Multifactorial Etiology of Anemia in Celiac Disease and Effect of Gluten-Free Diet: A Comprehensive Review
Abstract
:1. Introduction
2. Micronutrient Deficiencies and Celiac Disease
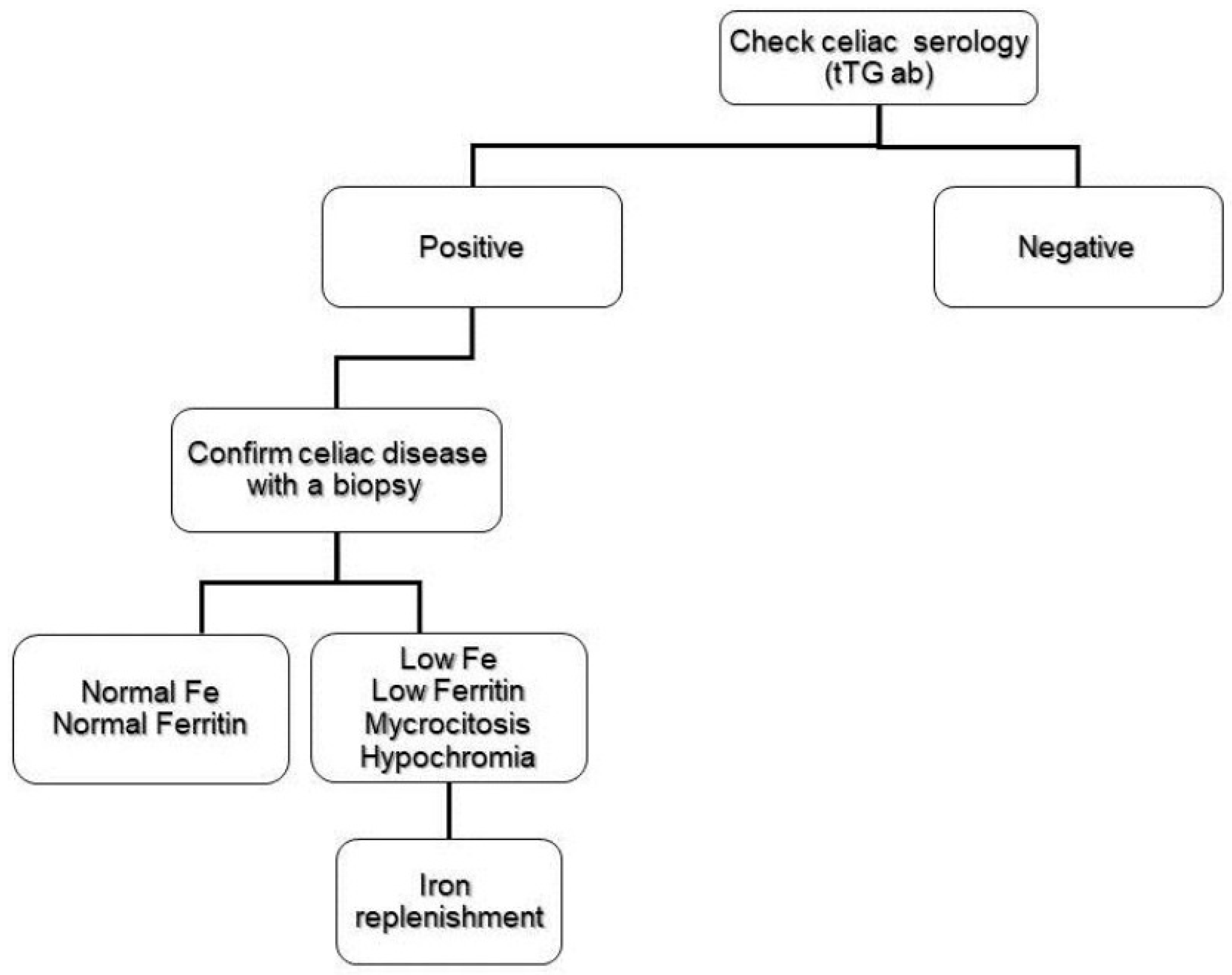
2.1. Iron Deficiency
2.2. Folate and Vitamin B12 Deficiency
2.3. Copper and Zinc Deficiency
3. Aplastic Anemia and Celiac Disease
4. Anemia of Chronic Disease
5. Refractory Anemia to the Gluten-Free Diet
6. Conclusions and Future Perspectives
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Rubio-Tapia, A.; Ludvigsson, J.F.; Brantner, T.L.; Murray, J.A.; Everhart, J.E. The Prevalence of Celiac Disease in the United States. Am. J. Gastroenterol. 2012, 107, 1538–1544. [Google Scholar] [CrossRef] [PubMed]
- Larson, S.A.; Khaleghi, S.; Rubio-Tapia, A.; Ovsyannikova, I.G.; King, K.S.; Larson, J.J.; Lahr, B.D.; Poland, G.A.; Camilleri, M.J.; Murray, J.A. Prevalence and Morbidity of Undiagnosed Celiac Disease from a Community-Based Study. Gastroenterology 2017, 152, 830–839. [Google Scholar]
- Mahadev, S.; Laszkowska, M.; Sundström, J.; Björkholm, M.; Lebwohl, B.; Green, P.H.; Ludvigsson, J.F. Prevalence of Celiac Disease in Patients With Iron Deficiency Anemia—A Systematic Review with Meta-analysis. Gastroenterology 2018, 155, 374–382. [Google Scholar] [CrossRef] [PubMed]
- Guandalini, S.; Assiri, A. Celiac disease: A review. JAMA Pediatr. 2014, 168, 272–278. [Google Scholar] [CrossRef] [PubMed]
- Husby, S.; Koletzko, S.; Korponay-Szabo, I.R.; Mearin, M.L.; Phillips, A.; Shamir, R.; Troncone, R.; Giersiepen, K.; Branski, D.; Catassi, C.; et al. European Society for Pediatric Gastroenterology, Hepatology, and Nutrition guidelines for the diagnosis of coeliac disease. J. Pediatr. Gastroenterol. Nutr. 2012, 54, 136–160. [Google Scholar] [CrossRef]
- Felli, C.; Balsassarre, A.; Masoptti, A. Intestinal and circulating microRNAs in coeliac disease. Int. J. Mol. Sci. 2017, 18, 1907. [Google Scholar] [CrossRef]
- Amr, K.S.; Bayoumi, F.S.; Eissa, E.; Abu-Zekry, M. Circulating microRNAs as potential non-invasive biomarkers in pediatric patients with celiac disease. Eur. Ann. Allergy Clin. Immunol. 2019, 51, 159–164. [Google Scholar] [CrossRef] [Green Version]
- Vaira, V.; Roncoroni, L.; Barisani, D.; Gaudioso, G.; Bosari, S.; Bulfamante, G.; Doneda, L.; Conte, D.; Tomba, C.; Bardella, M.T.; et al. MicroRNA profiles in coeliac patients distinguish different clinical phenotypes and are modulated by gliadin peptides in primary duodenal fibroblast. Clin. Sci. 2014, 126, 417–423. [Google Scholar] [CrossRef]
- Bledsoe, A.C.; King, K.S.; Larson, J.J.; Snyder, M.; Absah, I.; Murray, J.A. Micronutrient Deficiencies Are Common in Contemporary Celiac Disease Despite Lack of Overt Malabsorption Symptoms. Mayo Clin. Proc. 2019, 94, 1253–1260. [Google Scholar] [CrossRef]
- Halfdanarson, T.R.; Litzow, M.R.; Murray, J.A. Hematologic manifestations of celiac disease. Blood 2007, 109, 412–421. [Google Scholar] [CrossRef]
- Shahriari, M.; Honar, N.; Yousefi, A.; Javaherizadeh, H. Association of potential celiac disease and refractory iron deficiency anemia in children and adolescents. Arq. Gastroenterol. 2018, 55, 78–81. [Google Scholar] [CrossRef] [PubMed]
- Elli, L.; Norsa, L.; Zullo, A.; Carroccio, A.; Girelli, C.; Oliva, S.; Romano, C.; Leandro, G.; Bellini, M.; Marmo, R.; et al. Diagnosis of chronic anaemia in gastrointestinal disorders: A guideline by the Italian Association of Hospital Gastroenterologist and Endoscopist (AIGO) and the Italian Society of Pardiatric Gastroenterology Hepatology and Nutrition (SIGENP). Dig. Liver Dis. 2019, 51, 471–483. [Google Scholar] [CrossRef] [PubMed]
- Murray, J.A.; Watson, T.; Clearman, B.; Mitros, F. Effect of a gluten-free diet on gastrointestinal symptoms in celiac disease. Am. J. Clin. Nutr. 2004, 79, 669–673. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Leffler, D.A.; Dennis, M.; Hyett, B.; Kelly, E.; Schuppan, D.; Kelly, C.P. Etiologies and Predictors of Diagnosis in Nonresponsive Celiac Disease. Clin. Gastroenterol. Hepatol. 2007, 5, 445–450. [Google Scholar] [CrossRef] [PubMed]
- Muñoz, M.; Villar, I.; García-Erce, J.A. An update on iron physiology. World J. Gastroenterol. 2009, 15, 4617. [Google Scholar] [CrossRef] [PubMed]
- DeLoughery, T.G. Microcytic anemia. N. Engl. J. Med. 2014, 371, 1324–1331. [Google Scholar] [CrossRef]
- Leung, A.K.; Chan, K.W. Iron deficiency anemia. Adv. Pediatr. 2001, 48, 385–408. [Google Scholar]
- Rao, R.; Georgieff, M.K. Iron in fetal and neonatal nutrition. Semin. Fetal Neonatal Med. 2007, 12, 54–63. [Google Scholar] [CrossRef] [Green Version]
- Beard, J. Iron Deficiency Alters Brain Development and Functioning. J. Nutr. 2003, 133, 1468S–1472S. [Google Scholar] [CrossRef] [Green Version]
- Beard, J.L.; Wiesinger, J.A.; Connor, J.R. Pre- and Postweaning Iron Deficiency Alters Myelination in Sprague-Dawley Rats. Dev. Neurosci. 2003, 25, 308–315. [Google Scholar] [CrossRef]
- Beard, J.L.; Connor, J.R. Iron status and neural functioning. Annu. Rev. Nutr. 2003, 23, 41–58. [Google Scholar] [CrossRef] [PubMed]
- Rubio-Tapia, A.; Hill, I.D.; Kelly, C.P.; Calderwood, A.H.; Murray, J.A. ACG Clinical Guidelines: Diagnosis and Management of Celiac Disease. Am. J. Gastroenterol. 2013, 108, 656–676. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Harper, J.W.; Holleran, S.F.; Ramakrishnan, R.; Bhagat, G.; Green, P.H.R. Anemia in celiac disease is multifactorial in etiology. Am. J. Hematol. 2007, 82, 996–1000. [Google Scholar] [CrossRef] [PubMed]
- Annibale, B.; Severi, C.; Chistolini, A.; Antonelli, G.; Lahner, E.; Marcheggiano, A.; Iannoni, C.; Monarca, B.; Delle Fave, G. Efficacy of gluten-free diet alone on recovery from iron deficiency anemia in adult celiac patients. Am. J. Gastroenterol. 2001, 96, 132–137. [Google Scholar] [CrossRef] [PubMed]
- Smukalla, S.; Lebwohl, B.; Mears, J.G.; Leslie, L.A.; Green, P.H. How often do hematologists consider celiac disease in iron-deficiency anemia? Results of a national survey. Clin. Adv. Hematol. Oncol. 2014, 12, 100–105. [Google Scholar]
- Oxentenko, A.S.; Murray, J.A. Celiac Disease: Ten Things That Every Gastroenterologist Should Know. Clin. Gastroenterol. Hepatol. 2015, 13, 1396–1404. [Google Scholar] [CrossRef]
- Murray, J.A.; McLachlan, S.; Adams, P.C.; Eckfeldt, J.H.; Garner, C.P.; Vulpe, C.D.; Gordeuk, V.R.; Brantner, T.; Leiendecker–Foster, C.; Killeen, A.A.; et al. Association between celiac disease and iron deficiency in caucasians, but not non-caucasians. Clin. Gastroenterol. Hepatol. 2013, 11, 808–814. [Google Scholar] [CrossRef]
- Pirán Arce, M.F.; Aballay, L.R.; Leporati, J.L.; Navarro, A.; Forneris, M. Blood iron levels in accordance with adherence to a gluten-free diet in celiac school aged children. Nutr. Hosp. 2018, 35, 25–32. [Google Scholar]
- Brandimarte, G.; Tursi, A.; Giorgetti, G.M. Changing trends in clinical form of celiac disease. Which is now the main form of celiac disease in clinical practice? Minerva Gastroenterol. Dietol. 2002, 48, 121–130. [Google Scholar]
- Sharma, M.; Singh, P.; Agnihotri, A.; Das, P.; Mishra, A.; Verma, A.K.; Ahuja, A.; Sreenivas, V.; Khadgawat, R.; Gupta, S.D.; et al. Celiac disease: A disease with varied manifestations in adults and adolescents. J. Dig. Dis. 2013, 14, 518–525. [Google Scholar] [CrossRef]
- Rostami-Nejad, M.; Aldulaimi, D.; Livett, H.; Rostami, K.H. pylori associated with iron deficiency anemia even in celiac disease patients; strongly evidence based but weakly reflected in practice. Gastroenterol. Hepatol. Bed Bench. 2015, 8, 178. [Google Scholar] [PubMed]
- Samasca, G.; Deleanu, D.; Sur, G.; Lupan, I.; Giulia, A.; Carpa, R. Is it necessary to screen Helicobacter pylori infection in patients with celiac disease and iron deficiency? Gastroenterol. Hepatol. 2016, 9, 345. [Google Scholar]
- Elli, L.; Poggiali, E.; Tomba, C.; Andreozzi, F.; Nava, I.; Bardella, M.T.; Campostrini, N.; Girelli, D.; Conte, D.; Cappellini, M.D. Does TMPRSS6 RS855791 polymorphism contribute to iron defiociency in treated celiac disease? Am. J. Gastroenterol. 2015, 110, 200–202. [Google Scholar] [CrossRef] [PubMed]
- De Falco, L.; Tortora, R.; Imperatore, N.; Bruno, M.; Capasso, M.; Girelli, D.; Castagna, A.; Caporaso, N.; Iolascon, A.; Rispo, A. The role of TMPRSS6 and HFE variants in iron deficiency anemia in celiac disease. Am. J. Hematol. 2018, 93, 383–393. [Google Scholar] [CrossRef] [PubMed]
- Sharma, N.; Begum, J.; Eksteen, B.; Elagib, A.; Brookes, M.; Cooper, B.T.; Tselepis, C.; Iqbal, T.H. Differential ferritin expression is associated with iron defficiency in coeliac disease. Eur. J. Gastroenterol. Hepatol. 2009, 21, 794–804. [Google Scholar] [CrossRef] [PubMed]
- Tolone, C.; Bellini, G.; Punzo, F.; Papparella, A.; Miele, E.; Vitale, A.; Nobili, B.; Strisciuglio, C.; Rossi, F. The DMT1 IVS4+44C> A polymorphism and the risk of iron deficiency anemia in children with celiac disease. PLoS ONE 2017, 12, e0185822. [Google Scholar] [CrossRef]
- Elli, L.; Ferretti, F.; Branchi, F.; Tomba, C.; Lombardo, V.; Scricciolo, A.; Doneda, L.; Roncoroni, L. Sucrosomial iron supplementation in anemic patients with celiac disease not tolerating oral ferrous sulfate: A prospective study. Nutrients 2018, 10, 330. [Google Scholar] [CrossRef]
- Giancotti, L.; Talarico, V.; Mazza, G.A.; Marrazzo, S.; Gangemi, P.; Miniero, R.; Bertini, M. FeralgineTM a new approach for iron defficiency anemia in celiac patients. Nutrients 2019, 11, 887. [Google Scholar] [CrossRef]
- Zamani, F.; Mohamadnejad, M.; Shakeri, R.; Amiri, A.; Najafi, S.; Alimohamadi, S.M.; Tavangar, S.M.; Ghavamzadeh, A.; Malekzadeh, R. Gluten sensitive enteropathy in patients with iron deficiency anemia of unknown origin. World J. Gastroenterol. 2008, 14, 7381. [Google Scholar] [CrossRef]
- Lasa, J.S.; Olivera, P.; Soifer, L.; Moore, R. La anemia ferropénica como presentación de enfermedad celíaca subclínica en una población argentina. Rev. Gastroenterol. Méx. 2017, 82, 270–273. [Google Scholar] [CrossRef]
- Repo, M.; Lindfors, K.; Mäki, M.; Huhtala, H.; Laurila, K.; Lähdeaho, M.L.; Saavalainen, P.; Kaukinen, K.; Kurppa, K. Anemia and iron deficiency in children with potential celiac disease. J. Pediatr. Gastroenterol. Nutr. 2017, 64, 56–62. [Google Scholar] [CrossRef] [PubMed]
- Dinler, G.; Atalay, E.; Kalayci, A.G. Celiac disease in 87 children with typical and atypical symptoms in Black Sea region of Turkey. World J. Pediatr. 2009, 5, 282–286. [Google Scholar] [CrossRef] [PubMed]
- Wierdsma, N.; van Bokhorst-de van der Schueren, M.; Berkenpas, M.; Mulder, C.; van Bodegraven, A. Vitamin and Mineral Deficiencies Are Highly Prevalent in Newly Diagnosed Celiac Disease Patients. Nutrients 2013, 5, 3975–3992. [Google Scholar] [CrossRef] [PubMed]
- García-Manzanares, Á.; Lucendo, A.J. Review: Nutritional and Dietary Aspects of Celiac Disease. Nutr. Clin. Pract. 2011, 26, 163–173. [Google Scholar] [CrossRef]
- Carmel, R. Megaloblastic Anemias: Disorders Ofimpaired DNA Synthesis, 1st ed.; Wintrobe’s Clinical Hematology; Williams & Wilkins: Baltimore, MD, USA, 2004. [Google Scholar]
- Kuloğlu, Z.; Kirsaçlioğlu, C.T.; Kansu, A.; Ensari, A.; Girgin, N. Celiac disease: Presentation of 109 children. Yonsei Med. J. 2009, 50, 617–623. [Google Scholar] [CrossRef]
- Ward, P.C.J. Modern approaches to the investigation of vitamin B12 deficiency. Clin. Lab. Med. 2002, 22, 435–445. [Google Scholar] [CrossRef]
- Klee, G.G. Cobalamin and folate evaluation: Measurement of methylmalonic acid and homocysteine vs vitamin B(12) and folate. Clin. Chem. 2000, 46, 1277–1283. [Google Scholar]
- Guevara Pacheco, G.; Chávez Cortés, E.; Castillo-Durán, C. Deficiencia de micronutrientes y enfermedad celíaca. Arch. Argent Pediatr. 2014, 112, 457–463. [Google Scholar]
- Freeman, H.J. Neurological disorders in adult celiac disease. Can. J. Gastroenterol. 2008, 22, 909–911. [Google Scholar] [CrossRef]
- Halfdanarion, T.R.; Kumar, N.; Hogan, W.J.; Murray, J.A. Copper deficiency in celiac disease. J. Clin. Gastroenterol. 2009, 43, 162–164. [Google Scholar] [CrossRef]
- Cavallieri, F.; Fin, N.; Contardi, S.; Fiorini, M.; Corradini, E.; Valzania, F. Subacute copper-deficiency myelopathy in as patient with occult celiac disease. J. Spinal Cord Med. 2017, 40, 489–491. [Google Scholar] [CrossRef] [PubMed]
- Tran, C.D.; Katsikeros, R.; Manton, N.; Krebs, N.F.; Hambidge, K.M.; Butler, R.N.; Davidson, G.P. Zinc homeostasis and gut function in children with celiac disease. Am. J. Clin. Nutr. 2011, 94, 1026–1032. [Google Scholar] [CrossRef] [PubMed]
- Baydoun, A.; Maakaron, J.E.; Halawi, H.; Abou Rahal, J.; Taher, A.T. Hematological manifestations of celiac disease. Scand. J. Gastroenterol. 2012, 47, 1401–1411. [Google Scholar] [CrossRef] [PubMed]
- Irfan, O.; Mahmood, S.; Nand, H.; Billoo, G. Celiac disease associated with aplastic anemia in a 6-year-old girl: A case report and review of the literature. J. Med. Case Rep. 2018, 12, 16. [Google Scholar] [CrossRef] [PubMed]
- Grey-Davies, E.; Hows, J.M.; Marsh, J.C.W. Aplastic anaemia in association with coeliac disease: A series of three cases. Br. J. Haematol. 2008, 143, 258–260. [Google Scholar] [CrossRef]
- Maheshwari, A.; Nirupam, N.; Aneja, S.; Meena, R.; Chandra, J.; Kumar, P. Association of Celiac Disease with Aplastic Anemia. Indian J. Pediatr. 2012, 79, 1372–1373. [Google Scholar] [CrossRef]
- Salmeron, G.; Patey, N.; De Latour, R.P.; Raffoux, E.; Gluckman, E.; Brousse, N.; Socié, G.; Robin, M. Coeliac disease and aplastic anaemia: A specific entity? Br. J. Haematol. 2009, 146, 122–124. [Google Scholar] [CrossRef]
- Basu, A.; Ray, Y.; Bowmik, P.; Rahman, M.; Dikshit, N.; Goswami, R.P. Rare association of coeliac disease with aplastic anaemia: Report of a case from India. Indian J. Hematol. Blood Transfus. 2014, 30, 208–211. [Google Scholar] [CrossRef]
- Badyal, R.K.; Sachdeva, M.U.S.; Varma, N.; Thapa, B.R. A Rare Association of Celiac Disease and Aplastic Anemia: Case Report of a Child and Review of Literature. Pediatr. Dev. Pathol. 2014, 17, 470–473. [Google Scholar] [CrossRef]
- Garrdner, L.; Benz, E. Hematology. Basic Principles and Practice, 3rd ed.; Churchill Livinstone: London, UK, 2000. [Google Scholar]
- Weiss, G.; Goodnough, L.T. Anemia of Chronic Disease. N. Engl. J. Med. 2005, 352, 1011–1023. [Google Scholar] [CrossRef]
- Ciccocioppo, R.; Di Sabatino, A.; Bauer, M.; Della Riccia, D.N.; Bizzini, F.; Biagi, F.; Cifone, M.G.; Corazza, G.R.; Schuppan, D. Matrix metalloproteinase pattern in celiac duodenal mucosa. Lab. Investig. 2005, 85, 397–407. [Google Scholar] [CrossRef] [PubMed]
- Di Sabatino, A.; Ciccocioppo, R.; Cupelli, F.; Cinque, B.; Millimaggi, D.; Clarkson, M.M.; Paulli, M.; Cifone, M.G.; Corazza, G.R. Epithelium derived interleukin 15 regulates intraepithelial lymphocyte Th1 cytokine production, cytotoxicity, and survival in coeliac disease. Gut 2006, 55, 469–477. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wang, C.Q.; Udupa, K.B.; Lipschitz, D.A. Interferon-γ exerts its negative regulatory effect primarily on the earliest stages of murine erythroid progenitor cell development. J. Cell. Physiol. 1995, 162, 134–138. [Google Scholar] [CrossRef] [PubMed]
- Ludwiczek, S.; Aigner, E.; Theurl, I.; Weiss, G. Cytokine-mediated regulation of iron transport in human monocytic cells. Blood 2003, 101, 4148–4154. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Högberg, L.; Danielsson, L.; Jarleman, S.; Sundqvist, T.; Stenhammar, L. Serum zinc in small children with coeliac disease. Acta Paediatr. 2008, 98, 343–345. [Google Scholar] [CrossRef] [PubMed]
- Zerga, M. Anemia de los trastornos crónicos. Hematologia 2004, 8, 45–55. [Google Scholar]
- Mullarky, I.K.; Szaba, F.M.; Kummer, L.W.; Wilhelm, L.B.; Parent, M.A.; Johnson, L.L.; Smiley, S.T. Gamma interferon suppresses erythropoiesis via interleukin-15. Infect. Immun. 2007, 75, 2630–2633. [Google Scholar] [CrossRef]
- Benahmed, M.; Meresse, B.; Arnulf, B.; Barbe, U.; Mention, J.J.; Verkarre, V.; Allez, M.; Cellier, C.; Hermine, O.; Cerf–Bensussan, N. Inhibition of TGF-β Signaling by IL-15: A New Role for IL-15 in the Loss of Immune Homeostasis in Celiac Disease. Gastroenterology 2007, 132, 994–1008. [Google Scholar] [CrossRef]
- Diaz-Castro, J.; Muriel-Neyra, C.; Martin-Masot, R.; Moreno-Fernandez, J.; Maldonado, J.; Nestares, T. Oxidative stress, DNA stability and evoked inflammatory signaling in young celiac patients consuming a gluten-free diet. Eur. J. Nutr. 2019, 1–8. [Google Scholar] [CrossRef]
- Bergamaschi, G.; Markopoulos, K.; Albertini, R.; Di Sabatino, A.; Biagi, F.; Ciccocioppo, R.; Arbustini, E.; Corazza, G.R. Anemia of chronic disease and defective erythropoietin production in patients with celiac disease. Haematologica 2008, 93, 1785–1791. [Google Scholar] [CrossRef] [Green Version]
- Cataldo, F.; Lio, D.; Marino, V.; Scola, L.; Crivello, A.; Corazza, G.R.; Working Groups of the SIGEP and ′Club del Tenue′. Plasma cytokine profiles in patients with celiac disease and selective IgA deficiency. Pediatr. Allergy Immunol. 2003, 14, 320–324. [Google Scholar] [CrossRef] [PubMed]
- Fornari, M.C.; Pedreira, S.; Niveloni, S.; González, D.; Diez, R.A.; Vázquez, H.; Mazure, R.; Sugai, E.; Smecuol, E.; Boerr, L.; et al. Pre- and Post-Treatment Serum Levels of Cytokines IL-1β, IL-6, and IL-1 Receptor Antagonist in Celiac Disease. Are They Related to the Associated Osteopenia? Am. J. Gastroenterol. 1998, 93, 413–418. [Google Scholar] [CrossRef] [PubMed]
- Romaldini, C.C.; Barbieri, D.; Okay, T.S.; Raiz, R.; Cançado, E.L.R. Serum soluble interleukin-2 receptor, interleukin-6, and tumor necrosis factor-alpha levels in children with celiac disease: Response to treatment. J. Pediatr. Gastroenterol. Nutr. 2002, 35, 513–517. [Google Scholar] [CrossRef] [PubMed]
- Merendino, R.A.; Di Pasquale, G.; Sturniolo, G.C.; Ruello, A.; Albanese, V.; Minciullo, P.L.; Di Mauro, S.; Gangemi, S. Relationship between IL-18 and sICAM-1 serum levels in patients affected by coeliac disease: Preliminary considerations. Immunol. Lett. 2003, 85, 257–260. [Google Scholar] [CrossRef]
- Berry, N.; Basha, J.; Varma, N.; Varma, S.; Prasad, K.K.; Vaiphei, K.; Dhaka, N.; Sinha, S.K.; Kochhar, R. Anemia in celiac disease is multifactorial in etiology: A prospective study from India. JGH Open 2018, 2, 196–200. [Google Scholar] [CrossRef] [PubMed]
- Elli, L.; Ferretti, F.; Orlando, S.; Vecchi, M.; Monguzzi, E.; Roncoroni, L.; Schuppan, D. Management of celiac disease in daily clinical practice. Eur. J. Intern. Med. 2019, 61, 15–24. [Google Scholar] [CrossRef]
- Barratt, S.M.; Leeds, J.S.; Sanders, D.S. Quality of life in Coeliac Disease is determined by perceived degree of difficulty adhering to a gluten-free diet, not the level of dietary adherence ultimately achieved. J. Gastrointestin Liver Dis. 2011, 20, 241–245. [Google Scholar]
- Martín Masot, R.; Ortega Páez, E. El péptido del gluten en heces puede ser útil en el seguimiento de la enfermedad celíaca. Evid. Pediatr. 2018, 14, 37. [Google Scholar]
- Silvester, J.A.; Kurada, S.; Szwajcer, A.; Kelly, C.P.; Leffler, D.A.; Duerksen, D.R. Tests for Serum Transglutaminase and Endomysial Antibodies Do Not Detect Most Patients with Celiac Disease and Persistent Villous Atrophy on Gluten-free Diets: A Meta-analysis. Gastroenterology 2017, 153, 689–701. [Google Scholar] [CrossRef]
- Gerasimidis, K.; Zafeiropoulou, K.; Mackinder, M.; Ijaz, U.Z.; Duncan, H.; Buchanan, E.; Cardigan, T.; Edwards, C.A.; McGrogan, P.; Russell, R.K. Comparison of Clinical Methods With the Faecal Gluten Immunogenic Peptide to Assess Gluten Intake in Coeliac Disease. J. Pediatr. Gastroenterol. Nutr. 2018, 67, 356–360. [Google Scholar] [CrossRef] [Green Version]
- Rubio-Tapia, A.; Murray, J.A. Classification and management of refractory coeliac disease. Gut 2010, 59, 547–557. [Google Scholar] [CrossRef] [PubMed]
- van Gils, T.; Nijeboer, P.; van Wanrooij, R.L.; Bouma, G.; Mulder, C.J.J. Mechanisms and management of refractory coeliac disease. Nat. Rev. Gastroenterol. Hepatol. 2015, 12, 572–579. [Google Scholar] [CrossRef] [PubMed]
- Ryan, B.M.; Kelleher, D. Refractory celiac disease. Gastroenterology 2000, 119, 243–251. [Google Scholar] [CrossRef] [PubMed]
- Rishi, A.R.; Rubio-Tapia, A.; Murray, J.A. Refractory celiac disease. Expert Rev. Gastroenterol. Hepatol. 2016, 10, 537–546. [Google Scholar] [CrossRef]
- Mooney, P.D.; Evans, K.E.; Singh, S.; Sanders, D.S. Treatment failure in coeliac disease: A practical guide to investigation and treatment of non-responsive and refractory coeliac disease. J. Gastrointestin Liver Dis. 2012, 21, 197–203. [Google Scholar]
- Branchi, F.; Locatelli, M.; Tomba, C.; Conte, D.; Ferretti, F.; Elli, L. Enteroscopy and radiology for the management of celiac disease complications: Time for a pragmatic roadmap. Dig. Liver Dis. 2016, 48, 578–586. [Google Scholar] [CrossRef]
- Chetcuti Zammit, S.; Sanders, D.S.; Sidhu, R. Capsule endoscopy for patients with coeliac disease. Expert Rev. Gastroenterol. Hepatol. 2018, 12, 779–790. [Google Scholar] [CrossRef]
- Efthymakis, K.; Milano, A.; Laterza, F.; Serio, M.; Neri, M. Iron deficiency anemia despite effective gluten-free diet in celiac disease: Diagnostic role of small bowel capsule endoscopy. Dig. Liver Dis. 2017, 49, 412–416. [Google Scholar] [CrossRef]
- Rajalahti, T.; Repo, M.; Kivelä, L.; Huhtala, H.; Mäki, M.; Kaukinen, K.; Lindfors, K.; Kurppa, K. Anemia in Pediatric Celiac Disease. J. Pediatr. Gastroenterol. Nutr. 2017, 64, e1–e6. [Google Scholar] [CrossRef]
- Lewis, S.K.; Semrad, C.E. Capsule Endoscopy and Enteroscopy in Celiac Disease. Gastroenterol. Clin. 2019, 48, 73–84. [Google Scholar] [CrossRef]
- Rokkas, T.; Niv, Y. The role of video capsule endoscopy in the diagnosis of celiac disease. Eur. J. Gastroenterol. Hepatol. 2012, 24, 303–308. [Google Scholar] [CrossRef] [PubMed]
- Eigner, W.; Bashir, K.; Primas, C.; Kazemi-Shirazi, L.; Wrba, F.; Trauner, M.; Vogelsang, H. Dynamics of occurrence of refractory coeliac disease and associated complications over 25 years. Aliment. Pharmacol. Ther. 2017, 45, 364–372. [Google Scholar] [CrossRef] [PubMed]
- Oruc, N.; Ozütemız, O.; Tekın, F.; Sezak, M.; Tunçyürek, M.; Krasinskas, A.M.; Tombuloğlu, M. Celiac disease associated with B-cell lymphoma. Turk. J. Gastroenterol. 2010, 21, 168–171. [Google Scholar] [CrossRef] [PubMed]
- Ilus, T.; Kaukinen, K.; Virta, L.J.; Pukkala, E.; Collin, P. Incidence of Malignancies in Diagnosed Celiac Patients: A Population-based Estimate. Am. J. Gastroenterol. 2014, 109, 1471–1477. [Google Scholar] [CrossRef]
- Delabie, J.; Holte, H.; Vose, J.M.; Ullrich, F.; Jaffe, E.S.; Savage, K.J.; Connors, J.M.; Rimsza, L.; Harris, N.L.; Müller-Hermelink, K.; et al. Enteropathy-associated T-cell lymphoma: Clinical and histological findings from the international peripheral T-cell lymphoma project. Blood 2011, 118, 148–155. [Google Scholar] [CrossRef]

| Cause | Incidence |
|---|---|
| Iron deficiency | 12–69% (adults) 10–20% (children) |
| Folic acid deficiency | 20–30% |
| Vitamin B12 deficiency | 8–41% |
| Copper deficiency | Very low |
| Zinc deficiency | Very low * |
| Bad response to the gluten-free diet | 23% |
| Medullary aplasia | Very low (12 cases) |
| Chronic disease | 4–17% |
| Study Reported | Grey-Davies [51] | Salmeron [53] | Maheswari [52] | Basu [54] | Badyal [55] | Omar [50] |
|---|---|---|---|---|---|---|
| Number of cases | 3 | 5 | 1 | 1 | 1 | 1 |
| Anemia diagnosis | Bone marrow biopsy | Bone marrow biopsy | Bone marrow biopsy | Bone marrow biopsy | Bone marrow biopsy | Bone marrow biopsy |
| Age (years) | 23, 37, 43 | Not reported | 13 | 40 | 9 | 6 |
| Intestinal biopsy | Villus atrophy | Villus atrophy | Villus atrophy | Villus atrophy | Not available | Villus atrophy |
| Treatment | GFD, corticotherapy, antithymocyte globulin, cyclosporine | GFD, antithymocyte globulin, cyclosporine. hematopoietic cell transplantation | GFD | GFD, corticotherapy, cyclosporine | GFD, corticotherapy, antithymocyte globulin | GFD |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Martín-Masot, R.; Nestares, M.T.; Diaz-Castro, J.; López-Aliaga, I.; Alférez, M.J.M.; Moreno-Fernandez, J.; Maldonado, J. Multifactorial Etiology of Anemia in Celiac Disease and Effect of Gluten-Free Diet: A Comprehensive Review. Nutrients 2019, 11, 2557. https://doi.org/10.3390/nu11112557
Martín-Masot R, Nestares MT, Diaz-Castro J, López-Aliaga I, Alférez MJM, Moreno-Fernandez J, Maldonado J. Multifactorial Etiology of Anemia in Celiac Disease and Effect of Gluten-Free Diet: A Comprehensive Review. Nutrients. 2019; 11(11):2557. https://doi.org/10.3390/nu11112557
Chicago/Turabian StyleMartín-Masot, Rafael, Maria Teresa Nestares, Javier Diaz-Castro, Inmaculada López-Aliaga, Maria Jose Muñoz Alférez, Jorge Moreno-Fernandez, and José Maldonado. 2019. "Multifactorial Etiology of Anemia in Celiac Disease and Effect of Gluten-Free Diet: A Comprehensive Review" Nutrients 11, no. 11: 2557. https://doi.org/10.3390/nu11112557
APA StyleMartín-Masot, R., Nestares, M. T., Diaz-Castro, J., López-Aliaga, I., Alférez, M. J. M., Moreno-Fernandez, J., & Maldonado, J. (2019). Multifactorial Etiology of Anemia in Celiac Disease and Effect of Gluten-Free Diet: A Comprehensive Review. Nutrients, 11(11), 2557. https://doi.org/10.3390/nu11112557







