Association between Physical Condition and Body Composition, Nutrient Intake, Sociodemographic Characteristics, and Lifestyle Habits in Older Spanish Adults
Abstract
1. Introduction
2. Methods
2.1. Study Design, Population, and Ethics
2.2. Body Composition
2.3. Socioeconomic and Lifestyle Determinants
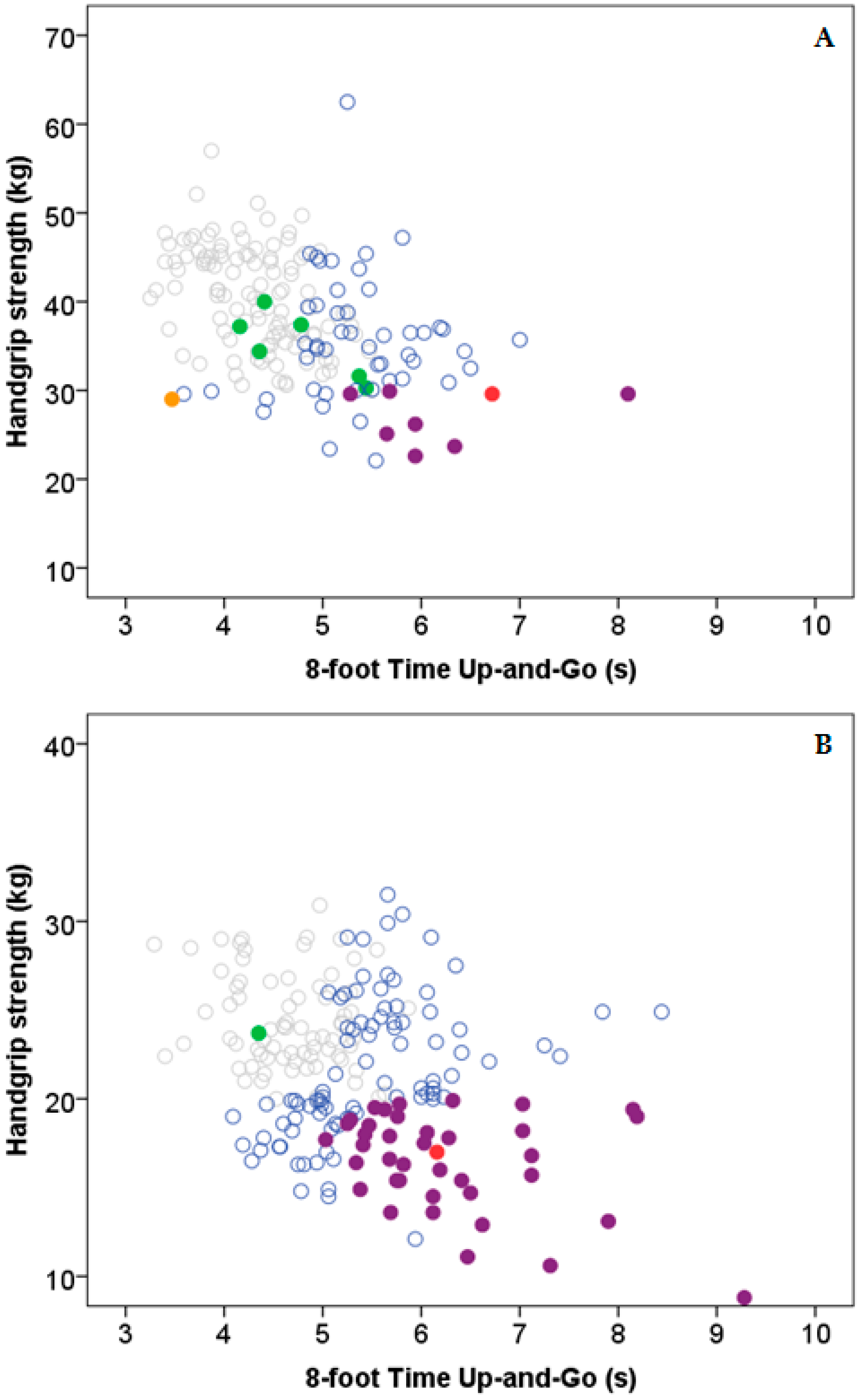
2.4. Physical Condition and Sarcopenia Definition
2.4.1. Handgrip Strength Test (HGS)
2.4.2. Agility/Dynamic Balance Test (8-f TUG)
2.5. Dietary Intake Assessment
2.6. Statistics
3. Results
4. Discussion
Strengths and Limitations
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Availability of Data and Materials
Abbreviations
| ASMI | appendicular skeletal muscle index |
| BMI | Body mass index |
| CI | Confidence interval |
| EWGSOP | European Working Group on Sarcopenia in Older People |
| 8-f TUG | 8-foot time up-and-go test; HGS: handgrip strength test |
| ISAK | International Society for the Advancement of Kinanthropometry |
| LTPA | Leisure-time physical activity |
| OR | Odds ratio |
| SPSS | Statistical Package for the Social Sciences |
| WHO | World Health Organization |
References
- Börsch-Supan, A.; Brugiavini, A.; Jürges, H.; Mackenbach, J.; Siegrist, J.; Weber, G. Health, ageing and retirement in Europe. First results from the Survey of Health, Ageing and Retirement in Europe. Manheim: Manheim Research Institute for the Economics of Aging. 2005. Available online: http://www.share-project.org/uploads/tx_sharepublications/SHARE_FirstResultsBookWave1.pdf (accessed on 18 February 2017).
- Ministerio de Sanidad, Servicios Sociales e Igualdad. Estrategia de Promoción de la Salud y Prevención en el SNS. Documento Consenso sobre Prevención de Fragilidad y Caídas en la Persona Mayor. 2014. Available online: http://www.msssi.gob.es/profesionales/saludPublica/prevPromocion/Estrategia/docs/FragilidadyCaidas_personamayor.pdf (accessed on 18 February 2017).
- Abellan van Kan, G.; Rolland, Y.; Bergman, H.; Morley, J.E.; Kritchevsky, S.B.; Vellas, B. The I.A.N.A Task Force on frailty assessment of older people in clinical practice. J. Nutr. Health Aging 2008, 12, 29–37. [Google Scholar] [CrossRef] [PubMed]
- Cruz-Jentoft, A.J.; Baeyens, J.P.; Bauer, J.M.; Boirie, Y.; Cederholm, T.; Landi, F.; Martin, F.C.; Michel, J.P.; Rolland, Y.; Schneider, S.M.; et al. Sarcopenia: European consensus on definition and diagnosis: Report of the European Working Group on Sarcopenia in Older People. Age Ageing 2010, 39, 412–423. [Google Scholar] [CrossRef] [PubMed]
- Clegg, A.; Young, J.; Iliffe, S.; Rikkert, M.O.; Rockwood, K. Frailty in elderly people. Lancet 2013, 38, 752–762. [Google Scholar] [CrossRef]
- Bijlsma, A.Y.; Meskers, C.G.M.; Ling, C.H.Y.; Narici, M.; Kurrle, S.E.; Cameron, I.D.; Westendorp, R.G.J.; Maier, A.B. Defining sarcopenia: The impact of different diagnostic criteria on the prevalence of sarcopenia in a large middle aged cohort. Age 2013, 35, 871–881. [Google Scholar] [CrossRef] [PubMed]
- Dupuy, C.; Lauwers-Cances, V.; Guyonnet, S.; Gentil, C.; Abellan van Kan, G.; Beauchet, O.; Schott, A.M.; Vellas, B.; Rolland, Y. Searching for a relevant definition of sarcopenia: Results from the cross-sectional EPIDOS study. J. Cachexia Sarcopenia Muscle 2015, 6, 144–154. [Google Scholar] [CrossRef] [PubMed]
- Patiño Villada, F.A.; Arboleda Franco, S.A.; De Paz Fernández, J.A. Sarcopenia in community-dwelling persons over 60 years of age from a northern Spanish city: Relationship between diagnostic criteria and association with the functional performance. Nutr. Hosp. 2015, 31, 2154–2160. [Google Scholar] [PubMed]
- Legrand, D.; Vaes, B.; Matheï, C.; Adriaensen, W.; Van Pottelbergh, G.; Degryse, J.M. Muscle strength and physical performance as predictors of mortality, hospitalization, and disability in the oldest old. J. Am. Geriatr. Soc. 2014, 62, 1030–1038. [Google Scholar] [CrossRef] [PubMed]
- Aggio, D.A.; Sartini, C.; Papacosta, O.; Lennon, L.T.; Ash, S.; Whincup, P.H.; Wannamethee, S.G.; Jefferis, B.J. Cross-sectional associations of objectively measured physical activity and sedentary time with sarcopenia and sarcopenic obesity in older men. Prev. Med. 2016, 91, 264–272. [Google Scholar] [CrossRef] [PubMed]
- Tseng, L.A.; Delmonico, M.J.; Visser, M.; Boudreau, R.M.; Goodpaster, B.H.; Schwartz, A.V.; Simonsick, E.M.; Satterfield, S.; Harris, T.; Newman, A.B. Body composition explains sex differential in physical performance among older adults. J. Gerontol. A Biol. Sci. Med. Sci. 2014, 69, 93–100. [Google Scholar] [CrossRef] [PubMed]
- Dagan, S.S.; Segev, S.; Novikov, I.; Dankner, R. waist circumference vs. body mass index in assosciation with cardiorespiratory fitness in healthy men and women: A cross sectional analysis of 403 subjects. Nutr. J. 2013, 12, 12. [Google Scholar] [CrossRef] [PubMed]
- Brach, J.S.; Van Swearingen, J.M.; Newman, A.B.; Kriska, A.M. Identifying early decline of physical function in community-dwelling older women: Performance- based and self-report measures. Phys. Ther. 2002, 82, 320–328. [Google Scholar] [PubMed]
- Jones, C.J.; Rikli, R.E. Measuring functional fitness of older adults. J. Active Aging 2002, 24–30. [Google Scholar]
- Bibiloni, M.D.M.; Julibert, A.; Argelich, E.; Aparicio-Ugarriza, R.; Palacios, G.; Pons, A.; Gonzalez-Gross, M.; Tur, J.A. Western and Mediterranean Dietary Patterns and Physical Activity and Fitness among Spanish Older Adults. Nutrients 2017, 9, 704. [Google Scholar] [CrossRef] [PubMed]
- Guasch-Ferré, M.; Salas-Salvadó, J.; Ros, E.; Estruch, R.; Corella, D.; Fitó, M.; Martínez-González, M.A.; PREDIMED Investigators. The PREDIMED trial, Mediterranean diet and health outcomes: How strong is the evidence? Nutr. Metab. Cardiovasc. Dis. 2017, 27, 624–632. [Google Scholar] [CrossRef] [PubMed]
- International Society for the Advancement of Kinanthropometry (ISAK). International Standards for Anthropometric Assessment. Underdale, S. Australia: International Society for the Advancement of Kinanthropometry. Available online: http://www.ceap.br/material/MAT17032011184632.pdf (accessed on 18 February 2017).
- TANITA. BC-418 Segmental Body Composition Analyzer. Available online: https://www.tanita.com/en/bc-418/ (accessed on 7 September 2018).
- Esquius, M.; Schwartz, S.; López Hellín, J.; Andreu, A.L.; García, E. Anthropometric reference parameters for the aged population. Med. Clin. 1993, 100, 692–698. [Google Scholar]
- Sociedad Española de Nutrición Parenteral y Enteral (SENPE); Sociedad Española de Geriatría y Gerontología (SEGG). Valoración Nutricional en el Anciano. Recomendaciones Prácticas de los Expertos en Geriatría y Nutrición; Galénitas-Nigra Trea: Bilbao, Spain, 2007; ISBN 978-84-95364-55-5. [Google Scholar]
- Gallagher, D.; Heymsfield, S.B.; Heo, M.; Jebb, S.A.; Murgatroyd, P.R.; Sakamoto, Y. Healthy percentage body fat ranges: An approach for developing guidelines based on body mass index. Am. J. Clin. Nutr. 2000, 72, 694–701. [Google Scholar] [CrossRef] [PubMed]
- Ashwell, M.; Gunn, P.; Gibson, S. Waist-to-height ratio is a better screening tool than waist circumference and BMI for adult cardiometabolic risk factors: Systematic review and meta-analysis. Obes. Rev. 2012, 13, 275–286. [Google Scholar] [CrossRef] [PubMed]
- Baumgartner, R.N.; Koehler, K.M.; Gallagher, D.; Romero, L.; Heymsfield, S.B.; Ross, R.R.; Garry, P.J.; Lindeman, R.D. Epidemiology of sarcopenia among the elderly in New Mexico. Am. J. Epidemiol. 1998, 147, 755–763. [Google Scholar] [CrossRef] [PubMed]
- Exernet Network. Procedures and Questionnaires. Available online: http://www.spanishexernet.com/procedimientos.php/ (accessed on 18 February 2017).
- Elosua, R.; Marrugat, J.; Molina, L.; Pons, S.; Pujol, E. Validation of the Minnesota Leisure Time Physical Activity Questionnaire in Spanish men. The MARATHOM Investigators. Am. J. Epidemiol. 1994, 139, 1197–1209. [Google Scholar] [CrossRef] [PubMed]
- Elosua, R.; Garcia, M.; Aguilar, A.; Molina, L.; Covas, M.I.; Marrugat, J. Validation of the Minnesota Leisure Time Physical Activity Questionnaire in Spanish Women. Investigators of the MARATDON Group. Med. Sci. Sports Exerc. 2000, 32, 1431–1437. [Google Scholar] [CrossRef] [PubMed]
- Oja, P.; Tuxworth, B.; Eurofit para Adultos. Test Europeo de Aptitud Física. Evaluación de la Aptitud Física en Relación con la Salud; Ministerio de Educación y Ciencia; Consejo Superior de Deportes: Madrid, Spain, 1998.
- Rikli, R.; Jones, C.J. Senior Fitness Test Manual; Human Kinetics: Champaign, IL, USA, 2001. [Google Scholar]
- Rikli, R.E.; Jones, C.J. Development and validation of criterion-referenced clinically relevant fitness standards for maintaining physical independence in later years. Gerontologist 2013, 53, 255–267. [Google Scholar] [CrossRef] [PubMed]
- Gómez, C.; Kohen, V.L.; Nogueira, T.L. Guía Visual de Alimentos y Raciones; EDIMSA: Madrid, Spain, 2007. [Google Scholar]
- Moreiras, O.; Carbajal, A.; Cabrera, L.; Cuadrado, C. Tablas de Composición de Alimentos, Guía de Prácticas, 17th ed.; Piramide: Madrid, Spain, 2015. [Google Scholar]
- Black, A.E. Critical evaluation of energy intake using the Goldberg cut-off for energy intake: Basal metabolic rate. A practical guide to its calculation, use and limitations. Int. J. Obes. Relat. Metab. Disord. 2000, 24, 1119–1130. [Google Scholar] [CrossRef] [PubMed]
- Kawamoto, R.; Ninomiya, D.; Kasai, Y.; Kusunoki, T.; Ohtsuka, N.; Kumagi, T.; Abe, M. Handgrip strength is associated with metabolic syndrome among middle-aged and elderly community-dwelling persons. Clin. Exp. Hypertens. 2016, 38, 245–251. [Google Scholar] [CrossRef] [PubMed]
- Ishii, S.; Tanaka, T.; Akishita, M.; Ouchi, Y.; Tuji, T.; Iijima, K.; Kashiwa Study Investigators. Metabolic syndrome, sarcopenia and role of sex and age: Cross-sectional analysis of Kashiwa cohort study. PLoS ONE 2014, 9, e112718. [Google Scholar] [CrossRef] [PubMed]
- Sayer, A.A.; Syddall, H.E.; Dennison, E.M.; Martin, H.J.; Phillips, D.I.; Cooper, C.; Byrne, C.D.; Hertfordshire Cohort. Grip strength and the metabolic syndrome: Findings from the Hertfordshire Cohort Study. QJM Int. J. Med. 2007, 100, 707–713. [Google Scholar] [CrossRef] [PubMed]
- Leong, D.P.; McKee, M.; Yusuf, S.; PURE Investigators. Population Muscle Strength Predicts Olympic Medal Tallies: Evidence from 20 Countries in the PURE Prospective Cohort Study. PLoS ONE 2017, 12, e0169821. [Google Scholar] [CrossRef] [PubMed]
- Fernández-Ballesteros, R.; Robine, J.M.; Walker, A.; Kalache, A. Active Aging: A Global Goal. Curr. Gerontol. Geriatr. Res. 2013, 2013, 298012. [Google Scholar] [CrossRef] [PubMed]
- Marcus, R.L.; Addison, O.; Kidde, J.P.; Dibble, L.E.; Lastayo, P.C. Skeletal muscle fat infiltration: Impact of age, inactivity, and exercise. J. Nutr. Health Aging 2010, 14, 362–366. [Google Scholar] [CrossRef] [PubMed]
- Shin, H.; Panton, L.B.; Dutton, G.R.; Ilich, J.Z. Relationship of Physical Performance with Body Composition and Bone Mineral Density in Individuals over 60 Years of Age: A Systematic Review. J. Aging Res. 2011, 2011, 191896. [Google Scholar] [CrossRef] [PubMed]
- Landi, F.; Calvani, R.; Cesari, M.; Tosato, M.; Martone, A.M.; Ortolani, E.; Savera, G.; Salini, S.; Sisto, A.N.; Picca, A.; et al. Sarcopenia: An overview on current definitions, diagnosis and treatment. Curr. Protein Pept. Sci. 2017. [Google Scholar] [CrossRef] [PubMed]
- Warburton, D.E.; Nicol, C.W.; Bredin, S.S. Health benefits of physical activity: The evidence. Can. Med. Assoc. J. 2006, 174, 801–809. [Google Scholar] [CrossRef] [PubMed]
- Shaw, B.A.; Spokane, L.S. Examining the association between education level and physical activity changes during early old age. J. Aging Health 2008, 20, 767–787. [Google Scholar] [CrossRef] [PubMed]
- Go, S.W.; Cha, Y.H.; Lee, J.A.; Park, H.S. Association between Sarcopenia, Bone Density, and Health-Related Quality of Life in Korean Men. Korean J. Fam. Med. 2013, 34, 281–288. [Google Scholar] [CrossRef] [PubMed]
- Volpato, S.; Bianchi, L.; Cherubini, A.; Landi, F.; Maggio, M.; Savino, E.; Bandinelli, S.; Ceda, G.P.; Guralnik, J.M.; Zuliani, G.; et al. Prevalence and clinical correlates of sarcopenia in community-dwelling older people: Application of the EWGSOP definition and diagnostic algorithm. J. Gerontol. A Biol. Sci. Med. Sci. 2014, 69, 438–446. [Google Scholar] [CrossRef] [PubMed]
- Humphreys, B.; Ruseski, J. An economic analysis of participation and time spent in physical activity. J. Econ. Anal. Policy 2011, 11, 1–38. [Google Scholar] [CrossRef]
- Farrell, L.; Shields, M.A. Investigating the economic and demographic determinants of sporting participation in England. J. R. Stat. Soc. Ser. A 2002, 165, 335–348. [Google Scholar] [CrossRef]
- Alexandre Tda, S.; Duarte, Y.A.; Santos, J.L.; Wong, R.; Lebrão, M.L. Prevalence and associated factors of sarcopenia among elderly in Brazil: Findings from the SABE study. J. Nutr. Health Aging 2014, 18, 284–290. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.K.; Lee, J.A.; Kim, J.Y.; Kim, Y.Z.; Park, H.S. The risk factors of Sarcopenia among Korean Elderly Men: Based on 2009 Korean National Health and Nutrition Examination Survey Data. Korean J. Obes. 2014, 23, 23–31. [Google Scholar] [CrossRef]
- McGregor, R.A.; Cameron-Smith, D.; Poppitt, S.D. It is not just muscle mass: A review of muscle quality, composition and metabolism during ageing as determinants of muscle function and mobility in later life. Longev. Healthspan 2014, 3, 9. [Google Scholar] [CrossRef] [PubMed]
- Mithal, A.; Bonjour, J.; Dawson-Hughes, B.; IOF CSA Nutrition Working Group. Impact of nutrition on muscle mass, strength, and performance in older adults: Response to Scott and Jones. Osteoporos. Int. 2014, 25, 793. [Google Scholar] [CrossRef] [PubMed]
- Charlton, K.; Batterham, M.; Langford, K.; Lateo, J.; Brock, E.; Walton, K.; Lyons-Wall, P.; Eisenhauer, K.; Green, N.; McLean, C. Lean Body Mass Associated with Upper Body Strength in Healthy Older Adults While Higher Body Fat Limits Lower Extremity Performance and Endurance. Nutrients 2015, 7, 7126–7142. [Google Scholar] [CrossRef] [PubMed]
- Sarti, S.; Ruggiero, E.; Coin, A.; Toffanello, E.D.; Perissinotto, E.; Miotto, F.; Pintore, G.; Inelmen, E.M.; Manzato, E.; Sergi, G. Dietary intake and physical performance in healthy elderly women: A 3-year follow-up. Exp. Gerontol. 2013, 48, 250–254. [Google Scholar] [CrossRef] [PubMed]
- Drewnowski, A.; Shultz, J.M. Impact of aging on eating behaviors, food choices, nutrition, and health status. J. Nutr. Health Aging 2001, 5, 75–79. [Google Scholar] [PubMed]
- Alexandre Tda, S.; Duarte, Y.A.; Santos, J.L.; Wong, R.; Lebrão, M.L. Sarcopenia according to the European Working Group on Sarcopenia in Older People (EWGSOP) versus dynapenia as a risk factor for mortality in the elderly. J. Nutr. Health Aging 2014, 18, 751–756. [Google Scholar] [CrossRef] [PubMed]
- Lourenço, R.A.; Pérez-Zepeda, M.; Gutiérrez-Robledo, L.; García-García, F.J.; Rodríguez Mañas, L. Performance of the European Working Group on Sarcopenia in Older People algorithm in screening older adults for muscle mass assessment. Age Ageing 2015, 44, 334–338. [Google Scholar] [CrossRef] [PubMed]
- Vogel, L. Overweight or overfat? Many Canadians are both. Can. Med. Assoc. J. 2017, 189, E1202. [Google Scholar] [CrossRef] [PubMed]
- Gordon, S.A.; Fredman, L.; Orwig, D.L.; Alley, D.E. Comparison of methods to measure height in older adults. J. Am. Geriatr. Soc. 2013, 61, 2244–2246. [Google Scholar] [CrossRef] [PubMed]
- Schatzkin, A.; Kipnis, V.; Carroll, R.J.; Midthune, D.; Subar, A.F.; Bingham, S.; Schoeller, D.A.; Troiano, R.P.; Freedman, L.S. A comparison of a food frequency questionnaire with a 24-hour recall for use in an epidemiological cohort study: Results from the biomarker-based Observing Protein and Energy Nutrition (OPEN) study. Int. J. Epidemiol. 2003, 32, 1054–1062. [Google Scholar] [CrossRef] [PubMed]
- Freedman, L.S.; Potischman, N.; Kipnis, V.; Midthune, D.; Schatzkin, A.; Thompson, F.E.; Troiano, R.P.; Prentice, R.; Patterson, R.; Carroll, R.; et al. A comparison of two dietary instruments for evaluating the fat-breast cancer relationship. Int. J. Epidemiol. 2006, 35, 1011–1021. [Google Scholar] [CrossRef] [PubMed]
| Variable | N | Maximum HGS (kg) | Maximum 8-f TUG (s) | ||
|---|---|---|---|---|---|
| Men/Women | Men | Women | Men | Women | |
| Sociodemographics | |||||
| All | 176/204 | 37.2 (11.1) | 21.8 (6.0) | 4.6 (1.1) | 5.2 (1.0) |
| Age (years) | |||||
| <65 (men)/67 (women) | 83/96 | 40.9 (9.7) | 22.7 (5.4) | 4.4 (1.0) | 5.0 (1.2) |
| ≥65 (men)/67 (women) | 93/108 | 36.3 (9.0) | 20.3 (6.6) | 4.9 (1.1) | 5.3 (1.0) |
| p | <0.001 | 0.007 | <0.001 | 0.003 | |
| Marital status | |||||
| Married/Coupled | 153/130 | 37.2 (11.3) | 22.0 (5.9) | 4.7 (1.1) | 5.3 (1.1) |
| Single | 23/74 | 36.7 (7.8) | 21.5 (6.5) | 4.6 (1.3) | 5.2 (1.0) |
| p | 0.448 | 0.629 | 0.242 | 0.794 | |
| Educational level | |||||
| Primary | 61/100 | 36.5 (9.7) | 21.4 (6.3) | 4.9 (1.1) | 5.5 (1.1) |
| Secondary or college | 115/104 | 38.1 (11.0) | 22.2 (5.4) | 4.6 (1.1) | 5.0 (0.9) |
| p | 0.124 | 0.398 | 0.011 | <0.001 | |
| Income | |||||
| <900 € | 27/106 | 36.3 (13.4) | 21.9 (6.2) | 4.9 (1.3) | 5.4 (1.2) |
| ≥900 € | 149/98 | 37.4 (10.9) | 21.8 (5.9) | 4.6 (1.0) | 5.0 (0.9) |
| p | 0.253 | 0.662 | 0.040 | <0.001 | |
| Body composition | |||||
| BMI (kg/m2) | |||||
| <27.0 | 74/113 | 36.8 (13.0) | 21.4 (6.0) | 4.4 (1.1) | 5.1 (1.0) |
| ≥27.0 | 102/91 | 37.5 (9.6) | 22.5 (5.8) | 4.8 (0.9) | 5.4 (1.2) |
| p | 0.989 | 0.202 | 0.128 | 0.007 | |
| Overfat | |||||
| No | 59/83 | 41.1 (12.2) | 20.4 (6.4) | 4.3 (1.0) | 5.1 (0.8) |
| Yes | 117/121 | 36.7 (8.1) | 22.5 (5.6) | 4.8 (0.9) | 5.3 (1.2) |
| p | 0.063 | 0.143 | <0.001 | 0.010 | |
| Abdominal obesity | |||||
| No | 23/62 | 43.3 (10.2) | 20.2 (6.3) | 4.2 (0.9) | 5.0 (0.7) |
| Yes | 153/142 | 36.9 (10.5) | 22.4 (5.9) | 4.7 (1.0) | 5.3 (1.0) |
| p | 0.017 | 0.140 | <0.001 | 0.002 | |
| Lifestyle variables | |||||
| Smoking habit | |||||
| Non-smoker | 161/191 | 37.2 (11.3) | 21.7 (5.5) | 4.6 (1.1) | 5.2 (1.0) |
| Smoker | 15/13 | 37.4 (9.6) | 22.9 (6.4) | 4.7 (1.3) | 5.2 (1.7) |
| p | 0.836 | 0.216 | 0.717 | 0.652 | |
| LTPA | |||||
| Inactive | 66/92 | 35.6 (6.2) a,b | 20.9 (6.2) | 5.0 (1.0) a,b | 5.5 (1.1) a,b |
| Slightly active | 43/59 | 38.7 (10.7) | 22.1 (6.3) | 4.4 (1.0) | 5.2 (0.9) |
| Active | 67/53 | 40.9 (10.2) | 22.4 (5.5) | 4.4 (1.0) | 4.8 (1.1) |
| p | 0.001 | 0.310 | <0.001 | <0.001 | |
| Variables | Maximum HGS | Maximum 8-f TUG | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| n | Normal | Low | p | Crude OR (95% CI) † | Sex- and/or Age-Adjusted OR (95% CI) ‡ | Normal | High | p | Crude OR (95% CI) † | Sex- and/or Age-Adjusted OR (95% CI) ‡ | |
| Sociodemographics | |||||||||||
| All | 380 | 287 (75.5) | 93 (24.5) | 240 (63.2) | 140 (36.8) | ||||||
| Sex | |||||||||||
| Men | 176 | 158 (89.8) | 18 (10.2) | <0.001 | 1.00 (ref.) | 1.00 (ref.) | 128 (72.7) | 48 (27.3) | <0.001 | 1.00 (ref.) | 1.00 (ref.) |
| Women | 204 | 129 (63.2) | 75 (36.8) | 5.10 (2.90–8.98) | 4.59 (2.56–8.23) | 112 (54.9) | 92 (45.1) | 2.19 (1.42–3.37) | 2.38 (1.52–3.72) | ||
| Age (years) | |||||||||||
| <65/67 | 179 | 151 (84.4) | 28 (15.6) | <0.001 | 1.00 (ref.) | 1.00 (ref.) | 106 (59.2) | 73 (40.8) | 0.133 | 1.00 (ref.) | 1.00 (ref.) |
| ≥65/67 | 201 | 136 (67.7) | 65 (32.3) | 2.58 (1.56–4.25) | 2.85 (1.68–4.82) | 134 (66.7) | 67 (33.3) | 0.73 (0.48–1.10) | 0.72 (0.47–1.10) | ||
| Marital status | |||||||||||
| Married/Coupled | 283 | 224 (79.2) | 59 (20.8) | 0.005 | 1.00 (ref.) | 1.00 (ref.) | 180 (63.6) | 103 (36.4) | 0.758 | 1.00 (ref.) | 1.00 (ref.) |
| Single | 97 | 63 (64.9) | 34 (35.1) | 2.05 (1.24–3.40) | 1.08 (0.61–1.91) | 60 (61.9) | 37 (38.1) | 1.08 (0.67–1.73) | 0.90 (0.54-1.49) | ||
| Educational level | |||||||||||
| Primary | 161 | 119 (73.9) | 42 (26.1) | 0.531 | 1.00 (ref.) | 1.00 (ref.) | 83 (51.6) | 78 (48.4) | <0.001 | 1.00 (ref.) | 1.00 (ref.) |
| Secondary or college | 219 | 168 (76.7) | 51 (23.3) | 0.86 (0.54–1.38) | 1.22 (0.73–2.05) | 157 (71.7) | 62 (28.3) | 0.42 (0.27–0.64) | 0.43 (0.27–0.66) | ||
| Income | |||||||||||
| <900 € | 133 | 89 (66.9) | 44 (33.1) | 0.004 | 1.00 (ref.) | 1.00 (ref.) | 65 (48.9) | 68 (51.1) | <0.001 | 1.00 (ref.) | 1.00 (ref.) |
| ≥900 € | 247 | 198 (80.2) | 49 (19.8) | 0.50 (0.31–0.81) | 1.00 (0.58–1.71) | 175 (70.9) | 72 (29.1) | 0.39 (0.25–0.61) | 0.44 (0.27–0.71) | ||
| Body composition | |||||||||||
| BMI (kg/m2) | |||||||||||
| <27.0 | 185 | 128 (69.2) | 57 (30.8) | 0.005 | 1.00 (ref.) | 1.00 (ref.) | 124 (67.0) | 61 (33.0) | 0.128 | 1.00 (ref.) | 1.00 (ref.) |
| ≥27.0 | 195 | 159 (81.5) | 36 (18.5) | 0.51 (0.32–0.82) | 0.59 (0.35–1.00) | 116 (59.5) | 79 (40.5) | 1.38 (0.91–2.11) | 1.61 (1.04–2.49) | ||
| Overfat | |||||||||||
| No | 142 | 98 (69.0) | 44 (31.0) | 0.023 | 1.00 (ref.) | 1.00 (ref.) | 99 (69.7) | 43 (30.3) | 0.041 | 1.00 (ref.) | 1.00 (ref.) |
| Yes | 238 | 189 (79.4) | 49 (20.6) | 0.58 (0.36–0.93) | 0.58 (0.34–0.98) | 141 (59.2) | 97 (40.8) | 1.58 (1.02–2.46) | 1.72 (1.10–2.72) | ||
| Abdominal obesity | |||||||||||
| No | 85 | 55 (64.7) | 30 (35.3) | 0.008 | 1.00 (ref.) | 1.00 (ref.) | 66 (77.6) | 19 (22.4) | 0.002 | 1.00 (ref.) | 1.00 (ref.) |
| Yes | 295 | 232 (78.6) | 63 (21.4) | 0.50 (0.30–0.84) | 0.57 (0.31–1.03) | 174 (59.0) | 121 (41.0) | 2.42 (1.38–4.23) | 3.38 (1.87–6.09) | ||
| Lifestyle variables | |||||||||||
| Smoking habit | |||||||||||
| Non–smoker | 352 | 263 (74.7) | 89 (25.3) | 0.193 | 1.00 (ref.) | 1.00 (ref.) | 222 (63.1) | 130 (36.9) | 0.898 | 1.00 (ref.) | 1.00 (ref.) |
| Smoker | 28 | 24 (85.7) | 4 (14.3) | 0.49 (0.17–1.46) | 0.61 (0.19–1.95) | 18 (64.3) | 10 (35.7) | 0.95 (0.43–2.12) | 0.97 (0.43–2.19) | ||
| LTPA | |||||||||||
| Inactive | 158 | 112 (70.9) | 46 (29.1) | 0.076 | 1.00 (ref.) | 1.00 (ref.) | 77 (48.7) | 81 (51.3) | <0.001 | 1.00 (ref) | 1.00 (ref.) |
| Slightly active/Active | 222 | 175 (78.8) | 47 (21.2) | 0.65 (0.41–1.05) | 0.79 (0.47–1.32) | 163 (73.4) | 59 (26.6) | 0.34 (0.22–0.53) | 0.33 (0.21–0.52) | ||
| Variables | Maximum HGS | Maximum 8-f TUG | ||||
|---|---|---|---|---|---|---|
| Normal (n = 287) | Low (n = 93) | p | Normal (n = 240) | High (n = 140) | p | |
| All (n = 380) | ||||||
| Energy intake (kcal/day) | 1679 (1394–2046) | 1547 (1269–1833) | 0.007 | 1708 (1394–2043) | 1559 (1277–1844) | 0.004 |
| Carbohydrate intake (% total energy) | 44.7 (38.2–50.0) | 47.3 (41.5–53.6) | 0.003 | 44.9 (38.0–50.0) | 46.6 (40.3–51.4) | 0.201 |
| Protein intake (% total energy) | 16.0 (14.2–18.6) | 16.1 (13.4–19.0) | 0.738 | 16.2 (14.4–18.7) | 15.8 (13.2–18.8) | 0.149 |
| Fat intake (% total energy) | 35.0 (30.0–40.0) | 32.5 (28.6–37.6) | 0.025 | 34.3 (29.8–39.8) | 34.0 (29.4–38.6) | 0.520 |
| PUFA (% total energy) | 4.2 (3.5–5.1) | 4.2 (3.5–5.7) | 0.369 | 4.3 (3.5–5.4) | 4.1 (3.3–5.0) | 0.084 |
| MUFA (% total energy) | 16.0 (13.4–18.6) | 14.0 (12.3–16.9) | 0.001 | 15.8 (13.2–18.6) | 15.1 (12.7–17.8) | 0.254 |
| SFA (% total energy) | 10.0 (8.2–12.5) | 9.6 (7.3–11.2) | 0.058 | 9.8 (8.0–12.0) | 10.1 (8.1–11.9) | 0.600 |
| Cholesterol intake (mg/1000 kcal) | 261.9 (177.4–383.9) | 211.1 (127.3–309.6) | 0.054 | 253.8 (170.4–384.2) | 245.7 (160.5–356.5) | 0.993 |
| Fiber intake (g/1000 kcal) | 65.6 (51.2–82.5) | 58.7 (45.3–71.2) | 0.006 | 64.5 (51.3–82.3) | 60.5 (45.1–78.1) | 0.625 |
| Men (n = 176) | n = 158 | n = 18 | n = 128 | n = 48 | ||
| Energy intake (kcal/day) | 1926 (1579–2255) | 1789 (1527–1892) | 0.068 | 1914 (1606–2202) | 1817 (1507–2265) | 0.528 |
| Carbohydrate intake (% total energy) | 43.8 (37.8–49.6) | 43.6 (34.5–53.4) | 0.914 | 44.2 (37.6–49.7) | 43.6 (38.5–50.2) | 0.847 |
| Protein intake (% total energy) | 15.7 (13.9–18.2) | 16.0 (14.1–19.7) | 0.461 | 15.9 (14.3–18.5) | 14.9 (12.9–18.2) | 0.092 |
| Fat intake (% total energy) | 34.8 (29.8–39.6) | 32.5 (29.6–40.8) | 0.907 | 34.1 (29.6–39.6) | 35.6 (31.2–40.1) | 0.361 |
| PUFA (% total energy) | 4.3 (3.5–5.1) | 5.0 (3.6–6.3) | 0.160 | 4.3 (3.5–5.3) | 4.2 (3.6–5.0) | 0.515 |
| MUFA (% total energy) | 16.1 (13.5–18.3) | 14.9 (12.9–18.3) | 0.646 | 16.0 (13.2–18.3) | 16.0 (13.8–18.3) | 0.740 |
| SFA (% total energy) | 10.2 (8.2–12.5) | 9.5 (7.3–11.6) | 0.470 | 9.8 (7.8–12.2) | 10.6 (8.9–13.1) | 0.059 |
| Cholesterol intake (mg/1000 kcal) | 149.6 (101.7–210.7) | 193.4 (94.1–277.3) | 0.372 | 141.2 (101.1–205.9) | 158.0 (102.6–220.5) | 0.570 |
| Fiber intake (g/1000 kcal) | 9.4 (7.2–12.2) | 10.2 (7.9–13.8) | 0.449 | 9.8 (7.6–12.7) | 8.5 (6.8–10.1) | 0.040 |
| Women (n = 204) | n = 129 | n = 75 | n = 112 | n = 92 | ||
| Energy intake (kcal/day) | 1456 (1236–1721) | 1515 (1235–1820) | 0.486 | 1463 (1286–1774) | 1486 (1193–1735) | 0.525 |
| Carbohydrate intake (% total energy) | 46.3 (38.5–51.1) | 48.3 (43.4–54.0) | 0.018 | 46.3 (38.9–51.3) | 47.4 (41.4–52.8) | 0.265 |
| Protein intake (% total energy) | 16.7 (14.5–19.5) | 16.1 (13.3–18.7) | 0.155 | 16.7 (14.6–19.1) | 16.1 (13.4–19.1) | 0.374 |
| Fat intake (% total energy) | 35.2 (30.3–40.3) | 32.5 (28.5–36.8) | 0.016 | 34.7 (30.2–40.2) | 33.6 (29.0–37.7) | 0.147 |
| PUFA (% total energy) | 4.1 (3.4–5.2) | 4.2 (3.4–5.3) | 0.700 | 4.3 (3.5–5.5) | 4.0 (3.3–5.1) | 0.106 |
| MUFA (% total energy) | 15.8 (13.4–18.7) | 13.7 (12.2–16.5) | 0.001 | 15.6 (13.2–18.6) | 14.7 (12.4–17.2) | 0.132 |
| SFA (% total energy) | 10.0 (8.3–12.1) | 9.6 (7.3–11.2) | 0.158 | 9.9 (8.2–11.5) | 9.8 (7.7–11.2) | 0.567 |
| Cholesterol intake (mg/1000 kcal) | 159.6 (119.6–232.0) | 123.2 (91.4–179.6) | 0.004 | 147.0 (111.0–202.2) | 142.3 (92.9–227.1) | 0.613 |
| Fiber intake (g/1000 kcal) | 10.9 (8.5–13.6) | 11.1 (9.6–14.4) | 0.159 | 11.1 (9.0–13.3) | 10.6 (9.0–14.5) | 0.779 |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bibiloni, M.d.M.; Karam, J.; Bouzas, C.; Aparicio-Ugarriza, R.; Pedrero-Chamizo, R.; Sureda, A.; González-Gross, M.; Tur, J.A. Association between Physical Condition and Body Composition, Nutrient Intake, Sociodemographic Characteristics, and Lifestyle Habits in Older Spanish Adults. Nutrients 2018, 10, 1608. https://doi.org/10.3390/nu10111608
Bibiloni MdM, Karam J, Bouzas C, Aparicio-Ugarriza R, Pedrero-Chamizo R, Sureda A, González-Gross M, Tur JA. Association between Physical Condition and Body Composition, Nutrient Intake, Sociodemographic Characteristics, and Lifestyle Habits in Older Spanish Adults. Nutrients. 2018; 10(11):1608. https://doi.org/10.3390/nu10111608
Chicago/Turabian StyleBibiloni, Maria del Mar, Joanne Karam, Cristina Bouzas, Raquel Aparicio-Ugarriza, Raquel Pedrero-Chamizo, Antoni Sureda, Marcela González-Gross, and Josep A. Tur. 2018. "Association between Physical Condition and Body Composition, Nutrient Intake, Sociodemographic Characteristics, and Lifestyle Habits in Older Spanish Adults" Nutrients 10, no. 11: 1608. https://doi.org/10.3390/nu10111608
APA StyleBibiloni, M. d. M., Karam, J., Bouzas, C., Aparicio-Ugarriza, R., Pedrero-Chamizo, R., Sureda, A., González-Gross, M., & Tur, J. A. (2018). Association between Physical Condition and Body Composition, Nutrient Intake, Sociodemographic Characteristics, and Lifestyle Habits in Older Spanish Adults. Nutrients, 10(11), 1608. https://doi.org/10.3390/nu10111608








