Validity of the Mediterranean Diet and Culinary Index (MediCul) for Online Assessment of Adherence to the ‘Traditional’ Diet and Aspects of Cuisine in Older Adults
Abstract
1. Introduction
2. Materials and Methods
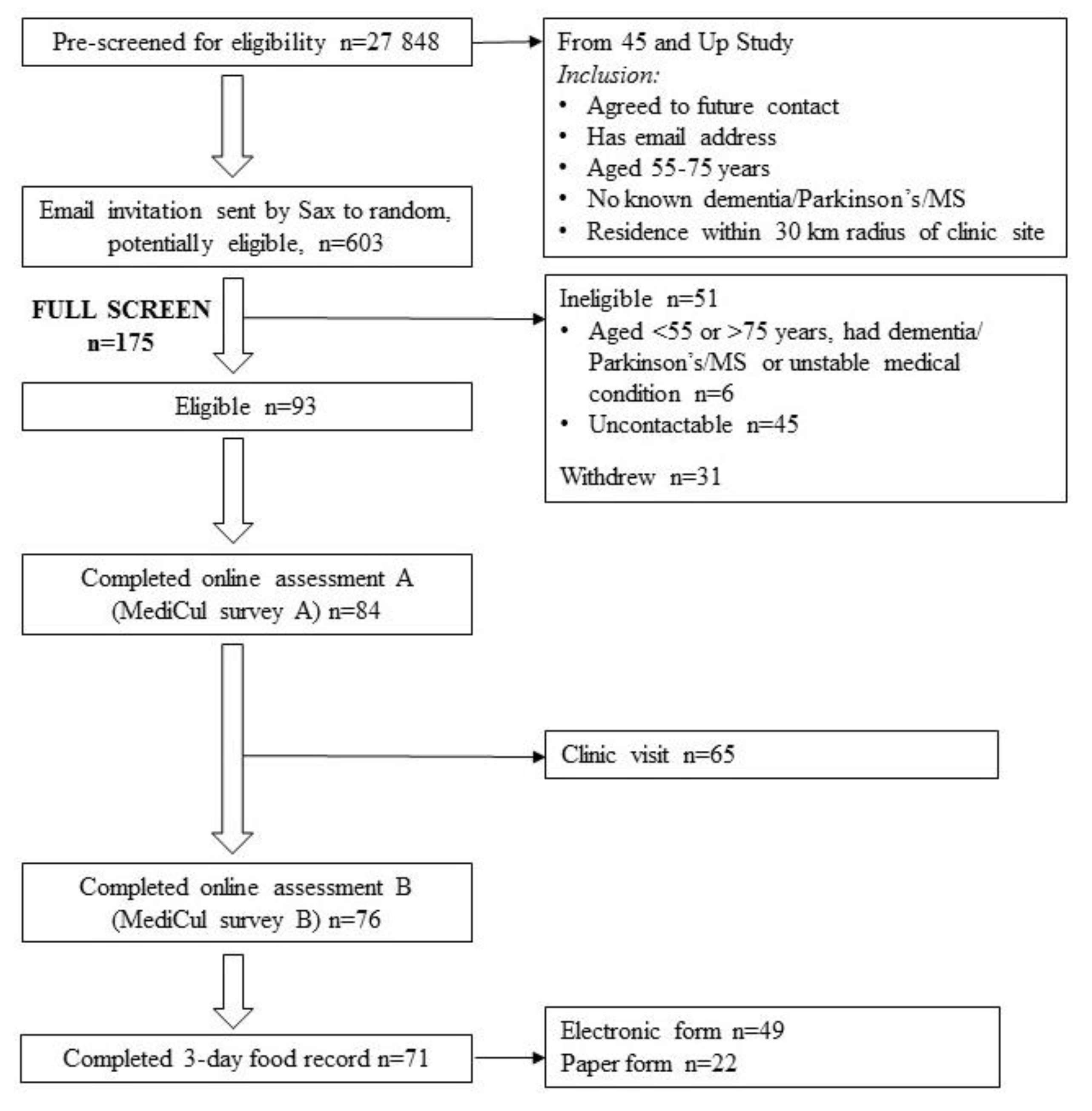
2.1. Participants
2.2. Assessments
2.3. The MediCul Tool
2.4. Dietary Analysis
2.5. Statistical Analysis
3. Results
3.1. Reliability
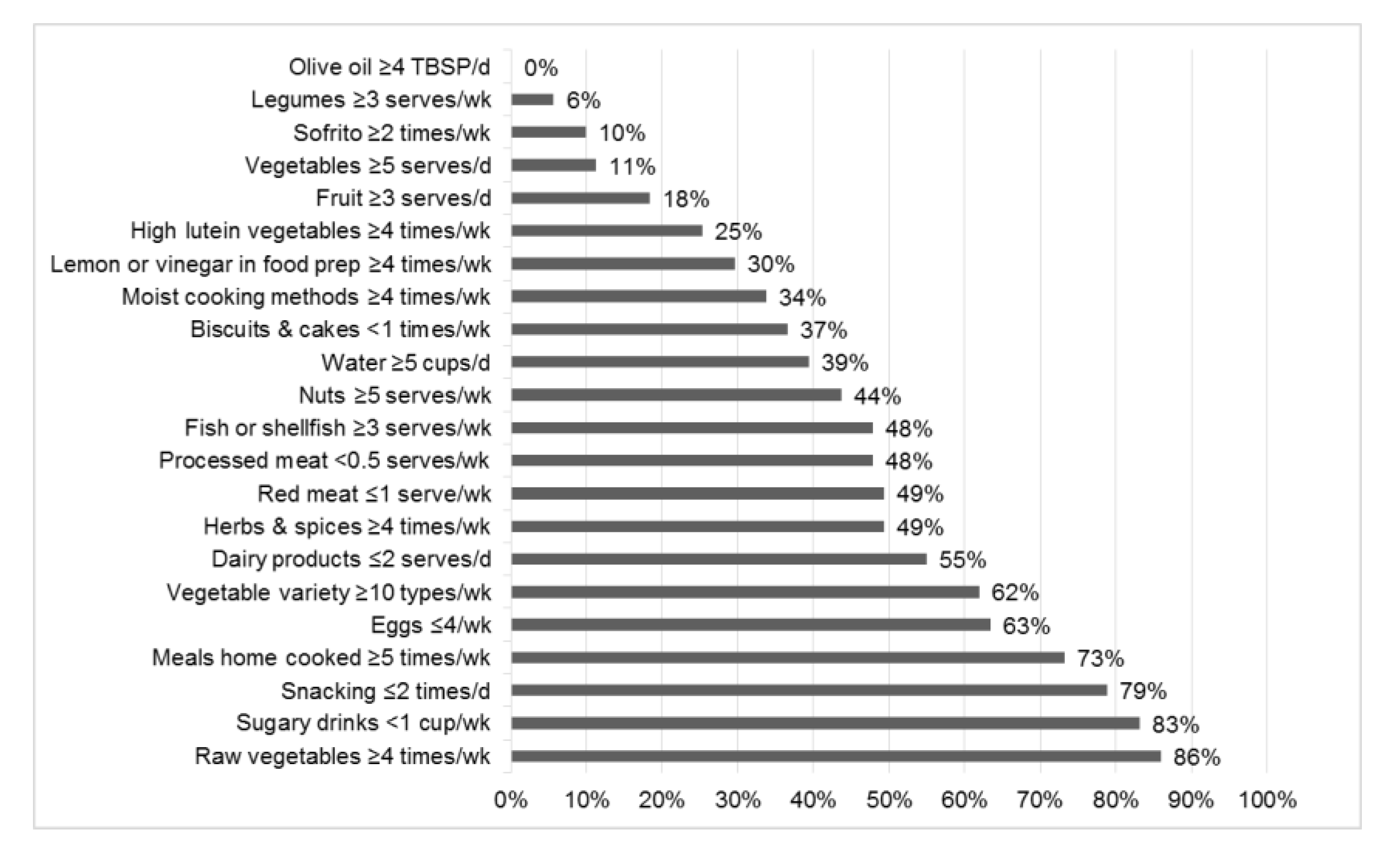
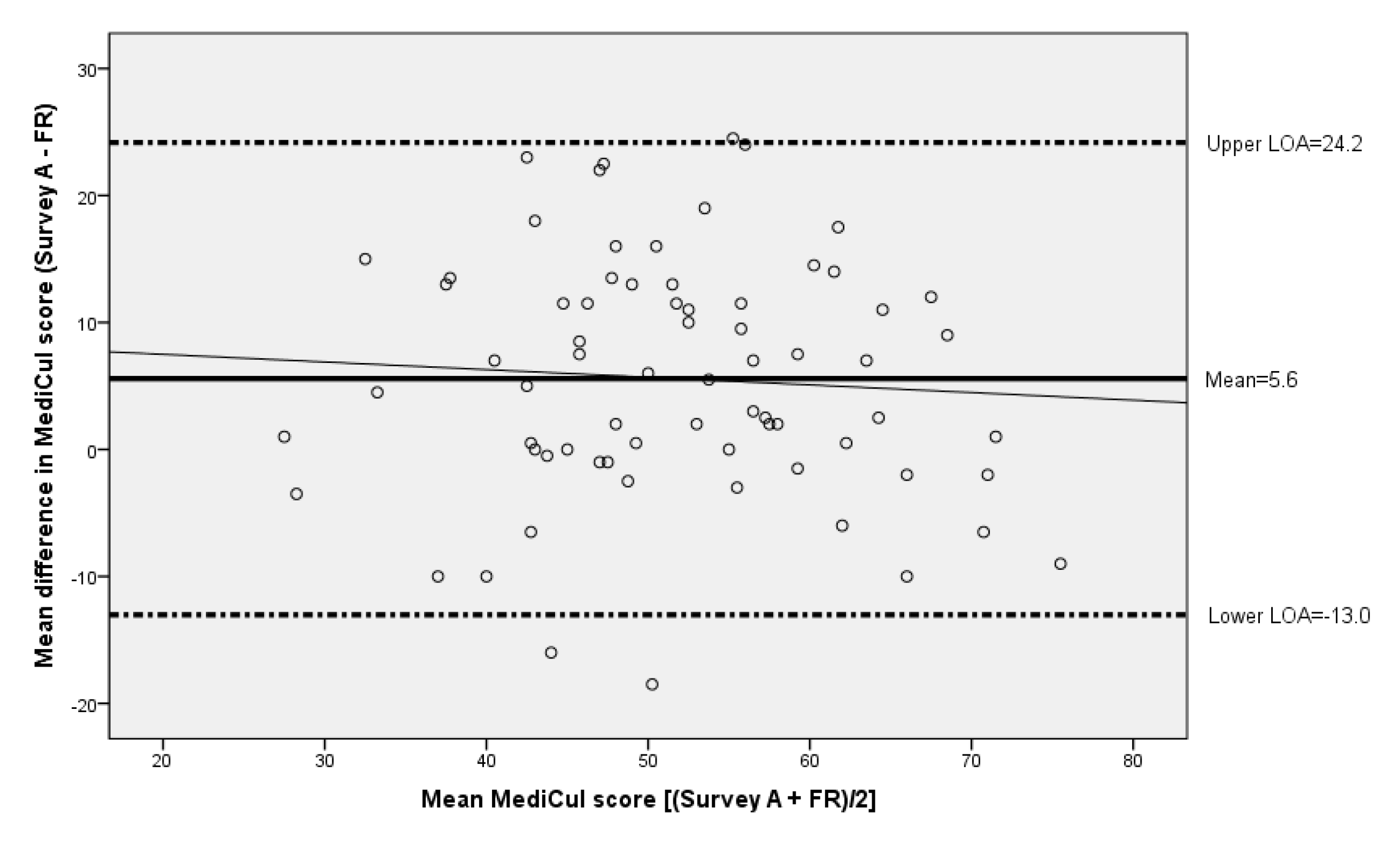
3.2. Validity
4. Discussion
Strengths and Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Esposito, K.; Maiorino, M.I.; Ceriello, A.; Giugliano, D. Prevention and control of type 2 diabetes by Mediterranean diet: A systematic review. Diabetes Res. Clin. Pract. 2010, 89, 97–102. [Google Scholar] [CrossRef] [PubMed]
- Estruch, R.; Ros, E.; Salas-Salvado, J.; Covas, M.I.; Corella, D.; Aros, F.; Gomez-Gracia, E.; Ruiz-Gutierrez, V.; Fiol, M.; Lapetra, J.; et al. Primary prevention of cardiovascular disease with a Mediterranean diet supplemented with extra-virgin olive oil or nuts. N. Engl. J. Med. 2018, 378, e34. [Google Scholar] [CrossRef] [PubMed]
- Jacka, F.N.; O’Neil, A.; Opie, R.; Itsiopoulos, C.; Cotton, S.; Mohebbi, M.; Castle, D.; Dash, S.; Mihalopoulos, C.; Chatterton, M.L.; et al. A randomised controlled trial of dietary improvement for adults with major depression (the ‘SMILES’ trial). BMC Med. 2017, 15, 23. [Google Scholar] [CrossRef] [PubMed]
- Kastorini, C.-M.; Milionis, H.J.; Esposito, K.; Giugliano, D.; Goudevenos, J.A.; Panagiotakos, D.B. The effect of Mediterranean diet on metabolic syndrome and its components: A meta-analysis of 50 studies and 534,906 individuals. J. Am. Coll. Cardiol. 2011, 57, 1299–1313. [Google Scholar] [PubMed]
- Parletta, N.; Zarnowiecki, D.; Cho, J.; Wilson, A.; Bogomolova, S.; Villani, A.; Itsiopoulos, C.; Niyonsenga, T.; Blunden, S.; Meyer, B.; et al. A Mediterranean-style dietary intervention supplemented with fish oil improves diet quality and mental health in people with depression: A randomized controlled trial (HELFIMED). Nutr. Neurosci. 2017. [Google Scholar] [CrossRef] [PubMed]
- Psaltopoulou, T.; Sergentanis, T.N.; Panagiotakos, D.B.; Sergentanis, I.N.; Kosti, R.; Scarmeas, N. Mediterranean diet, stroke, cognitive impairment, and depression: A meta-analysis. Ann. Neurol. 2013, 74, 580–591. [Google Scholar] [CrossRef] [PubMed]
- Radd-Vagenas, S.; Duffy, S.L.; Naismith, S.L.; Brew, B.J.; Flood, V.M.; Fiatarone Singh, M.A. Effect of the Mediterranean diet on cognition and brain morphology and function: A systematic review of randomized controlled trials. Am. J. Clin. Nutr. 2018, 107, 389–404. [Google Scholar] [CrossRef]
- Ryan, M.C.; Itsiopoulos, C.; Thodis, T.; Ward, G.; Trost, N.; Hofferberth, S.; O’Dea, K.; Desmond, P.V.; Johnson, N.A.; Wilson, A.M. The Mediterranean diet improves hepatic steatosis and insulin sensitivity in individuals with non-alcoholic fatty liver disease. J. Hepatol. 2013, 59, 138–143. [Google Scholar] [CrossRef]
- Sofi, F.; Cesari, F.; Abbate, R.; Gensini, G.F.; Casini, A. Adherence to Mediterranean diet and health status: Meta-analysis. BMJ 2008, 337, a1344. [Google Scholar] [CrossRef]
- Sofi, F.; Macchi, C.; Abbate, R.; Gensini, G.F.; Casini, A. Mediterranean diet and health status: An updated meta-analysis and a proposal for a literature-based adherence score. Public Health Nutr. 2014, 17, 2769–2782. [Google Scholar] [CrossRef]
- Trichopoulou, A.; Costacou, T.; Bamia, C.; Trichopoulos, D. Adherence to a Mediterranean diet and survival in a Greek population. N. Engl. J. Med. 2003, 348, 2599–2608. [Google Scholar] [CrossRef] [PubMed]
- D’Alessandro, A.; De Pergola, G. The Mediterranean Diet: Its definition and evaluation of a priori dietary indexes in primary cardiovascular prevention. Int. J. Food Sci. Nutr. 2018, 69, 647–659. [Google Scholar] [CrossRef] [PubMed]
- Radd-Vagenas, S.; Kouris-Blazos, A.; Fiatarone Singh, M.; Flood, V.M. Evolution of Mediterranean diets and cuisine: Concepts and definitions. Asia Pac. J. Clin. Nutr. 2017, 26, 749–763. [Google Scholar] [PubMed]
- Locke, A.; Schneiderhan, J.; Zick, S.M. Diets for health: Goals and guidelines. Am. Fam. Phys. 2018, 97, 721–728. [Google Scholar] [PubMed]
- Martínez-González, M.A.; Sánchez-Tainta, A.; Corella, D.; Salas-Salvadó, J.; Ros, E.; Arós, F.; Gómez-Gracia, E.; Fiol, M.; Lamuela-Raventós, R.M.; Schröder, H.; et al. A provegetarian food pattern and reduction in total mortality in the Prevención con Dieta Mediterránea (PREDIMED) study. Am. J. Clin. Nutr. 2014, 100, 320S–328S. [Google Scholar] [CrossRef] [PubMed]
- Uribarri, J.; Woodruff, S.; Goodman, S.; Cai, W.; Chen, X.; Pyzik, R.; Yong, A.; Striker, G.E.; Vlassara, H. Advanced glycation end products in foods and a practical guide to their reduction in the diet. J. Am. Diet. Assoc. 2010, 110, 911–916. [Google Scholar] [CrossRef] [PubMed]
- D’Alessandro, A.; De Pergola, G. Mediterranean diet and cardiovascular disease: A critical evaluation of a priori dietary indexes. Nutrients 2015, 7, 7863–7888. [Google Scholar] [CrossRef]
- Davis, C.; Bryan, J.; Hodgson, J.; Murphy, K. Definition of the Mediterranean diet: A literature review. Nutrients 2015, 7, 9139–9153. [Google Scholar] [CrossRef]
- Hoffman, R.; Gerber, M. Evaluating and adapting the Mediterranean diet for non-Mediterranean populations: A critical appraisal. Nutr. Rev. 2013, 71, 573–584. [Google Scholar] [CrossRef]
- Kim, H.; Caulfield, L.E.; Rebholz, C.M. Healthy plant-based diets are associated with lower risk of all-cause mortality in US adults. J. Nutr. 2018, 148, 624–631. [Google Scholar] [CrossRef]
- Satija, A.; Bhupathiraju, S.N.; Rimm, E.B.; Spiegelman, D.; Chiuve, S.E.; Borgi, L.; Willett, W.C.; Manson, J.E.; Sun, Q.; Hu, F.B. Plant-based dietary patterns and incidence of type 2 diabetes in US men and women: Results from three prospective cohort studies. PLoS Med. 2016, 13, e1002039. [Google Scholar] [CrossRef] [PubMed]
- Radd-Vagenas, S.; Fiatarone Singh, M.A.; Inskip, M.; Mavros, Y.; Gates, N.; Wilson, G.C.; Jain, N.; Meiklejohn, J.; Brodaty, H.; Wen, W.; et al. Reliability and validity of a Mediterranean diet and culinary index (MediCul) tool in an older population with mild cognitive impairment. Br. J. Nutr. 2018, 120, 1189–1200. [Google Scholar] [CrossRef] [PubMed]
- Tognon, G.; Hebestreit, A.; Lanfer, A.; Moreno, L.A.; Pala, V.; Siani, A.; Tornaritis, M.; De Henauw, S.; Veidebaum, T.; Molnár, D.; et al. Mediterranean diet, overweight and body composition in children from eight European countries: Cross-sectional and prospective results from the IDEFICS study. Nutr. Metab. Cardiovasc. Dis. 2013, 24, 205–213. [Google Scholar] [CrossRef] [PubMed]
- Sotos-Prieto, M.; Santos-Beneit, G.; Bodega, P.; Pocock, S.; Mattei, J.; Penalvo, J.L. Validation of a questionnaire to measure overall Mediterranean lifestyle habits for research application: The MEDiterranean LIFEstyle index (MEDLIFE). Nutr. Hosp. 2015, 32, 1153–1163. [Google Scholar] [PubMed]
- Trichopoulou, A.; Kouris-Blazos, A.; Wahlqvist, M.L.; Gnardellis, C.; Lagiou, P.; Polychronopoulos, E.; Vassilakou, T.; Lipworth, L.; Trichopoulos, D. Diet and overall survival in elderly people. BMJ 1995, 311, 1457–1460. [Google Scholar] [CrossRef] [PubMed]
- Panagiotakos, D.B.; Milias, G.A.; Pitsavos, C.; Stefanadis, C. MedDietScore: A computer program that evaluates the adherence to the Mediterranean dietary pattern and its relation to cardiovascular disease risk. Comput. Methods Programs Biomed. 2006, 83, 73–77. [Google Scholar] [CrossRef] [PubMed]
- Rumawas, M.E.; Dwyer, J.T.; Mckeown, N.M.; Meigs, J.B.; Rogers, G.; Jacques, P.F. The development of the Mediterranean-style dietary pattern score and its application to the American diet in the Framingham Offspring Cohort. J. Nutr. 2009, 139, 1150–1156. [Google Scholar] [CrossRef]
- Schroder, H.; Fito, M.; Estruch, R.; Martinez-Gonzalez, M.A.; Corella, D.; Salas-Salvado, J.; Lamuela-Raventos, R.; Ros, E.; Salaverria, I.; Fiol, M.; et al. A short screener is valid for assessing Mediterranean diet adherence among older Spanish men and women. J. Nutr. 2011, 141, 1140–1145. [Google Scholar] [CrossRef]
- Cerwinske, L.A.; Rasmussen, H.E.; Lipson, S.; Volgman, A.S.; Tangney, C.C. Evaluation of a dietary screener: The Mediterranean Eating Pattern for Americans tool. J. Hum. Nutr. Diet. 2017, 30, 596–603. [Google Scholar] [CrossRef]
- Alberti-Fidanza, A.; Fidanza, F. Mediterranean adequacy index of Italian diets. Public Health Nutr. 2004, 7, 937–941. [Google Scholar] [CrossRef]
- Vitale, M.; Racca, E.; Izzo, A.; Giacco, A.; Parente, E.; Riccardi, G.; Giacco, R. Adherence to the traditional Mediterranean diet in a population of South of Italy: Factors involved and proposal of an educational field-based survey tool. Int. J. Food Sci. Nutr. 2018. [Google Scholar] [CrossRef] [PubMed]
- Cade, J.; Thompson, R.; Burley, V.; Warm, D. Development, validation and utilisation of food-frequency questionnaires-A review. Public Health Nutr. 2002, 5, 567–587. [Google Scholar] [CrossRef] [PubMed]
- Peat, J. Health Science Research: A Handbook of Quantitative Methods, 1st ed.; Allen & Unwin: Crows Nest, Australia, 2001. [Google Scholar]
- 45 and Up Study Collaborators. Cohort Profile: The 45 and Up Study. Int. J. Epidemiol. 2008, 37, 941–947. [Google Scholar] [CrossRef] [PubMed]
- Heffernan, M.; Andrews, G.; Fiatarone Singh, M.A.; Valenzuela, M.; Anstey, K.; Maeder, A.; McNeil, J.J.; Jorm, L.; Lautenschlager, N.; Sachdev, P.; et al. Maintain Your Brain: Protocol of a 3-year randomised controlled trial of an individualised multi-modal eHealth intervention to prevent cognitive decline amongst community dwelling 55 to 77 year olds. J. Alzheimers Dis. 2018, in press. [Google Scholar] [CrossRef] [PubMed]
- Apple App Store. Research Food Diary Xyris Software (Australia) Pty Ltd. Available online: https://itunes.apple.com/au/app/research-food-diary/id1043440131 (accessed on 30 September 2018).
- Ambrosini, G.L.; Hurworth, M.; Giglia, R.; Trapp, G.; Strauss, P. Feasibility of a commercial smartphone application for dietary assessment in epidemiological research and comparison with 24-h dietary recalls. Nutr. J. 2018, 17, 5. [Google Scholar] [CrossRef] [PubMed]
- Lieffers, J.R.L.; Hanning, R.M. Dietary assessment and self-monitoring: With nutrition applications for mobile devices. Can. J. Diet. Pract. Res. 2012, 73, e253–e260. [Google Scholar] [CrossRef] [PubMed]
- Ingwersen, L.; Raper, N.; Anand, J.; Moshfegh, A. Validation study shows importance of probing for forgotten foods during a dietary recall (abstract). J. Am. Diet. Assoc. 2004, 104, 13. [Google Scholar] [CrossRef]
- NIH National Cancer Institute. Automated Self-Administered 24-hour (ASA24) Dietary Assessment Tool. Available online: https://epi.grants.cancer.gov/asa24/respondent/methodology.html (accessed on 2 August 2018).
- Australian Bureau of Statistics. 4364.0.55.007-Australian Health Survey: Nutrition First Results-Foods and Nutrients, 2011–2012; FSANZ: Canberra, Australia, 2014.
- Martínez-González, M.A.; García-Arellano, A.; Toledo, E.; Salas-Salvado, J.; Buil-Cosiales, P.; Corella, D.; Covas, M.I.; Schröder, H.; Arós, F.; Gómez-Gracia, E. A 14-item Mediterranean diet assessment tool and obesity indexes among high-risk subjects: The PREDIMED trial. PLoS ONE 2012, 7, e43134. [Google Scholar] [CrossRef]
- Rosner, B. Fundamentals of Biostatistics, 8th ed.; Cengage Learning: Boston, MA, USA, 2015. [Google Scholar]
- Bland, J.M.; Altman, D.G. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet 1986, 1, 307–310. [Google Scholar] [CrossRef]
- Landis, J.R.; Koch, G.G. The measurement of observer agreement for categorical data. Biometrics 1977, 33, 159–174. [Google Scholar] [CrossRef]
- National Health and Medical Research Council. Clinical Practice Guidelines for the Management of Overweight and Obesity in Adults, Adolescents and Children in Australia; National Health and Medical Research Council: Melbourne, Australia, 2013.
- Papadaki, A.; Johnson, L.; Toumpakari, Z.; England, C.; Rai, M.; Toms, S.; Penfold, C.; Zazpe, I.; Martínez-Gonzalez, M.A.; Feder, G. Validation of the English version of the 14-item Mediterranean Diet Adherence Screener of the PREDIMED study, in people at high cardiovascular risk in the UK. Nutrients 2018, 10, 138. [Google Scholar] [CrossRef] [PubMed]
- Schröder, H.; Marrugat, J.; Vila, J.; Covas, M.I.; Elosua, R. Adherence to the traditional Mediterranean diet is inversely associated with body mass index and obesity in a Spanish population. J. Nutr. 2004, 134, 3355–3361. [Google Scholar] [CrossRef] [PubMed]
- Toledo, E.; Salas-Salvadó, J.; Donat-Vargas, C.; Buil-Cosiales, P.; Estruch, R.; Ros, E.; Corella, D.; Fitó, M.; Hu, F.B.; Arós, F.; et al. Mediterranean diet and invasive breast cancer risk among women at high cardiovascular risk in the PREDIMED trial: Randomized clinical trial. JAMA. Intern. Med. 2015, 175, 1752–1760. [Google Scholar] [CrossRef] [PubMed]
- Valls-Pedret, C.; Sala-Vila, A.; Serra-Mir, M.; Corella, D.; de la Torre, R.; Martínez-González, M.Á.; Martínez-Lapiscina, E.H.; Fitó, M.; Pérez-Heras, A.; Salas-Salvadó, J. Mediterranean diet and age-related cognitive decline: A randomized clinical trial. JAMA. Intern. Med. 2015, 175, 1094–1103. [Google Scholar] [CrossRef] [PubMed]
- Australian Bureau of Statistics. National Health Survey: First Results, 2014-15-Australia, ‘Table 8.3 Body Mass Index, Waist Circumference, Height and Weight’, Time Series Spreadsheet, Cat. No. 4364.0.55.001. Available online: http://www.abs.gov.au/AUSSTATS/abs@.nsf/DetailsPage/4364.0.55.0012014-15?OpenDocument (accessed on 19 September 2018).
- Australian Bureau of Statistics. National Health Survey: First Results, 2014-15-Australia, ‘Table 3.3 Long-Term Health Conditions’, Time Series Spreadsheet, Cat. No. 4364.0.55.0013. Available online: http://www.abs.gov.au/AUSSTATS/abs@.nsf/DetailsPage/4364.0.55.0012014-15?OpenDocument (accessed on 19 September 2018).
- Thompson, F.E.; Subar, A.F. Chapter 1-Dietary Assessment Methodology. In Nutrition in the Prevention and Treatment of Disease, 4th ed.; Coulston, A.M., Boushey, C.J., Ferruzzi, M.G., Delahanty, L.M., Eds.; Academic Press: London, UK, 2017; pp. 5–48. [Google Scholar]
- Ambrosini, G.L.; Van Roosbroeck, S.A.H.; Mackerras, D.; Fritschi, L.; De Klerk, N.H.; Musk, A.W. The reliability of ten-year dietary recall: Implications for cancer research. J. Nutr. 2003, 133, 2663–2668. [Google Scholar] [CrossRef] [PubMed]
| Descriptive Statistics (Mean (SD) or Proportion) | |
|---|---|
| Age (years) | 65.4 (5.9) |
| Females (%) BMI * (kg/m2) | 60 26.1 (4.0) |
| <18.5 (%) | 1.5 |
| 18.5 to 24.9 (%) | 35.4 |
| 25.0 to 29.9 (%) | 47.7 |
| ≥30 (%) | 15.4 |
| Waist circumference *—females (cm) | 91.4 (12.4) |
| ≥88 cm (%) | 56.4 |
| Waist circumference *—males (cm) | 100.2 (8.2) |
| ≥102 cm (%) | 46.2 |
| Resting heart rate * (beats per minute) | 66 (8) |
| Primary cook at home (%) | 49 |
| Primary grocery shopper at home (%) | 51 |
| Supplement use (%) | 63 |
| Number of chronic illnesses/conditions | 1.7 (1.5) |
| Osteoarthritis (%) | 36 |
| Hypercholesterolemia (%) | 30 |
| Hypertension (%) | 24 |
| Gastro-esophageal reflux disease (%) | 16 |
| Depression (%) | 7 |
| Diabetes (%) | 4 |
| Number of medications (median (IQR)) | 1.5 (0.0, 3.0) |
| Mean Difference | 95% CI of the Difference | p Value | |
|---|---|---|---|
| A versus FR * | 5.32 | 3.03, 7.62 | <0.0001 |
| B versus FR | 6.38 | 4.16, 8.59 | <0.0001 |
| Mean AB versus FR | 5.85 | 3.70, 8.00 | <0.0001 |
| Nutrients from Food Record | Source of the MediCul Score Tertile Cut-Off Points | Nutrient Intake for Tertile 1 of the MediCul Score | Nutrient Intake for Tertile 2 of the MediCul Score | Nutrient Intake for Tertile 3 of the MediCul Score | Comparison of Nutrient Intakes across Tertiles of the MediCul Score p Value | Test for Trend p Value, Direction ↑ ↓ † | |||
|---|---|---|---|---|---|---|---|---|---|
| Mean/median | SD/IQR | Mean/median | SD/IQR | Mean/median | SD/IQR | ||||
| Energy kJ/d | FR | 9206 | 2322 | 8330 | 2323 | 9054 | 2342 | 0.386 | 0.810 |
| Survey | 9326 | 2450 | 8526 | 2124 | 8733 | 2435 | 0.468 | 0.380 | |
| Protein g/d | FR | 97 | 25 | 89 | 22 | 101 | 20 | 0.190 | 0.548 |
| Survey | 100 | 24 | 89 | 26 | 97 | 16 | 0.200 | 0.605 | |
| Protein % energy | FR | 18 | 3 | 19 | 4 | 19 | 3 | 0.474 | 0.224 |
| Survey | 19 | 3 | 18 | 4 | 20 | 4 | 0.208 | 0.301 | |
| Fat g/d | FR | 87 | 31 | 77 | 24 | 93 | 33 | 0.189 | 0.491 |
| Survey | 85 | 27 | 83 | 28 | 89 | 37 | 0.790 | 0.661 | |
| Fat % energy | FR | 34 | 6 | 34 | 6 | 38 | 7 | 0.129 | 0.083 |
| Survey | 34 | 5 | 36 | 6 | 37 | 8 | 0.242 | 0.097 | |
| SFA g/d | FR | 32 | 11 | 26 | 11 | 29 | 13 | 0.266 | 0.412 |
| Survey | 30 | 11 | 30 | 12 | 27 | 12 | 0.613 | 0.411 | |
| SFA % energy | FR | 13 | 2 | 12 | 3 | 12 | 4 | 0.428 | 0.269 |
| Survey | 12 | 2 | 13 | 3 | 11 | 3 | 0.191 | 0.588 | |
| SFA % fat | FR | 41 a | 6 | 38 | 8 | 33 | 8 | 0.004 | 0.001 ↓ |
| Survey | 39 | 7 | 39 b | 7 | 34 | 8 | 0.024 | 0.030 ↓ | |
| PUFA g/d | FR | 12 | 9, 16 | 11 b | 9, 16 | 14 | 12, 22 | 0.017 | 0.018 ↑ |
| Survey | 11 | 9, 15 | 12 | 10, 15 | 15 | 11, 22 | 0.146 | 0.087 | |
| PUFA % fat | FR | 16 a | 5 | 18 | 5 | 21 | 7 | 0.021 | 0.007 ↑ |
| Survey | 17 a | 5 | 17 | 5 | 21 | 7 | 0.026 | 0.013 ↑ | |
| MUFA g/d | FR | 35 | 14 | 31 | 10 | 39 | 14 | 0.169 | 0.300 |
| Survey | 35 | 11 | 33 | 12 | 37 | 16 | 0.594 | 0.559 | |
| MUFA % fat | FR | 43 | 4 | 45 | 6 | 45 | 6 | 0.242 | 0.099 |
| Survey | 45 | 5 | 43 | 5 | 45 | 7 | 0.453 | 0.721 | |
| n-3 LC PUFA mg/d | FR | 242 a | 125, 459 | 261 b | 97, 606 | 891 | 290, 1725 | 0.004 | 0.006 ↑ |
| Survey | 241 | 112, 409 | 290 | 176, 670 | 858 | 291, 1583 | 0.035 | 0.025 ↑ | |
| ALA mg/d | FR | 1499 a | 851, 1808 | 1445 | 966, 2005 | 1643 | 1437, 2757 | 0.027 | 0.012 ↑ |
| Survey | 1539 | 908, 2112 | 1489 | 992, 1758 | 1591 | 1308, 2757 | 0.064 | 0.069 | |
| EPA mg/d | FR | 70 a | 24, 138 | 72 b | 29, 200 | 372 | 78, 665 | 0.005 | 0.006 ↑ |
| Survey | 66 a | 24, 117 | 74 b | 42, 243 | 275 | 81, 567 | 0.023 | 0.009 ↑ | |
| DPA mg/d | FR | 69 | 47,129 | 55 | 29, 117 | 136 | 67, 312 | 0.054 | 0.083 |
| Survey | 57 | 37, 129 | 70 | 49, 113 | 130 | 48, 308 | 0.141 | 0.123 | |
| DHA mg/d | FR | 109 a | 43, 235 | 124 b | 30, 345 | 391 | 149, 751 | 0.005 | 0.004 ↑ |
| Survey | 109 a | 42,197 | 149 b | 47, 328 | 409 | 162, 640 | 0.023 | 0.009 ↑ | |
| MUFA:SFA ratio | FR | 1.1 a | 0.9, 1.2 | 1.1 | 0.9, 1.6 | 1.4 | 1.1, 1.7 | 0.010 | 0.003 ↑ |
| Survey | 1.2 | 1.0, 1.4 | 1.1 | 0.9, 1.2 | 1.6 | 1.0, 1.7 | 0.053 | 0.082 | |
| Unsaturated:SFA ratio | FR | 1.5 a | 0.3 | 1.8 | 0.6 | 2.1 | 0.7 | 0.002 | <0.001 ↑ |
| Survey | 1.7 a | 0.5 | 1.6 b | 0.5 | 2.1 | 0.8 | 0.007 | 0.010 ↑ | |
| Cholesterol mg/d | FR | 333 | 155 | 264 | 105 | 322 | 130 | 0.153 | 0.761 |
| Survey | 333 | 128 | 281 | 150 | 306 | 120 | 0.400 | 0.488 | |
| Carbohydrate g/d | FR | 205 | 55 | 192 | 69 | 196 | 63 | 0.782 | 0.618 |
| Survey | 208 | 63 | 197 | 58 | 187 | 66 | 0.500 | 0.241 | |
| Carbohydrate % energy | FR | 37 | 7 | 38 | 6 | 35 | 7 | 0.448 | 0.461 |
| Survey | 37 | 6 | 38 | 6 | 35 | 8 | 0.265 | 0.339 | |
| Sugars g/d | FR | 96 | 34 | 98 | 41 | 94 | 39 | 0.948 | 0.851 |
| Survey | 98 | 34 | 98 | 40 | 91 | 39 | 0.772 | 0.545 | |
| Alcohol g/d | FR | 21 a | 8, 31 | 13 | 1, 26 | 7 | 1, 15 | 0.035 | 0.010 ↓ |
| Survey | 27 a | 12, 34 | 8 | 2, 17 | 8 | 1, 15 | 0.014 | 0.008 ↓ | |
| Water g/d | FR | 2878 | 517 | 3106 | 692 | 3089 | 827 | 0.447 | 0.293 |
| Survey | 2995 | 466 | 2856 | 690 | 3245 | 837 | 0.148 | 0.229 | |
| Dietary fiber g/d | FR | 27 | 8 | 30 | 10 | 33 | 9 | 0.064 | 0.019 ↑ |
| Survey | 29 | 10 | 28 | 7 | 34 | 10 | 0.080 | 0.073 | |
| Vitamin C mg/d | FR | 128 | 43, 151 | 120 | 82, 198 | 120 | 79, 166 | 0.156 | 0.084 |
| Survey | 113 | 64, 166 | 128 | 73, 158 | 123 | 95, 202 | 0.190 | 0.092 | |
| Vitamin E mg/d | FR | 12 | 11, 15 | 14 | 11, 18 | 17 | 12, 22 | 0.083 | 0.042 ↑ |
| Survey | 13 | 12, 18 | 13 | 11, 15 | 18 | 11, 23 | 0.089 | 0.222 | |
| Vitamin B12 μg/d | FR | 4.8 | 3.7, 5.9 | 4.2 | 3.1, 5.2 | 4.5 | 3.6, 6.3 | 0.215 | 0.793 |
| Survey | 4.9 | 3.7, 6.5 | 4.4 | 3.5, 5.7 | 4.4 | 3.6, 5.0 | 0.524 | 0.472 | |
| Folate μg/d‡ | FR | 381 | 119 | 379 | 122 | 403 | 112 | 0.732 | 0.516 |
| Survey | 389 | 123 | 363 | 108 | 414 | 119 | 0.321 | 0.484 | |
| Retinol equivalents μg/d | FR | 1092 | 557 | 1193 | 568 | 1266 | 587 | 0.577 | 0.298 |
| Survey | 1153 | 404 | 972 b | 557 | 1454 | 637 | 0.012 | 0.016 | |
| Beta carotene μg/d | FR | 4567 | 3307 | 5619 | 3245 | 6047 | 3273 | 0.285 | 0.125 |
| Survey | 5043 | 2477 | 4167 b | 3112 | 7196 | 3593 | 0.004 | 0.013 | |
| Sodium mg/d | FR | 2330 | 753 | 2021 | 750 | 1920 | 688 | 0.141 | 0.058 |
| Survey | 2298 | 836 | 2064 | 699 | 1901 | 652 | 0.190 | 0.071 | |
| Potassium mg/d | FR | 3513 | 813 | 3690 | 1057 | 4105 | 945 | 0.096 | 0.036 ↑ |
| Survey | 3691 | 860 | 3520 | 939 | 4124 | 1028 | 0.089 | 0.135 | |
| Sodium:Potassium ratio | FR | 0.7 a | 0.3 | 0.6 | 0.2 | 0.5 | 0.2 | 0.006 | 0.001 ↓ |
| Survey | 0.6 | 0.2 | 0.6 | 0.2 | 0.5 | 0.2 | 0.072 | 0.031 ↓ | |
| Magnesium mg/d | FR | 390 a | 349, 500 | 361 b | 321, 466 | 470 | 440, 525 | 0.006 | 0.005 ↑ |
| Survey | 418 | 333, 489 | 393 | 365, 469 | 466 | 365, 557 | 0.154 | 0.148 | |
| Iron mg/d | FR | 12.1 | 3.3 | 11.7 | 3.4 | 13.2 | 3.5 | 0.288 | 0.254 |
| Survey | 12.9 | 3.6 | 11.1 | 2.7 | 13.1 | 3.7 | 0.091 | 0.030 | |
| Zinc mg/d | FR | 12.1 | 4.0 | 10.7 | 3.2 | 11.9 | 3.1 | 0.336 | 0.868 |
| Survey | 11.8 | 4.2 | 11.1 | 3.1 | 11.8 | 3.1 | 0.721 | 0.960 | |
| Selenium μg/d | FR | 89 | 70, 109 | 91 | 76, 105 | 103 | 92, 134 | 0.035 | 0.017 ↑ |
| Survey | 96 | 81, 117 | 92 | 68, 109 | 96 | 83, 110 | 0.435 | 0.751 | |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Radd-Vagenas, S.; Fiatarone Singh, M.A.; Daniel, K.; Noble, Y.; Jain, N.; O’Leary, F.; Mavros, Y.; Heffernan, M.; Meiklejohn, J.; Guerrero, Y.; et al. Validity of the Mediterranean Diet and Culinary Index (MediCul) for Online Assessment of Adherence to the ‘Traditional’ Diet and Aspects of Cuisine in Older Adults. Nutrients 2018, 10, 1913. https://doi.org/10.3390/nu10121913
Radd-Vagenas S, Fiatarone Singh MA, Daniel K, Noble Y, Jain N, O’Leary F, Mavros Y, Heffernan M, Meiklejohn J, Guerrero Y, et al. Validity of the Mediterranean Diet and Culinary Index (MediCul) for Online Assessment of Adherence to the ‘Traditional’ Diet and Aspects of Cuisine in Older Adults. Nutrients. 2018; 10(12):1913. https://doi.org/10.3390/nu10121913
Chicago/Turabian StyleRadd-Vagenas, Sue, Maria A. Fiatarone Singh, Kenneth Daniel, Yian Noble, Nidhi Jain, Fiona O’Leary, Yorgi Mavros, Megan Heffernan, Jacinda Meiklejohn, Yareni Guerrero, and et al. 2018. "Validity of the Mediterranean Diet and Culinary Index (MediCul) for Online Assessment of Adherence to the ‘Traditional’ Diet and Aspects of Cuisine in Older Adults" Nutrients 10, no. 12: 1913. https://doi.org/10.3390/nu10121913
APA StyleRadd-Vagenas, S., Fiatarone Singh, M. A., Daniel, K., Noble, Y., Jain, N., O’Leary, F., Mavros, Y., Heffernan, M., Meiklejohn, J., Guerrero, Y., Chau, T., Sachdev, P. S., Brodaty, H., & Flood, V. M. (2018). Validity of the Mediterranean Diet and Culinary Index (MediCul) for Online Assessment of Adherence to the ‘Traditional’ Diet and Aspects of Cuisine in Older Adults. Nutrients, 10(12), 1913. https://doi.org/10.3390/nu10121913







