Vegetarian Diets and Medical Expenditure in Taiwan—A Matched Cohort Study
Abstract
1. Introduction
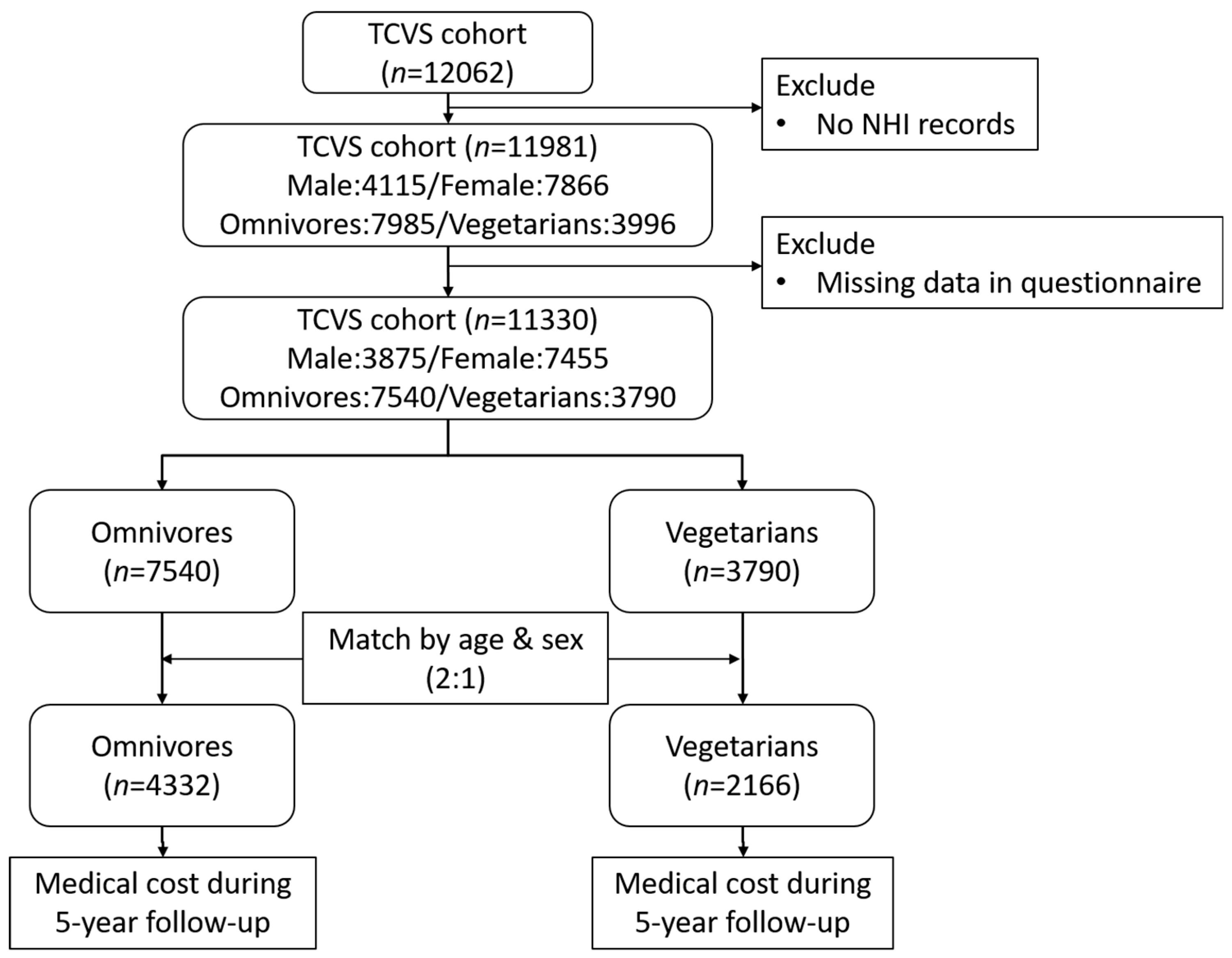
2. Materials and Methods
2.1. The Tzu Chi Vegetarian Study
2.2. Assessment of Healthcare Utilization and Expenditure
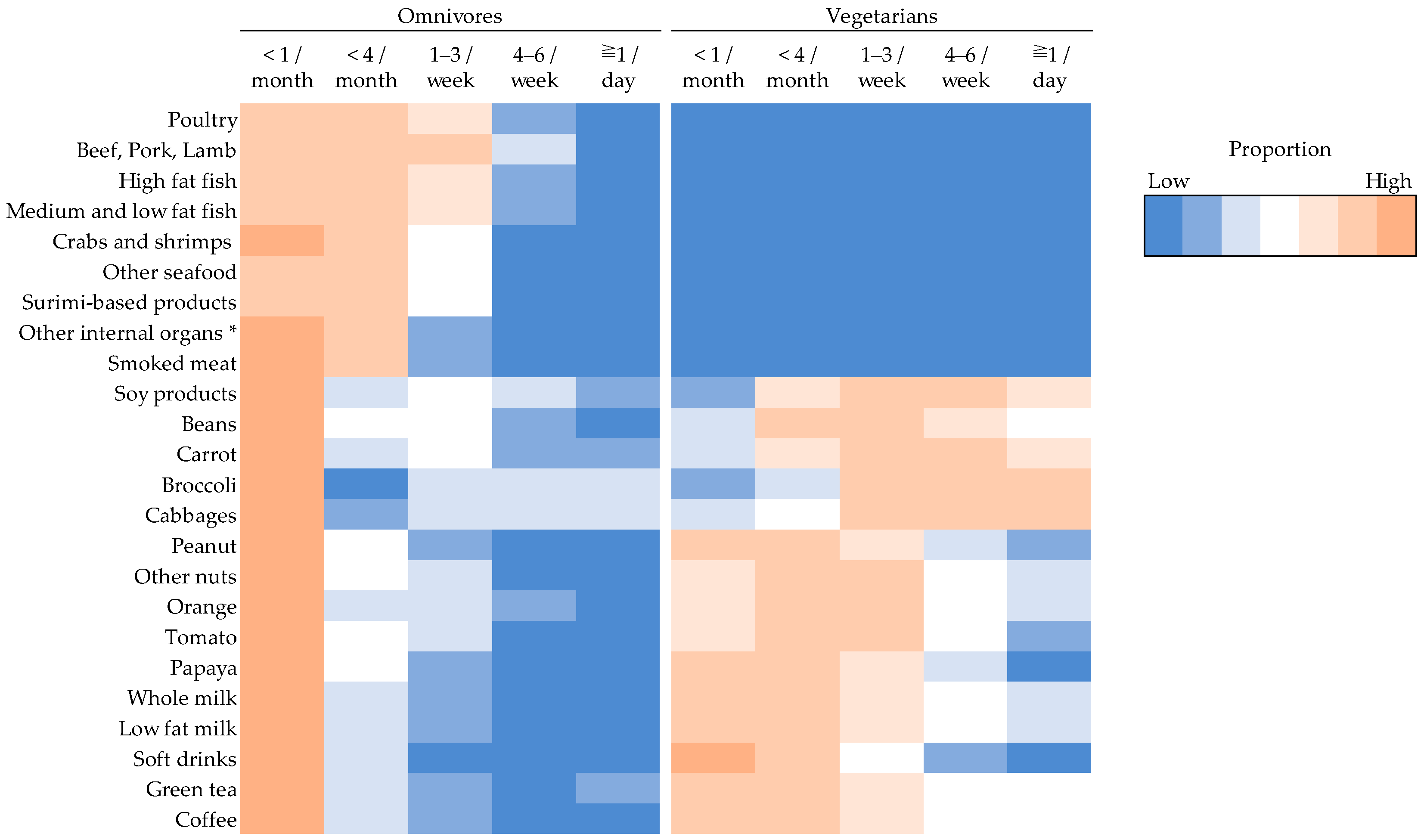
2.3. Assessment of Diet and Other Covariates
2.4. Statistical Analysis
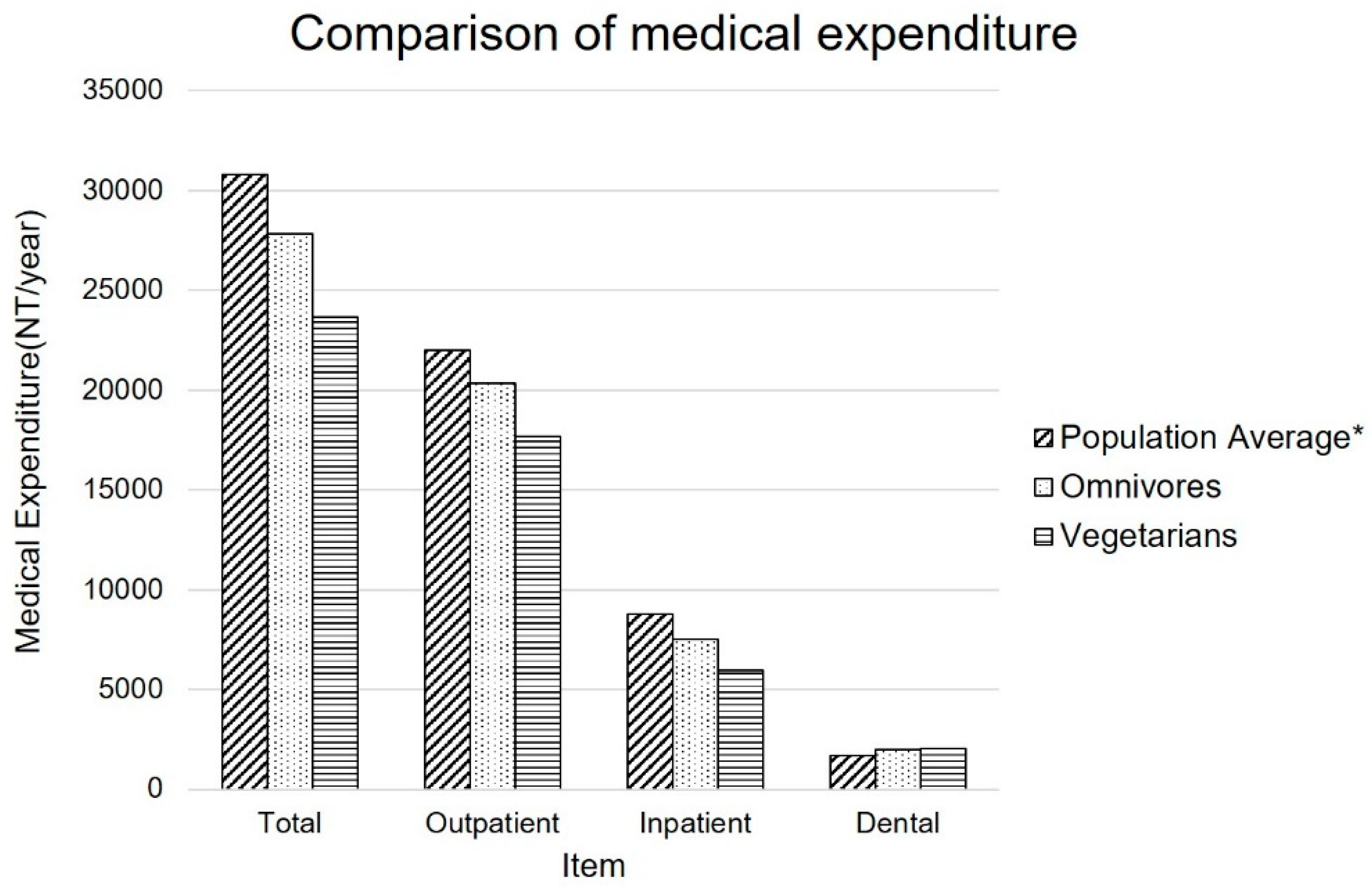
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Institute for Health Metrics and Evaluation (IHME). The Findings from the Global Burden of Disease Study 2017; IHME: Seattle, WA, USA, 2018. [Google Scholar]
- Taiwan | Institute for Health Metrics and Evaluation. Available online: http://www.healthdata.org/taiwan (accessed on 9 May 2019).
- Bauer, U.E.; Briss, P.A.; Goodman, R.A.; Bowman, B.A. Prevention of chronic disease in the 21st century: Elimination of the leading preventable causes of premature death and disability in the USA. Lancet 2014, 384, 45–52. [Google Scholar] [CrossRef]
- Warner, K.E.; Hodgson, T.A.; Carroll, C.E. Medical costs of smoking in the United States: Estimates, their validity, and their implications. Tob. Control 1999, 8, 290–300. [Google Scholar] [CrossRef] [PubMed]
- Tsalapati, K.; Vardavas, C.I.; Athanasakis, K.; Thireos, E.; Vozikis, A.; Pavi, E.; Behrakis, P.; Kyriopoulos, I. Going up in ashes? Smoking-attributable morbidity, hospital admissions and expenditure in Greece. Eur. J. Public Health 2014, 24, 477–479. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Xu, X.; Bishop, E.E.; Kennedy, S.M.; Simpson, S.A.; Pechacek, T.F. Annual healthcare spending attributable to cigarette smoking: An update. Am. J. Prev. Med. 2015, 48, 326–333. [Google Scholar] [CrossRef] [PubMed]
- Scarborough, P.; Bhatnagar, P.; Wickramasinghe, K.K.; Allender, S.; Foster, C.; Rayner, M. The economic burden of ill health due to diet, physical inactivity, smoking, alcohol and obesity in the UK: An update to 2006-07 NHS costs. J. Public Health (Oxf.) 2011, 33, 527–535. [Google Scholar] [CrossRef]
- Sacks, J.J.; Gonzales, K.R.; Bouchery, E.E.; Tomedi, L.E.; Brewer, R.D. 2010 National and State Costs of Excessive Alcohol Consumption. Am. J. Prev Med. 2015, 49, e73–e79. [Google Scholar] [CrossRef]
- Oldridge, N.B. Economic burden of physical inactivity: Healthcare costs associated with cardiovascular disease. Eur. J. Cardiovasc. Prev. Rehabilit. 2008, 15, 130–139. [Google Scholar] [CrossRef]
- Lee, I.M.; Shiroma, E.J.; Lobelo, F.; Puska, P.; Blair, S.N.; Katzmarzyk, P.T. Effect of physical inactivity on major non-communicable diseases worldwide: An analysis of burden of disease and life expectancy. Lancet 2012, 380, 219–229. [Google Scholar] [CrossRef]
- Ding, D.; Lawson, K.D.; Kolbe-Alexander, T.L.; Finkelstein, E.A.; Katzmarzyk, P.T.; van Mechelen, W.; Pratt, M. The economic burden of physical inactivity: A global analysis of major non-communicable diseases. Lancet 2016, 388, 1311–1324. [Google Scholar] [CrossRef]
- Barnard, N.D.; Nicholson, A.; Howard, J.L. The medical costs attributable to meat consumption. Prev. Med. 1995, 24, 646–655. [Google Scholar] [CrossRef]
- Sofi, F.; Macchi, C.; Abbate, R.; Gensini, G.F.; Casini, A. Mediterranean diet and health. Biofactors 2013, 39, 335–342. [Google Scholar] [CrossRef] [PubMed]
- Le, L.T.; Sabate, J. Beyond meatless, the health effects of vegan diets: Findings from the Adventist cohorts. Nutrients 2014, 6, 2131–2147. [Google Scholar] [CrossRef] [PubMed]
- Tsai, A.G.; Williamson, D.F.; Glick, H.A. Direct medical cost of overweight and obesity in the USA: A quantitative systematic review. Obes. Rev. 2011, 12, 50–61. [Google Scholar] [CrossRef] [PubMed]
- Pan, W.H.; Yeh, W.T.; Chen, H.J.; Chuang, S.Y.; Chang, H.Y.; Chen, L.; Wahlqvist, M.L. The U-shaped relationship between BMI and all-cause mortality contrasts with a progressive increase in medical expenditure: A prospective cohort study. Asia. Pac. J. Clin. Nutr. 2012, 21, 577–587. [Google Scholar] [PubMed]
- Aaron, K.J.; Colantonio, L.D.; Deng, L.; Judd, S.E.; Locher, J.L.; Safford, M.M.; Cushman, M.; Kilgore, M.L.; Becker, D.J.; Muntner, P. Cardiovascular Health and Healthcare Utilization and Expenditures Among Medicare Beneficiaries: The REasons for Geographic And Racial Differences in Stroke (REGARDS) Study. J. Am. Heart Assoc. 2017, 6, e005106. [Google Scholar] [CrossRef] [PubMed]
- Orlich, M.J.; Jaceldo-Siegl, K.; Sabate, J.; Fan, J.; Singh, P.N.; Fraser, G.E. Patterns of food consumption among vegetarians and non-vegetarians. Br. J. Nutr. 2014, 112, 1644–1653. [Google Scholar] [CrossRef]
- Ferdowsian, H.R.; Barnard, N.D. Effects of plant-based diets on plasma lipids. Am. J. Cardiol. 2009, 104, 947–956. [Google Scholar] [CrossRef]
- Appleby, P.N.; Davey, G.K.; Key, T.J. Hypertension and blood pressure among meat eaters, fish eaters, vegetarians and vegans in EPIC-Oxford. Public Health Nutr. 2002, 5, 645–654. [Google Scholar] [CrossRef]
- Alewaeters, K.; Clarys, P.; Hebbelinck, M.; Deriemaeker, P.; Clarys, J.P. Cross-sectional analysis of BMI and some lifestyle variables in Flemish vegetarians compared with non-vegetarians. Ergonomics 2005, 48, 1433–1444. [Google Scholar] [CrossRef]
- Tonstad, S.; Butler, T.; Yan, R.; Fraser, G.E. Type of vegetarian diet, body weight, and prevalence of type 2 diabetes. Diabetes Care 2009, 32, 791–796. [Google Scholar] [CrossRef]
- Fraser, G.E. Vegetarian diets: What do we know of their effects on common chronic diseases? Am. J. Clin. Nutr. 2009, 89, 1607s–1612s. [Google Scholar] [CrossRef] [PubMed]
- Orlich, M.J.; Singh, P.N.; Sabate, J.; Fan, J.; Sveen, L.; Bennett, H.; Knutsen, S.F.; Beeson, W.L.; Jaceldo-Siegl, K.; Butler, T.L.; et al. Vegetarian dietary patterns and the risk of colorectal cancers. JAMA Intern. Med. 2015, 175, 767–776. [Google Scholar] [CrossRef] [PubMed]
- Chiu, T.H.T.; Pan, W.H.; Lin, M.N.; Lin, C.L. Vegetarian diet, change in dietary patterns, and diabetes risk: A prospective study. Nutr. Diabetes 2018, 8, 12. [Google Scholar] [CrossRef] [PubMed]
- Chang, C.M.; Chiu, T.H.T.; Chang, C.C.; Lin, M.N.; Lin, C.L. Plant-Based Diet, Cholesterol, and Risk of Gallstone Disease: A Prospective Study. Nutrients 2019, 11, 335. [Google Scholar] [CrossRef]
- Chiu, T.H.; Lin, M.N.; Pan, W.H.; Chen, Y.C.; Lin, C.L. Vegetarian diet, food substitution, and nonalcoholic fatty liver. Ci Ji Yi Xue Za Zhi 2018, 30, 102–109. [Google Scholar] [CrossRef]
- Chiu, T.H.T.; Liu, C.H.; Chang, C.C.; Lin, M.N.; Lin, C.L. Vegetarian diet and risk of gout in two separate prospective cohort studies. Clin. Nutr. 2019, 27. [Google Scholar] [CrossRef]
- National Health Insurance Research Database. Available online: https://nhird.nhri.org.tw/en/index.html (accessed on 28 September 2018).
- Ho, C.W.S. Taiwan’s healthcare report 2010. EPMA J. 2010, 1, 563–585. [Google Scholar] [CrossRef]
- Chiu, T.H.; Huang, H.Y.; Chen, K.J.; Wu, Y.R.; Chiu, J.P.; Li, Y.H.; Chiu, B.C.; Lin, C.L.; Lin, M.N. Relative validity and reproducibility of a quantitative FFQ for assessing nutrient intakes of vegetarians in Taiwan. Public Health Nutr. 2014, 17, 1459–1466. [Google Scholar] [CrossRef]
- Taiwan Ministry of Health and Welfare. Available online: https://www.mohw.gov.tw (accessed on 2 May 2018).
- Battaglia Richi, E.; Baumer, B.; Conrad, B.; Darioli, R.; Schmid, A.; Keller, U. Health Risks Associated with Meat Consumption: A Review of Epidemiological Studies. Int. J. Vitam. Nutr. Res. 2015, 85, 70–78. [Google Scholar] [CrossRef]
- Daviglus, M.L.; Liu, K.; Pirzada, A.; Yan, L.L.; Garside, D.B.; Wang, R.; Van Horn, L.; Manning, W.G.; Manheim, L.M.; Dyer, A.R.; et al. Relationship of fruit and vegetable consumption in middle-aged men to medicare expenditures in older age: The Chicago Western Electric Study. J. Am. Diet. Assoc. 2005, 105, 1735–1744. [Google Scholar] [CrossRef]
- Lo, Y.T.; Wahlqvist, M.L.; Huang, Y.C.; Lee, M.S. Elderly Taiwanese who spend more on fruits and vegetables and less on animal-derived foods use less medical services and incur lower medical costs. Br. J. Nutr. 2016, 115, 823–833. [Google Scholar] [CrossRef] [PubMed]
- Bouchery, E.E.; Harwood, H.J.; Sacks, J.J.; Simon, C.J.; Brewer, R.D. Economic costs of excessive alcohol consumption in the U.S., 2006. Am. J. Prev. Med. 2011, 41, 516–524. [Google Scholar] [CrossRef] [PubMed]
- Balakrishnan, R.; Allender, S.; Scarborough, P.; Webster, P.; Rayner, M. The burden of alcohol-related ill health in the United Kingdom. J. Public Health (Oxf) 2009, 31, 366–373. [Google Scholar] [CrossRef] [PubMed]
- Stagnitti, M.N. National Health Care Expenses Per Person in the U.S. Civilian Noninstitutionalized Population, 2014. In Statistical Brief (Medical Expenditure Panel Survey (US)); Agency for Healthcare Research and Quality (US): Rockville, MD, USA, 2001. [Google Scholar]
- VanderWeele, T.J. Religion and health in Europe: Cultures, countries, context. Eur. J. Epidemiol. 2017, 32, 857–861. [Google Scholar] [CrossRef]
| Item | Omnivores | Vegetarians |
|---|---|---|
| Number of subjects | 4332 | 2166 |
| Age | 50.5 ± 9.4 | 50.5 ± 9.3 |
| Age Group | ||
| <50 | 2035 (47.0%) | 1030 (47.6%) |
| ≧50 | 2297 (53.0%) | 1136 (52.4%) |
| Sex | ||
| Male | 1548 (35.7%) | 774 (35.7%) |
| Female | 2784 (64.3%) | 1392 (64.3%) |
| Marriage | ||
| No | 372 (9.9%) | 235 (10.8%) |
| Yes | 3905 (90.1%) | 1931 (89.2%) |
| Education | ||
| Elementary school or less | 1025 (23.6%) | 481 (22.2%) |
| Secondary school | 2277 (52.6%) | 1124 (51.9%) |
| College or higher | 1030 (23.8%) | 561 (25.9%) |
| Smoking | ||
| Never | 3672 (84.8%) | 1868 (86.2%) |
| Past | 594 (13.7%) | 290 (13.4%) |
| Current | 66 (1.5%) | 8 (0.4%) |
| Alcohol drinking | ||
| Never | 3713 (85.7%) | 1861 (85.9%) |
| Past | 523 (12.1%) | 292 (13.5%) |
| Current | 96 (2.2%) | 13 (0.6%) |
| Exercise habits | ||
| No | 810 (18.7%) | 464 (21.4%) |
| Yes | 3522 (81.3%) | 1702 (78.6%) |
| Item | Crude | Adjusted † | ||||||
|---|---|---|---|---|---|---|---|---|
| Omnivores | Vegetarians | Savings (%) | p-Value | Omnivores | Vegetarians | Savings (%) | p-Value | |
| Total medical expenditure (NT/per year) | 27,841 ± 976 | 23,656 ± 1381 | 15% | 0.013 * | 25,222 ± 3060 | 20,949 ± 3300 | 17% | 0.011 * |
| Outpatient | ||||||||
| No. of visits (times/per year) | 19.8 ± 0.23 | 17.6 ± 0.28 | - | <0.001 * | - | - | - | - |
| Medical expenditure (NT/per year) | 20,333 ± 607 | 17,679 ± 858 | 13% | 0.012 * | 17,802 ± 1900 | 15,073 ± 2049 | 15% | 0.009 * |
| Inpatient | ||||||||
| No. of visits (times/per year) | 0.14 ± 0.01 | 0.12 ± 0.01 | - | 0.149 | - | - | - | - |
| Medical expenditure (NT/per year) | 7508 ± 617 | 5978 ± 872 | 20% | 0.152 | 7420 ± 1940 | 5876 ± 2092 | 21% | 0.149 |
| Dental | ||||||||
| No. of visits (times/per year) | 1.80 ± 0.03 | 1.83 ± 0.04 | - | 0.566 | - | - | - | - |
| Medical expenditure (NT/per year) | 1995 ± 30 | 2059 ± 42 | −3% | 0.217 | 1749 ± 94 | 1814 ± 101 | −4% | 0.209 |
| Item | <50 years of age (N = 3065) | ≧50 years of age (N = 3433) | Male (N = 2322) | Female (N = 4176) | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Adjusted † | Adjusted † | Adjusted ‡ | Adjusted ‡ | |||||||||
| Omnivores | Vegetarians | Saving (%) | Omnivores | Vegetarians | Saving (%) | Omnivores | Vegetarians | Saving (%) | Omnivores | Vegetarians | Saving (%) | |
| Total medical expenditure (NT/per year) | 19,325 ± 3375 | 15,445 ± 3662 | 20% p = 0.047 * | 31,074 ± 5206 | 26,396 ± 5556 | 15% p = 0.081 | 25,880 ± 3951 | 23,151 ± 4599 | 11% p = 0.391 | 21,131 ± 6761 | 16,106 ± 6911 | 24% p = 0.010 * |
| Outpatient medical expenditure (NT/per year) | 14,999 ± 2421 | 12,245 ± 2627 | 18% p = 0.049 * | 20,315 ± 2995 | 17,608 ± 3196 | 13% p = 0.080 | 18,244 ± 2534 | 17,082 ± 2950 | 6% p = 0.569 | 17,234 ± 4081 | 13,736 ± 4171 | 20% p = 0.003* |
| Inpatient medical expenditure (NT/per year) | 4325 ± 1784 | 3201 ± 1936 | 26% p = 0.275 | 10,759 ± 3508 | 8788 ± 3744 | 18% p = 0.276 | 7636 ± 2435 | 6069 ± 2834 | 21% p = 0.424 | 3897 ± 4384 | 2369 ± 4482 | 39% p = 0.226 |
| Dental medical expenditure (NT/per year) | 1700 ± 122 | 1783 ± 132 | −5% p = 0.241 | 1791 ± 146 | 1841 ± 156 | −3% p = 0.512 | 1797 ± 109 | 1939 ± 127 | −8% p = 0.106 | 1622 ± 223 | 1648 ± 228 | −2% p = 0.690 |
| Disease | Omnivores | Vegetarians | Savings (%) | p-Value |
|---|---|---|---|---|
| Hypertension | 3819 ± 683 | 2762 ± 737 | 28% | 0.005 * |
| Diabetes | 2529 ± 643 | 2079 ± 694 | 18% | 0.209 |
| Dyslipidemia | 1333 ± 273 | 914 ± 295 | 31% | 0.006 * |
| Cerebrovascular disease | 561 ± 943 | 252 ± 1018 | 55% | 0.557 |
| Renal disease | 1831 ± 1568 | 305 ± 1692 | 84% | 0.081 |
| Coronary heart disease | 1995 ± 430 | 1553 ± 464 | 22% | 0.065 |
| Depression | 794 ± 254 | 410 ± 274 | 48% | 0.007 * |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lin, C.-L.; Wang, J.-H.; Chang, C.-C.; Chiu, T.H.T.; Lin, M.-N. Vegetarian Diets and Medical Expenditure in Taiwan—A Matched Cohort Study. Nutrients 2019, 11, 2688. https://doi.org/10.3390/nu11112688
Lin C-L, Wang J-H, Chang C-C, Chiu THT, Lin M-N. Vegetarian Diets and Medical Expenditure in Taiwan—A Matched Cohort Study. Nutrients. 2019; 11(11):2688. https://doi.org/10.3390/nu11112688
Chicago/Turabian StyleLin, Chin-Lon, Jen-Hung Wang, Chia-Chen Chang, Tina H.T. Chiu, and Ming-Nan Lin. 2019. "Vegetarian Diets and Medical Expenditure in Taiwan—A Matched Cohort Study" Nutrients 11, no. 11: 2688. https://doi.org/10.3390/nu11112688
APA StyleLin, C.-L., Wang, J.-H., Chang, C.-C., Chiu, T. H. T., & Lin, M.-N. (2019). Vegetarian Diets and Medical Expenditure in Taiwan—A Matched Cohort Study. Nutrients, 11(11), 2688. https://doi.org/10.3390/nu11112688






