A Systematic Review and Meta-Analysis on the Effects of Probiotic Species on Iron Absorption and Iron Status
Abstract
1. Introduction
2. Materials and Methods
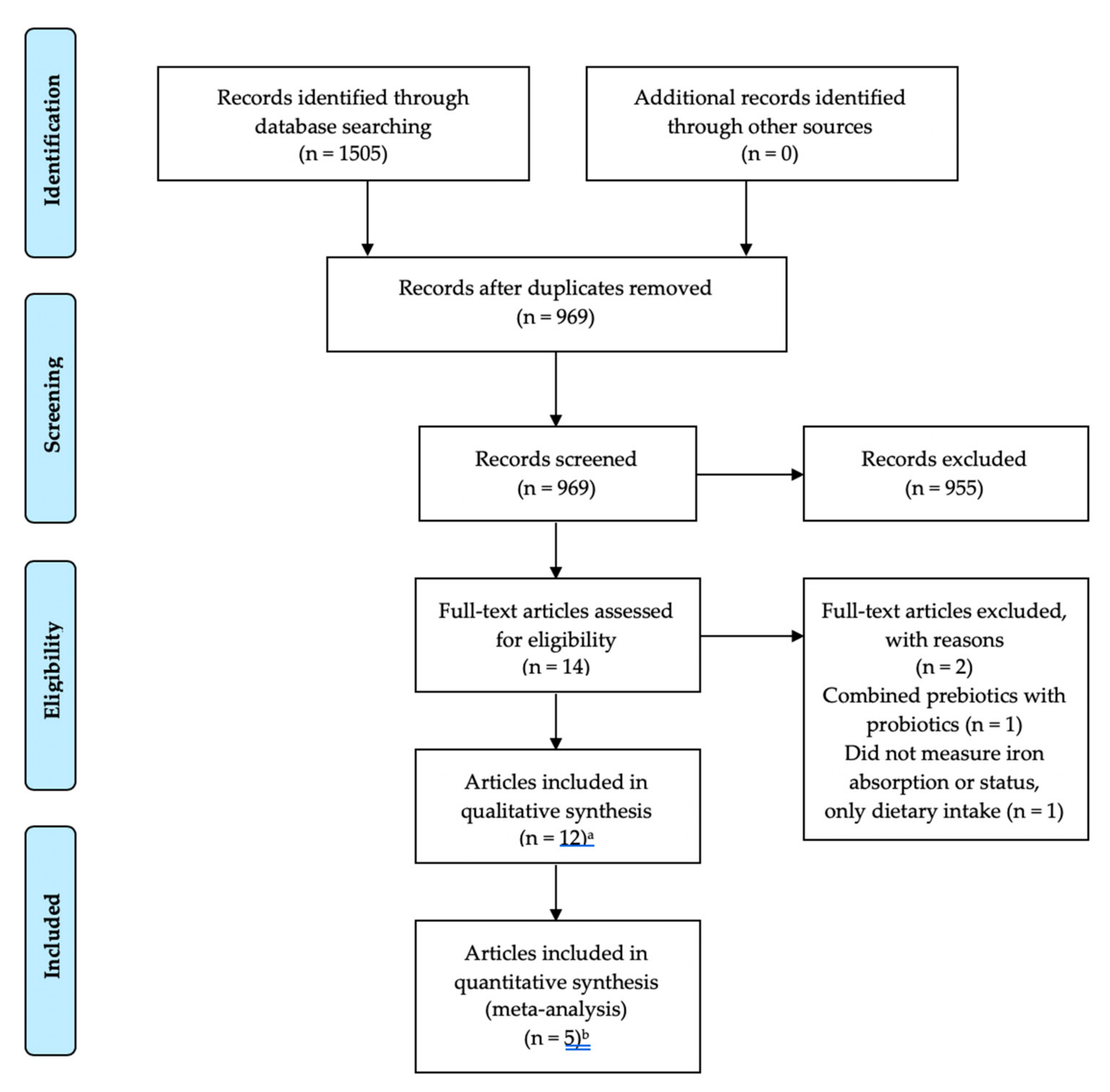
2.1. Search Strategy and Study Selection
2.2. Eligibility Criteria
2.3. Data Extraction and Management
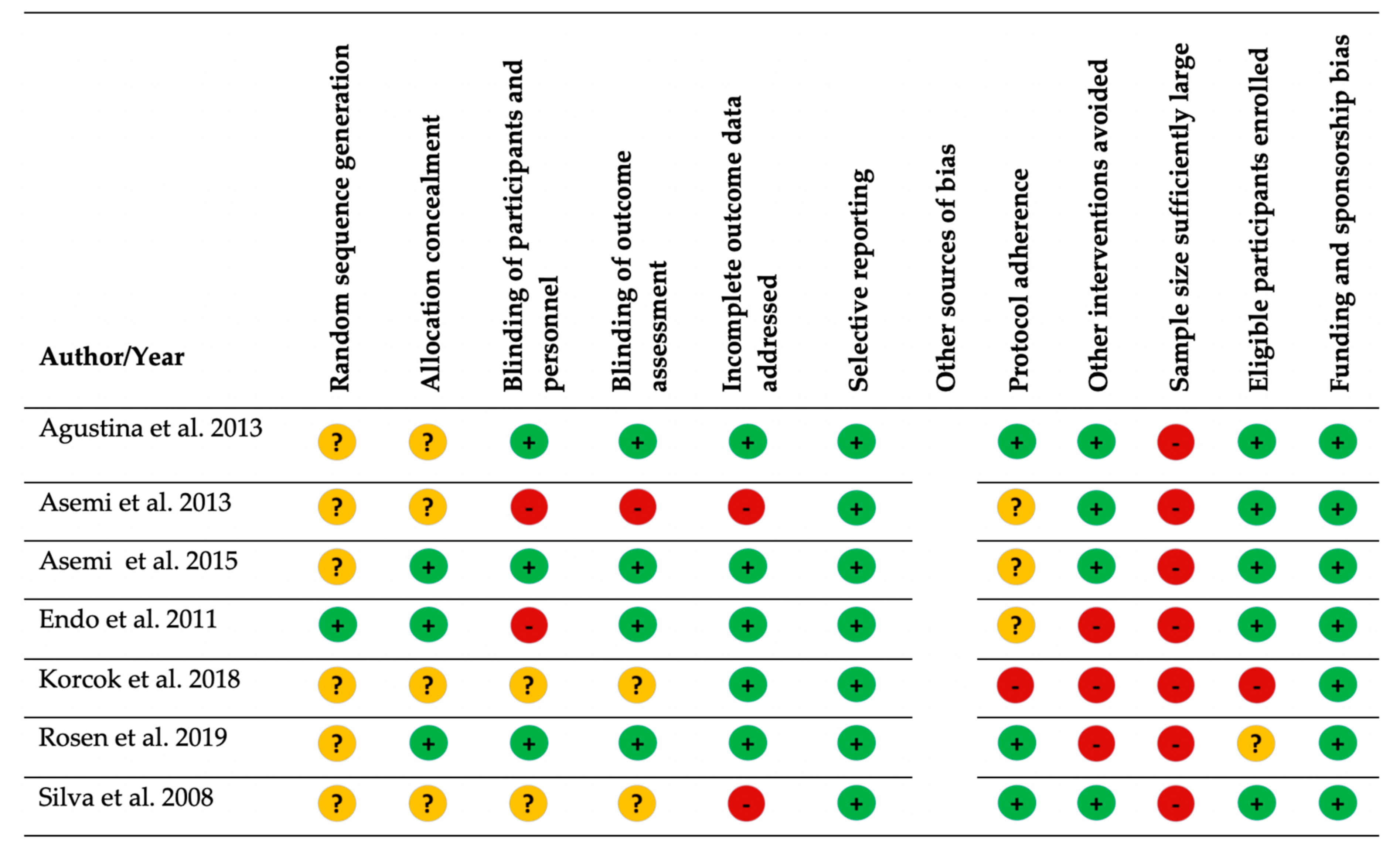
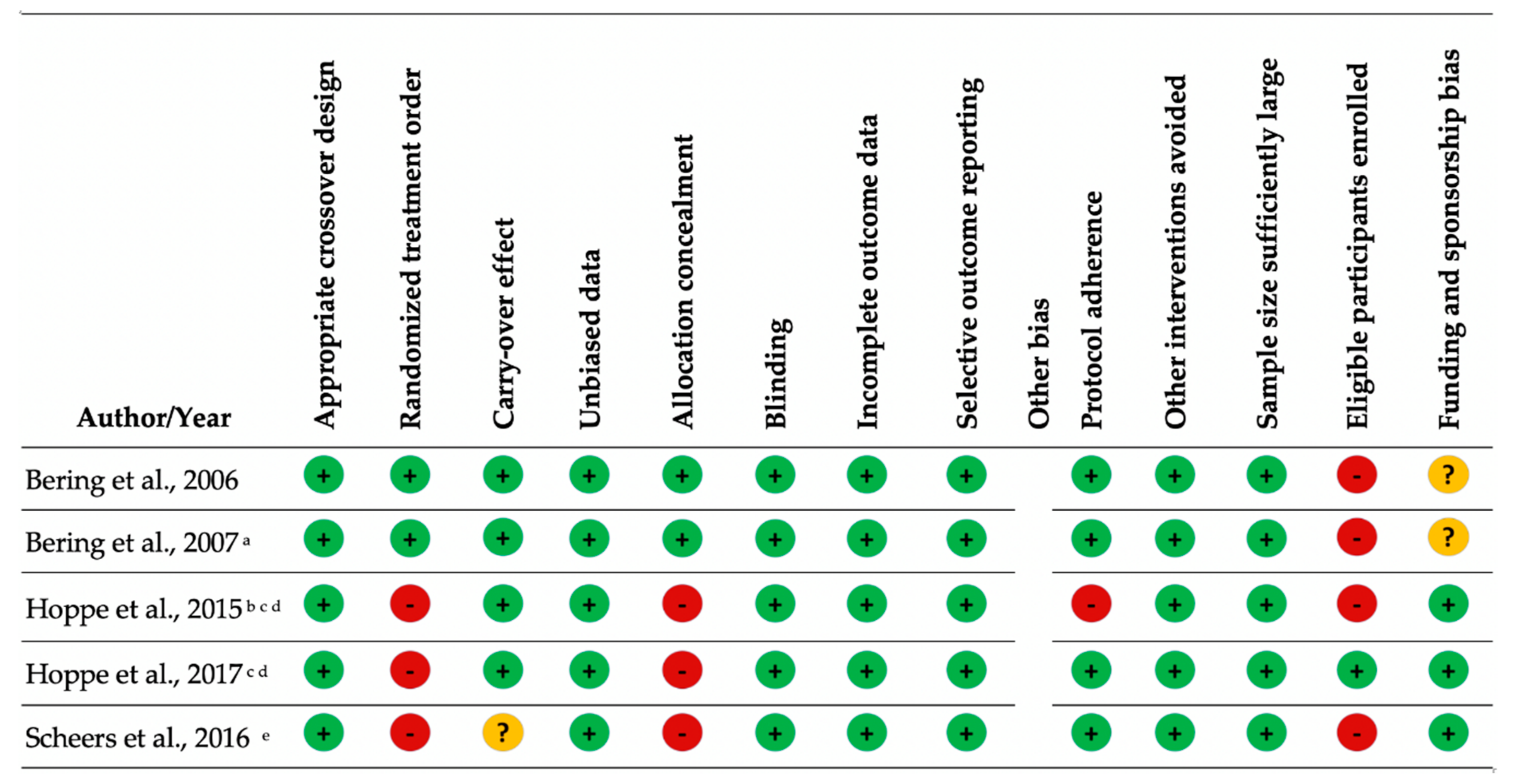
2.4. Assessment Methodological Quality of Included Studies
2.5. Data Synthesis
2.6. Meta-Analysis
3. Results
3.1. Description of Selected Articles
3.2. Bias
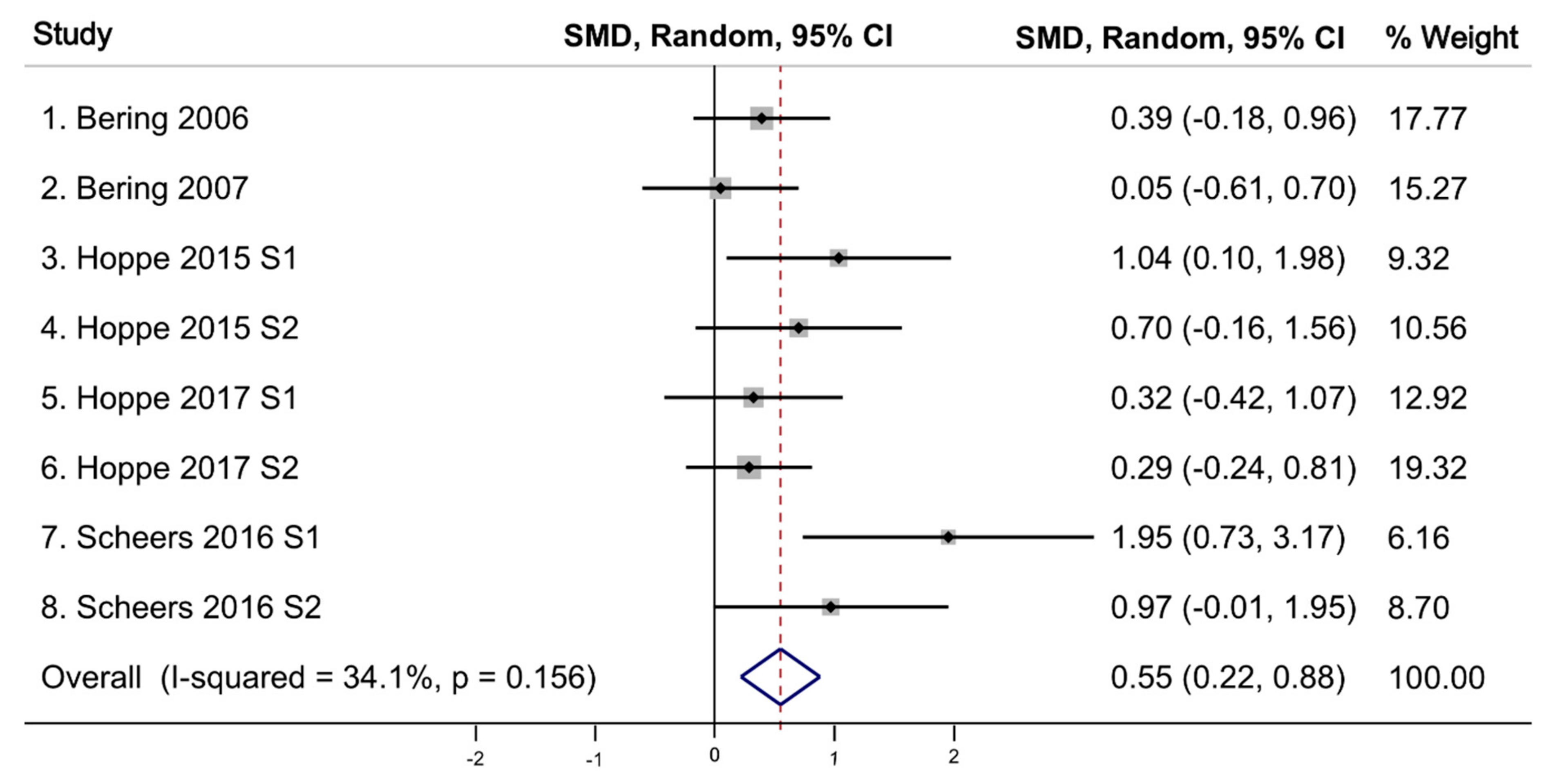
3.3. Iron Absorption
3.4. Iron Status Markers and Hemoglobin
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
References
- Stevens, G.A.; Finucane, M.M.; De-Regil, L.M.; Paciorek, C.J.; Flaxman, S.R.; Branca, F.; Peña-Rosas, J.P.; Bhutta, P.Z.A.; Ezzati, P.M.; Behalf of Nutrition Impact Model Study Group. Global, regional, and national trends in haemoglobin concentration and prevalence of total and severe anaemia in children and pregnant and non-pregnant women for 1995–2011: A systematic analysis of population-representative data. Lancet Glob. Health 2013, 1, E16–E25. [Google Scholar] [PubMed]
- Lawson, J.A. Comparative quantification of health risks. Global and regional burden of disease attributable to selected major risk factors. Can. J. Public Health-Rev. Can. Sante Publique 2006, 97, 319. [Google Scholar]
- Balarajan, Y.; Ramakrishnan, U.; Ozaltin, E.; Shankar, A.H.; Subramanian, S.V. Anaemia in low-income and middle-income countries. Lancet 2011, 378, 2123–2135. [Google Scholar] [CrossRef]
- Stolzfus, R.J.; Mullany, L.; Black, R.E. Iron deficiency aneamia. In Comparative Quantification of Health Risks: Global and Regional Burden of Disease Attributable to Selected Major Risk Factors; Ezzati, M., Lopez, A.D., Rodgers, A., Murray, C.J.L., Eds.; World Health Organization: Geneva, Switzerland, 2004; pp. 163–210. [Google Scholar]
- WHO. Global Health Estimates 2016: Deaths by Cause, Age, Sex, by Country and by Region, 2000–2016; World Health Organization: Geneva, Switzerland, 2018. [Google Scholar]
- Zimmermann, M.B.; Zeder, C.; Muthayya, S.; Winichagoon, P.; Chaouki, N.; Aeberli, I.; Hurrell, R.F. Adiposity in women and children from transition countries predicts decreased iron absorption, iron deficiency and a reduced response to iron fortification. Int. J. Obes. 2008, 32, 1098–1104. [Google Scholar] [CrossRef] [PubMed]
- Beck, K.L.; Conlon, C.A.; Kruger, R.; Coad, J. Dietary determinants of and possible solutions to iron deficiency for young women living in industrialized countries: A review. Nutrients 2014, 6, 3747–3776. [Google Scholar] [CrossRef] [PubMed]
- Tolkien, Z.; Stecher, L.; Mander, A.P.; Pereira, D.I.; Powell, J.J. Ferrous sulfate supplementation causes significant gastrointestinal side-effects in adults: A systematic review and meta-analysis. PLoS ONE 2015, 10, e0117383. [Google Scholar] [CrossRef]
- Jaeggi, T.; Kortman, G.A.; Moretti, D.; Chassard, C.; Holding, P.; Dostal, A.; Boekhorst, J.; Timmerman, H.M.; Swinkels, D.W.; Tjalsma, H.; et al. Iron fortification adversely affects the gut microbiome, increases pathogen abundance and induces intestinal inflammation in Kenyan infants. Gut 2015, 64, 731–742. [Google Scholar] [CrossRef]
- Jeroense, F.M.D.; Michel, L.; Zeder, C.; Herter-Aeberli, I.; Zimmermann, M.B. Consumption of Galacto-Oligosaccharides Increases Iron Absorption from Ferrous Fumarate: A Stable Iron Isotope Study in Iron-Depleted Young Women. J. Nutr. 2019, 149, 738–746. [Google Scholar] [CrossRef]
- Asemi, Z.; Esmaillzadeh, A. Effect of daily consumption of probiotic yoghurt on serum levels of calcium, iron and liver enzymes in pregnant women. Int. J. Prev. Med. 2013, 4, 949–955. [Google Scholar]
- Bering, S.; Suchdev, S.; Sjøltov, L.; Berggren, A.; Tetens, I.; Bukhave, K. A lactic acid-fermented oat gruel increases non-haem iron absorption from a phytate-rich meal in healthy women of childbearing age. Br. J. Nutr. 2006, 96, 80–85. [Google Scholar] [CrossRef]
- Hoppe, M.; Onning, G.; Hulthen, L. Freeze-dried Lactobacillus plantarum 299v increases iron absorption in young females-Double isotope sequential single-blind studies in menstruating women. PLoS ONE 2017, 12, e0189141. [Google Scholar] [CrossRef] [PubMed]
- Mack, D.R.; Ahrne, S.; Hyde, L.; Wei, S.; Hollingsworth, M.A. Extracellular MUC3 mucin secretion follows adherence of Lactobacillus strains to intestinal epithelial cells in vitro. Gut 2003, 52, 827–833. [Google Scholar] [CrossRef] [PubMed]
- Gonzalez, A.; Gálvez, N.; Martín, J.; Reyes, F.; Pérez-Victoria, I.; Dominguez-Vera, J.M. Identification of the key excreted molecule by Lactobacillus fermentum related to host iron absorption. Food Chem. 2017, 228, 374–380. [Google Scholar] [CrossRef] [PubMed]
- Wells, J.M. Immunomodulatory mechanisms of lactobacilli. Microb. Cell Fact. 2011, 10 (Suppl. S1), S17. [Google Scholar] [CrossRef]
- Hill, C.; Guarner, F.; Reid, G.; Gibson, G.R.; Merenstein, D.J.; Pot, B.; Morelli, L.; Canani, R.B.; Flint, H.J.; Salminen, S.; et al. Expert consensus document. The International Scientific Association for Probiotics and Prebiotics consensus statement on the scope and appropriate use of the term probiotic. Nat. Rev. Gastroenterol. Hepatol. 2014, 11, 506–514. [Google Scholar] [CrossRef]
- Hoppe, M.; Önning, G.; Berggren, A.; Hulthén, L. Probiotic strain Lactobacillus plantarum 299v increases iron absorption from 2 an iron-supplemented fruit drink: A double-isotope cross-over single-blind 3 study in women of reproductive age-ERRATUM. Br. J. Nutr. 2015, 114, 1195–1202. [Google Scholar] [CrossRef]
- Bering, S.; Sjøltov, L.; Wrisberg, S.S.; Berggren, A.; Alenfall, J.; Jensen, M.; Højgaard, L.; Tetens, I.; Bukhave, K. Viable, lyophilized lactobacilli do not increase iron absorption from a lactic acid-fermented meal in healthy young women, and no iron absorption occurs in the distal intestine. Br. J. Nutr. 2007, 98, 991–997. [Google Scholar] [CrossRef]
- Scheers, N.; Rossander-Hulthen, L.; Torsdottir, I.; Sandberg, A.S. Increased iron bioavailability from lactic-fermented vegetables is likely an effect of promoting the formation of ferric iron (Fe(3+)). Eur. J. Nutr. 2016, 55, 373–382. [Google Scholar] [CrossRef]
- Agustina, R.; Bovee-Oudenhoven, I.M.; Lukito, W.; Fahmida, U.; van de Rest, O.; Zimmermann, M.B.; Firmansyah, A.; Wulanti, R.; Albers, R.; van den Heuvel, E.G.; et al. Probiotics Lactobacillus reuteri DSM 17938 and Lactobacillus casei CRL 431 modestly increase growth, but not iron and zinc status, among Indonesian children aged 1-6 years. J. Nutr. 2013, 143, 1184–1193. [Google Scholar] [CrossRef]
- Endo, H.; Higurashi, T.; Hosono, K.; Sakai, E.; Sekino, Y.; Iida, H.; Sakamoto, Y.; Koide, T.; Takahashi, H.; Yoneda, M.; et al. Efficacy of Lactobacillus casei treatment on small bowel injury in chronic low-dose aspirin users: A pilot randomized controlled study. J. Gastroenterol. 2011, 46, 894–905. [Google Scholar] [CrossRef]
- Korcok, D.J.; Tršić-Milanović, N.A.; Ivanović, N.D.; Đorđević, B.I. Development of Probiotic Formulation for the Treatment of Iron Deficiency Anemia. Chem. Pharm. Bull. 2018, 66, 347–352. [Google Scholar] [CrossRef] [PubMed]
- Silva, M.R.; Dias, G.; Ferreira, C.L.; Franceschini, S.C.; Costa, N.M. Growth of preschool children was improved when fed an iron-fortified fermented milk beverage supplemented with Lactobacillus acidophilus. Nutr. Res. 2008, 28, 226–232. [Google Scholar] [CrossRef] [PubMed]
- Asemi, Z.; Bahmani, S.; Shakeri, H.; Jamal, A.; Faraji, A.-M. Effect of multispecies probiotic supplements on serum minerals, liver enzymes and blood pressure in patients with type 2 diabetes. Int. J. Diabetes Dev. Ctries. 2015, 35, 90–95. [Google Scholar] [CrossRef]
- Toews, L.C. Compliance of systematic reviews in veterinary journals with Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) literature search reporting guidelines. J. Med. Libr. Assoc. 2017, 105, 233–239. [Google Scholar] [CrossRef] [PubMed]
- Higgins, J.P.; Altman, D.G.; Gøtzsche, P.C.; Jüni, P.; Moher, D.; Oxman, A.D.; Savovic, J.; Schulz, K.F.; Weeks, L.; Sterne, J.A.; et al. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ 2011, 343, d5928. [Google Scholar] [CrossRef] [PubMed]
- Ding, H.; Hu, G.L.; Zheng, X.Y.; Chen, Q.; Threapleton, D.E.; Zhou, Z.H. The method quality of cross-over studies involved in Cochrane Systematic Reviews. PLoS ONE 2015, 10, e0120519. [Google Scholar] [CrossRef]
- Rosen, G.M.; Morrissette, S.; Larson, A.; Stading, P.; Griffin, K.H.; Barnes, T.L. Use of a Probiotic to Enhance Iron Absorption in a Randomized Trial of Pediatric Patients Presenting with Iron Deficiency. J. Pediatr. 2019, 207, 192–197.e1. [Google Scholar] [CrossRef]
- Goh, J.X.; Hall, J.A.; Rosenthal, R. Mini Meta-Analysis of Your Own Studies: Some Arguments on Why and a Primer on How. Soc. Personal. Psychol. Compass 2016, 10, 535–549. [Google Scholar] [CrossRef]
- Lotfaliany, M.; Akbarpour, S.; Zafari, N.; Mansournia, M.A.; Asgari, S.; Azizi, F.; Hadaegh, F.; Khalili, D. World Bank Income Group, Health Expenditure or Cardiometabolic Risk Factors? A Further Explanation of the Wide Gap in Cardiometabolic Mortality Between Worldwide Countries: An Ecological Study. Int. J. Endocrinol. Metab. 2018, 16, e59946. [Google Scholar] [CrossRef]
- Ganz, T.; Nemeth, E. Hepcidin and iron homeostasis. Biochim. Biophys. Acta 2012, 1823, 1434–1443. [Google Scholar] [CrossRef]
- Brise, H.; Hallberg, L. Absorbability of different iron compounds. Acta Med. Scand. Suppl. 1962, 376, 23–37. [Google Scholar] [CrossRef] [PubMed]
- Gomez-Ramirez, S.; Brilli, E.; Tarantino, G.; Muñoz, M. Sucrosomial((R)) Iron: A New Generation Iron for Improving Oral Supplementation. Pharmaceuticals 2018, 11, 97. [Google Scholar] [CrossRef] [PubMed]
| Study/Year | Subjects | Baseline Iron Status | Design/ Blinding | Study Groups or Product | Iron Compound | Intervention Delivery Method, Frequency and Duration | Effect on Iron Status or Iron Absorption | Included in Meta-Analysis |
|---|---|---|---|---|---|---|---|---|
| RCTs and Nonrandomized Clinical Trials | ||||||||
| Agustina et al., 2013 [21] | Indonesia N = 494 Children Age: 1–6 Healthy Non-breastfed | IDA n (%) Group 1: 12 (10) Group 2: 17 (14) Group 3: 13 (11) Group 4: 14 (11) | RCT double-blinded | Group 1: Placebo–Low calcium, ~50 mg/d Group 2: Placebo–Regular calcium, ~440 mg/d Group 3: L. casei 431 1: 5 × 108 CFU/d plus regular calcium Group 4: L. reuteri 17,938 5 × 108 CFU/d plus regular calcium | Not reported | 180 mL low-lactose milk and coated straws Twice daily across 6 months | ↔ Hb ↔ Hct ↔ serum ferritin↔ sTfR | No |
| Asemi et al., 2013 [11] | Iran N = 70 Pregnant, third trimester Age: 18–30 | Iron (mg/dL) Group 1: 124 ± 88.3 Group 2: 118 ± 61.8 | RCT single-blinded | Group 1: Placebo Group 2: L. acidophilus 1 × 107 CFU, B. lactis 1 × 107 CFU | Not reported | 200 g yogurt Daily across 9 weeks | ↔ serum iron | No |
| Asemi et al., 2015 [25] | Iran N = 58 Diabetic patients, not pregnant Age: 52.1 ± 6.9 (Group 1) 49.6 ± 9.9 (Group 2) Female % not reported | Iron (mg/dL) Group 1: 66.1 ± 33 Group 2: 69.5 ± 62.9 | RCT double-blinded | Group 1: Placebo Group 2: L. acidophilus 2 × 109 CFU, L. casei 7 × 109 CFU, L. bulgaricus 2 × 108 CFU, B. breve 2 × 108 CFU, B. longum 7 × 109 CFU, S. thermophiles 1.5 × 109 CFU | Not reported | Capsule Daily across 8 weeks | ↔ serum iron | No |
| Endo et al., 2011 [22] | Japan N = 25 Female 28% Age: 70.3 ± 6.2 (Group 1) 73.9 ± 8.5 (Group 2) Unexplained IDA on chronic low-dose aspirin | Hb (g/dl) Group 1: 10.9 ± 1.7 Group 2: 10.2 ± 2 | RCT single-blinded | Group 1: No placebo Group 2: L. casei 45 × 108–63 × 10 CFU | Not reported | Powder Daily for 3 months | ↔ Hb (between groups) ↑ Hb (within L. casei group) | No |
| Korcok et al., 2018 [23] | Serbia N = 20 Female 100% Healthy | Not reported | Two group comparison | Group 1: Placebo Group 2: L. plantarum 299v 1.1 × 109 CFU | Sucrosomal iron 10 mg | Capsule plus supplemental iron and 15 mg vitamin C 7 consecutive mornings Empty stomach | ↑ serum iron a↔ serum ferritin ↔ TIBC ↔ Hb | No |
| Rosen et al., 2019 [29] | United States N = 52 Children with mild iron deficiency (ferritin < 50 ng/mL), and insomnia or restless sleep, 58% had psychiatric and/or mental health diagnosis Age: 5–18 | Not reported | RCT Double-blinded | Group 1: placebo Group 2: L. plantarum 299v 1.7 × 1010 CFU | Ferrous sulphate 325 mg or ferrous sulphate 15 mg elemental iron/mL (if children < 20 kg, dose of 3 mg/kg/d up to maximum dose 65 mg; in children > 20 kg range 0.4–3 mg/kg/d) | Capsule plus supplemental iron and vitamin C (125 mg < 5 years of age and 250 mg > 5 years of age) 6–8 weeks No milk or food within 2 h of medication | ↔ serum ferritin | No |
| Silva et al., 2008 [24] | Brazil N = 109 Children Age: 20–62 months | Iron (µg/dL) Group 1: 48.9 ± 9.8 Group 2: 49 ± 10.5 Hb (g/dL) Group 1: 12.2 ± 0.7 G 2: 12.1 ± 0.7 Ferritin (ng/mL) Group 1: 41.2 ± 21.4 Group 2: 38.5 ± 19 | Two group comparison | Group 1: Placebo Group 2: L. acidophilus 108 CFU | Not reported | 80 mL whole milk beverage with 3 mg iron 1.2 g culture of L. acidophilus Daily between lunch and afternoon snack Monday to Friday during 101 class days | Between groups ↔ Hb Within L. acidophilus group ↓ Hb ↓ Hct ↓ serum iron ↓ serum ferritin Within Placebo group ↓ Hb ↓ Hct ↔ serum iron ↑ serum ferritin | No |
| Cross-over Studies | ||||||||
| Bering et al., 2006 [12] | Denmark N = 24 Female 100% Age: 25 ± 4 low iron stores not anemic, not pregnant, not lactating | Hb (g/L) Range: 111–137 Ferritin (µg/L) Range 12–40 | Cross-over double-blinded | Product A: L. plantarum 299v 1.1 × 109 CFU, fermented gruel Product B: pasteurized Product A Product C: non-fermented gruel (pH adjusted with lactic acid) Product D: control meal non-fermented gruel with added organic acids (lactic acid and acetic acid) | Not reported | 100 g oat gruel Product A, B & D: non-heme Fe 2.8 mg Product C: non-heme Fe 2.5 mg Twice on four consecutive mornings 12 h of fasting | ↑ non-heme iron absorption | Yes |
| Bering et al., 2007 [19] | Denmark N = 18 Female 100% Age: 22 ± 3 low iron stores not anemic, not pregnant, not lactating | Hb (g/L) Range: 116–135 Ferritin (µg/L) Range 13–29 | Cross-over double-blinded | Product A: heat-inactivated lactic acid gruel Product B: viable lypholized L. Plantarum 299v 1.1 × 109 CFU, heat-inactivated lactic acid gruel | Not reported | 100 g fermented, pasteurized oat gruel plus 140 g whole-wheat roll Product A & B: non-heme Fe 1.9 mg Twice on two consecutive mornings12 h of fasting | ↔ non-heme iron absorption | Yes |
| Hoppe et al., 2015 [18] | Sweden N = 10 (Study 1) N = 11 (Study 2) Female 100% Healthy Age: 24.3, range 20–40 (Total sample) | Iron (µmol/L) Study 1: 15 ± 6 Study 2: 18 ± 7 Hb (g/L) Study 1: 138 ± 8 Study 2: 135 ± 9 Ferritin (µg/L) Study 1: 33 ± 13 Study 2: 33 ± 14 | Cross-over single-blinded | Product A: Placebo Product B: L. plantarum 299v 1.3 × 109 CFU (Study 1) L. plantarum 299v 1.7 × 1010 CFU (Study 2) | Ferrous lactate dehydrate 4.2 mg | 200 mL fruit drink with fermented oat base plus iron (2.1 mg/100 mL) Product A: non-heme Fe 5.2 mg (Study 1) non-heme Fe 5.4 mg (Study 2) Product B: non-heme Fe 4.6 mg (Study 1) non-heme Fe 5.2 mg (Study 2) 4 consecutive days Empty stomach | ↑ non-heme iron absorption (Study 1) ↔ non-heme iron absorption (Study 2) | Yes |
| Hoppe et al., 2017 [13] | Sweden N = 14 (Study 1) N = 28 (Study 2) Female 100% Age: 26.2 ± 4.6 (Study 1) 25.6 ± 6.8 (Study 2) Healthy | Iron (µmol/L) Study 1: 15 ± 5 Study 2: 16 ± 7 Hb (g/L) Study 1: 135 ± 6 Study 2: 134 ± 10 Ferritin (µg/L) Study 1: 30 ± 21 Study 2: 27 ± 14 | Cross-over single-blinded | Product A: Placebo Product B: L. plantarum 299v 1010 CFU (Study 1 & 2) | Not reported | Capsule plus two wheat breakfast buns made with fermented dough Product A & B: non-heme Fe 4.2 mg 4 consecutive days Empty stomach | ↑ non-heme iron absorption (Study 1) ↑ non-heme iron absorption (Study 2) | Yes |
| Scheers et al., 2016 [20] | Sweden N = 8 low-phytate (Study 1) N = 9 high-phytate (Study 2) Female 35% Age: 21–54 Healthy | Not reported | Cross-over | Product A: Fresh vegetables Product B: L. plantarum 299v 2.4 × 109 CFU fermented vegetables | Not reported | 140 g bread rolls (low phytate had wheat flour; or high phytate had wheat bran and wheat flour) plus 100 g fermented or fresh vegetables Low phytate non-heme Fe 4.4 mg High phytate non-heme Fe 4.0 mg Alternate mornings on 4 consecutive days Overnight fast | ↑ non-heme iron absorption | Yes |
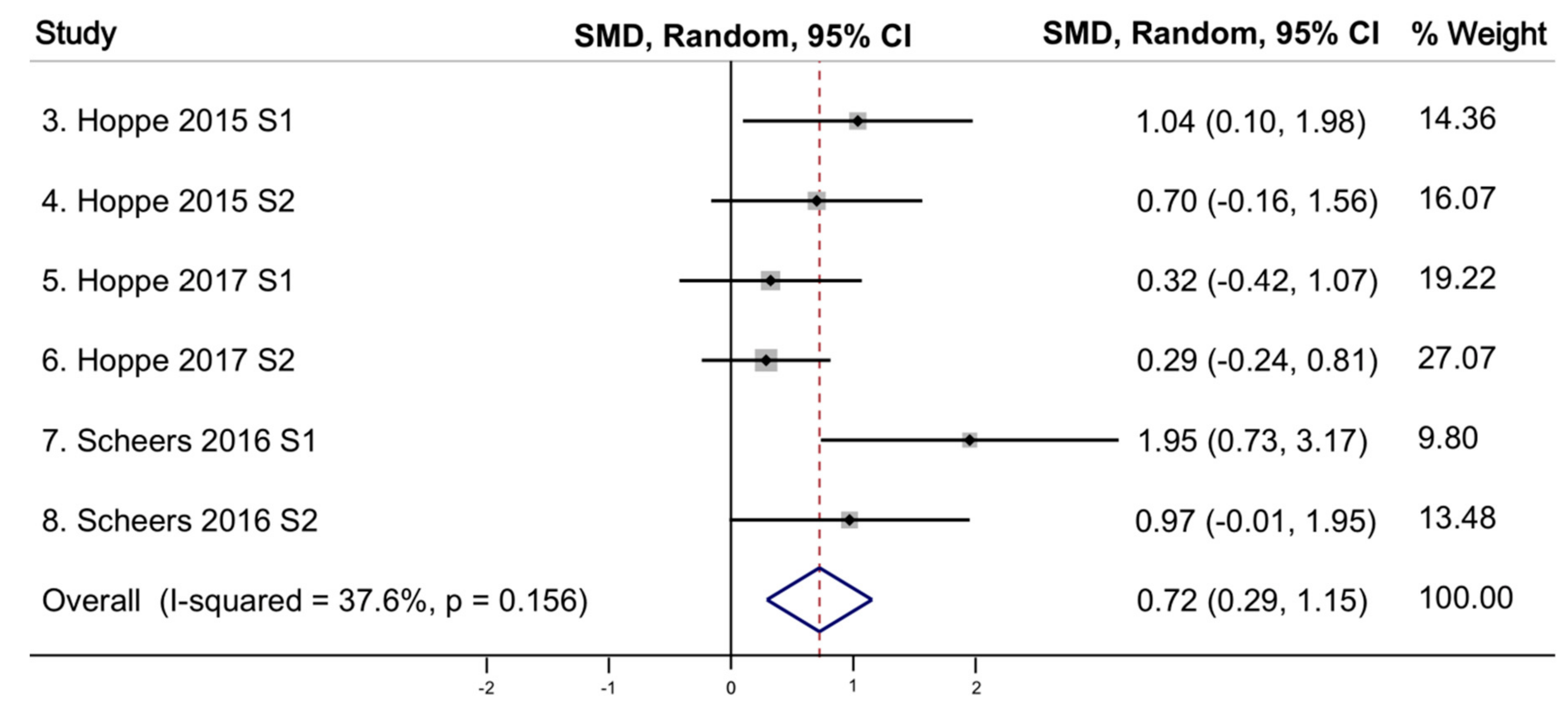
| Number of Studies | Model | Effect: Pooled SMD | 95% CI | p-Value | Q | p-Value | Tau Squared |
|---|---|---|---|---|---|---|---|
| 8 | random | 0.55 | 0.22, 0.88 | 0.001 | 10.62 | 0.156 | 0.0747 |
| 6 a | random | 0.72 | 0.29, 1.15 | 0.001 | 8.01 | 0.156 | 0.1058 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Vonderheid, S.C.; Tussing-Humphreys, L.; Park, C.; Pauls, H.; OjiNjideka Hemphill, N.; LaBomascus, B.; McLeod, A.; Koenig, M.D. A Systematic Review and Meta-Analysis on the Effects of Probiotic Species on Iron Absorption and Iron Status. Nutrients 2019, 11, 2938. https://doi.org/10.3390/nu11122938
Vonderheid SC, Tussing-Humphreys L, Park C, Pauls H, OjiNjideka Hemphill N, LaBomascus B, McLeod A, Koenig MD. A Systematic Review and Meta-Analysis on the Effects of Probiotic Species on Iron Absorption and Iron Status. Nutrients. 2019; 11(12):2938. https://doi.org/10.3390/nu11122938
Chicago/Turabian StyleVonderheid, Susan C., Lisa Tussing-Humphreys, Chang Park, Heather Pauls, Nefertiti OjiNjideka Hemphill, Bazil LaBomascus, Andrew McLeod, and Mary Dawn Koenig. 2019. "A Systematic Review and Meta-Analysis on the Effects of Probiotic Species on Iron Absorption and Iron Status" Nutrients 11, no. 12: 2938. https://doi.org/10.3390/nu11122938
APA StyleVonderheid, S. C., Tussing-Humphreys, L., Park, C., Pauls, H., OjiNjideka Hemphill, N., LaBomascus, B., McLeod, A., & Koenig, M. D. (2019). A Systematic Review and Meta-Analysis on the Effects of Probiotic Species on Iron Absorption and Iron Status. Nutrients, 11(12), 2938. https://doi.org/10.3390/nu11122938




