|---|---|
| Total cholesterol ≧ 200 mg/dL | Cases/person-years | 56/11,421 | 23/4638 | 33/6783 |
| HR (95% CI) | 0.89 (0.44, 1.81) | 1.39 (0.41, 4.76) | 0.77 (0.33, 1.79) | |
| Total cholesterol < 200 mg/dL | Cases/person-years | 48/17,874 | 20/7326 | 28/10,549 |
| HR (95% CI) | 0.56 (0.28, 1.11) | 1.31 (0.47, 3.70) | 0.34 (0.14, 0.82) |
| All | Male | Female | |
|---|---|---|---|
| Vegetarian with TCH < 200 mg/dL | 1 | 1 | 1 |
| Nonvegetarian with TCH < 200 mg/dL | 1.72 (0.88, 3.33) | 0.89 (0.32, 2.46) | 2.48 (1.05, 5.88) |
| Vegetarian with TCH ≧ 200 mg/dL | 2.20 (0.94, 5.14) | 2.12 (0.50, 8.99) | 2.64 (0.91, 7.65) |
| Nonvegetarian with TCH ≧ 200 mg/dL | 2.71 (1.40, 5.21) | 1.65 (0.60, 4.50) | 3.81 (1.61, 9.01) |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chang, C.-M.; Chiu, T.H.T.; Chang, C.-C.; Lin, M.-N.; Lin, C.-L. Plant-Based Diet, Cholesterol, and Risk of Gallstone Disease: A Prospective Study. Nutrients 2019, 11, 335. https://doi.org/10.3390/nu11020335
Chang C-M, Chiu THT, Chang C-C, Lin M-N, Lin C-L. Plant-Based Diet, Cholesterol, and Risk of Gallstone Disease: A Prospective Study. Nutrients. 2019; 11(2):335. https://doi.org/10.3390/nu11020335
Chicago/Turabian StyleChang, Chun-Ming, Tina H. T. Chiu, Chia-Chen Chang, Ming-Nan Lin, and Chin-Lon Lin. 2019. "Plant-Based Diet, Cholesterol, and Risk of Gallstone Disease: A Prospective Study" Nutrients 11, no. 2: 335. https://doi.org/10.3390/nu11020335
APA StyleChang, C.-M., Chiu, T. H. T., Chang, C.-C., Lin, M.-N., & Lin, C.-L. (2019). Plant-Based Diet, Cholesterol, and Risk of Gallstone Disease: A Prospective Study. Nutrients, 11(2), 335. https://doi.org/10.3390/nu11020335




