Substitution of Fish for Red Meat or Poultry and Risk of Ischemic Stroke
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Population
2.2. Exposure
2.3. Covariates
2.4. Ischemic Stroke Cases
2.5. Statistical Analyses
3. Results
3.1. Cohort and Ischemic Stroke Cases
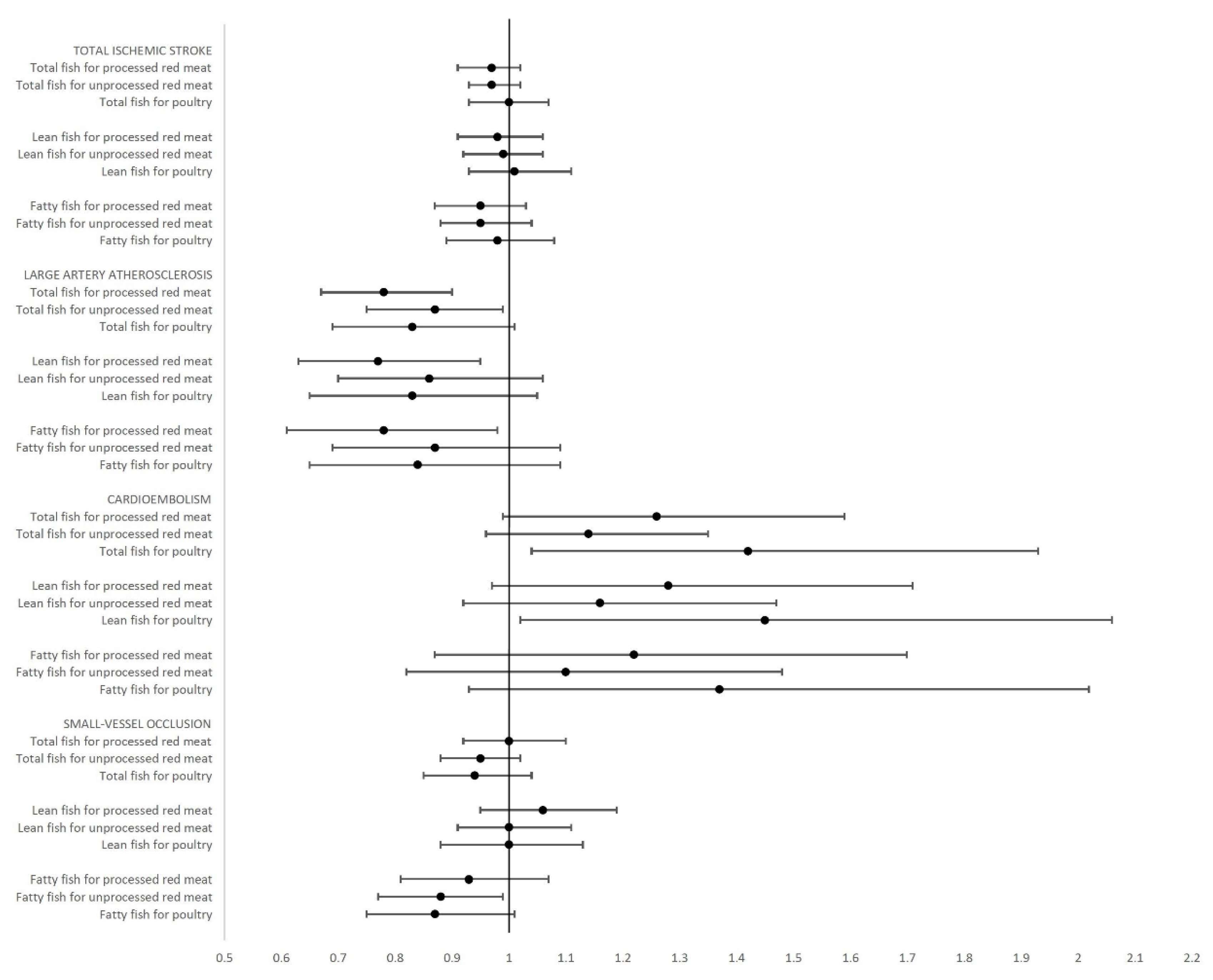
3.2. Total Ischemic Stroke
3.3. Large Artery Atherosclerosis
3.4. Cardioembolism
3.5. Small-Vessel Occlusion
3.6. Further Adjustment
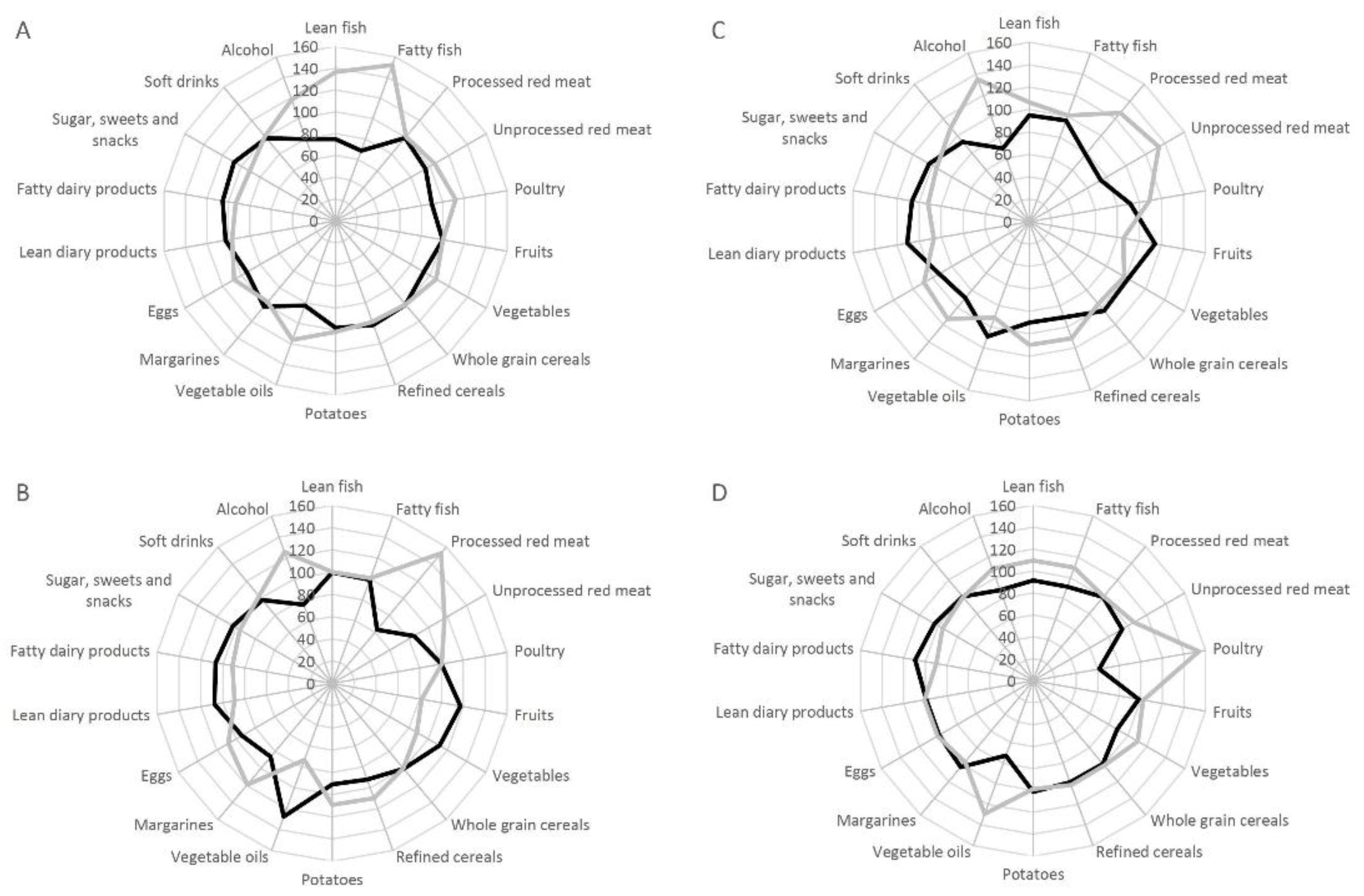
3.7. Dietary Pattern
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Strong, K.; Mathers, C.; Bonita, R. Preventing stroke: Saving lives around the world. Lancet Neurol. 2007, 6, 182–187. [Google Scholar] [CrossRef]
- Larsson, S.C.; Orsini, N. Fish Consumption and the risk of stroke: A dose-response meta-analysis. Stroke 2011, 42, 3621–3623. [Google Scholar] [CrossRef] [PubMed]
- Chowdhury, R.; Stevens, S.; Gorman, D.; Pan, A.; Warnakula, S.; Chowdhury, S.; Ward, H.; Johnson, L.; Crowe, F.; Hu, F.B.; et al. Association between fish consumption, long chain omega 3 fatty acids, and risk of cerebrovascular disease: Systematic review and meta-analysis. BMJ 2012, 345, e6698. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Xun, P.; Qin, B.; Song, Y.; Nakamura, Y.; Kurth, T.; Yaemsiri, S.; Djousse, L.; He, K. Fish consumption and risk of stroke and its subtypes: Accumulative evidence from a meta-analysis of prospective cohort Studies. Eur. J. Clin. Nutr. 2012, 66, 1199–1207. [Google Scholar] [CrossRef] [PubMed]
- Willett, W.C.; Howe, G.R.; Kushi, L.H. Adjustment for total energy intake in epidemiologic studies. Am. J. Clin. Nutr. 1997, 65, S1220–S1228. [Google Scholar] [CrossRef] [PubMed]
- Rimm, E.B.; Appel, L.J.; Chiuve, S.E.; Djousse, L.; Engler, M.B.; Kris-Etherton, P.M.; Mozaffarian, D.; Siscovick, D.S.; Lichtenstein, A.H.; American Heart Association Nutrition Committee of the Council on Lifestyle and Cardiometabolic Health; et al. Seafood long-chain n-3 polyunsaturated fatty acids and cardiovascular disease: A science advisory from the American Heart Association. Circulation 2018, 138, e35–e47. [Google Scholar] [CrossRef] [PubMed]
- Mozaffarian, D.; Wu, J.H. Omega-3 fatty acids and cardiovascular disease: Effects on risk factors, molecular pathways, and clinical events. J. Am. Coll. Cardiol. 2011, 58, 2047–2067. [Google Scholar] [CrossRef] [PubMed]
- De Caterina, R. N-3 fatty acids in cardiovascular disease. N. Engl. J. Med. 2011, 364, 2439–2450. [Google Scholar] [CrossRef] [PubMed]
- Larsson, S.C.; Virtamo, J.; Wolk, A. Red meat consumption and risk of stroke in Swedish men. Am. J. Clin. Nutr. 2011, 94, 417–421. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Larsson, S.C.; Virtamo, J.; Wolk, A. Red meat consumption and risk of stroke in Swedish women. Stroke 2011, 42, 324–329. [Google Scholar] [CrossRef] [PubMed]
- Bernstein, A.M.; Pan, A.; Rexrode, K.M.; Stampfer, M.; Hu, F.B.; Mozaffarian, D.; Willett, W.C. Dietary protein sources and the risk of stroke in men and women. Stroke 2012, 43, 637–644. [Google Scholar] [CrossRef] [PubMed]
- Takata, Y.; Shu, X.O.; Gao, Y.T.; Li, H.; Zhang, X.; Gao, J.; Cai, H.; Yang, G.; Xiang, Y.B.; Zheng, W. Red meat and poultry intakes and risk of total and cause-specific mortality: Results from cohort studies of Chinese adults in Shanghai. PLoS ONE 2013, 8, e56963. [Google Scholar] [CrossRef] [PubMed]
- Haring, B.; Misialek, J.R.; Rebholz, C.M.; Petruski-Ivleva, N.; Gottesman, R.F.; Mosley, T.H.; Alonso, A. Association of dietary protein consumption with incident silent cerebral infarcts and stroke: The Atherosclerosis Risk in Communities (ARIC) study. Stroke 2015, 46, 3443–3450. [Google Scholar] [CrossRef] [PubMed]
- Amiano, P.; Chamosa, S.; Etxezarreta, N.; Arriola, L.; Sanchez, M.J.; Ardanaz, E.; Molina-Montes, E.; Chirlaque, M.D.; Moreno-Iribas, C.; Huerta, J.M.; et al. Unprocessed red meat and processed meat consumption and risk of stroke in the Spanish cohort of the European Prospective Investigation into Cancer and Nutrition (EPIC). Eur. J. Clin. Nutr. 2016, 70, 313–319. [Google Scholar] [CrossRef] [PubMed]
- Tjønneland, A.; Olsen, A.; Boll, K.; Stripp, C.; Christensen, J.; Engholm, G.; Overvad, K. Study design, exposure variables, and socioeconomic determinants of participation in diet, cancer and health: A population-based prospective cohort study of 57,053 men and women in Denmark. Scand. J. Public Health 2007, 35, 432–441. [Google Scholar] [CrossRef] [PubMed]
- Overvad, K.; Tjønneland, A.; Haraldsdottir, J.; Ewertz, M.; Jensen, O.M. Development of a semiquantitative food frequency questionnaire to assess food, energy and nutrient intake in Denmark. Int. J. Epidemiol. 1991, 20, 900–905. [Google Scholar] [CrossRef] [PubMed]
- Tjønneland, A.; Overvad, K.; Haraldsdottir, J.; Bang, S.; Ewertz, M.; Jensen, O.M. Validation of a semiquantitative food frequency questionnaire developed in Denmark. Int. J. Epidemiol. 1991, 20, 906–912. [Google Scholar] [CrossRef] [PubMed]
- Lühdorf, P.; Overvad, K.; Schmidt, E.B.; Johnsen, S.P.; Bach, F.W. Predictive value of stroke discharge diagnoses in the Danish national patient register. Scand. J. Public Health 2017, 1403494817716582. [Google Scholar] [CrossRef] [PubMed]
- Venø, S.K.; Bork, C.S.; Jakobsen, M.U.; Lundbye-Christensen, S.; Bach, F.W.; Overvad, K.; Schmidt, E.B. Linoleic acid in adipose tissue and development of ischemic stroke: A Danish case-cohort study. J. Am. Heart Assoc. 2018, 7. [Google Scholar] [CrossRef] [PubMed]
- Adams, H.P.; Bendixen, B.H.; Kappelle, L.J.; Biller, J.; Love, B.B.; Gordon, D.L.; Marsh, E.E., 3rd. Classification of subtype of acute ischemic stroke. Definitions for use in a Multicenter Clinical Trial. TOAST. Trial of Org 10172 in Acute Stroke Treatment. Stroke 1993, 24, 35–41. [Google Scholar] [CrossRef] [PubMed]
- Willett, W.; Stampfer, M.J. Total energy intake: Implications for epidemiologic analyses. Am. J. Epidemiol. 1986, 124, 17–27. [Google Scholar] [CrossRef] [PubMed]
- Mozaffarian, D.; Appel, L.J.; Van Horn, L. Components of a cardioprotective diet: New insights. Circulation 2011, 123, 2870–2891. [Google Scholar] [CrossRef] [PubMed]
- Mozaffarian, D. Fish, Mercury, Selenium and cardiovascular risk: Current evidence and unanswered questions. Int. J. Environ. Res. Public. Health. 2009, 6, 1894–1916. [Google Scholar] [CrossRef] [PubMed]
- Thomsen, S.T.; Pires, S.M.; Devleesschauwer, B.; Poulsen, M.; Fagt, S.; Ygil, K.H.; Andersen, R. Investigating the risk-benefit balance of substituting red and processed meat with fish in a Danish diet. Food Chem. Toxicol. 2018, 120, 50–63. [Google Scholar] [CrossRef] [PubMed]
- Perkins, J.T.; Petriello, M.C.; Newsome, B.J.; Hennig, B. Polychlorinated biphenyls and links to cardiovascular disease. Environ. Sci. Pollut. Res. Int. 2016, 23, 2160–2172. [Google Scholar] [CrossRef] [PubMed]
- Salonen, J.T.; Seppanen, K.; Lakka, T.A.; Salonen, R.; Kaplan, G.A. Mercury accumulation and accelerated progression of carotid atherosclerosis: A population-based prospective 4-year follow-up study in men in Eastern Finland. Atherosclerosis 2000, 148, 265–273. [Google Scholar] [CrossRef]
- Micha, R.; Michas, G.; Mozaffarian, D. Unprocessed red and processed meats and risk of coronary artery disease and type 2 diabetes—An updated review of the evidence. Curr. Atheroscler. Rep. 2012, 14, 515–524. [Google Scholar] [CrossRef] [PubMed]
- Kaluza, J.; Wolk, A.; Larsson, S.C. Heme iron intake and risk of stroke: A prospective study of men. Stroke 2013, 44, 334–339. [Google Scholar] [CrossRef] [PubMed]
- Benjamin, E.J.; Blaha, M.J.; Chiuve, S.E.; Cushman, M.; Das, S.R.; Deo, R.; de Ferranti, S.D.; Floyd, J.; Fornage, M.; Gillespie, C.; et al. Heart disease and stroke statistics-2017 update: A report from the American Heart Association. Circulation 2017, 135, e146–e603. [Google Scholar] [CrossRef] [PubMed]
- Kotur-Stevuljevic, J.; Bogavac-Stanojevic, N.; Jelic-Ivanovic, Z.; Stefanovic, A.; Gojkovic, T.; Joksic, J.; Sopic, M.; Gulan, B.; Janac, J.; Milosevic, S. Oxidative stress and paraoxonase 1 status in acute ischemic stroke patients. Atherosclerosis 2015, 241, 192–198. [Google Scholar] [CrossRef] [PubMed]
- Honikel, K.O. The use and control of nitrate and nitrite for the processing of meat products. Meat Sci. 2008, 78, 68–76. [Google Scholar] [CrossRef] [PubMed]
- Lawes, C.M.; Bennett, D.A.; Feigin, V.L.; Rodgers, A. Blood pressure and stroke: An overview of published reviews. Stroke 2004, 35, 1024. [Google Scholar] [CrossRef] [PubMed]
- Mensink, R.P.; Zock, P.L.; Kester, A.D.; Katan, M.B. Effects of dietary fatty acids and carbohydrates on the ratio of serum total to hdl cholesterol and on serum lipids and apolipoproteins: A meta-analysis of 60 controlled trials. Am. J. Clin. Nutr. 2003, 77, 1146–1155. [Google Scholar] [CrossRef] [PubMed]
- Shen, J.; Johnson, V.M.; Sullivan, L.M.; Jacques, P.F.; Magnani, J.W.; Lubitz, S.A.; Pandey, S.; Levy, D.; Vasan, R.S.; Quatromoni, P.A.; et al. Dietary factors and incident atrial fibrillation: The Framingham Heart Study. Am. J. Clin. Nutr. 2011, 93, 261–266. [Google Scholar] [CrossRef] [PubMed]
- Rix, T.A.; Joensen, A.M.; Riahi, S.; Lundbye-Christensen, S.; Tjonneland, A.; Schmidt, E.B.; Overvad, K. A u-shaped association between consumption of marine n-3 fatty acids and development of atrial fibrillation/atrial flutter-a Danish cohort study. Europace 2014, 16, 1554–1561. [Google Scholar] [CrossRef] [PubMed]
| Cohort (n = 55,338) | Ischemic Stroke Cases (n = 1879) | |||
|---|---|---|---|---|
| Age at enrolment (year) | 56.1 | (50.7–64.2) | 58.8 | (51.0–64.7) |
| Sex % (n) | ||||
| Male | 47.6 | (26,351) | 61.7 | (1160) |
| Female | 52.4 | (28,987) | 38.3 | (719) |
| Total energy intake (kcal/week) | 15,911 | (9859–24,600) | 16,269 | (9978–25,485) |
| Length of schooling % (n) | ||||
| <7 years | 32.8 | (18,177) | 40.7 | (764) |
| 8–10 years | 46.1 | (25,515) | 42.5 | (799) |
| >10 years | 21.1 | (11,646) | 16.8 | (316) |
| Physical activity (hours/week) | 2.5 | (0.0–11.0) | 2.0 | (0.0–11.0) |
| Body mass index (kg/m2) | 25.5 | (20.5–33.3) | 26.2 | (20.7–34.8) |
| Waist circumference (cm) | 88.8 | (69.0–110.0) | 93.0 | (71.0–115.0) |
| Alcohol intake (g/day) | 12.9 | (0.7–64.6) | 14.6 | (0.4–79.4) |
| Alcohol abstain % (n) | ||||
| Yes | 2.3 | (1271) | 3.2 | (60) |
| No | 97.7 | (54,067) | 96.8 | (1819) |
| Smoking status % (n) | ||||
| Non-current smoker | 64.1 | (35,462) | 49.6 | (933) |
| Current smoker <15 g/day | 13.0 | (7214) | 15.5 | (291) |
| Current smoker ≥15 g/day | 22.9 | (12,662) | 34.9 | (655) |
| Hypercholesterolemia % (n) | ||||
| Yes | 7.3 | (4065) | 10.5 | (198) |
| No | 50.3 | (27,834) | 48.9 | (918) |
| Unknown | 42.4 | (23,444) | 40.6 | (763) |
| Hypertension % (n) | ||||
| Yes | 16.0 | (8865) | 28.4 | (533) |
| No | 70.9 | (39,226) | 58.3 | (1096) |
| Unknown | 13.1 | (7247) | 13.3 | (250) |
| Diabetes mellitus % (n) | ||||
| Yes | 2.0 | (1116) | 4.6 | (87) |
| No | 93.4 | (51,660) | 89.4 | (1679) |
| Unknown | 4.6 | (2562) | 6.0 | (113) |
| Atrial fibrillation/atrial flutter % (n) | ||||
| Yes | 0.8 | (423) | 1.5 | (28) |
| No | 99.2 | (54,915) | 98.5 | (1851) |
| Dietary intake | ||||
| Total fish | 38.1 | (11.3–91.5) | 39.2 | (11.5–94.6) |
| Lean fish | 22.5 | (6.6–57.2) | 23.4 | (5.7–60.2) |
| Fatty fish | 13.5 | (2.1–43.4) | 13.6 | (2.0–45.4) |
| Processed red meat | 24.6 | (5.2–75.1) | 28.2 | (6.5–84.7) |
| Unprocessed red meat | 74.4 | (29.6–158.9) | 82.0 | (32.6–168.4) |
| Poultry | 17.9 | (3.5–59.1) | 17.2 | (3.4–62.1) |
| Total Ischemic Stroke | Large Artery Atherosclerosis | Cardioembolism | Small-vessel Occlusion | Stroke of Other Etiology | Stroke of Undetermined Etiology | |
|---|---|---|---|---|---|---|
| Substitutions 150 g/week | HR (95% CI) | HR (95% CI) | HR (95% CI) | HR (95% CI) | HR (95% CI) | HR (95% CI) |
| Total fish | ||||||
| Processed red meat | 0.97 (0.91; 1.02) | 0.78 (0.67; 0.90) | 1.26 (0.99; 1.59) | 1.00 (0.92; 1.10) | 0.97 (0.77; 1.22) | 0.96 (0.87; 1.06) |
| Unprocessed red meat | 0.97 (0.93; 1.02) | 0.87 (0.75; 0.99) | 1.14 (0.96; 1.35) | 0.95 (0.88; 1.02) | 1.02 (0.83; 1.26) | 1.01 (0.93; 1.11) |
| Poultry | 1.00 (0.93; 1.07) | 0.83 (0.69; 1.01) | 1.42 (1.04; 1.93) | 0.94 (0.85; 1.04) | 1.11 (0.81; 1.54) | 1.09 (0.95; 1.25) |
| Lean fish | ||||||
| Processed red meat | 0.98 (0.91; 1.06) | 0.77 (0.63; 0.95) | 1.28 (0.97; 1.71) | 1.06 (0.95; 1.19) | 0.99 (0.73; 1.36) | 0.92 (0.80; 1.05) |
| Unprocessed red meat | 0.99 (0.92; 1.06) | 0.86 (0.70; 1.06) | 1.16 (0.92; 1.47) | 1.00 (0.91; 1.11) | 1.05 (0.78; 1.42) | 0.96 (0.84; 1.10) |
| Poultry | 1.01 (0.93; 1.11) | 0.83 (0.65; 1.05) | 1.45 (1.02; 2.06) | 1.00 (0.88; 1.13) | 1.14 (0.78; 1.69) | 1.03 (0.87; 1.22) |
| Fatty fish | ||||||
| Processed red meat | 0.95 (0.87; 1.03) | 0.78 (0.61; 0.98) | 1.22 (0.87; 1.70) | 0.93 (0.81; 1.07) | 0.93 (0.63; 1.36) | 1.03 (0.88; 1.20) |
| Unprocessed red meat | 0.95 (0.88; 1.04) | 0.87 (0.69; 1.09) | 1.10 (0.82; 1.48) | 0.88 (0.77; 0.99) | 0.98 (0.68; 1.41) | 1.08 (0.93; 1.25) |
| Poultry | 0.98 (0.89; 1.08) | 0.84 (0.65; 1.09) | 1.37 (0.93; 2.02) | 0.87 (0.75; 1.01) | 1.07 (0.69; 1.66) | 1.16 (0.97; 1.39) |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Venø, S.K.; Bork, C.S.; Jakobsen, M.U.; Lundbye-Christensen, S.; Bach, F.W.; McLennan, P.L.; Tjønneland, A.; Schmidt, E.B.; Overvad, K. Substitution of Fish for Red Meat or Poultry and Risk of Ischemic Stroke. Nutrients 2018, 10, 1648. https://doi.org/10.3390/nu10111648
Venø SK, Bork CS, Jakobsen MU, Lundbye-Christensen S, Bach FW, McLennan PL, Tjønneland A, Schmidt EB, Overvad K. Substitution of Fish for Red Meat or Poultry and Risk of Ischemic Stroke. Nutrients. 2018; 10(11):1648. https://doi.org/10.3390/nu10111648
Chicago/Turabian StyleVenø, Stine K., Christian S. Bork, Marianne U. Jakobsen, Søren Lundbye-Christensen, Flemming W. Bach, Peter L. McLennan, Anne Tjønneland, Erik B. Schmidt, and Kim Overvad. 2018. "Substitution of Fish for Red Meat or Poultry and Risk of Ischemic Stroke" Nutrients 10, no. 11: 1648. https://doi.org/10.3390/nu10111648
APA StyleVenø, S. K., Bork, C. S., Jakobsen, M. U., Lundbye-Christensen, S., Bach, F. W., McLennan, P. L., Tjønneland, A., Schmidt, E. B., & Overvad, K. (2018). Substitution of Fish for Red Meat or Poultry and Risk of Ischemic Stroke. Nutrients, 10(11), 1648. https://doi.org/10.3390/nu10111648






