Gluten-Induced Extra-Intestinal Manifestations in Potential Celiac Disease—Celiac Trait
Abstract
1. Introduction
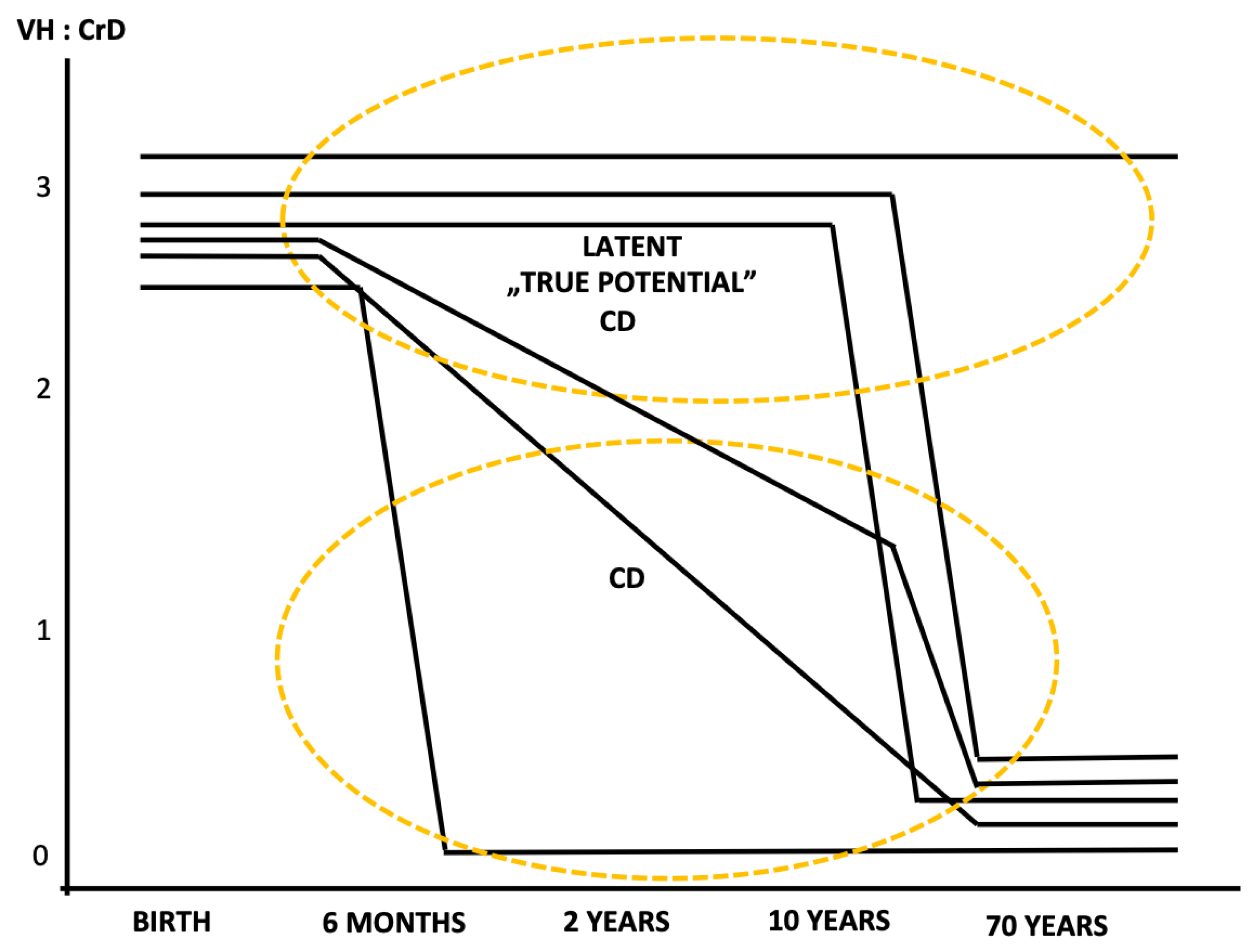
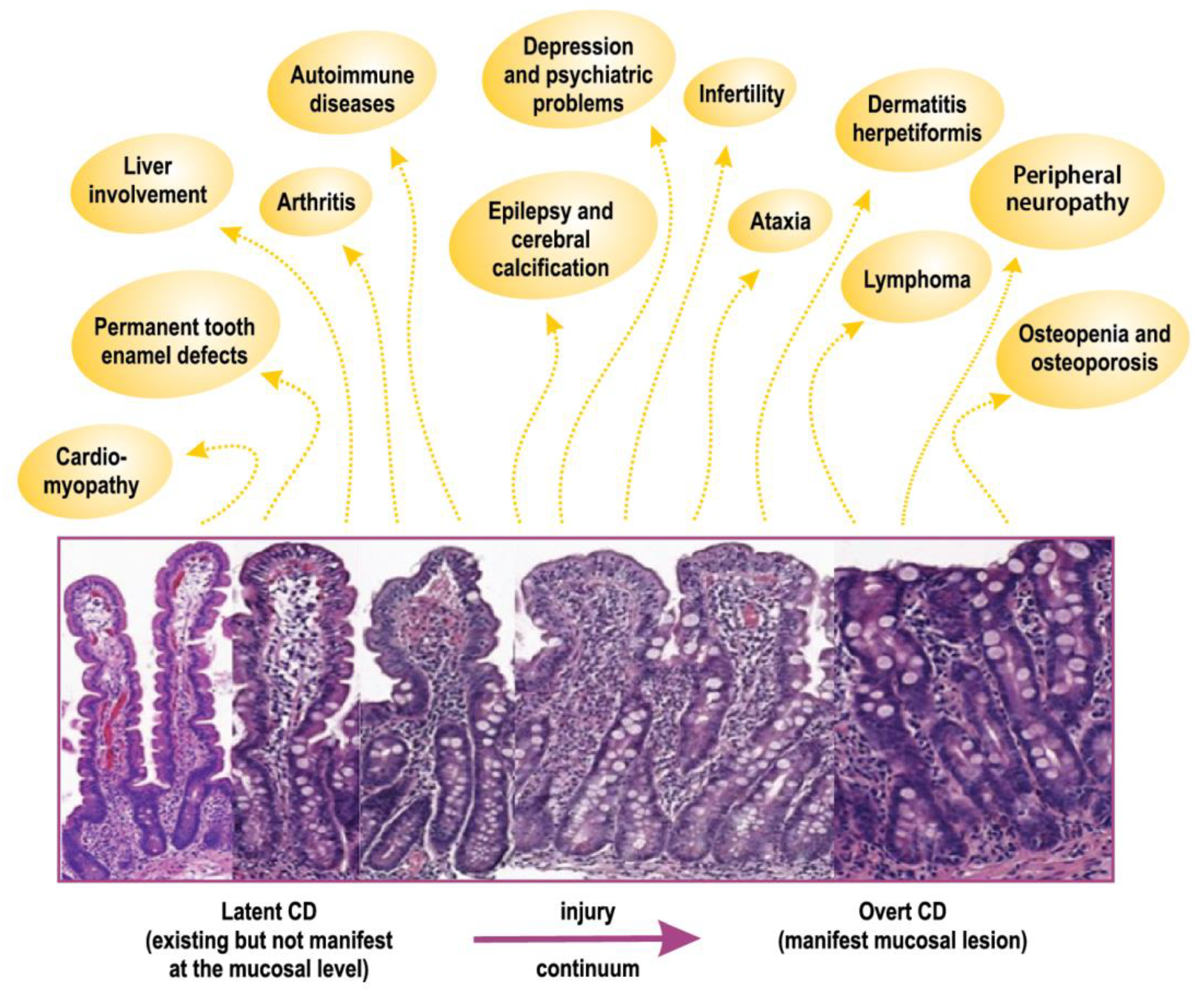
2. Latent or Potential Celiac Disease
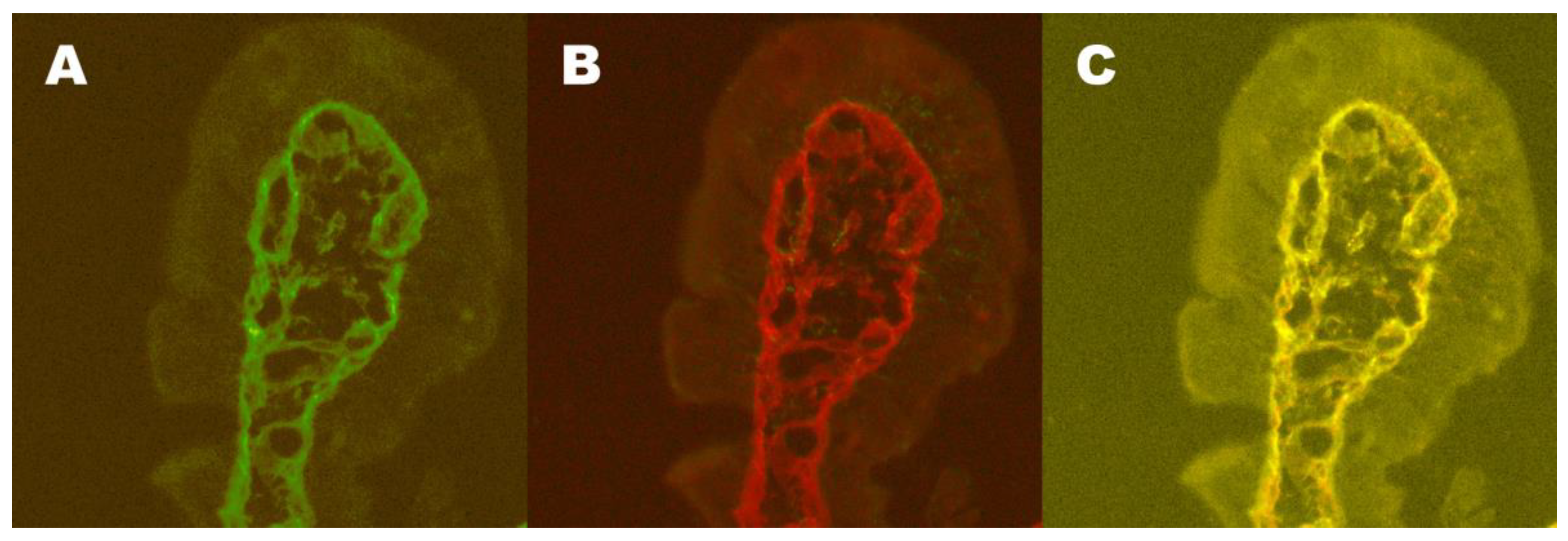
3. Markers of Existing Early Disease
4. Extraintestinal Manifestations
4.1. Dermatitis Herpetiformis
4.2. Central and Peripheral Nervous System
4.3. Bone Disease
4.4. Liver Diseases
4.5. Other Extraintestinal Manifestations
4.5.1. Permanent Tooth Dental Enamel Defects
4.5.2. Malignancies
5. Celiac Trait
Author Contributions
Funding
Conflicts of Interest
References
- Mäki, M.; Collin, P. Celiac disease. Lancet 1997, 349, 1755–1759. [Google Scholar] [CrossRef]
- Laurikka, P.; Nurminen, S.; Kivelä, L.; Kurppa, K. Extraintestinal manifestations of celiac disease: Early detection for better long-term outcomes. Nutrients 2018, 10, 1015. [Google Scholar] [CrossRef] [PubMed]
- Pinto-Sanchez, M.I.; Bercik, P.; Verdu, E.F.; Bai, J.C. Extraintestinal manifestations of celiac disease. Dig. Dis. 2015, 33, 147–154. [Google Scholar] [CrossRef] [PubMed]
- Kaukinen, K.; Collin, P.; Mäki, M. Celiac disease-a diagnostic and therapeutic challenge. Duodecim 2010, 126, 245–254. [Google Scholar] [PubMed]
- Collin, P.; Reunala, T.; Rasmussen, M.; Kyrönpalo, S.; Pehkonen, E.; Laippala, P.; Mäki, M. High incidence and prevalence of adult celiac disease: Augmented diagnostic approach. Scand. J. Gastroenterol. 1997, 32, 1129–1133. [Google Scholar] [CrossRef] [PubMed]
- Lohi, S.; Mustalahti, K.; Kaukinen, K.; Laurila, K.; Collin, P.; Rissanen, H.; Lohi, O.; Bravi, E.; Gasparin, M.; Reunanen, A.; et al. Increasing prevalence of celiac disease over time. Aliment. Pharmacol. Ther. 2007, 26, 1217–1225. [Google Scholar] [CrossRef] [PubMed]
- Virta, L.J.; Kaukinen, K.; Collin, P. Incidence and prevalence of diagnosed celiac disease in Finland: Results of effective case finding in adults. Scand. J. Gastroenterol. 2009, 44, 933–938. [Google Scholar] [CrossRef] [PubMed]
- Fry, L.; Riches, D.J.; Seah, P.P.; Hoffbrand, A.V. Clearance of skin lesions in dermatitis herpetiformis after gluten withdrawal. Lancet 1973, 301, 288–291. [Google Scholar] [CrossRef]
- Reunala, T.; Kosnai, I.; Karpati, S.; Kuitunen, P.; Török, E.; Savilahti, E. Dermatitis herpetiformis: Jejunal findings and skin response to gluten-free diet. Arch. Dis. Child. 1984, 59, 517–522. [Google Scholar] [CrossRef]
- Reunala, T.; Mäki, M. Dermatitis herpetiformis: A genetic disease. Eur. J. Dermatol. 1993, 3, 519–526. [Google Scholar]
- Hervonen, K.; Karell, K.; Holopainen, P.; Collin, P.; Partanen, J.; Reunala, T. Concordance of dermatitis herpetiformis and celiac disease in monozygous twins. J. Investig. Dermatol. 2000, 115, 990–993. [Google Scholar] [CrossRef] [PubMed]
- Molteni, N.; Caraceni, M.P.; Bardella, M.T.; Ortolani, S.; Gandolini, G.G.; Bianchi, P. Bone mineral density in adult celiac patients and the effect of gluten-free diet from childhood. Am. J. Gastroenterol. 1990, 85, 51–53. [Google Scholar] [PubMed]
- Mustalahti, K.; Collin, P.; Sievänen, H.; Salmi, J.; Mäki, M. Osteopenia in patients with clinically silent celiac disease warrants screening. Lancet 1999, 354, 744–745. [Google Scholar] [CrossRef]
- Heikkilä, K.; Pearce, J.; Mäki, M.; Kaukinen, K. Celiac disease and bone fractures: A systematic review and meta-analysis. J. Clin. Endocrinol. Metab. 2015, 100, 25–34. [Google Scholar] [CrossRef] [PubMed]
- Trotta, L.; Biagi, F.; Bianchi, P.I.; Marchese, A.; Vattiato, C.; Balduzzi, D.; Collesano, V.; Corazza, G.R. Dental enamel defects in adult celiac disease: Prevalence and correlation with symptoms and age at diagnosis. Eur. J. Intern. Med. 2013, 24, 832–834. [Google Scholar] [CrossRef] [PubMed]
- Mäki, M.; Hällström, O.; Verronen, P.; Reunala, T.; Lahdeaho, M.L.; Holm, K.; Visakorpi, J.K. Reticulin antibody, arthritis, and celiac disease in children. Lancet 1988, 1, 479–480. [Google Scholar] [CrossRef]
- Collin, P.; Korpela, M.; Hällström, O.; Viander, M.; Keyriläinen, O.; Mäki, M. Rheumatic complaints as a presenting symptom in patients with celiac disease. Scand. J. Rheumatol. 1992, 21, 20–23. [Google Scholar] [CrossRef] [PubMed]
- Daron, C.; Soubrier, M.; Mathieu, S. Occurrence of rheumatic symptoms in celiac disease: A meta-analysis: Comment on the article “Osteoarticular manifestations of celiac disease and non-celiac gluten hypersensitivity” by Dos Santos and Lioté. Jt. Bone Spine 2017, 84, 645–646. [Google Scholar] [CrossRef]
- Gobbi, G.; Bouquet, F.; Greco, L.; Lambertini, A.; Tassinari, C.A.; Ventura, A.; Zaniboni, M.G. Celiac disease, epilepsy and cerebral calcifications. The Italian Working Group on Celiac Disease and Epilepsy. Lancet 1992, 340, 439–443. [Google Scholar]
- Hadjivassiliou, M.; Grunewald, R.A.; Chattopadhyay, A.K.; Davies-Jones, G.A.; Gibson, A.; Jarrat, J.A.; Kandler, R.H.; Lobo, A.; Powell, T.; Smith, C.M. Clinical, radiological, neurophysiological, and neuropathological characteristics of gluten ataxia. Lancet 1998, 352, 1582–1585. [Google Scholar] [CrossRef]
- Luostarinen, L.; Pirttilä, T.; Collin, P. Celiac disease presenting with neurological disorders. Eur. Neurol. 1999, 42, 132–135. [Google Scholar] [CrossRef] [PubMed]
- Zis, P.; Sarrigiannis, P.G.; Rao, D.G.; Hadjivassiliou, M. Gluten neuropathy: Prevalence of neuropathic pain and the role of gluten-free diet. J. Neurol. 2018, 265, 2231–2236. [Google Scholar] [CrossRef] [PubMed]
- Volta, U.; De Franceschi, L.; Lari, F.; Molinaro, N.; Zoli, M.; Bianchi, F.B. Celiac disease hidden by cryptogenic hypertransaminasaemia. Lancet 1998, 352, 26–29. [Google Scholar] [CrossRef]
- Kaukinen, K.; Halme, L.; Collin, P.; Färkkilä, M.; Mäki, M.; Vehmanen, P.; Partanen, J.; Höckerstedt, K. Celiac disease in patients with severe liver disease: Gluten-free diet may reverse hepatic failure. Gastroenterology 2002, 122, 881–888. [Google Scholar] [CrossRef] [PubMed]
- Korpimäki, S.; Kaukinen, K.; Collin, P.; Haapala, A.-M.; Holm, P.; Laurila, K.; Kurppa, K.; Saavalainen, P.; Haimila, K.; Partanen, J.; et al. Gluten-sensitive hypertransaminasemia in celiac disease: An infrequent and often subclinical finding. Am. J. Gastroenterol. 2011, 106, 1689–1696. [Google Scholar] [CrossRef] [PubMed]
- Sher, K.S.; Jayanthi, V.; Probert, C.S.; Stewart, C.R.; Mayberry, J.F. Infertility, obstetric and gynaecological problems in celiac sprue. Dig. Dis. 1994, 12, 186–190. [Google Scholar] [CrossRef]
- Tersigni, C.; Castellani, R.; de Waure, C.; Fattorossi, A.; De Spirito, M.; Gasbarrini, A.; Scambia, G.; Di Simone, N. Celiac disease and reproductive gdisorders: Meta-analysis of epidemiologic associations and potential pathogenic mechanisms. Hum. Reprod. Update 2014, 20, 582–593. [Google Scholar] [CrossRef]
- Ventura, A.; Magazzu, G.; Greco, L. Duration of exposure to gluten and risk for autoimmune disorders in patients with celiac disease. Gastroenterology 1999, 117, 297–303. [Google Scholar] [CrossRef]
- Cosnes, J.; Cellier, C.; Viola, S.; Colombel, J.F.; Michaud, L.; Sarles, J.; Hugot, J.P.; Ginies, J.L.; Dabadie, A.; Mouterde, O. Groupe D’Etude et de Recherche Sur la Maladie Coeliaque. Incidence of autoimmune diseases in celiac disease: Protective effect of the gluten-free diet. Clin. Gastroenterol. Hepatol. 2008, 6, 753–758. [Google Scholar] [CrossRef]
- Holmes, G.K.T.; Prior, P.; Lane, M.R.; Pope, D.; Allan, R.N. Malignancy in celiac disease—Effect of a gluten free diet. Gut 1989, 30, 333–338. [Google Scholar] [CrossRef]
- Tio, M.; Cox, M.R.; Eslick, G.D. Meta-analysis: Celiac disease and the risk of all-cause mortality, any malignancy and lymphoid malignancy. Aliment. Pharmacol. Ther. 2012, 35, 540–551. [Google Scholar] [CrossRef] [PubMed]
- Mäki, M. Celiac disease. In Gastrointestinal Functions; Delvin, E.E., Lentze, M.J., Eds.; Nestlé Nutrition Workshop Series, Pediatric Program; Lippincott Williams & Wilkins: Vevey, Switzerland, 2001; Volume 46, pp. 257–274. ISBN 0-7817-3208-5. [Google Scholar]
- Freeman, H.J.; Chiu, B.K. Multifocal small bowel lymphoma and latent celiac sprue. Gastroenterology 1986, 90, 1992–1997. [Google Scholar] [CrossRef]
- Mäki, M.; Aine, L.; Lipsanen, V.; Koskimies, S. Dental enamel defects in first-degree relatives of celiac disease patients. Lancet 1991, 337, 763–764. [Google Scholar] [CrossRef]
- Savilahti, E.; Reunala, T.; Mäki, M. Increase of lymphocytes bearing the gamma/delta T-cell receptor in the jejunum of patients with dermatitis herpetiformis. Gut 1992, 33, 206–211. [Google Scholar] [CrossRef] [PubMed]
- Mäki, M.; Huupponen, T.; Holm, K.; Hällström, O. Seroconversion of reticulin autoantibodies predicts celiac disease in insulin-dependent diabetes mellitus. Gut 1995, 36, 239–242. [Google Scholar] [CrossRef] [PubMed]
- Ludvigsson, J.F.; Leffler, D.A.; Bai, J.C.; Biagi, F.; Fasano, A.; Green, P.H.; Hadjivassiliou, M.; Kaukinen, K.; Kelly, C.P.; Leonard, J.N.; et al. The Oslo definitions for celiac disease and related terms. Gut 2013, 62, 43–52. [Google Scholar] [CrossRef] [PubMed]
- Weinstein, W.M. Latent celiac sprue. Gastroenterology 1974, 66, 489–493. [Google Scholar]
- Ferguson, A.; Blackwell, J.N.; Barnetson, R.S. Effects of additional dietary gluten on the small-intestinal mucosa of volunteers and of patients with dermatitis herpetiformis. Scand. J. Gastroenterol. 1987, 22, 543–549. [Google Scholar] [CrossRef]
- Chorzelski, T.P.; Rosinska, D.; Beutner, E.H.; Sulej, J.; Kumar, V. Aggressive gluten challenge of dermatitis herpetiformis cases converts them from seronegative to seropositive for IgA-class endomysial antibodies. J. Am. Acad. Dermatol. 1988, 18, 672–678. [Google Scholar] [CrossRef]
- Doherty, M.; Barry, R.E. Gluten-induced mucosal changes in subjects without overt small-bowel disease. Lancet 1981, 1, 517–520. [Google Scholar] [CrossRef]
- Mäki, M.; Holm, K.; Koskimies, S.; Hallstrom, O.; Visakorpi, J.K. Normal small bowel biopsy followed by celiac disease. Arch. Dis. Child. 1990, 65, 1137–1141. [Google Scholar] [CrossRef] [PubMed]
- Mäki, M.; Holm, K.; Collin, P.; Savilahti, E. Increase in γ/δ T cell receptor bearing lymphocytes in normal small bowel mucosa in latent celiac disease. Gut 1991, 32, 1412–1414. [Google Scholar] [CrossRef] [PubMed]
- Mäki, M.; Holm, K.; Lipsanen, V.; Hällström, O.; Viander, M.; Collin, P.; Savilahti, E.; Koskimies, S. Serological markers and HLA genes among healthy first-degree relatives of patients with celiac disease. Lancet 1991, 338, 1350–1353. [Google Scholar] [CrossRef]
- Collin, P.; Helin, H.; Mäki, M.; Hällström, O.; Karvonen, A.L. Follow-up of patients positive in reticulin and gliadin antibody tests with normal small-bowel biopsy findings. Scand. J. Gastroenterol. 1993, 28, 595–598. [Google Scholar] [CrossRef] [PubMed]
- Ferguson, A.; Arranz, E.; O’Mahony, S. Clinical and pathological spectrum of celiac disease—Active, silent, latent, potential. Gut 1993, 34, 150–151. [Google Scholar] [CrossRef] [PubMed]
- Troncone, R. Latent celiac disease in Italy. Acta Paediatr. 1995, 84, 1252–1257. [Google Scholar] [CrossRef] [PubMed]
- Corazza, G.R.; Andreani, M.L.; Biagi, F.; Bonvicini, F.; Bernardi, M.; Gasbarrini, G. Clinical, pathological, and antibody pattern of latent celiac disease: Report of three adult cases. Am. J. Gastroenterol. 1996, 91, 2203–2207. [Google Scholar]
- Vilppula, A.; Kaukinen, K.; Luostarinen, L.; Kerkelä, I.; Patrikainen, H.; Valve, T.; Mäki, M.; Collin, P. Increasing prevalence and high incidence of celiac disease in elderly people: A population-based study. BMC Gastroenterol. 2009, 9, 49. [Google Scholar] [CrossRef]
- Kaukinen, K.; Collin, P.; Mäki, M. Latent celiac disease or celiac disease beyond villous atrophy? Gut 2007, 56, 1339–1340. [Google Scholar] [CrossRef]
- Mäki, M. Lack of consensus regarding definitions of celiac disease. Nat. Rev. Gastroenterol. Hepatol. 2012, 9, 305–306. [Google Scholar] [CrossRef]
- Not, T.; Ziberna, F.; Vatta, S.; Quaglia, S.; Martelossi, S.; Villanacci, V.; Marzari, R.; Florian, F.; Vecchiet, M.; Sulic, A.M.; et al. Cryptic genetic gluten intolerance revealed by intestinal antitransglutaminase antibodies and response to gluten-free diet. Gut 2011, 60, 1487–1493. [Google Scholar] [CrossRef] [PubMed]
- Kurppa, K.; Collin, P.; Viljamaa, M.; Haimila, K.; Saavalainen, P.; Partanen, J.; Laurila, K.; Huhtala, H.; Paasikivi, K.; et al. Diagnosing mild enteropathy celiac disease: A randomized, controlled clinical study. Gastroenterology 2009, 136, 816–823. [Google Scholar] [CrossRef] [PubMed]
- Husby, S.; Koletzko, S.; Korponay-Szabó, I.R.; Mearin, M.L.; Phillips, A.; Shamir, R.; Troncone, R.; Giersiepen, K.; Branski, D.; Catassi, C.; et al. European Society for Pediatric Gastroenterology, Hepatology, and Nutrition Guidelines for the Diagnosis of Celiac Disease. J. Pediatr. Gastroenterol. Nutr. 2012, 54, 136–160. [Google Scholar] [CrossRef] [PubMed]
- Mäki, M. The humoral immune system in celiac disease. Baillière’s Clin. Gastroenterol. 1995, 9, 231–249. [Google Scholar] [CrossRef]
- Simon-Vecsei, Z.; Király, R.; Bagossi, P.; Tóth, B.; Dahlbom, I.; Caja, S.; Csősz, E.; Lindfors, K.; Sblattero, D.; Nemes, E.; et al. A single conformational transglutaminase 2 epitope contributed by three domains is critical for celiac antibody binding and effects. Proc. Natl. Acad. Sci. USA 2012, 109, 431–436. [Google Scholar] [CrossRef] [PubMed]
- Yu, X.B.; Uhde, M.; Green, P.H.; Alaedini, A. Autoantibodies in the extraintestinal manifestations of celiac disease. Nutrients 2018, 10, 1123. [Google Scholar] [CrossRef] [PubMed]
- Rostami, K.; Aldulaimi, D.; Holmes, G.; Johnson, M.W.; Robert, M.; Srivastava, A.; Fléjou, J.-F.; Sanders, D.S.; Volta, U.; Derakhshan, M.H.; et al. Microscopic enteritis: Bucharest consensus. World J. Gastroenterol. 2015, 21, 2593–2604. [Google Scholar] [CrossRef] [PubMed]
- Salmi, T.T.; Collin, P.; Järvinen, O.; Haimila, K.; Partanen, J.; Laurila, K.; Korponay-Szabo, I.R.; Huhtala, H.; Reunala, T.; Mäki, M.; et al. Immunoglobulin A autoantibodies against transglutaminase 2 in the small intestinal mucosa predict forthcoming celiac disease. Aliment. Pharmacol. Ther. 2006, 24, 541–552. [Google Scholar] [CrossRef] [PubMed]
- Holm, K.; Mäki, M.; Savilahti, E.; Lipsanen, V.; Laippala, P.; Koskimies, S. Intraepithelial gamma/delta T-cell-receptor lymphocytes and genetic susceptibility to celiac disease. Lancet 1992, 339, 1500–1503. [Google Scholar] [CrossRef]
- Iltanen, S.; Holm, K.; Partanen, J.; Laippala, P.; Mäki, M. Increased density of jejunal γδ+ T cells in patients having normal mucosa—Marker of operative autoimmune mechanisms? Autoimmunity 1999, 29, 1787–1791. [Google Scholar] [CrossRef]
- Korponay-Szabo, I.R.; Halttunen, T.; Szalai, Z.; Laurila, K.; Király, R.; Kovács, J.B.; Fésüs, L.; Mäki, M. In vivo targeting of intestinal and extraintestinal transglutaminase 2 by celiac autoantibodies. Gut 2004, 53, 641–648. [Google Scholar] [CrossRef] [PubMed]
- Kaukinen, K.; Peräaho, M.; Collin, P.; Partanen, J.; Woolley, N.; Kaartinen, T.; Nuutinen, T.; Halttunen, T.; Mäki, M.; Korponay-Szabo, I. Small-bowel mucosal transglutaminase 2-specific IgA deposits in celiac disease without villous atrophy: A prospective and randomized clinical study. Scand. J. Gastroenterol. 2005, 40, 564–572. [Google Scholar] [CrossRef] [PubMed]
- Koskinen, O.; Collin, P.; Korponay-Szabo, I.; Salmi, T.; Iltanen, S.; Haimila, K.; Partanen, J.; Mäki, M.; Kaukinen, K. Gluten-dependent small bowel mucosal transglutaminase 2-specific IgA deposits in overt and mild enteropathy celiac disease. J. Pediatr. Gastroenterol. Nutr. 2008, 47, 436–442. [Google Scholar] [CrossRef] [PubMed]
- Maglio, M.; Ziberna, F.; Aitoro, R.; Discepolo, V.; Lania, G.; Bassi, V.; Miele, E.; Not, T.; Troncone, R.; Auricchio, R. Intestinal production of anti-tissue transglutaminase 2 antibodies in patients with diagnosis other than celiac disease. Nutrients 2017, 9, 1050. [Google Scholar] [CrossRef] [PubMed]
- Reunala, T.; Blomqvist, K.; Tarpila, S.; Halme, H.; Kangas, K. Gluten-free diet in dermatitis herpetiformis. I. Clinical response of skin lesions in 81 patients. Br. J. Dermatol. 1977, 97, 473–480. [Google Scholar] [CrossRef] [PubMed]
- Mansikka, E.; Hervonen, K.; Kaukinen, K.; Collin, P.; Huhtala, H.; Reunala, T.; Salmi, T. Prognosis of dermatitis herpetiformis patients with and without villous atrophy at diagnosis. Nutrients 2018, 10, 641. [Google Scholar] [CrossRef] [PubMed]
- Reunala, T.; Salmi, T.T.; Hervonen, K.; Kaukinen, K.; Collin, P. Dermatitis herpetiformis: A common extraintestinal manifestation of celiac disease. Nutrients 2018, 10, 602. [Google Scholar] [CrossRef]
- Salmi, T.T.; Hervonen, K.; Laurila, K.; Collin, P.; Mäki, M.; Koskinen, O.; Huhtala, H.; Kaukinen, K.; Reunala, T. Small bowel transglutaminase 2-specific IgA deposits in dermatitis herpetiformis. Acta Derm. Venereol. 2014, 94, 393–397. [Google Scholar] [CrossRef]
- Salmi, T.; Collin, P.; Korponay-Szabo, I.R.; Laurila, K.; Partanen, J.; Huhtala, H.; Kiraly, R.; Lorand, L.; Reunala, T.; Mäki, M.; et al. Endomysial antibody-negative celiac disease: Clinical characteristics and intestinal autoantibody deposits. Gut 2006, 55, 1746–1753. [Google Scholar] [CrossRef]
- Pasternack, C.; Mansikka, E.; Kaukinen, K.; Hervonen, K.; Reunala, T.; Collin, P.; Huhtala, H.; Mattila, V.M.; Salmi, T. Self-reported fractures in dermatitis herpetiformis compared to celiac disease. Nutrients 2018, 10, 351. [Google Scholar] [CrossRef]
- Hadjivassiliou, M.; Gibson, A.; Davies-Jones, G.A.; Lobo, A.J.; Stephenson, T.J.; Milford-Ward, A. Does cryptic gluten sensitivity play a part in neurological illness? Lancet 1996, 347, 369–371. [Google Scholar] [CrossRef]
- Hadjivassiliou, M.; Grünewald, R.A.; Sanders, D.S.; Zis, P.; Croall, I.; Shanmugarajah, P.D.; Sarrigiannis, P.G.; Trott, N.; Wild, G.; Hoggard, N. The significance of low titre antigliadin antibodies in the diagnosis of gluten ataxia. Nutrients 2018, 10, 1444. [Google Scholar] [CrossRef] [PubMed]
- Hadjivassiliou, M.; Davies-Jones, G.A.B.; Sanders, D.S.; Grunewald, R.A. Dietary treatment of gluten ataxia. J. Neurol. Neurosurg. Psychiatry 2003, 74, 1221–1224. [Google Scholar] [CrossRef] [PubMed]
- Hadjivassiliou, M.; Mäki, M.; Sanders, D.S.; Williamson, C.A.; Grunewald, R.A.; Woodroofe, N.M.; Korponay-Szabo, I.R. Antibody targeting of brain and intestinal trasnglutaminase in gluten ataxia. Neurology 2006, 66, 373–377. [Google Scholar] [CrossRef] [PubMed]
- Hadjivassiliou, M.; Aeschlimann, P.; Sanders, D.S.; Mäki, M.; Kaukinen, K.; Grünewald, R.A.; Bandmann, O.; Woodroofe, N.; Haddock, G.; Aeschlimann, D.P. Transglutaminase 6 antibodies in the diagnosis of gluten ataxia. Neurology 2013, 80, 1740–1745. [Google Scholar] [CrossRef] [PubMed]
- Zis, P.; Sarrigiannis, P.G.; Rao, D.G.; Hadjivassiliou, M. Quality of life in patients with gluten neuropathy: A case-controlled study. Nutrients 2018, 10, 662. [Google Scholar] [CrossRef] [PubMed]
- Hadjivassiliou, M.; Grünewald, R.A.; Kandler, R.H.; Chattopadhyay, A.K.; Jarratt, J.A.; Sanders, D.S.; Sharrack, B.; Wharton, S.B.; Davies-Jones, G.A. Neuropathy associated with gluten sensitivity. J. Neurol. Neurosurg. Psychiatry 2006, 77, 1262–1266. [Google Scholar] [CrossRef]
- Hadjivassiliou, M.; Kandler, R.H.; Chattopadhyay, A.K.; Davies-Jones, A.G.; Jarratt, J.A.; Sanders, D.S.; Sharrack, B.; Grünewald, R.A. Dietary treatment of gluten neuropathy. Muscle Nerve 2006, 34, 762–766. [Google Scholar] [CrossRef]
- Larussa, T.; Suraci, E.; Nazionale, I.; Abenavoli, L.; Imeneo, M.; Luzza, F. Bone mineralization in celiac disease. Gastroenterol. Res. Pract. 2012, 198025. [Google Scholar] [CrossRef]
- Zanchetta, M.B.; Longobardi, V.; Bai, J.C. Bone and celiac disease. Curr. Osteoporos. Rep. 2016, 14, 43–48. [Google Scholar] [CrossRef]
- Grace-Farfaglia, P. Bones of contention: Bone mineral density recovery in celiac disease—A systematic review. Nutrients 2015, 7, 3347–3369. [Google Scholar] [CrossRef] [PubMed]
- Kaukinen, K.; Mäki, M.; Partanen, J.; Sievänen, H.; Collin, P. Celiac disease without villous atrophy: Revision of criteria called for. Dig. Dis. Sci. 2001, 46, 879–887. [Google Scholar] [CrossRef] [PubMed]
- Dickey, W.; Hughes, D.F.; McMillan, S.A. Patients with serum IgA endomysial antibodies and intact duodenal villi: Clinical characteristics and management options. Scand. J. Gastroenterol. 2005, 40, 1240–1243. [Google Scholar] [CrossRef] [PubMed]
- Kurppa, K.; Collin, P.; Sievänen, H.; Huhtala, H.; Mäki, M.; Kaukinen, K. Gastrointestinal symptoms, quality of life and bone mineral density in mild enteropathic celiac disease: A prospective clinical trial. Scand. J. Gastroenterol. 2010, 45, 305–314. [Google Scholar] [CrossRef] [PubMed]
- Zanini, B.; Caselani, F.; Magni, A.; Turini, D.; Ferraresi, A.; Lanzarotto, F.; Villanacci, V.; Carabellese, N.; Ricci, C.; Lanzini, A. Celiac disease with mild enteropathy is not mild disease. Clin. Gastroenterol. Hepatol. 2013, 11, 253–258. [Google Scholar] [CrossRef] [PubMed]
- Volta, U. Pathogenesis and clinical significance of liver injury in celiac disease. Clin. Rev. Allergy Immunol. 2009, 36, 62–70. [Google Scholar] [CrossRef] [PubMed]
- Aine, L.; Mäki, M.; Collin, P.; Keyriläinen, O. Dental enamel defects in celiac disease. J. Oral Pathol. Med. 1990, 19, 241–245. [Google Scholar] [CrossRef]
- Aine, L.; Reunala, T.; Mäki, M. Dental enamel defects in children with dermatitis herpetiformis. J. Pediatr. 1991, 118, 572–574. [Google Scholar] [CrossRef]
- Aine, L.; Mäki, M.; Reunala, T. Celiac-type dental enamel defects in patients with dermatitis herpetiformis. Acta Derm. Venereol. 1992, 72, 25–27. [Google Scholar]
- Marsh, M.N. Gluten, major histocompatibility complex, and the small intestine. A molecular and immunologic approach to the spectrum of gluten sensitivity (‘celiac sprue’). Gastroenterology 1992, 102, 330–354. [Google Scholar] [CrossRef]
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Popp, A.; Mäki, M. Gluten-Induced Extra-Intestinal Manifestations in Potential Celiac Disease—Celiac Trait. Nutrients 2019, 11, 320. https://doi.org/10.3390/nu11020320
Popp A, Mäki M. Gluten-Induced Extra-Intestinal Manifestations in Potential Celiac Disease—Celiac Trait. Nutrients. 2019; 11(2):320. https://doi.org/10.3390/nu11020320
Chicago/Turabian StylePopp, Alina, and Markku Mäki. 2019. "Gluten-Induced Extra-Intestinal Manifestations in Potential Celiac Disease—Celiac Trait" Nutrients 11, no. 2: 320. https://doi.org/10.3390/nu11020320
APA StylePopp, A., & Mäki, M. (2019). Gluten-Induced Extra-Intestinal Manifestations in Potential Celiac Disease—Celiac Trait. Nutrients, 11(2), 320. https://doi.org/10.3390/nu11020320



