Increasing Dietary Carbohydrate as Part of a Healthy Whole Food Diet Intervention Dampens Eight Week Changes in Salivary Cortisol and Cortisol Responsiveness
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Subjects
2.3. Measurements
2.3.1. Dietary Measurements
2.3.2. Salivary Cortisol Measurements
2.3.3. Physical Measurements
2.4. Statistical Analysis
3. Results
4. Discussion
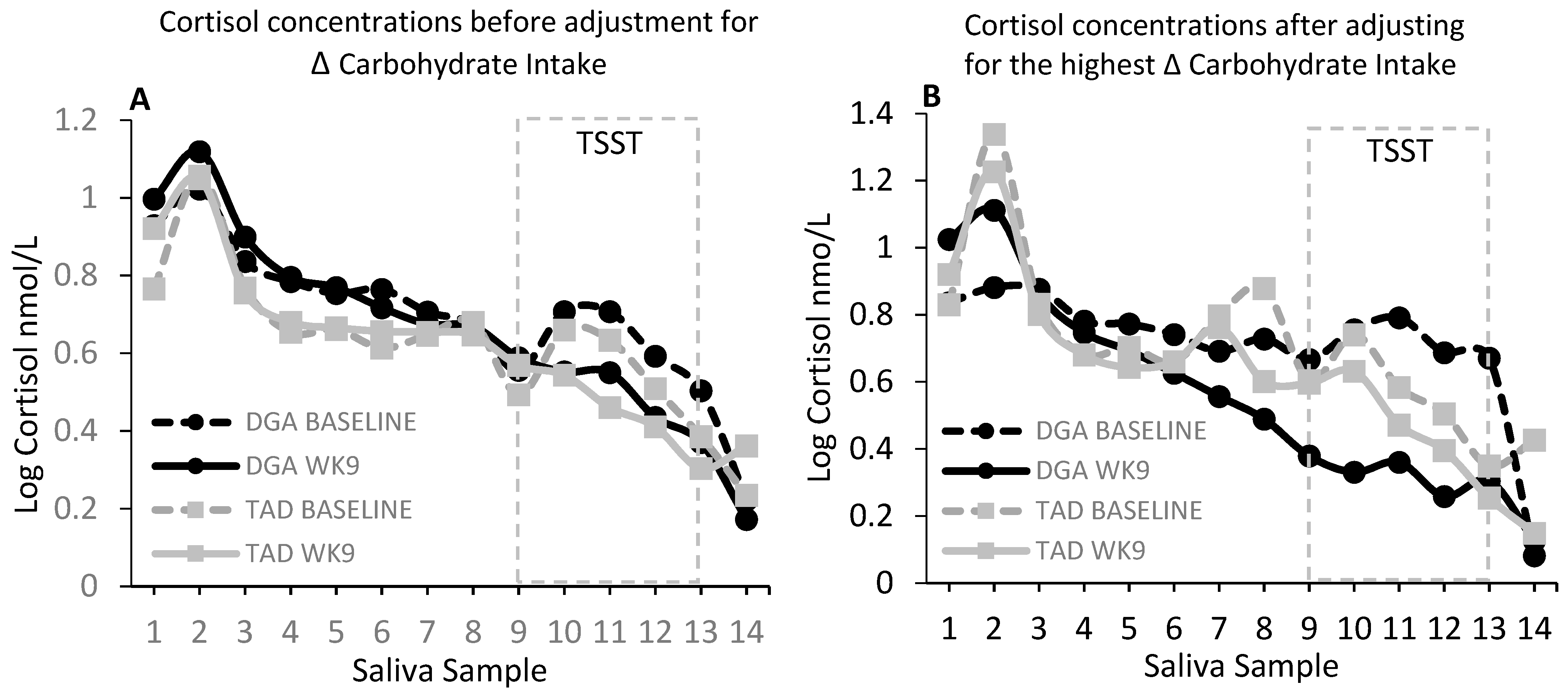
4.1. Differences in Dietary Carbohydrate Moderate Effects of the Diet Intervention on Salivary Cortisol
4.2. Limitations
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Sarris, J.; Logan, A.C.; Akbaraly, T.N.; Amminger, G.P.; Balanza-Martinez, V.; Freeman, M.P.; Hibbeln, J.; Matsuoka, Y.; Mischoulon, D.; Mizoue, T.; et al. Nutritional medicine as mainstream in psychiatry. Lancet Psychiatry 2015, 2, 271–274. [Google Scholar] [CrossRef]
- Brody, S.; Preut, R.; Schommer, K.; Schurmeyer, T.H. A randomized controlled trial of high dose ascorbic acid for reduction of blood pressure, cortisol, and subjective responses to psychological stress. Psychopharmacology 2002, 159, 319–324. [Google Scholar] [CrossRef] [PubMed]
- Carter, J.R.; Schwartz, C.E.; Yang, H.; Joyner, M.J. Fish oil and neurovascular reactivity to mental stress in humans. Am. J. Physiol. Regul. Integr. Comp. Physiol. 2013, 304, R523–R530. [Google Scholar] [CrossRef]
- Harris, E.; Kirk, J.; Rowsell, R.; Vitetta, L.; Sali, A.; Scholey, A.B.; Pipingas, A. The effect of multivitamin supplementation on mood and stress in healthy older men. Hum. Psychopharmacol. 2011, 26, 560–567. [Google Scholar] [CrossRef] [PubMed]
- Hellhammer, J.; Fries, E.; Buss, C.; Engert, V.; Tuch, A.; Rutenberg, D.; Hellhammer, D. Effects of soy lecithin phosphatidic acid and phosphatidylserine complex (PAS) on the endocrine and psychological responses to mental stress. Stress 2004, 7, 119–126. [Google Scholar] [CrossRef]
- Hellhammer, J.; Hero, T.; Franz, N.; Contreras, C.; Schubert, M. Omega-3 fatty acids administered in phosphatidylserine improved certain aspects of high chronic stress in men. Nutr. Res. 2012, 32, 241–250. [Google Scholar] [CrossRef]
- Hellhammer, J.; Vogt, D.; Franz, N.; Freitas, U.; Rutenberg, D. A soy-based phosphatidylserine/ phosphatidic acid complex (PAS) normalizes the stress reactivity of hypothalamus-pituitary-adrenal-axis in chronically stressed male subjects: A randomized, placebo-controlled study. Lipids Health Dis. 2014, 13, 121. [Google Scholar] [CrossRef]
- Jakulj, F.; Zernicke, K.; Bacon, S.L.; van Wielingen, L.E.; Key, B.L.; West, S.G.; Campbell, T.S. A high-fat meal increases cardiovascular reactivity to psychological stress in healthy young adults. J. Nutr. 2007, 137, 935–939. [Google Scholar] [CrossRef]
- Kennedy, D.O.; Veasey, R.; Watson, A.; Dodd, F.; Jones, E.; Maggini, S.; Haskell, C.F. Effects of high-dose B vitamin complex with vitamin C and minerals on subjective mood and performance in healthy males. Psychopharmacology 2010, 211, 55–68. [Google Scholar] [CrossRef] [Green Version]
- Long, S.J.; Benton, D. Effects of vitamin and mineral supplementation on stress, mild psychiatric symptoms, and mood in nonclinical samples: A meta-analysis. Psychosom. Med. 2013, 75, 144–153. [Google Scholar] [CrossRef]
- Markus, C.R.; Olivier, B.; de Haan, E.H. Whey protein rich in alpha-lactalbumin increases the ratio of plasma tryptophan to the sum of the other large neutral amino acids and improves cognitive performance in stress-vulnerable subjects. Am. J. Clin. Nutr. 2002, 75, 1051–1056. [Google Scholar] [CrossRef] [PubMed]
- Markus, C.R.; Olivier, B.; Panhuysen, G.E.; Van Der Gugten, J.; Alles, M.S.; Tuiten, A.; Westenberg, H.G.; Fekkes, D.; Koppeschaar, H.F.; de Haan, E.E. The bovine protein alpha-lactalbumin increases the plasma ratio of tryptophan to the other large neutral amino acids, and in vulnerable subjects raises brain serotonin activity, reduces cortisol concentration, and improves mood under stress. Am. J. Clin. Nutr. 2000, 71, 1536–1544. [Google Scholar] [CrossRef] [PubMed]
- Sayegh, R.; Schiff, I.; Wurtman, J.; Spiers, P.; McDermott, J.; Wurtman, R. The effect of a carbohydrate-rich beverage on mood, appetite, and cognitive function in women with premenstrual syndrome. Obstet. Gynecol. 1995, 86 Pt 1, 520–528. [Google Scholar] [CrossRef]
- Schubert, M.; Contreras, C.; Franz, N.; Hellhammer, J. Milk-based phospholipids increase morning cortisol availability and improve memory in chronically stressed men. Nutr. Res. 2011, 31, 413–420. [Google Scholar] [CrossRef]
- Schult, J.; Hero, T.; Hellhammer, J. Effects of powdered fertilized eggs on the stress response. Clin. Nutr. (Edinb. Scotl.) 2010, 29, 255–260. [Google Scholar] [CrossRef] [PubMed]
- Wurtman, J.J.; Brzezinski, A.; Wurtman, R.J.; Laferrere, B. Effect of nutrient intake on premenstrual depression. Am. J. Obstet. Gynecol. 1989, 161, 1228–1234. [Google Scholar] [CrossRef]
- Tannenbaum, B.M.; Brindley, D.N.; Tannenbaum, G.S.; Dallman, M.F.; McArthur, M.D.; Meaney, M.J. High-fat feeding alters both basal and stress-induced hypothalamic-pituitary-adrenal activity in the rat. Am. J. Physiol. 1997, 273, E1168–E1177. [Google Scholar] [CrossRef] [PubMed]
- Legendre, A.; Harris, R.B. Exaggerated response to mild stress in rats fed high-fat diet. Am. J. Physiol. Regul. Integr. Comp. Physiol. 2006, 291, R1288–R1294. [Google Scholar] [CrossRef]
- Hilimire, M.R.; DeVylder, J.E.; Forestell, C.A. Fermented foods, neuroticism, and social anxiety: An interaction model. Psychiatry Res. 2015, 228, 203–208. [Google Scholar] [CrossRef]
- Foster, M.T.; Warne, J.P.; Ginsberg, A.B.; Horneman, H.F.; Pecoraro, N.C.; Akana, S.F.; Dallman, M.F. Palatable foods, stress, and energy stores sculpt corticotropin-releasing factor, adrenocorticotropin, and corticosterone concentrations after restraint. Endocrinology 2009, 150, 2325–2333. [Google Scholar] [CrossRef]
- Laugero, K.D. Reinterpretation of basal glucocorticoid feedback: Implications to behavioral and metabolic disease. Vitam. Horm. 2004, 69, 1–29. [Google Scholar] [PubMed]
- Laugero, K.D.; Bell, M.E.; Bhatnagar, S.; Soriano, L.; Dallman, M.F. Sucrose ingestion normalizes central expression of corticotropin-releasing-factor messenger ribonucleic acid and energy balance in adrenalectomized rats: A glucocorticoid-metabolic-brain axis? Endocrinology 2001, 142, 2796–2804. [Google Scholar] [CrossRef] [PubMed]
- Laugero, K.D.; Gomez, F.; Manalo, S.; Dallman, M.F. Corticosterone infused intracerebroventricularly inhibits energy storage and stimulates the hypothalamo-pituitary axis in adrenalectomized rats drinking sucrose. Endocrinology 2002, 143, 4552–4562. [Google Scholar] [CrossRef] [PubMed]
- Tryon, M.S.; Stanhope, K.L.; Epel, E.S.; Mason, A.E.; Brown, R.; Medici, V.; Havel, P.J.; Laugero, K.D. Excessive Sugar Consumption May Be a Difficult Habit to Break: A View from the Brain and Body. J. Clin. Endocrinol. Metab. 2015, 100, 2239–2247. [Google Scholar] [CrossRef]
- Dallman, M.F.; Pecoraro, N.; Akana, S.F.; La Fleur, S.E.; Gomez, F.; Houshyar, H.; Bell, M.E.; Bhatnagar, S.; Laugero, K.D.; Manalo, S. Chronic stress and obesity: A new view of “comfort food”. Proc. Natl. Acad. Sci. USA 2003, 100, 11696–11701. [Google Scholar] [CrossRef]
- Ulrich-Lai, Y.M. Self-medication with sucrose. Curr. Opin. Behav. Sci. 2016, 9, 78–83. [Google Scholar] [CrossRef] [Green Version]
- United States Department of Agriculture. Report of the Dietary Guidelines Advisory Committee on the Dietary Guidelines for Americans; USDA: Washington, DC, USA, 2015.
- Van Horn, L.; Carson, J.A.S.; Appel, L.J.; Burke, L.E.; Economos, C.; Karmally, W.; Lancaster, K.; Lichtenstein, A.H.; Johnson, R.K.; Thomas, R.J.; et al. Recommended Dietary Pattern to Achieve Adherence to the American Heart Association/American College of Cardiology (AHA/ACC) Guidelines: A Scientific Statement from the American Heart Association. Circulation 2016, 134, e505–e529. [Google Scholar] [CrossRef]
- Franz, M.J.; VanWormer, J.J.; Crain, A.L.; Boucher, J.L.; Histon, T.; Caplan, W.; Bowman, J.D.; Pronk, N.P. Weight-Loss Outcomes: A Systematic Review and Meta-Analysis of Weight-Loss Clinical Trials with a Minimum 1-Year Follow-Up. J. Am. Diet. Assoc. 2007, 107, 1755–1767. [Google Scholar] [CrossRef]
- Look AHEAD Research Group. Association of the magnitude of weight loss and changes in physical fitness with long-term cardiovascular disease outcomes in overweight or obese people with type 2 diabetes: A post-hoc analysis of the Look AHEAD randomised clinical trial. Lancet Diabetes Endocrinol. 2016, 4, 913–921. [Google Scholar] [CrossRef]
- Berk, K.A.; Buijks, H.I.M.; Verhoeven, A.J.M.; Mulder, M.T.; Özcan, B.; van ’t Spijker, A.; Timman, R.; Busschbach, J.J.; Sijbrands, E.J. Group cognitive behavioural therapy and weight regain after diet in type 2 diabetes: Results from the randomised controlled POWER trial. Diabetologia 2018, 61, 790–799. [Google Scholar] [CrossRef]
- Look AHEAD Research Group. Eight-year weight losses with an intensive lifestyle intervention: The look AHEAD study. Obesity 2014, 22, 5–13. [Google Scholar] [CrossRef]
- Appelhans, B.M.; French, S.A.; Pagoto, S.L.; Sherwood, N.E. Managing temptation in obesity treatment: A neurobehavioral model of intervention strategies. Appetite 2016, 96, 268–279. [Google Scholar] [CrossRef] [PubMed]
- Elfhag, K.; Rössner, S. Who succeeds in maintaining weight loss? A conceptual review of factors associated with weight loss maintenance and weight regain. Obes. Rev. 2005, 6, 67–85. [Google Scholar] [CrossRef] [PubMed]
- MacLean, P.S.; Wing, R.R.; Davidson, T.; Epstein, L.; Goodpaster, B.; Hall, K.D.; Levin, B.E.; Perri, M.G.; Rolls, B.J.; Rosenbaum, M.; et al. NIH working group report: Innovative research to improve maintenance of weight loss. Obesity 2015, 23, 7–15. [Google Scholar] [CrossRef] [PubMed]
- Wing, R.R.; Papandonatos, G.; Fava, J.L.; Gorin, A.A.; Phelan, S.; McCaffery, J.; Tate, D.F. Maintaining large weight losses: The role of behavioral and psychological factors. J. Consult. Clin. Psychol. 2008, 76, 1015–1021. [Google Scholar] [CrossRef] [PubMed]
- Adam, T.C.; Epel, E.S. Stress, eating and the reward system. Physiol. Behav. 2007, 91, 449–458. [Google Scholar] [CrossRef]
- Dallman, M.F.; la Fleur, S.E.; Pecoraro, N.C.; Gomez, F.; Houshyar, H.; Akana, S.F. Minireview: Glucocorticoids-food intake, abdominal obesity, and wealthy nations in 2004. Endocrinology 2004, 145, 2633–2638. [Google Scholar] [CrossRef]
- Dixon, L.B.; Cronin, F.J.; Krebs-Smith, S.M. Let the pyramid guide your food choices: Capturing the total diet concept. J. Nutr. 2001, 131, 461s–472s. [Google Scholar] [CrossRef]
- George, G.C.; Milani, T.J.; Hanss-Nuss, H.; Freeland-Graves, J.H. Compliance with dietary guidelines and relationship to psychosocial factors in low-income women in late postpartum. J. Am. Diet. Assoc. 2005, 105, 916–926. [Google Scholar] [CrossRef]
- American Psychological Association. Stress in America: 2013; American Psychological Association: Washington, DC, USA, 2013. [Google Scholar]
- Dallman, M.F. Stress-induced obesity and the emotional nervous system. Trends Endocrinol. Metab. TEM 2010, 21, 159–165. [Google Scholar] [CrossRef] [Green Version]
- Murray, S.; Tulloch, A.; Gold, M.S.; Avena, N.M. Hormonal and neural mechanisms of food reward, eating behaviour and obesity. Nat. Rev. Endocrinol. 2014, 10, 540–552. [Google Scholar] [CrossRef]
- Wansink, B. From mindless eating to mindlessly eating better. Physiol. Behav. 2010, 100, 454–463. [Google Scholar] [CrossRef]
- Brown, K.W.; Ryan, R.M.; Creswell, J.D. Mindfulness: Theoretical Foundations and Evidence for its Salutary Effects. Psychol. Inq. 2007, 18, 211–237. [Google Scholar] [CrossRef]
- American Psychological Association, A.P. Stress in America: The State of Our Nation. Stress in AmericaTM Survey; American Psychological Association: Washington, DC, USA, 2017. [Google Scholar]
- Saad, L. Eight in 10 Americans Afflicted by Stress; Gallup: Washington, DC, USA, 2017. [Google Scholar]
- Mason, A.E.; Epel, E.S.; Aschbacher, K.; Lustig, R.H.; Acree, M.; Kristeller, J.; Cohn, M.; Dallman, M.; Moran, P.J.; Bacchetti, P.; et al. Reduced reward-driven eating accounts for the impact of a mindfulness-based diet and exercise intervention on weight loss: Data from the SHINE randomized controlled trial. Appetite 2016, 100, 86–93. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mason, A.E.; Epel, E.S.; Kristeller, J.; Moran, P.J.; Dallman, M.; Lustig, R.H.; Acree, M.; Bacchetti, P.; Laraia, B.A.; Hecht, F.M.; et al. Effects of a mindfulness-based intervention on mindful eating, sweets consumption, and fasting glucose levels in obese adults: Data from the SHINE randomized controlled trial. J. Behav. Med. 2016, 39, 201–213. [Google Scholar] [CrossRef]
- Krishnan, S.; Adams, S.H.; Allen, L.H.; Laugero, K.D.; Newman, J.W.; Stephensen, C.B.; Burnett, D.J.; Witbracht, M.; Welch, L.C.; Que, E.S.; et al. A Randomized Controlled Feeding Trial Based on the Dietary Guidelines for Americans on Cardiometabolic Health Indices. Am. J. Clin. Nutr. 2018, 108, 266–278. [Google Scholar] [CrossRef] [PubMed]
- Subar, A.F.; Kirkpatrick, S.I.; Mittl, B.; Zimmerman, T.P.; Thompson, F.E.; Bingley, C.; Willis, G.; Islam, N.G.; Baranowski, T.; McNutt, S. The Automated Self-Administered 24-h dietary recall (ASA24): A resource for researchers, clinicians, and educators from the National Cancer Institute. J. Acad. Nutr. Diet. 2012, 112, 1134–1137. [Google Scholar] [CrossRef] [PubMed]
- Firk, C.; Markus, C.R. Mood and cortisol responses following tryptophan-rich hydrolyzed protein and acute stress in healthy subjects with high and low cognitive reactivity to depression. Clin. Nutr. (Edinb. Scotl.) 2009, 28, 266–271. [Google Scholar] [CrossRef]
- McAllister, M.J.; Webb, H.E.; Tidwell, D.K.; Smith, J.W.; Fountain, B.J.; Schilling, M.W.; Williams, R.D., Jr. Exogenous Carbohydrate Reduces Cortisol Response from Combined Mental and Physical Stress. Int. J. Sports Med. 2016, 37, 1159–1165. [Google Scholar] [CrossRef]
- Anderson, D.A.; Shapiro, J.R.; Lundgren, J.D.; Spataro, L.E.; Frye, C.A. Self-reported dietary restraint is associated with elevated levels of salivary cortisol. Appetite 2002, 38, 13–17. [Google Scholar] [CrossRef]
- McLean, J.A.; Barr, S.I.; Prior, J.C. Cognitive dietary restraint is associated with higher urinary cortisol excretion in healthy premenopausal women. Am. J. Clin. Nutr. 2001, 73, 7–12. [Google Scholar] [CrossRef]
- Rutters, F.; Nieuwenhuizen, A.G.; Lemmens, S.G.; Born, J.M.; Westerterp-Plantenga, M.S. Hyperactivity of the HPA axis is related to dietary restraint in normal weight women. Physiol. Behav. 2009, 96, 315–319. [Google Scholar] [CrossRef] [PubMed]
- Bond, M.J.; McDowell, A.J.; Wilkinson, J.Y. The measurement of dietary restraint, disinhibition and hunger: An examination of the factor structure of the Three Factor Eating Questionnaire (TFEQ). Int. J. Obes. Relat. Metab. Disord. 2001, 25, 900–906. [Google Scholar] [CrossRef] [PubMed]
- Kirschbaum, C.; Pirke, K.M.; Hellhammer, D.H. The ‘Trier Social Stress Test’-a tool for investigating psychobiological stress responses in a laboratory setting. Neuropsychobiology 1993, 28, 76–81. [Google Scholar] [CrossRef] [PubMed]
- McEwen, B.S. Protection and damage from acute and chronic stress: Allostasis and allostatic overload and relevance to the pathophysiology of psychiatric disorders. Ann. N. Y. Acad. Sci. 2004, 1032, 1–7. [Google Scholar] [CrossRef]
- Sharma, S.T.; Nieman, L.K.; Feelders, R.A. Comorbidities in Cushing’s disease. Pituitary 2015, 18, 188–194. [Google Scholar] [CrossRef]
- Young, A.H. Cortisol in mood disorders. Stress 2004, 7, 205–208. [Google Scholar] [CrossRef]
- Seckl, J.R.; Fink, G. Use of in situ hybridization to investigate the regulation of hippocampal corticosteroid receptors by monoamines. J. Steroid Biochem. Mol. Biol. 1991, 40, 685–688. [Google Scholar] [CrossRef]
- Markus, R.; Panhuysen, G.; Tuiten, A.; Koppeschaar, H. Effects of food on cortisol and mood in vulnerable subjects under controllable and uncontrollable stress. Physiol. Behav. 2000, 70, 333–342. [Google Scholar] [CrossRef]
- Deuster, P.A.; Singh, A.; Hofmann, A.; Moses, F.M.; Chrousos, G.C. Hormonal responses to ingesting water or a carbohydrate beverage during a 2 h run. Med. Sci. Sports Exerc. 1992, 24, 72–79. [Google Scholar] [CrossRef]
- Carvalho, K.M.B.; Ronca, D.B.; Michels, N.; Huybrechts, I.; Cuenca-Garcia, M.; Marcos, A.; Molnár, D.; Dallongeville, J.; Manios, Y.; Schaan, B.D.; et al. Does the Mediterranean Diet Protect against Stress-Induced Inflammatory Activation in European Adolescents? The HELENA Study. Nutrients 2018, 10, 1770. [Google Scholar] [CrossRef]
- Cani, P.D.; Amar, J.; Iglesias, M.A.; Poggi, M.; Knauf, C.; Bastelica, D.; Neyrinck, A.M.; Fava, F.; Tuohy, K.M.; Chabo, C.; et al. Metabolic endotoxemia initiates obesity and insulin resistance. Diabetes 2007, 56, 1761–1772. [Google Scholar] [CrossRef] [PubMed]
- Bethin, K.E.; Vogt, S.K.; Muglia, L.J. Interleukin-6 is an essential, corticotropin-releasing hormone-independent stimulator of the adrenal axis during immune system activation. Proc. Natl. Acad. Sci. USA 2000, 97, 9317–9322. [Google Scholar] [CrossRef] [Green Version]
- Soltani, H.; Keim, N.L.; Laugero, K.D. Diet Quality for Sodium and Vegetables Mediate Effects of Whole Food Diets on 8-Week Changes in Stress Load. Nutrients 2018, 10, 1606. [Google Scholar] [CrossRef]
- Baudrand, R.; Campino, C.; Carvajal, C.A.; Olivieri, O.; Guidi, G.; Faccini, G.; Vohringer, P.A.; Cerda, J.; Owen, G.; Kalergis, A.M.; et al. High sodium intake is associated with increased glucocorticoid production, insulin resistance and metabolic syndrome. Clin. Endocrinol. 2014, 80, 677–684. [Google Scholar] [CrossRef]
- Ehrlich, E.N.; Lugibihl, K.; Laves, M.; Janulis, M. Reciprocal Variations in Urinary Cortisol and Aldosterone in Response to Increased Salt Intake in Humans. J. Clin. Endocrinol. Metab. 1966, 26, 1160–1169. [Google Scholar] [CrossRef] [PubMed]
- Wambach, G.; Bleienheuft, C.; Bonner, G. Sodium loading raises urinary cortisol in man. J. Endocrinol. Investig. 1986, 9, 257–259. [Google Scholar] [CrossRef] [PubMed]
- Lewicka, S.; Nowicki, M.; Vecsei, P. Effect of sodium restriction on urinary excretion of cortisol and its metabolites in humans. Steroids 1998, 63, 401–405. [Google Scholar] [CrossRef]
- Sabir, M.S.; Haussler, M.R.; Mallick, S.; Kaneko, I.; Lucas, D.A.; Haussler, C.A.; Whitfield, G.K.; Jurutka, P.W. Optimal vitamin D spurs serotonin: 1,25-dihydroxyvitamin D represses serotonin reuptake transport (SERT) and degradation (MAO-A) gene expression in cultured rat serotonergic neuronal cell lines. Genes Nutr. 2018, 13, 19. [Google Scholar] [CrossRef]
- Markus, C.R. Dietary amino acids and brain serotonin function; implications for stress-related affective changes. Neuromol. Med. 2008, 10, 247–258. [Google Scholar] [CrossRef]
- Dziurkowska, E.; Wesolowski, M.; Dziurkowski, M. Salivary cortisol in women with major depressive disorder under selective serotonin reuptake inhibitors therapy. Arch. Womens Ment. Health 2013, 16, 139–147. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cohen, S.; Janicki-Deverts, D.; Miller, G.E. Psychological stress and disease. JAMA 2007, 298, 1685–1687. [Google Scholar] [CrossRef] [PubMed]
- Tryon, M.S.; DeCant, R.; Laugero, K.D. Having your cake and eating it too: A habit of comfort food may link chronic social stress exposure and acute stress-induced cortisol hyporesponsiveness. Physiol. Behav. 2013, 114–115, 32–37. [Google Scholar] [CrossRef] [PubMed]
- Rideout, C.A.; Linden, W.; Barr, S.I. High cognitive dietary restraint is associated with increased cortisol excretion in postmenopausal women. J. Gerontol. Ser. A Biol. Sci. Med. Sci. 2006, 61, 628–633. [Google Scholar] [CrossRef] [PubMed]

| Sample Time (Sample Number) | Diet | Intervention Week | Slope | S.E. | P-Value |
|---|---|---|---|---|---|
| Pre-TSST (9) | DGA | Baseline | 0.001463 | 0.001487 | 0.3266 |
| DGA | 9 | −0.00312 | 0.001487 | 0.0372 | |
| 30 min post-TSST (10) | DGA | Baseline | 0.001142 | 0.001487 | 0.4434 |
| DGA | 9 | −0.0039 | 0.001487 | 0.0096 ** | |
| 60 min post-TSST (11) | DGA | Baseline | 0.001814 | 0.001507 | 0.2306 |
| DGA | 9 | −0.00312 | 0.001517 | 0.041 | |
| 90 min post-TSST (12) | DGA | Baseline | 0.001689 | 0.001493 | 0.2596 |
| DGA | 9 | −0.00298 | 0.00152 | 0.0516 | |
| 120 min post-TSST (13) | DGA | Baseline | 0.002341 | 0.001492 | 0.1186 |
| DGA | 9 | −0.00193 | 0.001488 | 0.1955 | |
| Pre-TSST (9) | TAD | Baseline | 0.000565 | 0.001402 | 0.687 |
| TAD | 9 | −0.00013 | 0.001438 | 0.93 | |
| 30 min post-TSST (10) | TAD | Baseline | 0.000172 | 0.001402 | 0.9023 |
| TAD | 9 | 0.000992 | 0.001438 | 0.4908 | |
| 60 min post-TSST (11) | TAD | Baseline | −0.00139 | 0.001402 | 0.3228 |
| TAD | 9 | 0.000077 | 0.001439 | 0.9571 | |
| 90 min post-TSST (12) | TAD | Baseline | −0.00083 | 0.001405 | 0.5551 |
| TAD | 9 | −0.00017 | 0.001442 | 0.9073 | |
| 120 min post-TSST (13) | TAD | Baseline | −0.00106 | 0.001406 | 0.4501 |
| TAD | 9 | −0.00041 | 0.001439 | 0.7742 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Soltani, H.; Keim, N.L.; Laugero, K.D. Increasing Dietary Carbohydrate as Part of a Healthy Whole Food Diet Intervention Dampens Eight Week Changes in Salivary Cortisol and Cortisol Responsiveness. Nutrients 2019, 11, 2563. https://doi.org/10.3390/nu11112563
Soltani H, Keim NL, Laugero KD. Increasing Dietary Carbohydrate as Part of a Healthy Whole Food Diet Intervention Dampens Eight Week Changes in Salivary Cortisol and Cortisol Responsiveness. Nutrients. 2019; 11(11):2563. https://doi.org/10.3390/nu11112563
Chicago/Turabian StyleSoltani, Hoda, Nancy L. Keim, and Kevin D. Laugero. 2019. "Increasing Dietary Carbohydrate as Part of a Healthy Whole Food Diet Intervention Dampens Eight Week Changes in Salivary Cortisol and Cortisol Responsiveness" Nutrients 11, no. 11: 2563. https://doi.org/10.3390/nu11112563
APA StyleSoltani, H., Keim, N. L., & Laugero, K. D. (2019). Increasing Dietary Carbohydrate as Part of a Healthy Whole Food Diet Intervention Dampens Eight Week Changes in Salivary Cortisol and Cortisol Responsiveness. Nutrients, 11(11), 2563. https://doi.org/10.3390/nu11112563




